SUMMARY
In September 2010, an outbreak of cryptosporidiosis affected members of a swimming club. A cohort study was undertaken to identify the number affected and risk factors for infection. Of 101 respondents, 48 met the case definition for probable cryptosporidiosis. Multivariate analysis demonstrated a strong and highly significant association between illness and attendance at a training session on 13 September 2010 (adjusted odds ratio 28, P < 0·0001). No faecal incidents were reported and pool monitoring parameters were satisfactory. The competitive nature of club swimming requires frequent training and participation in galas, potentially facilitating contamination into other pools and amplification of outbreaks among wider groups of swimmers. There was a lack of awareness of the 2-week exclusion rule among swimmers and coaches, and a high level of underreporting of illness. The study demonstrates the benefits of rapid field epidemiology in identifying the true burden of illness, the source of infection and limiting spread.
Key words: Cryptosporidium, outbreaks, swimming club
The protozoan parasite Cryptosporidium is an important cause of gastrointestinal illness. About 4000 laboratory-confirmed cases are reported to the Health Protection Agency each year from England and Wales (http://www.hpa.org.uk). Infection with Cryptosporidium causes watery diarrhoea, abdominal cramps, low grade fever, vomiting, nausea and loss of appetite. Cryptosporidium spp. infect animals as well as people, and transmission is via ingestion of oocysts shed in faeces. The incubation period is 3–12 days and the duration of illness varies but is usually about 12 days [1]. Some groups of immunocompromised patients suffer more severe and prolonged illness [2].
Infection is easily acquired because of a very low infectious dose [3] and the survival of oocysts for long periods in the environment. The parasite is resistant to conventional chlorine disinfection used in water treatment. Consequently, large waterborne outbreaks have been associated with contamination of both drinking water and recreational waters [4, 5]. Oocysts can be shed in stools for 2 weeks following cessation of symptoms: hence the advice for diagnosed cases not to swim while ill or for this period after cessation of symptoms [6]. This paper describes the investigation of an outbreak of cryptosporidiosis in members of a swimming club in Greater Manchester.
On 22 September 2010, Greater Manchester Health Protection Unit (GMHPU) was contacted by an Environmental Health Officer (EHO) from a local city council to report 11 children from a local amateur swimming club with diarrhoea and stomach cramps. All were contacted to complete a preliminary questionnaire and arrange for faecal samples to be submitted. Cryptosporidium surveillance at GMHPU had only identified one case who had swum in this pool earlier in February 2010. The club is based at a leisure centre with a 25-m swimming pool. There are over 200 members aged 4–20 years. The club trains four evenings each week and competes in regular galas. At other times, the pool is used by about 60 local schools, members of the public and for swimming classes for young babies and adults with learning difficulties. The pool is run by the local Leisure Trust and is not subject to regular pool inspection by the Environmental Health Team at the City Council.
Case-finding was undertaken by requesting neighbouring HPUs, local general practitioners, paediatricians, walk-in centres and microbiologists to report suspected cases of cryptosporidiosis linked to the swimming pool to GMHPU and to obtain a faecal specimen, where appropriate.
Initial questioning of eight cases suggested that illness was linked to attendance at a training event on 13 September 2010. The onset of illness was between 18 and 21 September 2010 and symptoms included diarrhoea, vomiting, nausea, pyrexia and abdominal cramps. The first case of cryptosporidiosis was laboratory confirmed by auramine microscopy on 27 September 2010 and two further cases were confirmed on 28 September 2010. The three positive specimens obtained were typed by the national Cryptosporidium Reference Unit, Public Health Wales, Swansea, by real-time PCR [7] and were C. hominis. An outbreak was declared and an Outbreak Control Team (OCT) established with representatives from GMHPU, City Council Environmental Health Department, HPA regional epidemiology, regional laboratory and communications, and local Primary Care Trust (PCT).
A retrospective cohort study was undertaken to identify risk factors for infection in members of the swimming club. A list of the 129 active members of the club was obtained. They were contacted using a combination of face-to-face interviews of parents at training sessions and telephone interviews.
A probable case was defined as a member of the swimming club with onset of illness in September 2010 and having one or more of the following symptoms: diarrhoea (⩾3 loose stools in 24 h), abdominal cramps, loss of appetite, fever, nausea, vomiting, without microbiological confirmation of Cryptosporidium infection.
A confirmed case was a probable case with microbiological confirmation of Cryptosporidium. Individuals with a history of foreign travel in the 2 weeks preceding onset of illness were excluded from the study.
A questionnaire was developed to collect information on the nature of illness and key exposures (including swimming at the pool on specified training dates, swimming at galas, eating/drinking at events and swimming at other pools). Questionnaire data were entered and checked using EpiData Entry software (EpiData Association, Denmark). After descriptive and univariate analysis the parameters of a multivariate logistic regression model of predictors of illness were estimated, using Stata statistical software (StataCorp LP, USA).
