Abstract
Addressing sleep disturbance can help to slow functional decline, delay nursing home admission, and improve overall health among older adults; however, sleep is not widely studied in high-risk older adults such as Adult Day Health Care (ADHC) participants. Sixty-eight ADHC participants were interviewed for sleep disturbance using a 28-item screening questionnaire. More than two thirds (n = 48, 70.6%) reported one or more characteristics of poor sleep, and 38% of participants met basic criteria for insomnia. Individuals with insomnia attended ADHC less frequently, reported worse sleep quality and shorter sleep duration, and were more likely to endorse trouble falling asleep, staying asleep, and waking up too early (ps < 0.001). Research is needed to better understand perceptions, predictors, and outcomes of sleep disturbance within ADHC participants.
Veterans Affairs (VA) Adult Day Health Care (ADHC) programs are designed to assist in activities of daily living, provide ongoing support in managing chronic diseases, and promote regular social and physical activity among older Veterans in need of such care (Veterans Health Administration, 2009). The ultimate goal of such programs is to slow further decline and disability, delay or prevent nursing home placement, and improve overall health outcomes (Gaugler & Zarit, 2001; Office of Public Affairs and Media Relations, 2005). Within VA ADHC, group-based health behavior education is provided by an interdisciplinary team of health care providers and is a central component to ADHC programming, typically focusing on diet, exercise, and medication management (Baumgarten, Level, Laprise, Leclerc, & Quinn, 2002). While healthy sleep is thought to be an essential component in promoting recovery and rehabilitation, maintaining functional independence, optimizing quality of life, and delaying institutionalization in older adults (Alessi et al., 2008; Foley et al., 1995; Schmitt, Sands, Weiss, Dowling, & Covinsky, 2010), it is not included as a core component of VA ADHC programming (Rivero, Hughes, Kramer, & Martin, 2012; Veterans Health Administration, 2009).
More than half of U.S. adults aged 65 and older report chronic sleep disturbance (Foley et al., 1995), and sleep naturally changes with age as a result of various neurological, physical, and hormonal changes associated with aging. Sleep complaints and poor health are believed to operate in a bidirectional fashion such that poor sleep negatively impacts normal, healthy aging; as health declines, sleep is disrupted, and this negatively affects overall health and begins the cycle anew (Cochen et al., 2009). In addition to increased comorbidities and medication use causing poor sleep, factors such as irregular postretirement sleep schedules, a reduction in regular social activities, low exposure to natural light, and age-related psychosocial stressors such as financial strain, relocation, and loss of friends and loved ones may contribute to poor sleep with advancing age (Bloom et al., 2009; Fragoso & Gill, 2007). Older adults who participate in ADHC programs are likely to experience many of these risk factors, some of which may potentially impact the frequency and intensity of participation in the ADHC program itself.
Older Veterans attending VA-sponsored ADHC programs often face additional challenges including combat-related injuries, significant psychosocial stressors, and long-standing, unresolved psychological difficulties such as posttraumatic stress disorder (PTSD; Rivero et al., 2012). Despite numerous risk factors for poor sleep that exist in this population, to our knowledge sleep problems in ADHC participants have not been studied. This study therefore represents the first look into sleep characteristics of frail older adults attending an ADHC program. The first aim of this analysis was to describe sleep characteristics and to estimate rates of clinically defined insomnia among frail, older Veterans participating in a VA ADHC program. To accomplish this, we developed and used a brief 28-item insomnia screening measure with the goal of identifying individuals appropriate for a sleep intervention program. Here we also examine differences between ADHC participants with and without insomnia, using criteria based on the screening questionnaire. We hypothesized that those who met criteria for insomnia would show greater sleep disturbance in multiple domains, and would be more likely to have sought help from health care providers. We also hypothesized that older age would be associated with a greater likelihood of having insomnia.
DESIGN AND METHODS
Participants
Data presented here were collected by research personnel during the screening phase of a randomized controlled trial of a sleep intervention program for VA Adult Day Health Care (ADHC) program participants. Data were collected via interview by a research social worker or a graduate-level research assistant, after obtaining verbal consent for screening, from Veterans enrolled in one ADHC program at a Los Angeles-based VA Ambulatory Care Center between November 2010 and June 2012. Inclusion criteria were: enrollment in the ADHC program at least 30 days prior to screening with planned attendance at least one day per week, and the ability to communicate verbally, in English, with study personnel to complete screening questions. During the study period, the program capacity was 75 patients. In total, 68 individuals (91% of total enrollees) agreed to complete the screening questionnaire. Reasons for not being screened included irregular attendance or extended absence from the program (n = 5), inability to verbally communicate (n = 1), or refusal to complete the screening (n = 1). Proxy interviews were not completed (i.e., a family member or caregiver was not asked to answer questions on the participant’s behalf). The study was approved by the Institutional Review Board of the Veterans Administration Greater Los Angeles Healthcare System.
