Abstract
Objective
The aim was to assess clinical improvement after US-guided injection of CSs into the SI joint of patients with SpA.
Methods
This was an observational, descriptive, retrospective study of patients with SpA and sacroiliitis who received an US-guided injection into the SI joint between 1 June 2020 and 31 May 2021. Means were compared using Student’s paired t-test for the variables visual analog scale (VAS), BASDAI, ASDAS, CRP and ESR before and after the procedure. We evaluated the association between these variables and the clinical response using the odds ratio.
Results
We analysed 32 patients with SpA [age 42.69 (8.19) years; female sex, 56.25%], with a VAS score of 7.88 (0.79), BASDAI of 5.43 (1.48) and ASDAS of 3.27 (0.86) before the procedure. At 2–3 months, 75% of patients had improved: VAS 3.81 (2.33) (−4.07, P < 0.0001) and BASDAI 3.24 (1.6) (−2.19, P < 0.0001). At 5–6 months, 59.37% had improved: VAS 4.63 (2.31) (−3.25, P < 0.0001), BASDAI 3.57 (1.67) (−1.86, P < 0.0001) and ASDAS 2.27 (0.71) (−1.0, P < 0.0001). Bone marrow oedema resolved in 87.5% of cases compared with the previous MRI scan. No significant association was identified with the clinical response to the injection.
Conclusion
US-guided injection of CSs into the SI joint of patients with SpA and active sacroiliitis leads to an improvement in symptoms that is maintained at 5–6 months. The procedure is effective, safe, inexpensive and easy to apply.
Keywords: spondyloarthritis, sacroiliitis, ultrasound-guided injection, disease activity
Key messages
This is the first study carried out in Spain on this procedure in this group of patients and whose outcome variables include activity measurements.
US-guided CS infiltration of the SI joint in patients with SpA could be a therapeutic alternative for those in whom clinical and radiological sacroiliitis predominates.
The incorporation of US into daily clinical practice would allow the performance of this procedure.
Introduction
The term SpA covers a group of chronic inflammatory rheumatic diseases that mainly affect the axial skeleton [1]. The worldwide prevalence of SpA is estimated to range between 0.23 and 1.8% [2]. The disease most typically affects the SI joints, where it first manifests in 75% of patients [3]. Sacroiliitis can be the main manifestation or a complication of any of the variants of SpA.
Imaging-guided CS injection has been considered an effective therapy for >20 years [4]. This approach provides a significant improvement in pain and inflammation for ≤1 year in patients who do not have SpA [5, 6].
The few studies performed in patients with SpA have mainly evaluated the improvement in pain using a visual analog scale (VAS) and are limited by the need for an operating room and guidance based on fluoroscopy, tomography or magnetic resonance [7–9]. The advent of new US devices has meant that during the last decade, alternative approaches have been proposed for US-guided injection of the SI joint. These are all highly effective, accurate and safe. The technique is relatively simple to perform and accurate, with no need for an operating room or exposure to ionizing radiation [10–13]. Therefore, US-guided injection is now considered a safe, valid and easy technique.
The primary objective of this study was to determine clinical improvement (BASDAI, ASDAS, acute-phase reactants and the VAS score) after US-guided injection of CSs into the SI joint of patients with SpA.
Methods
We performed an observational, descriptive and retrospective study at Ciudad Real General Teaching Hospital (HGUCR), Ciudad Real, Spain.
We reviewed the register of procedures carried out between 1 June 2020 and 31 May 2021 and included all patients fulfilling the Assessment of SpA International Society (ASAS) classification criteria for SpA with inflammatory low back pain resulting from sacroiliitis despite treatment with NSAIDs, biologics, or both. We excluded patients whose clinical history did not contain the study variables and in whom modifications to pharmacological treatment could have reduced the effectiveness of the injection.
All patients underwent US-guided injection of the SI joint with 12 mg betamethasone chronodose (6 mg acetate/6 mg phosphate) in each joint. The patient was placed in the prone position, with a pillow underneath the abdomen to minimize lumbar lordosis. A low-frequency curvilinear transducer was used. The transducer was placed transversely over the lower part of the sacrum (at the level of the sacral hiatus), and the lateral edge of the sacrum was identified. The transducer was moved laterally and cephalad until the bony contour of the ileum was clearly identified. The cleft seen between the medial border of the ileum and the lateral sacral edge represented the SI joint. A 22-gauge needle was inserted at the medial end of the transducer and advanced laterally under direct vision in plane with the US beam until it was seen entering the joint (Fig. 1).
