Highlights
-
•
Housing is a critical social determinant of health and health care utilization.
-
•
For low-income women of reproductive age, public housing may play an important role.
-
•
Women in public housing had fewer outpatient and more emergency department visits.
-
•
Significance of associations varied across racial/ethnic group and public housing site.
-
•
Race and place are key to understanding public housing and health care utilization.
Abbreviations: EHR, Electronic Health Records; ED, Emergency Department; RAD, Rental Assistance Demonstration Program; AANHPI/Other, Asian, Alaskan Native/Native American, Native Hawaiian/Pacific Islander, and Other
Keywords: Housing, Reproductive health, Health care utilization, Racial/ethnic disparities, Social determinants
Abstract
Housing is a key social determinant of health and health care utilization. Although stigmatized due to poor quality, public housing may provide stability and affordability needed for individuals to engage in health care utilization behaviors. For low-income women of reproductive age (15–44 y), this has implications for long-term reproductive health trajectories. In a sample of 5,075 women, we used electronic health records (EHR) data from 2006 to 2011 to assess outpatient and emergency department (ED) visits across six public housing sites in San Francisco, CA. Non-publicly housed counterparts were selected from census tracts surrounding public housing sites. Multivariable regression models adjusted for age and insurance status estimated incidence rate ratios (IRR) for outpatient visits (count) and odds ratios (OR) for ED visit (any/none). We obtained race/ethnicity-specific associations overall and by public housing site. Analyses were completed in December 2020. Public housing was consistently associated with health care utilization among the combined Asian, Alaskan Native/Native American, Native Hawaiian/Pacific Islander, and Other (AANHPI/Other) group. Public housing residents had fewer outpatient visits (IRR: 0.86; 95% Confidence Interval [CI]: 0.81, 0.93) and higher odds of an ED visit (OR: 1.81; 95% CI: 1.32, 2.48). Black women had higher odds of an ED visits (OR: 1.32; 95% CI: 1.07, 1.63), but this was driven by one public housing site (site-specific OR: 2.34; 95% CI: 1.12, 4.88). Variations by race/ethnicity and public housing site are integral to understanding patterns of health care utilization among women of reproductive age to potentially improve women’s long-term health trajectories.
1. Introduction
Housing is a critical social determinant of health especially among low-income populations for whom housing options may be limited.(Hernández and Swope, 2019, Sandel and Desmond, 2017, Krieger and Higgins, 2002) While existing research on housing and health largely focuses on access and quality, a growing body of evidence emphasizes the importance of other domains such as affordability and stability.(Baker et al., 2017, Dunn, 2000, Dunn et al., 2006, Hernández and Swope, 2019) Furthermore, research also links housing instability and poor housing quality to increased health care utilization.(Caswell and Zuckerman, 2018) Public housing is an important mechanism for housing affordability and stability, but often comes at the expense of quality due to decades of government underinvestment.(Swope and Hernández, 2019) Existing literature indicates that public housing residents have poorer health across numerous outcomes compared to those living in non-public housing, with poor quality often being cited as a driving mechanism.(Digenis-Bury et al., 2008, Heinrich et al., 2008, Hinds et al., 2019) Emerging work challenges these findings, showing that health among public housing residents is equivalent to or better than other low-income residents who are not publicly housed.(Digenis-Bury et al., 2008, Ellen et al., 2020, Fertig and Reingold, 2007, Hinds et al., 2018) These findings cite the fact that non-publicly housed low-income residents may also experience adverse health impacts due to stress from navigating less stable and less affordable housing options available through the traditional housing market.(Baker et al., 2017, Swope and Hernández, 2019) This may also decrease financial resources needed to use health care services that support their health.(Sandel and Desmond, 2017) Consideration of such nuances of public housing is integral to being able to support positive health and health care outcomes for populations already at risk.
Understanding such nuances is particularly relevant for addressing the health of low-income women of reproductive age (15–44 years), given that women and families make up a large proportion of public housing residents.(Bolton and Bravve, 2012) Reproductive health for this group extends beyond family planning and sexual health to include preconception, prenatal, postpartum, and interconception health that ensure holistic physical, mental, and social wellbeing in relation to reproduction.(World Health Organization, 2017) Maintaining holistic reproductive health across these multiple dimensions requires access to and utilization of health care.(Hall et al., 2014, Kane and Margerison-Zilko, 2017, Potter et al., 2009, Wilensky and Proser, 2008) In particular, consistent access to primary care supports the diagnosis and management of key conditions such as overweight/obesity, diabetes, hypertension, and behavioral health outcomes (i.e. substance use and mental health).(Johnson et al., 2015, Wilensky and Proser, 2008, World Health Organization, 2017) While national goals generally emphasize that health care utilization should align with diagnosis and management these health conditions, and thus expected health care visits can vary, they do recommend that women at least attend an annual well woman visit.(Johnson et al., 2015) However, data from the 2012 Behavioral Risk Factors Surveillance System suggest that almost 40% of women of reproductive age did not have a checkup or access preventative care in the prior year.(Margerison et al., 2020) Additionally, another national study finds that among women who do have a health service visit within the prior year, those with higher levels of social disadvantage have higher rates of health services use.(Hall et al., 2014) This suggests a greater utilization need in this population and thus a greater gap in being able to achieve holistic reproductive health if services are not accessible.
