Abstract
Voluminous vaccine campaigns have been used globally, since the COVID-19 pandemic has brought devastating mortality and destructively unprecedented consequences to different aspects of economies. This study aimed to identify how the numbers of new deaths and new cases per million changed after half of the population had been vaccinated. This paper used actual pandemic consequence variables (death and infected rates) together with vaccination uptake rates from 127 countries to shed new light on the efficacy of COVID-19 vaccines. The 50% uptake rate was chosen as the threshold to estimate the real benefits of vaccination campaigns for reducing COVID-19 infection and death cases using the difference-in-differences (DiD) imputation estimator. In addition, a number of control variables, such as government interventions and people’s mobility patterns during the pandemic, were also included in the study. The number of new deaths per million significantly decreased after half of the population was vaccinated, but the number of new cases did not change significantly. We found that the effects were more pronounced in Europe and North America than in other continents. Our results remain robust after using other proxies and testing the sensitivity of the vaccinated proportion. We show the causal evidence of significantly lower death rates in countries where half of the population is vaccinated globally. This paper expresses the importance of vaccine campaigns in saving human lives during the COVID-19 pandemic, and its results can be used to communicate the benefits of vaccines and to fight vaccine hesitancy.
Keywords: COVID-19, vaccination uptake rate, causal effect, difference-in-differences, death rates, new cases
JEL Classification Codes: I10; I18.
Introduction
The COVID-19 pandemic is not the worst in human history, but it has been one of the deadliest pandemics since the Spanish flu in the early 20th century (Feehan & Apostolopoulos, 2021). In the nearly 2 years since the initial outbreak in January 2020, the pandemic has killed more than 4.5 million people globally (WHO, 2021a). Herd immunity is one of the key strategies in controlling epidemics (Fontanet & Cauchemez, 2020), and mass vaccination programs have been widely accepted as optimal strategies for achieving herd immunity (Anderson & May, 1985; Jeyanathan et al., 2020; Matrajt et al., 2021). However, vaccine hesitancy has become a huge challenge to reaching global COVID-19 immunity (Machingaidze & Wiysonge, 2021). Social factors such as social norms and herding behaviors were found to dominate individual free-riding will in vaccine uptake decisions (Agranov et al., 2021). Thus, intensive media coverage about COVID-19 vaccine side effects instead of the vaccine’s real effects in controlling the pandemic could explain low vaccine uptake rates (Machingaidze & Wiysonge, 2021). The concept of herd immunity without a vaccine path has even been voiced by both governments and scientists (Aschwanden, 2021; de Vlas & Coffeng, 2021). In contrast, very little research has been conducted to provide empirical evidence on the immunity impacts of vaccination programs until now (Fontanet & Cauchemez, 2020; Rossman et al., 2021), partly either because of limited data or lack of interest. This study aims to fill this gap by providing real-world evidence on the effects of vaccination programs on controlling the COVID-19 pandemic before and after achieving a relatively high vaccinated population rate. More specifically, the main objective of this paper is to explore the global impacts of vaccination programs on reducing new infected cases and deaths caused by the COVID-19 pandemic, using evidence from more than 127 countries worldwide. We hypothesized that there would be significant differences in pandemic consequences (deaths and infection rates) between countries with high vaccination uptake rates (at or above 50%) and those with lower vaccination rates (below 50%). To ensure the causal relationships between vaccination and pandemic variables are appropriately estimated, this study utilizes the novel Difference-in-Differences (DiD) imputation procedures.
Governments worldwide have been compelled to implement public health policies in order to react to the COVID-19 pandemic and preserve people’s lives. In the absence of a viable and safe treatment or vaccine, non-pharmaceutical interventions (NPIs) such as public health policies are the most crucial measures used by many countries to prevent and control the transmission and spread of COVID-19 (Alhassan et al., 2021b; Iezadi et al., 2020). However, strict government policies such as social distancing or lockdowns could significantly harm economic outcomes (Alhassan et al., 2021b). Therefore, in the long-term, herd immunization through COVID-19 vaccination campaigns is the most sustainable solution for controlling the pandemic while also achieving positive effects on economies and peoples' lives (Ngo et al., 2022; Wang et al., 2021).
