Abstract
Introduction
We investigate the association neighborhood cohesion, as source of social support, has with psychological distress among white, Black, and Latinx lesbian, gay, and bisexual (LGB) individuals, compared to heterosexual individuals in the United States.
Method
We estimate zero-order multinomial logistic regression models to assess the likelihood of moderate and severe psychological distress among respondents.
Result
In the models accounting for neighborhood cohesion and all other covariates, white, Black, and Latinx lesbian, gay, and bisexual individuals are more likely to meet the criteria for moderate and severe psychological distress than non-LGB people.
Conclusion
Neighborhood cohesion has differing impact on psychological distress outcomes by racial/ethnic-sexual orientation groups, but in general provides a greater magnitude of protection against moderate psychological distress for non-LGB groups and a greater magnitude of protection against severe psychological distress for LGB groups.
Keywords: Psychological distress, Sexual orientation, Race, Ethnicity, Neighborhood cohesion
Highlights
-
•
Lesbian, gay, and bisexual (LGB) people are more likely to meet the criteria for psychological distress than non-LGB people.
-
•
Neighborhood cohesion (NC) has differing impact on psychological distress by race and sexual orientation.
-
•
NC provides greater protection against moderate distress for non-LGB groups and severe psychological distress for LGB groups.
1. Introduction
Public acceptance of lesbian, gay, and bisexual (LGB) individuals has changed drastically in recent years, yet mental health trends among lesbian, gay, and bisexual people are worrisome (Russell & Fish, 2016). Racism and homophobia diminish the health of people of color and LGB individuals through discrimination, stigmatization, and minority stress (Andersen et al., 2015; Eliason & Fogel, 2015; Frost et al., 2015; Hatzenbuehler, 2009; Krieger, 2020; Lick et al., 2013; Meyer, 2003; Riley, 2017; Walch et al., 2016; Williams et al., 2019).
Neighborhood context shapes mental health by facilitating emotional support via social networks as well as resources and information that facilitate optimal health (Diez Roux, 2001; Echeverría et al., 2008; Elliott et al., 2014; Hong et al., 2014; Kawachi & Berkman, 2001; E. S.; Kim et al., 2013). Specifically, neighborhood social cohesion measures how connected one feels to neighbors, how trusting one is of their neighborhood social network, and the level of shared values and norms among neighborhood residents (Granovetter, 1973; Henning-Smith & Gonzales, 2017; Sampson et al., 1997). Henning-Smith and Gonzales (Henning-Smith & Gonzales, 2017) argue LGB individuals perceive less neighborhood cohesion compared to their heterosexual counterparts; however, the impact neighborhood cohesion has on the mental health of sexual minorities is largely understudied, particularly along racial lines. It remains unestablished whether neighborhood cohesion has a similar impact on LGB and non-LGB individuals, or whether it influences unequal mental health outcomes by race and sexual orientation. We address this gap by investigating the effects of neighborhood cohesion on moderate and severe psychological distress among LGB individuals who identify as white, Black, or Latinx.
1.1. Lesbian, gay, and bisexual mental health
Since the 1980s, when evidence of poor mental health among sexual minorities first emerged (Gibson, n.d.), public opinion of the lesbian, gay, bisexual, transgender, queer, and other (LGBTQ+) community has dramatically shifted (Russell & Fish, 2016). In 2013, 92% of LGB adults surveyed viewed Americans as more accepting of the LGBTQ + community compared to the previous decade (Pew Research Center, 2013). Additionally, in 2019, 61% of adults surveyed reported they support same-sex marriage, compared to only 35% reporting support in 2001 (Pew Research Center, 2019). Despite these improvements, LGB individuals still experience significant levels of discrimination. More than one-third of LGBTQ Americans report experiencing discrimination in the past year; with 51% experiencing harassment or discrimination in public spaces, 36% in the workplace, 21% at school, 20% in an apartment community; and 15% in interactions with law enforcement (Mahowald et al., 2020). Other common stressors among LGB individuals are rejection, victimization, loss of financial security or employment, housing discrimination, and internalized homophobia and biphobia (Meyer, 2003; Russell & Fish, 2016). Mental health issues LGB individuals face are best understood under the minority stress framework, which posits that chronic stressors and the unique experiences of a stigmatized identity act as social determinants of poor mental health outcomes (Aneshensel, 1992; Meyer, 1995, 2003; Meyer & Frost, 2013).
Consequently, it is unsurprising that LGB individuals are at higher risk of depression, mood disorders, anxiety disorders, post-traumatic stress disorder, alcohol use, suicidality, and psychiatric comorbidity (Borgogna et al., 2019; Bränström & Pachankis, 2018; Cochran et al., 2003; Gilman et al., 2001; Goldstein et al., 2016; Gonzales et al., 2016; Gonzales & Henning-Smith, 2017; Hatzenbuehler, 2009; Kerridge et al., 2017; Lee et al., 2020; Parent et al., 2019; Plöderl & Tremblay, 2015; Remafedi et al., 1998; Rice et al., 2019; Weissman et al., 2021). Although there is a growing body of literature on the mental health of Black and Latinx LGB communities and an increasing understanding of intersectionality in LGB health research, existing work has several limitations, including small and/or non-representative samples. Additionally, early work on LGB health frequently focused on one racial/ethnic group or one sexual orientation and lacked a comparative component (Bowleg et al., 2003; Garrett-Walker & Longmire-Avital, 2018; Hughes & Matthews, 2004; Lassiter et al., 2019; Lassiter & Poteat, 2020; Walker & Longmire-Avital, 2015; Wilton et al., 2018). We recognize the significance and foundational value of this research to the study of LGB mental health. However, these studies do not provide a broader, comparative picture across race/ethnicity and sexual orientations (including whiteness and heterosexuality), which is the aim of our study. In sum, we are concerned with the effects of interlocking marginalizing identities and how they potentially reinforce health inequalities vis-à-vis those without marginalizing identities (Browne & Misra, 2003; Collins, 2000; Combahee River Collective, 1995; Crenshaw, 1991).
Some evidence suggests that Black and Latinx LGB individuals do not experience more mental health disorders (as defined by the DSM-IV) than white LGB individuals (Williams, 2001) likely due to the lower prevalence of mental disorders among Black and Latinx individuals generally. Although Black individuals experience higher levels of discrimination and lower access to socioeconomic (SES) resources, research suggests that Black Americans have equal or lower rates of mood, anxiety, and substance abuse disorders compared to whites (Barnes & Bates, 2017; Blazr et al., 1994; Erving & Thomas, 2018). This Black-White paradox (Williams, 2001) in mental health is attributed to the protective effect of social ties among Black Americans (Mouzon, 2014). Similarly, the literature suggests that Latinx individuals, particularly those who are foreign-born, have better mental health outcomes than their US-born counterparts and non-Latinx whites, despite experiencing heightened risk factors (Alegría et al., 2008; Harker, 2001; Ortega et al., 2000; Vega & Rumbaut, 1991). However, some studies have challenged the assertion of these advantages in mental health when considering sexual orientation. Black and Latinx LGB individuals are more likely to report a serious suicide attempt (Kiecolt et al., 2008) relative to white LGB people, and lesbian and bisexual women are more likely to report depression symptomatology when compared to non-LGB women (Cochran & Mays, 2000; Hirokazu; Yoshikawa et al., 2004).
Discrimination due to the overlap of racism, xenophobia, and homophobia can independently contribute to distress, anxiety, depressed mood, and suicidal ideation (Díaz et al., 2001). Thus, experiences of LGB Black and Latinx individuals might differ significantly from those of LGB white individuals. Evidence suggests LGB people of color are aware of limited educational, residential, and economic opportunities and are conscious of racism as a source of stress (Meyer et al., 2011). LGB people of color describe feeling disconnected between their racial and ethnic identities and sometimes even from the broader LGBTQ + community and cite their own culture's homophobia as an issue that exclusively affects LGB people of color basis (Ghabrial, 2017). They report experiencing stress related to experiences like financial woes and coming out and anxiety on a regular basis (Ghabrial, 2017). LGB people of color are also subject to microaggressions such as others' disapproval, being reduced to universal stereotypes regarding their sexuality, tokenization and exoticization, body policing, and intrusive questioning about their sexual practices (Weber et al., 2018). Additionally, LGB people of color face racial, sexual orientation, and mental illness discrimination when in mental health treatment contexts (Charles, 2013; Delphin-Rittmon et al., 2013; L.; Gonzales et al., 2015; Holley et al., n.d.; Kidd et al., 2011; Stromwall et al., 2011).
Interlocking modes of domination (Browne & Misra, 2003; Collins, 2000; Combahee River Collective, 1995; Crenshaw, 1991) reinforce health disparities in the context of race/ethnicity, gender, and sexual orientation. Literature concerning intersectionality and LGB health has provided mixed results. One body of work finds that with multiple marginalization, for example being LGB and a person of color, comes greater risk for adverse health outcomes (Cochran & Mays, 1994; Díaz et al., 2001; H.-J.; Kim & Fredriksen-Goldsen, 2012; Mereish & Bradford, 2014; Meyer et al., 2008; Park et al., 2022). Another body of work suggests a theory of resilience, where LGB people of color have lower risk compared to LGB white individuals because of support networks in communities of color (Balsam, 2004; Bostwick et al., 2014; Lytle et al., 2015). Finally, an additional body of literature supports either the multiple marginalization or the theory of resilience, depending on race/ethnicity-sexual orientation-gender groupings (Lehavot et al., 2019; López et al., 2021; Platt et al., 2018; Rodriguez-Seijas et al., 2019). For example, among a sample of women veterans, white heterosexual women report the lowest levels of psychological distress and heterosexual women of color report the highest (Lehavot et al., 2019). In the same sample, white LGB women report greater levels of adverse mental health than heterosexual white women; however, heterosexual women of color report similar or worse mental health compared to LGB women of color (Lehavot et al., 2019). In a nationally representative population-based study, gay men of color were more likely to experience psychological distress compared to gay white men; however, gay and lesbian white women and gay and lesbian women of color had similar psychological distress profiles (Platt et al., 2018).