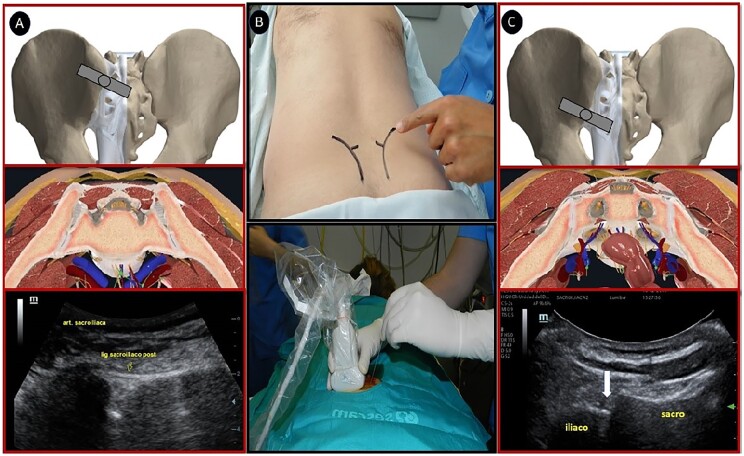
Fig. 1.
Technique used for US-guided injection into the SI joint
(A) Anatomical and US image when approaching the upper two-thirds of the SI joint (syndesmosis). (B) Positioning of the patient and approach in the joint plane with a curved transducer. (C) Anatomical and US image when approaching the lower one-third of the SI joint (synovial).
We recorded data for the study variables (age, sex, type of SpA, time since diagnosis, HLA B27, SI joint X-rays, sacroiliac MRI scans, pharmacological treatment, VAS score, BASDAI, ASDAS, CRP and ESR) from the clinical history before the procedure and for 6–8 months after it. The outcome measures were the presence of adverse effects/complications, reduction in the VAS score for inflammatory pain (>0 = 3 points), reduction of ≥1.1 points in the ASDAS, reduction of ≥2 points in the BASDAI, and reduction of CRP and ESR values. These data were analysed by comparing means (Student’s t-test) for the variables VAS, BASDAI, ASDAS, CRP and ESR. The potential association between the variables and a favourable clinical response was evaluated by calculating the odds ratio. All analyses were performed with a 95% CI using StatPlus v.7.3.32 from AnalystSoft Inc. (USA).
The protocol was approved by the Research and Ethics Committee of Integrated Care Management, Ciudad Real, Spain.
Results
Of a total of 47 patients, we included 32 for the final analysis. Table 1 shows the clinical and serological characteristics, radiographic findings, treatments and procedures.
Table 1.
Clinical profile of patients
| Variable | n (%) |
|---|---|
| Sex | |
| Male | 14 (43.75) |
| Female | 18 (56.25) |
| Age, mean (s.d.), years | 42.69 (8.19) |
| Type of SpA | |
| Ankylosing | 14 (43.75) |
| Non-radiographic | 13 (40.62) |
| IBD associated | 3 (9.38) |
| Psoriatic | 2 (6.25) |
| Time since diagnosis, mean (s.d.), years | 3.94 (2.55) |
| Presence of HLA B27 (+) | 14 (43.75) |
| X-ray of SI joint according to New York criteria | |
| Grade 0 | 8 (25) |
| Grade 1 | 7 (21.88) |
| Grade 2 | 13 (40.63) |
| Grade 3 | 4 (12.49) |
| Grade 4 | 0 0 |
| Sacroiliitis on the MRI according to ASAS criteria | |
| Right | 7 (21.87) |
| Left | 7 (21.87) |
| Bilateral | 14 (43.75) |
| Negative | 4 (12.51) |
| Extra-axial manifestations | 16 (50) |
| Peripheral involvement | 10 (31.25) |
| IBD | 3 (9.38) |
| Psoriasis | 2 (6.25) |
| Uveitis | 1 (3.13) |
| Treatment | |
| Non-opiate analgesics | 10 (31.25) |
| Opiate analgesics | 15 (45.87) |
| NSAIDs | 17 (53.12) |
| CSs | 8 (25) |
| DMARDs | 10 (31.25) |
| MTX | 5 (15.62) |
| SSZ | 3 (9.38) |
| Mesalazine | 1 (3.13) |
| AZA | 1 (3.13) |
| Biologics | 18 (56.25) |
| Adalimumab | 8 (25) |
| Golimumab | 5 (15.62) |
| Etanercept | 2 (6.25) |
| Secukinumab | 2 (6.25) |
| Vedolizumab | 1 (3.13) |
| Previous ASDAS, mean (s.d.) | 3.27 (0.86) |
| Grade of disease activity | |
| Inactive (<1.3) | 0 (0) |
| Low–moderate (<2.1) | 2 (6.25) |
| High (≤3.5) | 19 (59.37) |
| Very high (>3.5) | 11 (34.38) |
| Previous BASDAI, mean (s.d.) | 5.43 (1.48) |
| Degree of activity | |
| Low (BASDAI <4) | 2 (6.25) |
| High (BASDAI ≥4) | 30 (93.75) |
| Previous CRP, mean (s.d.) (normal, ≤0.5 mg/dl) | 0.61 (0.78) |
| Previous ESR, mean (s.d.) (normal, ≤10 mm) | 10.88 (8.94) |