The percentage of vaccinated people necessary to achieve herd immunity has varied for different epidemics (i.e., 95% for measles, 80% for polio) (WHO, 2021b). Using simulated data and mathematical models, many studies have found that a vaccine with an acceptable level of effectiveness (i.e., ≥ 50%) or efficacy (i.e., ≥ 70%) would be sufficient to significantly contain the COVID-19 pandemic (i.e., reduce severe symptoms and mortality rates) if a major proportion of the population was vaccinated (MacIntyre et al., 2021; Swan et al., 2021; Deplanque & Launay, 2021). Vaccination rates ranging from 60% to 90% of the population have been suggested as herd immunity levels for the COVID-19 pandemic (Aschwanden, 2021; Matrajt et al., 2021). If we add the proportion of the population that is immune because they have already been infected to the 50% of the population that has been vaccinated, we might approach the proposed COVID-19 herd immunity in some countries. Therefore, using a DiD imputation estimator following Borusyak, Jaravel, and Spiess, (2021), this study attempts to explore the causal relationship between pandemic infection rates, mortality rates, and the event of having 50% of the population vaccinated against COVID-19.
However, vaccination hesitancy in the population may result in large disparities in vaccination pace among countries globally. Furthermore, anti-vaccine conspiracy beliefs, which have been prominent since the beginning of the COVID-19 epidemic, are substantially linked to lower vaccination intentions (Jolley & Douglas, 2014). Moore, (2018) claims that conspiracy theorists are more common among the poor and uneducated. Trust in science and the effectiveness of vaccines is also the key to promoting people’s acceptance of taking the COVID-19 vaccine (Sturgis, Brunton-Smith, and Jackson, 2021). Therefore, the evidence provided in this study about the real-world herd immunity impacts of mass vaccination programs could help to mitigate the vaccine hesitancy and achieve higher vaccine uptake rates faster, which could alleviate the pressure on healthcare systems globally.
The following section summarizes our data and methodologies. The Results and Findings section shows the results of DiD estimations, and the Conclusion and Implication section summarizes and concludes the study.
Data and Methodologies
Data
We examined the changes in new deaths and new cases per million when half of the population has been vaccinated, using vaccination data from 127 countries1. Although herd immunity for the COVID-19 pandemic has been defined as having 60–90% the population vaccinated (Aschwanden, 2021), the threshold of 50% was chosen for this study given the availability of data (more than 30 observations satisfied the uptake rate needed for DiD regression) at the early stage of the global vaccination program from February 2021 to August 2021 (see Table A43 in Online Appendix 4). Figure 1 presents the distribution of vaccination uptake rates for different regions globally. Until August 2021, only 43 countries had vaccination uptake rates of over 50% of their total populations. To control for other factors that could strongly influence COVID-19 death and infection rates, two sets of control variables—government measures to control the pandemic spread (Containment and Economics) and mobility index data (Recreation, Park, Workplaces, and Residential—were also added. Government measures and public health policies such as social distancing and lockdowns have been proven to be effective in containing the pandemic and possibly reducing infection death rates significantly. They have been adopted by many governments (Davies et al., 2020; Iezadi et al., 2020). In addition to government mandates, people also need to adapt to new behaviors and lifestyles to protect themselves and their families from viruses. Mobility indexes, which can be used to track these behavioral changes, were collected from the COVID-19 Google community. In addition, a dummy variable was added to the DiD regression to control for the event of the Delta variant appearance, which significantly increased the infection probabilities. Table 1 summarizes key statistics for these variables (see Table A1.1 in online Appendix 1 for descriptions and sources of data).
Figure 1.
COVID-19 vaccination uptake rate distribution by continent up to 26 August 2021. African countries show the lowest COVID-19 vaccine uptake rate, with the average number of vaccinated people per one hundred capita at only 5.4. European and North American countries have the highest and second highest COVID-19 vaccine uptake rates, with average numbers of vaccinated people per one hundred at 25.63 and 24.06, respectively. The statistics for South American, Asian, and Oceanian countries are 22.24, 20.83, and 14.59, respectively. *China is not included in the sample due to data unavailability.
Table 1.