Prior research on public housing and women’s healthcare utilization is limited and has important methodological challenges. The first limitation is that few studies specifically investigate health care utilization among women of reproductive age. Most focus on public housing and health outcomes and are conducted among either children, the elderly, or all adults.(Fenelon et al., 2017, Fertig and Reingold, 2007, Kramer et al., 2012, Slopen et al., 2018) A few studies have been conducted among mothers,(Fertig and Reingold, 2007, Kramer et al., 2012) but they exclude women early in their reproductive trajectory before their first child. Next, existing research that compares health outcomes of public housing residents to the total population may overestimate detrimental health impacts because social stratification limits the ability of low-income populations to access comparable housing options as higher-income populations.(Baker et al., 2017, Lim et al., 2020, Swope and Hernández, 2019) Relatedly, those who are eligible and apply for public housing systematically differ from those who do not in ways that may also bias findings.(Fertig and Reingold, 2007) Recent studies account for these selection related issues by including more comparable, non-publicly housed low-income populations. These studies report varied findings, with some still indicating that public housing residents fare worse for outcomes ranging from smoking to obesity to overall health condition burden,(Antonakos and Colabianchi, 2018, Cunningham et al., 2017, Ellen et al., 2020) and others finding no association for outcomes such as alcohol consumption, physical activity, diabetes, and body mass index.(Antonakos and Colabianchi, 2018, Ellen et al., 2020, Fertig and Reingold, 2007, Lim et al., 2020) Some studies also report better outcomes, for example on general health and lower psychological distress, among public housing residents compared to non-public housing residents.(Fenelon et al., 2017) Thus, addressing methodological issues relating to selection of comparison populations is important as research moves beyond health outcomes to fill the gap in understanding how public housing is associated with health care utilization specifically among women of reproductive age.
The objective of this study was to investigate associations between public housing and health care utilization among women of reproductive age, accounting for such comparison populations issues, across six public housing sites in San Francisco. We hypothesize that public housing tenancy will be associated with increased outpatient health care utilization and decreased emergency department use compared to non-publicly housed women of reproductive age in the same neighborhood.
2. Methods
2.1. Study sample
This study combined data from two mixed methods studies investigating the health impacts of public housing transformation on residents in 11 public housing sites in San Francisco, CA. Public housing is one of multiple affordable housing options for low-income residents, which also includes privately owned below market rate housing and individual housing vouchers for use on the private housing market.(Rahaim et al., 2018, San Francisco Planning Department, 2020) While estimates vary, recent data suggests that public housing units comprise approximately 6,000 of 33,000 affordable housing units of varying types available in San Francisco.(Mason, 2022, San Francisco Planning Department, 2020) These units have long been challenged by deterioration due to underfunding and disinvestment, but as housing affordability has become a crisis in San Francisco, the city has redirected attention to programs to rehabilitate public housing stock.(Dubbin et al., 2019, Hagan et al., 2020, San Francisco Planning Department, 2020) For the current study, reflecting the aims of the parent studies from which we obtained data, housing sites were limited to those participating in either the HOPE SF program,(Public Housing Task Force, 2007) which is San Francisco’s local redesign of the national Housing Opportunities for People Everywhere (HOPE VI) program focused on redeveloping public housing sites with public–private partnerships in collaboration with the communities, or the Rental Assistance Demonstration(RAD) program, which focuses on renovating physically deteriorated public housing units without redeveloping the whole site. (Dubbin et al 2019) Details about each study are described elsewhere.(Dubbin et al., 2019, Hagan et al., 2020) Briefly, these studies used qualitative interviews from residents and quantitative electronic health record (EHR) data from two large health networks, to understand the impact of public housing transformation programs on health. The current study leveraged EHR data from 4 large hospitals and 18 public clinics that were geocoded by address; records without a valid address were excluded (5% of records). We limited our study population to women of reproductive age (ages 15–44), excluding three public housing sites for the elderly, and two additional sites for small sample size. We limited to records from 2006 to 2011 in order to ensure that visits occurred before planned renovation and/or redevelopment activities were initiated at any of the sites.(Dubbin et al., 2019, Hagan et al., 2020).
We limited the study population to women with an address in the same census tract as one of the six public housing sites included (n = 7 census tracts) or any of the census tracts that bordered the public housing census tracts (n = 26 census tracts). Census tracts are defined as sociodemographically homogenous areas with an optimal size of 4,000 individuals per tract.(Census Bureau Glossary, 2019) Comparison populations from such an area are likely exposed to similar socioeconomic and structural factors impacting housing, access to health care, and utilization.(Kersten et al., 2018, Williams and Collins, 2001) In fact, the census tracts in our study population were concentrated in the southeastern part of the city, which has higher concentrations of neighborhoods with residents living below the poverty line, relying on some form of public support for rental assistance, experiencing higher crime, and lower levels of perceived safety.(Rahaim et al., 2018, San Francisco Health Improvement Partnership, 2016).
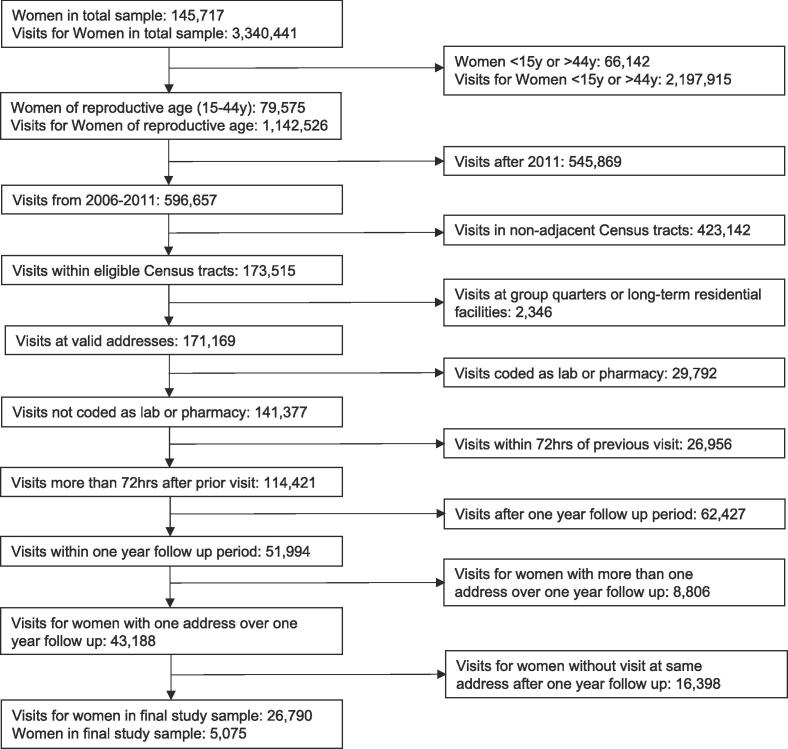
We confined our follow-up period to one year after a woman’s first visit within the reproductive age window to ensure a standard follow-up period for all participants and limited our sample to women with a stable address over the year.(Kersten et al., 2018) We excluded participants without at least one visit after the follow-up period at the same address to ensure the same housing type exposure for the full year. We excluded addresses at group quarters or residential long-term care facilities. Lab or pharmacy visits and visits that occurred within 72 hrs of a prior visit were excluded as either non-valid or as part of a previous care episode, respectively. Our final study sample included 26,790 emergency department (ED) or outpatient health care visit records from 5,075 women (Fig. 1). Women included in our sample were more likely to live in public housing, had more outpatient visits, were less likely to be white, more likely to have other public insurance, and less likely to be uninsured. This study was reviewed and approved by the University of California San Francisco Institutional Review Board with reliance granted by the Drexel University Institutional Review Board.
