Highlights
-
•
Early childhood vaccination coverage is low in rural areas of the United States.
-
•
Reminder-recall & positive family-provider relationships facilitate vaccine uptake.
-
•
Parental hesitancy is a barrier to early childhood vaccination in the rural U.S.
-
•
Vaccine referrals & distance to providers are also rural-specific barriers.
-
•
To increase vaccine coverage, interventions across rural populations are needed.
Keywords: Early childhood immunizations, Rural health, Preventive health, Systematic review, PRISMA
Abstract
Early childhood vaccination rates are lower in rural areas of the U.S. compared with suburban and urban areas. Our aim was to identify barriers to and facilitators of early childhood immunization in rural U.S. communities. We completed a systematic review of original research conducted in the U.S. between January 1, 2000-July 25, 2021. We searched PubMed, Cumulative Index for Nursing and Allied Health Literature, and Web of Science. We included studies that examined barriers to and facilitators of routine immunizations in children <36 months old in rural areas. Following the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines, we reported studies’ methodologies and targeted populations, definitions of rurality, and common themes across studies that reflected barriers to or facilitators of vaccination. Ultimately, 17 papers met inclusion criteria for review. The majority of studies (10/17) were conducted within one U.S. state, and the same number (10/17) were conducted prior to 2005. Facilitators of vaccine uptake in rural communities identified across studies included reminder/recall systems and parents’ relationships with providers. Parental hesitancy, negative clinic experiences, referrals outside of primary care settings, and distance to providers were identified as barriers to vaccination in rural settings. This review revealed a limited scope of evidence on barriers to and facilitators of early childhood immunization in rural communities. More investigations of the causes of low vaccine coverage and the effectiveness of interventions for increasing vaccine uptake are urgently needed in rural pediatric populations to address persistent rural–urban immunization disparities.
1. Introduction
Vaccinations have been an outstanding public health achievement, preventing millions of illnesses and deaths (CDC, 2011). The U.S. Advisory Committee on Immunization Practices (ACIP) recommends children receive routine vaccinations at ages 0, 2, 4, 6, 12–15, and 15–18 months. The ten different vaccine series that are recommended are: hepatitis B (HepB), rotavirus, diphtheria-tetanus-acellular pertussis (DTaP), Haemophilus influenzae type b (Hib), pneumococcal conjugate vaccine (PCV), inactivated poliovirus, measles-mumps-rubella (MMR), varicella (VAR), hepatitis A (HepA), and influenza (CDC, 2022). The Centers for Disease Control and Prevention (CDC) tracks completion of these vaccine series by the child’s second birthday. Overall, vaccine coverage at state and national levels is high compared to historical averages (Hill et al., 2020, Whitney et al., 2014). However, recent studies have shown that over half of U.S. children under 2 years old fall behind in receiving recommended vaccines (Freeman et al., 2022, Kurosky et al., 2016). Also, high vaccine coverage at state and national levels mask low vaccine coverage at smaller community levels. Falling behind on vaccinations and living in communities with low vaccine coverage are both risk factors for vaccine-preventable diseases (Gahr et al., 2014, Glanz et al., 2013, Kurosky et al., 2016, Zucker et al., 2020).
The CDC conducts the National Immunization Survey-Child (NIS-Child) annually to assess early childhood immunization coverage among children 19–35 months old at national and state levels (CDC, 2018). The NIS-Child survey reports national vaccination rates of children using classifications established by the U.S. Census Bureau as living in a metropolitan statistical area (MSA) principal city (population >50,000 and living in a core metropolitan city), an MSA non-principal city (population >50,000 and not living in the core metropolitan city), and non-MSAs (population <50,000), which are often used to coarsely represent urban, suburban, and rural stratifications, respectively ( Hart et al., 2005, Hill et al., 2020, Ingram and Franco, 2012). According to NIS-Child data, by 2 years old, children born in 2016 and 2017 who lived in non-MSA areas of the U.S. had lower vaccination rates compared to children living in an MSA (Hill et al., 2020). For example, children living in non-MSAs were 6.3 and 9.7 percentage points behind children living in MSA, principal cities for rotavirus and influenza vaccine series completion, respectively. Also, 2.0% of children living in non-MSAs were completely unvaccinated (i.e., had received no vaccines), as compared with 1.1% among both children living in MSA, principal cities and MSA, non-principal cities (Hill et al., 2020).
These rural–urban disparities exist despite the federal Vaccines for Children (VFC) program, which ensures free vaccines to uninsured and underinsured children under 18 years old in the U.S. Following the VFC program’s implementation in 1994, immunization rates increased substantially nationwide (CDC, 2016, Schwartz and Colgrove, 2020, Whitney et al., 2014); however, rates in rural areas have continued to fall behind rates in urban areas (Hill et al., 2020). Prior research has proposed explanations for childhood undervaccination (i.e., late in receipt or failure to complete recommended early childhood vaccination series). One barrier to timely immunization is parents’ hesitancy to vaccinate their children (Bianco et al., 2019, World Health Organization, 2014), due to reasons such as concerns regarding vaccine safety or beliefs that vaccines are not necessary (Lannon et al., 1995, Mical et al., 2021, Taylor et al., 2002,). However, structural barriers to preventive care services, including difficulties accessing clinics, transportation challenges, and primary care provider shortages, may also present challenges to timely vaccination in rural pediatric populations (Grant et al., 2014, Lannon et al., 1995, Shipman et al., 2011, Tierney et al., 2003, Weigel et al., 2016).
Additionally, research investigating rurality requires recognition of its heterogeneity which encompasses a variety of population sizes, access to resources, socio-economics, and cultures (Bennett et al., 2019). It is well established in the U.S. that rural communities experience poorer health outcomes, including pediatric outcomes such as lower use of preventive health services, higher rates of obesity, greater risk of death by unintentional injury (Probst et al., 2018), and lower vaccination rates (Zhai et al., 2020). Studies have demonstrated persistent disparities in rural settings compared to urban areas in general health care access (Douthit et al., 2015) and mortality (Moy et al., 2017) indicating unique challenges to accessing medical care and preventive health services in rural communities. Although studies have demonstrated rural versus urban differences in variation in immunization delivery (Fagnan et al., 2011, O'Leary et al., 2015), explanations specific to why rural children are undervaccinated remains understudied.
To target interventions for increasing early childhood immunizations rates in rural communities, there is a need to identify the barriers that exist for parents of children living in rural areas, and also facilitators of vaccination in these communities. The objective of this study was to identify barriers to and facilitators of early childhood immunization uptake in rural areas within the U.S. Therefore, we conducted a systematic review to synthesize the current body of research focused on early childhood immunizations within rural settings.
2. Methods
We used the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines for paper selection (Page et al., 2021).
2.1. Information sources and search strategy
Two study team members (ANA, JT) independently and systematically searched PubMed, Cumulative Index for Nursing and Allied Health Literature (CINAHL), and Web of Science using specific terms and phrases (Table 1). Except for the date of publication, we did not use additional filters for any of the 3 databases. We started the review process with the PubMed database and focused on phrases that included ‘immunization’ or ‘vaccine’. In our CINAHL search, we utilized additional variations of the term ‘rural’ (e.g., RUCA) to complement its more broadly defined search tactics (Table 1). Our search in the final database, Web of Science, verified that we did not miss a subsection of papers.
Table 1.
Search criteria utilized in the literature search, presented by database.
| Database | Search Criteria |
|---|---|
| PubMeda | (((((((((“rural*”[tw] AND “vaccin*”[MeSH] AND “hesitan*”[tw])) OR ((“rural*”[tw] AND “vaccin*”[MESH] AND (“barrier”[tw] OR “barrier s”[tw] OR “barriers”[tw])))) OR ((“parent*”[tw] AND “hesitan*”[tw] AND “vaccin*”[MESH] AND “rural*”[tw]))) OR ((“missed opportunities”[tw] AND (“rural*”[tw] AND “vaccin*”[MESH])))) OR ((“rural*”[tw] AND (“childhood”[tw] OR “childhoods”[tw]) AND “immuniz*”[MESH] AND (“barrier”[tw] OR “barrier s”[tw] OR “barriers”[tw])))) OR ((“rural*”[tw] AND (“primary health care”[MeSH Terms] OR (“primary”[tw] AND “health”[MESH] AND “care”[tw]) OR “primary health care”[MESH] OR (“primary”[tw] AND “care”[tw]) OR “primary care”[tw]) AND (“vaccin*”[MESH] AND (“barrier”[tw] OR “barrier s”[tw] OR “barriers”[tw]))))) OR (((“immuniz*”[MESH] AND “rural*”[tw]) AND ((“primary health care”[MeSH Terms] OR (“primary”[tw] AND “health”[MESH] AND “care”[tw]) OR “primary health care”[MESH] OR (“primary”[tw] AND “care”[tw]) OR “primary care”[tw]))))) OR ((“vaccin*”[MESH] AND “hesitan*”[tw] AND “rural*”[tw] AND “communit*”[tw]))) AND ((“2000/01/01″[PDAT]: ”2021/07/25″[PDAT])) |
| Cumulative Index for Nursing and Allied Health Literature (CINAHL) |
((rural OR “RUCA” OR nonmetropolitan OR non-metropolitan OR frontier OR “geographically isolated”)) AND ((vaccin* OR immunization* OR “childhood immunization*”)) AND ((barrier* OR hesitancy OR “missed opportunit*” OR refusal OR acceptan* OR confiden* OR “immunization* coverage” OR “vaccin* coverage” OR “immunization* status” OR “vaccin* status”))) AND DT 20000101-20210725 |
| Web of Science | ((TS=((childhood vaccin* hesitanc*) OR (childhood vaccin* refus*) OR (childhood vaccin* accept*))) AND TS=(rural*)) AND DOP=(2000-01-01/2021-07-25) |
We utilized a ‘text word’ (tw) search for ‘rural’ which tells PubMed to look for ‘rural’ in titles, abstracts, and MESH headings. However, if a rural-specific study excluded the term ‘rural’ in the abstract or title, it may not have been identified in PubMed search results. Therefore, in our CINAHL database search we included multiple rurality phrases and we checked references in each selected article for additional papers.