Summary Statistics of Key Variables.
| Variable | Obs | Mean | Std. Dev. | Min | Max |
|---|---|---|---|---|---|
| New deaths per million | 64,083 | 1.727 | 3.938 | 0 | 215.334 |
| New cases per million | 68,015 | 88.471 | 174.791 | 0 | 3558.259 |
| Recreation | 67,761 | −18.734 | 26.184 | −100 | 142 |
| Park | 67,432 | 5.001 | 55.218 | −100 | 670 |
| Workplaces | 68,340 | −20.551 | 19.213 | −99 | 88 |
| Residential | 67,918 | 7.791 | 9.029 | −35 | 55 |
| Containment | 67,339 | 57.307 | 15.739 | 0 | 92.02 |
| Economic | 67,362 | 48.904 | 30.627 | 0 | 100 |
| Delta dummy | 67,997 | 0.115 | 0.319 | 0 | 1 |
Methodologies
In this study, we applied a DiD imputation estimator when 50% population was vaccinated at different times across countries, following Borusyak et al. (2021). The heterogeneous treatment effects that occur when units in the panel receive treatment effects at differential timings is a limitation when examining event studies using conventional two-way fixed effect regression (Goodman-Bacon, 2021). Imbens and Angrist (1994) initially stated that the estimator of the Average Treatment Effects (ATE) could be written as a weighted average. Indeed, the famous monotonicity condition (nonincreasing or nondecreasing) that they employ ensures that they do not get negative weights. The staggered DiD can be interpreted as a weighted average of two-period DIDs, named Variance Weighted Average Treatment Effect on the Treated (VWATT) (de Chaisemartin & D'Haultfœuille, 2020; Goodman-Bacon, 2021; Sun & Abraham, 2020). In summary, Goodman-Bacon (2021) comprehensively explains why the negative weights occur: already-treated units acting as controls experience changes in their treatment effects over time. This negative weighting arises when treatment effects vary over time, in which case it typically biases regression DiD estimates away from the sign of the true treatment effect.
The imputation estimator developed by Borusyak et al. (2021) is a finite-sample, efficient, and unbiased estimator among some emerging DiD estimators robust to unrestricted heterogeneous treatment effects (Callaway & Sant'Anna, 2020; de Chaisemartin & D'Haultfœuille, 2020). Apart from that, Cunningham (2021) suggests that the approach given by Borusyak et al. (2021) is a simple and proper solution for the negative weight problems of the standard two-way fixed effects DiD estimator.
The imputation estimation process follows three steps. First, we estimate a model for untreated (i.e., never-treated and not-yet-treated) potential outcomes using untreated observations only in a two-way fixed effects regression:
| (1) |
While comprises outcome variables including new deaths per million and new cases per million, and are country and year fixed effects accordingly. The standard error is clustered at the unit (country) level, following Abadie et al. (2017). stands for covariates including lag outcome variables, mobility variables (changes in retail and recreation, parks, workplaces, residential mobility), government policies (economic support and containment), and a dummy variable standing for delta variants. The summary statistic, variable description, and sources are in Online Appendix 1. Next, we extrapolate the equation (1) to treated observations, imputing untreated potential outcomes , and calculate treatment effects .2
| (2) |
Finally, we take the averages of these individual imputation-based treatment effects, called , which shows how the new deaths or new cases change after a specific event date. We also test the parallel trend assumption for DiD using the approach proposed by Borusyak et al. (2021) and Sun and Abraham (2020). In other words, we test if there is an insignificant difference between the treatment and control groups before the event dates before conducting any DiD regressions.
In particular, we run the regression below on the untreated sample to falsify the parallel trend violation:
| (3) |
where represents the sets of indicators for observations during some periods before treatment (, with the periods before t serving as the reference group. For example, observations at periods before the treatment date will receive the value of ; otherwise, observations will receive the value of .
We estimate by using OLS on untreated observations only, followed by a joint null test in which using the Chi-squared test.
The Prob > chi2 of the joint null test is higher than 0.1, supporting the parallel trend assumption. In other words, it means that there is an insignificant difference between the treatment and control groups before the event date. Although there is no universal optimal choice of (Borusyak et al., 2021), we follow Dasgupta and Žaldokas, (2019) and choose . We also go further and test the parallel trend assumption at to solidify our results.
