Abstract
Several large-scale clinical trials have conclusively demonstrated that voluntary medical male circumcision (VMMC) could provide a 50%–70% reduction in HIV acquisition, but willingness to undergo VMMC has been lowest in Zambia compared to other countries in eastern and southern Africa. This manuscript describes training for “task-shifting” among local healthcare workers at Community Health Centers (CHCs) applying state of the art strategies (e.g., Training of Trainers, i.e., ToT, and Training of Facilitators, ToF) to provide novel clinical services. Staff at 96 CHCs from four Provinces in Zambia were sequentially trained to provide the Spear & Shield intervention. A total of 45,630 men (n = 23,236) and women (n = 22,394) volunteered to participate in the S&S intervention service program when offered in the CHCs. Group session (total = 5313 sessions; 2,736 men’s and 2,582 women’s sessions) were conducted over 4.5 years. Remarkably, both men and women’s groups achieved 97% retention. Of these, 256 sessions recorded from 128 group leaders were assessed and scored for intervention fidelity; fidelity was 80%–90% among the majority of clinics. S&S program sustainment exceeded expectations among 85% of clinics (82/96) in all provinces across the duration of the study. Of note, attendance in the S&S program was encouraged by CHC staff, but no financial incentives were provided to those attending S&S. This study examined the effectiveness of the ToT/ToF model in dissemination of the S&S program, which proved to be feasible even in resource-limited settings. Benefits and challenges are discussed.
Keywords: Spear & Shield, Voluntary medical male circumcision, Zambia, HIV prevention, Implementation science
We describe training models used with health care workers Community Health Centers in delivering an intervention to increase the uptake of male circumcision in Zambia.
Implications.
Practice: In this study, remarkably, both men and women’s groups achieved 97% retention, and fidelity was 80%–90%. Sustainment of the S&S program exceeded expectations; the program was sustained in all four provinces across the entire duration of the study by 85% of the participating clinics (82/96). The Training of Trainers may enhance implementation and dissemination of evidence-based interventions.
Policy: Using a Training of Trainers may be a cost-effective strategy for implementing and disseminating evidence-based interventions such as Spear & Shield and facilitate scale-up of voluntary medical male circumcision (VMMC).
Research: VMMC scale-up is a proven effective strategy part of regional and global efforts to increase awareness and prevent HIV infection. Notwithstanding these advances, significant challenges remain, especially at the subnational level.
INTRODUCTION
Increasing the acceptance of voluntary medical male circumcision (VMMC) within the Zambian population has the potential to reduce the transmission of sexually transmitted infections (STIs) and HIV by 50%–70% [1–3] and could avert over 300,000 HIV/AIDs-associated deaths over a 10-year time span [4]. VMMC also reduces the risk of acquiring syphilis [5], human papilloma virus (HPV) [6] cervical cancer, and urinary tract infections [7]. In sub-Saharan Africa, rates of HIV infection are disproportionately high, with upwards of 1.2 million Zambians with HIV, translating to an HIV infection prevalence of 11.3% among adults [8]. Despite the benefits of male circumcision, only 13% of Zambian men had been circumcised by 2013 [8]. As of this date, it is estimated that 87.2% of Zambian adult males remain uncircumcised [9].
The Spear & Shield 1 (S&S 1) program is a randomized clinical trial with the primary purpose of increasing the acceptance and availability of VMMC in Zambia [1, 10, 11]. The program includes two components: (1) training of qualified health professionals to perform VMMC and (2) training CHC HIV counseling staff to conduct the Spear and Shield (S&S) intervention. The S&S 1 program drew eligible participants, i.e., men who expressed no interest in undergoing VMMC, from 15 community healthcare centers (CHCs) in Zambia. All CHCs received training in performing VMMCs to control for the availability of MC services across all sites. CHCs were randomized to experimental (six CHCs), control (six CHCs), or observation-only (three CHCs) conditions. The S&S intervention was offered at the experimental CHCs only. The intervention consisted of four group sessions, guided by an instruction manual, to address sexually transmitted infections, condom use, recognizing and controlling high-risk circumstances and intensive information about the “myths and truths” associated with male circumcision. Sessions applied a cognitive behavioral framework to reframe thoughts and feelings that prevented participants from considering MC as a viable strategy to prevent HIV infection. Female partners of male participants were also invited to participate in parallel women-only sessions, which contributed to a statistically significant 6% increase in the likelihood of undergoing VMMC in the experimental condition [12]. The control arm included only VMMC training and assessment, and the observation condition included only VMMC training. The S&S program found that participants in the experimental group were significantly more likely to undergo VMMC (2.45 times more likely than the control group, eight times more likely than the observation-only group). Longitudinally, condom use in the experimental group also increased pre to post, compared with no change in the control group. Results demonstrated the efficacy and acceptability of the S&S program [1].