2.2. Eligibility criteria and selection process
The selected papers described original research completed in the U.S. and published between January 1, 2000-July 25, 2021. Additional inclusion criteria included 1) at least one research aim/objective that examined barriers to or facilitators of vaccination in a rural area, and 2) the investigation focused on the uptake of recommended routine immunizations to children <36 months old. We focused on this age group since CDC monitors early childhood immunization coverage in this age category (CDC, 2018). Of note, since 2000, there have been minimal changes to the vaccines recommended to children. Changes include the addition of the rotavirus vaccine in 2006 and expanded recommendations for universal administration of the Hepatitis A vaccine to young children ≥1 year in 2006 (Advisory Committee on Immunization Practices ACIP et al., 2006, Parashar et al., 2022).
We excluded grey literature, case reports, and reviews from the analysis. Additionally, studies were excluded if they investigated barriers to immunization but only utilized urbanicity or rurality in the analysis and not as a focus or objective of these studies (i.e., criteria #1) (Megel et al., 2002, O'Leary et al., 2018, Smith et al., 2009).
After each team member (ANA, JT) made their selections independently, they collectively assessed each paper and selected the final papers for review. Four papers required a third researcher (SRN) to make the final decision to include or exclude.
2.3. Data extraction
For each study, team members (ANA, JT) extracted the following information: location, study population, methodology, immunization focus, and sample size. We extracted selected results and analyzed all selected papers for consistent themes that fit within our objective for the review. Once the main results were identified from each study, team members (ANA, SRN) independently compiled results into broad themes that demonstrated either barriers to or facilitators of early childhood immunization uptake. The team discussed and refined themes until all authors reached agreement.
3. Results
3.1. Study selection
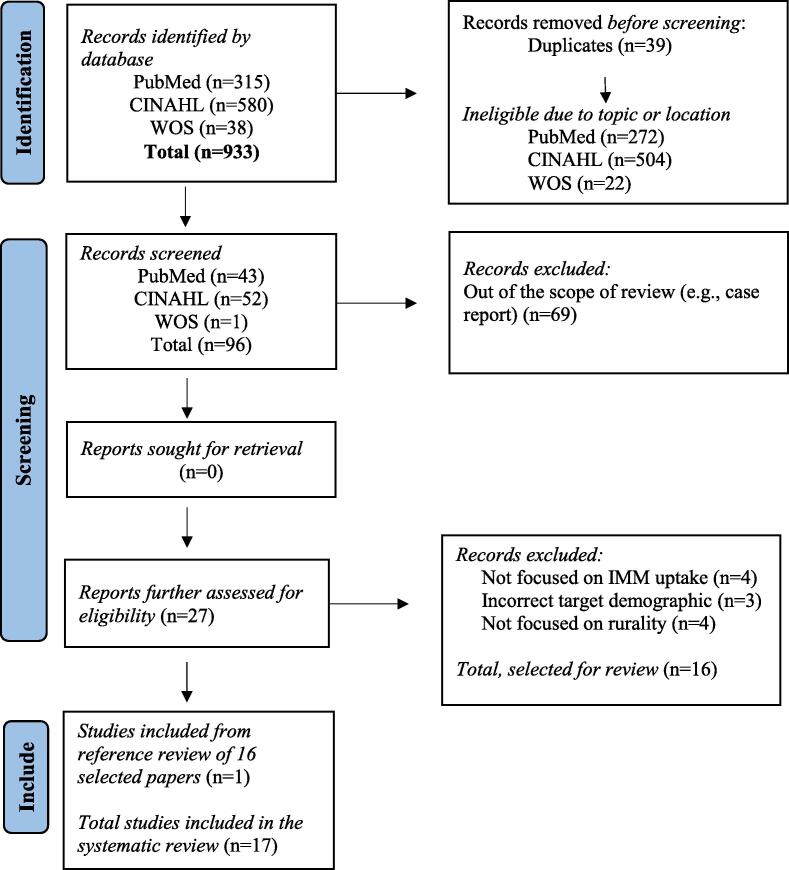
The initial search yielded 933 papers (315 PubMed, 580 CINAHL, 38 Web of Science). After removal of duplicates, we were left with 894 papers. Then, based on title and abstract review, we removed articles that were outside of the U.S. or unrelated to childhood immunizations (n = 798). For the remaining articles (n = 96), we screened methodology, and eliminated articles that were out of the scope of the review (e.g., case report) (n = 69). The remaining articles were read in their entirety to assess eligibility (n = 27). Of those, we eliminated studies that 1) did not focus on immunization uptake (n = 4), 2) the target demographic included a broad age range (e.g., 2–16 years) instead of focusing on children under 36 months of age (n = 3), and 3) if results from urban, suburban, and rural were grouped together and generalized without a specific focus on rurality (n = 4). Through the selection process, sixteen papers were selected for review (Albright et al., 2014, Bardenheier et al., 2004, Daley et al., 2005, Deutchman et al., 2000, Fagnan et al., 2011, Glazner et al., 2001, Hicks et al., 2007, Kempe et al., 2001, Kettunen et al., 2017, Mical et al., 2021, Newcomer et al., 2021, Renfrew et al., 2001, Rosenthal et al., 2004, Saville et al., 2014, Thomas et al., 2004, Wilson, 2000). One team member (ANA) checked references in each selected article for any potential papers by scanning for relevant titles (e.g., rural, vaccine) published in 2000–2021. We found one additional study to include (Stokley et al., 2001), therefore, the total number of articles in the review is 17 (Fig. 1).
Fig. 1.
PRISMA 2020 flow diagram for systematic review (Page et al., 2021).
3.2. Study characteristics
Study methodologies were identified as qualitative interviews (Wilson, 2000), mixed-methods (Rosenthal et al., 2004, Thomas et al., 2004), immunization registry analyses (Kempe et al., 2001, Newcomer et al., 2021, Renfrew et al., 2001, Stokley et al., 2001), economic analysis (Glazner et al., 2001), use of questionnaires/surveys (Bardenheier et al., 2004, Daley et al., 2005, Deutchman et al., 2000, Fagnan et al., 2011, Kettunen et al., 2017, Saville et al., 2014), or an intervention-based study (Albright et al., 2014, Hicks et al., 2007, Mical et al., 2021). Ten studies were published in 2005 or earlier (Bardenheier et al., 2004, Daley et al., 2005, Deutchman et al., 2000, Glazner et al., 2001, Kempe et al., 2001, Renfrew et al., 2001, Rosenthal et al., 2004, Thomas et al., 2004, Wilson, 2000, Stokley et al., 2001), and seven were published in 2006–2021 (Albright et al., 2014, Fagnan et al., 2011, Hicks et al., 2007, Kettunen et al., 2017, Mical et al., 2021, Newcomer et al., 2021, Saville et al., 2014). The majority of study locations were in Colorado (Albright et al., 2014, Bardenheier et al., 2004, Daley et al., 2005, Deutchman et al., 2000, Glazner et al., 2001, Hicks et al., 2007, Kempe et al., 2001, Renfrew et al., 2001, Rosenthal et al., 2004, Saville et al., 2014). Across the studies, data were collected either from parents or caregivers of children (Bardenheier et al., 2004, Hicks et al., 2007, Kettunen et al., 2017, Mical et al., 2021, Rosenthal et al., 2004, Saville et al., 2014, Thomas et al., 2004, Wilson, 2000), health care providers (Albright et al., 2014, Daley et al., 2005, Deutchman et al., 2000, Fagnan et al., 2011, Glazner et al., 2001), or an immunization registry (Kempe et al., 2001, Newcomer et al., 2021, Renfrew et al., 2001, Stokley et al., 2001). All papers in our review focused on immunizations for children 0–35 months of age, but a few also examined immunizations through 4 to 5 years of age (Daley et al., 2005, Mical et al., 2021, Wilson, 2000).
Although the majority of papers focused on routine vaccination, there was variation in immunization focus. Eleven studies explicitly stated the immunizations of interest (Bardenheier et al., 2004, Daley et al., 2005, Fagnan et al., 2011, Glazner et al., 2001, Hicks et al., 2007, Kempe et al., 2001, Newcomer et al., 2021, Renfrew et al., 2001, Rosenthal et al., 2004, Thomas et al., 2004, Stokley et al., 2001) while other papers referred more generally to recommendations for routine early childhood immunizations (Albright et al., 2014, Deutchman et al., 2000, Kettunen et al., 2017, Mical et al., 2021, Saville et al., 2014, Wilson, 2000) (Table 2).
Table 2.