Fig. 1.
Study Sample Size Determined by Inclusion and Exclusion Criteria Applied to Electronic Health Records.
2.2. Outcome
Health care utilization was operationalized as the cumulative number of visits over a one-year period. Visits included both outpatient and ED. Outpatient visits included any visit to a primary care provider, community clinic, health center, or specialty clinic that met inclusion criteria. ED visits included those occurring at the ED of the four large hospitals within the health care networks. We tallied counts separately for outpatient and ED visits. ED visits were also measured dichotomously (any/none) due to their zero inflated distribution.
2.3. Exposure
Our main exposure was residence in public housing sites currently participating in the HOPE SF or RAD programs. Individuals residing in public housing sites not included in either HOPE SF or RAD locations were excluded (n = 263).
2.4. Covariates
Additional analytic variables included age at baseline visit, primary insurance payer at baseline visit, and race/ethnicity. Age and insurance payer categories are listed in Table 1. Race/ethnicity included Non-Latinx Black, Non-Latinx White, Latinx, Asian, Alaskan Native/Native American, Native Hawaiian/Pacific Islander, and Other. Due to small sample size, we combined Asian (n = 717), Alaskan Native/Native American (n = 44), Native Hawaiian/Pacific Islander (n = 161), and Other (n = 365) to create a heterogeneous “AANHPI/Other” category. Individuals with race/ethnicity missing were excluded (n = 8).
Table 1.
Distributions of Analytic Variables Overall and by Race/Ethnicity.
| Race/Ethnicity | |||||||
|---|---|---|---|---|---|---|---|
| Overall (n = 5,067) |
White (n = 399; 7.9%) | Black (n = 1712; 33.8%) | Latina (n = 1669; 32.9%) | AANHPI/Other1 (n = 1287; 25.4%) | p-value | ||
| Housing Type, % | |||||||
| Non-Public Housing | 80.3 | 91.2 | 64.0 | 93.2 | 81.9 | <0.0001 | |
| Public Housing | 19.7 | 8.8 | 35.9 | 6.8 | 18.1 | ||
| Health Care Visit Counts | |||||||
| Outpatient, mean(SD) | 4.8 (5.3) | 3.8 (4.4) | 4.3 (4.7) | 5.8 (6.1) | 4.7 (5.1) | <0.0001 | |
| Emergency Department, mean(SD) | 0.4 (0.8) | 0.4 (0.8) | 0.5 (0.9) | 0.3 (0.7) | 0.3 (0.7) | <0.0001 | |
| One or more ED visit, % | 26.2 | 32.8 | 31.1 | 21.4 | 23.8 | <0.0001 | |
| Age, % | |||||||
| 15–19 | 25.6 | 10.5 | 31.3 | 23.7 | 25.1 | <0.0001 | |
| 20–24 | 20.3 | 17.0 | 23.0 | 20.5 | 17.6 | ||
| 25–29 | 18.0 | 25.6 | 16.8 | 17.6 | 18.0 | ||
| 30–34 | 14.4 | 17.3 | 11.1 | 16.5 | 15.1 | ||
| 35–39 | 13.0 | 20.1 | 10.1 | 14.3 | 13.0 | ||
| 40–44 | 8.7 | 9.5 | 7.8 | 7.5 | 11.2 | ||
| Insurance Type, % | |||||||
| Medi-Cal | 32.9 | 16.8 | 39.8 | 33.1 | 28.4 | <0.0001 | |
| Other Public | 37.6 | 38.6 | 34.0 | 36.6 | 43.4 | ||
| Commercial | 2.7 | 6.0 | 1.9 | 2.1 | 3.7 | ||
| Uninsured | 26.8 | 38.6 | 24.3 | 28.2 | 24.6 | ||
1AANHPI/Other refers to a combined Asian, Alaskan Native/Native American, Native Hawaiian/Pacific Islander, and Other racial/ethnic group.
2.5. Statistical analysis
We used bivariate statistics to assess variation in outcomes by exposure and covariates as well as racial/ethnic differences in analytic variables. We ran multivariable regression models to estimate adjusted associations between public housing residence and health care utilization, controlling for covariates above. Because differences in the social context of racial/ethnic groups produces differences in access to and representation across public housing sites, we estimated race/ethnicity specific findings. Poisson link functions were used to estimate associations for count-based outcomes and logistic link functions were used for dichotomous outcomes. We ran all analyses overall and by each public housing site and its comparison area (referred to as “public housing site study area” going forward). In overall comparisons, women were only included once, but given that census tracts could be adjacent to more than one public housing census tract, women could be included in more than one public housing site study area. In order to preserve anonymity of specific sites and the residents living in them, sites are referred to as sites A-F. Statistical significance for main associations was assessed as alpha < 0.05. All analyses were run in Stata 15 (StataCorp, College Station, TX).
