Abstract
Breast and cervical are top cancers for women globally, but few studies have summarised how gender norms influence screening uptake, given sexual connotations and physical exposure. These beliefs may play a central role in decision-making, and understanding them is crucial to improving screening rates and services. This review scopes international literature for gender-based qualitative factors influencing women’s screening uptake. A systematic search of peer-reviewed English articles in PubMed, Scopus, and CINAHL was conducted from inception until December 2019. Articles were included if they were about breast or cervical cancer screening, had mixed or qualitative methodology, and sampled women from the general population. 72 studies spanning 34 countries were analysed. Eight studies also included healthcare providers’ views. Our narrative thematic analysis summarised primary themes extracted from each study into first-level subthemes, then synthesising second-level and third-level themes: (I) gender socialisation of women, (II) gender inequality in society, and (III) lack of empowerment to women in making screening decisions. Women tended to face sociocultural/role-based constraints, were expected to prioritise family, and keep bodily exposure to their husbands. Women showed low awareness and had fewer opportunities for health education compared to men. Male relations were often gatekeepers to financial resources needed to pay for screening tests. Screening risked community norms about women’s or husbands’ perceived embarrassing sexual behaviours. These findings suggest that interventions targeting unhelpful stigmatising beliefs about women’s cancer screening must concurrently address community general norms, familial role-based beliefs, as well as at male relations who hold the purse-strings.
1. Introduction
Breast and cervical cancer are respectively the top and fourth most common cancer in women, with a combined incidence of over two million cases globally per year (Ginsburg et al., 2017, Global Cancer Observatory, n.d.). Unlike the other “female” cancers (i.e., uterine and ovarian), there is extant literature supporting the efficacy and cost-effectiveness of breast and cervical cancer screening (Rim et al., 2019, Bleyer and Welch, 2012, Siu, 2016, Lees et al., 2016, Pimple et al., 2016). Nonetheless, breast and cervical cancer screening rates in the general population have yet to achieve optimal coverage rates in many countries despite support from both regional and international authorities. A recent study on screening attendance in 17 European Union nations, for example, showed that nearly half of these countries failed to achieve the 70% coverage threshold for breast and cervical cancer screening as recommended by the European Council (Gianino et al., 2018).
There is considerable evidence to suggest that the decision-making process in women to undergo breast and cervical cancer screening is complex and multifactorial. On an individual level, studies have found barriers that include structural or socioeconomic (e.g. perceived costs of screening poor accessibility to screening, poor awareness of cancer screening), psychological (e.g. fear of screening outcomes, low perceived risk of cancer), and cultural or religious (e.g. potential embarrassment from screening procedures, taboos regarding nakedness, contact with intimate body parts) dimensions (Damiani et al., 2012, Akinlotan et al., 2017, Alexandraki and Mooradian, 2010, Armstrong et al., 2012, George, 2000). These are often interwoven with provider- and system-level factors such as patient-provider communication, availability of subsidies or other financial assistance, and trust in the healthcare system and medical professionals (Akinlotan et al., 2017, Alexandraki and Mooradian, 2010, Schueler et al., 2008).
While such factors have been used to inform breast and cervical cancer screening initiatives, much less research has been conducted to understand the qualitative influence of gender itself in relation to these screening determinants. Gender is commonly defined as a conceptualisation of the roles, expectations, and resources in society that are ascribed to an individual’s sex, and commonly involves multiple social constructs including norms, socialisation, and power dynamics relating to gender (Cislaghi and Heise, 2020, Heise et al., 2019). These have increasingly been applied to better understand healthcare-related issues in recent years (Cislaghi and Heise, 2020, Cislaghi and Heise, 2019, Mackie and LeJeune, 2009). For example, embarrassment due to nudity is a common barrier not only for breast and cervical cancer screening, but also other health screening procedures undertaken by both genders (Chorley et al., 2017, Teo et al., 2016). However, studies have additionally shown that some female patients report more severe feelings of embarrassment specifically when having a male doctor carry out cervical screening on them, due to the sexual connotations of the procedure and the perceived vulnerability of being naked with a male stranger (Chorley et al., 2017, Logan and McIlfatrick, 2011).
As recent studies on women’s health have increasingly acknowledged the need to consider and adapt qualitative findings to improve the contextual relevance of medical practice guidelines, we argue that a deeper understanding of these gender-related nuances is crucial to the medical and public health community’s continued efforts to promote breast and cervical cancer screening (Abadir et al., 2014, Coombs et al., 2017, How et al., 2015).
The present review therefore aims to scope the international body of qualitative literature to better understand how existing gender norms influence women’s decision to undergo breast or cervical cancer screening in the general population. In doing so, we hope to identify persisting gaps in knowledge and suggest potential directions for future research and efforts to increase breast and cervical cancer screening uptake around the world.
2. Methods
2.1. Search strategy
A systematic search of peer-reviewed literature from three databases (PubMed, Scopus, CINAHL) was conducted from inception until December 2019. We utilised the following search strategy, using MeSH terms where appropriate:
(“breast cancer” OR “breast carcinoma” OR “mammary cancer” OR “mammary carcinoma”) AND (“screening” OR “prevention” OR “health screening” OR “mammography” OR “breast MRI” OR “mammogram” OR “breast exam”)
OR.
(“cervical cancer” OR “cervical lesion” OR “cervical carcinoma”) AND (“screening” OR “prevention” OR “health screening” OR “pap smear” OR “pap test” OR “HPV test”)
AND.
(“qualitative” OR “mixed-methods”)
The search strategy was applied to titles, abstracts and keywords within the three databases, and was restricted to English language publications.
2.2. Study selection
We included studies if (I) the context of the research was breast or cervical cancer screening as per US Preventive Services Task Force (USPSTF) recommendations (i.e. mammography for females aged 50 – 74 years; hrHPV or cervical cytology for females aged 30 – 65 years), (II) the study included a qualitative (e.g. in-depth interviews, focus group discussions) methodology, and (III) the study sample focused on women recruited from the general (i.e. non-migrant) population of each country in which the study was conducted. Due to the heterogeneity and broad variation of breast and cervical cancer screening guidelines across the world, the USPSTF was selected as a frame of reference in this study for two reasons: 1) USPSTF guidelines have commonly been used as a basis for evidence-based development of other national- or federal-level guidelines in countries where these exist, and 2) USPSTF recommendations for breast and cervical screening age ranges have been shown to match and/or overlap with the respective screening age eligibility in most other countries with existing guidelines (Ebell et al., 2018).
Studies were excluded if they (I) did not utilise a qualitative or mixed methods design, (II) were a review or meta-analysis or (III) were grey literature (i.e., not peer-reviewed). We excluded grey literature to ensure quality and scientific integrity in the included articles.
Additionally, for the context of this study and manuscript, we defined gender to represent and be used interchangeably with biological sex (i.e., biologically male or female at birth).
2.3. Data extraction and analysis
Studies were extracted from the three databases by one reviewer (GJW). Duplicates were identified and removed via EndNote X8. A preliminary screening of titles and abstracts was conducted by one reviewer (GJW). Full texts of shortlisted studies were reviewed independently by two reviewers (JL and PS). Disputes on study inclusion were resolved through discussion sessions among the three reviewers (GJW, JL and PS).
Data extraction from the included studies was performed by two reviewers (JL and PS). We used a standardised data spreadsheet to consolidate data on study design and methodology, description of participants, year and setting where study was conducted, and the key findings from each study. We then performed a narrative synthesis of the data to organise study findings into common themes for interpretation and discussion.
