The 2018-19 global measles resurgence was the largest measles epidemic in over two decades and prompted calls for the declaration of a Public Health Emergency of International Concern. The enormous number of measles cases with global spread and ensuing deaths was characterised as “an extraordinary event that may constitute a public health risk to other countries through international spread of disease and may require an international coordinated response.”1 However, this momentous epidemic was soon overshadowed as the world wrestled with the immense threat posed by the COVID-19 pandemic.
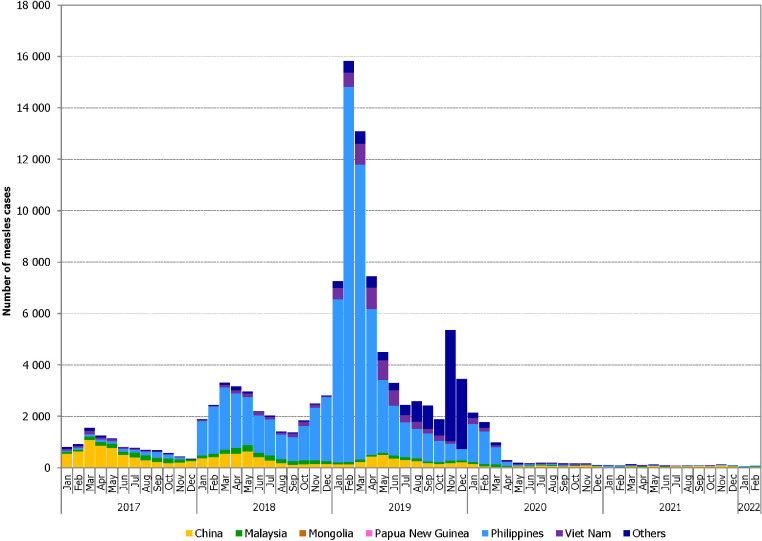
COVID-19 mitigation and response measures had a profound effect on reducing the spread of other infectious agents, including measles virus. Reported measles cases in the Western Pacific Region (WPR) dropped to historically low levels due to the unparalleled restrictions on international travel and other non-pharmaceutical public health measures, which stemmed the flow of cross-border measles importations and smothered in-country measles transmission (Figure 1).2 While the pandemic and response has negatively affected measles surveillance quality, this only partially accounts for the enormous decrease in reported cases. The current lull in measles transmission is a welcome reprieve from the 2018-2019 resurgence. However, the low levels of transmission may result in fewer individuals with immunity from measles infections, and in the absence of vaccination, could lead to an accumulation of susceptibility.
Figure 1.
Total (confirmed and compatible) measles cases by selected country and month of rash onset, WHO Western Pacific Region, 2017–2022 (as of 20 March 2022).
Unfortunately, the COVID-19 pandemic had concurrent detrimental impacts on childhood vaccination programs. In May 2020, 66 countries had postponed immunisation campaigns which are essential for maintaining high levels of population immunity in low- and middle-income countries. As of January 2022, vaccination campaigns were postponed in 37 countries.3 Despite intense efforts to reboot routine immunisation in the latter part of 2020, first-dose measles-containing vaccine coverage dropped globally from 86% in 2019 to 84% in 2020, representing about 3 million fewer children protected.4 Measles’ high transmissibility demands at least 95% coverage with two measles-containing vaccine doses in each birth cohort to achieve elimination.5 Sub-optimal historical first and second dose coverage, COVID-19 related coverage decreases, delays in campaigns to fill coverage gaps and current low measles incidence all combine to generate rapid accumulation of population susceptibility to measles. The relaxation of COVID-19 response measures in the face of increasing measles susceptibility provides “perfect storm” conditions. Recent outbreaks in several regions suggest that the next global measles pandemic is on the horizon unless this calm between the storms is seized to re-energise measles elimination efforts.6
An inspiring regional model of achieving and sustaining measles elimination is urgently needed. All WHO Regions need to move beyond simply endorsing elimination feasibility and nominating target dates while tolerating underwhelming and erratic progress.7 No Region has yet achieved and sustained measles elimination. Although the Americas achieved measles elimination verification in 2016, endemic measles transmission was re-established in Venezuela during 2016 and Brazil during 2018. Since 2016, endemic transmission has been re-established in nine other countries that had previously eliminated measles in the European and Western Pacific Regions (Albania, Cambodia, Czechia, Germany, Lithuania, Mongolia, Slovakia, the United Kingdom, and Uzbekistan).8 The WPR is well-positioned to be that inspiring regional model. The 16 national verification committees and one sub-regional verification committee (covering the 21 Pacific Island Countries and Areas) annually provide comprehensive reports documenting their steady progress towards elimination across the five lines of evidence (measles epidemiology, quality of epidemiological and laboratory surveillance, population immunity, vaccination program sustainability, and genotyping data).9 Six countries and two special administrative regions (SAR) have achieved and maintained measles elimination: Australia, Macao SAR, Republic of Korea, since 2014; Brunei Darussalam, Japan since 2015; Hong Kong SAR since 2016; New Zealand since 2017; and Singapore since 2018.