Results and Findings
Half of the Population Vaccinated and its Causal Effects on COVID-19 Infection and Mortality Rates
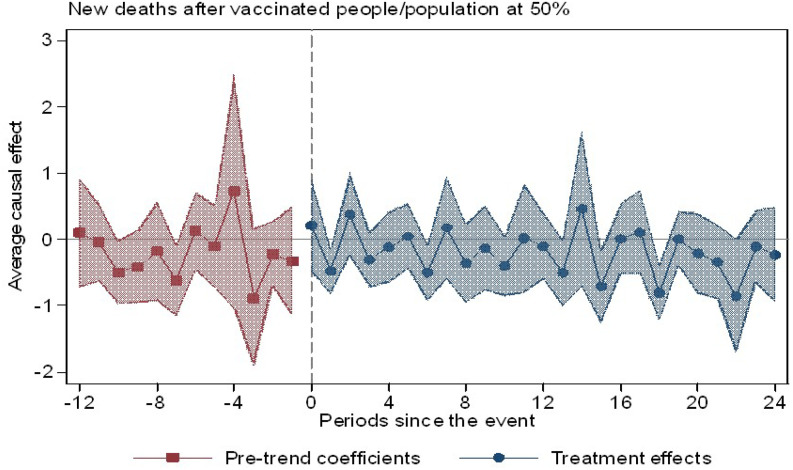
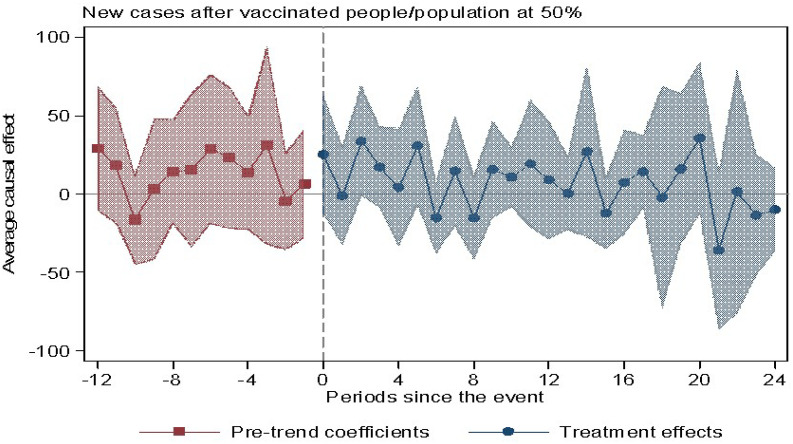
In Table 2, we test the changes in COVID-19 new deaths per million and new cases per million based on different specifications. The variable of interest here is . In specification (1), we control the lag outcome variables, country and year fixed effects, and cluster by country. In column (2), we further control government policies. In column (3), we control for mobility variables and delta variants. Given the satisfied parallel trend assumption (Table A2.1 in online Appendix 2), we examine how new deaths and new cases change when half of the population has been vaccinated. In Table 2, we can see that the number of new deaths per million decreases by 0.445 people after 50% of the population is vaccinated, while there is an insignificant change in new cases on average. The changes of the two outcome variables are visualized in Figures 2 and 3, supporting our statistical results.
Table 2.
The Treatment Effects on New Deaths and New Cases per Million When Half of the Population has Been Vaccinated.
| Panel A: New deaths per million | Panel B: New case per million | |||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (1) | (2) | (3) | |
| −0.618*** | −0.559*** | −0.445** | −7.037 | −2.234 | 2.168 | |
| (0.003) | (0.004) | (0.025) | (0.406) | (0.802) | (0.819) | |
| Lag | 0.545*** | 0.539*** | 0.514*** | 0.671*** | 0.647*** | 0.629*** |
| (0.000) | (0.000) | (0.000) | (0.000) | (0.000) | (0.000) | |
| Containment | 0.0372*** | 0.0177*** | 1.223*** | 0.686*** | ||
| (0.000) | (0.000) | (0.000) | (0.000) | |||
| Economic | −0.0022*** | −0.0014** | −0.0836*** | −0.0749*** | ||
| (0.001) | (0.039) | (0.001) | (0.003) | |||
| Recreation | −0.0097*** | 0.0324 | ||||
| (0.000) | (0.497) | |||||
| Park | −0.0064*** | −0.247*** | ||||
| (0.000) | (0.000) | |||||
| Workplaces | −0.0004 | 0.0447 | ||||
| (0.759) | (0.346) | |||||
| Residential | 0.0208*** | 1.246*** | ||||
| (0.000) | (0.000) | |||||
| Delta dummy | −0.0502 | 0.549 | ||||
| (0.475) | (0.842) | |||||
| N | 61,536 | 60,452 | 59,359 | 65,489 | 64,373 | 63,207 |
| Adj. R-sq | 0.483 | 0.517 | 0.526 | 0.612 | 0.613 | 0.616 |
Note: New deaths per million and new cases per million are the daily recorded COVID-19 new deaths and new cases per million, while Lag represents their one-period lag variables. Mobility indices include Recreation, Park, Workplaces, and Residential, collected from Google data. The government policies include Containment and Economic supports. The Delta dummy receives the value of 0 before the first delta variant case recorded in each country and 1 otherwise. P-values are in parentheses. *, **, and *** denote significance at the 10%, 5%, and 1% levels, respectively.