1.2. Social support and neighborhood cohesion
Social support is instrumental for LGB individuals because they often rely on members of their community (i.e., fictive kin or chosen families), for social support more than they rely on family members (Frost et al., 2016; Weston, 1997). Social support, broadly defined as resources provided by others (Cohen & Syme, 1985), serves three distinct purposes: it leads one to believe they are loved and cared for, it creates the belief that one is valued, and it creates a sense of belonging to a group. This perception of belonging and being valued and cared for has significant associations with health (Cobb, 1976). Among bisexual individuals, low levels of perceived social support are associated with depression, poor life satisfaction, and internalized biphobia (Sheets & Mohr, 2009). Perceived support is associated with health, wellbeing, and life satisfaction among lesbian and gay adults (Dominguez-Fuentes et al., 2012; Lauby et al., 2012). Furthermore, social support and supportive environments have a positive impact on the health, wellbeing, and educational outcomes of LGB youth (Detrie & Lease, 2007; Hatzenbuehler et al., 2014; Ryan et al., 2009; Toomey et al., 2011). However, compared to LGB whites, LGB people of color receive fewer dimensions of social support (Frost et al., 2016), which highlights the need to examine the impact of social support on health among this population.
A substantial body of research supports the relationship between community-level social cohesion and health (Browning et al., 2003; Kawachi & Berkman, 2000; Lochner et al., 2003). Social cohesion is “the extent of connectedness and solidarity among groups in society” (Kawachi & Berkman, 2000). The literature dealing with this psychosocial resource employs various constructs in terms of measurement, including collective efficacy, social capital, and civic participation (Berkman et al., 2014; Lochner et al., 2003; Macinko & Starfield, 2001; Sampson et al., 1997). Neighborhood cohesion, a feeling of connectedness to one's own neighborhood, is associated with numerous health outcomes (Granovetter, 1973; Henning-Smith & Gonzales, 2017; Sampson et al., 1997). Neighborhood cohesion facilitates the development of social networks that provide emotional, informational, and instrumental support, including the sharing of health information (Diez Roux, 2001; Echeverría et al., 2008; Elliott et al., 2014; Hong et al., 2014; Kawachi & Berkman, 2000, 2001; E. S.; Kim et al., 2013). Higher neighborhood cohesion decreases the risk of poor mental health outcomes, smoking and alcohol consumption, and stroke. Neighborhood interactions are important for LGB individuals as experiences of stigmatization, discrimination, and minority stress are a major pathway for poor mental health outcomes (Hatzenbuehler, 2009; Henning-Smith & Gonzales, 2017; Meyer, 2003). Compared to non-LGB individuals, LGB individuals are less likely to say they live in a close-knit neighborhood, that they can count on and trust their neighbors, and less likely to say that their neighbors help each other out (Henning-Smith & Gonzales, 2017). Neighborhood cohesion has important implications for health and wellbeing and the literature thus far has not addressed how it affects the mental health of sexual minorities, especially along racial lines. Our study aims to address this gap.
2. Data and methods
We use the IPUMS Health Surveys, a harmonized version of the National Health Interview Survey (NHIS) (Blewett et al., 2019). NHIS is a cross-sectional household survey that measures physical and mental health outcomes, as well as social and demographic variables. We utilized six years of data from 2013 to 2018 to increase the size of our LGB sample. Of the 568,494 respondents in those six waves of data, 4,920 identify as lesbian, gay or bisexual. Due to the use of secondary data, this study was granted exempt status from the Institutional Review Board at the first author's institution. Data are weighted to address complex survey design.
2.1. Key variables
Psychological Distress. Our outcome variable is psychological distress, a composite measure known as the Kessler 6 (K6) (Kessler et al., 1994, 2002, 2003). The six variables ask individuals how often they have felt that everything is an effort, felt hopeless, nervous, restless, sad and/or worthless, during the past 30 days. The attributes range from none of the time (0) to all the time (4). Responses are summed to measure nonspecific psychological distress with scores ranging from 0 to 24. Individuals scoring 13 or greater are likely to be experiencing severe psychological distress (Kessler et al., 2003) while individuals scoring between 5 and 12 meet the criteria for moderate psychological distress (Prochaska et al., 2012). Thus, we categorize distress in three ways, 1) Less than Moderate Distress (score of 4 or less); 2) Moderate Distress (score of 5–12); and 3) Severe Distress (score of 13 or over).
Explanatory Variables. We identify individuals into mutually exclusive racial and ethnic groups by sexual orientation (referred to as racial/ethnic-sexual orientation groups). The NHIS has included a sexual orientation question since 2013. It asks respondents, “Which of the following best represents how you think of yourself?” The attributes to this variable are, lesbian or gay; straight, that is, not lesbian or gay; bisexual; something else; I don't know the answer; and refused. The study's subsample includes those who identified as lesbian or gay, bisexual, and straight. To assess race and ethnicity, the NHIS asks two questions. The race question reads, “What race or races do you consider yourself to be?” Respondents can select more than one of the sixteen available categories. For ethnicity, the question is, “Do you consider yourself to be Hispanic or Latino?”, and respondents can answer yes, no, or unknown. For our subsample, we selected those who identified as white and non-Latino, Black and non-Latino, and Latino. Because of limited sample size of LGB Asian and LGB American Indian/Alaska Native individuals, we do not include Asian or American Indian/Alaska Native adults in our analysis. Thus, our subsample is comprised of six self-identified racial/ethnic-sexual orientation groups: heterosexual (non-LGB) non-Latinx (NL) white adults (N = 115,784), NL Black adults (N = 22,061) and Latinx adults (N = 26,036) as well as self-identified lesbian, gay, or bisexual, NL white adults (N = 3,293), LGB NL Black adults (N = 577) and LGB Latinx adults (N = 691). There is some evidence that suggests that Latinx and Black survey respondents have higher non-response rates for self-identified sexual orientation questions than NL whites (H. J. Kim & Fredriksen-Goldsen, 2013). Hence, Black and LGB respondents may be undercounted. Additionally, because NHIS does not measure gender identity, we are unable to identify transgender individuals for this analysis. It is important to note that we do not suggest sexual orientation and race categories themselves determine the health outcomes of LGB populations and people of color. Instead, we conceptualize these categories as “markers” used to identify individuals at risk for exposure to racism, homophobia, and biphobia which are created, maintained, and reproduced by social structures (Ford & Airhihenbuwa, 2011; Poteat, 2021; Zuberi & Bonilla-Silva, 2008).
Neighborhood Cohesion was constructed from four Likert-scale items (Henning-Smith & Gonzales, 2017; Murillo et al., 2016; Yi et al., 2016). These items asked respondents how much they agree that their neighborhood is close-knit, that they can count on neighbors, that neighbors can be trusted, and that neighbors help each other out. We dichotomize each item and create a summed score with a range from 0 to 4.
Controls. In each model, we control for Time in Neighborhood (less than one year, 1–3 years, 4–10 years, 11–20 years and 20+ years). Sociodemographic control variables include Gender (coded 0 for male and 1 for female), Age (continuous), Marital Status (coded 0 for unmarried and 1 for married or living with a partner) and Region (Northeast, North Central/Midwest, South and West). For SES measures, we include Educational Attainment (less than high school, high school graduate, some college and bachelor's degree and above; bachelor's degree and above is the reference group in all models) and Employment (coded 0 for unemployed and 1 for employed).
2.2. Analytic techniques
We use descriptive statistics to characterize the study sample and estimate the prevalence of moderate and severe psychological distress by racial/ethnic-sexual orientation group. We then estimate zero-order multinomial logistic regression models for psychological distress. We first test the relationship between racial/ethnic-sexual orientation groups and psychological distress. Next, we add neighborhood cohesion to the model, and finally, we add all other control variables: time in neighborhood, gender, age, marital status, education attainment, employment status, and region. We use non-LGB, non-Latinx white as the reference group in these models for several reasons. First, because this subgroup is the largest, because non-LGB NL whites have the highest average rating of neighborhood cohesion, and because this subgroup has the lowest prevalence of moderate and severe psychological distress, we compare other groups to non-LGB NL whites. Second, as supported through the minority stress framework, chronic stressors and the unique experiences related to a stigmatized identity act as social determinants of mental health outcomes for non-LGB people of color and LGB people (Andersen et al., 2015; Aneshensel, 1992; Díaz et al., 2001; Eliason & Fogel, 2015; Frost et al., 2015; Hatzenbuehler, 2009; Lick et al., 2013; Meyer, 1995, 2003; Meyer & Frost, 2013; Walch et al., 2016). We conducted the analysis using Stata 17 (StataCorp, 2021).