Service providers have struggled to identify interventions which would effectively address the conceptions and misconceptions concerning VMMC. Sexual performance, sexual pleasure, cultural and religious taboos, partner response to their circumcision are a few of the determining issues raised by men (and women) in the group sessions related to VMMC. Given the positive impact of the S&S program on VMMC uptake, an extensive implementation and dissemination program (S&S 2) was proposed to the US National Institutes of Health (NIH) to be conducted in 96 CHCs in four Zambian provinces with high HIV rates and low VMMC uptake. In addition, in Zambia, there are only approximately nine physicians for every 100,000 patients, suggesting the need for task shifting of certain responsibilities [13]. Previous case studies found that the demand for VMMC providers greatly exceeded the available resources, especially when considering the national shortages of physicians, surgical specialists, and nurses/midwives [14].
The program used a staged roll out for the Training of Trainers (ToT) and of Facilitators (ToF) model to train trainers and group facilitators to lead the manualized S&S intervention. Two or three clinical staff (e.g., Clinical Officers, physicians, nurses) from each CHC were provided the World Health Organization (WHO) VMMC training program to ensure sufficient numbers of skilled healthcare workers were available to meet the anticipated increase in VMMC demand from the S&S participants [1]. This is no simple effort, but is achievable as illustrated by Ford et al. (2012). This meta-analysis revealed that MC programs in Kenya, South Africa, Swaziland, and Zimbabwe have taken up task-shifting efforts such as shifting roles to nonphysician clinicians with success; other high-risk HIV prevalent areas can do the same, safely, with adequate training [15]. While more research is needed when specifically evaluating the use of task shifting in VMMC and S&S programs across Zambia, task shifting can be a dynamic approach to combating health care provider scarcities and employing an innovative training model, i.e., ToT/ToF. The ToT/ToF model has been widely used in various disciplines to disseminate interventions and information in community contexts, including HIV prevention programs [16]. The aim of the ToT model in the current context was to train local CHC staff to not only conduct the manualized S&S program at their sites, but also to train staff from neighboring sites based on quality control assessments and productivity, thereby reducing the need for outside consultants to provide training for the intervention. In turn, consultants can train additional healthcare workers to further expand the provision of the S&S intervention within and between clinic sites [1].
This manuscript describes training for “task shifting” among local healthcare workers to provide novel clinical services applying state of the art strategies, e.g., ToT/ToF, with the goal of both facilitating the implementation and provision of evidence-based interventions (such as S&S), and of using the training “process” to conduct an evaluation of the training programs, i.e., the methodology/technology of skill training, and to improve the design. Using ToT/ToF as an indigenous resource within clinical sites is particularly important if evidence-based programs such as S&S are to become sustainable within the realities of high levels of staff turnover, frequent task shifting, and limited resources.
The staged rollout of the ToT/ToF model in the process of dissemination of the S&S program was designed to (1) maximize the number of CHCs providing S&S and VMMC and (2) ensure implementation, dissemination, and sustainment of the S&S program by using intensive experiential training techniques, fidelity monitoring, and implementation science strategies to identify and resolve challenges (e.g., planning, organization, scheduling, local climate, cultural characteristics, and logistics). This descriptive manuscript was created to provide guidance on the provision of a staged roll out of the ToT/ToF strategy at the community clinic level in Zambia.
METHODS
Ethical approvals
Prior to study onset, ethical board approval was obtained in both the United States and Zambia by the associated XXXX, XXXX, and XXXX.