The narrative thematic analysis was performed by first summarising the primary themes extracted from each study into first-level (descriptive) subthemes. This was performed independently by two reviewers (JL and PS) and cross-checked to ensure completeness of the data summary. Second-level and third-level (analytical) themes were then synthesized from the first-level subthemes through mutual discussion and agreement among all co-authors. Primary themes identified in the original articles were used as a reference to check the study team’s understanding of the verbatim quotes provided. All verbatim quotes were also aggregated according to the analytical themes that arose for analysis across studies.
3. Results
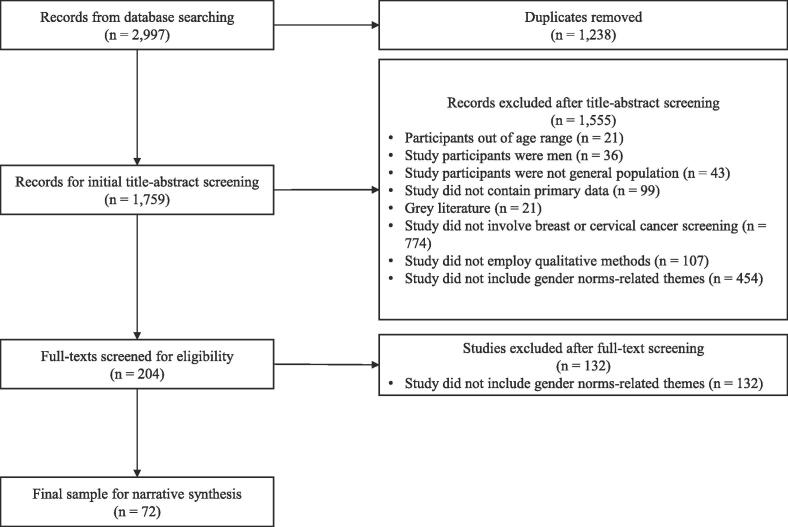
Our initial search of the three databases yielded 2997 records. Of these, 1238 were removed as duplicates, resulting in a total of 1759 records for initial screening of titles and abstracts. From these, we excluded 1555 records based on the inclusion and exclusion criteria described in the previous section. Of the 204 records shortlisted for full text screening, 132 were further excluded, resulting in a final sample of 72 studies to be included in this review. The systematic search and selection process, along with reasons for study exclusion, can be found in Fig. 1.
Fig. 1.
PRISMA flowchart depicting article search, screening, and selection process.
All themes were concretely present in every WHO subregion. However, we found that certain subthemes were more or less pertinent depending on country of origin. Following the description of each theme, we tabled how much emphasis each subtheme received. Then, we began a discussion by WHO subregion that provided a nuanced presentation of emphasised subthemes and built a likely profile for each WHO subregion. We defined a subtheme as being of emphasis in the country if at least 50% of articles (rounded down to nearest whole number) originating from that country had included this subtheme.
3.1. Characteristics of the included articles
The 72 studies spanned 34 countries. Excluding male participants and healthcare providers (HCP), the included studies comprised 3,821 women (aged 18 years and above). Of these, 28 studies focused exclusively on breast cancer, while 40 examined cervical cancer only, and the remaining four studies included both breast and cervical cancer. Eight studies also included perspectives from healthcare providers recruited as a subset of the respective samples. A description of each study’s year of publication, methodology, sample characteristics, and key findings, sorted by country of origin, is presented in Supplementary Table 1.
Three overarching third-level analytical themes pertaining to women’s decision to screen for breast and/or cervical cancer were generated from the narrative synthesis of primary themes extracted from each of the included studies. These pertained to the (I) gender socialisation of women, (II) gender inequality in women’s respective societies, and (III) lack of empowerment for women to make decisions to screen. The first-level descriptive and second-level analytical themes that comprise these three overarching themes are presented in Supplementary Table 2. To provide a better understanding of these themes in the included literature, we included verbatim extracts from participants in each of these studies (where relevant) and sorted the findings by WHO sub-region (World Health Organization, 2021) and by country of origin.
3.2. Gender socialisation of women (Theme 1)
Several subthemes characterised gender socialisation of women in the included studies. Women’s decision to screen was found to be constrained by established gender norms (Theme 1.1). These were based on a woman’s role in the household (Theme 1.1.1); women were expected to prioritise looking after their family’s needs and managing domestic responsibilities due to their position as wives and mothers (Macdonald et al., 2015, Urrutia et al., 2017, Yang et al., 2019, Trigoni et al., 2008, Nyblade et al., 2017, Thomas et al., 2011, Safizadeh et al., 2018, Shirzadi et al., 2020, Rasul et al., 2015, Baron-Epel et al., 2004, Azaiza and Cohen, 2008, Ngugi et al., 2012, Wong et al., 2008, Markovic et al., 2005, Khan and Woolhead, 2015, Daley et al., 2012, Filippi et al., 2013, Tessaro et al., 1994, Nekhlyudov et al., 2003, Nolan et al., 2014, Nonzee et al., 2015). Women in the included studies also expressed that there were sociocultural expectations on female behaviour (Theme 1.1.2); they were expected to care for others’ health above their own (Trigoni et al., 2008, Wong et al., 2008, Filippi et al., 2013, Tessaro et al., 1994, Thomas et al., 2011, Safizadeh et al., 2018, Shirzadi et al., 2020, Rasul et al., 2015, Nolan et al., 2014, Nonzee et al., 2015, McMichael et al., 2000, Manderson and Hoban, 2006, Dey et al., 2016, Savabi-Esfahani et al., 2018, Khazaee-pool et al., 2014, Khazir et al., 2019), and were expected to have a sense of modesty that was incompatible with the bodily exposure required during breast or cervical screening (Macdonald et al., 2015, Azaiza and Cohen, 2008, Isa Modibbo et al., 2016, Püschel et al., 2010, Ndejjo et al., 2017). However, women in several studies also mentioned that there was a motivation to engage in cancer screening in order to stay healthy for the sake of their family.
Personal barriers (Theme 1.2) were also present in most studies. These included embarrassment (Theme 1.2.1) in having to expose private body parts to healthcare providers, especially if these were male or if the women were circumcised (Ngugi et al., 2012, Daley et al., 2012, Khazaee-pool et al., 2014, Ackerson, 2010, Khazaee-Pool et al., 2014). Screening was also seen as an invasion of privacy (Theme 1.2.2) where relative strangers were permitted to not only see intimate parts of the woman’s body, but also their medical conditions or records (Bayrami et al., 2015, Armstrong et al., 2012). Lastly, personal barriers also included the possible loss of femininity/womanhood (Theme 1.2.3) due to the fear of sexual organs being removed (e.g. mastectomy) due to cancer detected via screening (Thomas et al., 2011, Safizadeh et al., 2018, Tessaro et al., 1994, McMichael et al., 2000, Khazaee-pool et al., 2014, Baron-Epel et al., 2004, Azaiza and Cohen, 2008, Ngugi et al., 2012, Granado et al., 2014, Bahmani et al., 2016, Malhotra et al., 2016, Gu et al., 2017); this was accompanied in some studies by the additional concern of the women not being able to remain sexually active with their spouses after undergoing breast or cervical cancer treatment (Safizadeh et al., 2018, Azaiza and Cohen, 2008, Ngugi et al., 2012, McMichael et al., 2000, Granado et al., 2014, Gu et al., 2017).
Religion (Theme 1.3) was another subtheme that featured how women were gender socialised. Religious teaching or common beliefs (Theme 1.3.1) promoted a sense of responsibility amongst women to take care of their own health, but conversely dissuaded women from being immodest by exposing themselves to men other than their spouses (even if the man was a healthcare provider) (Isa Modibbo et al., 2016, Kahn et al., 2006). Some women, on the other hand, professed more fatalistic beliefs regarding health, and declined screening as having cancer was seen as “fate” or the “will of God” (Safizadeh et al., 2018, Rasul et al., 2015, Azaiza and Cohen, 2008, Khan and Woolhead, 2015, Nolan et al., 2014, Khazaee-pool et al., 2014, Kahn et al., 2006, Binka et al., 2019, Lunsford et al., 2017, Hassani et al., 2017, Khodayarian et al., 2016, Sabih et al., 2012, Arabaci and Ozsoy, 2012, Shaw et al., 2018).
