SUMMARY
To date many studies have measured the effect of key child survival interventions on the main cause of mortality while anecdotally reporting effects on all-cause mortality. We conducted a systematic literature review and abstracted cause-specific and all-cause mortality data from included studies. We then estimated the effect of the intervention on the disease of primary interest and calculated the additional deaths prevented (i.e. the indirect effect). We calculated that insecticide-treated nets have been shown to result in a 12% reduction [95% confidence interval (CI) 0·0–23] among non-malaria deaths. We found pneumonia case management to reduce non-pneumonia mortality by 20% (95% CI 8–22). For measles vaccine, seven of the 10 studies reporting an effect on all-cause mortality demonstrated an additional benefit of vaccine on all-cause mortality. These interventions may have benefits on causes of death beyond the specific cause of death they are targeted to prevent and this should be considered when evaluating the effects of implementation of interventions.
Key words: Child survival, indirect effects, interventions, INTs, malaria, pneumonia case management, measles vaccine, ORS
INTRODUCTION
Although child mortality rates are continuing to decline globally, there are still more than 8 million children who die each year before reaching their fifth birthday [1]. Infectious diseases, including diarrhoea, pneumonia, and malaria remain the leading causes of death despite simple and effective interventions for each of the main causes of child mortality [2]. The Child Health Epidemiology Reference Group (CHERG) recently reviewed the scientific evidence for all key child survival interventions and estimated the effect size for each intervention on cause-specific mortality [3].
Child survival interventions are often thought of as acting on one infection and one cause of death (COD), e.g. insecticide-treated nets (ITNs) prevent malaria infections and thus malaria deaths. However, for many years it has been noted that selected child survival interventions appear to benefit more than the targeted disease. Extensive literature reviews and effect-size estimates for interventions such as ITNs and malaria case management, case management of pneumonia, oral rehydration solution (ORS) for diarrhoea, and measles vaccine have been published [4–8]. Analyses have also attempted to predict the impact of malaria intervention scale-up on all-cause mortality, under various assumptions of the burden of indirect malaria mortality [9]. We sought to go beyond these published reviews and analyses to quantify the benefit of selected interventions on: (1) disease-specific mortality for the disease targeted by the intervention (i.e. the direct effect), and (2) disease-specific mortality for diseases not targeted by the intervention or all-cause mortality (i.e. the indirect effect). Our estimates are based on data from published intervention studies.
METHODS
Identification and selection of studies
We conducted a systematic search in PubMed and Cochrane Library databases for studies published to the end of 2009 (Supplementary online Appendix). We searched without restrictions on year or study design including randomized controlled studies, observational studies, community studies, case-control, pre- vs. post-intervention comparisons, and natural experiments according to the CHERG standards for systematic reviews [3].
For malaria interventions we used the following key words and MeSH terms in various combinations: malaria, chemoprophylaxis, treatment, ITN, and child mortality. For pneumonia case management we used the following key words and MeSH terms in various combinations: pneumonia, case management, and child mortality. For oral rehydration solution we used the following key words and MeSH terms in various combinations: diarrhoea, dysentery, fluid therapy, oral rehydration solution, and oral rehydration therapy and child mortality. We included only studies where ORS was compared to intravenous fluids or no treatment, excluding studies that used different ORS formulations in the comparison arm. Because ORS is relatively widespread and contamination of the comparison arm is a concern in ORS studies, we excluded studies that did not adequately describe the coverage levels achieved in the intervention and comparison arms, and studies where there was little difference in coverage between intervention and comparison arms. For measles vaccine we used the following key words and MeSH terms in various combinations: measles, measles vaccine or vaccination, and child mortality. We included only studies evaluating the standard medium-titre measles vaccine as the main intervention with either concurrent controls or historical comparisons. We screened all titles and abstracts and the full articles of papers meeting all inclusion and exclusion criteria based on abstract review. Studies were also identified by hand searching the reference lists of retrieved articles. Studies that met the above criteria and that reported the effect of the intervention on all-cause mortality or on causes other than those the intervention was intended to impact were double-abstracted into a database. Studies conducted in special populations, adults, or high-income settings, and thus not generalizable to children in low- and middle-income settings, were excluded. We also excluded cohort and quasi-experimental studies including pre-post study designs that did not control for confounding.
We verified that each study was represented only once in the database: in cases where our searches found multiple publications for a single study, data from all the publications were abstracted into a single row to avoid double counting. Variables abstracted included the study setting, design, population, definition of the intervention, co-interventions, mortality rates, effect sizes for all-cause and cause-specific mortality, and confounders adjusted for in the analysis. For the pneumonia case-management studies, we were able to obtain and abstract all-cause and pneumonia-specific mortality data from the unpublished data tables for a previously published meta-analysis [10], to supplement the information available from the published reports of the studies (Tables 1, 3, 5, 7). In all other cases, we relied on published data.
Table 1.
Insecticide treated nets: characteristics of included studies
| Study identifiers, context, and population | Study design and limitations | |||||||
|---|---|---|---|---|---|---|---|---|
| Study (first-named author, year of publication) | Country | Study years | Study population | Study design | Sample size and number of total clusters | Ascertainment of deaths | Co-interventions | Intervention coverage in ITN arm |
| Studies with all-cause data | ||||||||
| Phillips-Howard, 2003 [20] | Kenya | 1997–99 | 1–59 mo. | Cluster RCT | 18 500 children, 221 clusters | Bi-yearly census | None | 66% (direct observation) |
| Habluetzel, 1997 [18] | Burkina Faso | 1994–96 | 6–59 mo. | Cluster RCT | 16 540 children, 16 clusters | Yearly census, DSS rounds every 3 weeks | None | 59–78% (direct observation) |
| Nevill, 1996 [19] | Kenya | 1993–95 | 1–59 mo. | Cluster RCT | 22 998 children, 56 clusters | Bi-yearly census, vital registration visits every 6–8 weeks | None | 65% in dry season; 77% in rainy season (direct observation) |
| Fegan, 2007 [17] | Kenya | 2005–06 | 1–59 mo. | Prospective cohort | 6507·6 child-yr; 3484 children | Yearly census | ACT introduced 3rd quarter 2006 (coverage 1·3% in Aug. 2006) | 67% (reported) at endline |
| Schellenberg, 2001 [21] | Tanzania | 1997–2000 | 1–59 mo. | Case-control | 423 cases, 1911 controls | Cases and age-matched controls identified from DSS; 3-month recall for exposure | None | 44–49% (reported) |
| Studies with cause-specific data | ||||||||
| Binka, 1996 [15] | Ghana | 1993–95 | 6–59 mo. | Cluster RCT | 19 900 children, 96 clusters | Bi-yearly census, DSS visits every 3 mo., birth/death registration by key informants, VA (recall 3 mo.) | None | 50–97% (range across seasons and years) |
| D'Alessandro, 1995 [16] | The Gambia | 1992–93 | 1–9 yr | Matched cluster RCT | 18 911 children, 104 clusters | Yearly census, DSS (frequency NR), VA (recall NR) | None | 67% |
ACT, Artemisinin-based combination therapy; DSS, demographic surveillance site; ITN, insecticide-treated net; RCT, randomized controlled trial; VA, verbal autopsy.
Table 3.
