Abstract
Objectives
Since the 1980s, life expectancy at birth (e0) in the United States has fallen steadily behind that of other high-income countries, widening the U.S. e0 disadvantage. We estimate how that disadvantage was affected by high mortality rates in 2020, the first full year of the coronavirus disease 2019 pandemic.
Methods
We contrast male and female e0 in the United States and 18 peer countries for years 1980, 1995, 2010, 2019, and 2020. Using Arriaga decomposition, we show how differences in age-specific death rates have contributed to U.S. e0 disadvantages.
Results
In 2020, U.S. male and female e0 changed by −2.33 (−2.50, −2.15) and −1.69 (−1.85, −1.53) years, respectively, whereas corresponding changes in peer countries averaged −0.67 (−0.82, −0.51) and −0.50 (−0.65, −0.35) years, respectively. This accelerated a longstanding and widening U.S. e0 disadvantage relative to its peers, which increased from 3.49 to 5.15 years in males and from 2.78 to 3.97 years in females between 2019 and 2020. Whereas deaths before age 65 accounted for 55% and 40% of declines in U.S. male and female life expectancy, respectively, they accounted for only 24% and 11% of the respective declines in peer countries.
Discussion
U.S. life expectancy declines in 2020 were larger than in peer countries and involved deaths across a broader age range, particularly among young and middle-aged adults. Both the longstanding U.S. e0 disadvantage and acute losses of life in 2020 signal the need for systemic policy changes in the United States.
Keywords: Comparative demography, Epidemiology, Health disparities, Life expectancy, Measurement
Since the 1980s, increases in U.S. life expectancy have been smaller than increases in other high-income countries, steadily widening the gap between the United States and its peers. In 2019, the United States ranked 40th among all countries on life expectancy at birth (World Health Organization, 2021). The low and worsening international ranking of the United States in life expectancy and other measures of health has motivated research to understand the underlying causes of these trends (Avendano & Kawachi, 2014; Reynolds & Avendano, 2018; Woolf et al., 2018). The National Academies of Sciences, Engineering, and Medicine (NASEM) has published three consensus studies on the topic: the first examining U.S. mortality after age 50 relative to peer countries (National Research Council [NRC], 2011); the second documenting a U.S. health disadvantage up to age 75 (National Research Council and Institute of Medicine [NRC & IOM], 2013); and the third focusing on high and rising mortality rates among “working age” Americans (i.e., aged 25–64; NASEM, 2021).
The 2020 mortality consequences of the global coronavirus disease 2019 (COVID-19) pandemic varied considerably across high-income countries. The United States experienced higher all-cause mortality than most other countries (Aburto, Kashyap et al., 2021; Bilinski & Emanuel, 2020; Woolf et al., 2020; Woolf, Masters et al., 2021). U.S. excess deaths in 2020 increased at higher rates among younger adults (Rossen et al., 2020) and were disproportionately concentrated among U.S. Black, Indigenous, and Latinx populations (Andrasfay & Goldman, 2021; APM Research Lab, 2021; Arias et al., 2021; Rossen et al., 2020; Woolf, Chapman et al., 2021). In an earlier study (Woolf, Masters, & Aron, 2021), we compared U.S. life expectancy and average life expectancy in 16 other high-income countries between 2010 and 2020. That study used earlier data, compared life expectancy between 2018 and 2020, excluded several large high-income countries for lack of data (e.g., Canada, Germany, and Italy), and used the Human Mortality Database (HMDB)—Short-Term Mortality Fluctuation data. The latter uses wide age intervals to report 2020 mortality rates rather than the death counts available in original source data files.
In this study, we estimate how increases in all-cause mortality in 2020, the first full year of the COVID-19 pandemic, affected the life expectancy differences between the United States and its peers, with special attention given to age patterns. This study improves on the prior analysis by including Canada, Germany, and Italy in the peer comparison group; updating the 2020 death counts from September 2021 data releases; using weekly death counts from original sources to calculate mortality rates at more granular, 5-year age intervals; and providing life expectancy changes between 2019 and 2020 for all countries. We review differences in countries’ age-specific mortality risk (nqx) and life expectancy at birth (e0) for years 1980, 1995, and 2010. We then use novel methods to estimate these for 2019 and 2020. Finally, we decompose e0 differences to determine how deaths at specific ages contributed to the growing U.S. life expectancy disadvantage (a) between 1980 and 2019 and (b) again in 2020, when the COVID-19 pandemic was spreading globally. We show that, between 1980 and 2019, U.S. male and female e0 became an increasing outlier among its peers, mostly due to relatively poorer survival trends at older ages (i.e., ages 65 and older). Between 2019 and 2020, however, increases in U.S. mortality rates at nearly all ages exacerbated the outlier status of U.S. e0, with large mortality increases at younger ages disproportionately contributing to the 2020 declines in U.S. e0.
Analytic Strategy
We contrast male and female life expectancy at birth (e0) in the United States and among 18 other high-income countries for years 1980, 1995, 2010, 2019, and 2020 (see Author Note 1). We also compare countries based on their estimated mortality risk (nqx) for ages (15–65), (65–85), and (85–95) in each of these years. We decompose the age-specific mortality contributions to the e0 gap—the differences between the U.S. e0 and the composite e0 estimated from peer countries’ average nqx and ax—in all years to determine how trends in age-specific death rates affected changes in the gap (a) between 1980 and 2019 and (b) from 2019 to 2020. We also decompose the age-specific mortality contributions to changes in each country’s e0 between 2019 and 2020 to highlight between-country variation in the ages most affected by increases in deaths in 2020.
U.S. Life Table Data
We report U.S. male and female nqx and e0 from official U.S. life tables for years 1980 (NCHS, 1984), 1995 (NCHS, 1998), and 2010 (Arias et al., 2014). We sum weekly age-specific death counts among the U.S. male and female populations in 2018, 2019, and 2020 (NCHS, 2021) and merge them with male and female population estimates derived from U.S. Census Bureau (USCB, 2019) to calculate 2018, 2019, and 2020 all-cause death rates (mx) for the 15-year age group (0–15), and for 5-year age groups (15–20), …, (80–85), and for all ages 85 and older. We calculate mx ratios (RRs) between the 2020 estimates and the 2018 estimates and the 2019 estimates and 2018 estimates in these data and combine these age-specific RRs with the 2018 official 5-year abridged life tables (Arias & Xu, 2020) to estimate 5-year abridged life tables for 2019 and 2020 (see Supplementary Appendix for details; see Author Note 2).