Measures
For the purpose of identifying potential participants for an insomnia intervention trial, a brief 28-item sleep screening questionnaire was compiled by the authors using items from validated sleep questionnaires with simplified response options. These items were selected to align with the International Classification of Sleep Disorders-2 (ICSD-2), which defines insomnia as chronically nonrestorative or poor-quality sleep (Criterion A) despite adequate opportunity and circumstances (Criterion B), that results in daytime consequences (Criterion C). Additionally, we elected to specify a duration of at least 3 months of sleep problems to define insomnia, which is consistent with the research diagnostic criteria proposed by Edinger et al. (2004).
The screening questionnaire included items from the Pittsburgh Sleep Quality Index (PSQI; Buysse, Reynolds, Monk, Berman, & Kupfer, 1989) and the Insomnia Severity Index (ISI; Bastien, Vallieres, & Morin, 2001) with supplemental items developed to address other aspects of the insomnia diagnostic criteria (American Academy of Sleep Medicine, 2005) and selected other sleep-related concerns. Adaption of items from published instruments used standard survey development methodologies, including cognitive interviewing with the target population in an iterative process until items had satisfactory face validity and provided sufficient information to identify sleep-related difficulties (Willis, Royston, & Bercini, 1991).
Demographics.
All participants were asked to report their age and how long they had been participating in the ADHC program. We included only individuals who had taken part in the program for at least one month, since acute changes in sleep may accompany beginning a new structured daytime activity, such as taking part in the ADHC program. Medical record information was not available given that questionnaires were completed prior to obtaining written informed consent.
Sleep schedule and sleep characteristics (Criterion A).
Using 5 items from the PSQI in their original form (Buysse et al., 1989), participants were asked to think about their sleep over the past 7 days and to report the following: (a) bedtime (time you got into bed, turned out the lights and tried to fall asleep), (b) number of minutes it took to fall asleep, (c) rise time (time you got out of bed to start your day), (d) hours of actual sleep, and (e) general sleep quality (very good, fairly good, fairly bad, very bad). Total time in bed (from go-to-bed time until get-out-of-bed time) and sleep efficiency (hours of actual sleep/total time in bed) were calculated from these items.
Participants were then asked 4 dichotomous questions, adapted from the ISI (Bastien et al., 2001) about whether they had trouble falling asleep, staying asleep, or waking up too early, or had difficulty waking up in the morning. This adaptation from multiple response options to a yes/no format was made after cognitive interviewing revealed our target population had difficulties in selecting among multiple response options for these questions.
Sleep opportunity and circumstances (Criterion B).
Participants were asked if their sleep problems were caused by the place in which they slept (i.e., uncomfortable bed, noise, light, another person), as inadequate circumstances for sleep would indicate that the individual does not meet the diagnostic criteria for an insomnia disorder (American Academy of Sleep Medicine, 2005). The face validity of this item was confirmed with cognitive interviews. Those reportedly spending less than 5 hr in bed (derived from the PSQI items listed above) were also considered not to meet Criterion B (i.e., did not have adequate opportunity for sleep).
Daytime consequences (Criterion C).
Participants were asked whether they experienced any of the daytime symptoms listed in the ICSD-2 as a result of not sleeping well at night (in yes/no format): feel tired or fatigued during the day; have trouble paying attention, concentrating, or remembering things; have difficulty with work or social life; feel irritable, depressed, or anxious; feel sleepy during the day; have less motivation, energy, or drive; make mistakes or have accidents; feel achy, have headaches, or experience stomach problems; take a nap or doze off during the daytime; or worry about your sleep. One or more of these daytime consequences are required for insomnia diagnosis (American Academy of Sleep Medicine, 2005). The face validity of these items was confirmed with cognitive interviews.
Other sleep items.