Lastly, cultural stigma (Theme 1.4) was often cited as a barrier, especially due to the sexual context of breast and cervical screening (Theme 1.4.1). Here, “sexual context of screening” refers to the recognition of the perceived exclusiveness and cultural significance of being allowed to view and/or touch a woman’s sexual organs. It is this normative perception of privilege or exclusiveness that causes men and women to feel uncomfortable with the perceived inappropriateness about interactions involving a woman’s sexual organs that are not specifically with her husband. In addition to the fear of being seen as promiscuous due to the nature of cervical cancer, women reported that these two cancers – and female health issues in general – were generally taboo topics that should not be discussed except in private (Thomas et al., 2011, Azaiza and Cohen, 2008, Khan and Woolhead, 2015, Khazir et al., 2019, Bayrami et al., 2015, Malhotra et al., 2016, Lunsford et al., 2017, Shaw et al., 2018, Onyenwenyi and Mchunu, 2018).
Table 1 details the presence of Theme 1 subthemes by WHO subregion. The subthemes of invasion of privacy (1.2.2) and loss of womanhood (1.2.3) did not qualify for emphasis in any WHO subregion. Conversely, the subthemes on embarrassment (1.2.1) and sexual context of the screening (1.4) received emphasis across all WHO subregions. Women’s role in household (1.1.1), while not as emphasised, was also present for all WHO subregions.
Table 1.
Presence of Theme 1 (gender socialisation of women) by WHO subregions.
| Africa (n = 10) | Americ-as (n = 17) | Eastern Mediterranean (n = 16) | Europe (n = 11) | South-east Asia (n = 5) | Western Pacific Region (n = 11) | Total no. sub-regions with sub-theme | |
|---|---|---|---|---|---|---|---|
| Role in household (1.1.1) | 1 | 10* | 7 | 5* | 2* | 3 | 6 |
| Socio-cultural expectation (1.1.2) | 0 | 1 | 0 | 1 | 2* | 0 | 3 |
| Embarrass-ment (1.2.1) | 5* | 14* | 13* | 8* | 5* | 6* | 6 |
| Invasion of privacy (1.2.2) | 0 | 3 | 1 | 2 | 0 | 1 | 4 |
| Losing womanhood (1.2.3) | 1 | 2 | 4 | 2 | 0 | 3 | 5 |
| Religious/ common beliefs (1.3) | 5* | 5 | 7* | 3 | 0 | 1 | 5 |
| Sexual context/ stigma (1.4) | 6* | 12* | 8* | 6* | 5* | 8* | 6 |
Note: Indicates emphasis received in WHO subregion based on 50% threshold of articles (rounded down to nearest whole number) from that subregion capturing the subtheme.
3.3. Gender inequality in society (Theme 2)
Gender inequality was comprised of one second-level analytical theme in that men tended to have more power and receive more priority than women in their respective societies (Theme 2.1). Husbands were noted to be a key barrier (Theme 2.1.1) as women were often unable to decide to undergo breast or cervical screening by themselves and needed the approval of their husbands, who sometimes did not believe that screening was required (Shirzadi et al., 2020, Binka et al., 2019, Onyenwenyi and Mchunu, 2018, William et al., 2013, Keshavarz et al., 2011). Even if husbands permitted their wives to attend screening, women reported that it was a requirement to be accompanied by them (Baron-Epel et al., 2004, Khazaee-pool et al., 2014). Men also tended to control the household finances, which required women to have their husbands pay for screening-related or other healthcare costs (Hassani et al., 2017, Keshavarz et al., 2011). The effect of breast and cervical cancer on marital relations (Theme 2.1.2) was also evident, as participants highlighted that a sick woman would be perceived as being unable to contribute in a marital relationship (Baron-Epel et al., 2004, Bahmani et al., 2016). Women were also fearful that this would then lead to abandonment and/or divorce by their husbands (Safizadeh et al., 2018, Shirzadi et al., 2020, Baron-Epel et al., 2004, Khan and Woolhead, 2015, McMichael et al., 2000, Khazaee-pool et al., 2014, Ndejjo et al., 2017, Gu et al., 2017, Sabih et al., 2012, Onyenwenyi and Mchunu, 2018, Mutyaba et al., 2007, Pelcastre-Villafuerte et al., 2007, Ansink et al., 2008). Family was often seen as a barrier (Theme 2.1.3) as women’s health needs were de-prioritised compared to that of male relatives, and women needed the approval of their family members when deciding on healthcare matters in general (Hassani et al., 2017, Darj et al., 2019).
Table 2 details the presence of Theme 2 subthemes across WHO subregions. The subtheme of male priority in the family (2.1.3) did not receive any emphasis, and the other two subthemes were only emphasized in one subregion each. However, the subtheme effect on marital relationship (2.1.2) was present across all WHO subregions.
Table 2.
Presence of Theme 2 (gender inequality in society) by WHO subregion.
| Africa (n = 10) | Americ-as (n = 17) | Eastern Mediterranean (n = 16) | Europe (n = 11) | South-east Asia (n = 5) | Western Pacific Region (n = 11) | Total no. sub-regions with sub-theme | |
|---|---|---|---|---|---|---|---|
| Husband barrier (2.1.1) | 6* | 3 | 4 | 3 | 1 | 1 | 6 |
| Effect on marital relationship (2.1.2) | 3 | 1 | 6 | 2 | 3* | 2 | 6 |
| Male priority (2.1.3) | 0 | 0 | 1 | 0 | 1 | 0 | 2 |
Note: Indicates emphasis received in WHO subregion based on 50% threshold of articles (rounded down to nearest whole number) from that subregion capturing the subtheme.
3.4. Lack of empowerment (Theme 3)
A general lack of empowerment of women was also evidenced from the included studies. Women tended to reflect poor knowledge (Theme 3.1) in both a health (i.e. understanding the aims and benefits of cancer screening) and general education (i.e. fewer opportunities to learn and/or acquire information) context (Macdonald et al., 2015, Yang et al., 2019, Ngugi et al., 2012, Markovic et al., 2005, Daley et al., 2012, Filippi et al., 2013, Nolan et al., 2014, Ndejjo et al., 2017, Kahn et al., 2006, Binka et al., 2019, Onyenwenyi and Mchunu, 2018, Brandt et al., 2019, Teng et al., 2014, Oscarsson et al., 2008). Women were also more likely to need financial support (Theme 3.2) and be financially dependent on spouses or their families (Shirzadi et al., 2020, Ngugi et al., 2012, Filippi et al., 2013, Tessaro et al., 1994, Ndejjo et al., 2017, Binka et al., 2019, Shaw et al., 2018, Mutyaba et al., 2007, Pelcastre-Villafuerte et al., 2007, Darj et al., 2019, Urrutia et al., 2017, Yang et al., 2019, Trigoni et al., 2008, Dey et al., 2016, Savabi-Esfahani et al., 2018, Khazaee-pool et al., 2014, Khazir et al., 2019, Granado et al., 2014, Bahmani et al., 2016, Malhotra et al., 2016, Gu et al., 2017, Andrasik et al., 2008, Ersin and Bahar, 2011, Lovell et al., 2007, Holroyd et al., 2004). Lastly, women in several studies highlighted practical barriers (Theme 3.3) that prevented them from attending breast and cervical screening programmes, even if there was the intention to do so. Most prominently, this included the inability to find alternative arrangements for motherhood responsibilities (e.g. childcare services) (Holroyd et al., 2004).