Peer Country Life Table Data
We obtain 5-year abridged male and female life tables for each peer country from the HMDB for 1980, 1995, and 2010 (HMDB, 2021). Some countries’ life tables in 2019 are obtained from HMDB. For Germany, 1980 life table data are for West Germany alone; 2018 and 2019 life tables are obtained directly from the Federal Statistical Office of Germany (Destatis, 2021). Direct sources were also used to generate 2019 life tables for New Zealand (Stats NZ, 2021) and Israel (CBS, 2021). We obtain estimates for peer country’s male and female weekly 2018, 2019, and 2020 age-specific death counts from the HMDB—Short-Term Mortality Fluctuations original input data (HMDB-STMF, 2021a). Age-specific death rates (mx) for each peer countries’ male and female populations in 2018, 2019, and 2020 were calculated by merging the death counts with age-specific population counts from each country’s official statistical agency. We then calculate mortality rate ratios (RR) between 2020 mx and 2018 mx and 2019 mx and 2018 mx for each peer country’s male and female populations. Original input data for Canada, New Zealand, and the Netherlands provide no additional age-specific information than the mx estimates in the HMDB-STMF. For these three countries, we therefore calculate RRs using the 2018, 2019, and 2020 mx for ages (0–15), (15–65), (65–75), (75–85), and 85+ (HMDB-STMF, 2021b). To estimate 2019 and 2020 life tables for each country’s male and female populations, we combine the estimated age-specific RRs with 2018 HMDB life tables.
Simulating 2020 Life Tables
We use Python (version 3.9.1) to simulate 50,000 2020 life tables for each country’s male and female populations. We simulate each country’s 2020 life table using estimated 2020 nqx with 10% random uncertainty and each population’s 2018 ax. We report the median estimates (P50) for countries’ 2020 e0 and the median estimates of the 2019–2020 change in each country’s e0. We indicate uncertainty in all 2020 estimates by providing the values of the fifth (P5) and ninety-fifth (P95) percentiles in the simulated distributions. Finally, we report the average P50, P5, and P95 for 2020 e0 among peer populations and the average 2019–2020 changes in peer e0 and contrast these with the P50, P5, and P95 estimates for 2020 U.S. e0 and the 2019–2020 changes in U.S. e0.
Decomposition of Life Expectancy Differences
We use Arriaga decomposition to estimate the contribution of age-specific deaths to male and female e0 differences between the United States and a peer composite life table estimated from the average nqx and average ax in 1980, 1995, 2010, 2019, and 2020 (Arriaga, 1984). We calculate age-specific contributions to e0 differences as:
where is the contribution of deaths between ages x and x + n to the difference in male and female e0 between the United States and the peer composite in time t, where t = 1980, …, 2020; l0 is a hypothetical cohort of 100,000 persons; lx is the number of cohort members alive at age x; and nLx is the number of person-years lived between age x and x + n, for age groups (0–1), (1–4), (5–9), …, (90–95), and (95–100). For the open-ended age group 100+, the contribution to e0 differences is estimated as:
We also decompose differences in 2020 male and female e0 and 2019 male and female e0 for the United States and for each peer country. We compare e0 changes in peer countries with the United States to identify differences in how age-specific deaths contributed to 2019–2020 e0 changes.
Results
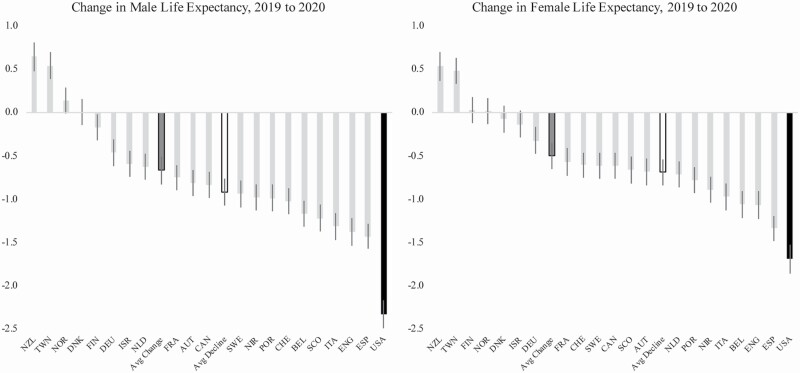
Table 1 presents life expectancy at birth (e0) for U.S. male and female populations and the average e0 among peer male and female populations for years 1980, 1995, 2010, and 2019. For 2020, we show P50e0 from simulated life tables as well as P5 and P95 to provide a range of 2020 e0 estimates. The minimum (Min), maximum (Max), and standard deviation (S) for peers’ e0 are also included to contrast U.S. e0 against the peer distribution. Also, Figure 1 graphs female and male e0 changes between 2019 and 2020 for the United States and every peer country to display the range of e0 changes across countries (see Supplementary Appendix for a table containing data for individual countries).
Table 1.
U.S. Female and Male Life Expectancy at Birth and Average Female and Male Life Expectancy at Birth in 18 Peer Countries, 1980, 1995, 2010, 2019, and 2020
| Peer country comparison group | United States | |||||||
|---|---|---|---|---|---|---|---|---|
| (P5, P95) | e 0 | S | Min | Max | (P5, P95) | e 0 | Z-score | |
| Female population | ||||||||
| 2020 | (83.54, 83.94) | 83.69 | 1.10 | 80.60 | 85.06 | (79.56, 79.88) | 79.72 | −3.61 |
| 2019 | 84.19 | 1.11 | 81.26 | 86.21 | 81.41 | −2.50 | ||
| 2010 | 83.05 | 1.10 | 80.61 | 85.00 | 81.04 | −1.83 | ||
| 1995 | 79.99 | 1.35 | 77.64 | 81.90 | 78.90 | −0.81 | ||
| 1980 | 77.13 | 1.51 | 74.48 | 79.17 | 77.50 | 0.25 | ||
| Male population | ||||||||
| 2020 | (79.01, 79.32) | 79.16 | 1.21 | 76.06 | 81.32 | (73.84, 74.19) | 74.01 | −4.21 |
| 2019 | 79.83 | 1.21 | 77.28 | 81.89 | 76.34 | −2.88 | ||
| 2010 | 78.25 | 1.41 | 76.14 | 81.52 | 76.20 | −1.45 | ||
| 1995 | 74.00 | 1.59 | 71.86 | 78.82 | 72.50 | −0.94 | ||
| 1980 | 70.78 | 1.87 | 68.11 | 75.74 | 70.00 | −0.42 | ||
Notes: Peer country source: Human Mortality Database 5 X 1 Period Life Tables, 1980, 1995, 2010. US source: Official United States Life Tables, 1980, 1995, 2010. Z-score for the United States is calculated as (U.S.–peer average)/peer standard deviation.
Figure 1.
Changes in male and female life expectancy at birth, 2019–2020, in the United States and 18 other high-income countries. Note: Vertical lines indicate the error range (P5 to P95) in the estimated e0 change.