3. Results
3.1. Descriptive statistics
Table 1 displays the weighted distributions and means by race and sexual orientation. All LGB groups have a higher proportion of respondents in moderate and severe distress compared to non-LGB groups. The LGB white group has the highest proportion of respondents in moderate distress (28.7%), while the LGB Black and LGB Latinx groups have the highest proportions of respondents meeting the criteria for severe distress (9.4% and 8.3%). Non-LGB individuals have higher average neighborhood cohesion than their LGB counterparts. Among LGB individuals, the LGB white group has the highest rated neighborhood cohesion (3.0). LGB individuals are more likely to have resided in their neighborhoods for less than one year and 1–3 years. Non-LGB individuals have longer neighborhood tenures. Women are almost equally represented in all groups, except for the LGB Black group (60.7%). LGB individuals are also younger than non-LGB individuals, the youngest being LGB Black and Latinx individuals (35.7 and 35.5 years old). Non-LGB individuals are married or living with a partner in higher proportions. LGB and non-LGB Black individuals have the lowest proportion of marriage or living with a partner. White individuals reported higher levels of education, with the highest proportions of college-educated respondents found in both non-LGB white and LGB white groups. The proportion of respondents employed and unemployed are slightly higher for all LGB groups in the sample compared to non-LGB groups, and the proportion of respondents not in the labor force is higher among non-LGB groups compared to LGB groups.
Table 1.
Weighted descriptive statistics of sample respondents by race, ethnicity, and sexual orientation across independent and control variables (N = 162,044).
| NL White (N = 115,784) |
NL Black (N = 22,061) |
Latinx (N = 26,036) | LGB NL White (N = 3,293) | LGB Black (N = 577) | LGB Latinx (N = 691) | |
|---|---|---|---|---|---|---|
| Less than Moderate Distress | 80.0% | 79.4% | 79.4% | 63.8% | 64.0% | 63.4% |
| Moderate Distress | 16.7% | 17.4% | 16.9% | 28.7% | 26.6% | 28.2% |
| Severe Distress | 3.3% | 3.3% | 3.7% | 7.6% | 9.4% | 8.3% |
| Neighborhood Cohesion (Range 0–4) | 3.3 | 2.9 | 2.8 | 3.0 | 2.4 | 2.7 |
| Time in Neighborhood | ||||||
| Less than 1 year | 11.6% | 15.7% | 14.0% | 20.7% | 28.8% | 24.8% |
| 1–3 years | 18.9% | 23.6% | 24.7% | 25.0% | 32.1% | 28.5% |
| 4–10 years | 23.8% | 25.8% | 29.7% | 26.1% | 19.0% | 25.1% |
| 11–20 years | 20.2% | 16.8% | 18.9% | 16.5% | 11.6% | 14.5% |
| 20+ years | 25.4% | 18.1% | 12.8% | 11.8% | 8.5% | 7.1% |
| Female | 51.3% | 54.8% | 49.9% | 54.3% | 60.7% | 51.3% |
| Age (Range 18–85+) | 49.7 | 45.0 | 41.3 | 41.2 | 35.7 | 35.5 |
| Married/Living with Partner | 64.7% | 41.4% | 60.6% | 48.0% | 24.3% | 40.8% |
| Educational Attainment | ||||||
| Less than High School | 8.0% | 14.6% | 31.2% | 5.7% | 13.3% | 18.2% |
| High School | 24.7% | 30.0% | 26.9% | 18.2% | 26.9% | 23.7% |
| Some College | 31.8% | 33.5% | 27.1% | 32.4% | 39.2% | 32.7% |
| Bachelor's and More | 35.6% | 21.9% | 14.8% | 43.8% | 20.6% | 25.5% |
| Employment Status | ||||||
| Employed | 61.33% | 58.60% | 65.24% | 67.44% | 58.90% | 69.59% |
| Unemployed | 2.93% | 7.79% | 4.82$ | 5.73% | 14.02% | 7.61% |
| Not in Labor Force | 35.74% | 33.60% | 29.94% | 26.84% | 27.08% | 22.80% |
| Region | ||||||
| Northeast | 19.0% | 15.9% | 13.5% | 19.4% | 13.4% | 14.9% |
| North Central/Midwest | 27.7% | 16.7% | 9.2% | 22.8% | 20.7% | 11.5% |
| South | 33.8% | 59.7% | 37.4% | 31.6% | 55.1% | 36.4% |
| West | 19.6% | 7.8% | 40.0% | 26.2% | 10.9% | 37.2% |
Notes: NL indicates non-Latinx; LGB indicates lesbian, gay, and bisexual.
3.2. Psychological distress
Table 2 displays the results of multinomial logistic models expressed as relative risk ratios (RR). For each comparison, moderate psychological distress compared to less than moderate distress, and severe psychological distress compared to less than moderate distress, we first show baseline models by race and sexual orientation. Our second models include neighborhood cohesion, and third models account for all covariates. We conduct a final fourth model including interaction terms for racial/ethnic-sexual orientation groups and neighborhood cohesion (shown in predicted probability figures below). In the three baseline models, except for Latinx respondents for severe psychological distress (RR = 1.13, p > .05), non-LGB Black and Latinx respondents are not significantly different from non-LGB white individuals, the reference group for all models.
Table 2.
Multinomial logistic models of psychological distress expressed in relative risk ratios.
| Moderate Distress Compared to less than Moderate Distress | Severe Distress Compared to less than Moderate Distress | |||||
|---|---|---|---|---|---|---|
| Racial and Ethnic Group by Sexual Orientation (Ref. White) | ||||||
| Black | 1.04 (0.032) | 0.95 (0.030) | 0.82*** (0.026) | 1.03 (0.061) | 0.84** (0.051) | 0.60*** (0.038) |
| Latinx | 1.03 (0.027) | 0.92** (0.025) | 0.77*** (0.023) | 1.13* (0.056) | 0.90* (0.046) | 0.67*** (0.040) |
| LGB NL White | 2.15*** (0.121) | 2.05*** (0.117) | 1.90*** (0.111) | 2.86*** (0.258) | 2.59*** (0.237) | 2.69*** (0.267) |
| LGB NL Black | 2.07*** (0.294) | 1.76*** (0.261) | 1.32 (0.195) | 3.83*** (0.827) | 2.75*** (0.632) | 1.67* (0.404) |
| LGB Latinx | 2.17*** (0.275) | 1.92*** (0.251) | 1.58*** (0.216) | 3.32*** (0.699) | 2.59*** (0.572) | 2.11*** (0.477) |
| Neighborhood Cohesion | 0.82*** (0.006) | 0.85*** (0.006) | 0.69*** (0.009) | 0.73*** (0.009) | ||
| Time in Neighborhood (Ref. less than one year) | ||||||
| 1–3 years | 0.86*** (0.027) | 0.97 (0.060) | ||||
| 4–10 years | 0.87*** (0.029) | 0.99 (0.063) | ||||
| 11–20 years | 0.76*** (0.027) | 0.80** (0.057) | ||||
| 20+ years | 0.75*** (0.028) | 0.70*** (0.053) | ||||
| Female | 1.31*** (0.026) | 1.39*** (0.056) | ||||
| Age | 0.99*** (0.001) | 0.99*** (0.001) | ||||
| Married/Living with Partner | 0.80*** (0.016) | 0.65*** (0.026) | ||||
| Education (Ref. Bachelor's degree and above) | ||||||
| Less than HS | 1.58*** (0.052) | 3.71*** (0.254) | ||||
| High School | 1.33*** (0.035) | 2.63*** (0.158) | ||||
| Some College | 1.31*** (0.034) | 2.25*** (0.140) | ||||
| Employment Status (Ref. Unemployed) | ||||||
| Employed | 0.53*** (0.024) | 0.23*** (0.018) | ||||
| Not in Labor Force | 0.73*** (0.033) | 0.78*** (0.060) | ||||
| Region (Ref. Northeast) | ||||||
| North Central/Midwest | 1.05 (0.034) | 1.15* (0.084) | ||||
| South | 0.97 (0.030) | 1.19** (0.079) | ||||
| West | 1.14*** (0.040) | 1.19* (0.087) | ||||
Notes: N = 158,320. Standard Errors in parentheses. ***p < .001, **p < .01, *p < .05.
NL indicates non-Latinx; LGB indicates lesbian, gay, and bisexual.
After controlling for neighborhood cohesion in the second models, all non-LGB groups are significantly less likely to be psychologically distressed with the exception of Black individuals for moderate distress compared to less than moderate distress. For LGB groups, once we account for neighborhood cohesion, they all remain significantly more likely to be moderately and severely distressed, although to a lesser extent. Though the association of race and sexual orientation is lower in these models, neighborhood cohesion has the lowest association among the LGB white group, for whom the inclusion of this variable slightly reduces the association of the main independent variable.
In the third model, controlling for all covariates, heterosexual Black and Latinx individuals are significantly less likely to be moderately and severely distressed. Among LGB groups, white individuals are at higher risk of moderate and severe distress compared to non-LGB, non-Latinx whites (RR = 1.90, p < .001 for moderate distress; RR = 2.69, p < .001 for severe distress). Black individuals are also at higher risk of severe distress (1.67, p < .05) compared to non-LGB, non-Latinx whites. Finally, Latinx respondents are at significantly higher risk for both types of distress (RR = 1.58, p < .001 for moderate distress; 2.11, p < .001 for severe distress) when compared to non-LGB, non-Latinx whites. Neighborhood cohesion overall significantly decreases the likelihood of meeting the criteria for both moderate and severe psychological distress (RR = 0.85, p < .001; RR = 0.73, p < .001) as does time in the neighborhood. Longer neighborhood tenure significantly decreases the likelihood of distress, especially for those in the 11–20 and 20+ years of residence in the neighborhood. Age, being married, and being employed or not in the labor force significantly decrease the likelihood of meeting the criteria for moderate and severe distress. Being a woman and having less than a bachelor's degree has the opposite relationship. In terms of region, compared to the Northeast, respondents in the West are more likely to be moderately distressed, while those in the other regions are more likely to be severely distressed.