Malaria case management: characteristics of included studies
| Study identifiers, context, and population | Study design and limitations | |||||||
|---|---|---|---|---|---|---|---|---|
| Study (first-named author, year of publication) | Country | Study years | Study population | Study design | Sample size and number of total clusters | Ascertainment of deaths | Co-interventions | Intervention coverage |
| Studies with all-cause data | ||||||||
| Kidane, 2000 [22] | Ethiopia | 1997 | 0–59 mo. | Cluster-matched RCT | 13 677 children, 24 clusters | VA reported by study coordinators | None | NR |
| Menon, 1990 [23] | The Gambia | 1985–89 | 3–59 mo. | Cluster, but not randomized | 41 villages | VA reported by a physician | No | 60% received maloprim chemoprophylaxis, chloroquine coverage not reported |
NR, Not reported; RCT, randomized controlled trial; VA, verbal autopsy.
Table 5.
Pneumonia case management: characteristics of included studies
| Study identifiers, context, and population | Study design and limitations | |||||||
|---|---|---|---|---|---|---|---|---|
| Study (first-named author, year of publication) | Country | Study years | Age of study population | Study design | Sample size and total number of clusters | Ascertainment of deaths | Co- interventions | Intervention coverage |
| Studies with cause-specific data | ||||||||
| Mtango, 1986 [28] | Tanzania | 1983–85 | 0–59 mo. | Cluster RCT | 16 126 children, 16 clusters | Reporting by VHWs, yearly census, VA (2 wk recall) | None | NR |
| Pandey, 1991 [29] | Nepal | 1984–87 | 0–59 mo. | Step wedge | 2393 children, number of clusters unclear | Village-based registration with vital events confirmed by interviewers, VA (1 month recall) | None | 0·85 antibiotic treatments per child-yr |
| Fauveau, 1992 [25] | Bangladesh | 1988–89 | 0–59 mo. | Quasi- experimental | 31 632 children, 2 units of analysis | DSS, reporting by CHWs, VA | Diarrhoea management, EPI | NR |
| Bang, 1990 [24] | India | 1988–89 | 0–59 mo. | Quasi- experimental | 10 122 children, 2 units of analysis | Reporting by VHWs, bi-yearly census, VA | None | 76%, calculated based on expected number of pneumonia cases |
| Khan, 1990 [26] | Pakistan | 1985–86 | 0–59 mo. | Quasi- experimental | 4978 children, 38 clusters | Yearly census, active surveillance by CHWs in intervention area, quarterly census in comparison area, VA | Maternal health education | NR |
| Studies with all-cause data | ||||||||
| Kielmann, 1978 [27] | India | 1970–72 | 0–59 mo. | Quasi- experimental | 2735 children, 10 clusters | Vital registration via CHW reports, bi-monthly visits to key informants, registration by key informants | None | NR |
CHWs, Community health workers; DSS, demographic surveillance site; EPI, expanded programme on immunizations; NR, not reported; VA, verbal autopsy; VHWs, village health workers.
Table 7.
Measles vaccine: characteristics of included studies
| Study identifiers, context, and population | Study design and limitations | |||||||
|---|---|---|---|---|---|---|---|---|
| First-named author, year of publication | Country | Study years | Study population | Study design | Sample size and number of clusters | Ascertainment of deaths | Co-interventions | Measles vaccine coverage |
| All-cause data | ||||||||
| Aaby, 2006 [47] | Malawi | 1997–2002 | 6–60 mo. | Cohort | 751 children | Monthly home visits (0–18 mo.), quarterly home visits (>18 mo.) | Nutritional surveillance | 12 mo: 64% 24 mo: 81% |
| Elguero, 2005 [48] | Senegal | 1997–99 | 0–23 mo. | Cohort | 4114 children | Quarterly home visits | None | 20% |
| Lehmann, 2005 [44] | Papua New Guinea | 1989–95 | 1–23 mo. | Cohort | 3113 children | Monthly home visits | Pneumococcal vaccine study | 12 mo: 74% |
| Breiman, 2004 [40] | Bangladesh | 1986–2001 | 9–60 mo. | Cohort | 36 650 children | DSS | Enhanced MCH services | 9 mo: 83% 60 mo: 98% |
| Nyarko, 2001 [50] | Ghana | 1994–99 | 9–59 mo. | Cohort | Total sample size 17 701, sample included in this analysis is unclear | Quarterly home visits | Community-based delivery of PHC in about 60% of study area | 12 mo: 25 |
| Kristensen, 2000 [43] | Guinea Bissau | 1990–96 | 7–19 mo. | Cohort | 3414 children | Home visits every 5–7 mo. | None | 12 mo: 38% 18 mo: 77% |
| Aaby, 1990 [46] | Guinea Bissau | 1984–87 | 4–30 mo. | Cohort | 722 children | 50% of study area received monthly home visits; Other 50% received visits every 3–5 mo. | None | 12–23 mo: 81% (district 1), 61% (district 2) |
| Kabir, 2003, Kumar, 2000 [42, 49] | India (Haryana) | 1991–98 | 12–59 mo. | Case control | 636 children | Home visits (frequency not recorded) with 20% of data verified annually, annual census | None | NA |
| Velema, 1991 [45] | Benin | 1986–87 | 4–35 mo. | Case control | 294 children | 4 demographic surveys | ARI, malaria and diarrhoea CCM; deworming; IPTi | NA |
| Holt, 1990 [41] | Haiti | 1982–85 | 9–44 mo. | Case control | 1291 children | Census | None | NA |
| Cause-specific data | ||||||||
| Aaby, 2003 [51]; Koenig, 1990 [53]; Clemens, 1988 [52] | Bangladesh | 1982–85 | 10–60 mo. | Cohort | 16 268 children | Bi-monthly home visits, completion of cause of death form | Enhanced MCH services | >60% |
ARI, Acute respiratory infection; CCM, community case management; DSS, demographic surveillance site; IPTi, intermittent preventive treatment of malaria in infants; MCH, maternal and child health; NA, not applicable; PHC, primary health care.