In 1980, e0 in the U.S. female population was higher than the average e0 among peer female populations (77.50 vs. 77.13 years), although the difference was relatively small (Z-score 0.25). Life expectancy at birth in 1980 in the U.S. male population was lower than the average male e0 in peer countries (70.00 vs. 70.78 years), but the difference was relatively small (Z-score −0.42). In the three decades spanning 1980 and 2010, e0 in both U.S. male and female populations steadily fell behind the average e0 in peer male and female populations, largely because mortality reductions in peer countries outpaced those in the United States. By 2010, male and female e0 in the United States were more than 2 years shorter than the corresponding average e0 in peer countries. This trend continued in the following decade from 2010 to 2019, during which U.S. female e0 increased by only 0.37 years (81.04–81.41 years), while average e0 among peer female populations increased by 1.14 years. Similarly, from 2010 to 2019, U.S. male e0 increased by only 0.14 years (76.20–76.34 years), while the average e0 among peer male populations increased by 1.58 years. By 2019, U.S. female and male e0 were conspicuous outliers among high-income countries; both were over 2 SD below the peer averages.
Between 2019 and 2020, we estimate that U.S. female e0 declined by 1.69 years (P5 = −1.85, P95 = −1.53) to 79.72 years (79.56, 79.88). In contrast, the average change in female e0 in peer countries was much smaller, declining only 0.50 years (−0.65, −0.35) to 83.69 years (83.54, 83.94). Between 2019 and 2020, U.S. male e0 declined by 2.33 years (−2.50, −2.15) to 74.01 years (73.84, 74.19), whereas in peer countries the average change in male e0 was −0.67 years (−0.82, −0.51) to 79.16 years (79.01, 79.32). Thus, 2020 decreases in U.S. female and male e0 were about 3.5 times greater than the corresponding average 2020 decreases in peer countries.
Figure 1 shows the large declines in U.S. female and male e0 between 2019 and 2020 and the range of outcomes across peer countries. Two countries experienced an increase in female and male e0, 0.48 years (0.33, 0.48) and 0.54 years (0.37, 0.72) in Taiwan, and 0.53 years (0.40, 0.67) and 0.65 years (0.50, 0.80) in New Zealand, respectively. Among peer countries experiencing decreases in e0, decreases in female e0 ranged from 0.32 years in Germany (−0.47, −0.17) to 1.33 years in Spain (−1.48, −1.19), while decreases in male e0 ranged from 0.17 years in Finland (−0.33, −0.01) to 1.43 years in Spain (−1.59, −1.27). No country experienced e0 declines comparable to those in the United States: the upper bound of error (P95) for Spain, the country with the largest decline in e0 among the peer group, was still much lower than the U.S. decline.
Mortality in 2020 significantly widened the longstanding e0 gap between the United States and its peer countries. The difference in male e0 between the United States and its peers grew from −0.78 years (U.S. Z-score = −0.42) to −3.49 years (U.S. Z-score = −2.88) between 1980 and 2019 and then increased to −5.15 years (U.S. Z-score = −4.21) between 2019 and 2020. And for female e0, the difference between the United States and its peers reverted from a 0.37-year advantage (U.S. Z-score = 0.25) to a 2.78-year disadvantage (U.S. Z-score = 2.50) between 1980 and 2019, and that disadvantage increased to 3.97 years (U.S. Z-score = −3.61) between 2019 and 2020.
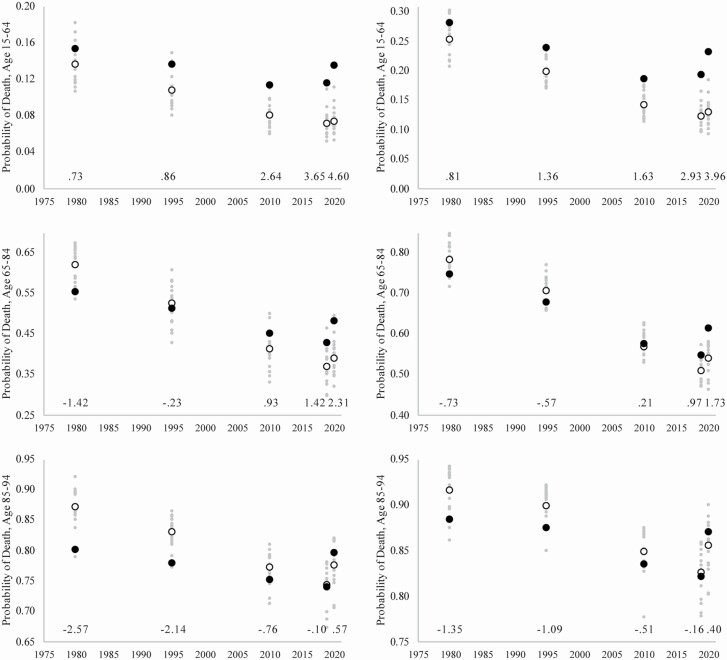
Figure 2 plots the probability of death between ages 15–64 (50q15), 65–84 (20q65), and 85–94 (10q85) for male and female populations in the United States and peer countries. Between 1980 and 2010, 50q15 in the United States became an increasingly conspicuous outlier among its peers, as U.S. reductions in younger-age mortality failed to keep pace with reductions in peer countries.
Figure 2.
Probability of death at ages 15–64, 65–84, and 85–94 among female populations and male populations. Note: Black circle indicates the United States, white circle indicates peer country average, and small gray circles denote individual peer countries. Numbers above x-axis indicate Z-score for U.S. probability relative to peer average probability.
In the following decade, however, between 2010 and 2019, male and female 50q15 continued to decline in peer countries but both increased in the United States. And between 2019 and 2020, male and female 50q15 increased considerably in the United States but remained relatively stable for men and women in peer countries. The distinctly high 50q15 that made the United States an increasing outlier from peer countries between 1980 and 2019 grew even larger in 2020, reflecting the COVID-19 pandemic’s disproportionate mortality effect on U.S. young adults (Rossen et al., 2020).
In 1980, the probability of death between ages 65 and 85 (20q65) was lower in the United States compared to peer countries, but that advantage eroded to near parity in the mid-1990s and reverted to a disadvantage thereafter. Male and female 20q65 were higher in the United States than in peer populations in 2010 and 2019 due to relatively smaller declines in U.S. 20q65 during that decade. The 2020 increases in 20q65 among the U.S. male and female populations were much larger than the respective increases in peer populations, once again exacerbating the outlier status of the United States.
Although U.S. men and women at oldest ages (i.e., 85+) have historically experienced lower mortality rates than their counterparts in peer countries, that advantage narrowed between 1980 and 2019 as declines in 10q85 among peer populations exceeded those of U.S. populations (Ho & Preston, 2010; NASEM, 2021; Palloni & Yonker, 2016; NRC, 2011). And between 2019 and 2020, 10q85 among U.S. men and women increased much more than among peer populations and for the first time exceeded the respective 10q85 averages in peer countries. The mortality advantage that U.S. adults of advanced age had experienced for decades ended in 2020, when the COVID-19 pandemic elevated U.S. 10q85 to levels not seen since the 1980s.