Extracted data from each selected paper: first author/year/citation number, location, study population, methodology, immunization focus, and sample size.
| First Author (year) | Location | Study Population | Methodology | Immunization focus | Sample size | |
|---|---|---|---|---|---|---|
| 1 | Albright (2014) | 14 counties in Colorado (4 rural, 10 non-rural) | HCP | Mixed methods study utilizing Colorado IIS for reminder/recall. Conducted HCP and staff interviews and surveys about provider experiences, attitudes, and current utility of reminder/recall systems. | IMM not specified Age: 19–35 months |
253 surveys; 82 interviews |
| 2 | Bardenheier (2004) | Manhattan, Detroit, San Diego, and rural Colorado (made up of 4 counties) | Parents/ caregivers |
Cross-sectional household surveys gathered demographic information and parental knowledge of and experiences with early childhood immunization. | DTP/DTaP, Polio, Hib, HepB Age: 3 months |
847(New York)771 (Detroit)843 (San Diego)1091 (Colorado) |
| 3 | Daley (2005) | 2 large rural areas in Colorado & Denver, Colorado for urban | HCP | Survey to assess vaccine recommendations providers used during vaccine shortage and when supply was adequate. | PCV7 Age: 0–5 years*, focused on <2 years |
32 (rural)52 (urban pediatricians)129 (urban family medicine) |
| 4 | Deutchman (2000) | Colorado (across 52 rural counties) | HCP | Mailed questionnaire to HCPs about their perception of immunization challenges in their community and current vaccine practices at their facility. | Early childhood IMM Age: <2years |
158 |
| 5 | Fagnan (2011) | Rural Oregon | HCP | Mailed survey to HCPs about immunization practices, barriers to immunization, and their opinions and perceptions of early childhood immunizations. | DTaP, Polio, MMR, Hib, HepB, PCV, VAR, Influenza, HepA Age: <36 months |
407 |
| 6 | Glazner (2001) | Rural Colorado | HCP | Quantitative study. Cost assessment of reimbursement rates. Selected clinics tracked time spent on vaccine-related tasks over a month. Data were assessed from multiple private practices, health departments, and FQHCs. | DTaP, MMR, Hib, HepB, Polio, VAR, DTaP-Hib Age: <36 months |
13 clinics (6 private practice, 4 health departments, 3 FQHC) |
| 7 |
Hicks (2007) |
Rural northeast Colorado | Parents/ caregivers |
Quantitative study of reminder-recall in a Family Health Center. The intervention included reminder cards in preferred language and posters in exam rooms. Vaccines rates were quantified pre and post intervention among Latinx patients. | DTaP, Polio, Hib, HepB, MMR, VAR Age: 13–35 months |
240 baseline, 263 post-intervention |
| 8 | Kempe (2001) | Rural south-central Colorado (Alamosa and Rio Grande Counties) | Data source: Registry Study population: Children |
Quantified immunization rates after implementation of a regional immunization registry. | DTP, Polio, Hib, HepB, MMR Age: 3–35 months |
876 |
| 9 | Kettunen (2017) | Rural Ashtabula County in Ohio | Parents/ caregivers |
Survey sent to Amish parents to collect information about parental experience with and knowledge of early childhood immunizations. | * | 84 |
| 10 | Mical (2021) | Not specified, rural focused | Parents/ caregivers |
Qualitative improvement study that evaluated provider-level interventions to decrease parental hesitancy and increase vaccine uptake in a rural clinic setting. Participants were provided a pre and post intervention survey to determine a level of vaccine hesitancy. | All recommended childhood vaccinations, excluding influenza Age: 2 months-5 years |
70 |
| 11 | Newcomer (2021) | Analysis of children’s vaccination status throughout Montana, rural and non-rural communities included | Data source: Registry Study population: Children |
Quantitative study that analyzed data from state immunization registry to investigate vaccine timeliness and under-vaccination patterns. | Combined 7-vaccine series (DTaP, Polio, MMR, HepB, Hib, VAR, PCV) Age: 0–24 months |
31,422 |
| 12 | Renfrew (2001) | 5 sites in rural Northeast Colorado and 5 sites in south-central Colorado (San Luis Valley) | Data source: Registry Study population: Children |
Quantified changes in immunization rates at primary care sites based using chart reviews to update immunization status at primary care facilities. Used to assess potential effects of a regional immunization registry. | DTP, HepB, Hib, Polio, MMR Age: 12–18 months, 24–30 months |
1533 |
| 13 | Rosenthal (2004) | Urban sites: Detroit, New York, San Diego Rural site: rural Colorado |
Parents/ caregivers |
Interviews collected data about parental perception of early childhood immunizations, their use of immunization services, participation in federally funded programs, resource availability (e.g., transportation), and demographic information. A quantitative analysis assessed relationships of child immunization status and parental/family characteristics collected during the interview. | DTP, Polio, MMR, Hib, HepB Age: 12–35 months |
502(Detroit),520 (New York) 555(San Diego) 713 (Colorado) |
| 14 | Saville (2014) | 7 counties in Colorado, urban and rural counties |
Parents/ caregivers |
Mailed survey about parents’ reminder/recall preferences. | Early childhood IMM recommended by ACIP (influenza excluded) Age: 19–35 months |
178(rural) & 156(urban) |
| 15 | Stokley (2001) | U.S., urban and rural | Data source: Registry Study population: Children |
Quantitative study that analyzed National Immunization Survey-Child data to compare suburban, urban, and rural vaccine coverage. | DTP, Polio, MCV, Hib, HepB, VAR Age: 19–35 months |
25,521 |
| 16 | Thomas (2004) | Semi-rural community in Bakersfield, California | Parents/ caregivers |
Door-to-door surveys and follow-up focus groups. Participants were asked about barriers, perceptions, and attitudes about their experiences with early childhood immunizations. Mixed-methods study. | Polio, DTP, Hib, HepB, MMR, VAR Age: <3years |
18(focus group) & 207 (surveys) |
| 17 | Wilson (2000) | Rural Missouri | Parents/caregivers | Qualitative study using phone or in-person interviews with parents which described experiences with child IMM and assessed parental knowledge. | IMM recommended to children under 4 years by CDC Age: 2 months-4 years |
12 |
Abbreviations (non-vaccines): Health Care Provider (HCP); Immunization (IMM); Immunization Information System (IIS); Advisory Committee on Immunization Practices (ACIP); Parent/caregiver (P/CG); Federally Qualified Health Center (FQHC). Abbreviations (vaccines): Diphtheria, Tetanus, Pertussis (or acellular Pertussis) (DTP, DTaP); Measles, Mumps, Rubella (MMR); Varicella (VAR); Hepatitis B (HepB); Hepatitis A (HepA); Haemophilus influenzae type b (Hib); Meningococcal conjugate vaccine (MCV); Poliovirus (Polio); Pneumococcal conjugate vaccine (PCV7).
*Kettunen et al. (2017) did not specify immunizations. They refer to childhood immunizations and mention pertussis, rubella, measles, varicella, and Hib and the recommended vaccine schedule for early childhood immunizations.
3.3. Study themes
We identified five themes across studies that represented barriers to or facilitators of early childhood immunization uptake: relationships with clinic staff and providers, immunization tracking and reminder/recall, parental vaccine hesitancy, accessing health services, and other immunization challenges in rural areas (Table 3). We also identified variation in the way rural was defined across studies, including whether it was explicitly defined at all. Five studies defined rural based on selected study locations for the Colorado Rural Immunization Services Project (CRISP) (Colorado Children’s Immunization Coalition, 2013), a CDC funded project (Daley et al., 2005, Deutchman et al., 2000, Glazner et al., 2001, Kempe et al., 2001, Renfrew et al., 2001). Other studies defined rural as more than 10 miles from a city with a population greater than 30,000 (Fagnan et al., 2011), used metropolitan and non-metropolitan statistical area definitions by the U.S. Census Bureau (Newcomer et al., 2021, U.S. Census Bureau, 2020), considered rural an area outside of an MSA (Rosenthal et al., 2004), used the Office of Management and Budget (OMB) parameter classification (Stokley et al., 2001), or identified rural as <10,000 people (Wilson, 2000). Seven papers did not provide their methodology for defining rurality in their study (Albright et al., 2014, Bardenheier et al., 2004, Hicks et al., 2007, Kettunen et al., 2017, Mical et al., 2021, Saville et al., 2014, Thomas et al., 2004) (Table 4).
Table 3.
Selected results and associated themes that demonstrate the barriers to and facilitators of early childhood immunization in rural areas from papers selected for the current systematic review.