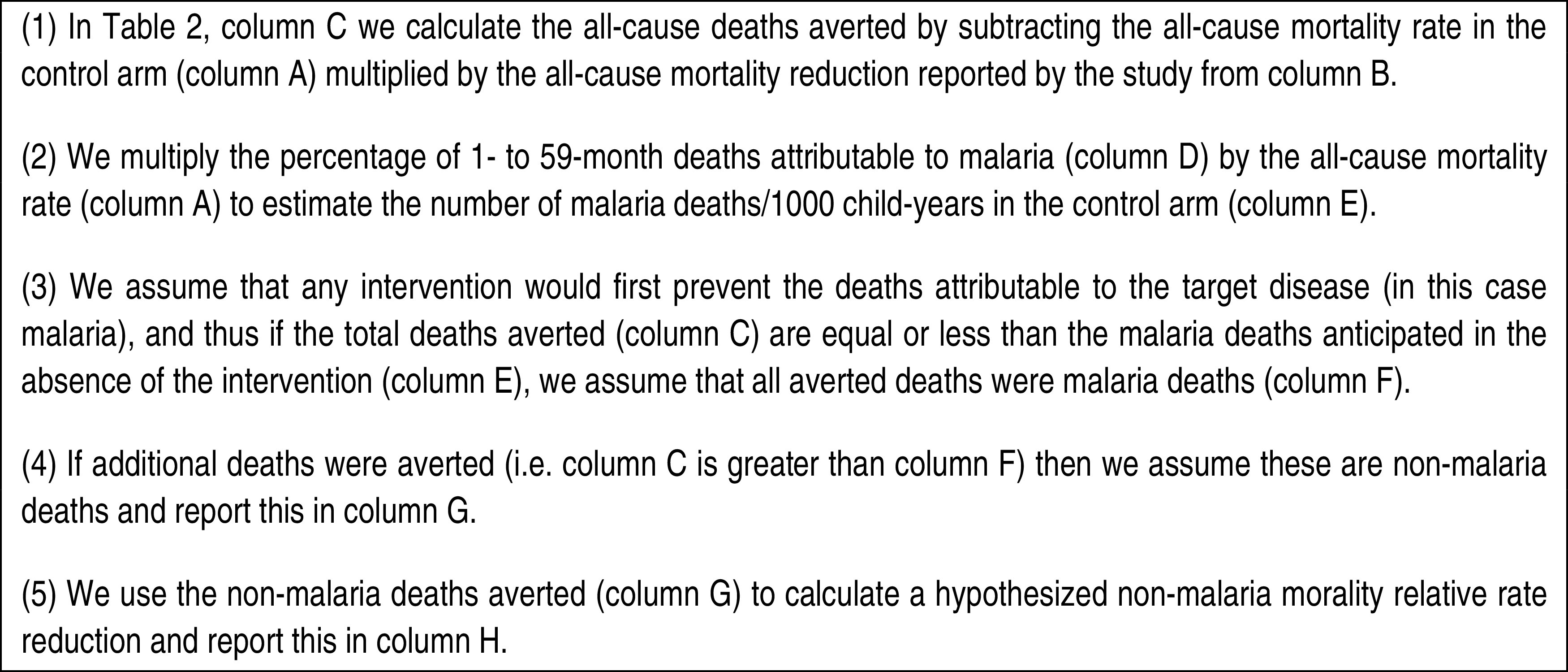
Analytical methods
We used the same analytical techniques for each of the interventions. As this approach contains numerous steps, we provide a detailed example for a malaria study in Fig. 1; this method was used for all interventions, with the modifications described below. For studies reporting only the effect of the intervention on all-cause mortality, we estimated the all-cause deaths averted (per 1000 child-years or live births, as appropriate) by the intervention by multiplying the baseline or comparison mortality rate by the study all-cause mortality relative rate reduction or hazard ratio. We then assumed that the intervention prevented deaths attributable to the targeted COD first (i.e. ITNs would prevent all malaria deaths before preventing deaths from other causes). Where possible, we abstracted the proportion of deaths by cause reported in the paper for the control/baseline group. If no COD data were reported in the study, if COD data were not disaggregated by intervention and comparison group, or if COD definitions or verbal autopsy methods were not clearly described, we used the country-, age-, and year-specific COD profiles from the Lives Saved Tool (LiST) to estimate the proportion of deaths from the targeted cause. The LiST tool uses peer-reviewed COD estimates that have undergone extensive review by CHERG and country consultation [2, 11–13]. In the case of measles vaccine, where the vaccine is very effective and coverage levels are generally high, we modelled the country-specific COD profile in LiST, setting the measles vaccine coverage to 0%, to simulate a counterfactual population for which measles vaccine was not available. We calculated the anticipated number of deaths in the control/baseline group for the targeted COD by multiplying the all-cause mortality rate in the control/baseline group by the reported or modelled proportion for that COD (Tables 2, 4, 6, 8). We then compared the all-cause deaths averted by the intervention with the estimated number of deaths from the targeted COD in the control/baseline group and calculated the excess deaths averted. We attributed all excess deaths averted to the indirect effects of the intervention. If there were no excess deaths averted, i.e. the all-cause deaths averted were less than the deaths expected from the targeted cause we assumed that the intervention had no indirect effect on mortality in that particular study; all deaths averted were from the targeted cause.
Fig. 1.
Method of calculating cause-specific and all-cause deaths averted: the example of malaria.
Table 2.
Indirect effects of ITNs estimated from studies reporting all-cause mortality
| Study (first-named author, year of publication) | A | B | C | D | E | F | G | H |
|---|---|---|---|---|---|---|---|---|
| All-cause MR in control arm | Study reported all-cause mortality reduction (all-cause MR in ITN arm)/ (all-cause MR in control arm) | All-cause deaths averted by intervention/ 1000 child-yr [A*(1 – B)] | % 1–59 month deaths attributable to malaria | Assumed malaria deaths in control arm/ 1000 child-yr [A*D] | Assumed malaria deaths averted by intervention/ 1000 child-yr [if E < C, E, else C] | Assumed non-malaria deaths averted by intervention/ 1000 child-yr [if E < C, C − F, else none] | Non-malaria mortality relative rate [if E < C, (A*(1 − D) – G)/ (A*(1 − D)), else none] | |
| Cluster RCT | ||||||||
| Phillips-Howard, 2003 [20] | 51·9/1000 child-yr | 0·84 (0·75–0·94) | 8·30 | 26·7% (Alex Rowe, personal communication) | 13·86 | 8·30 | None | None |
| Habluetzel, 1997 [18] | 38·2/1000 child-yr | 0·85 (0·70–1·04) | 5·73 | 28 (1995)a | 10·7 | 5·73 | None | None |
| Nevill, 1996 [19] | 13·2/1000 children | 0·70 (0·53–0·93) | 3·96 | 17 (1994)a | 2·24 | 2·24 | 1·72 | 0·84 |
| Binka, 1996 [15] | 27·9/1000 child-yr | 0·83 (0·69–0·97) | 4·74 | 36·1 (6–59 mo.) | 10·07 | 2·12b | 1·78 | 0·90 |
| D'Alessandro, 1995 [16] | 8·0/1000 child-yr | 0·79 | 1·66 | 46·7 (1–9 yr) | 3·74 | 0·52c | 1·24 | 0·71 |
| Cohort | ||||||||
| Fegan, 2007 [17] | 16·1/1000 child-yr among non-users of ITNs | 0·56 (0·33–0·96) | 7·08 | 19 (2006)a | 3·06 | 3·06 | 4·03 | 0·69 |
| Case-control | ||||||||
| Schellenberg, 2001 [21] | 86·2/1000 live births pre- intervention | 0·73 (0·55–0·97) | 23·27 | 31 (2000–2003)a | 26·72 | 23·27 | None | None |
ITN, Insecticide-treated net; MR, mortality rate; RCT, randomized control trial.
Study did not report percent of deaths attributable to malaria. Estimate abstracted from LiST with year of estimate given.
Study reported malaria-specific relative mortality reduction of 0·79 was used to calculate the malaria deaths averted.
Study reported malaria-specific relative mortality reduction of 0·86 was used to calculate the malaria deaths averted.
Table 4.
Indirect effects of malaria case management estimated from studies reporting all-cause mortality
| Study (first-named author, year of publication) | A | B | C | D | E | F | G | H |
|---|---|---|---|---|---|---|---|---|
| All-cause MR in control arm | Study reported all-cause mortality reduction (all-cause MR in ITN arm)/ (all-cause MR in control arm) | All-cause deaths averted by intervention/ 1000 child-yr [A*(1 – B)] | % under 5-yr-old deaths attributable to malaria (reported in control arm) | Assumed malaria deaths in control arm/1000 child-yr [A*D] | Assumed malaria deaths averted by intervention/ 1000 child-yr [if E < C, E, else C] | Assumed non-malaria deaths averted by intervention/ 1000 child-yr [if E < C, C − F, else none] | Non-malaria mortality relative rate [if E < C, (A*(1 – D) – G)/ (A*(1 – D)), else none] | |
| Quasi-experimental | ||||||||
| Kidane, 2000 [22] | 50·2/1000 child-yr | 0·59 (0·49–0·71) | 20·58 | 57 | 28·61 | 20·58 | None | NA |
| Menon, 1997 [23] | 49·7/1000 child-yr (for 3–59 mo.) | 0·52 | 23·86 | 19·2 | 9·54 | 9·54 | 14·32 | 0·64 |
ITN, Insecticide-treated net; MR, mortality rate; NA, not applicable.