Table 3 illustrates the presence of Theme 3 subthemes in each WHO subregion. A demonstration of poor knowledge of sexual health (3.1) received the most emphasis of four of the six WHO subregions and were present in all of them. The subthemes of lacking finances (3.2) and practical barriers to screening (3.3) received emphasis from only two and one WHO subregions respectively but were present in five and all WHO subregions respectively.
Table 3.
Presence of Theme 3 (Lack of empowerment) by WHO subregion.
| Africa (n = 10) | Americ-as (n = 17) | Eastern Mediterranean (n = 16) | Europe (n = 11) | South-east Asia (n = 5) | Western Pacific Region (n = 11) | Total no. sub-regions with sub-theme | |
|---|---|---|---|---|---|---|---|
| Poor knowledge (3.1) | 6* | 7 | 12* | 7 | 4* | 3 | 6 |
| Lacking finances (3.2) | 4 | 7 | 6 | 2 | 2* | 6* | 5 |
| Practical barriers (3.3) | 2 | 7 | 3 | 5* | 1 | 4 | 6 |
Note: Indicates emphasis received in WHO subregion based on 50% threshold of articles (rounded down to nearest whole number) from that subregion capturing the subtheme.
4. Discussion
To the best of our knowledge, this was the first review that attempts to comprehensively understand how pre-existing gender norms qualitatively influenced women’s decision to undergo breast and cervical cancer screening from an international perspective. The studies in our review collectively involved women from a wide selection of populations across 34 countries, covering nearly every continent. All derived themes of gender socialisation of women (Theme 1), gender inequality in society (Theme 2), and lack of women empowerment (Theme 3) were concretely represented for all WHO subregions. This attests to the consistency and applicability of all three abstracted themes globally.
In conducting this review, we sometimes categorised single quotes under multiple categories, and some developed subthemes like personal barriers or cultural stigmas had some conceptual overlap. The different subthemes reflect many sources of value judgements experienced by women, hence, for nuances to be more clearly defined, we differentiated them. However, these subthemes are all tied to the underlying concept of these women being female leading to the apparent conceptual overlap. The appearance of quotes under multiple themes also demonstrates the extent to which these barriers/beliefs are intertwined with the role and identity of women as they consider themselves in relation to their communities.
In terms of distribution of subthemes, the WHO subregions reveal interesting variations. First, there are particular subthemes that receive widespread emphasis across most or all WHO subregions. Under gender socialization (Theme 1), embarrassment (1.2.1) and sexual context of the screening (1.4) received emphasis across all WHO subregions; on lack of empowerment of women (Theme 3), a demonstration of poor knowledge of sexual health (3.1) received the most emphasis of four of the six WHO subregions. These could be candidates for more generic or global intervention aims and standards that remain impactful to women. Problems posed by gender inequality in society (Theme 2) and other subthemes from gender socialization and empowerment of women present in greater variation across WHO subregions and are likely to require more nuanced and locale-centric interventions. Researchers can use the region profiles presented in the results as rough guides for the likely issues that need to be addressed in their country of interest.
In general, we found that women’s decision to go for screening across the included studies was most commonly constrained by sociocultural expectations on what it meant to be a woman. This ranged from established beliefs in which women were expected to prioritise the role(s) of being a daughter, wife, or mother above their own health and wellbeing needs, to personal barriers of modesty and privacy concerns surrounding breast and cervical screening manifested as expected in the included studies – often in tandem, however, with influence that stemmed from religious teachings (e.g. immodesty around strangers of opposing gender) and cultural taboos surrounding women’s and sexual health. Women seemed to have a values judgement on being the lowest priority in the family; they used expressions like “have to” and “should” to express these strong implicit beliefs. This also resulted in women inflicting these normative judgements on each other and possibly preventing them from supporting other women’s attempts to screen by pooling resources as a community to do things like caring for neighbours’ children while they go for screening. There also seemed to be a strong idea that women needed to be “whole” to be regarded as a woman, and this seemed to threaten both women’s self-identity and worth to their families. Thus, the possible loss of sexual organs and the reconceptualization of what it means to be a woman independent of her physical self could be key targets for normative interventions.
Gender inequalities were also a common and interesting finding in this review. While international literature on healthcare access has consistently noted disparities in health services utilisation between men and women, our review found that there seemed to be two key dimensions to this issue within the context of female cancer screening (Cockerham et al., 2017, Ghose et al., 2017, Parra-Casado et al., 2018, García-Altés et al., 2018). On an instrumental level, women’s access depended on the husband or male family members’ approval and ability to financially facilitate screening. However, women also expressed normative beliefs that being found to be ill with breast or cervical cancer would somehow be their fault, and lead to abandonment if their husbands decided that they were no longer able to contribute to the marital or family relationship. This created fearfulness that factored into decisions against going for breast or cervical cancer screening. Such fearfulness may be more difficult to deal with as it is interpersonal in nature and requires the support and endorsement of husbands to change.
Undercutting these abovementioned broad issues was the finding that women often demonstrated relatively poor health awareness and fewer opportunities to access such education compared to men, compounded by socioeconomic and functional inequalities that are consistent across the literature (Tweed et al., 2018, Sarti and Espinola, 2018). This highlights the limited reach that current efforts have when familial demands prevent women from screening. More ground-level outreach may be necessary to bring women’s health education to them in a way that is practically convenient, palatable to their families, and perhaps even places benefit to families and husbands as a primary outcome. This could lower practical barriers and minimise social stigma against women’s screening for sexual health. Only one article (623) in this review had both current and non-current or naïve screeners for mammogram as a comparison that raised access and difficulty in arranging follow ups as structural barriers. Other studies did not make this comparison but also cited other structural factors that are heterogenous even within WHO subregions.
From women’s discussions of screening, it was also apparent that they tended to value themselves in terms of their usefulness to their husbands and their families, and not as individuals. Examples of phrases that expressed this implicit sentiment were “property (Africa)”, “husband did not let me (Eastern Mediterranean)”, “has to tell her husband (Europe)”, “husband is going to look at you stupid (Western Pacific)”, “perception of family members about her changes (South-east Asia)”, and “your husband is not going to want you (Americas)”. This not only reflects the disempowered state that being a woman constrains an individual into, but also suggests that women in some places are perceived as valuable insofar as they are “owned” and “useful” to the husband or family. This means that for women’s screening to be acceptable in the community, it must contribute to the welfare and image of the family and women’s husbands. More studies could also be conducted with husbands of women in the community to better triangulate whether unhelpful normative beliefs are also held by and propagated by them.
Both breast and cervical cancer screening were discussed together in this review as we have found no distinct differences in abstracted perceived barriers to screening between these groups of studies. The only notable qualitative difference is the heightened fear of losing the uterus as it is more conceptually and biologically tied to motherhood. This fear has both positive and negative impacts as it can prevent some women from wanting to find out whether they have cancer as they would rather die than lose motherhood, or it can spur them to screen to catch cancer early. Those planning interventions may want to conduct preliminary surveys or interviews to understand the local perceptions of motherhood and loss of childbearing before deciding on a narrative.
4.1. Limitations and conclusions
This study has broadly characterised the prominent barriers to women’s decision to screen for breast and cervical cancers that have been elicited qualitatively. However, there are a few limitations in our review that should be considered. Firstly, we excluded non-peer reviewed literature and only limited our search to established international scientific databases. While this may have improved the quality of studies yielded from our search strategy, it may have resulted in fewer yields from certain WHO regions, especially from countries in which English is not the predominant language of academic writing and publication. Because studies are more limited for some of these countries (represented only by one or two studies), these findings may need to be more strongly supported with further qualitative and quantitative exploration within these communities of women. Additionally, as there are no standards for what topics qualify as being emphasised in a country, our 50% threshold for emphasis is an arbitrary benchmark that should be verified with pre-emptive quantitative studies before actual interventions are planned, in order to ensure that the intended communities’ unmet needs are properly met. Lastly, while our intention was to focus on the qualitative body of literature with the addition of the ad hoc filter terms “qualitative” and “mixed-methods” in the search strategy, this could have inadvertently excluded a proportion of studies which could have used pseudo-qualitative methods or components within their study design but did not define their terminology as such.