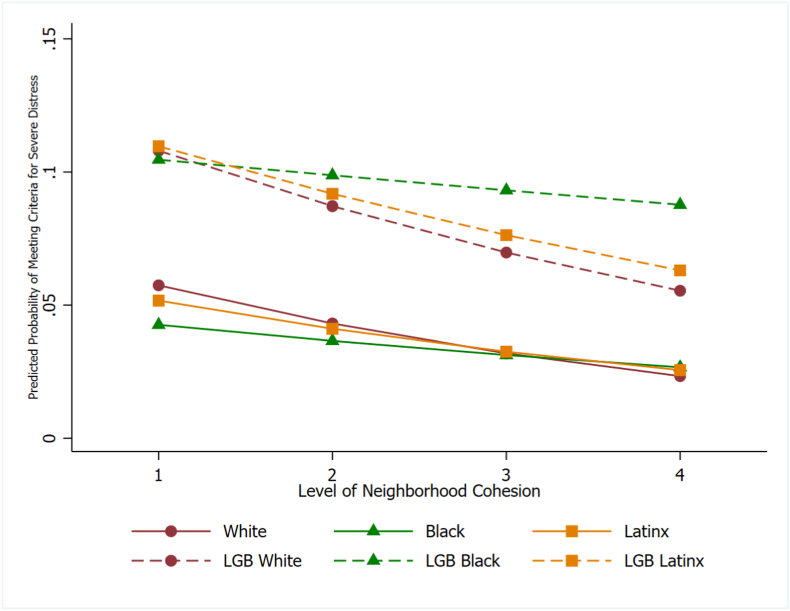
In the final model, after controlling for all covariates and adding interaction terms, we present predicted probabilities of meeting the criteria for moderate distress compared to less than moderate distress (Table 3 and Fig. 1) and severe distress compared to less than moderate distress (Table 4 and Fig. 2).
Table 3.
Predicted probability of meeting the criteria for moderate distress, by level of neighborhood cohesion.
| White | Black | Latinx | LGB White | LGB Black |
LGB Latinx | ||
|---|---|---|---|---|---|---|---|
| Level of Neighborhood Cohesion | |||||||
| 1 | 22.76 | 20.17 | 19.38 | 31.87 | 25.53 | 29.46 | |
| 2 | 19.83 | 18.46 | 17.93 | 30.28 | 26.64 | 28.84 | |
| 3 | 17.10 | 16.83 | 16.51 | 28.55 | 27.77 | 28.12 | |
| 4 | 14.60 | 15.30 | 15.14 | 26.73 | 28.92 | 27.32 | |
Notes: N = 158,320. Covariates not show are set to their means. NL indicates non-Latinx; LGB indicates lesbian, gay, and bisexual.
Fig. 1.
Predicted Probabilities of Meeting Criteria for Moderate Distress by Racial/Ethnic-Sexual Orientation Group, by Level of Neighborhood Cohesion. Covariates not show are set to their means. NL indicates non-Latinx; LGB indicates lesbian, gay, and bisexual.
Table 4.
Predicted probability of meeting the criteria for severe distress, by level of neighborhood cohesion.
| White | Black | Latinx | LGB White | LGB Black |
LGB Latinx | ||
|---|---|---|---|---|---|---|---|
| Level of Neighborhood Cohesion | |||||||
| 1 | 5.74 | 4.26 | 5.17 | 10.80 | 10.46 | 10.97 | |
| 2 | 4.31 | 3.66 | 4.11 | 8.72 | 9.88 | 9.18 | |
| 3 | 3.19 | 3.13 | 3.25 | 6.98 | 9.31 | 7.63 | |
| 4 | 2.34 | 2.67 | 2.56 | 5.54 | 8.77 | 6.31 | |
Notes: N = 158,320. Covariates not show are set to their means. NL indicates non-Latinx; LGB indicates lesbian, gay, and bisexual.
Fig. 2.
Predicted Probabilities of Meeting Criteria for Severe Distress by Racial/Ethnic-Sexual Orientation Group, by Level of Neighborhood Cohesion. Covariates not show are set to their means. NL indicates non-Latinx; LGB indicates lesbian, gay, and bisexual.
The impact of neighborhood cohesion is not equal across racial/ethnic-sexual orientation groups. Table 3, Table 4 report predicted probabilities for meeting the criteria for moderate and severe psychological distress by racial/ethnic-sexual orientation group, at each level of neighborhood cohesion.
For moderate and severe psychological distress, with equal levels of neighborhood cohesion, each LGB racial/ethnic group is more likely to meet the criteria for moderate distress when compared to their respective non-LGB group. Neighborhood cohesion overall significantly decreases the likelihood of meeting the criteria for both moderate and severe psychological distress for all racial/ethnic-sexual orientation groups, with the exception of moderate distress for LGB Black adults. Quite surprisingly, as levels of neighborhood cohesion increase, the predicted likelihood of meeting the criteria for moderate distress also increases for LGB Black adults, although this association is not significant in multinomial models.
For moderate distress, neighborhood cohesion appears to provide a greater magnitude of protection for non-LGB groups in comparison to their respective LGB group. When considering the difference in predicted probabilities between a neighborhood cohesion score of 1 and 4, each non-LGB group sees a larger decrease in predicted probabilities for moderate psychological distress compared to their respective LGB group (a difference of 8.16 for white versus a difference of 5.14 for LGB white; 4.87 for Black versus a 3.39 increase for LGB Black; and a difference of 5.14 for Latinx versus 2.14 for LGB Latinx).
This relationship flips for severe psychological distress. When considering the difference in predicted probabilities between a neighborhood cohesion score of 1 and 4, each LGB group sees a larger decrease in predicted probabilities for severe psychological distress compared to their respective non-LGB group (5.26 for LGB white versus 3.41 for white; 1.69 for LGB Black versus 1.59 for Black; and 4.66 for LGB Latinx compared to 2.61).
In sum, all LGB groups have higher proportions of respondents in moderate and severe distress than non-LGB groups. Additionally, in regression analyses, all LGB individuals are almost or over two times more likely to meet the criteria for moderate and severe psychological distress than non-LGB, non-Latinx white individuals. Neighborhood cohesion appears to provider a greater magnitude of protection against moderate psychological distress for non-LGB groups compared to their respective LGB group and a greater magnitude of protection against severe psychological distress for LGB groups compared to their respective non-LGB group.
4. Discussion
We anticipated that LGB Black and Latinx individuals would have a higher likelihood of meeting the criteria for psychological distress than LGB white individuals when compared to non-LGB white individuals because of the multiple minority stressors queer people of color face (Díaz et al., 2001; Hughes et al., 2008; Zamboni & Crawford, 2007).We find little support for this across models. In baseline models, LGB white individuals are more likely to meet the criteria for moderate distress compared to non-LGB white individuals, but LGB people of color are more likely to meet the criteria for severe psychological distress compared to non-LGB white individuals; however, in subsequent models, this association does not hold. In analysis not shown (see Supplementary material), we test the significance of a linear combination of coefficients and see that each LGB group does not significantly differ from the other for severe psychological distress, and only LGB white and LGB Black individuals differ from each other for moderate psychological distress.
We further expected neighborhood cohesion to reduce the likelihood of meeting the criteria for psychological distress, and we find support for this across models. After controlling for neighborhood cohesion, all groups in the study were less likely to meet the criteria for psychological distress; however, the magnitude of impact was not equal across groups. Neighborhood cohesion was less impactful for LGB groups on moderate psychological distress but more impactful on severe psychological distress for LGB groups, compared to their respective non-LGB group. Although for LGB Black adults, greater levels of neighborhood cohesion was associated with a higher predicted probability of meeting the criteria for moderate psychological distress, multinomial logistic models show that LGB Black individuals do not significantly differ from non-LGB white individuals on moderate distress. The association observed for LGB Black individuals on severe psychological distress is significant and follows the association of other LGB groups. Neighborhood cohesion had the second highest magnitude of impact on LGB white individuals for moderate psychological distress, and the greatest magnitude of impact on LGB white individuals for severe psychological distress. This suggests that neighborhood cohesion is especially important for buffering severe psychological distress for LGB people but has less of an association on moderate psychological distress.
Neighborhood cohesion alone falls short in protecting the mental health of LGB people. We suspect that LGB white individuals experience the greatest protective effect from neighborhood cohesion because of the combination of other protective influences they receive with more cohesive neighborhoods. In our sample, LGB white individuals have on average longer tenure in their neighborhoods, are more likely to be married, more likely to be employed, and have higher educational attainment – all significant factors in reducing the likelihood of psychological distress. Thus, we can posit that LGB people of color benefit at a lower magnitude from neighborhood cohesion considering the lack of other protective factors. Although not available through public NHIS data, neighborhood racial composition, socioeconomic status of the neighborhood, and other contextual factors, are likely playing a role among LGB white individuals; in other words, they are likely to be in a more advantageous position than LGB people of color, and neighborhood cohesion is associated with these larger advantages. Again, sexual orientation and race categories themselves do not determine the health outcomes of LGB populations and people of color. As indicated in this discussion of neighborhood cohesion having larger magnitudes of protection for LGB white individuals compared to others, we understand racial/ethnic-sexual orientation categories to be “markers” of exposure to racism, homophobia, biphobia, and the intersections of these modes of domination (Ford & Airhihenbuwa, 2011; Poteat, 2021; Zuberi & Bonilla-Silva, 2008).
Despite these findings, we must note several limitations. The subsample that identifies as lesbian, gay, and bisexual is relatively small, so to preserve statistical power, we group these individuals together. Along similar lines, because the NHIS is secondary data, there may be respondent bias on the sexual orientation question. However, because individuals may be less likely to disclose their LGB identities, if our findings err from selection bias, they do so in an underestimate of the inequalities presented here. Given that the NHIS only allows for cross-sectional analysis, we are also largely unable to explore causal mechanisms of our variables of interest.