| First Author (year) | Selected Results | Associated Theme(s) | |
|---|---|---|---|
| 1 | Albright et al. (2014) | Compared to urban HCPs, rural HCPs were 1) more supportive of collaboration between health departments and clinics, 2) conducted more reminder/recalls and 3) reported more of a preference towards health department involvement in reminder/recall for early childhood immunizations. Overall, rural providers’ willingness to engage in a collaborative relationship with health departments was considered a facilitator to centralized reminder/recall systems and ultimately vaccine uptake for early childhood immunizations. | Immunization tracking and reminder/recall systems |
| 2 | Bardenheier et al. (2004) | In rural Colorado, facilitators of vaccination included being the first-born child, living above poverty level, or having private insurance. Other urban areas investigated in this study had evidence of different risk factors for under immunization, such as having unmarried parents. | Other immunization challenges in rural areas |
| 3 | Daley et al. (2005) | Overall, PCV7 was recommended via ACIP guidelines for high-risk children during shortages. PCV7 was recommended less often by urban family medicine providers versus rural providers or urban pediatric providers. Additionally, low volume could be a barrier to higher immunization rates. For example, when clinics immunized <50 children per week, PCV7 vaccine rates were lower than in higher volume clinics. | Other immunization challenges in rural areas |
| 4 | Deutchman et al. (2000) | A potential barrier to vaccination in rural settings was the amount of immunization referrals, which were common. Other barriers included lack of screening and tracking systems for patients that were due or overdue for vaccinations. Providers felt that parent education, low reimbursement, record scatter, and only vaccinating at well-child visits were barriers to vaccine uptake in rural communities. | Immunization tracking and reminder/recall systems, Parental vaccine hesitancy, Health services, Other immunization challenges in rural areas |
| 5 | Fagnan et al. (2011) | HCPs in rural areas commonly referred children for immunizations outside of their primary care clinic, and 20% reported referring all children for vaccination. While pediatricians were more likely than family doctors to provide immunizations, a barrier to early childhood immunization was the lack of pediatricians in rural communities. Referral was necessary because of low vaccine reimbursement rates, inadequate vaccine storage, and inability to deal with immunization record keeping. | Immunization tracking and reminder/recall systems, Health services, Other immunization challenges in rural areas |
| 6 | Glazner et al. (2001) | Low reimbursement rates could potentially increase barriers to childhood immunizations. Low reimbursement was one reason for private rural providers referring patients to the health department for vaccinations. However, at least in Colorado, while public providers had reduced costs, their reimbursement for immunization services was lower than for private providers. | Other immunization challenges in rural areas |
| 7 | Hicks et al. (2007) | Sending reminder cards to parents in their preferred language increased immunization rates from ∼61% to ∼73%. Facilitators to vaccine uptake were living <10 miles from a medical facility with immunization services and having insurance. | Immunization tracking and reminder/recall systems, Other immunization challenges in rural areas |
| 8 | Kempe et al. (2001) | After investigation of dispersed immunization records, the study found over 33% of children had received immunizations outside of their primary care clinic. When data were combined from external sources to make a regional registry, clinics’ immunizations rates increased up to 25%. The highest increase was due to addition of records from public health clinics. Therefore, lack of immunization registry and record scatter were barriers to adequate tracking of early childhood immunizations. | Other immunization challenges in rural areas |
| 9 | Kettunen et al. (2017) | Most parents in the rural Amish community in Ashtabula County accepted at least some of the immunizations recommended for their child, and almost 60% accepted all immunizations. Facilitators of vaccine adherence were knowledge, and positive beliefs and opinions about vaccines. Most barriers to uptake were concerns about vaccine safety, risk of adverse events, and questions about their child’s immune system. Neither religion nor knowledge were barriers to vaccine uptake. Parents in this rural area agreed that immunizations were beneficial, but tried to manage risk of adverse events by altering the vaccine schedule. | Parental vaccine hesitancy |
| 10 | Mical et al. (2021) | Provider-level intervention strategies such as use of presumptive language and motivational interviewing with vaccine hesitant parents were considered successful. Almost 82% of parents that were considered hesitant prior to the healthcare visit were non-hesitant after implementation of provider-patient discussion strategies. Barriers to early childhood immunizations were parental concerns about vaccine ingredients and the safety of giving multiple injections at one visit. | Relationships with clinic staff and providers, Parental vaccine hesitancy |
| 11 | Newcomer et al. (2021) | In Montana, most children received immunizations in a rural area, however, rural immunization rates were lower compared to urban rates. Compared to urban communities, rural children were more likely to be undervaccinated. The patterns of undervaccination were indicative not only of structural barriers (∼19%) but also parental vaccine hesitancy (∼19%). | Parental vaccine hesitancy |
| 12 | Renfrew et al. (2001) | While dispersed health information from use of private and public immunization services in rural areas was a potential barrier to early childhood immunization, compiling patient charts to create a registry was a facilitator to immunization. Indeed, records from facilities outside of the primary care provider resulted in higher immunization rates once records were combined, which demonstrated the importance of an immunization registry in facilitating vaccine uptake in rural communities. | Other immunization challenges in rural areas |
| 13 | Rosenthal et al. (2004) | Rural early childhood immunization coverage was better than one of the urban study areas, Detroit, but lower than New York or San Diego. Barriers to rural coverage were immunizations received from private providers only versus from a mix (i.e., private and public facilities). Across all study sites, presence of an immunization card and being up-to-date at 3 months old were facilitators of vaccine uptake at 19–35 months. | Immunization tracking and reminder/recall systems |
| 14 | Saville et al. (2014) | While urban and rural parents support reminder/recalls for early childhood immunization, a potential facilitator for rural parents would be involvement of the health department in the reminder/recall system for early childhood immunizations. Indeed, rural parents were much more likely to support the health department’s role in the reminder/recall system for their child compared to urban parents. | Immunization tracking and reminder/recall systems |
| 15 | Stokley et al. (2001) | Rural children were administered their early childhood immunization at public facilities more often compared to urban and suburban children. | Other immunization challenges in rural areas |
| 16 | Thomas et al. (2004) | Rural parents were confused about the early childhood immunization schedule and its importance, and reported being dependent on HCPs for vaccine information. Other barriers for parents to vaccine uptake were not vaccinating their child if they were sick and sometimes parents forgot to take their child in for their vaccine. Provider and clinic barriers to early childhood immunization included limited appointment availability, poor scheduling options, difficulty with staff, long wait times, and lack of consistent vaccine messaging with staff and providers. Additionally, parents in rural areas with unreliable or lack of transportation found this to be the greatest barrier to get their child vaccinated. | Relationships with clinic staff and providers, Health services |
| 17 | Wilson (2000) | Barriers to vaccination in rural Missouri included parental vaccine hesitancy (e.g., vaccine ingredients, experts disagree, natural immunity satisfactory), competing factors (e.g., parents are busy, difficult to miss time away from work), and provider or clinic barriers (e.g., confusion about the immunization schedule, wait time, the provider will not vaccinate a sick child). | Relationships with clinic staff and providers, Immunization tracking and reminder/recall systems, Health services, Parental vaccine hesitancy |
Abbreviations: Health care provider (HCP); Pneumococcal conjugate vaccine (PCV7); Advisory Committee on Immunization Practices (ACIP).
TABLE 4.
Definitions of ‘rural’ that were provided from selected studies within the systematic review.
| Rural Definition | First Author (year) |
|---|---|
| Based on rural definition provided by CRISP | Daley et al. (2005)a, Deutchman et al., 2000, Glazner et al., 2001, Kempe et al., 2001, Renfrew et al., 2001 |
| The Office of Rural Health definition, which is “…areas 10 or more miles from population centroid of a population of 30,000 or more”. Also utilized RUCA designations to further delineate areas. | Fagnan et al. (2011) |
| U.S. Census Bureau | Newcomer et al. (2021) |
| An area outside of an MSA. An MSA was defined as a population with at least 100,000 people | Rosenthal et al. (2004) |
| Defined using OMB parameters and rural as non-MSA | Stokley et al. (2001) |
| Population of <10,000 people | Wilson (2000) |
| No explicit definition provided | Albright et al., 2014, Bardenheier et al., 2004b, Hicks et al., 2007, Kettunen et al., 2017, Mical et al., 2021, Saville et al., 2014, Thomas et al., 2004 |
Abbreviations: Colorado Rural Immunization Services Project (CRISP), Rural Urban Commuting Area (RUCA), Metropolitan Statistical Area (MSA), Office of Management and Budget (OMB).
Daley et al. (2005) provided a citation to Kempe et al. (2001) which utilized CRISP.
Bardenheier et al. (2004) utilized health professional shortage areas where distance to provider was greater than 30 min, as a proxy for rurality.
3.3.1. Relationships with clinic staff and providers
In rural communities, the relationship of patients with clinic staff and providers was a facilitator to early childhood immunization uptake and a critical factor for rural parents when deciding whether or not to vaccinate their children. Parents of young children rely on health care personnel to provide accurate immunization information, debunk false vaccine rumors, and help them maneuver the immunization schedule (Wilson, 2000). In another study, the same parents that relied on health care providers to give vaccine information also said providers did not make time for questions; half identified a provider as a source of vaccine information (Thomas et al., 2004). Overall, the way providers interacted, communicated, and supported parents influenced children’s immunization status. In one study of rural parents, when providers used evidence-based tactics (e.g., presumptive language, motivational interviewing) during well-child exams, most parents/caregivers who were initially hesitant about vaccines before the visit were identified as non-hesitant after the visit (Mical et al., 2021).
3.3.2. Immunization tracking and reminder/recall
Another facilitator to early childhood immunization uptake was use of immunization tracking and reminder/recall systems. One study found that in medically underserved areas, possession of an immunization card was associated with higher immunization coverage (Rosenthal et al., 2004). Another study found that rural parents that did not have their child’s vaccine records were less likely to have fully vaccinated children, and only 37% of parents could provide complete documentation of immunizations (Thomas et al., 2004). Furthermore, providers with a system to track patient immunizations consistently recommended immunizations (Fagnan et al., 2011). In a study of primary care providers in Oregon, rural clinics that had systems in place to identify and contact parents of children who were due or overdue for their immunizations (i.e., reminder/recall systems) had higher vaccine uptake compared to clinics without these systems (Fagnan et al., 2011). However, other studies reported that rural immunization providers without a reminder/recall system were concerned it would be expensive, require more staff, or lead to confidentiality concerns (Albright et al., 2014, Deutchman et al., 2000). Several studies reported that rural parents did want reminder/recall systems to help them keep up with the immunization schedule (Saville et al., 2014, Wilson, 2000). Rural parents have reported confusion about childhood immunizations and the importance of the recommended vaccine schedule (Thomas et al., 2004, Wilson, 2000). Sometimes, missed immunizations resulted from not knowing vaccines were due or because the parents forgot vaccines were due (Thomas et al., 2004). In rural Colorado, 50% of physicians claimed to call parents about missed immunizations, but about 65% had no consistent reminder or tracking system (Deutchman et al., 2000). Finally, one study in Colorado found that providers could improve language barriers to immunizations and increase vaccine uptake by simply sending a reminder card in the patient’s preferred language (Hicks et al., 2007).