To determine whether participants had experienced sleep problems for 3 months or more (Edinger et al., 2004), they were asked to indicate how long they have had problems with sleep: more than 12 months, 3–12 months, less than 3 months, or don’t have sleep problems. Responses indicating insomnia lasting 3 months or longer were used to identify individuals with chronic insomnia. Participants were asked whether they were taking any prescription or over-the-counter medication to help with sleep (yes/no), and whether they had ever talked to a doctor about their sleep problems (yes, no, or I don’t have sleep problems). Again, the utility and face validity of these items was tested and confirmed with cognitive interviews.
Data Analysis
Analyses were performed using SPSS 16.0 (SPSS, 2011) and Stata/MP 12.1 (StataCorp, 2011). Descriptive statistics were calculated for the sample on all variables. There were very few missing data points in this study. When demographic information was not known by the participant (e.g., respondent was unsure about duration of program participation), this was obtained from ADHC program staff. Remaining missing items were not imputed. The main analyses were descriptive in nature, focusing on the criteria for an insomnia disorder using the ICSD (American Academy of Sleep Medicine, 2005). For the purposes of this study, the criteria were defined as follows:
Criterion A.
Positively endorsing one or more of the following: sleep that is chronically poor or nonrestorative (defined as any one or more of the following: 30+ minutes to fall asleep, yes to difficulty falling asleep, yes to difficulty staying asleep, yes to wake up earlier than wanted, sleep efficiency less than 80%, or poor or very poor self-rated sleep quality).
Criterion B.
Not endorsing that sleep problems were caused by the place that the individual sleeps and spending a minimum of 5 hours in bed.
Criterion C.
One or more daytime consequences as listed above.
Criterion D.
Sleep problems lasting at least three months (based on the research diagnostic criteria for insomnia (Edinger et al., 2004).
Participants who met all four of these criteria (A, B, C, and D) were considered likely to have an insomnia disorder, and are described as “with insomnia” within our analyses.
Individuals meeting all of these criteria were then compared to those who did not meet the insomnia criteria on questionnaire items using t-tests, z-tests of proportions (for binary outcomes), and chi-square tests (for multinomial outcomes). Given the relatively small sample size and exploratory nature of this study, confidence intervals and effect size estimates are provided. Finally, logistic regression analysis was used to predict insomnia rates as a function of age.
RESULTS
Demographic Information and Sleep Characteristics
Demographic information and sleep characteristics are shown in Table 1. A majority of participants endorsed one or more items suggesting poor sleep, and rates of all types of sleep complaints were high in our sample. Approximately one-half of individuals endorsed difficulty staying asleep, sleeping 6 hours or less, or having sleep efficiency < 80%.
TABLE 1.
Characteristics of VA ADHC Participants (N = 68 Unless Noted)
| N | % | |
|---|---|---|
| Gender, male | 65 | 96% |
| Reported use of prescription sleep aid (n = 67) | 13 | 19% |
| Reported use of OTC sleep aid (n = 67) | 1 | 1% |
|
| ||
| M (SD) | Range | |
|
| ||
| Age (years) | 79.0 (9.7) | 59–96 |
| Months of participation in VA ADHC program (n = 67) | 32.3 (36.7) | 0–180 |
| Days per week in attendance at ADHC | 2.46 (0.8) | 1–5 |
| Bedtime | 10:00 p.m. (1:25) | 7:00 p.m.–2:30 a.m. |
| Time to fall asleep (mins) | 30.76 (39.1) | 0–180 |
| Get-out-of-bed time | 6:46 a.m. (1:32) | 2:30 a.m.–10:30 a.m. |
| Hours spent in bed | 8.8 (1.7) | 4.0–12.5 |
| Hours of actual sleep | 6.6 (2.2) | 2.0–12.0 |
| Sleep efficiency (time asleep/total time in bed) | 75.2% (20.5%) | 18.2–100% |
Rate of insomnia among ADHC participants.
The four-step algorithm aligning with the ICSD diagnostic criteria for insomnia lasting 3 months or more (described above) was used to identify those with an insomnia disorder. The results of this process are shown in Figure 1. Overall, 70.6% of respondents had reported sleep disturbance (ICSD Criterion A), of whom 79.2% met Criterion B as well (having adequate opportunity and circumstances for sleep). Among those meeting both Criteria A and B, all reported one or more daytime consequences related to poor sleep, and 68.4% indicated that their sleep difficulties had persisted for three months or longer. Thus, out of the 68 total participants, 26 met all criteria for an insomnia disorder lasting at least 3 months, yielding a 38.2% rate of insomnia (95% CI = [26.4%, 50.1%]). Of note, 35.3% (CI = [23.6%, 46.9%]) endorsed insomnia (Criteria A, B, and C) lasting one year or more.