Despite these shortcomings, our findings still indicate that LGB individuals experience greater levels of psychological distress compared to non-LGB people. Although neighborhood cohesion lessens these disparities, it does not lessen them to the same magnitude as non-LGB individuals for moderate psychological distress, nor does it have equal impact by race and ethnicity. Interventions beyond the community or neighborhood level, then, are required to address these disparities. Structural causes of health trends and inequalities (Karas Montez et al., 2021) must be addressed to truly remedy the disparities identified in this analysis.
5. Conclusion
Henning-Smith and Gonzales (Henning-Smith & Gonzales, 2017) made a substantial contribution in identifying that LGB individuals experience lower levels of neighborhood cohesion. They argued for the need to better understand why LGB adults feel this way and what the health implications may be (Henning-Smith & Gonzales, 2017). We have answered one of these questions by demonstrating that there is a greater likelihood of meeting the criteria for moderate and severe psychological distress among LGB individuals as well as the differential impact neighborhood cohesion has on psychological distress for LGB groups compared to their non-LGB counterparts. We echo the need for further research to improve our understanding of diminished neighborhood cohesion and other health implications this disparity produces.
The fact that neighborhood cohesion does not equally protect LGB groups from psychological distress suggests the need for interventions to fill the gap. It is likely that this disparity will exist until the stigmatization, discrimination, and minority stress that accompanies being a sexual minority is remedied. Additionally, because neighborhood cohesion provides a greater magnitude of protection for LGB white individuals than LGB people of color, the stigmatization, discrimination, and minority stress that accompanies being a person of color amplifies these disparities. Efforts to create truly inclusive neighborhoods would be a first step; however, this is not enough. As our analysis shows, when neighborhood cohesion is rated at a maximum score of 4/4, the predicted probabilities of psychological distress among LGB individuals is still more than double that of the non-LGB individuals, and among LGB groups, the predicted probabilities of psychological distress are much higher for LGB Black individuals than others. Greater LGB protections, outside of inclusive neighborhoods, are necessary to address this disparity. City ordinances, state legislation, and federal anti-discrimination protections, truly inclusive health care and access for LGB communities and communities of color, and policies aimed to eliminate other forms of stratification and inequality are essential in diminishing the gap we find in our analysis.
Funding details
We have no sources of funding to disclose.
Data availability statement
The primary data was collected by the Census Bureau, under a contractual agreement with the National Center for Health Statistics (NCHS), a part of the Centers for Disease Control and Prevention (CDC). The data was harmonized across waves by the IPUMS Health Surveys’ team at the University of Minnesota Population Center. Data available at: https://nhis.ipums.org/nhis/
Declaration of competing interest
The authors declare that they have no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2022.101134.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Alegría M., Canino G., Shrout P.E., Woo M., Duan N., Vila D., Torres M., Chen C.N., Meng X.L. Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. American Journal of Psychiatry. 2008;165(3):359–369. doi: 10.1176/APPI.AJP.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen J.P., Zou C., Blosnich J. Multiple early victimization experiences as a pathway to explain physical health disparities among sexual minority and heterosexual individuals. Social Science & Medicine. 2015;133:111–119. doi: 10.1016/J.SOCSCIMED.2015.03.043. [DOI] [PubMed] [Google Scholar]
- Aneshensel C.S. Social stress: Theory and research. Annual Review of Sociology. 1992;18(1):15–38. doi: 10.1146/ANNUREV.SO.18.080192.000311. [DOI] [Google Scholar]
- Balsam K.F. Trauma, stress, and resilience among sexual minority women: Rising Like the phoenix (issue 4) Routledge; 2004. Trauma, stress, and resilience among sexual minority women: Rising like the phoenix. [DOI] [PubMed] [Google Scholar]
- Barnes D.M., Bates L.M. Do racial patterns in psychological distress shed light on the black-white depression paradox? A systematic review. Social Psychiatry and Psychiatric Epidemiology. 2017;52(8):913–928. doi: 10.1007/s00127-017-1394-9. [DOI] [PubMed] [Google Scholar]
- Berkman L.F., Kawachi I., Glymour M.M. Social epidemiology. 2nd ed. Oxford University Press; 2014. https://books.google.com/books?hl=en&lr=&id=qHpYCwAAQBAJ&oi=fnd&pg=PP1&dq=Berkman,+L.+F.,+Kawachi,+I.,+%26+Glymour,+M.+M.+(Eds.).+(2014).+Social+epidemiology.+Oxford+University+Press.&ots=8bjz9DfYmw&sig=n8azc9bwB2Tt_UpRLOLyhMSsXPk [Google Scholar]
- Blazr D.G., Kessler R.C., McGonagle K.A., Swartz M.S. The prevalence and distribution of major depression in a national community sample: The national comorbidity survey. American Journal of Psychiatry. 1994 doi: 10.1176/ajp.151.7.979. https://books.google.com/books?hl=en&lr=&id=fQdYAQAAQBAJ&oi=fnd&pg=PA1&dq=53.%09Blazer,+D.+G.,+Kessler,+R.+C.,+McGonagle,+K.+A.,+%26+Swartz,+M.+S.+(1994).+The+prevalence+and+distribution+of+major+depression+in+a+national+community+sample:+the+National+Comorbidity+Survey.+The+American+journal+of+psychiatry.&ots=IKkTYeYA8F&sig=km12Jd6sn7vu3rpei5Ns7Ufa4Aw#v=onepage&q&f=false [DOI] [PubMed] [Google Scholar]
- Blewett L.A., Drew J.A.R., King M.L., Williams K.C.W. IPUMS. IPUMS. 2019. IPUMS health surveys: National health Interview survey, version 6.4. [DOI] [Google Scholar]
- Borgogna N.C., McDermott R.C., Aita S.L., Kridel M.M. Anxiety and depression across gender and sexual minorities: Implications for transgender, gender nonconforming, pansexual, demisexual, asexual, queer, and questioning individuals. Psychology of Sexual Orientation and Gender Diversity. 2019;6(1) https://psycnet.apa.org/buy/2018-46063-001 [Google Scholar]
- Bostwick W.B., Meyer I., Aranda F., Russell S., Hughes T., Birkett M., Mustanski B. Mental health and suicidality among racially/ethnically diverse sexual minority youths. American Journal of Public Health Bostwick et al. | Peer Reviewed | Research and Practice. 2014;104(6):1129. doi: 10.2105/AJPH.2013.301749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L., Huang J., Brooks K., Black A., Burkholder G. Triple jeopardy and beyond: Multiple minority stress and resilience among Black lesbians. Journal of Lesbian Studies. 2003;7(4):87–108. doi: 10.1300/J155v07n04_06. [DOI] [PubMed] [Google Scholar]
- Bränström R., Pachankis J.E. Sexual orientation disparities in the co-occurrence of substance use and psychological distress: A national population-based study (2008–2015) Social Psychiatry and Psychiatric Epidemiology. 2018;53(4):403–412. doi: 10.1007/S00127-018-1491-4/TABLES/3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne I., Misra J. The intersection of gender and race in the labor market. Annual Review of Sociology. 2003;29:487–513. doi: 10.1146/ANNUREV.SOC.29.010202.100016. [DOI] [Google Scholar]
- Browning C.R., Cagney K.A., Wen M. Explaining variation in health status across space and time: Implications for racial and ethnic disparities in self-rated health. Social Science & Medicine. 2003;57(7):1221–1235. doi: 10.1016/s0277-9536(02)00502-6. https://www.sciencedirect.com/science/article/pii/S0277953602005026 [DOI] [PubMed] [Google Scholar]
- Charles J.L.K. Mental health provider-based stigma: Understanding the experience of clients and families. Social Work in Mental Health. 2013;11(4):360–375. doi: 10.1080/15332985.2013.775998. [DOI] [Google Scholar]
- Cobb S. Social support as a moderator of life stress. Psychosomatic Medicine. 1976;38:300–314. doi: 10.1097/00006842-197609000-00003. https://psycnet.apa.org/record/1977-13045-001 [DOI] [PubMed] [Google Scholar]
- Cochran S.D., Mays V.M. Depressive distress among homosexually active African American men and women. American Journal of Psychiatry. 1994;151(4):524–529. doi: 10.1176/ajp.151.4.524. https://www.ncbi.nlm.nih.gov/pmc/articles/pmc3606487/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran S.D., Mays V.M. Relation between psychiatric syndromes and behaviorally defined sexual orientation in a sample of the US population. American Journal of Epidemiology. 2000;151(5):516–523. doi: 10.1093/OXFORDJOURNALS.AJE.A010238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran S.D., Sullivan J.G., Mays V.M. Prevalence of mental disorders, psychological distress, and mental health services use among lesbian, gay, and bisexual adults in the United States. Journal of Consulting and Clinical Psychology. 2003;71(1):53–61. doi: 10.1037/0022-006X.71.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Syme S.L. Academic Press; 1985. Social support and health.https://psycnet.apa.org/record/1985-97489-000 [Google Scholar]
- Collins P.H. 2nd ed. Routledge; 2000. Black feminist thought: Knowledge, consciousness, and the politics of empowerment.https://books.google.com/books?hl=en&lr=&id=WMGTAgAAQBAJ&oi=fnd&pg=PP1&dq=Collins,+Patricia+Hill.+2000.+Black+Feminist+Thought.+New+York:+Routledge.&ots=qudp4joDrY&sig=N4iGHc-87tg8zZ_hifrj_zN-we0#v=onepage&q=Collins%2C%20Patricia%20Hill.%202000.%20Black%20Feminist%20Thought.%20New%20York%3A%20Routledge.&f=false [Google Scholar]
- Crenshaw K. Mapping the margins: Intersectionality, identity politics, and violence against women of color mapping the margins: Intersectionality, identity politics, and violence against women of color. 1991. http://www.jstor.orgURL:http://www.jstor.org/stable/1229039http://www.jstor.org/stable/1229039?seq=1&cid=pdf-reference#references_tab_contents Stanford Law Review, 1241–1299.