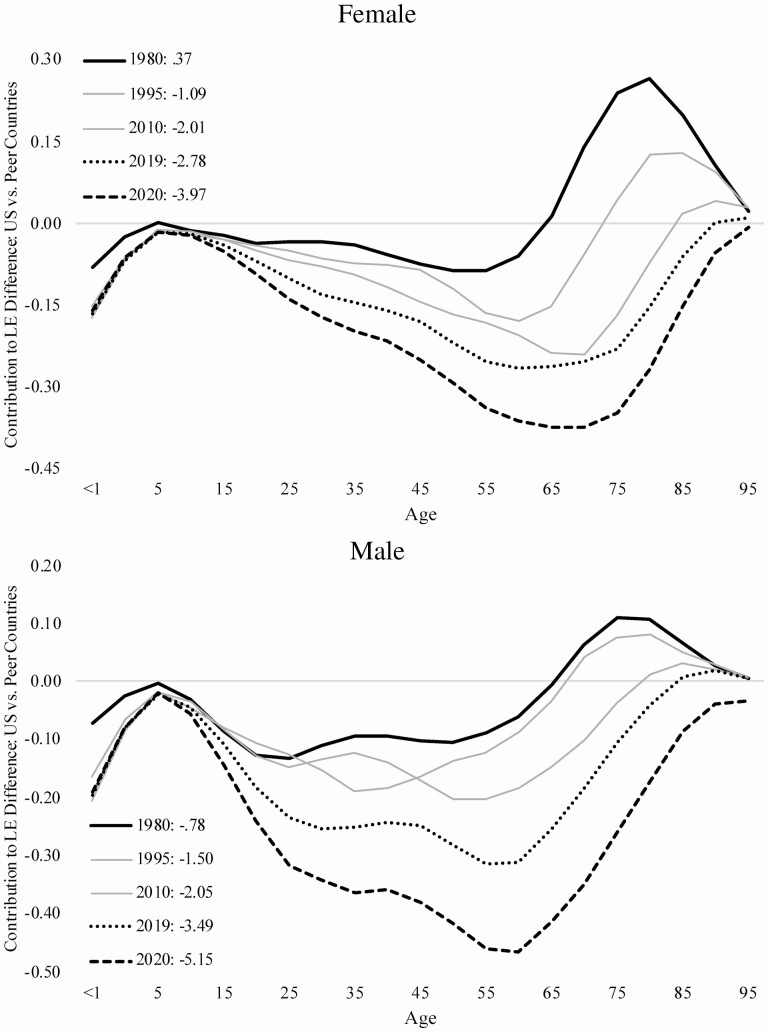
Figure 3 plots the results from Arriaga decompositions of U.S.–peer differences in female and male e0 for years 1980, 1995, 2010, 2019, and 2020. It shows how U.S.–peer differences in age-specific death rates contributed to e0 gaps in each year. Positive values on the y-axis indicate survival advantages for U.S. populations relative to peers and negative values indicate survival disadvantages.
Figure 3.
Contributions of age-specific deaths to differences between U.S. life expectancy and peer country averages among women and men, 1980, 1995, 2010, 2019, and 2020. Note: The numbers in the figure legends indicate the size (in years) of U.S.–peer life expectancy differences.
For example, the 1980 U.S. female e0 advantage of 0.37 years was due entirely to survival advantages experienced by older U.S. women (aged 65–95). Figure 3 shows that, compared to the peer country composite female e0, the U.S. female population in 1980 was disadvantaged by greater loss of life in infancy and young childhood (0–4) and in younger and middle-aged adulthood (20–64). However, the survival advantage among U.S. women aged 65–95 years more than offset these mortality disadvantages, yielding an overall 0.37-year e0 advantage compared to women in peer countries. Yet, by 2019, that advantage had become a 2.78-year disadvantage for U.S. women, the product of a 3.15-year relative reduction in e0 caused by a deepening U.S. female survival disadvantage among (a) infants and young children (aged 0–4), accounting for 4% of the 3.15-year loss in relative life expectancy, (b) adolescents and young adults (aged 15–39; 10%), (c) middle-aged adults (aged 40–64; 23%), and (d) older adults (aged 65–99; 63%).
These trends worsened in 2020, except for those at the very youngest ages (Figure 3). The increase in the U.S.–peer female e0 gap between 2019 and 2020 (1.19 years) accounted for 27% of the total change in that gap between 1980 and 2020 (4.34 years). The age patterns of e0 losses among the U.S. female population in 2020, which continued longer-term trends between 1980 and 2019, highlight that the U.S. survival disadvantage now reflects a broader age range than past research has indicated (Ho, 2013; Ho & Hendi, 2018; NRC & IOM, 2013). For example, although past research has emphasized the U.S. mortality disadvantage for younger adults (e.g., below age 50), these deaths have contributed less and less to the U.S.–peer e0 gap over time. Whereas about 60% of the U.S. female survival disadvantage in 1980 was due to deaths before age 50, the respective proportions in 1995, 2010, and 2019 were 46%, 38%, and 37%, respectively. By 2020, only about one third of the U.S.–peer female e0 gap was due to deaths before age 50. Between 1980 and 2020, deaths between ages 65 and 85 contributed most to the worsening U.S.–peer female e0 gap.
Figure 3 shows that U.S. males had a relative survival advantage at older ages (65 and older) in 1980, but loss of life in infancy and young childhood and at ages 15–64 produced a 0.78-year U.S.–peer e0 gap. By 2019, the gap had widened to 3.49 years, due to a worsening U.S. survival disadvantage during (a) infancy and childhood (ages 0–14; accounting for 7% of the 2.71-year relative e0 loss), (b) adolescence and young adulthood (ages 15–39; 19%), (c) middle-aged adulthood (ages 40–64; 37%), and (d) a survival advantage in older adulthood (ages 65 and older) that reverted to a disadvantage (36%). As such, older-aged mortality exerted a growing influence on the gap in male e0 over time. Indeed, the contribution of deaths before age 50 to the U.S. gap in male e0 was over 70% in 1980 (74%) and 1995 (77%), but dropped to 60% in 2010 and 54% in 2019, and was only 47% in 2020.
As occurred with the U.S. female population, conditions in 2020 exacerbated these trends, except at the very youngest ages, and the U.S.–peer male e0 gap in 2020 widened to 5.15 years. The change in the U.S.–peer male e0 gap between 2019 and 2020 (−1.66 years) accounted for 38% of the total change in that gap between 1980 and 2020 (−4.37 years).