Study design and procedures
Design
The S&S 2 project spanned four of Zambian provinces, Lusaka, Central, Southern, and Copperbelt Provinces. The four provinces were selected based upon high HIV prevalence and low rates of MC. The provinces were activated sequentially over a four-year period enabling the implementation of each province to be informed by each of the earlier province(s). As each province was activated, provincial and district health leaders received a full day briefing on the study and participated in study planning and review of the local climate for implementation. Following the provincial briefing, 24 CHCs in each province were selected to participate with District and Provincial guidance. The 24 CHCs were randomized into two groups for roll out of “immediate” (12) or “delayed “(12) S&S activation, due to the intensive S&S training requirements and limited research staff resources. All 24 CHCs in each province received VMMC training prior to study initiation. In the “immediate” CHCs, VMMC plus S&S intervention training was provided simultaneously. After a period of 6 months, intensive S&S training for the “delayed” CHCs was initiated over a 6-month period.
Procedures
Community health centre criteria
CHCs were identified and selected based on clinic size and catchment area, VCT, VMMC and HIV rates, available staff and space to provide intervention and VMMC procedures. District health leaders suggested appropriate clinics based on study criteria. Clinic leaders were visited by the S&S II program team, briefed on the study aims and invited to participate.
Randomization
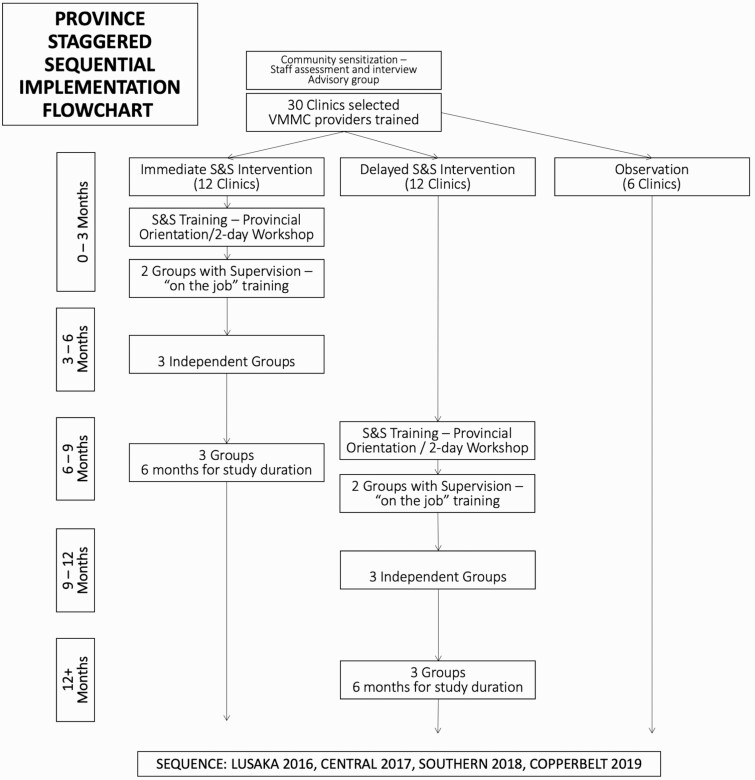
A three-stage clinic randomization process was conducted by Zambian investigators with a random allocation computer-generated sequence; trial statisticians did not participate in randomization. Before randomization, CHCs were stratified by catchment population, availability of space for VMMC and monthly VCT rates, and distance of the rural facility to the District Health Office; to ensure comparable sized comparisons, CHCs were randomized by large, medium, and small catchment population; a staged randomization procedure was performed in each province based on the 16 largest, 6 smallest, and 16 middle-size CHCs. In stage 1, the 16 largest CHCs and the 16 middle-size CHCs were randomized by computer, with random ordering of assignment (i.e., random ordering of the immediate, delayed and observation-only groups). In stage 2, the smallest 16 community health centers were allocated to a group in a similar manner. Last, in stage 3, all community health centers were randomized in two substages A and B (see Fig. 1). Substage A randomly assigned 24 selected community health centers to either delayed or immediate facilities conditions. The remaining clinics were only included as observation clinics. In this way, all CHCs had an equal chance of being chosen for any of the three groups until their quota was filled.