| VAS score for previous low back pain, mean (s.d.) | 7.88 (0.79) |
| Injection into SI joint | |
| Right | 10 (31.25) |
| Left | 8 (25) |
| Bilateral | 14 (43.75) |
ASAS: Assessment of SpondyloArthritis International Society; VAS: visual analog scale.
We observed an improvement in 75% of patients at 2–3 months, with a mean (s.d.) reduction of ≥3 points in the VAS for low back pain [3.81 (2.33)] (−4.07, P < 0.0001) and an improvement in the BASDAI value in 65.62% [3.24 (1.6)] (−2.19, P < 0.0001). At ∼6 months, the improvement in pain remained unchanged, at 59.37% for the VAS [4.63 (2.31)] (−3.25, P < 0.0001), 46.87% for BASDAI [3.57 (1.67)] (−1.86, P < 0.0001) and 43.75% for ASDAS-CRP [2.27 (0.71)] (−1.0, P < 0.0001), whereas only 18.75% experienced a considerable improvement in ASDAS-CRP (reduction ≥2). Most patients reported some degree of subjective benefit of the procedure for ≤8 months. No very significant reductions were recorded for acute-phase reactants: CRP, 0.28 (0.33) (−0.33, P = 0.0312); and ESR, 7.91 (6.55) (−2.97, P = 0.1346). After the procedure, only eight patients had undergone a follow-up MRI scan of the SI joint at 5.88 (1.25) months. Compared with the previous scan, bone marrow oedema had resolved in 87.5%.
Analysis of factors potentially associated with improved clinical response, as measured using the VAS, BASDAI and ASDAS, did not reveal a significant association with the variables analysed [age, time since diagnosis, grade of sacroiliitis by radiography, presence of HLA B27 (+), peripheral and extra-articular manifestations, and type of treatment]. However, all the patients whose symptoms improved (VAS score, BASDAI and ASDAS) had had bone marrow oedema on their MRI scan <1 year before the treatment.
Only five patients experienced injection site pain, which lasted 1–2 days. No other adverse effects were reported.
Discussion
In the 1990s, Maugars et al. [7] first reported that fluoroscopy-guided injection of CSs into the SI joints of patients with SpA reduced pain by 50–64%. In the first double-blind study [14] (CSs vs placebo injection), the authors observed a significant improvement in the VAS (P < 0.05), with a 58–70% reduction in the group that received CSs [6.8 (0.6) to 1.3 (0.3)] until 6 months, whereas no significant reduction was observed in the placebo group [7.0 (0.6) to 5.2 (0.5)]. Subsequent studies with fluoroscopy-guided injection reported similar results, mainly with respect to the VAS score [15].
Braun et al. [8] reported their findings with a CT-guided procedure, namely, an 83.3% improvement in the VAS score (from 8.5 to 3 points), which remained at 8.9 (5.3) months, and an improvement in inflammation assessed using MRI in ∼50% of patients. Other studies with CT guidance reported similar results, with significant improvement in symptoms (P < 0.05) based on the VAS score and in inflammation based on MRI at 8 months [16, 17]. Various studies using MRI reported an improvement in the VAS score over a mean of 11–12 months in 78–90% of patients with SpA [9], and bone marrow oedema resolved completely in 38% and partially in 89–100% of patients [18, 19]. Studies on US-guided injection of CSs into the SI joint of patients with SpA reported a 80–100% improvement in inflammatory low back pain (VAS, 6.9 to 3.9) at 3 months (P < 0.05) [13, 20].