Forty-eight cases fitting the probable case definition and 53 non-cases were recruited to the cohort study (a response rate of 78%). Cases had a median age of 9 years (range 4–26 years) and non-cases had a median age of 9 years (range 4–17 years). Fifty-two percent (25/48) of cases were male compared to 42% (22/53) of non-cases. Cases attended 22 different schools.
Cases reported a median duration of illness of 3 days (range 1–9 days, mean 3·75 days). The commonest symptom reported was diarrhoea (77%) followed by vomiting (75%), loss of appetite (71%), abdominal pain (67%), nausea (67%), and fever (52%). No cases reported blood in their stools. Thirty-five cases reported taking time off work or school due to illness and two cases were hospitalized. Univariate analysis showed association of illness with three swimming events: 6, 13 and 17 September 2010 (Table 1).
Table 1.
Risk factor analysis of exposure and illness
| Risk factor | Exposed | Not exposed | RR | 95% CI | P | aOR | s.e. | P | 95% CI | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | n | Ill | AR (%) | 95% CI | n | Ill | AR (%) | 95% CI | ||||||||
| Training 6 Sept. 2010 | 101 | 51 | 35 | 68·6 | 55·0–79·7 | 50 | 13 | 26 | 15·9–39·6 | 2·64 | 1·60–4·37 | <0·0001 | — | — | — | — |
| Training 8 Sept. 2010 | 101 | 25 | 15 | 60 | 40·7–76·6 | 76 | 33 | 43·4 | 32·9–54·6 | 1·38 | 0·92–2·08 | 0·1499 | — | — | — | — |
| Training 10 Sept. 2010 | 101 | 55 | 24 | 43·6 | 31·4–56·7 | 46 | 24 | 52·2 | 38·1–65·9 | 0·84 | 0·56–1·26 | 0·3922 | — | — | — | — |
| Training 11 Sept. 2010 | 101 | 19 | 12 | 63·2 | 41·0–80·9 | 82 | 36 | 43·9 | 33·7–54·7 | 1·44 | 0·94–2·19 | 0·1299 | — | — | — | — |
| Training 13 Sept. 2010 | 101 | 56 | 41 | 73·2 | 60·4–83·0 | 45 | 7 | 15·6 | 7·7–28·8 | 4·71 | 2·34–9·47 | <0·0001 | 28·14 | 18·03 | 0 | 8·02–98·77 |
| Training 15 Sept. 2010 | 101 | 19 | 11 | 57·9 | 36·3–76·9 | 82 | 37 | 45·1 | 34·8–55·9 | 1·28 | 0·82–2·02 | 0·3151 | — | — | — | — |
| Training 17 Sept. 2010 | 101 | 49 | 16 | 32·7 | 21·2–46·6 | 52 | 32 | 61·5 | 48·0–73·5 | 0·53 | 0·34–0·84 | 0·0037 | — | — | — | — |
| Training 18 Sept. 2010 | 101 | 15 | 8 | 53·3 | 30·1–75·2 | 86 | 40 | 46·5 | 36·3–57·0 | 1·15 | 0·68–1·94 | 0·6254 | — | — | — | — |
| Gala 5 Sept. 2010 | 101 | 18 | 12 | 66·7 | 43·7–83·7 | 83 | 36 | 43·4 | 33·2–54·1 | 1·54 | 1·02–2·31 | 0·0728 | — | — | — | — |
| Gala 6 Sept. 2010 | 101 | 7 | 6 | 85·7 | 48·7–97·4 | 94 | 42 | 44·7 | 35·0–54·7 | 1·92 | 1·32–2·80 | 0·0511 | 37·89 | 54·98 | 0·012 | 2·21–650·94 |
| Gala 11 Sept. 2010 | 101 | 5 | 3 | 60 | 23·1–88·2 | 96 | 45 | 46·9 | 37·2–56·8 | 1·28 | 0·61–2·70 | 0·6664 | — | — | — | — |
| Gala 12 Sept. 2010 | 101 | 3 | 2 | 66·7 | 20·8–93·9 | 98 | 46 | 46·9 | 37·4–56·7 | 1·42 | 0·62–3·25 | 0·6031 | — | — | — | — |
| Gala 17 Sept. 2010 | 101 | 19 | 12 | 63·2 | 41·0–80·9 | 82 | 36 | 43·9 | 33·7–54·7 | 1·44 | 0·94–2·19 | 0·1299 | — | — | — | — |
AR, Attack rate; CI, confidence interval; RR, relative risk; OR, odds ratio.