3.3.3. Parental vaccine hesitancy
In addition to facilitators, we also found evidence of barriers to early childhood vaccination in rural communities. In our review, studies reported that parental vaccine hesitancy manifested in a variety of ways within rural communities. Parents were concerned that their child receiving multiple vaccines at once was unsafe and expressed uncertainty about the necessity of immunizations and potential vaccine contraindications (Deutchman et al., 2000, Mical et al., 2021). Parents living in rural communities also expressed worry about vaccine ingredients (Mical et al., 2021, Wilson, 2000), had questions about vaccine safety (Kettunen et al., 2017), and sometimes needed more information for vaccine buy-in (Mical et al., 2021). Furthermore, parents’ misunderstandings about immunity and vaccines led to negative opinions on immunizations (Wilson, 2000), and parents’ positive beliefs about immunizations were associated with a higher percentage of fully vaccinated children (Bardenheier et al., 2004). In Montana, where most children live in rural areas, the prevalence of young children undervaccinated due to parental hesitancy was similar to the prevalence of children undervaccinated due to other structural barriers to accessing immunization services (Newcomer et al., 2021). Interestingly, even though parents from a rural community in Ohio reported that immunizations were important and had significant benefits, because of the risk of adverse events, parents felt they could help mitigate their perceived risks of vaccination by using an alternative immunization schedule (Kettunen et al., 2017).
3.3.4. Accessing health services
While some aspects of clinical practices were facilitators to early childhood immunizations, several studies reported barriers associated with challenges in accessing health services. For example, in rural Colorado, immunization providers created missed opportunities to vaccinate young children by not offering immunizations during sick visits or not screening for immunizations at every appointment (Deutchman et al., 2000). Other studies found that rural parents could also be hesitant to vaccinate their child outside of the well-child visit (Thomas et al., 2004, Wilson, 2000). Additionally, some immunization providers in rural Oregon were uncomfortable incorporating new vaccines into their practice (Fagnan et al., 2011). In two studies, one that interviewed a small group of individuals living in Bakersfield, California and the other talked to parents in a rural community in Missouri, parents reported that staff were viewed as difficult to engage with and appointment scheduling was challenging if the facility was only open during traditional hours (Thomas et al., 2004, Wilson, 2000). In rural Missouri, between the associated travel time and wait time with health care visits, if rural parents had inflexible jobs or unreliable transportation, they were overwhelmed by these additional barriers and, consequently, missed immunization visits (Thomas et al., 2004).
3.3.5. Other immunization challenges in rural areas
Within this review, we synthesized study results that were evidence of barriers to early childhood immunization specific to rural communities. For example, distance to clinic was identified as a barrier to early childhood immunization in two studies. Children 13–35 months old with parents living more than 10 miles from a clinic had lower vaccination rates than children that lived closer to a clinic that offered immunizations (Hicks et al., 2007). In rural Oregon, a study by Fagnan and associates of rural providers found as rurality increased, immunization coverage decreased (Fagnan et al., 2011). Within that study, each medical facility was designated according to the Rural Urban Commuting Area (RUCA) classification, from least to most rural, which meant the setting was either metropolitan, large rural town, small rural town, or isolated rural town. Ultimately, it was less likely that all recommended early childhood immunizations were administered as distance increased from a metropolitan area towards most rural (i.e., isolated rural town).
Nationally, rural children were more likely to be vaccinated at public facilities than urban or suburban children (Stokley et al., 2001). In one study in Oregon, surveyed providers in rural areas reported that most childhood immunizations are administered at a county health department (90%) or community health center (30%), and some providers referred all children outside of their clinic for vaccines (20%) (Fagnan et al., 2011). Similarly, in rural Colorado, about 33% of children ages 3–35 months were administered vaccines somewhere other than the child’s primary care provider, mostly at public health facilities (Kempe et al., 2001). Additionally, rural parents were more supportive than urban parents in receiving reminders to vaccinate their child from the local public health department (Saville et al., 2014). However, in a study by Bardenheier and associates, rural children in Colorado were more likely to be vaccinated at a private clinic compared to other urban areas (Bardenheier et al., 2004).
Multiple studies offered explanations for increased immunization referrals in rural communities. Referrals are often necessary because of the inability of rural providers and clinics to stock all recommended vaccines, difficulties keeping vaccine records, and staffing shortages (Fagnan et al., 2011). Rural communities tend to have fewer pediatricians (Weigel et al., 2016), which more often provided all immunizations to children as compared with family medicine or other general practice physicians (Fagnan et al., 2011). Even though the number of recommended immunizations has increased in the past 10 years, reimbursement rates have decreased (Fagnan et al., 2011) and are inadequate to cover the expense of storing and administering vaccines (Deutchman et al., 2000, Glazner et al., 2001). Therefore, rural private providers benefit by referring immunization services outside of their clinic to public facilities. However, public facilities have even lower reimbursement rates for vaccination than private rural clinics (Glazner et al., 2001) Referrals also cause disjointed child immunization records which makes it difficult for rural providers to maintain accurate vaccination history (Kempe et al., 2001). Research in rural areas has shown that using linked immunization registries can alleviate some of the effects of record scatter on early childhood immunization rates (Kempe et al., 2001, Renfrew et al., 2001). Lastly, another potential barrier with implications for rural practices identified by Daley and associates was that providers were less likely to recommend a new vaccine at the time of the study, 7-valent PCV, if their clinic vaccinated <50 children a week as compared to higher volume clinics (Daley et al., 2005).
4. Discussion
In this systematic review, we identified only 17 papers that investigated barriers to and facilitators of early childhood immunization in rural areas of the U.S. (Table 2).(Albright et al., 2014, Bardenheier et al., 2004, Daley et al., 2005, Deutchman et al., 2000, Fagnan et al., 2011, Glazner et al., 2001, Hicks et al., 2007, Kempe et al., 2001, Kettunen et al., 2017, Mical et al., 2021, Newcomer et al., 2021, Renfrew et al., 2001, Rosenthal et al., 2004, Saville et al., 2014, Stokley et al., 2001, Thomas et al., 2004, Wilson, 2000). Over half of studies were conducted within rural communities in just one U.S. state (Colorado), and over 70% of studies were completed before 2012. The existing body of research that we identified revealed that while some barriers to and facilitators of early childhood immunization were similar to those previously identified in other non-rural populations, some immunization barriers were specific to rural communities. Interventions to increase childhood vaccine uptake are most effective when targeted to specific barriers in specific geographic and clinical settings (Cataldi et al., 2020). Our review indicates that more research, including studies evaluating interventions to increase vaccine uptake in rural communities, is needed to bridge rural–urban disparities in early childhood vaccine coverage nationwide.
In our literature review, we identified themes reported in previous studies of early childhood immunization that did not focus on rural populations. For example, similar to our finding that the relationship between providers and parents facilitated vaccine uptake among rural children, parental perception of trustworthiness and confidence in their child's immunization nurse has been previously identified as an important factor in vaccine acceptance among parents (Keller, 2008). Moreover, multiple prior studies have found providers' vaccine recommendation style is linked with vaccine uptake, with presumptive approaches (i.e., assuming the parent intends to vaccinate) being more effective than participatory styles (i.e., asking if the parent would like to consider vaccination) (Brewer et al., 2017, Cataldi et al., 2020, Opel et al., 2013, Opel et al., 2015). It is unclear how frequently rural immunization providers adopt such vaccine communication strategies.
A barrier to early childhood vaccination identified across many studies was vaccine hesitancy, which the World Health Organization defines as “a delay in acceptance or refusal of vaccination despite the availability of vaccination services” (MacDonald, 2015, World Health Organization, 2014). Although vaccine hesitancy is not limited to rural communities (Larson et al., 2014), studies that have investigated the intersection of hesitancy and regionality demonstrate that more research is necessary to understand vaccine-hesitant concerns and behaviors at a community level, including within rural communities (Hausman et al., 2020, Lebrun-Harris et al., 2020, Vanderpool et al., 2015). While it is established that rural children and adolescents are undervaccinated compared to their urban counterparts nationally, it is unclear how much of this disparity is due to increased vaccine hesitancy in rural communities versus other barriers to preventive care access experienced by rural families (Hill et al., 2020, Walker et al., 2019). Evidence-based interventions to address parental hesitancy and increase vaccine uptake are distinct from interventions that address other structural barriers to accessing immunization services (Cataldi et al., 2020, Newcomer et al., 2021). Of note, while some older studies in our review indicated that vaccination data tracking was a challenge in rural areas, more recently, there have been marked improvements in centralized immunization information systems (IIS). Indeed, 49 states maintain IIS and almost all states report that 80% or more of children have at least two immunizations on record (CDC, 2020, Murthy et al., 2017, Scharf et al., 2021). Since some alternative vaccination patterns indicative of parental hesitancy are readily identifiable in such electronic immunization records (Hargreaves et al., 2020, Robison et al., 2012), moving forward, state IIS data may serve as a rich resource for tracking childhood undervaccination due to parental hesitancy across multiple geographies (Mbaeyi et al., 2020, National Vaccine Advisory Committee, 2015, Newcomer et al., 2021).
While all studies in our review focused on examining factors associated with vaccine uptake in a rural area, rurality was inconsistently defined throughout the studies. A recent literature review of interventions to improve adolescent human papillomavirus vaccine uptake in rural communities also reported a broad spectrum of definitions used to determine rurality (Brandt et al., 2021). Inconsistencies in defining rurality reflect the variation in ways that rural is described across national organizations. For example, the U.S. Census Bureau defines rural as a lack of urbanicity. Therefore, rural is any population that is not urban (at least 50,000 people) or an urbanized cluster (2,500–49,999 people) (U.S. Census Bureau, 2010). Other options to define rurality exist at the county level, by zip code, via RUCA guidelines, or using the Index of Relative Rurality (IRR) (Hawley et al., 2017). Additionally, the Office of Management and Budget (OMB) utilizes a metropolitan and nonmetropolitan designation, often reported as synonymous with urban and rural, which at times can be inappropriate because the MSA and non-MSA designation is a statistical calculation which can include both urban and non-urban areas within MSAs or non-MSAs (Bennett et al., 2019, Office of Management and Budget OMB, 2010). This systematic review indicates that more consistent and well-defined parameters of rurality would be helpful for elucidating differences between rural and non-rural barriers to early childhood immunizations. Furthermore, Doogan and associates suggest that current measures of rurality are not designed for health systems research, and better designations are necessary for interpretable results (Doogan et al., 2018). Ideally, a better understanding of characteristics specific to rural settings would facilitate more effective intervention methods to increase vaccine rates in rural areas (Douthit et al., 2015, Hart et al., 2005). However, without additional community-based research on barriers to and facilitators of early childhood immunization in rural populations, it is difficult to provide effective guidelines for future intervention strategies. Of note, our systematic review revealed that in the last 20 years, there were only three intervention-based papers focused on strategies to increase early childhood immunization uptake in rural communities (Albright et al., 2014, Hicks et al., 2007, Mical et al., 2021).