While existing reviews have contributed to the literature by focusing on specific cancers (either breast or cervical) (Dieleman et al., 2022, Özkan and Taylan, 2021, Pagliarin et al., 2021), or on specific subpopulations (by geographical region, ethnicity, or cultural background) (Kandasamy et al., 2021, Christy et al., 2021, Chua et al., 2021, McFarland et al., 2016), the present research represents a novel attempt to apply an international focus on the qualitative factors surrounding breast and cervical cancer screening for women around the world. To conclude, our review suggests that while the broad themes of gender socialisation, inequality, and empowerment of women are common across studies, every WHO subregion has its own characteristic subtleties that are themselves influenced by sociocultural norms. Nonetheless, embarrassment (1.2.1) and the often sexual context of breast and cervical screening (1.4) were expressed by women in all WHO subregions; future educative interventions can perhaps target changing these foundational normative beliefs about the social implications of these screenings as a starting point in tackling this complex and highly nuanced problem.
Funding
This work was supported by the Singapore Ministry of Health’s National Medical Research Council under the Centre Grant Programme – Singapore Population Health Improvement Centre (NMRC/CG/C026/2017_NUHS).
CRediT authorship contribution statement
Jerrald Lau: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Writing – original draft, Writing – review & editing. Pami Shrestha: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Writing – review & editing. Janelle Shaina Ng: Data curation, Writing – original draft, Writing – review & editing. Gretel Jianlin Wong: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. Helena Legido-Quigley: Funding acquisition, Supervision, Writing – review & editing. Ker-Kan Tan: Conceptualization, Funding acquisition, Supervision, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2022.101816.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Abadir A.M., Lang A., Klein T., Abenhaim H.A. Influence of qualitative research on women's health screening guidelines. Am. J. Obstet. Gynecol. 2014;210(1):44.e41. doi: 10.1016/j.ajog.2013.09.021. [DOI] [PubMed] [Google Scholar]
- Ackerson K. Personal influences that affect motivation in Pap smear testing among African American women. J. Obstet. Gynecol. Neonatal. Nurs. 2010;39(2):136–146. doi: 10.1111/j.1552-6909.2010.01104.x. [DOI] [PubMed] [Google Scholar]
- Akinlotan M., Bolin J.N., Helduser J., Ojinnaka C., Lichorad A., McClellan D. Cervical cancer screening barriers and risk factor knowledge among uninsured women. J. Community Health. 2017;42(4):770–778. doi: 10.1007/s10900-017-0316-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexandraki I., Mooradian A.D. Barriers related to mammography use for breast cancer screening among minority women. J. Natl Med. Assoc. 2010;102(3):206–218. doi: 10.1016/s0027-9684(15)30527-7. [DOI] [PubMed] [Google Scholar]
- Andrasik M.P., Rose R., Pereira D., Antoni M. Barriers to cervical cancer screening among low-income HIV-positive African American women. J. Health Care Poor Underserved. 2008;19(3):912–925. doi: 10.1353/hpu.0.0037. [DOI] [PubMed] [Google Scholar]
- Ansink A., Tolhurst R., Haque R., Saha S., Datta S., Van den Broek N. Cervical cancer in Bangladesh: community perceptions of cervical cancer and cervical cancer screening. Trans. R. Soc. Trop. Med. Hyg. 2008;102(5):499–505. doi: 10.1016/j.trstmh.2008.01.022. [DOI] [PubMed] [Google Scholar]
- Arabaci Z., Ozsoy S. The pap-smear test experience of women in Turkey: a qualitative study. Asian Pac. J. Cancer Prev. 2012;13(11):5687–5690. doi: 10.7314/apjcp.2012.13.11.5687. [DOI] [PubMed] [Google Scholar]
- Armstrong N., James V., Dixon-Woods M. The role of primary care professionals in women’s experiences of cervical cancer screening: a qualitative study. Fam. Pract. 2012;29(4):462–466. doi: 10.1093/fampra/cmr105. [DOI] [PubMed] [Google Scholar]
- Armstrong N., James V., Dixon-Woods M. The role of primary care professionals in women's experiences of cervical cancer screening: a qualitative study. Fam. Pract. 2012;29(4):462–466. doi: 10.1093/fampra/cmr105. [DOI] [PubMed] [Google Scholar]
- Azaiza F., Cohen M. Between traditional and modern perceptions of breast and cervical cancer screenings: a qualitative study of Arab women in Israel. Psycho-Oncology. 2008;17(1):34–41. doi: 10.1002/pon.1180. [DOI] [PubMed] [Google Scholar]
- Bahmani A., Baghianimoghadam M.H., Enjezab B., Mahmoodabad S.S.M., Askarshahi M. Factors affecting cervical cancer screening behaviors based on the precaution adoption process model: a qualitative study. Global J. Health Sci. 2016;8(6):211. doi: 10.5539/gjhs.v8n6p211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron-Epel O., Granot M., Badarna S., Avrami S. Perceptions of breast cancer among Arab Israeli women. Women Health. 2004;40(2):101–116. doi: 10.1300/J013v40n02_07. [DOI] [PubMed] [Google Scholar]
- Bayrami R., Taghipour A., Ebrahimipour H. Personal and socio-cultural barriers to cervical cancer screening in Iran, patient and provider perceptions: a qualitative study. Asian Pac. J. Cancer Prev. 2015;16(9):3729–3734. doi: 10.7314/apjcp.2015.16.9.3729. [DOI] [PubMed] [Google Scholar]
- Binka C., Nyarko S.H., Awusabo-Asare K., Doku D.T. Barriers to the uptake of cervical cancer screening and treatment among rural women in Ghana. Biomed Res. Int. 2019;2019:1–8. doi: 10.1155/2019/6320938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleyer A., Welch H.G. Effect of three decades of screening mammography on breast-cancer incidence. N. Engl. J. Med. 2012;367(21):1998–2005. doi: 10.1056/NEJMoa1206809. [DOI] [PubMed] [Google Scholar]
- Brandt T., Wubneh S.B., Handebo S., Debalkie G., Ayanaw Y., Alemu K., Jede F., von Knebel Doeberitz M., Bussmann H. Genital self-sampling for HPV-based cervical cancer screening: a qualitative study of preferences and barriers in rural Ethiopia. BMC Public Health. 2019;19(1) doi: 10.1186/s12889-019-7354-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chorley A.J., Marlow L.A.V., Forster A.S., Haddrell J.B., Waller J. Experiences of cervical screening and barriers to participation in the context of an organised programme: a systematic review and thematic synthesis. Psycho-oncology. 2017;26(2):161–172. doi: 10.1002/pon.4126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christy K., Kandasamy S., Majid U., Farrah K., Vanstone M. Understanding Black Women's Perspectives and Experiences of Cervical Cancer Screening: A Systematic Review and Qualitative Meta-synthesis. J. Health Care Poor Underserved. 2021;32(4):1675–1697. doi: 10.1353/hpu.2021.0159. [DOI] [PubMed] [Google Scholar]