Figure 2.
New deaths before and after vaccinated people/population reaches 50%. Note: The dots show the average treatment effects for each day around the event date. Blue dots primarily lie under the x-axis, implying a decrease in new deaths after vaccinated people/population reaches 50%.
Figure 3.
New cases before and after vaccinated people/ population reaches 50%. Note: The dots show the average treatment effects for each day around the event date. The blue dots fluctuate around the x-axis, implying the indecisive movement of new cases after vaccinated people/population reaches 50%.
Does Vaccine Origin Matter?
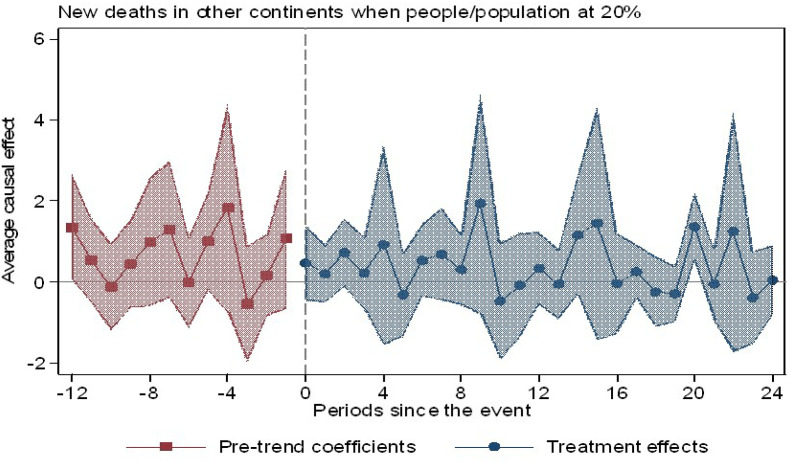
We further classify the data into two subsamples based on vaccine origin. One subsample includes European and North American countries, where most globally accepted vaccines come from, while the other includes countries from four other continents: Africa, Asia, Oceania, and South America.
Due to data limitation, we are only able to test these subsamples until the vaccinated population reaches 30% for African, Asian, Oceanian, and South American countries (see Tables A4.4 and A4.5 in online Appendix 4). However, because the parallel trend assumption is violated at this level (30%), we conduct the imputation estimator for both outcomes in these two subsamples when the vaccinated population reaches 20% (see Table A2.2 in online Appendix 2). The statistical results show that when vaccinated people comprise one-fifth of the population, new deaths decrease in Europe and North America. In contrast, there is an insignificant change in both new deaths and new cases in the other four continents. It is a caveat in our study that the follow-up research will have a broader vision with more data available for higher percentages of vaccinated people in these subsamples.
We also visualize the changes in new deaths of these two subsamples when the vaccinated population reaches 20% in Figures 4 and 5. These two figures also support our conclusion.
Figure 4.
New deaths in Europe and North America before and after vaccinated population is at 20%. Note: The dots show the average treatment effects for each day around the event date in North America and Europe. The blue dots mainly lie under the x-axis, implying a decrease in new deaths in these two continents after the vaccinated population reaches 20%.
Figure 5.
New deaths in Asia, Oceania, South America, and Africa before and after vaccinated population reaches 20%. Note: The dots show the average treatment effects for each day around the event date for four continents: Asia, Oceania, South America, and Africa. The blue dots mostly fluctuate around the x-axis, implying the indecisive movement of new cases after the vaccinated population reaches 20%.
Robustness Tests
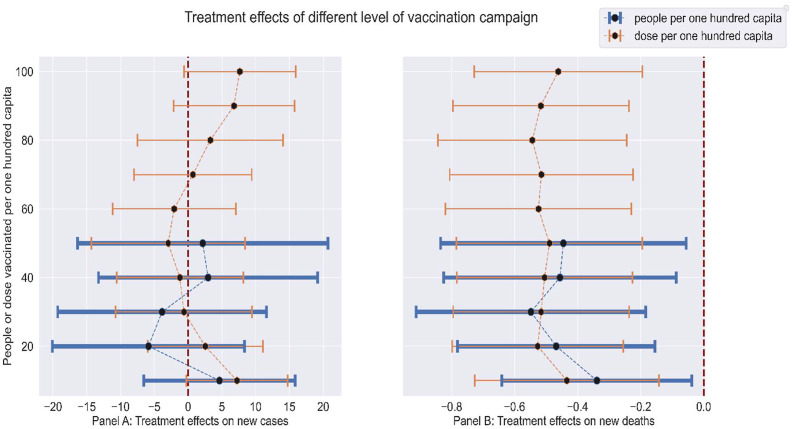
We also use total vaccination doses per hundred capita (doses/population) as a measure of vaccination uptake rate for each country. For the parallel trend test (see Table A4.2 in online Appendix 4), the level of 70% doses/population is used to robustly test the main result. Our results when using this alternative benchmark are still robust to the main results (see Table 3A.1 in online Appendix 3). In an additional analysis, we report the statistical and visualized sensitivity tests on the causal effects of different levels of vaccinated people/population and doses/population (see Figure 6 and online Appendixes 4 and 5).