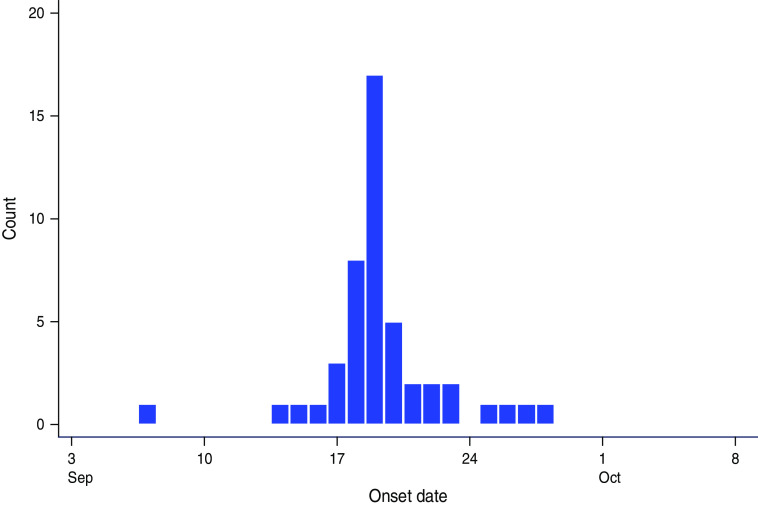
The epidemic curve illustrates a point-source outbreak (Fig. 1). Later cases may indicate secondary spread within families or schools. Case 1 is a potential source of the outbreak as he had the earliest onset of illness in this incident.
Fig. 1.
[colour online]. Epidemic curve by date of onset of probable cases.
Multivariate analysis (Table 1) supported the hypothesis that the training event on 13 September 2010 was a significant exposure. The association was strong and highly statistically significant. There was also a strong association between illness and attendance at the gala on 6 September 2010 [odds ratio (OR) 28, P < 0·0001]. This suggests more than one exposure event. However, the exposure on 13 September 2010 would explain a higher proportion of cases and is consistent with a point-source exposure as represented on the epidemic curve. In the final multivariable logistic regression model, swimmers aged ⩾12 years were significantly less likely to be cases (adjusted OR 0·18, 95% confidence interval 0·03–0·70, P = 0·017). There was no evidence of association between illness and factors such as eating specific food items, use of toilets, changing rooms or showers. Most respondents reported putting their head under water.
The Environmental Health team arranged an inspection of the pool, plant room, changing areas and records on 28 September 2010. The Leisure Trust undertook pool water testing three times a day for free chlorine, combined chlorine and pH and monthly pool water testing for microbiology. Standards of cleanliness and repair were satisfactory. On 6 October 2010, a further visit to the pool was made and water samples obtained for microbiological analysis in accordance with swimming pool water, treatment and quality standards (PWTAG 2009) [8]. The pool water filtration system comprised two multi-grade sand filters (comprising 450 mm 16/30 grade sand over 465 mm multi-grade course media) and automatic coagulant dosing with polyaluminium chloride. The pool water turnover rate is 2·5 h. Backwashing occurred once a week on a Wednesday at noon. There had been no recorded incidents of faecal or vomiting contamination at the pool since the beginning of September 2010. The poolside daily monitoring sheets showed that on Thursday, 9 September 2010, there appears to have been an airlock overnight in the chlorine pump causing a fall in the free chlorine level. This was cleared and free chlorine levels had risen to acceptable levels by pool opening the following morning. Combined chlorine levels were acceptable on this date. All other records reviewed indicated that the pool was operating within agreed operating parameters.
A decision was taken on 29 September 2010 not to sample the pool water for Cryptosporidium following consultation with the Head of Cryptosporidium Reference Unit, Public Health Wales, as the pool was well managed, the suspected contamination event had been over 2 weeks ago, there were no cases outside the swimming club members, case numbers had declined and the turnover rate meant that the pool would have been capable of removing oocysts within six turnovers – a period of 15 h.
Control measures were established: cases were excluded from school until symptom free for 48 h and from swimming until free of symptoms for 2 weeks in line with national guidance [8]. A letter to all local general practitioners informing them of the outbreak included a reminder about the need to exclude patients from school, work or swimming. The swimming club put this information on their website and put up posters at all of their pools. It was recommended that the weekly filter backwashing should be undertaken at the end of the day following closure of the pool rather than at noon. A holding press statement was prepared, but there was no media interest. Proactive messages to raise public awareness of the ‘two-week no-swim rule’ were made in a local newspaper and the City Council magazine. This opportunity was also used to develop a suite of materials, including posters and web-based information for pool operators and swimming teachers.
These were disseminated prior to the autumn peak for cryptosporidiosis.