Measles genotyping provides further compelling evidence of progress toward measles elimination in WPR. Globally the number of measles genotypes decreased from 13 in 2002 to just three in 2020; B3, D4 and D8.8 Of note, the H1 genotype, which was historically endemic in China and other WPR countries, was last detected globally in China during July 2019.9
There have been bold WPR country initiatives during the COVID-19 pandemic, notably a national campaign in the Philippines during 2020-2021 which achieved unprecedented coverage with measles-rubella containing vaccine.9 This success is particularly pertinent given the Philippines's major contribution to international seeding of genotype B3 measles during 2018-2019.9
To achieve measles elimination all WPR countries must reinvigorate routine immunization programs, rebuild confidence in vaccination to counter vaccine hesitancy, prioritise “catch-up” campaigns, ensure appropriate infection control to keep families and vaccinators safe from COVID-19, respond effectively to measles outbreaks, re-establish high functioning surveillance including laboratory, and capitalise on new surveillance and vaccine delivery tools accelerated by the COVID-19 pandemic.6 Strategically implementing these key measures using measles-rubella containing vaccines has the potential of concurrent rubella elimination.10 Regional measles and rubella elimination requires every country to be a strong link in the elimination program chain. No country, and no child, should be left behind!
Declaration of interests
The authors have no conflicts of interest to declare.
Acknowledgement
We are grateful to Dr Jeffrey McFarland, former RVC member for his review and suggestions.
References
- 1.Durrheim DN, Crowcroft NS, Blumberg LH. Is the global measles resurgence a “Public Health Emergency of International Concern”? Int J Infect Dis. 2019;83:95–97. doi: 10.1016/j.ijid.2019.04.016. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization Regional Office for the Western Pacific. Measles-Rubella Bulletin. 2022 https://apps.who.int/iris/handle/10665/352587 Vol-16-No-03. WHO Regional Office for the Western Pacific. [Google Scholar]
- 3.World Health Organization. Highlights from the meeting of the Strategic Advisory Group of Experts (SAGE) on Immunization, 4-7 April 2022.https://cdn.who.int/media/docs/default-source/immunization/sage/sage-pages/sage_april2022meetinghighlights_11apr2022_final.pdf?sfvrsn=c2bd9f68_1. Accessed 13 April 2022
- 4.Maltezou HC, Medic S, Cassimos DC, Effraimidou E, Poland GA. Decreasing routine vaccination rates in children in the COVID-19 era. Vaccine. 2022;40:2525–2527. doi: 10.1016/j.vaccine.2022.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hübschen JM, Gouandjika-Vasilache I, Dina J. Measles. Lancet. 2022;399:678–690. doi: 10.1016/S0140-6736(21)02004-3. [DOI] [PubMed] [Google Scholar]
- 6.Durrheim DN, Andrus JK, Tabassum S, et al. A dangerous measles future looms beyond the COVID-19 pandemic. Nat Med. 2021;27:360–361. doi: 10.1038/s41591-021-01237-5. [DOI] [PubMed] [Google Scholar]
- 7.Durrheim DN. Measles eradication – retreating is not an option. Lancet Infect Dis. 2020;20:138–141. doi: 10.1016/S1473-3099(20)30052-9. [DOI] [PubMed] [Google Scholar]
- 8.Dixon MG, Ferrari M, Antoni S, et al. Progress toward Regional Measles Elimination — Worldwide, 2000–2020. MMWR Morb Mortal Wkly Rep. 2021;70:1563–1569. doi: 10.15585/mmwr.mm7045a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Ninth annual meeting of the Regional Verification Commission for measles and rubella elimination in the Western Pacific, 17-21 May 2021.https://apps.who.int/iris/bits tream/handle/10665/344160/RS-2021-GE-13-virtual-eng.pdf?sequence=1. Accessed 13 April 2022
- 10.Winter AK, Moss WJ. Rubella. Lancet. 2022;399:1336–1346. doi: 10.1016/S0140-6736(21)02691-X. [DOI] [PubMed] [Google Scholar]