Figure 6.
Mean and 95% confidence interval of treatment effects at different vaccination uptake rates. Panel A shows that the treatment effects on new cases per million is not significant at all levels of vaccination campaigns for both people vaccinated/population and doses vaccinated/population rates. In contrast, Panel B shows that at all levels of vaccination uptake rates, the difference-in-differences treatment effects on new deaths per million is significant and negative, with mean treatment effects of approximately −0.451 and −0.503 for people vaccinated/population and doses vaccinated/population, respectively.
Conclusion and Implication
Our paper provides causal evidence of significantly lower death rates (but an insignificant change in new cases) after achieving a high vaccination rate globally. While it is based on early vaccination data, this finding strongly contributes to the research stream exploring the real-world effects of vaccination campaigns (Haas et al., 2021; Jara et al., 2021). Our main goal was to estimate the lives saved by expanding and expediting the vaccination campaign. The statistical results show significantly lower death rates in countries where half of the population has been vaccinated globally; however, the number of new cases shows an insignificant change. This finding in our study confirms results in current literature on the effects of mass vaccination in reducing severe symptoms and deaths from infected cases. However, we found no causal evidence that high vaccinations uptake rates among populations reduce overall COVID-19 cases, which supports previous research (Jara et al., 2021). In addition, instead of focusing on using data from one specific country like previous research, our study is one of the first attempts to study the effects of vaccination campaigns in a cross-country context. Together with the DiD method to provide causal inferences, the global aspects of this study could give an early overall picture of the actual benefits of COVID-19 vaccination campaigns.
Our results have important implications for policymakers. Given the faster spread and evolution of different variants, vaccines are effective pharmaceutical interventions to save human lives during the COVID-19 pandemic by establishing herd immunity. Therefore, it is possible to generalize the causal evidence to using vaccines to release the burden on the healthcare system when the number of deaths increases. This study expresses the importance of vaccine campaigns in saving human lives during the COVID-19 pandemic, and its results can be used to communicate the benefits of vaccines and to fight vaccine hesitancy. However, the pronounced effect of vaccinations in Europe and North America compared to other regions presented in this study also raises the issue of vaccine inequality, emphasizing the necessity of equally distributing vaccines from advanced countries to developing ones to contain the spread of more dangerous variants. International organizations such as the WHO and pharmaceutical companies could play a key role in fighting vaccine nationalism and supporting the COVID-19 Vaccines Global Access (COVAX) program. Wealthier nations must join the United States, Russia, and China in realizing that distributing vaccine production fairly across the globe helps everyone. Therefore, waiving the intellectual property protection on coronavirus vaccines could be the path ahead (Burki, 2021).
This study suffers from some drawbacks. First, because COVID-19 vaccination data is limited since most countries have only recently started their vaccination campaigns, countries that have fully vaccinated 50% of their total populations do not comprise large portions of the dataset. Thus, more research should be conducted at the later pandemic stages, when vaccination campaigns are more mature and more data is available to test the robustness of this study’s findings. Second, this study uses infection and death rates to gauge the results of vaccination efforts. Although we control multiple factors using sets of variables, death and infection rates are dependent on many different factors, so bias could still exist. More methodologies, especially a better set of outcome variables based on epidemiological models, could be used to better investigate the causal effects of COVID-19 vaccination campaigns. Finally, the relationship between vaccination and pandemic outcomes is an important and complex topic. It needs more attention from scholars in different fields of knowledge to enrich our understanding of how governments could improve their public health and vaccination policies to deal with pandemics in the future.