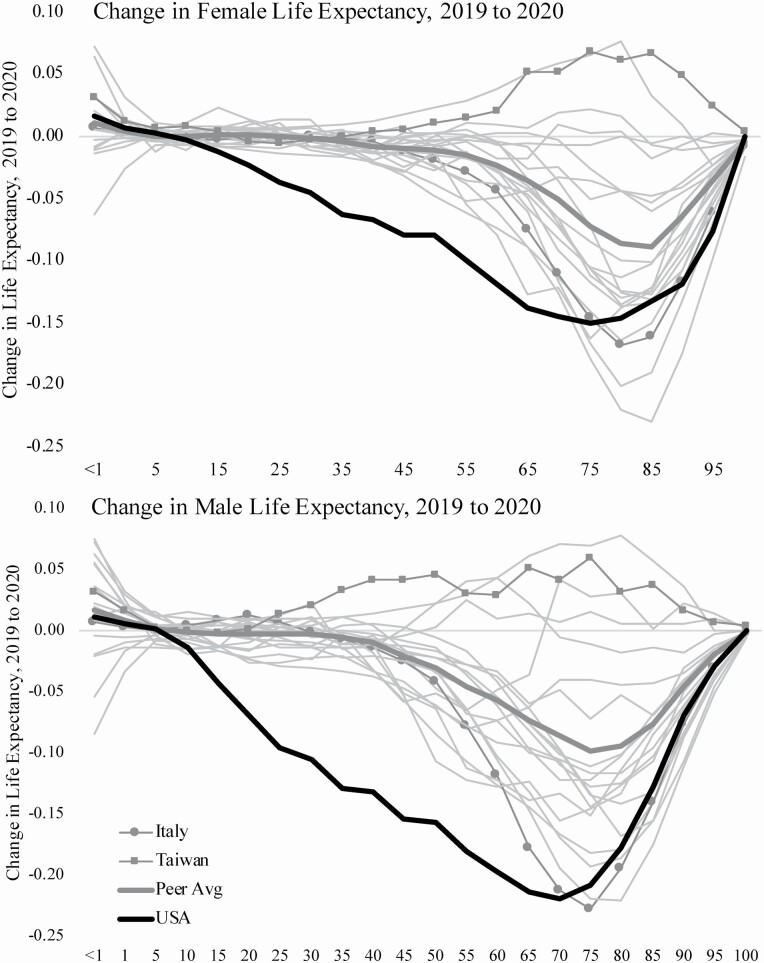
Figure 4 plots the results of Arriaga decompositions showing how loss of life at each age contributed to changes in each country’s e0 between 2019 and 2020. Age-specific changes in U.S. e0 between 2019 and 2020 (bold black line) are contrasted with the average change in peer countries (bold gray line) and with changes in two countries with diverse outcomes: Italy—which experienced relatively high excess deaths in 2020—and Taiwan—where e0increased between 2019 and 2020. The contrast underscores the larger loss of U.S. e0 in 2020, as well as the younger ages at which this loss occurred.
Figure 4.
Contributions of age-specific deaths to changes in life expectancy between 2019 and 2020 in the United States and peer countries. Note: Bolded black line indicates the United States, bolded gray line indicates average of peer countries, square markers indicate Taiwan, circle markers indicate Italy, and light gray lines indicate other peer countries.
In Taiwan, the increase in male and female e0 between 2019 and 2020 resulted from mortality reductions at all ages, although most gains were made among older-aged adults. For example, 45% of the 2020 increase in Taiwan’s male e0 was due to reductions in death rates older than age 65, with 10% due to reductions in death rates for ages older than 85. And 80% of the increase in Taiwan’s female e0 reflected improved survival after 65, with nearly a third of the increase due to improved survival after age 85.
In Italy and the United States, e0 losses between 2018 and 2020 were larger than in other high-income countries, yet notable differences in the two countries’ losses are observed by age and sex. In Italy, the loss of life in 2020 was heavily concentrated at older ages. Only about 17% of the loss in male e0 between 2019 and 2020 involved deaths below age 65; in fact, at all ages younger than 35, male survival in Italy actually improved in 2020. It was deaths after age 40 that contributed to Italy’s 1.36-year decline in male e0 between 2019 and 2020; deaths between ages 65 and 85 contributed to 63% of this decline, and deaths after age 85 contributed 17%. The decline in Italy’s female e0 in 2020 was even more heavily concentrated at older ages. Only about 10% of the decline was due to deaths before age 65; 52% was attributable to deaths between ages 65 and 85, and 37% was due to deaths after age 85.
In contrast, reductions in U.S. male and female e0 were both larger and more evenly distributed across ages than those in Italy. Deaths before age 65 accounted for about 38% of the U.S. female e0 decline between 2019 and 2020 and the majority (54%) of the U.S. male e0 decline. Nearly one third of the decline in U.S. male e0 was due to deaths between ages 15 and 50. Deaths between ages 65 and 85 accounted for only 43% of the decline in female e0 and only 37% of the decline in male e0. Finally, deaths after age 85 accounted for about 19% of the U.S. decline in female e0 and only 9% of the decline in male e0. Notwithstanding the large losses in Italy e0, Figure 4 shows that changes in U.S. e0 between 2019 and 2020 were more conspicuous outliers, both in the absolute size of the declines and in the young age profile of these losses.
Discussion
On almost all measures of population health and survival, the United States has been on a downward trajectory relative to other high-income countries since the late 1970s. A major 2013 report by the NRC and the IOM documented a widespread “U.S. health disadvantage” and identified potential causes and solutions (NRC & IOM, 2013). The report noted the “limited political support among both the public and policymakers to enact the policies and commit the necessary resources” as important reasons for the steady decline in U.S. health rankings. These policies and resources span not only health care and biomedical research, but also social, economic, and environmental spheres, which shape the nonmedical or social determinants of health and the risk factors related to disease and injury (Berkman, 2009; Braveman & Gottlieb, 2014; Gutin & Hummer, 2021; Link & Phelan, 1995; Phelan et al., 2010; Pickett & Wilkinson, 2015; Schoeni et al., 2008; Williams et al., 2019).
The United States entered 2020 in a fundamentally weakened state in terms of its overall population health, so the findings of this current analysis come as no surprise. The United States stands out from peer countries in excess deaths in 2020, largely due to the COVID-19 pandemic; the disproportionate impact of these deaths on younger adults; and the enormous racial and ethnic disparities in COVID-19 infections, hospitalizations, and deaths (Ahmad, Cisewski et al., 2021; APM Research Lab, 2021; Arias et al., 2021; Rossen et al., 2020; Woolf, Chapman et al., 2021). Most high-income democracies were more effective in protecting the health of their populations before and during the first year of the COVID-19 pandemic (Bilinski & Emanuel, 2020).
Cross-national studies such as this one can provide critical insights into underlying vulnerabilities and resiliencies of national populations, many of which are amenable to policies and interventions. In this case, it will be important to learn from countries that more successfully managed the early stages of the pandemic. For example, this study contrasts patterns in countries with large losses of life in 2020—the United States and Italy—with Taiwan, which saw its life expectancy increase and highlighted differences in affected age groups. Comparisons of the epidemiology, culture, and policy choices of countries with disparate outcomes can provide important clues for further research and evidence-informed action (Council on Foreign Relations, 2020; Parker, 2021; Shokoohi et al., 2020). Indeed, there is a critical need to examine the policies and decisions that left the United States so ill-prepared to sustain and respond to a global pandemic; that enabled uncontrolled viral transmission, which overwhelmed the health care system and claimed more than 500,000 lives in 2020 (Woolf, Chapman et al., 2021); and that can guide the country through the remaining stages of the pandemic and prepare it for future public health crises.