Regardless of discrepancies in how rurality was defined, we found notable themes specific to rural communities in the current review. For example, in rural communities, primary care providers refer patients to public facilities for immunizations more than those in non-rural settings (Fagnan et al., 2011, Kempe et al., 2001, Stokley et al., 2001). Vaccine referrals outside of the rural primary care clinic are indicative of barriers that exist for rural healthcare providers, including challenges in stocking all recommended vaccines due to staffing shortages and inadequate vaccine storage capabilities (Fagnan et al., 2011). Immunization referral outside of the child's primary care clinic increases missed opportunities for vaccine administration and decreases early childhood vaccination rates (Deutchman et al., 2000, Fagnan et al., 2011). Vaccine referrals also contribute to record scatter and create structural barriers for parents in rural communities who have to schedule their child's vaccine appointments outside of the primary care clinic.
Studies within this review reported that distance to immunization providers was a structural barrier to early childhood immunization uptake in rural settings (Fagnan et al., 2011, Hicks et al., 2007). Hicks and associates found that children with parents living more than 10 miles from their healthcare provider had lower immunization rates (Hicks et al., 2007). In Oregon, as rurality increased and moved farther from a metropolitan area, vaccine rates decreased (Fagnan et al., 2011). These rural specific challenges have been found in previous research and reflect the health disparities and structural barriers to health care access that exist in rural communities (Statz and Evers, 2020, Lam et al., 2018). Even though there is evidence that regionality and community differences influence the extent that barriers affect healthcare in rural communities (Lam et al., 2018), the reasons for difficulties in health care delivery to rural areas are complex. Weinhold and Gurtner suggested that insufficient health care in rural areas is rooted in problems with infrastructure, because of economic reasons, professional burdens on rural providers, and educational barriers (e.g., lack of rural medical students) (Weinhold and Gurtner, 2014). However, more research is needed to prevent negative alterations on health services like immunization delivery, especially as rural health disparities and inequities continue to increase.
Lastly, findings from this review point to evidence-based strategies that can be tailored to rural areas to increase immunization rates. For example, our review found that the relationships between parents and medical providers is an important facilitator of vaccine uptake in rural children. However, while most prior research on effective vaccine communication has focused on doctors working in private clinics (Brewer et al., 2017, Opel et al., 2013, Opel et al., 2015), public facilities play a substantial role in immunization services delivery in rural settings (Fagnan et al., 2011, Williams et al., 2020). Therefore, parents’ relationships with immunization nurses who staff public clinics is a component to parental vaccine behavior that requires consideration. Future studies in rural areas should aim to understand how public health nurse-patient communication strategies influence immunization (Wallace-Brodeur et al., 2020), and how public clinics can promote early childhood vaccination. Moving forward, tailoring evidence-based strategies for increasing vaccine uptake should acknowledge that where vaccines are received and who recommends those vaccines may be different in rural versus urban areas.
4.1. Limitations
Although the current systematic review utilized PRISMA guidelines (Page et al., 2021) to guide our searching and reporting process, due to the low number of papers, and since our systematic review goal did not include meta-analyses, we did not complete a risk of bias assessment. Additionally, the small sample size was not conducive to conducting a thorough meta-analysis.
Also, we recognize that the state of Colorado represented 10 out of 17 selected studies. Although low geographic variety of studies is an important finding of the review, it is also a limitation that potentially introduced bias to the rural specific findings. Barriers to and facilitators of early childhood immunization uptake in Colorado rural communities may not reflect the barriers and facilitators experienced by other rural areas. Overall, the small number of studies makes extrapolation of results difficult, and we suggest more work across a broader range of rural communities is required.
5. Conclusions
In this synthesis of current evidence on barriers to and facilitators of early childhood immunization uptake in rural communities, we identified a limited amount of recent research on this topic. Moving forward, investigations of immunization barriers in rural areas that have low vaccine uptake will be critical to informing interventions to increase vaccination rates. Additionally, more analyses examining the sensitivity of results to various rural/urban classification schemes that establish regional barriers to and facilitators of vaccine uptake would be helpful for targeting effective interventions. More work is needed to address barriers to early childhood vaccination in rural communities, identify facilitators of vaccine uptake, build lasting vaccine confidence, and achieve immunization equity across community settings.
Disclosure of ethical compliance
As this is a review of existing original articles, no ethical review was required.
This project was supported by a Center for Biomedical Research Excellence award from the National Institutes of Health, National Institute of General Medical Sciences (1P20GM130418). The authors have no other relevant sources of financial support or potential conflicts of interest to report.
Funding sources
This project was supported by a Center for Biomedical Research Excellence award from the National Institutes of Health, National Institute of General Medical Sciences (1P20GM130418).
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Alexandria N. Albers, Email: alexandria.albers@umontana.edu.
Juthika Thaker, Email: juthika.thaker@umontana.edu.
Sophia R. Newcomer, Email: sophia.newcomer@umontana.edu.
References
- Advisory Committee on Immunization Practices (ACIP), Fiore AE, Wasley A, Bell BP, 2006. Prevention of hepatitis A through active or passive immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm. Rep. 55 (RR-7), 1-23. Available at: https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5507a1.htm. Accessed February 6, 2022. [PubMed]
- Albright K., Saville A., Lockhart S., Widmer Racich K., Beaty B., Kempe A. Provider attitudes toward public-private collaboration to improve immunization reminder/recall: a mixed-methods study. Acad. Pediatr. 2014;14(1):62–70. doi: 10.1016/j.acap.2013.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardenheier B.H., Yusuf H.R., Rosenthal J., Santoli J.M., Shefer A.M., Rickert D.L., Chu S.Y. Factors associated with underimmunization at 3 months of age in four medically underserved areas. Public Health Rep. 2004;119(5):479–485. doi: 10.1016/j.phr.2004.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett K.J., Borders T.F., Holmes G.M., Kozhimannil K.B., Ziller E. What is rural? challenges and implications of definitions that inadequately encompass rural people and places. Health Aff. (Millwood). 2019;38(12):1985–1992. doi: 10.1377/hlthaff.2019.00910. [DOI] [PubMed] [Google Scholar]
- Bianco A., Mascaro V., Zucco R., Pavia M. Parent perspectives on childhood vaccination: how to deal with vaccine hesitancy and refusal? Vaccine. 2019;37(7):984–990. doi: 10.1016/j.vaccine.2018.12.062. [DOI] [PubMed] [Google Scholar]
- Brandt H.M., Vanderpool R.C., Pilar M., Zubizarreta M., Stradtman L.R. A narrative review of HPV vaccination interventions in rural U.S. communities. Prev. Med. 2021;145:106407. doi: 10.1016/j.ypmed.2020.106407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer N.T., Hall M.E., Malo T.L., Gilkey M.B., Quinn B., Lathren C. Announcements versus conversations to improve HPV vaccination coverage: a randomized trial. Pediatrics. 2017;139(1) doi: 10.1542/peds.2016-1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cataldi J.R., Kerns M.E., O'Leary S.T. Evidence-based strategies to increase vaccination uptake: a review. Curr. Opin. Pediatr. 2020;32(1):151–159. doi: 10.1097/MOP.0000000000000843. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Child and adolescent immunization schedule. Available at: https://www.cdc.gov/vaccines/schedules/hcp/imz/child-adolescent.html. Updated February 17, 2022. Accessed February 20, 2022.
- Centers for Disease Control and Prevention (CDC). 2020 IISAR data participation rates. Immunization Information System Annual Report, CY2020. Available at: https://www.cdc.gov/vaccines/programs/iis/annual-report-iisar/2020-data.html#child. Updated October 19, 2021. Accessed February 6, 2022.
- Centers for Disease Control and Prevention (CDC). About the National Immunization Surveys (NIS). Available at: https://www.cdc.gov/vaccines/imz-managers/nis/about.html. Updated January 23, 2018. Accessed August 28, 2021.
- Centers for Disease Control and Prevention (CDC). About VFC, the VFC program: at a glance. Available at: https://www.cdc.gov/vaccines/programs/vfc/about/index.html. Updated February 18, 2016. Accessed February 6, 2022.
- Centers for Disease Control and Prevention (CDC), 2011. Ten great public health achievements—worldwide, 2001-2010. MMWR Morb. Mortal. Wkly. Rep. 60 (24), 814–818. Available at: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6024a4.htm. Accessed August 28, 2021. [PubMed]
- Colorado Children’s Immunization Coalition. Colorado immunization information system environmental scan: a review of the history, background and current state of CIIS. Available at: https://www.immunizecolorado.org/uploads/CIISEnvironmentalScan_11152013.pdf. Published November 15, 2013. Accessed August 28, 2021.