Supplemental Material
Supplemental Material, sj-pdf-1-erx-10.1177_0193841X221085352 for The race Against Time to Save Human Lives During the COVID-19 With Vaccines: Global Evidence by Phuc Van Nguyen, Toan L. D. Huynh, Vu Minh Ngo, and Huan Huu Nguyen in Evaluation Review
Notes
China was not included in our sample due to data unavailability.
The period-t potential outcome of unit i if it is never treated
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research is funded by University of Economics Ho Chi Minh City, Vietnam (UEH) (Grant No. 2022-01-06-0756).
Supplemental Material: Supplemental material for this article is available online.
ORCID iDs
Phuc Van Nguyen https://orcid.org/0000-0002-7144-7550
Vu Minh Ngo https://orcid.org/0000-0002-0997-4720
References
- Abadie A., Athey S., Imbens G. W., Wooldridge J. M. (2017). When should you adjust standard errors for clustering? 10.3386/W24003 [DOI]
- Agranov M., Elliott M., Ortoleva P. (2021). The importance of Social Norms against Strategic Effects: The case of Covid-19 vaccine uptake. Economics Letters, 206, 109979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alhassan G. N., Öztürk İ., Adedoyin F. F., Bekun F. V. (2021. b). Telehealth as a panacea amidst global pandemic (COVID-19) in Africa. Duzce Medical Journal, 23(Special Issue), 43–47. 10.18678/dtfd.898373 [DOI] [Google Scholar]
- Anderson R. M., May R. M. (1985). Vaccination and herd immunity to infectious diseases. Nature, 318(6044), 323–329. [DOI] [PubMed] [Google Scholar]
- Aschwanden C. (2021). Five reasons why COVID herd immunity is probably impossible. Nature, 591, 520–522. [DOI] [PubMed] [Google Scholar]
- Borusyak K., Jaravel X., Spiess J. (2021). Revisiting event study designs: Robust and efficient estimation. arXiv preprint arXiv:2108.12419. [Google Scholar]
- Burki T. K. (2021). Ensuring fair distribution of COVID-19 vaccines: Is an intellectual waiver the answer? The Lancet Respiratory Medicine, 9(7), e64. 10.1016/s2213-2600(21)00241-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaway B., PedroSant’Anna H. C. (2020). Difference-in-differences with multiple time periods. Journal of Econometrics, 225(2), 200–230. 10.1016/J.JECONOM.2020.12.001 [DOI] [Google Scholar]
- Cunningham S. (2021). Causal inference: The mixtape. Yale University Press. [Google Scholar]
- de Chaisemartin C., D’Haultfœuille X. (2020). Two-way fixed effects estimators with heterogeneous treatment effects. American Economic Review, 110(9), 2964–2996. 10.1257/AER.20181169 [DOI] [Google Scholar]
- Dasgupta S., Žaldokas A. (2019). Anticollusion enforcement: Justice for consumers and equity for firms. Review of Financial Studies, 32(7), 2587–2624. 10.1093/rfs/hhy094 [DOI] [Google Scholar]
- Davies N. G., Kucharski A. J., Eggo R. M., Gimma A., Edmunds W. J., Jombart T., Liu Y. (2020). Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: A modelling study. The Lancet Public Health, 5(7), e375–e385. 10.1016/S2468-2667(20)30133-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vlas S. J., Coffeng L. E. (2021). Achieving herd immunity against COVID-19 at the country level by the exit strategy of a phased lift of control. Scientific Reports, 11(1), 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deplanque D., Launay O. (2021). Efficacy of COVID-19 vaccines: From clinical trials to real life. Therapie, 76, 277–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feehan J., Apostolopoulos V. (2021). Is COVID-19 the worst pandemic? Maturitas, 149, 56–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontanet A., Cauchemez S. (2020). COVID-19 herd immunity: where are we? Nature Review Immunology, 20, 583–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman-Bacon A. (2021). Difference-in-differences with variation in treatment timing. Journal of Econometrics, 225(2), 254–277. 10.1016/J.JECONOM.2021.03.014 [DOI] [Google Scholar]
- Haas E. J., Angulo F. J., McLaughlin J. M., Anis E., Singer S. R., Khan F., Brooks N., Smaja M., Mircus G., Pan K., Southern J., Swerdlow D. L., Jodar L., Levy Y., Alroy-Preis S. (2021). Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. The Lancet, 397(10287), 1819–1829. 10.1016/s0140-6736(21)00947-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imbens G. W., Angrist J. D. (1994). Identification and estimation of local average treatment effects. Econometrica, 62(2), 467. 10.2307/2951620 [DOI] [Google Scholar]