The findings presented here should concern Americans of all ages. Compared to their peers in other high-income countries, they are least likely to reach age 65. This was true in 1980 (Figure 2), but the United States has only slipped further behind since then. By 2019, the probability that U.S. women and men would die between ages 15 and 64 was 63% and 58% higher, respectively, than those residing in peer countries. A recent National Academies report focused attention on the high mortality rates of young and middle-aged U.S. adults. These rates have substantially increased relative to peer countries (NASEM, 2021) and were exacerbated in 2020 by younger-aged Americans’ disproportionately higher mortality rates. These deaths are not only claiming Americans in the prime of life, but also creating profound ripple effects for children, families, and communities through the loss of essential caregiving, employment, economic productivity, and social security (Bosman, 2021).
Nor do these findings bode well for older-aged Americans. For many years, the disproportionately high mortality rates in the United States had one notable exception: Americans older than age 65 were less likely to die than those in peer countries (Ho & Preston, 2010; NRC, 2011; NRC & IOM, 2013; Palloni & Yonker, 2016). Our study finds that this small health advantage has been lost. The probability of surviving to age 85 is now lower in the United States than in peer countries, and the probabilities of dying between ages 65 and 84 and between ages 85 and 94 are now higher. These changes carry profound implications for older-age survival in the United States and the U.S. mortality gap. Indeed, the relative loss of life among Americans older than age 65 has been the greatest contributor to the widening U.S.–peer life expectancy gap, and U.S.–peer differences in older-aged mortality will likely be the predominant driver of future trends after the COVID-19 pandemic.
This study has several limitations to consider. First, the peer countries chosen for comparison differ from those examined in existing cross-country analyses of life expectancy trends (NRC, 2011; NRC & IOM, 2013). Data limitations precluded inclusion of some high-income countries (e.g., Australia, Japan) that future work should examine. Second, the study relies on provisional data to estimate 2020 life expectancy, and some between-country differences might reflect proficiency in accurately and fully reporting 2020 deaths (see Author Note 3). Third, the analysis is limited to 2020. Future cross-national comparisons should look beyond 2020 to fully document the full range of health and mortality outcomes of the pandemic. Fourth, the mortality consequences of the pandemic have differed considerably in the United States by race/ethnicity, with disproportionately higher deaths among Black, Latino/a, and Indigenous populations. Future work should examine age-specific patterns in racial/ethnic inequities in U.S. lives lost in 2020, as U.S. mortality in 2020 fell on predictable race/ethnic lines in American society due to policies, decisions, and actions shaped by systemic racism and its attendant injustices (Woolf, Chapman et al., 2021). Finally, we did not decompose 2019–2020 life expectancy changes by cause of death. While the vast majority of the changes are directly attributable to the broad mortality consequences of the COVID-19 pandemic, some changes in the U.S.–peer life expectancy gap might reflect mortality trends that predate the pandemic such as rising drug-related deaths in the United States (Ahmad, Rossen et al., 2021; Friedman & Hansen, 2022).
This study builds on prior research on the broad effects of the COVID-19 pandemic on U.S. life expectancy in 2020. For example, Andrasfay and Goldman (2021) calculated that total life expectancy in the United States declined by 1.31 years in 2020 due to COVID-19-related deaths, and provisional life tables published by NCHS suggest that U.S. female and male life expectancy declined by 1.5 and 2.1, respectively, in 2020 (Murphy, Kochanek et al., 2021). We previously published a comparison of changes in life expectancy in the United States and peer countries in 2020, reporting reductions between 2018 and 2020 of 1.50 and 2.16 years for females and males in the United States, respectively, and 0.13 and 0.29 in peer countries (N = 16). Later that year, Aburto, Schöley et al. (2021) estimated 2019–2020 declines in U.S. female and male life expectancy of 1.65 and 2.23 years, respectively. Here, we report slightly larger reductions in U.S. life expectancy than we previously estimated, 1.69 years and 2.33 years, which are statistically and substantively nondifferent from estimates in the work of Aburto, Schöley et al. (2021). Likewise, the larger reductions in female and male life expectancy in peer countries, 0.50 years and 0.67 years, respectively, also reflect changes from 2019 instead of 2018, greater precision in death counts derived from more recent data, and a larger pool of comparison countries (N = 18).
In 2020, the COVID-19 pandemic exposed longstanding deficiencies in U.S. investments in public health leadership and infrastructure (Mendenhall, 2020; Samet et al., 2017), the quality and consistency of public health messaging and communications (Finset et al., 2020; OECD, 2020; Shah, 2020), and Americans’ trust in public health officials and agencies (Hotez, 2021; Weiss & Paasche-Orlow, 2020). These and other issues deserve greater policy research, both to investigate their connections to health outcomes such as those documented here and to inform policy development going forward. Pandemic-specific policies deserving greater scrutiny include school and business closings and openings, social distancing and mask-wearing, travel bans and restrictions, housing and eviction prevention, employment and income protection and safety net programs, and vaccine distribution and access. Policy studies comparing specific national and subnational approaches will be critical to learning how this pandemic could have been managed more effectively and saved more lives. Unlike global viruses, policies and practices do know geographic boundaries. But more upstream policies and life conditions that perpetuate the longstanding U.S. health and longevity disadvantages will be especially important for understanding why 2020 was such a grim year for the United States, and why a “return to normal” postpandemic will leave the United States at a health and longevity disadvantage compared to its peers.
Supplementary Material
Acknowledgments
An earlier version of this paper was presented at the 2021 Annual Meeting of the TRENDS Network, May 13–14. We thank Catherine Talbot, MS, University of Colorado Boulder, for her advice with Python simulations. We also thank Bob Schoeni, Neil Mehta, and participants of the TRENDS Network for helpful feedback on an earlier version of this manuscript. The views expressed are those of the authors alone and do not represent those of their employers or any funding agency.
Contributor Information
Ryan K Masters, Department of Sociology, University of Colorado Boulder, Boulder, Colorado, USA; University of Colorado Population Center, Boulder, Colorado, USA.
Steven H Woolf, Center on Society and Health, Virginia Commonwealth University, Richmond, Virginia, USA.
Laudan Y Aron, Health Policy Center, Urban Institute, District of Columbia, USA.
Author Note
1. The 18 countries comprising the peer comparison group are Austria, Belgium, Canada, Denmark, Finland, France, Germany, Israel, Italy, the Netherlands, New Zealand, Norway, Portugal, Spain, Sweden, Switzerland, Taiwan, and the United Kingdom (England and Wales, Northern Ireland, and Scotland were analyzed separately such that the peer comparison group is composed of 20 cases). The countries comprising the peer comparison group are all high-income advanced democracies, and the composition of the group is similar to existing international analyses of life expectancy (NASEM, 2021; NRC & IOM, 2013; NRC, 2011; Woolf, Masters et al., 2021). However, data limitations preclude the inclusion of some countries that often appear in peer comparison groups (e.g., Australia, Japan, and South Korea).
2. We do not generate 2020 life tables from the 2020 NCHS-Census data because deaths at older ages are underestimated in national vital statistics data (Anderson, 1999; Arias, 2012). See Supplementary Appendix for the biasing effects of these undercounts on 2020 life expectancy estimates.