FIGURE 1.
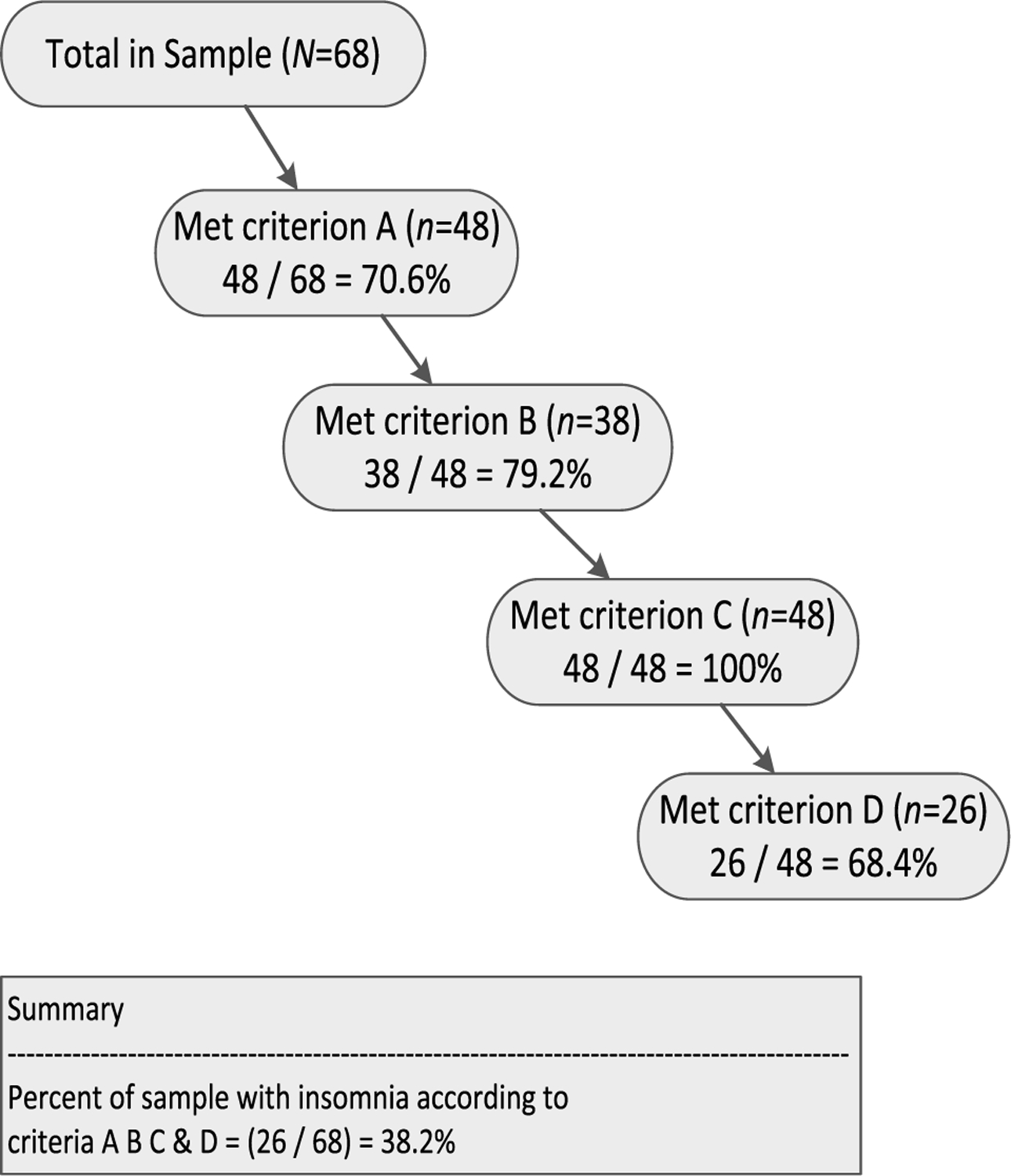
Number and percentage of participants who successively meet each of the ICSD diagnostic criteria for insomnia based on questionnaire responses.