- Delphin-Rittmon M., Bellamy C.D., Ridgway P., Guy K., Ortiz J., Flanagan E., et al. ‘I never really discuss that with my clinician’: U. S. Consumer perspectives on the place of culture in behavioural healthcare. Diversity and Equality in Health and Care. 2013;10:143–154. https://scholar.google.com/scholar?hl=en&as_sdt=0%2C25&q=%E2%80%A2%09Delphin-Rittmon+et+al.+2013+-+Delphin-Rittmon%2C+M.%2C+Bellamy%2C+C.+D.%2C+Ridgway%2C+P.%2C+Guy%2C+K.%2C+Ortiz%2C+J.%2C+Flanagan%2C+E.%2C+et+al.+%282013%29.+%E2%80%98I+never+really+discuss+that+with+my+clinician%E2%80%99%3A+U.+S.+consumer+perspectives+on+the+place+of+culture+in+behavioural+healthcare.+Diversity+and+Equality+in+Health+and+Care%2C+10%2C+143%E2%80%93154.&btnG= [Google Scholar]
- Detrie P., Lease S.H. The relation of social support, connectedness, and collective self-esteem to the psychological well-being of lesbian, gay, and bisexual youth. Journal of Homosexuality. 2007;53(4):173–199. doi: 10.1080/00918360802103449. [DOI] [PubMed] [Google Scholar]
- Díaz R.M., Ayala G., Bein E., Henne J., Marin B.v. The impact of homophobia, poverty, and racism on the mental health of gay and bisexual Latino men: Findings from 3 US cities. American Journal of Public Health. 2001;91(6):932. doi: 10.2105/AJPH.91.6.927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux A.v. Investigating neighborhood and area effects on health. American Journal of Public Health. 2001;91(11):1783–1789. doi: 10.2105/ajph.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dominguez-Fuentes J.M., Hombrados-Mendieta M., Garcia-Leiva P. Social support and life satisfaction among gay men in Spain. Journal of Homosexuality. 2012;59(2):241–255. doi: 10.1080/00918369.2012.648879. [DOI] [PubMed] [Google Scholar]
- Echeverría S., Diez-Roux A.v., Shea S., Borrell L.N., Jackson S. Associations of neighborhood problems and neighborhoodsocial cohesion with mental health and health behaviors: The Multi-Ethnic Study of Atherosclerosis. Health & Place. 2008;14(4):853–865. doi: 10.1016/j.healthplace.2008.01.004. https://reader.elsevier.com/reader/sd/pii/S1353829208000105?token=BA334FAC34206658C54D152B4912315F762961A3A783599CC03D1595ECA464BFC4CB9C4F8AF9D66D6C6B3015586CDEF9&originRegion=us-east-1&originCreation=20211018205705 [DOI] [PubMed] [Google Scholar]
- Eliason M.J., Fogel S.C. An ecological framework for sexual minority women's health: Factors associated with greater body mass. Journal of Homosexuality. 2015;62(7):845–882. doi: 10.1080/00918369.2014.1003007. [DOI] [PubMed] [Google Scholar]
- Elliott J., Gale C.R., Parsons S., Kuh D., The HALCyon Study Team Neighbourhood cohesion and mental wellbeing among older adults: A mixed methods approach. Social Science & Medicine. 2014;107:44–51. doi: 10.1016/J.SOCSCIMED.2014.02.027. [DOI] [PubMed] [Google Scholar]
- Erving C.L., Thomas C.S. Race, emotional reliance, and mental health. Society and Mental Health. 2018;8(1):69–83. doi: 10.1177/2156869317713552. [DOI] [Google Scholar]
- Ford C.L., Airhihenbuwa C.O. Critical race theory, race equity, and public health: Toward antiracism praxis. 2011. Https://Doi.Org/10.2105/AJPH.2009.171058, 100(SUPPL. 1) [DOI] [PMC free article] [PubMed]
- Frost D.M., Lehavot K., Meyer I.H. Minority stress and physical health among sexual minority individuals. Journal of Behavioral Medicine. 2015;38(1):1–8. doi: 10.1007/S10865-013-9523-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost D.M., Meyer I.H., Schwartz S. Social support networks among diverse sexual minority populations. American Journal of Orthopsychiatry. 2016;86(1):91–102. doi: 10.1037/ORT0000117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrett-Walker J.J., Longmire-Avital B. Resilience and depression: The roles of racial identity, sexual identity, and social support on well-being for Black LGB emerging adults. Journal of Black Sexuality and Relationships. 2018;4(4):1–15. https://muse.jhu.edu/article/705355/summary [Google Scholar]
- Ghabrial M.A. Trying to figure out where we belong”: Narratives of racialized sexual minorities on community, identity, discrimination, and health. Sexuality Research and Social Policy. 2017;14(1):42–55. doi: 10.1007/s13178-016-0229-x. [DOI] [Google Scholar]
- Gibson P. Gay male and lesbian youth suicide. Prevention and intervention in youth suicide (report to the secretary's task force on youth suicide. https://ci.nii.ac.jp/naid/10026901423/ n.d. Vol. 3, Retrieved October 17, 2021, from.
- Gilman S.E., Cochran S.D., Mays V.M., Hughes M., Ostrow D., Kessler R.C. Risk of psychiatric disorders among individuals reporting same-sex sexual partners in the National Comorbidity Survey. American Journal of Public Health. 2001;91(6):939. doi: 10.2105/AJPH.91.6.933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein N.D., Burstyn I., LeVasseur M.T., Welles S.L. Drug use among men by sexual behaviour, race and ethnicity: Prevalence estimates from a nationally representative US sample. International Journal of Drug Policy. 2016;36:148–150. doi: 10.1016/J.DRUGPO.2016.01.008. [DOI] [PubMed] [Google Scholar]
- Gonzales L., Davidoff K.C., Nadal K.L., Yanos P.T. Microaggressions experienced by persons with mental illnesses: An exploratory study. Psychiatric Rehabilitation Journal. 2015;38(3):234–241. doi: 10.1037/prj0000096. https://psycnet.apa.org/buy/2014-48757-001 [DOI] [PubMed] [Google Scholar]
- Gonzales G., Henning-Smith C. Health disparities by sexual orientation: Results and implications from the behavioral risk factor surveillance system. Journal of Community Health. 2017;42(6):1163–1172. doi: 10.1007/S10900-017-0366-Z. [DOI] [PubMed] [Google Scholar]
- Gonzales G., Przedworski J., Henning-Smith C. Comparison of health and health risk factors between lesbian, gay, and bisexual adults and heterosexual adults in the United States: Results from the national health Interview survey. JAMA Internal Medicine. 2016;176(9):1344–1351. doi: 10.1001/JAMAINTERNMED.2016.3432. [DOI] [PubMed] [Google Scholar]
- Granovetter M.S. The strength of weak ties. American Journal of Sociology. 1973;78(6):1360–1380. https://www.jstor.org/stable/pdf/2776392.pdf [Google Scholar]
- Combahee River Collective . In: Words of fire: An anthology of African American feminist thought. Guy-Sheftall B., editor. New Press; 1995. The Combahee River collective statement; pp. 232–240. [DOI] [Google Scholar]
- Harker K. Immigrant generation, assimilation, and adolescent psychological well-being. Social Forces. 2001;79(3):969–1004. doi: 10.1353/SOF.2001.0010. [DOI] [Google Scholar]
- Hatzenbuehler M.L. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological Bulletin. 2009;135(5):707–730. doi: 10.1037/A0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler M.L., Birkett M., van Wagenen A., Meyer I.H. Protective school climates and reduced risk for suicide ideation in sexual minority youths. American Journal of Public Health. 2014;104(2):279–286. doi: 10.2105/AJPH.2013.301508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henning-Smith C., Gonzales G. Differences by sexual orientation in perceptions of neighborhood cohesion: Implications for health. Journal of Community Health. 2017;43(3):578–585. doi: 10.1007/S10900-017-0455-Z. [DOI] [PubMed] [Google Scholar]
- Holley, L. C., Tavassoli, K. Y., & Stromwall, L. K. (n.d.). Mental illness discrimination in mental health treatment programs: Intersections of race, ethnicity, and sexual orientation. Community Mental Health Journal, 52. 10.1007/s10597-016-9990-9. [DOI] [PubMed]
- Hong S., Zhang W., Walton E. Neighborhoods and mental health: Exploring ethnic density, poverty, and social cohesion among Asian Americans and Latinos. Social Science & Medicine. 2014;111:117–124. doi: 10.1016/J.SOCSCIMED.2014.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes T.L., Johnson T.P., Matthews A.K. Sexual orientation and smoking: Results from a multisite women's health study. Substance Use & Misuse. 2008;43(8–9):1218–1239. doi: 10.1080/10826080801914170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes T.L., Matthews A.K. Race/ethnicity and sexual orientation: Intersecting identities. Cultural Diversity and Ethnic Minority Psychology. 2004;10(3):241–254. doi: 10.1037/1099-9809.10.3.241. [DOI] [PubMed] [Google Scholar]
- Karas Montez J., Hayward M.D., Zajacova A. Trends in U.S. Population health: The central role of policies, politics, and profits. Journal of Health and Social Behavior. 2021;62(3):286–301. doi: 10.1177/00221465211015411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I., Berkman L. In: Social epidemiology. Kawachi I., Berkman L., editors. Oxford University Press; 2000. Social cohesion, social capital, and health; pp. 174–190.https://books.google.com/books?hl=en&lr=&id=i0qWxy5-X1gC&oi=fnd&pg=PA174&dq=96.%09Kawachi,+I.,+%26+Berkman,+L.+(2000).+Social+cohesion,+social+capital,+and+health.+In+L.+F.+Berkman,+%26+I.+Kawachi+(Eds.),+Social+epidemiology+(pp.+174%E2%80%93190).+Oxford:+Oxford+University+Press.&ots=NKS69bnp67&sig=IfPQ9jw7I8atoDVpbfGTeblgsK8 [Google Scholar]