- Chua B., Ma V., Asjes C., Lim A., Mohseni M., Wee H.L. Barriers to and Facilitators of Cervical Cancer Screening among Women in Southeast Asia: A Systematic Review. Int. J. Environ. Res. Public Health. 2021;18(9):4586. doi: 10.3390/ijerph18094586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cislaghi B., Heise L. Using social norms theory for health promotion in low-income countries. Health Promotion Int. 2019;34(3):616–623. doi: 10.1093/heapro/day017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cislaghi B., Heise L. Gender norms and social norms: differences, similarities and why they matter in prevention science. Sociol. Health Illn. 2020;42(2):407–422. doi: 10.1111/1467-9566.13008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cockerham W.C., Hamby B.W., Hankivsky O., Baker E.H., Rouhani S. Self-rated health and barriers to healthcare in Ukraine: The pivotal role of gender and its intersections. Communist Post-Communist Stud. 2017;50(1):53–63. [Google Scholar]
- Coombs M.A., Davidson J.E., Nunnally M.E., Wickline M.A., Curtis J.R. Using qualitative research to inform development of professional guidelines: a case study of the society of critical care medicine family-centered care guidelines. Crit. Care Med. 2017;45(8):1352–1358. doi: 10.1097/CCM.0000000000002523. [DOI] [PubMed] [Google Scholar]
- Daley C.M., Kraemer-Diaz A., James A.S., Monteau D., Joseph S., Pacheco J., Bull J.W., Cully A., Choi W.S., Greiner K.A. Breast cancer screening beliefs and behaviors among American Indian women in Kansas and Missouri: A qualitative inquiry. J. Cancer Educ. 2012;27(S1):32–40. doi: 10.1007/s13187-012-0334-3. [DOI] [PubMed] [Google Scholar]
- Damiani G., Federico B., Basso D., Ronconi A., Bianchi C.B.N.A., Anzellotti G.M., Nasi G., Sassi F., Ricciardi W. Socioeconomic disparities in the uptake of breast and cervical cancer screening in Italy: a cross sectional study. BMC Public Health. 2012;12(1) doi: 10.1186/1471-2458-12-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darj E., Chalise P., Shakya S. Barriers and facilitators to cervical cancer screening in Nepal: A qualitative study. Sexual Reproductive Healthcare. 2019;20:20–26. doi: 10.1016/j.srhc.2019.02.001. [DOI] [PubMed] [Google Scholar]
- Dey S., Sharma S., Mishra A., Krishnan S., Govil J., Dhillon P.K. Breast cancer awareness and prevention behavior among women of Delhi, India: identifying barriers to early detection. Breast Cancer: Basic Clin. Res. 2016;10 doi: 10.4137/BCBCR.S40358. BCBCR.S40358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dieleman M., de Waard J., Wisman G.B.A., Schuuring E.d., Esajas M.D., Vermeulen K.M., de Bock G.H. Preferences and Experiences Regarding the Use of the Self-Sampling Device in hrHPV Screening for Cervical Cancer. Patient. 2022;15(2):245–253. doi: 10.1007/s40271-021-00550-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebell M.H., Thai T.N., Royalty K.J. Cancer screening recommendations: an international comparison of high income countries. Public Health Rev. 2018;39:7. doi: 10.1186/s40985-018-0080-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ersin F., Bahar Z. Inhibiting and facilitating factors concerning breast cancer early diagnosis behavior in Turkish women: a qualitative study according to the health belief and health development models. Asian Pac. J. Cancer Prev. 2011;12(7):1849–1854. [PubMed] [Google Scholar]
- Filippi M.K., Ndikum-Moffor F., Braiuca S.L., Goodman T., Hammer T.L., James A.S., Choi W.S., Greiner K.A., Daley C.M. Breast cancer screening perceptions among American Indian women under age 40. J. Cancer Educ. 2013;28(3):535–540. doi: 10.1007/s13187-013-0499-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Altés A., Ruiz-Muñoz D., Colls C., Mias M., Bassols N.M. Socioeconomic inequalities in health and the use of healthcare services in Catalonia: analysis of the individual data of 7.5 million residents. J. Epidemiol. Community Health. 2018;72(10):871–879. doi: 10.1136/jech-2018-210817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George S.A. Barriers to breast cancer screening: an integrative review. Health Care Women Int. 2000;21(1):53–65. doi: 10.1080/073993300245401. [DOI] [PubMed] [Google Scholar]
- Ghose B., Feng D.a., Tang S., Yaya S., He Z., Udenigwe O., Ghosh S., Feng Z. Women’s decision-making autonomy and utilisation of maternal healthcare services: results from the Bangladesh Demographic and Health Survey. BMJ Open. 2017;7(9):e017142. doi: 10.1136/bmjopen-2017-017142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gianino M.M., Lenzi J., Bonaudo M., Fantini M.P., Siliquini R., Ricciardi W., Damiani G. Organized screening programmes for breast and cervical cancer in 17 EU countries: trajectories of attendance rates. BMC Public Health. 2018;18(1) doi: 10.1186/s12889-018-6155-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg O., Bray F., Coleman M.P., Vanderpuye V., Eniu A., Kotha S.R., Sarker M., Huong T.T., Allemani C., Dvaladze A., Gralow J., Yeates K., Taylor C., Oomman N., Krishnan S., Sullivan R., Kombe D., Blas M.M., Parham G., Kassami N., Conteh L. The global burden of women's cancers: a grand challenge in global health. Lancet (London, England). 2017;389(10071):847–860. doi: 10.1016/S0140-6736(16)31392-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Global Cancer Observatory. Cancer Today. https://gco.iarc.fr/today/home. Published n.d. Accessed.
- Granado M.N., Guell C., Hambleton I.R., Hennis A.J., Rose A.M. Exploring breast cancer screening barriers among Barbadian women: a focus group study of mammography in a resource-constrained setting. Crit. Public Health. 2014;24(4):429–444. [Google Scholar]
- Gu C., Chen W.-T., Zhang Q., Chow K.M., Wu J., Tao L., Chan C.W.H. Exploring Chinese women’s perception of cervical cancer risk as it impacts screening behavior: A qualitative study. Cancer Nurs. 2017;40(4):E17–E25. doi: 10.1097/NCC.0000000000000400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassani L., Dehdari T., Hajizadeh E., Shojaeizadeh D., Abedini M., Nedjat S. Barriers to Pap Smear Test for the Second Time in Women Referring to Health Care Centers in the South of Tehran: A Qualitative Approach. Int. J. Community Based Nurs. Midwifery. 2017;5(4):376. [PMC free article] [PubMed] [Google Scholar]
- Heise L., Greene M.E., Opper N., Stavropoulou M., Harper C., Nascimento M., Zewdie D., Darmstadt G.L., Greene M.E., Hawkes S., Heise L., Henry S., Heymann J., Klugman J., Levine R., Raj A., Rao Gupta G. Gender inequality and restrictive gender norms: framing the challenges to health. The Lancet. 2019;393(10189):2440–2454. doi: 10.1016/S0140-6736(19)30652-X. [DOI] [PubMed] [Google Scholar]
- Holroyd E., Twinn S., Adab P. Socio-cultural influences on Chinese women's attendance for cervical screening. J. Adv. Nurs. 2004;46(1):42–52. doi: 10.1111/j.1365-2648.2003.02964.x. [DOI] [PubMed] [Google Scholar]
- How J.A., Abitbol J., Lau S., Gotlieb W.H., Abenhaim H.A. The impact of qualitative research on gynaecologic oncology guidelines. J. Obstetr. Gynaecol. Canada. 2015;37(2):138–144. doi: 10.1016/S1701-2163(15)30335-2. [DOI] [PubMed] [Google Scholar]