3. Results
Our population was majority Black (33.8%), Latina (32.9%), and AANHPI/Other (25.4%) women (Table 1). Overall, 19.7% of our sample lived in public housing, and this varied across racial/ethnic groups. Black women had the highest prevalence of residing in public housing (35.9%) and Latina women (6.8%) had the lowest. The mean age was 26.5 years (SD = 8.3), and this also varied by racial/ethnic group. A higher proportion of White women were older than 30y. Finally, the majority of women were publicly insured (70.5%) with 26.8% being uninsured. This varied by race/ethnicity, with a higher proportion of White women (38.6%) being uninsured.
Health care utilization varied by race/ethnicity. On average, women had 4.8 (SD = 5.3) outpatient visits annually and over one quarter (26.2%) visited the ED. White women (3.8; SD = 4.4) had fewer outpatient visits than Black (4.3; SD = 4.7), Latina (5.8; SD = 6.1), and AANHPI/Other women (4.7; SD = 5.1). ED visits were highest among White (32.8%) and Black women (31.1%), with slightly over twenty percent of Latina (21.4%) or AANHPI/Other women (23.8%) reporting at least one ED visit over the year.
Racial/ethnic composition varied across housing site specific study areas (Table 2). Sites C, E and F had higher proportions of Latina women, site B had higher proportions of AANHPI/Other women, and site A was predominantly Black. The prevalence of public housing exposure varied from 5.1 to 32.5% across housing site areas, but the mean number of outpatient visits (4.7[SD = 5.1] to 5.1[SD = 5.7]) and prevalence of ED visits (23.2–28.6%) did not vary much by public housing site. Most women were publicly insured with the uninsured rate ranging from 23.8 to 32.1%.
Table 2.
Distribution of Analytic Variables for each Public Housing Site and its Surrounding Study Area.
| Public Housing Site A (n = 1199) | Public Housing Site B (n = 1393) | Public Housing Site C (n = 935) | Public Housing Site D (n = 1198) | Public Housing Site E (n = 634) | Public Housing Site F (n = 624) | ||
|---|---|---|---|---|---|---|---|
| Housing Type, % | |||||||
| Non-Public Housing | 92.2 | 75.9 | 67.5 | 86.5 | 89.0 | 94.9 | |
| Public Housing | 7.8 | 24.1 | 32.5 | 13.5 | 11.0 | 5.1 | |
| Visit Count, mean (SD) | |||||||
| Outpatient | 4.7(5.1) | 5.0 (5.4) | 4.6 (5.1) | 5.1 (5.7) | 4.8 (5.2) | 4.8 (5.1) | |
| Emergency Department | 0.4 (0.7) | 0.4 (0.7) | 0.4 (1.0) | 0.3 (0.7) | 0.3 (0.6) | 0.3 (0.6) | |
| One or more ED visit, % | 27.1 | 25.7 | 28.6 | 23.9 | 23.2 | 25.0 | |
| Race/Ethnicity, % | |||||||
| White | 3.5 | 4.6 | 18.4 | 3.0 | 9.8 | 15.1 | |
| Black | 57.3 | 31 | 26.3 | 37.4 | 12.5 | 7.2 | |
| Latina | 25.9 | 28.3 | 36.4 | 36 | 43.7 | 55.9 | |
| AANHPI/ Other | 13.4 | 36.1 | 18.8 | 24.1 | 34 | 21.8 | |
| Age, mean (SD) | 25.5 (8.3) | 26.0 (8.3) | 27.9 (8.1) | 26.0 (8.4) | 27.3 (8.5) | 27.6 (8.1) | |
| Age Category, % | |||||||
| 15–19 | 30.4 | 27.4 | 18.7 | 29.2 | 23.7 | 19.7 | |
| 20–24 | 21.0 | 21.8 | 18.8 | 19.4 | 18.4 | 20.0 | |
| 25–29 | 17.1 | 16.7 | 20.8 | 17.0 | 16.7 | 20.4 | |
| 30–34 | 12.8 | 14.9 | 16.1 | 13.9 | 16.7 | 14.7 | |
| 35–39 | 11.09 | 10.7 | 15.6 | 12.3 | 13.9 | 16.7 | |
| 40–44 | 7.5 | 8.5 | 10.0 | 8.2 | 10.6 | 8.5 | |
| Insurance Type, % | |||||||
| Medi-Cal | 35.4 | 33.2 | 31.8 | 34.9 | 28.6 | 29.8 | |
| Other Public | 36.4 | 40.1 | 34.9 | 36.1 | 40.5 | 37.0 | |
| Commercial | 2.2 | 2.9 | 3.8 | 2.9 | 2.0 | 1.1 | |
| Uninsured | 26.0 | 23.8 | 29.5 | 26.1 | 28.9 | 32.1 | |
1AANHPI/Other refers to a combined Asian, Alaskan Native/Native American, Native Hawaiian/Pacific Islander, and Other racial/ethnic group.
Table 3 shows results from multivariable models overall and stratified by public housing site study area. Public housing was consistently associated with health care utilization only among AANHPI/Other women. In the overall model, AANHPI/Other women residing in public housing had fewer outpatient visits (IRR = 0.86; 95% CI = 0.81,0.93) than non-public housing residents. This association varied across public housing site study areas. For all but three sites (sites B, C and E), AANHPI/Other women who resided in public housing had fewer outpatient visits compared to their counterparts living in non-public housing. In site E, women who resided in public housing had more outpatient visits than their non-publicly housed counterparts; in sites B and C, there was no association.
Table 3.