3. See Supplementary Appendix for stability of e0 estimates across data release dates.
Funding
Funding for this research was provided by the National Institute on Aging (P30AG012846), the Eunice Kennedy Shriver National Institute of Child Health and Human Development (2P2CHD066613), and by the National Center for Advancing Translational Sciences (UL1TR002649). This paper was published as part of a supplement sponsored by the University of Michigan with support from the National Institute on Aging (P30AG012846).
Conflict of Interest
None declared.
References
- Aburto, J. M., Kashyap, R., Schöley, J., Angus, C., Ermisch, J., Mills, M. C., & Dowd, J. B. (2021). Estimating the burden of the COVID-19 pandemic on mortality, life expectancy and lifespan inequality in England and Wales: A population-level analysis. Journal of Epidemiology and Community Health, 75(8), 735–740. doi: 10.1136/jech-2020-215505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aburto, J. M., Schöley, J., Kashnitsky, I., Zhang, L., Rahal, C., Missov, T. I., Mills, M. C., Dowd, J. B.,& Kashyap, R. (2021). Quantifying impacts of the COVID-19 pandemic through life-expectancy losses: A population-level study of 29 countries. International Journal of Epidemiology, 51(1), 63–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmad, F. B., Cisewski, J. A., Miniño, A., & Anderson, R. N. (2021). Provisional mortality data—United States, 2020. Morbidity and Mortality Weekly Report, 70(14), 519. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm#citation [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmad, F. B., Rossen, L. M., & Sutton, P. (2021). Provisional drug overdose death counts. National Center for Health Statistics. [Google Scholar]
- Anderson, R. N. (1999). Method for constructing complete annual US life tables (Vol. 129). National Center for Health Statistics. [PubMed] [Google Scholar]
- Andrasfay, T., & Goldman, N. (2021). Association of the COVID-19 pandemic with estimated life expectancy by race/ethnicity in the United States, 2020. JAMA Network Open, 4(6), e2114520. doi: 10.1001/jamanetworkopen.2021.14520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- APM Research Lab . (2021) The color of coronavirus: COVID-19 deaths by race and ethnicity in the U.S. (website). https://www.apmresearchlab.org/covid/deaths-by-race
- Arias, E. (2012). United States Life Tables, 2008. In National Vital Statistics Reports (Vol. 61, no. 3). National Center for Health Statistics. [PubMed] [Google Scholar]
- Arias, E. (2014). United States life tables, 2010. National Vital Statistics Reports, 63(7). National Center for Health Statistics. [PubMed] [Google Scholar]
- Arias, E., Tejada-Vera, B., Ahmad, F., Kochanek, K. D. (2021). Provisional life expectancy estimates for 2020. Vital Statistics Rapid Release (15). National Center for Health Statistics. doi: 10.15620/cdc:107201 [DOI] [Google Scholar]
- Arias, E., & Xu, J. (2020). United States life tables, 2018. National Vital Statistics Reports, 69(12). National Center for Health Statistics. [PubMed] [Google Scholar]
- Arriaga, E. E. (1984). Measuring and explaining the change in life expectancies. Demography, 21(1), 83–96. doi: 10.2307/2061029 [DOI] [PubMed] [Google Scholar]
- Avendano, M., & Kawachi, I. (2014). Why do Americans have shorter life expectancy and worse health than do people in other high-income countries? Annual Review of Public Health, 35, 307–325. doi: 10.1146/annurev-publhealth-032013-182411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman, L. F. (2009). Social epidemiology: Social determinants of health in the United States: Are we losing ground? Annual Review of Public Health, 30, 27–41. doi: 10.1146/annurev.publhealth.031308.100310 [DOI] [PubMed] [Google Scholar]
- Bilinski, A., & Emanuel, E. J. (2020). COVID-19 and excess all-cause mortality in the US and 18 comparison countries. Journal of the American Medical Association, 324(20), 2100–2102. doi: 10.1001/jama.2020.20717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosman, J. (2021, February 21). A ripple effect of loss. New York Times. [Google Scholar]
- Braveman, P., & Gottlieb, L. (2014). The social determinants of health: It’s time to consider the causes of the causes. Public Health Reports (Washington, D.C.: 1974), 129(Suppl. 2), 19–31. doi: 10.1177/00333549141291S206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Central Bureau of Statistics . (2021). Complete life tables of Israel 2014–2018. https://www.cbs.gov.il/en/publications/Pages/2020/Complete-Life-Tables-Of%20Israel-2014-2018.aspx
- Council on Foreign Relations . (2020). Improving pandemic preparedness: Lessons from COVID-19. Independent Task Force Report No. 78. Council on Foreign Relations. [Google Scholar]
- Destatis. (2021). Code 12621-001: Life table (period life table): Germany, period of years, sex, completed age. https://www-genesis.destatis.de/genesis//online?operation=table&code=12621-0001&bypass=true&levelindex=0&levelid=1623101602066#abreadcrumb
- Finset, A., Bosworth, H., Butow, P., et al. (2020). Effective health communication—A key factor in fighting the COVID-19 pandemic. Patient Education and Counseling, 103(5), 873. doi: 10.1016/j.pec.2020.03.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman, J. R., & Hansen, H. (2022). Evaluation of increases in drug overdose mortality rates in the US by race and ethnicity before and during the COVID-19 pandemic. JAMA Psychiatry. doi: 10.1001/jamapsychiatry.2022.0004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutin, I., & Hummer, R. A. (2021). Social inequality and the future of U.S. life expectancy. Annual Review of Sociology, 47(1), 501–520. doi: 10.1146/annurev-soc-072320-100249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- HMDB. (2021). Human Mortality Database. University of California, Berkeley (USA), and Max Planck Institute for Demographic Research (Germany). [Google Scholar]
- HMDB-STMF. (2021a). Original input data in standardized format. 2021-7-26 data.