- Isa Modibbo F., Dareng E., Bamisaye P., Jedy-Agba E., Adewole A., Oyeneyin L., Olaniyan O., Adebamowo C. Qualitative study of barriers to cervical cancer screening among Nigerian women. BMJ Open. 2016;6(1):e008533. doi: 10.1136/bmjopen-2015-008533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn L.S., Fox C.H., Krause-Kelly J., Berdine D.E., Cadzow R.B. Identifying barriers and facilitating factors to improve screening mammography rates in women diagnosed with mental illness and substance use disorders. Women Health. 2006;42(3):111–126. doi: 10.1300/j013v42n03_07. [DOI] [PubMed] [Google Scholar]
- Kandasamy S., Jonathan Y., Majid U., Farrah K., Vanstone M. Indigenous women's experiences of cervical cancer screening: Incorporating Indigenous ways of knowing into a systematic review and meta-synthesis of qualitative research. Glob Public Health. 2021:1–14. doi: 10.1080/17441692.2021.2010115. [DOI] [PubMed] [Google Scholar]
- Keshavarz Z., Simbar M., Ramezankhani A. Factors for performing breast and cervix cancer screening by Iranian female workers: a qualitative-model study. Asian Pac. J. Cancer Prev. 2011;12(6):1517–1522. [PubMed] [Google Scholar]
- Khan S., Woolhead G. Perspectives on cervical cancer screening among educated Muslim women in Dubai (the UAE): a qualitative study. BMC Women's Health. 2015;15(1):1–13. doi: 10.1186/s12905-015-0252-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khazaee-pool M., Majlessi F., Foroushani A.R., Montazeri A., Nedjat S., Shojaeizadeh D., Tol A., Salimzadeh H. Perception of breast cancer screening among Iranian women without experience of mammography: a qualitative study. Asian Pac. J. Cancer Prev. 2014;15(9):3965–3971. doi: 10.7314/apjcp.2014.15.9.3965. [DOI] [PubMed] [Google Scholar]
- Khazaee-Pool M., Montazeri A., Majlessi F., Foroushani A.R., Nedjat S., Shojaeizadeh D. Breast cancer-preventive behaviors: exploring Iranian women’s experiences. BMC Women's Health. 2014;14(1):1–9. doi: 10.1186/1472-6874-14-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khazir Z., Morowatisharifabad M.A., Vaezi A., Enjezab B., Yari F., Fallahzadeh H. Perceived behavioral control in mammography: a qualitative study of Iranian women’s experiences. Int. J. Cancer Manage. 2019;12(8) [Google Scholar]
- Khodayarian M., Mazloomi-Mahmoodabad S.S., Lamyian M., Morowatisharifabad M.A., Tavangar H. Response costs of mammography adherence: Iranian women’s perceptions. Health Promotion Perspect. 2016;6(2):85. doi: 10.15171/hpp.2016.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lees B.F., Erickson B.K., Huh W.K. Cervical cancer screening: evidence behind the guidelines. Am. J. Obstet. Gynecol. 2016;214(4):438–443. doi: 10.1016/j.ajog.2015.10.147. [DOI] [PubMed] [Google Scholar]
- Logan L., McIlfatrick S. Exploring women's knowledge, experiences and perceptions of cervical cancer screening in an area of social deprivation. Eur. J. Cancer Care (Engl). 2011;20(6):720–727. doi: 10.1111/j.1365-2354.2011.01254.x. [DOI] [PubMed] [Google Scholar]
- Lovell S., Kearns R.A., Friesen W. Sociocultural barriers to cervical screening in South Auckland, New Zealand. Soc. Sci. Med. 2007;65(1):138–150. doi: 10.1016/j.socscimed.2007.02.042. [DOI] [PubMed] [Google Scholar]
- Lunsford N.B., Ragan K., Smith J.L., Saraiya M., Aketch M. Environmental and psychosocial barriers to and benefits of cervical cancer screening in Kenya. Oncologist. 2017;22(2):173. doi: 10.1634/theoncologist.2016-0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macdonald C., Martin-Misener R., Steenbeek A., Browne A. Discourse/Discours-Honouring Stories: Mi'kmaq Women's Experiences With Pap Screening in Eastern Canada. Can. J. Nurs. Res. Arch. 2015;47(1):72–96. doi: 10.1177/084456211504700106. [DOI] [PubMed] [Google Scholar]
- Mackie, G., LeJeune, J., 2009. Social dynamics of abandonment of harmful practices: A new look at the theory.
- Malhotra C., Bilger M., Liu J., Finkelstein E. Barriers to Breast and Cervical Cancer Screening in Singapore a Mixed Methods Analysis. Asian Pac. J. Cancer Prev. 2016;17(8):3887–3895. [PubMed] [Google Scholar]
- Manderson L., Hoban E. Cervical cancer services for Indigenous women: advocacy, community-based research and policy change in Australia. Women Health. 2006;43(4):69–88. doi: 10.1300/J013v43n04_05. [DOI] [PubMed] [Google Scholar]
- Markovic M., Kesic V., Topic L., Matejic B. Barriers to cervical cancer screening: a qualitative study with women in Serbia. Soc. Sci. Med. 2005;61(12):2528–2535. doi: 10.1016/j.socscimed.2005.05.001. [DOI] [PubMed] [Google Scholar]
- McFarland D.M., Gueldner S.M., Mogobe K.D. Integrated Review of Barriers to Cervical Cancer Screening in Sub-Saharan Africa. J. Nurs. Scholarsh. 2016;48(5):490–498. doi: 10.1111/jnu.12232. [DOI] [PubMed] [Google Scholar]
- McMichael C., Kirk M., Manderson L., Hoban E., Potts H. Indigenous women's perceptions of breast cancer diagnosis and treatment in Queensland. Aust. N. Z. J. Public Health. 2000;24(5):515–519. doi: 10.1111/j.1467-842x.2000.tb00502.x. [DOI] [PubMed] [Google Scholar]
- Mutyaba T., Faxelid E., Mirembe F., Weiderpass E. Influences on uptake of reproductive health services in Nsangi community of Uganda and their implications for cervical cancer screening. Reproductive Health. 2007;4(1):1–9. doi: 10.1186/1742-4755-4-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ndejjo R., Mukama T., Kiguli J., Musoke D. Knowledge, facilitators and barriers to cervical cancer screening among women in Uganda: a qualitative study. BMJ Open. 2017;7(6):e016282. doi: 10.1136/bmjopen-2017-016282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nekhlyudov L., Ross-Degnan D., Fletcher S.W. Beliefs and expectations of women under 50 years old regarding screening mammography. J. Gen. Intern. Med. 2003;18(3):182–189. doi: 10.1046/j.1525-1497.2003.20112.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngugi C.W., Boga H., Muigai A.W., Wanzala P., Mbithi J.N. Factors affecting uptake of cervical cancer early detection measures among women in Thika, Kenya. Health Care Women Int. 2012;33(7):595–613. doi: 10.1080/07399332.2011.646367. [DOI] [PubMed] [Google Scholar]
- Nolan J., Renderos T.B., Hynson J., Dai X., Chow W., Christie A., Mangione T.W. Barriers to cervical cancer screening and follow-up care among black women in Massachusetts. J. Obstet. Gynecol. Neonatal. Nurs. 2014;43(5):580–588. doi: 10.1111/1552-6909.12488. [DOI] [PubMed] [Google Scholar]
- Nonzee N.J., Ragas D.M., Ha Luu T., Phisuthikul A.M., Tom L., Dong XinQi, Simon M.A. Delays in cancer care among low-income minorities despite access. J. Women's Health. 2015;24(6):506–514. doi: 10.1089/jwh.2014.4998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyblade L., Stockton M., Travasso S., Krishnan S. A qualitative exploration of cervical and breast cancer stigma in Karnataka, India. BMC Women's Health. 2017;17(1):1–15. doi: 10.1186/s12905-017-0407-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onyenwenyi A., Mchunu G. Barriers to cervical cancer screening uptake among rural women in South West Nigeria: A qualitative study. South Afr. J. Obstetr. Gynaecol. 2018;24(1):19–23. [Google Scholar]