Criterion A: Positively endorsing one or more of the following: sleep that is chronically poor or non-restorative (defined as any one or more of the following: 30C minutes to fall asleep, “yes” to difficulty falling asleep, “yes” to difficulty staying asleep, “yes” to wake up earlier than wanted, sleep efficiency less than 80%, or “poor” or “very poor” self-rated sleep quality.
Criterion B: Not endorsing that sleep problems were caused by the place that the individual sleeps and spending a minimum of 5 hours in bed.
Criterion C: One or more daytime consequences as listed above.
Criterion D: Sleep problems lasting at least three months.
Comparison of ADHC participants with and without insomnia.
Comparisons between those with and without insomnia are shown in Table 2. Individuals with insomnia participated an average of half a day less per week in the ADHC program than those without insomnia. As expected, individuals with insomnia reported multiple aspects of worse sleep quality, including taking longer to fall asleep, fewer hours of sleep at night, and trouble falling asleep, trouble staying asleep, and waking up too early. Interestingly, they also were more likely to report all of the daytime consequences related to insomnia (although difficulty with social life was not statistically different across groups). Importantly, 53% of those with insomnia had spoken to a doctor about their sleep problems, while 17% of those without insomnia had done so.
TABLE 2.
Sleep Characteristics of VA ADHC Participants With and Without Insomnia
| With Insomnia (N = 26) Mean (SD) | Without Insomnia (N = 42) Mean (SD) | p Value | Difference & (95% CI) | |
|---|---|---|---|---|
| Demographics | ||||
| Age | 79.84 (9.72) | 78.45 (9.71) | .567 | 1.39 (−3.44, 6.23) |
| Months of participation | 40.25 (42.34) | 27.24 (32.07) | .159 | 13.00 (−5.20, 31.21) |
| Days of participation per week | 2.11 (.52) | 2.67 (0.93) | 0.007 | −.55 (−.95, −.15) |
| Sleep characteristics | ||||
| Bedtime | 22:13 (1:31) | 21:52 (1:20) | 0.307 | 00:21.5 (−00:20.5, 01:04.2) |
| Minutes to fall asleep | 43.2 (38.7) | 23.0 (37.7) | 0.0375 | 20.2 (1.2, 39.2) |
| Rise time | 6:54 (1:41) | 6:40 (1:25) | 0.535 | 00:14.3 (−00:31.5, 01:00.2) |
| Hours of sleep per night | 5.75 (1.82) | 7.05 (2.30) | .0168 | −.13 (−2.4, −.2) |
| N (%) | N (%) | |||
| Trouble falling asleep | 19 (73.1%) | 6 (14.3%) | < 0.001 | 58.8% (38.7%, 24.9%) |
| Trouble staying asleep | 24 (73.1%) | 9 (21.4%) | < 0.001 | 70.9% (54.8%, 87.0%) |
| Waking up too early | 20 (76.9%) | 10 (23.8%) | < 0.001 | 53.1% (32.4%, 73.8%) |
| Trouble waking up in the morning | 7 (15.0%) | 3 (7.14%) | 0.377 | 7.8% (−9.6%, 25.3%) |
| Consequences of poor sleep | N (%) | N (%) | ||
| Feel tired or fatigued during the day? | 18 (69.2%) | 8 (19.1%) | < 0.001 | 50.2% (28.8%, 71.5%) |
| Have trouble paying attention, concentrating, or remembering things? | 13 (50.0%) | 5 (11.9%) | 0.001 | 38.1% (16.5%, 60.0%) |
| Have difficulty with social life? | 6 (23.1%) | 3 (7.14%) | 0.076 | 15.9% (−2.0%, 33.9%) |
| Feel irritable, depressed, or anxious? | 13 (50.0%) | 5 (11.9%) | 0.001 | 38.1% (16.5%, 59.7%) |
| Feel sleepy during the day? | 24 (92.3%) | 20 (47.6%) | < 0.001 | 44.7% (26.4%, 62.9%) |
| Have less motivation during the day? | 14 (53.9%) | 7 (16.7%) | 0.002 | 37.2% (15.0%, 59.4%) |
| Make mistakes? | 7 (26.9%) | 2 (4.76%) | 0.022 | 22.2% (4.0%, 40.4%) |
| Feel achy, have headaches, or have stomach problems? | 6 (23.1%) | 1 (2.38%) | 0.011 | 20.7% (3.8%, 37.5%) |
| Worry about your sleep? | 10 (38.5%) | 4 (9.52%) | 0.006 | 28.9% (8.2%, 49.6%) |
| Take a nap or doze off during the daytime? | 18 (69.2%) | 25 (59.5%) | 0.451 | 9.7% (−13.4%, 32.8%) |
| Other sleep items | ||||
| How would you describe your sleep during the past seven days? | ||||
| a. Very bad | 1 (3.85%) | 2 (4.76%) | < 0.001 | N/A |
| b. Fairly bad | 9 (34.6%) | 1 (2.38%) | ||
| c. Fairly good | 13 (50.0%) | 14 (33.3%) | ||
| d. Very good | 3 (11.5%) | 25 (59.5%) | ||
| How long have you had problems with your sleep? | ||||
| a. More than 12 months | 24 (92.3%) | 7 (16.7%) | < 0.001 | N/A |
| b. 3 months to 12 months | 2 (7.79%) | 1 (2.38%) | ||
| c. Less than 3 months | 0 (0.0%) | 3 (7.14%) | ||
| d. I don’t have sleep problems | 0 (0.0%) | 31 (73.8%) | ||
| Talked to a doctor about sleep problems? (N = 60) | 10 (52.6%) | 7 (17.1%) | 0.012 | 35.6% (10.3%, 60.8%) |
Insomnia and age.