A systematic review of PubMed performed in 2019 to identify articles on injection of CSs into the SI joint of patients with SpA/sacroiliitis dating from 1990 yielded 46 references, corresponding to 468 injections in 268 patients. Inflammatory pain and stiffness improved in 80% of patients, with a mean duration of 6–8 months. The factors associated with an improved response were shorter time since diagnosis and MRI-based evidence of bone marrow oedema in the joint at baseline [21]. Finally, a recent study published in 2021 [22] showed an improvement in low back pain according to the VAS score, which was 90% at 1 month and was maintained in 68.4% at 6 months after fluoroscopy-guided injection into the SI joint in patients with SpA. The difference was significant with respect to patients who continued with their habitual treatment with NSAIDs, anti-TNF-α agents, or both, although no differences were detected in either group with respect to the improvement in BASDAI, CRP and ESR.
Our results are consistent with those reported elsewhere, indicating reduced low back pain (VAS score) in 75% and reduced disease activity, which is clearly significant during the first 2–3 months and is maintained at ∼6 months according to the VAS score (−3.25, P < 0.0001), BASDAI (−1.86, P < 0.0001) and ASDAS (−1.0, P < 0.0001). In line with other authors, we recorded no significant changes in levels of CRP or ESR. However, bone marrow oedema resolved in 87.5% of patients who underwent MRI after the procedure (Supplementary Table S1, available at Rheumatology Advances in Practice online).
Our results enable us to conclude that US-guided injection of the SI joint is a safe, effective, inexpensive and easy complementary technique in patients with SpA and recent-onset sacroiliitis that does not respond to standard treatment. Therefore, procedures of this type should be added to the rheumatologist’s therapeutic arsenal.
Supplementary Material
Acknowledgements
The authors thank the Spanish Foundation of Rheumatology for providing medical writing/editorial assistance during the preparation of the manuscript (Cod.FERBT2022).
Funding: No specific funding was received from any bodies in the public, commercial or not-for-profit sectors to carry out the work described in this article.
Disclosure statement: The authors have declared no conflicts of interest.
Data availability statement
The data underlying this article cannot be shared publicly owing to the privacy of individuals who participated in the study. The data will be shared on reasonable request to the corresponding author.
Supplementary data
Supplementary data are available at Rheumatology Advances in Practice online.
References
- 1. Collantes-Estevez E. New paradigms in the diagnosis and classification of the spondylarthritis. Reumatol Clin 2013;9:199–200. [DOI] [PubMed] [Google Scholar]
- 2. Sivera F, Quilis N.. Espondilitis anquilosante. EPISER2016: Estudio de prevalencia de las enfermedades reumáticas en población adulta en España. Madrid [Sociedad Española de Reumatología] 2018;1:69–78. ISBN 978-84-09-07043-5 [Google Scholar]
- 3. Sieper J, van der Heijde D, Landewé R. et al. New criteria for inflammatory back pain in patients with chronic back pain: a real patient exercise by experts from the Assessment of Spondyloarthritis International Society (ASAS). Ann Rheum Dis 2009;68:784–8. [DOI] [PubMed] [Google Scholar]
- 4. Hansen HC, McKenzie-Brown AM, Cohen SP. et al. Sacroiliac joint interventions: a systematic review. Pain Physician 2007;10:165–84. [PubMed] [Google Scholar]
- 5. Luukkainen RK, Wennerstrand PV, Kautiainen HH, Sanila MT, Asikainen EL.. Efficacy of periarticular corticosteroid treatment of the sacroiliac joint in non-spondylarthropathic patients with chronic low back pain in the region of the sacroiliac joint. Clin Exp Rheumatol 2002;20:52–4. [PubMed] [Google Scholar]
- 6. Kennedy D, Engel A, Kreiner S. et al. Fluoroscopically guided diagnostic and therapeutic intra-articular sacroiliac joint injections: a systematic review. Pain Med 2015;16:1500–18. [DOI] [PubMed] [Google Scholar]