Table 6.
Indirect effects of pneumonia case management estimated from studies reporting all-cause mortality
| Study (first-named author, year of publication) | A | B | C | D | E | F | G | H |
|---|---|---|---|---|---|---|---|---|
| All-cause MR in control arm | Study reported all-cause mortality reduction (all-cause MR in ITN arm)/ (all-cause MR in control arm) | All-cause deaths averted by intervention/ 1000 child-yr [A*(1 – B)] | % <5 deaths attributable to pneumonia (reported in control arm) | Assumed pneumonia deaths in control arm/ 1000 child-yr [A*D] | Assumed pneumonia deaths averted by intervention/ 1000 child-yr [if E < C, E else, C] | Assumed non-pneumonia deaths averted by intervention/ 1000 child-yr [if E < C, C − F, else none] | Non-pneumonia mortality relative rate [if E < C, (A*(1 − D) − G)/ (A*(1 − D)), else none] | |
| cRCT | ||||||||
| Mtango, 1986 [28] | 40·6/1000 children | 0·83 | 6·90 | 35 | 14·33 | 2·72a | 4·18 | 0·84 |
| Quasi-experimental | ||||||||
| Fauveau, 1992 [25] | 33·6/1000 child-yr | 0·61 | 13·104 | 20 | 5·95 | 2·91b | 9·78 | 0·64 |
| Bang, 1990 [24] | 41/1000 children | 0·69 | 12·71 | 43 | 11·64 | 6·29c | 3·22 | 0·86 |
| Khan, 1990 [26] | 39/1000 child-yr | 0·67 | 12·87 | 36 | 14·31 | 10·31d | 2·71 | 0·89 |
| Kielmann, 1978 [27] | 55/1000 child-yr | 0·58 | 23·10 | 25 | 12·21 | 12·21 | 9·54 | 0·77 |
| Step wedge | ||||||||
| Pandey, 1991 [29] | 81·4/1000 child-yr | 0·95 (0·80–1·12) | 4·07 | 16 | 17·26 | Nonee | 4·07 | 0·94 |
ITN, Insecticide-treated net; MR, mortality rate; cRCT, cluster randomized controlled trial.
Study reported pneumonia-specific relative mortality reduction of 0·81 was used to calculate the pneumonia deaths averted.
Study reported pneumonia-specific relative mortality reduction of 0·51 was used to calculate the pneumonia deaths averted.
Study reported pneumonia-specific relative mortality reduction of 0·46 was used to calculate the pneumonia deaths averted.
Study reported pneumonia-specific relative mortality reduction of 0·28 was used to calculate the pneumonia deaths averted.
Study reported pneumonia-specific relative mortality reduction of 1·07 was used to calculate the pneumonia deaths averted.
Table 8.
Indirect effects of measles vaccine estimated from studies reporting all-cause mortality
| Study (first-named author, year of publication) | A | B | C | D | E | F | G | H |
|---|---|---|---|---|---|---|---|---|
| All-cause MR in measles vaccine- negative children | Study reported all-cause mortality reduction (all-cause MR in ITN arm)/ (all-cause MR in control arm) | All-cause deaths averted by intervention per 1000 child-yr [A*(1 – B)] | % 1–59 mo. deaths attributable to measles (year of LiST estimate) | Assumed measles deaths in control arm/ 1000 child-yr [A*D] | Assumed measles deaths averted by intervention/ 1000 child-yr [if E < C, E, else, C] | Assumed non-measles deaths averted by intervention/1000 child-yr [if E < C, C − F, else, none] | Non-measles mortality relative rate [(A*(1 – D) – G)/ (A*(1 – D))]a | |
| Cohort | ||||||||
| Aaby, 2006 [47] | NR | 0·47 (0·19–1·14) | NA | 22 (1998) | NA | NA | NA | 0·60 |
| Elguero, 2005 [48] | 6·74/1000 child-yr | 0·87 (0·57–1·30) | 0·88 | 9 (1997) | 0·61 | 0·61 | 0·27 | 0·96 |
| Lehmann, 2005 [44] | NR | 0·94 (0·48–1·84) | NA | 32 (1992) | NA | NA | NA | 1·38 |
| Breiman, 2004 [40] | NR | HR = 0·93 (0·65–1·34) | NA | 9 (1994) | NA | NA | NA | 1·02 |
| Nyarko, 2001 [50] | NA | 0·50 (0·40–0·64) | NA | 12 (1996) | NA | NA | NA | 0·57 |
| Kristensen, 2000 [43] | 39·5/1000 children | 0·48 (0·27–0·87) | 20·54 | 10 (1993) | 3·95 | 3·95 | 16·59 | 0·53 |
| Aaby, 1990 [46] | NR | 0·34 (0·17–0·68) | NA | 10 (1986) | NA | NA | NA | 0·38 |
| Aaby, 2003 [51]; Koenig, 1990 [53]; Clemens, 1988 [52] | 25·5/1000 children | 0·55 (0·46–0·66) | 11·48 | 2b | 0·51 | 0·48c | 10·99 | 0·56 |
| Case-control | ||||||||
| Kabir, 2003 [42]; Kumar, 2000 [49] | NR | 0·36 (0·23–0·56) | NA | 7 (1994) | NA | NA | NA | 0·39 |
| Velema, 1991 [45] | NR | 0·67 (0·39–1·18) | NA | 8 (1985) | NA | NA | NA | 0·73 |
| Holt, 1990 [41] | 66·3/1000 children | 0·16 (0·04–0·63) | 55·69 | 16 (1985) | 10·61 | 10·61 | 45·08 | 0·19 |
ITN, Insecticide-treated net; MR, mortality rate; NA, not applicable; NR, not reported.
The formula simplifies to 1 – (1 – B)/D.
Study reported estimate of % measles deaths.
Study reported measles-specific relative mortality reduction of 0·05 was used to calculate the measles deaths averted.
For studies that reported intervention effect sizes for cause-specific mortality, we calculated the all-cause and cause-specific number of deaths assumed to have been averted by the intervention. The total number of all-cause deaths averted was calculated as described above. For the effect of the intervention on cause-specific mortality we multiplied the proportion of deaths in the control/baseline group from the targeted cause (as reported or from LiST) by the control/baseline mortality rate to calculate the total number of cause-specific deaths that the intervention theoretically could prevent. We then estimated the cause-specific deaths averted by the intervention by multiplying the cause-specific mortality relative rate reduction by the number of cause-specific deaths in the baseline/control group (Tables 2, 4, 6, 8). If the study-reported cause-specific mortality relative rate was >1, we assumed that the intervention averted no deaths from that cause, not that the intervention caused additional deaths.
If the difference between the total and cause-specific deaths averted was positive, these ‘excess deaths averted’ were attributed to the indirect effects of the intervention on other causes of mortality and a relative mortality rate for causes other than those targeted by the intervention was calculated or abstracted from the paper, where available. When at least three studies reported an effect on all-cause mortality, we performed fixed- and random-effects meta-analyses in Stata statistical software, version 11 [14]. If there was statistical evidence of heterogeneity or if the study settings or designs varied substantially, we reported the DerSimonian–Laird pooled relative risk and 95% confidence ntervals (CIs); in other cases we reported the Mantel–Haenszel pooled relative risk and 95% CIs. In the case of measles vaccine, where the study designs varied greatly and the estimates of the proportion of mortality due to measles were modelled resulting in a wide range of effect sizes, we did not compute a summary measure.