We then investigated the rate of insomnia across ages (mean age = 79 years; SD = 9.7 years; range = 59–96 years). A logistic regression analysis predicting insomnia from age found no significant contribution of age (p = .561). Including a quadratic term for age yielded no significant association with respect to age (p = .978) or age squared (p = .951).
DISCUSSION
This report represents a first look at sleep characteristics in older adults participating in VA Adult Day Health Care (ADHC). In this sample of older Veterans, sleep problems were common in terms of clinical markers of poor sleep, such as sleeping 6 hours or less, sleep efficiency below 80%, reported difficulty falling or staying asleep, or difficulty with morning rise time (either early morning awakenings or trouble waking up in the morning).
When we employed a prespecified algorithm for identifying each of the ICSD diagnostic criteria for insomnia, we found that 71% of the sample reported some indication of poor sleep quality. We made this criterion intentionally broad to capture all types of sleep disturbance that might lead to seeking clinical attention. A majority of individuals who reported sleep complaints reported that it was not the result of where they slept, and they spent at least 5 hours in bed. While assessing this criterion (Criterion B) poses some challenges in a questionnaire format, we felt that these two items would help identify patients who might be inappropriate for behavioral treatments, for example, because they do not have a bed to sleep in or because they are in bed a very short period of time and therefore cannot obtain sufficient sleep. Interestingly, all of the individuals who met these two criteria reported one or more daytime consequences. This suggests that sleep difficulties, when they do occur, are related to daytime impairments in this population. Interestingly, only 68% of those meeting criteria A through C indicated that their sleep problems had persisted for more than 3 months. We found that the overall rate of insomnia in this study was 38% (95% CI = 26.4–50.1). This rate is consistent with some prior studies among community-dwelling older adults (Foley et al., 1995), but lower than studies of older individuals with comorbidities (Foley, Ancoli-Israel, Britz, & Walsh, 2004; Foley et al., 1995; Ohayon, 2002).
Some of the most notable findings from our study include the multiple discrepancies between markers of poor sleep and each endorsement of sleep problems and positively rated sleep quality. These discrepancies suggest that frail older Veterans who attend ADHC programs may not perceive poor sleep to be a significant impairment that warrants a “bad” sleep quality rating. This could be due to several reasons. First, older adults may believe that poor sleep is an expected consequence of aging and that treatment would not be effective or beneficial. Second, older adults also may not view sleep as a priority compared to other health conditions such as diabetes, heart disease, or chronic pain. Third, after decades of problems, older adults may simply become accustomed to poor sleep and may not believe anything can be done to improve their sleep quality (Brouwer, van Exel, & Stolk, 2005). Further research is needed to better understand how such attitudes may or may not affect help-seeking and treatment behaviors.
We were also struck by the frequency with which symptoms of daytime sleepiness were endorsed as a consequence of sleep disturbance. In fact, 92% of those with insomnia reported feeling sleepy, and 69% of those with insomnia reported feeling tired or fatigued. This suggests that, while insomnia in younger patients may be accompanied by hyperarousal, among these medically complex older patients, daytime sleepiness may be the most significant consequence of poor sleep.