- Oscarsson M.G., Wijma B.E., Benzein E.G. ‘I do not need to… I do not want to… I do not give it priority…’–why women choose not to attend cervical cancer screening. Health Expect. 2008;11(1):26–34. doi: 10.1111/j.1369-7625.2007.00478.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Özkan İ., Taylan S. Barriers to women's breast cancer screening behaviors in several countries: A meta-synthesis study. Health Care Women Int. 2021;42(7–9):1013–1043. doi: 10.1080/07399332.2020.1814777. [DOI] [PubMed] [Google Scholar]
- Pagliarin F., Pylkkanen L., Salakari M., Deandrea S. Are women satisfied with their experience with breast cancer screening? Systematic review of the literature. Eur. J. Public Health. 2021;31(1):206–214. doi: 10.1093/eurpub/ckaa202. [DOI] [PubMed] [Google Scholar]
- Parra-Casado L., Mosquera P.A., Vives-Cases C., San S.M. Socioeconomic inequalities in the use of healthcare services: Comparison between the Roma and general populations in Spain. Int. J. Environ. Res. Public Health. 2018;15(1):121. doi: 10.3390/ijerph15010121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelcastre-Villafuerte B.E., Tirado-Gómez L.L., Mohar-Betancourt A., López-Cervantes M. Cervical cancer: a qualitative study on subjectivity, family, gender and health services. Reproductive Health. 2007;4(1):1–10. doi: 10.1186/1742-4755-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pimple S., Mishra G., Shastri S. Global strategies for cervical cancer prevention. Curr. Opin. Obstet. Gynecol. 2016;28(1):4–10. doi: 10.1097/GCO.0000000000000241. [DOI] [PubMed] [Google Scholar]
- Püschel K., Thompson B., Coronado G., Gonzalez K., Rain C., Rivera S. ‘If I feel something wrong, then I will get a mammogram’: understanding barriers and facilitators for mammography screening among Chilean women. Fam. Pract. 2010;27(1):85–92. doi: 10.1093/fampra/cmp080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasul V., Cheraghi M., Moqadam Z.B. Influencing factors on cervical cancer screening from the Kurdish women’s perspective: A qualitative study. J. Med. Life. 2015 [PMC free article] [PubMed] [Google Scholar]
- Rim S.H., Allaire B.T., Ekwueme D.U., Miller J.W., Subramanian S., Hall I.J., Hoerger T.J. Cost-effectiveness of breast cancer screening in the National Breast and Cervical Cancer Early Detection Program. Cancer Causes Control. 2019;30(8):819–826. doi: 10.1007/s10552-019-01178-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabih W.K., Taher J.A., El Jabari C., Hajat C., Adib S.M., Harrison O. Barriers to breast cancer screening and treatment among women in Emirate of Abu Dhabi. Ethn. Dis. 2012;22(2):148–154. [PubMed] [Google Scholar]
- Safizadeh H., Hafezpour S., Shahrbabaki P.M. Health damaged context: Barriers to breast cancer screening from viewpoint of Iranian health volunteers. Asian Pacif. J. Cancer Prevent.: APJCP. 2018;19(7):1941. doi: 10.22034/APJCP.2018.19.7.1941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarti S., Espinola S.R. Health inequalities in Argentina and Italy: A comparative analysis of the relation between socio-economic and perceived health conditions. Res. Social Stratification Mobility. 2018;55:89–98. [Google Scholar]
- Savabi-Esfahani M., Taleghani F., Tabatabaeian M., Noroozi M., Lynge E. A qualitative exploration of personality factors in breast cancer screening behavior. Social Behav. Personality. 2018;46(1):91–97. [Google Scholar]
- Schueler K.M., Chu P.W., Smith-Bindman R. Factors associated with mammography utilization: a systematic quantitative review of the literature. J. Women's Health. 2008;17(9):1477–1498. doi: 10.1089/jwh.2007.0603. [DOI] [PubMed] [Google Scholar]
- Shaw T., Ishak D., Lie D., Menon S., Courtney E., Li S.-T., Ngeow J. The influence of Malay cultural beliefs on breast cancer screening and genetic testing: a focus group study. Psycho-Oncology. 2018;27(12):2855–2861. doi: 10.1002/pon.4902. [DOI] [PubMed] [Google Scholar]
- Shirzadi S., Allahverdipour H., Sharma M., Hasankhani H. Perceived barriers to mammography adoption among women in Iran: a qualitative study. Korean J. Family Med. 2020;41(1):20–27. doi: 10.4082/kjfm.18.0054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siu A.L. on behalf of the USPSTF. Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann. Intern. Med. 2016;164(4):279–296. doi: 10.7326/M15-2886. [DOI] [PubMed] [Google Scholar]
- Teng F.F., Mitchell S.M., Sekikubo M., Biryabarema C., Byamugisha J.K., Steinberg M., Money D.M., Ogilvie G.S. Understanding the role of embarrassment in gynaecological screening: a qualitative study from the ASPIRE cervical cancer screening project in Uganda. BMJ Open. 2014;4(4):e004783. doi: 10.1136/bmjopen-2014-004783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teo C.H., Ng C.J., Booth A., White A. Barriers and facilitators to health screening in men: A systematic review. Soc. Sci. Med. 2016;165:168–176. doi: 10.1016/j.socscimed.2016.07.023. [DOI] [PubMed] [Google Scholar]
- Tessaro I., Eng E., Smith J. Breast cancer screening in older African-American women: qualitative research findings. Am. J. Health Promotion. 1994;8(4):286–293. doi: 10.4278/0890-1171-8.4.286. [DOI] [PubMed] [Google Scholar]
- Thomas E., Escandón S., Lamyian M., Ahmadi F., Setoode S.M., Golkho S. Exploring Iranian Women's Perceptions regarding Control and Prevention of Breast Cancer. Qualitative Rep. 2011;16(5):1214–1229. [Google Scholar]
- Trigoni M., Griffiths F., Tsiftsis D., Koumantakis E., Green E., Lionis C. Mammography screening: views from women and primary care physicians in Crete. BMC Women's Health. 2008;8(1):1–12. doi: 10.1186/1472-6874-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tweed E., Allardice G., McLoone P., Morrison D. Socio-economic inequalities in the incidence of four common cancers: a population-based registry study. Public Health. 2018;154:1–10. doi: 10.1016/j.puhe.2017.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urrutia M.-T., Araya A., Jaque M.-F. Why do Chilean women choose to have or not have Pap tests? J. Obstet. Gynecol. Neonatal. Nurs. 2017;46(1):e3–e12. doi: 10.1016/j.jogn.2016.09.002. [DOI] [PubMed] [Google Scholar]
- William M., Kuffour G., Ekuadzi E., Yeboah M., ElDuah M., Tuffour P. Assessment of psychological barriers to cervical cancer screening among women in Kumasi, Ghana using a mixed methods approach. Afr. Health Sci. 2013;13(4):1054–1061. doi: 10.4314/ahs.v13i4.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong L., Wong Y., Low W., Khoo E., Shuib R. Cervical cancer screening attitudes and beliefs of Malaysian women who have never had a pap smear: a qualitative study. Int. J. Behav. Med. 2008;15(4):289–292. doi: 10.1080/10705500802365490. [DOI] [PubMed] [Google Scholar]
- World Health Organization. WHO regional offices. https://www.who.int/about/who-we-are/regional-offices. Published 2021. Accessed.
- Yang H., Li S.-P., Chen Q., Morgan C. Barriers to cervical cancer screening among rural women in eastern China: a qualitative study. BMJ Open. 2019;9(3):e026413. doi: 10.1136/bmjopen-2018-026413. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.