RESULTS
Malaria
We identified 1242 studies for screening in the initial review. After title, abstract, and review of the full papers, a total of seven ITN studies from five countries met our inclusion and exclusion criteria [15–21] (Table 1). Five studies reported the effect of ITNs on all-cause mortality [17–21] while two studies reported cause-specific reductions in malaria and non-malaria mortality [15, 16]. In Table 2 we estimate the malaria and non-malaria deaths averted in ITN studies that reported reductions in all-cause and cause-specific mortality.
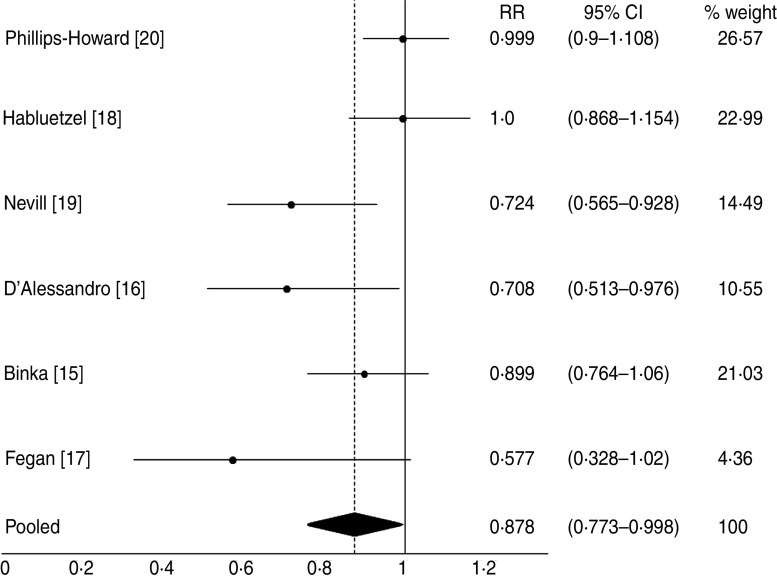
Of seven studies reporting effects of ITNs on all-cause or cause-specific mortality, four observed a reduction in all-cause deaths greater than what would be expected from reduction in malaria deaths alone ranging from 1·24 to 4·03 deaths averted/1000 child-years (Table 2). We included all seven studies in the random-effects meta-analysis and found a pooled non-malaria mortality relative rate of 0·878 (955 CI 0·773–0·998) of borderline statistical significance (P = 0·046), equivalent to a reduction of 12% in non-malaria mortality in children aged 1–59 months (Fig. 2). Among the studies that recorded reductions in other causes of death, Binka et al. [15] reported a non-significant increase in deaths from acute respiratory infection (ARI) in the ITN arm but a non-significant decrease in deaths from diarrhoea [15]. The effect of ITNs on diarrhoea may have averted 1·78 deaths/1000 child-years (data not shown).
Fig. 2.
Forest plot of ITN studies contributing to the random-effects meta-analysis.
We identified one study assessing the effects of malaria prophylaxis and of case management with chloroquine and one assessing the effect of case management alone on all-cause mortality [22, 23]; we did not find any studies reporting the effect of case management on causes of death other than malaria (Tables 3 and 4). In the study by Menon et al., we calculated that 14 non-malaria deaths/1000 child-years were averted by chloroquine chemoprophylaxis, which is equivalent to a 36% reduction in non-malaria deaths, relative to the control arm [23]. In the study by Kidane & Morrow [22], the effect on all-cause mortality was less than what would be expected had all malaria deaths been averted; thus we assumed no indirect effect on non-malaria deaths.
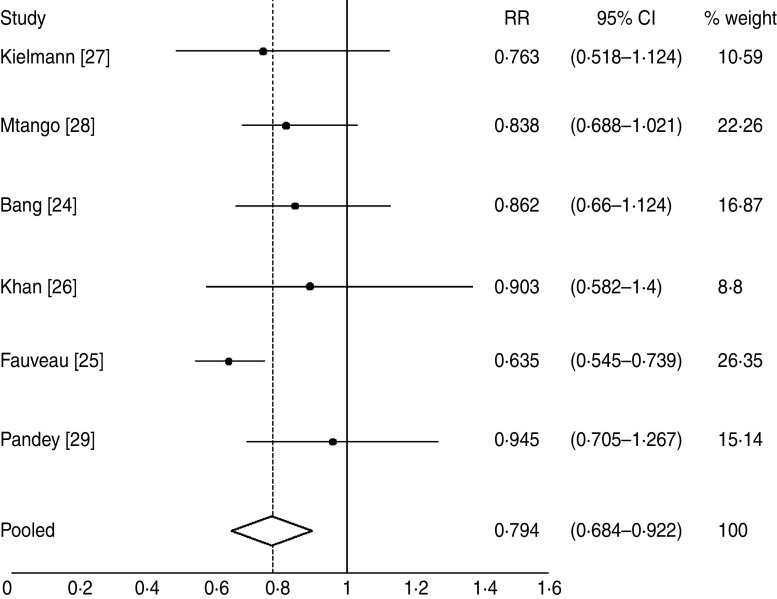
Pneumonia
We identified 3376 studies for screening in the initial review. After title, abstract, and review of the full papers, a total of six eligible studies of pneumonia case management were included (Table 5) [24–29]. These studies were also included in a previously published meta-analysis [10]; no new studies were identified for the analysis presented here. Five of six studies reported the effect of pneumonia case management on non-pneumonia causes of death while one reported a reduction in all-cause mortality. All six studies reported fewer non-pneumonia deaths, relative to the control arm (Table 6). Of the five studies reporting non-pneumonia reductions in mortality, three identified specific causes other than pneumonia for at least some deaths, while two reported COD only as pneumonia or non-pneumonia. Reductions were noted in diarrhoea mortality (0·77–1·47 deaths/1000 child-years, n = 3 studies) [24, 26, 28], measles mortality (1·10 deaths/1000 child-years, n = 1 study) [26], and malaria mortality (2·33 deaths/1000 child-years, n = 1 study) [28] (data not shown). A random-effects meta-analysis of the six studies found a pooled non-pneumonia mortality relative rate of 0·794 (95% CI 0·784–0·922), or a 20% reduction in non-pneumonia mortality (Fig. 3).
Fig. 3.
Forest plot of pneumonia case management studies contributing to the random-effects meta-analysis.
Diarrhoea
We identified 254 studies for screening in the initial review. After title, abstract, and review of the full papers, there were no papers that met our inclusion and exclusion criteria. Although several quasi-experimental and pre/post studies did assess the effect of ORS on all-cause or diarrhoea mortality, none of these studies controlled for confounding and many did not report coverage levels, or had similar coverage of ORS in both arms [30–39]. No RCTs or cluster RCTs were found that met our inclusion criteria.
Measles
We found 583 studies for screening in the initial review. After title, abstract, and review of the full papers, a total of 11 papers were included reporting on 10 unique studies assessing the effect of measles vaccine on all-cause mortality [40–50] and three papers reporting on one study assessing the effect of the vaccine on non-measles causes of death [51–53] (Table 7). Of the 10 studies reporting benefits of measles vaccine on all-cause mortality, seven found all-cause mortality reductions consistent with a benefit of the vaccine on non-measles deaths, taking into account the modelled proportion of measles deaths in the study setting in the absence of measles vaccine (Table 8). Similarly, the study reporting the effects of measles vaccine on other causes of death reported a reduction in non-measles mortality relative to the control arm [51–53]. The greatest reduction was observed in diarrhoea deaths, a 46% decline which would have resulted in a reduction of 5·13 deaths/1000 child-years among measles-vaccinated children in the study [51–53].