- Iezadi S., Azami-Aghdash S., Ghiasi A., Rezapour A., Pourasghari H., Pashazadeh F., Gholipour K. (2020). Effectiveness of the non-pharmaceutical public health interventions against COVID-19; a protocol of a systematic review and realist review. PLoS One, 15(11), e0239554. 10.1371/journal.pone.0239554 PMID: 32991604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jara A., Undurraga E. A., González C., Paredes F., Fontecilla T., Jara G., Pizarro A., Acevedo J., Leo K., Leon F., Sans C., Leighton P., Suarez P., Garcia-Escorza H., Araos R. (2021). Effectiveness of an inactivated SARS-CoV-2 vaccine in Chile. New England Journal of Medicine, 385(10), 875–884. 10.1056/nejmoa2107715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeyanathan M., Afkhami S., Smaill F., Miller M. S., Lichty B. D., Xing Z. (2020). Immunological considerations for COVID-19 vaccine strategies. Nature Review Immunology, 20, 615–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jolley D., Douglas K.M. (2014). The effects of anti-vaccine conspiracy theories on vaccination intentions. PLOS ONE, 9(2), e89177. 10.1371/journal.pone.0089177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machingaidze S., Wiysonge C. S. (2021). Understanding COVID-19 vaccine hesitancy. Nature Medicine, 27, 1338–1339. [DOI] [PubMed] [Google Scholar]
- MacIntyre C. R., Costantino V., Trent M. (2021). Modelling of COVID-19 vaccination strategies and herd immunity, in scenarios of limited and full vaccine supply in NSW, Australia. Vaccine. 10.1016/J.VACCINE.2021.04.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matrajt L., Eaton J., Leung T., Brown E. R. (2021). Vaccine optimization for COVID-19: Who to vaccinate first? Science Advances, 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore A. (2018). Conspiracies, conspiracy theories and democracy. Political Studies Review, 16(1), 2–12. 10.1111/1478-9302.12102 [DOI] [Google Scholar]
- Ngo V. M., Nguyen H. H., Phan H. T., Tran P. T. T. (2022). Lives and livelihoods trade-offs: Which COVID-19 strategies for which countries? Cogent Economics & Finance, 10(1), 2022859. 10.1080/23322039.2021.2022859 [DOI] [Google Scholar]
- Rossman H., Shilo S., Meir T., Gorfine M., Shalit U., Segal E. (2021). COVID-19 dynamics after a national immunization program in Israel. Nature Medicine, 27, 1055–1061. [DOI] [PubMed] [Google Scholar]
- Sun L., Abraham S. (2020). Estimating dynamic treatment effects in event studies with heterogeneous treatment effects. Journal of Econometrics, 225(2), 175–199. 10.1016/J.JECONOM.2020.09.006 [DOI] [Google Scholar]
- Sturgis P., Brunton-Smith I., Jackson J. (2021). Trust in science, social consensus and vaccine confidence. Nature Human Behaviour, 5(11), 1528–1534. 10.1038/s41562-021-01115-7 [DOI] [PubMed] [Google Scholar]
- Swan D. A., Bracis C., Janes H., Moore M., Matrajt L., Reeves D. B., Burns E., Donnell D., Cohen M. S., Schiffer J. T., Dimitrov D. (2021). COVID-19 vaccines that reduce symptoms but do not block infection need higher coverage and faster rollout to achieve population impact. Scientific Reports, 11(1), 1–9. 10.1038/s41598-021-94719-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X., Du Z., Johnson K. E., Pasco R. F., Fox S. J., Lachmann M., McLellan J. S., Meyers L. A. (2021). Effects of COVID-19 vaccination timing and risk prioritization on mortality rates, United States. Emerging Infectious Diseases, 27(7), 1976. 10.3201/eid2707.210118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . (2021. a). WHO Coronavirus (COVID-19) Dashboard. https://covid19.who.int/ (Accessed 03 October 2021). [Google Scholar]
- WHO . (2021. b). Coronavirus disease (COVID-19): Herd immunity, lockdowns and COVID-19. https://www.who.int/news-room/q-a-detail/herd-immunity-lockdowns-and-covid-19 (Accessed 03 October 2021). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-erx-10.1177_0193841X221085352 for The race Against Time to Save Human Lives During the COVID-19 With Vaccines: Global Evidence by Phuc Van Nguyen, Toan L. D. Huynh, Vu Minh Ngo, and Huan Huu Nguyen in Evaluation Review