- Kawachi I., Berkman L.F. Social ties and mental health. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2001;78(3) doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerridge B.T., Pickering R.P., Saha T.D., Ruan W.J., Chou S.P., Zhang H., Jung J., Hasin D.S. Prevalence, sociodemographic correlates and DSM-5 substance use disorders and other psychiatric disorders among sexual minorities in the United States. Drug and Alcohol Dependence. 2017;170:82–92. doi: 10.1016/J.DRUGALCDEP.2016.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Andrews G., Colpe L.J., Hiripi E., Mroczek D.K., normand S.L.T., Walters E.E., Zaslavsky A.M. Short screening scales to monitor population prevalence and trends in non-specific psychological distress. Psychological Medicine. 2002;32(6):959–976. doi: 10.1017/S0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Barker P.R., Colpe L.J., Epstein J.F., Gfroerer J.C., Hiripi E., Howes M.J., Normand S.-L.T., Manderscheid R.W., Walters E.E., Zaslavsky A.M. Screening for serious mental illness in the general population. Archives of General Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. https://jamanetwork.com/journals/jamapsychiatry/article-abstract/207204 [DOI] [PubMed] [Google Scholar]
- Kessler R.C., McGonagle K.A., Zhao S., Nelson C.B., Hughes M., Eshleman S., Wittchen H.-U., Kendler K.S. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the national comorbidity survey. Archives of General Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. http://apsychoserver.psych.arizona.edu/JJBAReprints/PSYC621/Kessler%20et%20al_Lifetime%20and%2012%20months%20prevalence_Archives%20of%20Gen%20Psychiatry_%60994.pdf [DOI] [PubMed] [Google Scholar]
- Kidd S.A., Veltman A., Gately C., Chan K.J., Cohen J.N. Lesbian, gay, and transgender persons with severe mental illness: Negotiating wellness in the context of multipl... Cite this paper related papers severe ment al Illness in LGBT populat ions: A scoping review. American Journal of Psychiatric Rehabilitation. 2011;14:13–39. doi: 10.1080/15487768.2011.546277. [DOI] [Google Scholar]
- Kiecolt K.J., Hughes M., Keith V.M. Race, social relationships, and mental health. Personal Relationships. 2008;15(2):229–245. doi: 10.1111/J.1475-6811.2008.00195.X. [DOI] [Google Scholar]
- Kim H.-J., Fredriksen-Goldsen K.I. Hispanic lesbians and bisexual women at heightened risk or health disparities. American Journal of Public Health. 2012;102:9–15. doi: 10.2105/AJPH.2011.300378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H.J., Fredriksen-Goldsen K.I. Nonresponse to a question on self-identified sexual orientation in a public health survey and its relationship to race and ethnicity. American Journal of Public Health. 2013;103(1):67–69. doi: 10.2105/AJPH.2012.300835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim E.S., Park N., Peterson C. Perceived neighborhood social cohesion and stroke. Social Science & Medicine. 2013;97:49–55. doi: 10.1016/J.SOCSCIMED.2013.08.001. [DOI] [PubMed] [Google Scholar]
- Krieger N. Enough: COVID-19, structural racism, police brutality, plutocracy, climate change—and time for health justice, democratic governance, and an equitable, sustainable future. American Journal of Public Health. 2020;110 doi: 10.2105/AJPH.2020.305886. https://ajph.aphapublications.org/doi/pdfplus/10.2105/AJPH.2020.305886 –111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lassiter J.M., Poteat T. Religious coping and depressive symptoms among black Americans living with HIV: An intersectional approach. Psychology of Religion and Spirituality. 2020;12(3):268. doi: 10.1037/REL0000284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lassiter J.M., Saleh L., Grov C., Starks T., Ventuneac A., Parsons J.T. Spirituality and multiple dimensions of religion are associated withMental health in gay and bisexual men: Results from the one thousand strong cohort. Psychology of Religion and Spirituality. 2019;11(4):416. doi: 10.1037/REL0000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauby J.L., Marks G., Bingham T., Liu K.-L., Liau A., Stueve A., Millett G.A. Having supportive social relationships is associated with reduced risk of unrecognized HIV infection among black and Latino men who have sex with men. AIDS and Behavior. 2012;16(3):508–515. doi: 10.1007/s10461-011-0002-3. [DOI] [PubMed] [Google Scholar]
- Lee J.G.L., Shook-Sa B.E., Gilbert J., Ranney L.M., Goldstein A.O., Boynton M.H. Risk, resilience, and smoking in a national, probability sample of sexual and gender minority adults, 2017, USA. Health Education & Behavior. 2020;47(2):272–283. doi: 10.1177/1090198119893374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehavot K., Beckman K.L., Chen J.A., Simpson T.L., Williams E.C. Race/ethnicity and sexual orientation disparities in mental health, sexism, and social support among women veterans. Psychol Sex Orientat Gend Divers. 2019;6(3):347–358. doi: 10.1037/sgd0000333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lick D.J., Durso L.E., Johnson K.L. Minority stress and physical health among sexual minorities. Perspectives on Psychological Science. 2013;8(5):521–548. doi: 10.1177/1745691613497965. [DOI] [PubMed] [Google Scholar]
- Lochner K.A., Kawachi I., Brennan R.T., Buka S.L. Social capital and neighborhood mortality rates in Chicago. Social Science & Medicine. 2003;56(8):1797–1805. doi: 10.1016/s0277-9536(02)00177-6. https://www.sciencedirect.com/science/article/pii/S0277953602001776 [DOI] [PubMed] [Google Scholar]
- López J.D., Duncan A., Shacham E., McKay V. Disparities in health behaviors and outcomes at the intersection of race and sexual identity among women: Results from the 2011–2016 National Health and Nutrition Examination Survey. Preventive Medicine. 2021;142 doi: 10.1016/J.YPMED.2020.106379. [DOI] [PubMed] [Google Scholar]
- Lytle M.C., de Luca S.M., Blosnich J.R., Brownson C. Associations of racial/ethnic identities and religious affiliation with suicidal ideation among lesbian, gay, bisexual, and questioning individuals. Journal of Affective Disorders. 2015;178:39–45. doi: 10.1016/J.JAD.2014.07.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macinko J., Starfield B. The utility of social capital in research on health determinants. The Milbank Quarterly. 2001;79(3):387–427. doi: 10.1111/1468-0009.00213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahowald L., Gruberg S., Halpin J. The state of the LGBTQ community in 2020. 2020. https://cdn.americanprogress.org/content/uploads/2020/10/02103624/LGBTQpoll-report.pdf
- Mereish E.H., Bradford J.B. Intersecting identities and substance use problems: Sexual orientation, gender, race, and lifetime substance use problems. Journal of Studies on Alcohol and Drugs. 2014;75(1):179–188. doi: 10.15288/JSAD.2014.75.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer I.H. Minority stress and mental health in gay men. Journal of Health and Social Behavior. 1995;36:38–56. doi: 10.2307/2137286. [DOI] [PubMed] [Google Scholar]
- Meyer I.H. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. https://psycnet.apa.org/buy/2003-99991-002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer I.H., Frost D.M. In: Handbook of psychology and sexual orientation. Patterson C.J., D'Augelli A.R., editors. Oxford University Press; 2013. Minority stress and the health of sexual minorities; pp. 252–266.https://psycnet.apa.org/record/2012-32754-018?fbclid=IwAR1VEV_u7htVFNGV_a_huxb6Kh7luQUB33TS0Ezzqo34wMrRpgkvHVeAKTk [Google Scholar]
- Meyer I.H., Ouellette S.C., Haile R., McFarlane T.A. We'd Be free”: Narratives of life without homophobia, racism, or sexism. Sexuality Research and Social Policy. 2011;8(3):204–214. doi: 10.1007/S13178-011-0063-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer I.H., Schwartz S., Frost D.M. Social patterning of stress and coping: Does disadvantaged social statuses confer more stress and fewer coping resources? Social Science & Medicine. 2008;67(3):368–379. doi: 10.1016/J.SOCSCIMED.2008.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouzon D.M. Relationships of choice: Can friendships or fictive kinships explain the race paradox in mental health? Social Science Research. 2014;44:32–43. doi: 10.1016/J.SSRESEARCH.2013.10.007. [DOI] [PubMed] [Google Scholar]
- Murillo R., Echeverria S., Vasquez E. Differences in neighborhood social cohesion and aerobic physical activity by Latino subgroup. SSM - Population Health. 2016;2:536–541. doi: 10.1016/j.ssmph.2016.08.003. https://www.sciencedirect.com/science/article/pii/S2352827316300490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortega A.N., Rosenheck R.M.D., Alegria M., Desai R.A. Acculturation and the lifetime risk of psychiatric and substance use disorders among hispanics. The Journal of Nervous and Mental Disease. 2000;188(11):728–735. doi: 10.1097/00005053-200011000-00002. https://journals.lww.com/jonmd/Abstract/2000/11000/Acculturation_and_the_Lifetime_Risk_of_Psychiatric.2.aspx [DOI] [PubMed] [Google Scholar]