DISCUSSION
We sought to quantify the effects of key child survival interventions on child mortality above and beyond the observed effect on the targeted COD. While the idea that child survival interventions might impact more than one COD is not new, to our knowledge this is the first systematic approach to estimate the magnitude of these indirect effects.
Among malaria interventions we demonstrated that there does seem to be a small additional effect of ITNs on non-malaria causes of death in some settings. It is unclear which non-malaria causes of death were impacted, given that only one study reported disaggregated non-malaria causes of death [15]. Although most studies reported statistically significant reductions in all-cause mortality, these effects were accounted for by the high rates of malaria mortality in many of these study sites. We observed that in 3/7 studies, the mortality reduction could be completely explained by possible reductions in malaria mortality in the intervention setting. Because malaria is difficult to define in the field, where slide-confirmed malaria is still not routine and other causes of fever such as pneumonia may be confused with malaria, the relatively small magnitude of the indirect effects observed may in part be explained by misclassification in assigning COD. A study of malaria chemoprophylaxis and case management in a setting with moderate malaria mortality, however, did provide evidence suggesting a relatively large indirect effect from chloroquine. This result, however, is based on estimates of the proportion of malaria deaths in that setting, and could therefore be skewed by the difficulty in measuring malaria mortality; a second study of malaria case management, with a higher estimate of the proportion of malaria deaths, showed no indirect effect. There have been several studies of indoor residual spraying alone or in combination with other malaria control measures that have recorded beneficial effects of malaria control on more than just malaria mortality [54–56]. Unfortunately, many of these studies have been observational with no adjustment for confounding and thus were excluded from our review. However, it is worth noting that the consistently observed benefit is suggestive of a benefit on mortality that extends beyond malaria-specific mortality, but studies with the ability to appropriately control for confounding are needed before conclusions can be drawn.
The effect of pneumonia case management was consistent in studies reporting cause-specific and all-cause reductions in mortality. Although one study observed no effect of case management on pneumonia mortality, all studies found an effect on one or multiple non-pneumonia causes of death as well as on the overall non-pneumonia mortality rate. Pneumonia case management involves widespread promotion of antibiotics that can influence the faecal flora and prove to be protective against certain diarrhoea pathogens and thus diarrhoea mortality in general. We did not include the pneumococcal conjugate or Haemophilus influenzae type b vaccines in this analysis because attributing aetiology-specific mortality at the study or country level has not yet been done. However, it has been reported that the benefit of vaccine may well go beyond the reduction in pneumonia-mortality that would be expected if the vaccine only impacted one specific pneumonia aetiology [57]. This supports the effect observed in pneumonia case management and also suggests that pneumonia may be a contributing COD even in deaths directly attributable to other causes.
Most studies of measles vaccine suggested a moderate to large effect of the vaccine on non-measles mortality, but only one study provided cause-specific mortality data explaining which other causes of death the vaccine may have acted upon. Measles leads to a decrease in immune function, increasing the susceptibility of the child to secondary infections for weeks or possibly months following illness [58]; vaccination may decrease the rates of these secondary infections. Our analysis of the indirect effects of measles vaccine, however, was hampered by the fact that many studies reported only the relative all-cause mortality risk in children who had received measles vaccine vs. those who had not, adjusted for possible confounders. Our estimates of the relative risk of non-measles mortality in vaccine recipients relative to non-recipients thus depend in large part on modelled estimates of the proportion of measles deaths expected in the absence of measles vaccine, which may explain the wide range of indirect effects we found, ranging from no effect to an 81% reduction in non-measles mortality. In a few cases, the overall indirect mortality relative rate was >1. For both studies, the all-cause mortality reduction was small, and the proportion of deaths due to measles was large relative to the all-cause effect size. Thus for both studies the measles vaccine only averted some of the measles deaths; because of the formula we used to calculate the indirect relative mortality rate reduction, this appears as an effect size >1.
We were not able to estimate the indirect effects of ORS because we were unable to find studies that met our inclusion and exclusion criteria. Because it would be unethical to actively deny rehydration treatment to children with diarrhoea, no RCTs exist with a comparator that would allow us to estimate the indirect effect of ORS on mortality. Natural experiments and pre/post studies in the 1970s and 1980s took advantage of the introduction of ORS to attempt to measure its effect on mortality; however, these studies did not control for confounding and in some cases experienced contamination of the comparison area or poor coverage in the ORS arm. Given these limitations, the data could not be used to attempt to assess the indirect effects of ORS.
Most studies included in this review did not calculate mortality rates or deaths averted for the targeted cause or other causes of deaths. To perform this analysis we used all available data from the included studies, provided methods were adequately described, and in some cases country-level COD profiles from the LiST tool to estimate the presumed deaths averted from the targeted cause [2, 11, 12] (Table 9). LiST, including country COD profiles and the effectiveness values for interventions, has been used in a number of previous analyses and proven to be an excellent tool for modelling reductions in child mortality [59, 60]. However, there are important limitations in using published country-level COD estimates in lieu of study-specific estimates. LiST estimates are country-level, published peer-reviewed estimates, but are not site-specific which means that there could be great variability in these estimates compared to the actual proportions that would have been observed in the study site. In using this method, for studies reporting only all-cause mortality reductions, we assumed that the intervention would target the index disease first and prevent 100% of the possible deaths from that cause before preventing deaths from other causes. Although this assumption may be flawed, it is the most conservative approach to estimating possible indirect effects and allows for a consistent approach across diseases and interventions. Although all quasi-experimental studies included in this analysis did control for confounding, the full effect of the coverage of other child survival interventions in the intervention areas was not fully described in these papers and thus cannot be fully accounted for in this analysis.
Table 9.
Availability of data on the proportion of deaths from the targeted cause
| Intervention | Number of included studies for which study-reported cause-specific mortality data were used | Number of included studies for which modelled (from LiST) cause-specific mortality data were used |
|---|---|---|
| Insecticide-treated bednets | 3a | 4 |
| Malaria case management | 2 | 0 |
| Pneumonia case management | 6 | 0 |
| Measles vaccine | 1 | 10b |
Includes one study where a measured estimate from the same country, but a different study, was used.
Although several of these studies included estimates of the proportion of measles deaths, most did not provide a definition of a measles death, and those that did used widely varying definitions. Therefore in the interest of consistency modelled estimates from LiST were used.
In this review we included all types of study designs to capture as many studies as possible; all studies were included in previously published primary reviews of their main effects on cause-specific mortality [4–6 4–6, 10], except in the case of ITNs where we included several additional studies. However, we applied our own inclusion and exclusion criteria to ensure all studies met a minimum quality standard specific for this analysis. We were limited in our interpretation to the published studies that often included rigorous studies implemented under conditions not typical of real life. In some cases, despite attempts made by the researchers to mimic real life, the presence of a study benefits the control group in that mortality is decreased without an intervention. This may bias our results towards the null.