- Daley M.F., Crane L.A., Beaty B.L., Barrow J., Pearson K., Stevenson J.M., Berman S., Kempe A. Provider adoption of pneumococcal conjugate vaccine and the impact of vaccine shortages. Ambul. Pediatr. 2005;5(3):157–164. doi: 10.1367/A04-142R.1. [DOI] [PubMed] [Google Scholar]
- Deutchman M., Brayden R., Siegel C.D., Beaty B., Crane L. Childhood immunization in rural family and general practices: current practices, perceived barriers and strategies for improvement. Ambul. Child Health. 2000;6(3):181–189. [Google Scholar]
- Doogan N.J., Roberts M.E., Wewers M.E., Tanenbaum E.R., Mumford E.A., Stillman F.A. Validation of a new continuous geographic isolation scale: a tool for rural health disparities research. Soc. Sci. Med. 2018;215:123–132. doi: 10.1016/j.socscimed.2018.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douthit N., Kiv S., Dwolatzky T., Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. 2015;129(6):611–620. doi: 10.1016/j.puhe.2015.04.001. [DOI] [PubMed] [Google Scholar]
- Fagnan L.J., Shipman S.A., Gaudino J.A., Mahler J.o., Sussman A.L., Holub J. To give or not to give: approaches to early childhood immunization delivery in Oregon rural primary care practices. J. Rural Health. 2011;27(4):385–393. doi: 10.1111/j.1748-0361.2010.00356.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman R.E., Thaker J., Daley M.F., Glanz J.M., Newcomer S.R. Vaccine timeliness and prevalence of undervaccination patterns in children ages 0-19 months, U.S., National Immunization Survey-Child 2017. Vaccine. 2022;40(5):765–773. doi: 10.1016/j.vaccine.2021.12.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gahr P., DeVries A.S., Wallace G., Miller C., Kenyon C., Sweet K., Martin K., White K., Bagstad E., Hooker C., Krawczynski G., Boxrud D., Liu G., Stinchfield P., LeBlanc J., Hickman C., Bahta L., Barskey A., Lynfield R. An outbreak of measles in an undervaccinated community. Pediatrics. 2014;134(1):e220–e228. doi: 10.1542/peds.2013-4260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz J.M., Narwaney K.J., Newcomer S.R., Daley M.F., Hambidge S.J., Rowhani-Rahbar A., Lee G.M., Nelson J.C., Naleway A.L., Nordin J.D., Lugg M.M., Weintraub E.S. Association between undervaccination with diphtheria, tetanus toxoids, and acellular pertussis (DTaP) vaccine and risk of pertussis infection in children 3 to 36 months of age. JAMA Pediatr. 2013;167(11):1060–1064. doi: 10.1001/jamapediatrics.2013.2353. [DOI] [PubMed] [Google Scholar]
- Glazner J.E., Steiner J.F., Haas K.J., Renfrew B., Deutchman M., Berman S. Is reimbursement for childhood immunizations adequate? evidence from two rural areas in Colorado. Public Health Rep. 2001;116(3):219–225. doi: 10.1093/phr/116.3.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant R., Gracy D., Goldsmith G., Sobelson M., Johnson D. Transportation barriers to child health care access remain after health reform. JAMA Pediatr. 2014;168(4):385. doi: 10.1001/jamapediatrics.2013.4653. [DOI] [PubMed] [Google Scholar]
- Hargreaves A.L., Nowak G., Frew P.M., Hinman A.R., Orenstein W.A., Mendel J., Aikin A., Nadeau J.A., McNutt L.-A., Chamberlain A.T., Omer S.B., Randall L.A., Bednarczyk R.A. Adherence to timely vaccinations in the United States. Pediatrics. 2020;145(3) doi: 10.1542/peds.2019-0783. [DOI] [PubMed] [Google Scholar]
- Hart L.G., Larson E.H., Lishner D.M. Rural definitions for health policy and research. Am. J. Public Health. 2005;95(7):1149–1155. doi: 10.2105/AJPH.2004.042432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hausman B.L., Lawrence H.Y., Marmagas S.W., Fortenberry L., Dannenberg C.J. H1N1 vaccination and health beliefs in a rural community in the Southeastern United States: lessons learned. Crit. Public Health. 2020;30(2):245–251. [Google Scholar]
- Hawley, L.R., Koziel, N.A., Bovaird, J.A., 2017. Defining and communicating rural. In: Nugent GC, Kunz GM, Sheridan SM, Glover TA, Knoche LL, eds. Rural education research in the United States: state of the science and emerging directions. [ebook]. Switzerland: Springer International Publishing. 31–54. Available at: http://ndl.ethernet.edu.et/bitstream/123456789/32675/1/297.Gwen%20C.%20Nugent.pdf#page=35. Published 2017. Accessed August 28, 2021.
- Hicks P., Tarr G.A., Hicks X.P. Reminder cards and immunization rates among Latinos and the rural poor in Northeast Colorado. J. Am. Board Fam. Med. 2007;20(6):581–586. doi: 10.3122/jabfm.2007.06.060071. [DOI] [PubMed] [Google Scholar]
- Hill H.A., Yankey D., Elam-Evans L.D., Singleton J.A., Pingali S.C., Santibanez T.A. Vaccination coverage by age 24 months among children born in 2016 and 2017 - National Immunization Survey-Child, United States, 2017–2019. MMWR Morb. Mortal. Wkly Rep. 2020;69(42):1505–1511. doi: 10.15585/mmwr.mm6942a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingram, D.D., Franco, S.J., 2012. NCHS urban–rural classification scheme for counties. National Center for Health Statistics. Vital Health Stat. 2 (166), 1-81. Available at: https://www.cdc.gov/nchs/data/series/sr_02/sr02_166.pdf. Accessed August 28, 2021. [PubMed]
- Keller T. Mexican American parent’s perceptions of culturally congruent interpersonal processes of care during childhood immunization episodes: a pilot study. J. Rural. Nurs. Health Care. 2008;8(2):33–41. doi: 10.14574/ojrnhc.v8i2.115. [DOI] [Google Scholar]
- Kempe A., Steiner J.F., Renfrew B.L., Lowery E., Haas K., Berman S. How much does a regional immunization registry increase documented immunization rates at primary care sites in rural Colorado? Ambul. Pediatr. 2001;1(4):213–216. doi: 10.1367/1539-4409(2001)001<0213:hmdari>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Kettunen C., Nemecek J., Wenger O. Evaluation of low immunization coverage among the Amish population in rural Ohio. Am. J. Infect. Control, 2017;45(6):630–634. doi: 10.1016/j.ajic.2017.01.032. [DOI] [PubMed] [Google Scholar]
- Kurosky S.K., Davis K.L., Krishnarajah G. Completion and compliance of childhood vaccinations in the United States. Vaccine. 2016;34(3):387–394. doi: 10.1016/j.vaccine.2015.11.011. [DOI] [PubMed] [Google Scholar]
- Lam, O., Roderick. B., Toor, S. How far Americans live from the closest hospital differs by community type. Pew Research Center. Available at: https://www.pewresearch.org/fact-tank/2018/12/12/how-far-americans-live-from-the-closest-hospital-differs-by-community-type/. Published December 12, 2018. Accessed August 28, 2021.
- Lannon C., Brack V., Stuart J., et al. What mothers say about why poor children fall behind on immunizations: a summary of focus groups in North Carolina. Arch. Pediatr. Adolesc. Med. 1995;149(10):1070–1075. doi: 10.1001/archpedi.1995.02170230024003. [DOI] [PubMed] [Google Scholar]
- Larson H.J., Jarrett C., Eckersberger E., Smith D.M.D., Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. 2014;32(19):2150–2159. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- Lebrun-Harris L.A., Mendel Van Alstyne J.A., Sripipatana A. Influenza vaccination among U.S. pediatric patients receiving care from federally funded health centers. Vaccine. 2020;38(39):6120–6126. doi: 10.1016/j.vaccine.2020.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald N.E. SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- Mbaeyi S., Cohn A., Messonnier N. A call to action: strengthening vaccine confidence in the United States. Pediatrics. 2020;145(6) doi: 10.1542/peds.2020-0390. [DOI] [PubMed] [Google Scholar]
- Megel M.E., Heser R., Matthews K. Parents' assistance to children having immunizations. Issues Compr. Pediatr. Nurs. 2002;25(3):151–165. doi: 10.1080/01460860290042585. [DOI] [PubMed] [Google Scholar]
- Mical R., Martin-Velez J., Blackstone T., Derouin A. Vaccine hesitancy in rural pediatric primary care. J. Pediatr. Health Care. 2021;35(1):16–22. doi: 10.1016/j.pedhc.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moy E., Garcia M.C., Bastian B., Rossen L.M., Ingram D.D., Faul M., Massetti G.M., Thomas C.C., Hong Y., Yoon P.W., Iademarco M.F. Leading causes of death in nonmetropolitan and metropolitan areas— United States, 1999–2014. MMWR Surveill. Summ. 2017;66(1):1–8. doi: 10.15585/mmwr.ss6601a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murthy N., Rodgers L., Pabst L., Fiebelkorn A.P., Ng T. Progress in childhood vaccination data in immunization information systems — United States, 2013–2016. MMWR Morb. Mortal. Wkly Rep. 2017;66(43):1178–1181. doi: 10.15585/mmwr.mm6643a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Vaccine Advisory Committee Assessing the state of vaccine confidence in the United States: recommendations from the National Vaccine Advisory Committee: Approved by the National Vaccine Advisory Committee on June 10, 2015. Public Health Rep. 2015;130(6):573–595. doi: 10.1177/003335491513000606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomer S.R., Freeman R.E., Wehner B.K., Anderson S.L., Daley M.F. Timeliness of early childhood vaccinations and undervaccination patterns in Montana. Am. J. Prev. Med. 2021;61(1):e21–e29. doi: 10.1016/j.amepre.2021.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of Management and Budget (OMB). 2010 standards for delineating metropolitan and micropolitan statistical areas: a notice by the management and budget office. Available at: https://www.federalregister.gov/documents/2010/06/28/2010-15605/2010-standards-for-delineating-metropolitan-and-micropolitan-statistical-areas. Published June 28, 2010. Accessed August 28, 2021.