- Parent M.C., Arriaga A., Gobble T., Wille L. Stress and substance use among sexual and gender minority individuals across the lifespan. Neurobiology of Stress. 2019;10 doi: 10.1016/J.YNSTR.2018.100146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park I.Y., Speer R., Whitfield D.L., Kattari L., Walls E.N., Christensen C. Predictors of bullying, depression, and suicide attempts among youth: The intersection of race/ethnicity by gender identity. Children and Youth Services Review. 2022;139 doi: 10.1016/J.CHILDYOUTH.2022.106536. [DOI] [Google Scholar]
- Pew Research Center A survey of LGBT Americans. 2013. https://www.pewresearch.org/social-trends/2013/06/13/a-survey-of-lgbt-americans/
- Pew Research Center Attitudes on same-sex marriage. 2019, May 14. https://www.pewforum.org/fact-sheet/changing-attitudes-on-gay-marriage/
- Platt L., Jen S., Goldsen J.… Sexual orientation and psychological distress: Differences by race and gender related papers who says I do: T he changing cont ext of marriage and healt h and qualit y of life for LGBT old. Journal of Gay & Lesbian Mental Health. 2018 doi: 10.1080/19359705.2018.1437583. [DOI] [Google Scholar]
- Plöderl M., Tremblay P. Mental health of sexual minorities. A systematic review. International Review of Psychiatry. 2015;27(5):367–385. doi: 10.3109/09540261.2015.1083949. [DOI] [PubMed] [Google Scholar]
- Poteat T. Navigating the storm: How to apply intersectionality to public health in times of crisis. American Journal of Public Health. 2021;111(1):91–92. doi: 10.2105/AJPH.2020.305944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska J.J., Sung H.Y., Max W., Shi Y., Ong M. Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. International Journal of Methods in Psychiatric Research. 2012;21(2):88–97. doi: 10.1002/MPR.1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remafedi G., French S., Story M., Resnick M.D., Blum R. The relationship between suicide risk and sexual orientation: Results of a population-based study. American Journal of Public Health. 1998;88(1):57–60. doi: 10.2105/AJPH.88.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice C.E., Vasilenko S.A., Fish J.N., Lanza S.T. Sexual minority health disparities: An examination of age-related trends across adulthood in a national cross-sectional sample. Annals of Epidemiology. 2019;31:20–25. doi: 10.1016/J.ANNEPIDEM.2019.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley A.R. Neighborhood disadvantage, residential segregation, and beyond—lessons for studying structural racism and health. Journal of Racial and Ethnic Health Disparities. 2017;5(2):357–365. doi: 10.1007/S40615-017-0378-5. 2017 5:2. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Seijas C., Eaton N.R., Pachankis J.E. Prevalence of psychiatric disorders at the intersection of race and sexual orientation: Results from the national epidemiologic survey of alcohol and related. Journal of Consulting and Clinical Psychology. 2019;87(4):321–331. doi: 10.1037/ccp0000377. [DOI] [PubMed] [Google Scholar]
- Russell S.T., Fish J.N. Mental health in lesbian, gay, bisexual, and transgender (LGBT) youth. Annual Review of Clinical Psychology. 2016;12:465–487. doi: 10.1146/ANNUREV-CLINPSY-021815-093153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan C., Huebner D., Diaz R.M., Sanchez J. Family rejection as a predictor of negative health outcomes in white and Latino lesbian, gay, and bisexual young adults. Pediatrics. 2009;123(1):346–352. doi: 10.1542/PEDS.2007-3524. [DOI] [PubMed] [Google Scholar]
- Sampson R.J., Raudenbush S.W., Earls F. Neighborhoods and violent crime: A multilevel study in collective efficacy. Science. 1997;227:918–924. doi: 10.1126/science.277.5328.918. http://users.soc.umn.edu/∼uggen/Sampson_SCI_97.pdf [DOI] [PubMed] [Google Scholar]
- Sheets R.L., Jr., Mohr J.J. Perceived social support from friends and family and psychosocial functioning in bisexual young adult college students. Journal of Counseling Psychology. 2009;56(1):152–163. https://psycnet.apa.org/record/2009-00624-006 [Google Scholar]
- StataCorp . Vol. 17. StataCorp; 2021. (Stata statistical software: Release). (No. 17) [Google Scholar]
- Stromwall L.K., Holley L.C., Bashor K.E. Stigma in the mental health workplace: Perceptions of peer employees and clinicians. Community Mental Health Journal. 2011;47(4):472–481. doi: 10.1007/S10597-010-9349-6. [DOI] [PubMed] [Google Scholar]
- Toomey R.B., Ryan C., Diaz R.M., Russell S.T. High school gay-straight alliances (GSAs) and young adult well-being: An examination of GSA presence, participation, and perceived effectiveness. Applied Developmental Science. 2011;15(4):175–185. doi: 10.1080/10888691.2011.607378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vega W.A., Rumbaut R.G. Ethnic minorities and mental health. American Review of Sociology. 1991;15:351–383. https://www.jstor.org/stable/pdf/2083347.pdf [Google Scholar]
- Walch S.E., Ngamake S.T., Bovornusvakool W., Walker S.v. Discrimination, internalized homophobia, and concealment in sexual minority physical and mental health. Psychology of Sexual Orientation and Gender Diversity. 2016;3(1):37–48. https://psycnet.apa.org/buy/2015-55071-001 [Google Scholar]
- Walker J.J., Longmire-Avital B. Racial and sexual identities as potential buffers to risky sexual behavior for Black gay and bisexual emerging adult men. Health Psychology. 2015;34(8) doi: 10.1037/hea0000187. [DOI] [PubMed] [Google Scholar]
- Weber A., Collins S.-A., Robinson-Wood T., Zeko-Underwood E., Poindexter B. Subtle and severe: Microaggressions among racially diverse sexual minorities. Journal of Homosexuality. 2018;65(4):540–559. doi: 10.1080/00918369.2017.1324679. [DOI] [PubMed] [Google Scholar]
- Weissman J.D., Lim S., Durr M., el Shahawy O., Russell D. The current social environment and its association with serious psychological distress among adults who identify as lesbian, gay, and bisexual: Findings from the national health Interview survey (2013–2018) Journal of Public Health. 2021 doi: 10.1007/S10389-021-01633-8. [DOI] [Google Scholar]
- Weston K. Columbia University Press; 1997. Families we choose: Lesbians, gays, kinship.https://books.google.com/books?hl=en&lr=&id=prYIC_uH474C&oi=fnd&pg=PR11&dq=84.%09Weston,+K.+(1997).+Families+we+choose:+Lesbians,+gays,+kinship.+Columbia+University+Press.&ots=tl9p9BJqUp&sig=B8mZkRom3he0KPvP7l4zHmrPCKA [Google Scholar]
- Williams D.R. In: America becoming: Racial trends and their consequences. Smesler N., Wilson W.J., Mitchell F., editors. National Academy of Sciences Press; 2001. Racial variations in adult health status: Patterns, paradoxes and prospects; pp. 371–410.https://scholar.harvard.edu/davidrwilliams/dwilliam/publications/racial-variations-adult-health-status-patterns-paradoxes-and-prospects [Google Scholar]
- Williams D.R., Lawrence J.A., Davis B.A. Racism and health: Evidence and needed research. Annual Review of Public Health. 2019;40:105–125. doi: 10.1146/ANNUREV-PUBLHEALTH-040218-043750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilton L., Chiasson M.A., Nandi V., Lelutiu-Weinberger C., Frye V., Hirshfield S., Hoover D.R., Downing M.J., Lucy D., Usher D., Koblin B. Characteristics and correlates of lifetime suicidal thoughts and attempts among young black men who have sex with men (MSM) and transgender women. Journal of Black Psychology. 2018;44(3):273–290. doi: 10.1177/0095798418771819. [DOI] [Google Scholar]
- Yi S.S., Trinh-Shevrin C., Yen I.H., Kwon S.C. Racial/ethnic differences in associations between neighborhood social cohesion and meeting physical activity guidelines, United States, 2013–2014. Preventing Chronic Disease: Public Health Research, Practice, and Policy. 2016;13 doi: 10.5888/pcd13.160261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshikawa H., Alan-David Wilson P., Chae D.H., Cheng J.-F. Do family and friendship networks protect against the influence of discrimination on mental health and HIV risk among Asian and Pacific Islander gay men? AIDS Education and Prevention. 2004;16(1):84–100. doi: 10.1521/AEAP.16.1.84.27719. [DOI] [PubMed] [Google Scholar]
- Zamboni B.D., Crawford I. Minority stress and sexual problems among African-American gay and bisexual men. Archives of Sexual Behavior. 2007;36(4):569–578. doi: 10.1007/S10508-006-9081-Z. [DOI] [PubMed] [Google Scholar]
- Zuberi T., Bonilla-Silva E. In: White logic, white methods: Racism and methodology. Zuberi T., Bonilla S.-E., editors. Rowman & Littlefield; 2008. https://books.google.com/books?hl=en&lr=&id=WTBtAAAAQBAJ&oi=fnd&pg=PP1&dq=+White+logic,+white+methods:+Racism+and+methodology.+Rowman+%26+Littlefield+Publishers.&ots=vchPj1z97t&sig=40PT_1GWi4L-VNBDx4Sc1uMc4vs#v=onepage&q=White%20logic%2C%20white%20methods%3A%20Racism%20and%20methodology.%20Rowman%20%26%20Littlefield%20Publishers.&f=false [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The primary data was collected by the Census Bureau, under a contractual agreement with the National Center for Health Statistics (NCHS), a part of the Centers for Disease Control and Prevention (CDC). The data was harmonized across waves by the IPUMS Health Surveys’ team at the University of Minnesota Population Center. Data available at: https://nhis.ipums.org/nhis/