This analysis was designed to bring together published literature in an effort to quantify the indirect effects, if any, of selected interventions on causes of death other than those the interventions were intended to prevent. While in some cases we observed effect sizes larger than what might be expected if an intervention were only operating on its targeted disease, additional studies are needed to determine if these larger effect sizes (consistent with indirect effects of the interventions) are consistent across populations with different COD profiles. In addition, as new studies are designed and performed to assess mortality reductions, possible indirect effects should be considered and causes of death recorded for the major childhood diseases despite power and sample size restrictions. Until COD data are reported in addition to all-cause mortality reduction, we will not be able to move beyond projected indirect effects using modelling as we did in this analysis. With additional data to better describe averted COD, programmes such as LiST would be better able to capture the true mortality reduction. In addition, future versions of LiST may be able to incorporate uncertainty bounds on estimated mortality reductions.
At the present time, while we know some interventions do avert more deaths than the direct cause, the indirect causes are often ignored during the scale up of interventions and not captured as part of ongoing programme evaluations. It should also be noted that as the impact of interventions may be greater than what has been demonstrated in tightly controlled trials, the reverse would also be true. That is, eliminating or scaling back selected child survival interventions could result in a higher than expected increase in child mortality. Both of these effects, i.e. the indirect effects possible if choosing to initiate or scale up an intervention as well as the potential indirect effects of limiting or discontinuing an intervention should be considered during the programme planning process. Finally, as multiple interventions are rolled out simultaneously in many countries to increase child survival, research needs to be done to quantify the combined effect of intervention scale up. If indirect effects can be observed when considering isolated interventions designed to target one disease, it is possible these effect sizes may change with several interventions delivered at once.
Supplementary Material
Supplementary information supplied by authors.
ACKNOWLEDGEMENTS
This work was supported by a grant from the Bill and Melinda Gates Foundation to the US Fund for UNICEF for support of the work of the Child Health Epidemiology Reference Group. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. We thank Hilda Ndirangu for her assistance with abstraction of the included papers and Ingrid Friberg for her assistance with abstracting and modelling LiST data for this analysis.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0950268812001525.
click here to view supplementary material
DECLARATION OF INTEREST
None.
REFERENCES
- 1.You D, et al. Levels and trends in under-5 mortality, 1990–2008. Lancet 2010; 375: 100–103. [DOI] [PubMed] [Google Scholar]
- 2.Black RE, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet 2010; 375: 1969–1987. [DOI] [PubMed] [Google Scholar]
- 3.Walker N, et al. Standards for CHERG reviews of intervention effects on child survival. International Journal of Epidemiology 2010; 39 (Suppl. 1): i21–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eisele TP, Larsen D, Steketee RW. Protective efficacy of interventions for preventing malaria mortality in children in Plasmodium falciparum endemic areas. International Journal of Epidemiology 2010; 39 (Suppl. 1): i88–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sudfeld CR, Navar AM, Halsey NA. Effectiveness of measles vaccination and vitamin A treatment. International Journal of Epidemiology 2010; 39 (Suppl. 1): i48–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Theodoratou E, et al. The effect of case management on childhood pneumonia mortality in developing countries. International Journal of Epidemiology 2010; 39 (Suppl. 1): i155–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thwing J, Eisele TP, Steketee RW. Protective efficacy of malaria case management and intermittent preventive treatment for preventing malaria mortality in children: a systematic review for the Lives Saved Tool. BMC Public Health 2011; 11 (Suppl. 3): S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Munos MK, Walker CL, Black RE. The effect of oral rehydration solution and recommended home fluids on diarrhoea mortality. International Journal of Epidemiology 2010; 39 (Suppl. 1): i75–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rowe AK, Steketee RW. Predictions of the impact of malaria control efforts on all-cause child mortality in sub-Saharan Africa. American Journal of Tropical Medicine and Hygiene 2007; 77: 48–55. [PubMed] [Google Scholar]
- 10.Sazawal S, Black RE. Effect of pneumonia case management on mortality in neonates, infants, and preschool children: a meta-analysis of community-based trials. Lancet Infectious Diseases 2003; 3: 547–556. [DOI] [PubMed] [Google Scholar]
- 11.Bryce J, et al. WHO estimates of the causes of death in children. Lancet 2005; 365: 1147–1152. [DOI] [PubMed] [Google Scholar]
- 12.The Futures Institute. The Lives Saved Tool, version 3.45. Glastonbury, CT, 2010. [Google Scholar]
- 13.Winfrey W, McKinnon R, Stover J. Methods used in the Lives Saved Tool (LiST). BMC public health 2011; 11 (Suppl. 3): S32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.StataCorp. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP, 2009. [Google Scholar]
- 15.Binka FN, et al. Impact of permethrin-impregnated bednets on child mortality in Kassena-Nankana District, Ghana: a randomized controlled trial. Tropical Medicine and International Health 1996; 1: 147–154. [DOI] [PubMed] [Google Scholar]
- 16.D'Alessandro U, Olaleye BO. Mortality and malaria in Gambian children after introduction of an impregnated bednet programme. Lancet 1995; 345: 479. [DOI] [PubMed] [Google Scholar]
- 17.Fegan GW, et al. Effect of expanded insecticide-treated bednet coverage on child survival in rural Kenya: a longitudinal study. Lancet 2007; 370: 1035–1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Habluetzel A, et al. Do insecticide-treated curtains reduce all-cause child mortality in Burkina Faso? Tropical Medicine and International Health 1997; 9: 855–862. [DOI] [PubMed] [Google Scholar]
- 19.Nevill CG, et al. Insecticide-treated bednets reduce mortality and severe morbidity from malaria among children on the Kenyan coast. European Journal of Tropical Medicine and International Health 1996; 1: 139–146. [DOI] [PubMed] [Google Scholar]
- 20.Phillips-Howard PA, et al. Efficacy of permethrin-treated nets in the prevention of mortality in young children in an area of high perennial malaria transmission in Western Kenya. American Journal of Tropical Medicine and Hygiene 2003; 68: 23–29. [PubMed] [Google Scholar]
- 21.Schellenberg JR, et al. Effect of large-scale social marketing of insecticide-treated nets on child survival in rural Tanzania. Lancet 2001; 357: 1241. [DOI] [PubMed] [Google Scholar]
- 22.Kidane G, Morrow RH. Teaching mothers to provide home treatment of malaria in Tigray, Ethiopia: a randomised trial. Lancet 2000; 356: 550–555. [DOI] [PubMed] [Google Scholar]
- 23.Menon A, et al. Sustained protection against mortality and morbidity from malaria in rural Gambian children by chemoprophylaxis given by village health workers. Transactions of the Royal Society of Tropical Medicine and Hygiene 1990; 84: 768–772. [DOI] [PubMed] [Google Scholar]
- 24.Bang AT, et al. Reduction in pneumonia mortality and total childhood mortality by means of community-based intervention trial in Gadchiroli, India. Lancet 1990; 336: 201–206. [DOI] [PubMed] [Google Scholar]