Associations from multivariable models by Race/Ethnicity; point estimates in bold are significant and point estimates in italics are borderline significant.
| Outpatient | Emergency Department1 | ||||||
|---|---|---|---|---|---|---|---|
| IRR | 95% CI | OR | 95% CI | ||||
| All Public Housing Sites (n = 5,067) | |||||||
| Non-Public Housing | ref. | ref. | ref. | ref. | ref. | ref. | |
| Public Housing | |||||||
| Black | 1.02 | 0.97 | 1.07 | 1.32 | 1.07 | 1.63 | |
| White | 1.00 | 0.84 | 1.19 | 0.89 | 0.41 | 1.94 | |
| Latina | 1.02 | 0.94 | 1.10 | 1.43 | 0.92 | 2.22 | |
| AANHPI/Other2 | 0.86 | 0.81 | 0.93 | 1.81 | 1.32 | 2.48 | |
| Public Housing Site A (n = 1198) | |||||||
| Non-Public Housing | ref. | ref. | ref. | ref. | ref. | ref. | |
| Public Housing | |||||||
| Black | 1.05 | 0.92 | 1.20 | 0.84 | 0.43 | 1.61 | |
| White | 1.53 | 0.90 | 2.59 | – | – | – | |
| Latina | 0.88 | 0.66 | 1.17 | 1.24 | 0.24 | 6.41 | |
| AANHPI/Other2 | 0.56 | 0.45 | 0.70 | 2.58 | 1.11 | 5.98 | |
| Public Housing Site B (n = 1391) | |||||||
| Non-Public Housing | ref. | ref. | ref. | ref. | ref. | ref. | |
| Public Housing | |||||||
| Black | 1.03 | 0.94 | 1.12 | 1.38 | 0.91 | 2.09 | |
| White | 0.89 | 0.64 | 1.25 | 0.48 | 0.09 | 2.64 | |
| Latina | 1.02 | 0.89 | 1.16 | 1.97 | 0.92 | 4.23 | |
| AANHPI/Other2 | 0.99 | 0.89 | 1.10 | 1.82 | 1.11 | 3.00 | |
| Public Housing Site C (n = 934) | |||||||
| Non-Public Housing | ref. | ref. | ref. | ref. | ref. | ref. | |
| Public Housing | |||||||
| Black | 0.91 | 0.79 | 1.06 | 2.34 | 1.12 | 4.88 | |
| White | 1.23 | 0.92 | 1.64 | 0.97 | 0.28 | 3.35 | |
| Latina | 0.91 | 0.78 | 1.06 | 1.41 | 0.65 | 3.07 | |
| AANHPI/Other2 | 0.91 | 0.78 | 1.07 | 1.30 | 0.64 | 2.66 | |
| Public Housing Site D (n = 1195) | |||||||
| Non-Public Housing | ref. | ref. | ref. | ref. | ref. | ref. | |
| Public Housing | |||||||
| Black | 1.05 | 0.95 | 1.16 | 1.01 | 0.62 | 1.63 | |
| White | 0.32 | 0.16 | 0.66 | 2.65 | 0.37 | 18.73 | |
| Latina | 0.81 | 0.62 | 1.06 | 0.43 | 0.05 | 3.44 | |
| AANHPI/Other2 | 0.66 | 0.54 | 0.80 | 0.87 | 0.34 | 2.23 | |
| Public Housing Site E (n = 632) | |||||||
| Non-Public Housing | ref. | ref. | ref. | ref. | ref. | ref. | |
| Public Housing | |||||||
| Black | 0.85 | 0.69 | 1.05 | 1.13 | 0.42 | 3.03 | |
| White: | 0.66 | 0.27 | 1.61 | – | – | – | |
| Latina | 1.08 | 0.85 | 1.37 | 1.98 | 0.63 | 6.18 | |
| AANHPI/Other2 | 2.18 | 1.71 | 2.78 | 4.13 | 0.96 | 17.74 | |
| Public Housing Site F (n = 624) | |||||||
| Non-Public Housing | ref. | ref. | ref. | ref. | ref. | ref. | |
| Public Housing | |||||||
| Black | 1.04 | 0.75 | 1.44 | 0.73 | 0.16 | 3.28 | |
| White | 1.17 | 0.73 | 1.86 | 0.84 | 0.08 | 8.73 | |
| Latina | 2.92 | 2.19 | 3.91 | 2.03 | 0.18 | 23.33 | |
| AANHPI/Other2 | 0.68 | 0.49 | 0.95 | 3.08 | 0.86 | 11.02 | |
Point estimates for Emergency Department (ED) visits among White women are excluded due to small sample size introducing instability in estimation.
AANHPI/Other refers to a combined Asian, Alaskan Native/Native American, Native Hawaiian/Pacific Islander, and Other racial/ethnic group.
For ED visits, residing in public housing increased the odds of an ED visit among AANHPI/Other women as well as Black women in the overall model. Across public housing site study areas, this association held for AANHPI/Other women in sites A and B. However, for Black women, only those residing in public housing at site C had higher odds of an ED visit.
4. Discussion
We assessed associations between public housing and health care utilization for women of reproductive age across six public housing sites. Within most racial/ethnic groups, public housing residents and their non-publicly housed counterparts had similar patterns of outpatient and ED visits. Among AANHPI/Other women, however, we observed associations across multiple public housing sites, with public housing residents largely having fewer outpatient visits and more ED visits compared to non-publicly housed counterparts. Among Black women, there was an indication that public housing residents had increased odds of ED visits compared to non-publicly housed counterparts, but this was driven by one public housing site. Our findings suggest that more comprehensive consideration of variability across public housing sites and by race/ethnicity is important for better understanding public housing as a social determinant of health care utilization among women of reproductive age.
Our findings add to a sparse literature with mixed findings. Researchers using data from the Boston Behavioral Risk Factor Surveillance Survey found that health care utilization for public housing residents matched that of their non-publicly housed counterparts.(Digenis-Bury et al., 2008) Similarly, researchers in New York using Medicaid data found that changes in health system utilization prior to and after move-in did not differ for renovated versus non-renovated public housing, although they did not additionally compare to non-publicly housed residents.(Ellen et al., 2020) Alternatively, researchers in Manitoba, Canada found that those moving into public housing had higher health care utilization compared to non-publicly housed counterparts.(Hinds et al., 2019) Heterogeneous findings may be due to differences in geographic locations, but direct comparison with our findings is difficult given that studies did not focus on women of reproductive age. More research is needed to better understand health care utilization during this period, especially given that health care utilization contributes to prevention or management of preconception health outcomes.(Johnson et al., 2015).