- HMDB-STMF. (2021b). Pooled mortality rates.https://www.mortality.org
- Ho, J.Y. (2013). Mortality under age 50 accounts for much of the fact that U.S. life expectancy lags that of other high-income countries. Health Affairs, 32(3):459–467. doi: 10.1377/hlthaff.2012.0574 [DOI] [PubMed] [Google Scholar]
- Ho, J. Y., & Hendi, A. S. (2018). Recent trends in life expectancy across high income countries: Retrospective observational study. BMJ (Clinical Research ed.), 362, k2562. doi: 10.1136/bmj.k2562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho, J. Y., & Preston, S. H. (2010). US mortality in an international context: Age variations. Population and Development Review, 36(4), 749–773. doi: 10.1111/j.1728-4457.2010.00356.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hotez, P. J. (2021). Anti-science kills: From Soviet embrace of pseudoscience to accelerated attacks on U.S. biomedicine. PLoS Biology, 19(1), e3001068. doi: 10.1371/journal.pbio.3001068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link, B. G., & Phelan, J. (1995). Social conditions as fundamental causes of disease. Journal of Health and Social Behavior, Spec No, 80–94. doi: 10.2307/2626958 [DOI] [PubMed] [Google Scholar]
- Mendenhall, E. (2020). The COVID-19 syndemic is not global: Context matters. Lancet (London, England), 396(10264), 1731. doi: 10.1016/S0140-6736(20)32218-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy, S. L., Kochanek, K. D., Xu, J. Q., & Arias, E. (2021). Mortality in the United States, 2020. NCHS Data Brief, no 427. National Center for Health Statistics. doi: 10.15620/cdc:112079 [DOI] [PubMed] [Google Scholar]
- NASEM (National Academies of Sciences, Engineering, and Medicine). (2021). High and rising mortality rates among working-age adults. The National Academies Press. doi: 10.17226/25976 [DOI] [PubMed] [Google Scholar]
- NCHS (National Center for Health Statistics) . (1984). Vital statistics of the United States, 1980. Life tables. II, Section 6. DHHS Publication No. (PHS) 84-1104. National Center for Health Statistics. [Google Scholar]
- NCHS (National Center for Health Statistics) . (1998). Vital statistics of the United States, 1995. II, Mortality, Part A, Section 6 Life Tables. National Center for Health Statistics. [Google Scholar]
- NCHS . (2021). AH excess deaths by sex, age, and race. National Center for Health Statistics. HealthData.gov. [Google Scholar]
- NRC (National Research Council). (2011). Explaining divergent levels of longevity in high-income countries. In Crimmins E. M., Preston S. H., & Cohen B. (Eds.), Panel on Understanding Divergent Trends in Longevity in High-Income Countries. Committee on Population, Division of Behavioral and Social Sciences and Education. The National Academies Press. [PubMed] [Google Scholar]
- NRC and IOM (National Research Council and Institute of Medicine) . (2013). U.S. health in international perspective: Shorter lives, poorer health. Panel on understanding cross-national health differences among high-income countries. In Woolf S.H. & Aron L. (Eds.), Committee on Population, Division of Behavioral and Social Sciences and Education, and Board of Population Health and Public Health Practice, Institute of Medicine. National Academies Press. [PubMed] [Google Scholar]
- OECD . (2020). Transparency, communication and trust: The role of public communication in responding to the wave of disinformation about the new coronavirus. https://www.oecd.org/coronavirus/policy-responses/transparency-communication-and-trust-the-role-of-public-communication-in-responding-to-the-wave-of-disinformation-about-the-new-coronavirus-bef7ad6e/
- Palloni, A., & Yonker, J. A. (2016). Is the US old-age mortality advantage vanishing? Population and Development Review, 42(3), 465–489. doi: 10.1111/j.1728-4457.2016.00157.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker, R. W. (2021). Why America’s response to the COVID-19 pandemic failed: Lessons from New Zealand’s success. Administrative Law Review, 73, 77–103. https://heinonline.org/HOL/LandingPage?handle=hein.journals/admin73&div=8&id=&page= [Google Scholar]
- Phelan, J. C., Link, B. G., & Tehranifar, P. (2010). Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications. Journal of Health and Social Behavior, 51, S28–S40. doi: 10.1177/0022146510383498 [DOI] [PubMed] [Google Scholar]
- Pickett, K. E., & Wilkinson, R. G. (2015). Income inequality and health: A causal review. Social Science & Medicine, 128, 316–326. doi: 10.1016/j.socscimed.2014.12.031 [DOI] [PubMed] [Google Scholar]
- Reynolds, M. M., & Avendano, M. (2018). Social policy expenditures and life expectancy in high-income countries. American Journal of Preventive Medicine, 54(1), 72–79. doi: 10.1016/j.amepre.2017.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossen, L. M., Branum, A. M., Ahmad, F. B., Sutton, P., & Anderson, R. N. (2020). Excess deaths associated with COVID-19, by age and race and ethnicity—United States, January 26–October 3, 2020. Morbidity and Mortality Weekly Report, 69(42), 1522. doi: 10.15585/mmwr.mm6942e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samet, J. M., Burke, T. A., & Goldstein, B. D. (2017). The Trump administration and the environment—Heed the science. The New England Journal of Medicine, 376(12), 1182–1188. doi: 10.1056/NEJMms1615242 [DOI] [PubMed] [Google Scholar]
- Schoeni, R.F., House, J.S., Kaplan, G.A., & Pollack, H. (Eds.). (2008). Making Americans healthier: Social and economic policy as health policy. Russell Sage Foundation. [Google Scholar]
- Shah, M. (2020, September 3). The failure of public health messaging about COVID-19. Scientific American. [Google Scholar]
- Shokoohi, M., Osooli, M., & Stranges, S. (2020). COVID-19 pandemic: What can the west learn from the east? International Journal of Health Policy and Management, 9(10), 436–438. doi: 10.34172/ijhpm.2020.85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stats, N. Z. (2021). National and subnational period life tables: 2017–2019. Stats NZ and licensed by Stats NZ for reuse under the Creative Commons Attribution 4.0 International licence. https://www.stats.govt.nz/information-releases/national-and- subnational-period-life-tables-2017–2019 [Google Scholar]
- USCB (United States Census Bureau). (2019). Population estimates by age, sex, race, and Hispanic origin. Table SC-EST2019-ALLDATA5. https://www.census.gov/newsroom/press-kits/2020/ population-estimates-detailed.html
- Weiss, B. D., & Paasche-Orlow, M. K. (2020). Disparities in adherence to COVID-19 public health recommendations. Health Literacy Research and Practice, 4(3), e171–e173. doi: 10.3928/24748307-20200723-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (World Health Organization) . (2021). Healthy life expectancy (HALE) data by country. Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- Williams, D. R., Lawrence, J. A., & Davis, B. A. (2019). Racism and health: Evidence and needed research. Annual Review of Public Health, 40, 105–125. doi: 10.1146/annurev-publhealth-040218-043750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf, S.H., Chapman, D.A., Buchanich, J.M., Bobby, K.J., and Zimmerman, E.B. (2018). Changes in midlife death rates across racial and ethnic groups in the United States: A systematic analysis of vital statistics. British Medical Journal, 362, 3096. doi: 10.1136/bmj.k3096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf, S. H., Chapman, D. A., & Lee, J. H. (2021). COVID-19 as the leading cause of death in the United States. Journal of the American Medical Association, 325(2), 123–124. doi: 10.1001/jama.2020.24865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf, S. H., Chapman, D. A., Sabo, R. T., Weinberger, D. M., Hill, L., & Taylor, D. D. H. (2020). Excess deaths from COVID-19 and other causes, March–July 2020. Journal of the American Medical Association, 324(15), 1562–1564. doi: 10.1001/jama.2020.19545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf, S. H., Masters, R. K., & Aron, L. Y. (2021). Effect of the COVID-19 pandemic in 2020 on life expectancy across populations in the USA and other high income countries: Simulations of provisional mortality data. BMJ (Clinical Research ed.), 373, n1343. doi: 10.1136/bmj.n1343 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.