- 7. Maugars Y, Mathis C, Vilon P, Prost A.. Corticosteroid injection of the sacroiliac joint in patients with seronegative spondylarthropathy. Arthritis Rheum 1992;35:564–8. [DOI] [PubMed] [Google Scholar]
- 8. Braun J, Bollow M, Seyrekbasan F. et al. Computed tomography guided corticosteroid injection of the sacroiliac joint in patients with spondyloarthropathy with sacroiliitis: clinical outcome and followup by dynamic magnetic resonance imaging. J Rheumatol 1996;23:659–64. [PubMed] [Google Scholar]
- 9. Günaydin I, Pereira P, Daikeler T. et al. Magnetic resonance imaging guided corticosteroid injection of the sacroiliac joints in patients with therapy resistant spondyloarthropathy: a pilot study. J Rheumatol 2000;27:424–8. [PubMed] [Google Scholar]
- 10. Le Goff B, Berthelot JM, Maugars Y.. Ultrasound assessment of the posterior sacroiliac ligaments. Clin Exp Rheumatol 2011;29:1014–7. [PubMed] [Google Scholar]
- 11. De Luigi AJ, Saini V, Mathur R, Saini A, Yokel N.. Assessing the accuracy of ultrasound-guided needle placement in sacroiliac joint injections. Am J Phys Med Rehabil 2019;98:666–70. [DOI] [PubMed] [Google Scholar]
- 12. Soneji N, Bhatia A, Seib R. et al. Comparison of fluoroscopy and ultrasound guidance for sacroiliac joint injection in patients with chronic low back pain. Pain Pract 2016;16:537–44. [DOI] [PubMed] [Google Scholar]
- 13. Hartung W, Ross CJ, Straub R. et al. Ultrasound-guided sacroiliac joint injection in patients with established sacroiliitis: precise IA injection verified by MRI scanning does not predict clinical outcome. Rheumatology (Oxford) 2010;49:1479–82. [DOI] [PubMed] [Google Scholar]
- 14. Maugars Y, Mathis C, Berthelot JM, Charlier C, Prost A.. Assessment of the efficacy of sacroiliac corticosteroid injections in spondylarthropathies: a double-blind study. Br J Rheumatol 1996;35:767–70. [DOI] [PubMed] [Google Scholar]
- 15. Karabacakoglu A, Karaköse S, Ozerbil O, Odev K.. Fluoroscopy-guided intraarticular corticosteroid injection into the sacroiliac joints in patients with ankylosing spondylitis. Acta Radiol 2002;43:425–7. [DOI] [PubMed] [Google Scholar]
- 16. Fischer T, Biedermann T, Hermann K-GA. et al. Sacroiliitis in children with spondyloarthropathy: therapeutic effect of CT-guided intra-articular corticosteroid injection. Rofo 2003;175:814–21. [DOI] [PubMed] [Google Scholar]
- 17. Althoff CE, Bollow M, Feist E. et al. CT-guided corticosteroid injection of the sacroiliac joints: quality assurance and standardized prospective evaluation of long-term effectiveness over six months. Clin Rheumatol 2015;34:1079–84. [DOI] [PubMed] [Google Scholar]
- 18. Pereira PL, Günaydin I, Trübenbach J. et al. Interventional MR imaging for injection of sacroiliac joints in patients with sacroiliitis. AJR Am J Roentgenol 2000;175:265–6. [DOI] [PubMed] [Google Scholar]
- 19. Fritz J, König CW, Günaydin I. et al. Magnetic resonance imaging-guided corticosteroid-infiltration of the sacroiliac joints: pain therapy of sacroiliitis in patients with ankylosing spondylitis. Rofo 2005;177:555–63. [DOI] [PubMed] [Google Scholar]
- 20. Klauser AS, Sailer-Hoeck M, Abdellah MMH. et al. Feasibility of ultrasound-guided sacroiliac joint injections in children presenting with sacroiliitis. Ultraschall Med 2016;37:393–8. [DOI] [PubMed] [Google Scholar]
- 21. Wendling D. Local sacroiliac injections in the treatment of spondyloarthritis. What is the evidence? Joint Bone Spine 2020;87:209–13. [DOI] [PubMed] [Google Scholar]
- 22. Kokar S, Kayhan Ö, Şencan S, Gündüz OH.. The role of sacroiliac joint steroid injections in the treatment of axial spondyloarthritis. Arch Rheumatol 2021;36:80–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article cannot be shared publicly owing to the privacy of individuals who participated in the study. The data will be shared on reasonable request to the corresponding author.