We were also interested in whether these individuals had discussed sleep issues with their providers. While we recognize the limitations of gathering this information in self-report format, we were impressed with the fact that only one half of those meeting criteria for insomnia had spoken to a doctor. It is possible that some did not recall such a conversation that occurred in the past; however, this does suggest that doctors should screen for sleep difficulties in ADHC patients to identify sleep difficulties that may be present. This is also significant as these complaints may be the result of untreated sleep apnea. Although sleep apnea was not assessed in our study, this is an area that should be investigated in future research.
We were surprised to find that there was no relationship (linear or quadratic) between insomnia and age. Given that the age range of our participants was broad, spanning 30 years, we anticipated that there would be a relationship between age and insomnia. This may be the result of studying a sample within VA.
While our study has multiple strengths, including our ability to screen nearly all program participants (91%), the sample size is fairly small, and the data were gathered at only one site. There are several other limitations. First, this data is based on the screening phase of a larger study, and since data were gathered after obtaining only verbal consent, we were not permitted to review patient medical records or inquire about sensitive medical or psychiatric information. While our screening items were derived from well-established questionnaires, some had to be simplified or modified for the ADHC population. For example, we elected to utilize a broad definition of sleep disturbance for Criterion A as we believed alternative components such as low sleep efficiency can be used to identify poor sleep quality in a population of older adults who might otherwise dismiss sleep disturbances (i.e., trouble falling or staying asleep) as an expected consequence of aging and/or illness. Because we had limited time to complete screening questions with potential participants between scheduled ADHC program activities, we also did not assess for sleep apnea, restless leg syndrome, depression, or anxiety in this phase of the study. Clearly comorbid sleep disorders may play a significant role. Second, our sample may be biased in several ways. Since participants were recruited in a VA program, nearly all were male. All participants were attending ADHC programs because of one or more health or medical conditions that put them at risk for functional decline and thus are representative of a higher risk, vulnerable subgroup of older adults. It is unclear whether these findings would generalize to older women or to non-Veterans participating in community-based ADHC programs. These findings also may not generalize to healthier groups of individuals in the same age range, or to individuals that were too frail to participate in the ADHC program (e.g., those who are home-bound or institutionalized). Finally, cognitive limitations and/or communication difficulties among the ADHC respondents may impact the ability of some individuals to accurately recall their recent sleep experiences and report them during screening. We elected to include data from all participants, as we believe this is indicative of the screening challenges inherent in this population and highlights the need for future scale development and validation in frail older adults with cognitive and functional limitations.
This report highlights the high prevalence of sleep disturbance among older adults participating in VA ADHC. Our findings are not surprising given the high frequency and severity of comorbidities amongst ADHC program participants; yet, the discrepancies between quantitative markers of clinically defined poor sleep, endorsement of sleep problems, and “good” sleep quality ratings were unexpected. A better understanding of older adults’ beliefs and attitudes toward sleep, including causal attributions of sleep disturbance, perceptions of sleep quality, and attitudes toward sleep-related treatments is needed. Further work on how to best screen for sleep disorders in frail older adults is clearly warranted.
Understanding sleep problems in VA ADHC participants has important research and clinical implications given that poor sleep is known to affect health-related quality-of-life and mortality risk, and that effective evidence-based behavioral treatments exist for alleviating sleep complaints. We believe that if ADHC programs are to continue helping frail older adults maintain their overall health and function, sleep quality must receive greater attention and should become a more integral part of ADHC patient assessment and education.
ACKNOWLEDGMENTS
The authors wish to thank Jo Ellen Baur, MSW, LCSW; Maureen Burrell, MSW, LCSW; Michael Mitchell, PhD; Karen Josephson, MPH; Terry Vandenberg, MA; and Sergio Martinez for their assistance with this project.
FUNDING
This work was supported by the National Institute on Aging [K23 AG028452 and L30 AG032916 to Martin]; VA Rehabilitation Research and Development [1RX000135–01 to Martin]; and VA Greater Los Angeles Healthcare System Geriatric Research, Education, and Clinical Center.