Our findings suggested that differences in health care utilization were most consistent among women in the AANHPI/Other group. However, this group is quite heterogeneous. For example, within the NHPI subgroup, a large Samoan population resides in San Francisco public housing.(Hagan et al., 2020) Literature has shown that both within and across ethnic subgroups there is variation in health outcomes due to differences in the sociopolitical contexts that groups occupy.(Gee et al., 2009, Hagan et al., 2020) More robust investigation is needed in samples intentionally designed to address sample size issues across racial/ethnic subgroups in order to better understand implications of findings within this AANHPI/Other group.
Additionally, associations varied across public housing site. In particular, the higher odds of ED visits among publicly housed Black women was mainly driven by public housing site study area C. Among AANHPI/Other women, three sites suggested lower rates, one site suggested higher rates, and two sites suggested equal rates of outpatient visits among publicly housed residents compared to non-publicly housed counterparts. This variation indicates that public housing site specific characteristics may be important to consider in research going forward. Findings from the qualitative arm of the mixed method study from which these data were obtained provide potential insight into mechanisms driving this variation.(Hagan et al., 2020) Interviews at two public housing sites emphasized that services available to residents were often not targeted to their needs in socially and geographically accessible ways. (Hagan et al., 2020) Such disconnects may partially drive differences in health care utilization in public housing sites where outpatient visits are lower or emergency department visits are higher, although further research is needed to fully elucidate these nuances. Alternatively, residents described rich and tight-knit social networks that formed in response to disconnected resource access, through which they obtained other forms of resource, such as food and childcare. (Hagan et al., 2020) If such networks also can provide resources that facilitate utilization of health care, such as transportation, then this could be a mechanism that is amplified at sites where health care utilization patterns are similar between publicly housed and non-publicly housed residents. Going forward, further mixed methods studies, especially among women of reproductive age, will aid in better understanding factors underlying variation across sites in associations between public housing and health care utilization.
5. Limitations:
Our study has a few limitations to consider. First, residual confounding due to incomplete measurement of socioeconomic status may bias our findings. Socioeconomic status is a multidimensional measure and we were limited to using health insurance type as a proxy for this measure.(Braveman et al., 2010) While this remains a challenge of research using EHR, we additionally restricted to neighborhoods surrounding public housing sites which may partially mitigate potential bias.(Williams and Collins, 2001) Second, we were not able to control for women’s health status, such as depressive symptoms or chronic conditions, at baseline given that EHR records were limited to visit characteristics only. Some literature suggests that individuals in public housing are sicker than comparable populations and health status may select individuals into public housing.(Biederman et al., 2022, Hinds et al., 2019, Hinds et al., 2018, Hinds et al., 2016) However, other studies indicate that differences in health care utilization persist after adjusting for baseline health status,(Digenis-Bury et al., 2008, Hinds et al., 2019, Hinds et al., 2018) although we were not able to assess this in our study. Nonetheless, more research is needed to robustly understand implications for bias. Third, we only included those who remained at one address for the duration of follow up and had at least two visits at that address. Low-income populations can be highly mobile(Newman, 2008, Swope and Hernández, 2019) and indeed, we excluded around 8.9% percent of women because of a non-stable address. Mobility may impact health care utilization, especially if public housing residents are more likely to stay within the public housing system rather than have to navigate traditional housing markets. This relates to another limitation; we were not able to identify individuals with other types of housing assistance, such as Section 8. This would have improved our understanding of mobility patterns for publicly and non-publicly housed women of reproductive age.
These limitations are balanced by several strengths. First, we included health records from two health networks that captured a broad health care context, including neighborhood clinics and large hospitals. Second, our ability to compare to socially, structurally, and spatially comparable populations is important because it allows us to account, to some extent, for potential unmeasured factors driving differences in publicly housed and non-publicly housed individuals’ health care utilization. In particular, low-income women who are not publicly housed are often exposed to similar neighborhood environments that present similar challenges to accessing and using health care.(Williams and Collins, 2001) Finally, few studies have focused on public housing and health care utilization among women of reproductive age and additionally assessed racial/ethnic variation in associations, which our findings indicate are important to consider.
6. Conclusion
Understanding mechanisms driving health care utilization among women of reproductive age has important implications for lifetime and generational health trajectories. Our findings suggest that the role of public housing is nuanced and further research is needed to better understand how it operates within the context of housing and health in this socially vulnerable population. In particular, while our findings suggest that public housing is consistently associated with health care utilization for women in the AANHPI/Other group, comprehensive consideration of variation across sites and by racial/ethnic group is needed to better identify mechanisms driving heterogeneity in associations. This is important as health care systems increasingly find ways to incorporate the social and structural determinants of health in their provision of care (Gottlieb et al., 2015, Sandel and Desmond, 2017) in order to ensure that effective approaches to action can be developed to positively impact women’s reproductive health care utilization and long-term health trajectories.
CRediT authorship contribution statement
Irene E. Headen: Conceptualization, Methodology, Formal analysis, Writing – original draft, Writing – review & editing. Leslie Dubbin: Investigation, Resources, Writing – review & editing, Supervision, Funding acquisition. Alison J. Canchola: Formal analysis, Data curation, Writing – review & editing. Ellen Kersten: Formal analysis, Data curation, Writing – review & editing. Irene H. Yen: Investigation, Resources, Writing – original draft, Writing – review & editing, Supervision, Funding acquisition.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
This work was supported by the Robert Wood Johnson Foundation [grant number 74080]. The Robert Wood Johnson Foundation had no involvement in any of the research and/or preparation of this article. No financial disclosures were reported by the authors of this paper. IEH was involved in conceptualization, methodology, formal analysis, data curation, writing, reviewing, and editing. IHY and LD were involved in funding acquisition, project administration, investigation, methodology, writing, reviewing, and editing. EK was involved in data curation, investigation, review and editing of the manuscript. AJC was involved in data curation, methodology, review and editing of the manuscript. An early version of the contents of this manuscript were presented as part of a webinar for the Society of Pediatric and Perinatal Research entitled “Social and structural determinants of pregnancy health.”