Although the cause of illness in cases was suspected at an early stage to be Cryptosporidium, it took almost 5 days from the date of reporting of the outbreak to confirm the diagnosis. Despite a high attack rate and EHOs requesting faecal samples from symptomatic cases only three samples were submitted. Therefore, this outbreak would not have been detected by laboratory-based surveillance alone. This emphasizes the benefits of field epidemiology in the early stages of an outbreak to optimize case ascertainment. The cohort study confirmed an unexpectedly high attack rate of 48% in swimming club members. The watery nature of diarrhoea, the high bather load and high frequency of organized activity in training sessions all increase the likelihood that a faecal release can go undetected by coaches. Pool operators hand over the pool to the club for these sessions and do not monitor the pool.
There is a lack of knowledge in swimmers and coaches about the risks of spread of cryptosporidiosis within pools and the importance of exclusion in preventing outbreaks. In this outbreak, parents and coaches were often reluctant to comply with the recommended exclusion as this could adversely affect performance. Previous outbreak reports have highlighted the potential for amplification and perpetuation of outbreaks due to contamination of surrounding pools following an outbreak. In Japan, following a swimming training event in a hotel pool, cases contaminated two pools in their local sports centre; a follow-up study of those who used two pools identified 48 additional cases who had not attended the original training event [9].
In this outbreak, the questionnaire enquired about training and galas attended between 6 and 18 September 2010. During this period, there were eight training sessions and two galas at the implicated pool and three galas at three different pools, providing multiple opportunities for spread of infection to others. In USA, it is recommended that pools are not closed following identification of outbreaks because investigators have found that patrons will swim elsewhere and contaminate other pools [10].
Undertaking the cohort study was important in assessing the size of the outbreak and identifying the cause. A very high response rate was achieved by interviewing at pool training sessions and by telephone. Interviewing parents also provided opportunities to give advice about Cryptosporidium, in particular, messages about reducing spread to family members, school-mates and fellow swimming club members.
Typing of isolates was helpful in excluding a case from another area who had been swimming at a gala during the period of interest. In the UK, C. hominis peaks in the late summer and is more often associated with foreign travel, swimming in a toddler pool and in children aged < 1 year and adults; in contrast, C. parvum is associated with farm animal contact [1]. Typing is important in outbreak investigation to enable linking of epidemiological information with type and provide more information on sources of infection and vehicles of transmission.
In summary, a rapid retrospective cohort study of this outbreak provided the opportunity to:
-
(1)
Assess the burden of illness in members of the swimming club (which would not have been possible by descriptive epidemiology or laboratory ascertainment).
-
(2)
Exclude symptomatic children from swimming, thereby possibly limiting secondary and tertiary spread.
-
(3)
Develop and disseminate materials to swimming pool operators to mitigate the autumn peak of cryptosporidiosis.
ACKNOWLEDGEMENTS
The authors thank HPA Food, Water & Environmental Microbiology Network (Preston Laboratory), the Greater Manchester swimming club involved in the outbreak, and the Microbiology Department at Salford Royal Foundation Trust.
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Hunter PR, et al. Sporadic cryptosporidiosis case-control study with genotyping. Emerging Infectious Diseases 2004; 20: 1241–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hunter PR, Nichols G. Epidemiology and clinical features of Cryptosporidium infection in immunocompromised patients. Clinical Microbiology Review 2002; 15: 145–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chappell CL, et al. Cryptosporidium homonis: experimental challenge of healthy adults. American Journal of Tropical Medicine & Hygiene 2006; 75: 851–857. [PubMed] [Google Scholar]
- 4.Smith A, et al. Outbreaks of waterborne infectious intestinal disease in England and Wales 1992–2003. Epidemiology and Infection 2006; 134: 1141–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karanis P, Kourenti C, Smith H. Waterborne transmission of protozoan parasites: a worldwide review of outbreaks and lessons learnt 2007. Journal of Water and Health 2007; 5: 1–38. [DOI] [PubMed] [Google Scholar]
- 6.Anon. Preventing person-to-person spread following gastrointestinal infections: guidelines for public health physicians and environmental health officers. Communicable Disease and Public Health 2004; 7: 362–384. [PubMed] [Google Scholar]
- 7.Hadfield SJ, et al. Detection and differentiation of Cryptosporidium spp. in human clinical samples by use of real-time PCR. Journal of Clinical Microbiology 2011; 49: 918–924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.PWTAG. Swimming Pool Water: Treatment and Quality Standards for Pools and Spas. Pool Water Treatment Advisory Group. [Google Scholar]
- 9.Ichinohe S, et al. Secondary transmission of cryptosporidiosis associated with swimming pool use. Japan Journal of Infectious Disease 2005; 58: 400–401. [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Cryptosporidiosis outbreaks associated with recreational water use – five states, 2006. Morbidity and Mortality Weekly Report 2007; 56: 729–732. [PubMed] [Google Scholar]