Contributor Information
Jaime M. Hughes, School of Social Work University of North Carolina at Chapel Hill
Jennifer L. Martin, Geriatric Research, Education, and Clinical Center VA Greater Los Angeles Healthcare System; David Geffen School of Medicine University of California at Los Angeles
REFERENCES
- Alessi CA, Martin JL, Webber AP, Alam T, Littner M, Harker JO, & Josephson K (2008). More daytime sleeping predicts less functional recovery among older people undergoing inpatient post-acute rehabilitation. Sleep, 31, 1291–1300. [PMC free article] [PubMed] [Google Scholar]
- American Academy of Sleep Medicine. (2005). Insomnia. In International classification of sleep disorders (2nd ed., pp. 1–31). Chicago, IL: Author. [Google Scholar]
- Bastien CH, Vallieres A, & Morin CM (2001). Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Medicine, 2, 297–307. [DOI] [PubMed] [Google Scholar]
- Baumgarten M, Level P, Laprise H, Leclerc C, & Quinn C (2002). Adult day care for the frail elderly: Outcomes, satisfaction, and cost. Journal of Aging and Health, 14, 237–259. [DOI] [PubMed] [Google Scholar]
- Bloom HG, Ahmed I, Alessi CA, Ancoli-Israel S, Buysse DJ, Kryger MH, … Zee PC (2009). Evidence-based recommendations for the assessment and management of sleep disorders in older persons. Journal of the American Geriatrics Society, 57, 761–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouwer WBF, van Exel NJA, & Stolk EA (2005). Acceptability of less than perfect health states. Social Science and Medicine, 60, 237–246. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, & Kupfer DJ (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 23, 193–213. [DOI] [PubMed] [Google Scholar]
- Cochen V, Arbus C, Soto ME, Villars H, Tiberge M, Montemayor T, … Vellis B (2009). Sleep disorders and their impacts on healthy, dependent, and frail older adults. The Journal of Nutrition, Health, and Aging, 13, 322–329. [DOI] [PubMed] [Google Scholar]
- Edinger JD, Bonnet MH, Bootzin RR, Doghramji K, Dorsey CM, Espie CA, … Stepanski EJ (2004). Derivation of research diagnostic criteria for insomnia: Report of an American Academy of Sleep Medicine work group. Sleep, 27, 1567–1596. [DOI] [PubMed] [Google Scholar]
- Foley DJ, Ancoli-Israel S, Britz P, & Walsh J (2004). Sleep disturbance and chronic disease in older adults: Results of the 2003 National Sleep Foundation Sleep in America Survey. Journal of Psychosomatic Research, 56, 407–502. [DOI] [PubMed] [Google Scholar]
- Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, & Blazer DG (1995). Sleep complaints among elderly persons: An epidemiological study of three communities. Sleep, 18, 425–432. [DOI] [PubMed] [Google Scholar]
- Fragoso CAV, & Gill TM (2007). Sleep complaints in community-living older persons: A multifactorial geriatric syndrome. Journal of the American Geriatrics Society, 55, 1835–1866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler JE, & Zarit SH (2001). The effectiveness of adult day services for disabled older people. Journal of Aging and Social Policy, 12, 23–47. [DOI] [PubMed] [Google Scholar]
- Office of Public Affairs and Media Relations. (2005). VA long-term care Washington, DC: Department of Veterans Affairs. [Google Scholar]
- Ohayon MM (2002). Epidemiology of insomina: What we know and what we still need to learn. Sleep Medicine Reviews, 6, 97–111. [DOI] [PubMed] [Google Scholar]
- Perlis ML, Smith LJ, Lyness JM, Matteson SR, Pigeon WR, Jungquist C, … Tu X (2006). Insomnia as a risk factor for onset of depression in the elderly. Behavioral Sleep Medicine, 4, 104–113. [DOI] [PubMed] [Google Scholar]
- Rivero T, Hughes JM, Kramer BJ, & Martin JL (2012, November). Veterans Health Administration adult day health care programs: Variations and common features Poster session presented at the meeting of the Gerontological Society of America, San Diego, CA. [Google Scholar]
- Schmitt EM, Sands LP, Weiss S, Dowling G, & Covinsky K (2010). Adult day health center participation and health-related quality of life. The Gerontologist, 50, 531–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SPSS. (2011). SPSS 16.0 [Computer software] Chicago, IL: Author. [Google Scholar]
- StataCorp. (2011). Stata Statistical Software [computer software] College Station, TX: Author. [Google Scholar]
- Veterans Health Administration. (2009). Adult day health care (Rep. No. HA Handbook 1141.03) Washington, DC: Department of Veterans Affairs. [Google Scholar]
- Willis GB, Royston P, & Bercini D (1991). The use of verbal report methods in the development and testing of survey questionnaires. Applied Cognitive Psychology, 5, 251–267. [Google Scholar]