Conflict of Interest and Financial Disclosure: Funding for the study was provided through Robert wood Johnson Foundation (RWJF), Grant Number 74080. RWJF did not have any role in the study design, data collection, analysis, interpretation of data, writing the report, or the decision to submit the report for publication. No financial disclosures were reported by the authors of this paper.
REFERENCES
- Antonakos C.L., Colabianchi N. Impact of Rental Assistance on Modifiable Health Risk Factors and Behaviors in Adults. Cityscape. 2018;20:133. [PMC free article] [PubMed] [Google Scholar]
- Baker E., Beer A., Lester L., Pevalin D., Whitehead C., Bentley R. Is Housing a Health Insult? IJERPH. 2017;14:567. doi: 10.3390/ijerph14060567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman D.J., Callejo-Black P., Douglas C., O’Donohue H.A., Daeges M., Sofela O., Brown A. Changes in health and health care utilization following eviction from public housing. Public Health Nursing. 2022;39:363–371. doi: 10.1111/phn.12964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolton M., Bravve E. Housing Spotlight: Who lives in federally assisted housing? Housing Spotlight. 2012;2:1–5. [Google Scholar]
- Braveman P.A., Cubbin C., Egerter S., Williams D.R., Pamuk E. Socioeconomic Disparities in Health in the United States: What the Patterns Tell Us. Am J Public Health. 2010;100:S186–S196. doi: 10.2105/AJPH.2009.166082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caswell K.J., Zuckerman S. Urban Institute; Washington, DC: 2018. Food Insecurity, Housing Hardship, and Medical Care Utilization (Research Report) [Google Scholar]
- Census Bureau Glossary, 2019. . United States Census Bureau.
- Cunningham A., Mautner D., Ku B., Scott K., LaNoue M. Frequent emergency department visitors are frequent primary care visitors and report unmet primary care needs: Frequent ED Visitors Report Unmet Primary Care Needs. J Eval Clin Pract. 2017;23(3):567–573. doi: 10.1111/jep.12672. [DOI] [PubMed] [Google Scholar]
- Digenis-Bury E.C., Brooks D.R., Chen L., Ostrem M., Horsburgh C.R. Use of a Population-Based Survey to Describe the Health of Boston Public Housing Residents. Am J Public Health. 2008;98:85–91. doi: 10.2105/AJPH.2006.094912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubbin L., Neufeld S., Kersten E., Yen I.H. Health Effects After Renovation (HEAR) Study: Community-Engaged Inquiry Into the Health and Social Impacts of the Rental Assistance Demonstration Program Implementation in San Francisco. Housing Policy Debate. 2019;29:432–439. doi: 10.1080/10511482.2018.1530273. [DOI] [Google Scholar]
- Dunn J.R. Housing and Health Inequalities: Review and Prospects for Research. Housing Studies. 2000;15:341–366. doi: 10.1080/02673030050009221. [DOI] [Google Scholar]
- Dunn J.R., Hayes M.V., Hulchanski J.D., Hwang S.W., Potvin L. Housing as a Socio-Economic Determinant of Health: Findings of a National Needs, Gaps and Opportunities Assessment. Canadian Journal of Public Health / Revue Canadienne de Santé Publique. 2006;97:S11–S15. [PubMed] [Google Scholar]
- Ellen I.G., Dragan K.L., Glied S. Renovating Subsidized Housing: The Impact On Tenants’ Health: An evaluation of whether public housing renovations and the transfer of ownership to a public-private partnership led to improvements in tenants’ health as measured by Medicaid claims. Health Affairs. 2020;39:224–232. doi: 10.1377/hlthaff.2019.00767. [DOI] [PubMed] [Google Scholar]
- Fenelon A., Mayne P., Simon A.E., Rossen L.M., Helms V., Lloyd P., Sperling J., Steffen B.L. Housing Assistance Programs and Adult Health in the United States. Am J Public Health. 2017;107:571–578. doi: 10.2105/AJPH.2016.303649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fertig A.R., Reingold D.A. Public housing, health, and health behaviors: Is there a connection? J. Pol. Anal. Manage. 2007;26:831–860. doi: 10.1002/pam.20288. [DOI] [PubMed] [Google Scholar]
- Gee G.C., Ro A., Shariff-Marco S., Chae D. Racial Discrimination and Health Among Asian Americans: Evidence, Assessment, and Directions for Future Research. Epidemiologic Reviews. 2009;31:130–151. doi: 10.1093/epirev/mxp009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlieb L.M., Tirozzi K.J., Manchanda R., Burns A.R., Sandel M.T. Moving Electronic Medical Records Upstream. American Journal of Preventive Medicine. 2015;48:215–218. doi: 10.1016/j.amepre.2014.07.009. [DOI] [PubMed] [Google Scholar]
- Hagan M.J., Hall A.R., Mamo L., Ramos J., Dubbin L. Homeplace: Care and resistance among public housing residents facing mixed-income redevelopment. American Journal of Orthopsychiatry. 2020;90:523–534. doi: 10.1037/ort0000452. [DOI] [PubMed] [Google Scholar]
- Hall K.S., Dalton V., Johnson T.R.B. Social disparities in women’s health service use in the United States: a population-based analysis. Annals of Epidemiology. 2014;24:135–143. doi: 10.1016/j.annepidem.2013.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinrich K.M., Lee R.E., Regan G.R., Reese-Smith J.Y., Howard H.H., Haddock C.K., Poston W.S.C., Ahluwalia J.S. How Does the Built Environment Relate to Body Mass Index and Obesity Prevalence among Public Housing Residents? Am J Health Promot. 2008;22:187–194. doi: 10.4278/ajhp.22.3.187. [DOI] [PubMed] [Google Scholar]