- O'Leary S.T., Barnard J., Lockhart S., Kolasa M., Shmueli D., Dickinson L.M., Kile D., Dibert E., Kempe A. Urban and rural differences in parental attitudes about influenza vaccination and vaccine delivery models. J. Rural Health. 2015;31(4):421–430. doi: 10.1111/jrh.12119. [DOI] [PubMed] [Google Scholar]
- O'Leary S.T., Brewer S.E., Pyrzanowski J., Barnard J., Sevick C., Furniss A., Dempsey A.F. Timing of information-seeking about infant vaccines. J. Pediatr. 2018;203:125–130.e1. doi: 10.1016/j.jpeds.2018.07.046. [DOI] [PubMed] [Google Scholar]
- Opel D.J., Heritage J., Taylor J.A., Mangione-Smith R., Salas H.S., DeVere V., Zhou C., Robinson J.D. The architecture of provider-parent vaccine discussions at health supervision visits. Pediatrics. 2013;132(6):1037–1046. doi: 10.1542/peds.2013-2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opel D.J., Mangione-Smith R., Robinson J.D., Heritage J., DeVere V., Salas H.S., Zhou C., Taylor J.A. The influence of provider communication behaviors on parental vaccine acceptance and visit experience. Am. J. Public Health. 2015;105(10):1998–2004. doi: 10.2105/AJPH.2014.302425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., Chou R., Glanville J., Grimshaw J.M., Hróbjartsson A., Lalu M.M., Li T., Loder E.W., Mayo-Wilson E., McDonald S., McGuinness L.A., Stewart L.A., Thomas J., Tricco A.C., Welch V.A., Whiting P., Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J. Clin. Epidemiol. 2021;134:178–189. doi: 10.1016/j.jclinepi.2021.03.001. [DOI] [PubMed] [Google Scholar]
- Parashar, U.D., Alexander, J.P., Glass, R.I.; Advisory Committee on Immunization Practices (ACIP), Centers for Disease Control and Prevention (CDC), 2006. Prevention of rotavirus gastroenteritis among infants and children. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm. Rep. 55 (RR-12), 1–13. Available at: https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5512a1.htm. Accessed February 18, 2022. [PubMed]
- Probst J.C., Barker J.C., Enders A., Gardiner P. Current state of child health in rural America: how context shapes children's health. J. Rural Health. 2018;34(Suppl 1):s3–s12. doi: 10.1111/jrh.12222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renfrew B.L., Kempe A., Lowery N.E., Chandramouli V., Steiner J.E., Berman S. The impact of immunization record aggregation on up-to-date rates–implications for immunization registries in rural areas. J. Rural Health. 2001;17(2):122–126. doi: 10.1111/j.1748-0361.2001.tb00268.x. [DOI] [PubMed] [Google Scholar]
- Robison S.G., Groom H., Young C. Frequency of alternative immunization schedule use in a metropolitan area. Pediatrics. 2012;130(1):32–38. doi: 10.1542/peds.2011-3154. [DOI] [PubMed] [Google Scholar]
- Rosenthal J., Rodewald L., McCauley M., Berman S., Irigoyen M., Sawyer M., Yusuf H., Davis R., Kalton G. Immunization coverage levels among 19- to 35-month-old children in 4 diverse, medically underserved areas of the United States. Pediatrics. 2004;113(4):e296–e302. doi: 10.1542/peds.113.4.e296. [DOI] [PubMed] [Google Scholar]
- Saville A.W., Beaty B., Dickinson L.M., Lockhart S., Kempe A. Novel immunization reminder/recall approaches: rural and urban differences in parent perceptions. Acad. Pediatr. 2014;14(3):249–255. doi: 10.1016/j.acap.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scharf L.G., Coyle R., Adeniyi K., Fath J., Harris L., Myerburg S., Kurilo M.B., Abbott E. Current challenges and future possibilities for immunization information systems. Acad. Pediatr. 2021;21(4):S57–S64. doi: 10.1016/j.acap.2020.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz J.L., Colgrove J. The vaccines for children program at 25 - access, affordability, and sustainability. NEJM. 2020;382(24):2277–2279. doi: 10.1056/NEJMp2000891. [DOI] [PubMed] [Google Scholar]
- Shipman S.A., Lan J., Chang C.H., Goodman D.C. Geographic maldistribution of primary care for children. Pediatrics. 2011;127(1):19–27. doi: 10.1542/peds.2010-0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith P.J., Molinari N.A., Rodewald L.E. Underinsurance and pediatric immunization delivery in the United States. Pediatrics. 2009;124(Suppl 5):S507–S514. doi: 10.1542/peds.2009-1542J. [DOI] [PubMed] [Google Scholar]
- Statz M., Evers K. Spatial barriers as moral failings: What rural distance can teach us about women's health and medical mistrust author names and affiliations. Health Place. 2020;64 doi: 10.1016/j.healthplace.2020.102396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokley S., Smith P.J., Klevens R.M., Battaglia M.P. Vaccination status of children living in rural areas in the United States: are they protected? Am. J. Prev. Med. 2001;20(4 Suppl):55–60. doi: 10.1016/s0749-3797(01)00280-x. [DOI] [PubMed] [Google Scholar]
- Taylor J.A., Darden P.M., Brooks D.A., Hendricks J.W., Wasserman R.C., Bocian A.B. Association between parents’ preferences and perceptions of barriers to vaccination and the immunization status of their children: a study from Pediatric Research in Office Settings and the National Medical Association. Pediatrics. 2002;110(6):1110–1116. doi: 10.1542/peds.110.6.1110. [DOI] [PubMed] [Google Scholar]
- Thomas M., Kohli V., King D. Barriers to childhood immunization: findings from a needs assessment study. Home Health Care Serv. Q. 2004;23(2):19–39. doi: 10.1300/J027v23n02_02. [DOI] [PubMed] [Google Scholar]
- Tierney C.D., Yusuf H., McMahon S.R., Rusinak D., O’ Brien M.A., Massoudi M.S., Lieu T.A. Adoption of reminder and recall messages for immunizations by pediatricians and public health clinics. Pediatrics. 2003;112(5):1076–1082. doi: 10.1542/peds.112.5.1076. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. How does the U.S. Census Bureau define “rural?”. Available at: https://mtgis-portal.geo.census.gov/arcgis/apps/MapSeries/index.html?appid=49cd4bc9c8eb444ab51218c1d5001ef6. Published 2010. Accessed August 28, 2021.
- U.S. Census Bureau. Metropolitan and micropolitan statistical areas map. Available at: https://www.census.gov/geographies/reference-maps/2020/geo/cbsa.htmlTaggedEnd. Updated November 4, 2020. Accessed August 28, 2021.
- Vanderpool R.C., Dressler E.V., Stradtman L.R., Crosby R.A. Fatalistic beliefs and completion of the HPV vaccination series among a sample of young Appalachian Kentucky women. J. Rural Health. 2015;31(2):199–205. doi: 10.1111/jrh.12102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace-Brodeur R., Li R., Davis W., Humiston S., Albertin C., Szilagyi P.G., Rand C.M. A quality improvement collaborative to increase human papillomavirus vaccination rates in local health department clinics. Prev. Med. 2020;139 doi: 10.1016/j.ypmed.2020.106235. 106235. [DOI] [PubMed] [Google Scholar]
- Walker T.Y., Elam-Evans L.D., Yankey D., Markowitz L.E., Williams C.L., Fredua B., Singleton J.A., Stokley S. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 Years – United States, 2018. MMWR Morb. Mortal. Wkly Rep. 2019;68(33):718–723. doi: 10.15585/mmwr.mm6833a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weigel P.A., Ullrich F., Shane D.M., Mueller K.J. Variation in primary care service patterns by rural-urban location. J. Rural Health. 2016;32(2):196–203. doi: 10.1111/jrh.12146. [DOI] [PubMed] [Google Scholar]
- Weinhold I., Gurtner S. Understanding shortages of sufficient health care in rural areas. Health Policy. 2014;118(2):201–214. doi: 10.1016/j.healthpol.2014.07.018. [DOI] [PubMed] [Google Scholar]
- Whitney, C.G., Zhou, F., Singleton, J., et al. 2014. Benefits from immunization during the vaccines for children program era - United States, 1994-2013. MMWR Morb. Mortal. Wkly. Rep. 63 (16), 352-355. Available at: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6316a4.htm. Accessed August 28, 2021. [PMC free article] [PubMed]
- Williams C.L., Walker T.Y., Elam-Evans L.D., Yankey D., Fredua B., Saraiya M., Stokley S. Factors associated with not receiving HPV vaccine among adolescents by metropolitan statistical area status, United States, National Immunization Survey-Teen, 2016–2017. Hum. Vaccin. Immunother. 2020;16(3):562–572. doi: 10.1080/21645515.2019.1670036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson T. Factors influencing the immunization status of children in a rural setting. J. Pediatr. Health Care. 2000;14(3):117–121. doi: 10.1016/s0891-5245(00)70022-8. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO). Report of the SAGE working group on vaccine hesitancy. Available at: https://www.who.int/immunization/sage/meetings/2014/october /1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf. Updated October 1, 2014. Accessed August 28, 2021.
- Zhai Y., Santibanez T.A., Kahn K.E., Srivastav A., Walker T.Y., Singleton J.A. Rural, urban, and suburban differences in influenza vaccination coverage among children. Vaccine. 2020;38(48):7596–7602. doi: 10.1016/j.vaccine.2020.10.030. [DOI] [PubMed] [Google Scholar]
- Zucker J.R., Rosen J.B., Iwamoto M., et al. Consequences of undervaccination – measles outbreak, New York City, 2018–2019. NEJM. 2020;382(11):1009–1017. doi: 10.1056/NEJMoa191251. [DOI] [PubMed] [Google Scholar]