- 25.Fauveau V, et al. Impact on mortality of a community-based programme to control acute lower respiratory tract infections. Bulletin of the World Health Organization 1992; 70: 109–116. [PMC free article] [PubMed] [Google Scholar]
- 26.Khan AJ, et al. Acute respiratory infections in children: a case management intervention in Abbottabad District, Pakistan. Bulletin of the World Health Organization 1990; 68: 577–585. [PMC free article] [PubMed] [Google Scholar]
- 27.Kielmann AA, et al. The Narangwal experiment on interactions of nutrition and infections: II. Morbidity and mortality effects. Indian Journal of Medical Research 1978; 68 (Suppl.): 21–41. [PubMed] [Google Scholar]
- 28.Mtango FD, Neuvians D. Acute respiratory infections in children under five years. Control project in Bagamoyo District, Tanzania. Transactions of the Royal Society of Tropical Medicine and Hygiene 1986; 80: 851–858. [DOI] [PubMed] [Google Scholar]
- 29.Pandey MR, et al. Reduction in total under-five mortality in western Nepal through community-based antimicrobial treatment of pneumonia. Lancet 1991; 338: 993–997. [DOI] [PubMed] [Google Scholar]
- 30.Barzgar MA, Ourshano S, Amini JN. The Evaluation of the effectiveness of oral rehydration in acute diarrhea of children under 3 years of age in West Azerbaijan, Iran. Journal of Tropical Pediatrics 1980; 26: 217–222. [Google Scholar]
- 31.David CB, Pyles LL, Pizzuti AM. Oral rehydration therapy: comparison of a commercial product with the standard solution. Journal of Diarrhoeal Disease Research 1986; 4: 222–226. [PubMed] [Google Scholar]
- 32.International Study Group. Beneficial effects of oral electrolyte – sugar solutions in the treatment of children's diarrhoea. 1. Studies in two ambulatory care clinics. Journal of Tropical Pediatrics 1981; 27: 62–67. [DOI] [PubMed] [Google Scholar]
- 33.Kielmann AA, et al. Control of deaths from diarrheal disease in rural communities. I. Design of an intervention study and effects on child mortality. Tropical Medicine and Parasitology 1985; 36: 191–198. [PubMed] [Google Scholar]
- 34.Kumar V, Kumar R, Datta N. Oral rehydration therapy in reducing diarrhoea-related mortality in rural India. Journal of Diarrhoeal Disease Research 1987; 5: 159–164. [PubMed] [Google Scholar]
- 35.Lasch EE, et al. Evaluation of the impact of oral rehydration therapy on the outcome of diarrheal disease in a large community. Israeli Journal of Medical Science 1983; 19: 995–997. [PubMed] [Google Scholar]
- 36.Rahaman MM, et al. Diarrhoeal mortality in two Bangladeshi villages with and without community-based oral rehydration therapy. Lancet 1979; 2: 809–812. [DOI] [PubMed] [Google Scholar]
- 37.Rahman AM, Bari A. Feasibility of home treatment of diarrhoea with packaged rice – ORS. Journal of Diarrhoeal Disease Research 1990; 8: 18–23. [PubMed] [Google Scholar]
- 38.Tekce B. Oral rehydration therapy: an assessment of mortality effects in rural Egypt. Studies in Family Planning 1982; 13: 315–327. [PubMed] [Google Scholar]
- 39.Thane T, et al. Oral rehydration therapy in the home by village mothers in Burma. Transactions of the Royal Society of Tropical Medicine and Hygiene 1984; 78: 581–589. [DOI] [PubMed] [Google Scholar]
- 40.Breiman RF, et al. Effect of infant immunisation on childhood mortality in rural Bangladesh: analysis of health and demographic surveillance data. Lancet 2004; 364: 2204–2211. [DOI] [PubMed] [Google Scholar]
- 41.Holt EA, et al. Childhood survival in Haiti: protective effect of measles vaccination. Pediatrics 1990; 85: 188–194. [PubMed] [Google Scholar]
- 42.Kabir Z, et al. Non-specific effect of measles vaccination on overall child mortality in an area of rural India with high vaccination coverage: a population-based case-control study. Bulletin of the World Health Organization 2003; 81: 244–250. [PMC free article] [PubMed] [Google Scholar]
- 43.Kristensen I, et al. Routine vaccinations and child survival: follow up study in Guinea-Bissau, West Africa Commentary: an unexpected finding that needs confirmation or rejection. British Medical Journal 2000; 321: 1435–1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lehmann D, et al. Benefits of routine immunizations on childhood survival in Tari, Southern Highlands Province, Papua New Guinea. International Journal of Epidemiology 2005; 34: 138–148. [DOI] [PubMed] [Google Scholar]
- 45.Velema JP, et al. Childhood mortality among users and non-users of primary health care in a rural west African community. International Journal of Epidemiology 1991; 20: 474–479. [DOI] [PubMed] [Google Scholar]
- 46.Aaby P, et al. Measles incidence, vaccine efficacy, and mortality in two urban African areas with high vaccination coverage. Journal of Infectious Diseases 1990; 162: 1043–1048. [DOI] [PubMed] [Google Scholar]
- 47.Aaby P, et al. Sex differential effects of routine immunizations and childhood survival in rural Malawi. Pediatric Infectious Disease Journal 2006; 25: 721–727. [DOI] [PubMed] [Google Scholar]
- 48.Elguero E, et al. Non-specific effects of vaccination on child survival? A prospective study in Senegal. Tropical Medicine and International Health 2005; 10: 956–960. [DOI] [PubMed] [Google Scholar]
- 49.Kumar G, et al. Scale for identification of ‘at risk’ families for underfive deaths. Indian Journal of Pediatrics 2000; 67: 411–417. [DOI] [PubMed] [Google Scholar]
- 50.Nyarko P, Pence B, Debpuur C .Immunization status and child survival in rural Ghana: Population Council, 2001.
- 51.Aaby P, et al. The survival benefit of measles immunization may not be explained entirely by the prevention of measles disease: a community study from rural Bangladesh. International Journal of Epidemiology 2003; 32: 106–116. [DOI] [PubMed] [Google Scholar]
- 52.Clemens JD, et al. Measles vaccination and childhood mortality in rural Bangladesh. American Journal of Epidemiology 1988; 128: 1330–1339. [DOI] [PubMed] [Google Scholar]
- 53.Koenig MA, et al. Impact of measles vaccination on childhood mortality in rural Bangladesh. Bulletin of the World Health Organization 1990; 68: 441–447. [PMC free article] [PubMed] [Google Scholar]
- 54.Kleinschmidt I, et al. Combining indoor residual spraying and insecticide-treated net interventions. American Journal of Tropical Medicine and Hygiene 2009; 81: 519–524. [PMC free article] [PubMed] [Google Scholar]
- 55.Kleinschmidt I, et al. Marked increase in child survival after four years of intensive malaria control. American Journal of Tropical Medicine and Hygiene 2009; 80: 882–888. [PMC free article] [PubMed] [Google Scholar]
- 56.Pringle G. Malaria in the Pare area of Tanzania. 3. The course of malaria transmission since the suspension of an experimental programme of residual insecticide spraying. Transactions of the Royal Society of Tropical Medicine and Hygiene 1967; 61: 69–79. [DOI] [PubMed] [Google Scholar]
- 57.Cutts FT, et al. Efficacy of nine-valent pneumococcal conjugate vaccine against pneumonia and invasive pneumococcal disease in The Gambia: randomised, double-blind, placebo-controlled trial. Lancet 2005; 365: 1139–1146. [DOI] [PubMed] [Google Scholar]
- 58.Moss WJ, Ota MO, Griffin DE. Measles: immune suppression and immune responses. International Journal of Biochemistry and Cell Biology 2004; 36: 1380–1385. [DOI] [PubMed] [Google Scholar]
- 59.Hazel E, et al. Comparing modelled to measured mortality reductions: applying the Lives Saved Tool to evaluation data from the Accelerated Child Survival Programme in West Africa. International Journal of Epidemiology 2010; 39 (Suppl. 1): i32–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Larsen D, Friberg I, Eisele T. Comparison of Lives Saved Tool model child mortality estimates against measured data from vector control studies in sub-Saharan Africa. BMC Public Health 2011; 11: S34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information supplied by authors.
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0950268812001525.
click here to view supplementary material