- Hernández D., Swope C.B. Housing as a Platform for Health and Equity: Evidence and Future Directions. Am J Public Health. 2019;109:1363–1366. doi: 10.2105/AJPH.2019.305210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinds A.M., Bechtel B., Distasio J., Roos L.L., Lix L.M. Public housing and healthcare use: an investigation using linked administrative data. Can J Public Health. 2019;110:127–138. doi: 10.17269/s41997-018-0162-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinds A.M., Bechtel B., Distasio J., Roos L.L., Lix L.M. Changes in healthcare use among individuals who move into public housing: a population-based investigation. BMC Health Serv Res. 2018;18:411. doi: 10.1186/s12913-018-3109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinds A.M., Bechtel B., Distasio J., Roos L.L., Lix L.M. Health and social predictors of applications to public housing: a population-based analysis. J Epidemiol Community Health. 2016;70:1229–1235. doi: 10.1136/jech-2015-206845. [DOI] [PubMed] [Google Scholar]
- Johnson K., Balluff M., Abresch C., Verbiest S., Atrash H. CityMatCH; Omaha, NE: 2015. Summary of Findings from the Reconvened Select Panel on Preconception Health and Health Care. [Google Scholar]
- Kane J.B., Margerison-Zilko C. Theoretical Insights into Preconception Social Conditions and Perinatal Health: The Role of Place and Social Relationships. Popul Res Policy Rev. 2017;36:639–669. doi: 10.1007/s11113-017-9430-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kersten E.E., Adler N.E., Gottlieb L., Jutte D.P., Robinson S., Roundfield K., LeWinn K.Z. Neighborhood Child Opportunity and Individual-Level Pediatric Acute Care Use and Diagnoses. Pediatrics. 2018;141 doi: 10.1542/peds.2017-2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer M.R., Waller L.A., Dunlop A.L., Hogue C.R. Housing Transitions and Low Birth Weight Among Low-Income Women: Longitudinal Study of the Perinatal Consequences of Changing Public Housing Policy. Am J Public Health. 2012;102:2255–2261. doi: 10.2105/AJPH.2012.300782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger J., Higgins D.L. Housing and Health: Time Again for Public Health Action. Am J Public Health. 2002;92:758–768. doi: 10.2105/AJPH.92.5.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim S., Liu S.Y.(., Jacobson M.H., Poirot E., Crossa A., Locke S., Brite J., Hamby E., Bailey Z., Farquhar S. Housing stability and diabetes among people living in New York city public housing. SSM - Population Health. 2020;11:100605. doi: 10.1016/j.ssmph.2020.100605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margerison C.E., MacCallum C.L., Chen J., Zamani-Hank Y., Kaestner R. Impacts of Medicaid Expansion on Health Among Women of Reproductive Age. American Journal of Preventive Medicine. 2020;58(1):1–11. doi: 10.1016/j.amepre.2019.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason L. San Francisco Housing Authority; San Francisco, CA: 2022. Housing Authority of the City and County of San Francisco: Five Year Plan Fiscal Year 2022–2027 Annual Plan Fiscal Year 2022. [Google Scholar]
- Newman S.J. Does housing matter for poor families? A critical summary of research and issues still to be resolved: Policy Retrospectives. J. Pol. Anal. Manage. 2008;27:895–925. doi: 10.1002/pam.20381. [DOI] [Google Scholar]
- Potter J., Trussell J., Moreau C. Trends and determinants of reproductive health service use among young women in the USA. Human Reproduction. 2009;24:3010–3018. doi: 10.1093/humrep/dep333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Public Housing Task Force . Mayor’s Office; San Francisco, CA: 2007. HOPE SF: Rebuilding Public Housing and Restoring Opportunity for its Residents. Summary of Task Force Recommendations to the Mayor and Board of Supervisors. [Google Scholar]
- Rahaim, J., Rodgers, A., Switzky, J., Ojeda, T., Peterson, P., Pappas, J., Ambati, S., Dow, P., Chen, G., 2018. San Francisco Housing Needs and Trends Report (Final Report). San Francisco Planning Department.
- San Francisco Health Improvement Partnership . San Francisco Department of Public Health; Population Health Division, San Francisco, CA: 2016. San Francisco Community Health Needs Assessment 2016. [Google Scholar]
- San Francisco Planning Department . San Francisco Planning Department; San Francisco, CA: 2020. San Francisco Housing Affordability Strategies (Final Report) [Google Scholar]
- Sandel M., Desmond M. Investing in Housing for Health Improves Both Mission and Margin. JAMA. 2017;318:2291. doi: 10.1001/jama.2017.15771. [DOI] [PubMed] [Google Scholar]
- Slopen N., Fenelon A., Newman S., Boudreaux M. Housing Assistance and Child Health: A Systematic Review. Pediatrics. 2018;141 doi: 10.1542/peds.2017-2742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swope C.B., Hernández D. Housing as a determinant of health equity: A conceptual model. Social Science & Medicine. 2019;243 doi: 10.1016/j.socscimed.2019.112571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilensky S., Proser M. Community Approaches to Women's Health. Women's Health Issues. 2008;18(6):S52–S60. doi: 10.1016/j.whi.2008.06.007. [DOI] [PubMed] [Google Scholar]
- Williams D.R., Collins C. Racial Residential Segregation: A Fundamental Cause of Racial Disparities in Health. PUBLIC HEALTH REPORTS. 2001;116(5):404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2017. Sexual health and its linkages to reproductive health: an operational approach. [Google Scholar]