Fig. 1.
The timeline of the implementation and dissemination of Spear & Shield.
VMMC training
Clinical staff from all 24 CHCs in each province received a 10-day surgical training to provide VMMC following study activation, three months before implementation of the S&S intervention training began. Facilities that had one or no current VMMC provider identified at least two new health workers (nurse or clinical officer) to be trained in accordance with the VMMC guidelines from the Zambian Ministry of Health. Training followed the WHO VMMC training manual and focused on the dorsal slit method as recommended by the Surgical Society of Zambia and Ministry of Health. At all participating CHC sites, monthly clinic-level data (numbers of persons receiving voluntary HIV counseling and testing, monthly VMMCs conducted) were collected to assess rates of VCT and VMMC.
S&S trainee selection criteria
S&S training workshops targeted both VCT volunteers/lay counselors and those employed by the Government of Republic of Zambia (GRZ), all of whom were over 18 years and trained in approaches to mitigate and prevent HIV infection using HIV counseling and testing protocols in accordance with GRZ and WHO guidelines.
S&S training
Following the provincial briefing, leadership at each facility identified at least two lead voluntary counseling and testing counselors, one male and one female, and at least two assistant group leaders, one male and one female, to be trained to administer the S&S intervention and to participate in site On-the-Job Training (OJT) using “training of trainers” strategies. Assistant group leaders were not required to conduct S&S groups. Prior to study start, each facility was visited by the team for a study overview and planning session with site leadership and the trainees. Trainees (Group Leaders) from each of the facilities were scheduled by the district leaders to participate in a two-day intensive training workshop on the intervention and study protocol. The overall training objective was to equip group leaders with the necessary skills to conduct S&S sessions in their respective facilities. Trainings were both didactic and interactive and included presentations on VMMC, sexual risk (e.g., HIV, HPV and other STI exposure), and the extensive use of role plays depicting real life situations that addressed myths, misconceptions and knowledge gaps on VMMC for HIV prevention that impact both men and their female partners (see Jones et al., 2018; Rodriguez et al., 2019 for details of intervention content).
After the two-day training, trainees who felt they were ready were invited to volunteer to begin OJT, during which each trainee (Group Leader) co-led three groups of four sessions each at their clinic, supervised by a S&S program study trainer to provide rigorous, practical OJT. Emphasis was also placed on development of training of trainer strategies and understanding of intervention content to establish skills to train the subsequent CHC staff trainees to conduct and facilitate the S&S intervention.
During the intervention training, group leaders were also trained to recruit clinic patients to attend the S&S interventions; clinic patients attending VCT were targeted as they were, by definition, men and women who perceived themselves to be at risk of HIV infection. Depending on the clinic, men and women could also be referred to the intervention from Out-Patient Departments, youth friendly corners, and Maternal and Child Health clinics. Sessions were held at clinics at a day and time designated by the group leaders due to competing work requirements; conducting sessions at the clinics was preferred as it enabled access to medical personnel in case of emergency and maintained linkages with clinic staff.
Following S&S session training, group leaders immediately commenced recruitment of clinic clients (i.e., at least three groups of 8–10 men and women) to enable OJT with the S&S trainers. The OJT included a sequence of three groups: Group 1, the S&S trainer conducted the sessions while the group leader trainee observed; Group 2, topics within sessions were divided between the S&S trainer and trainee group leader, with the former using a checklist to ensure fidelity by the latter; Group 3, the trainee group leader conducted sessions while the S&S trainer observed using the checklist. When both trainer and trainee were comfortable, the trainee group leader conducted subsequent sessions independently while ensuring that each session was audio recorded. Group leaders had oversight for both recruitment and attendance and ensured that participants attended all four sessions. An attendance summary was provided to their respective trainers on a bi-monthly basis, who then compiled a summarized report on each site for the Project Manager, who then compiled a final report for each province that was submitted to the investigators in the United States and Zambia.
During training and following the completion of training, sessions were recorded and randomly selected to be reviewed by coordinators in Zambia and U.S. investigators to develop a feedback loop for guiding group leaders. Process evaluation following the training included the review of a random sampling of 10% of the intervention audiotapes and facilitator checklists (collected from sessions for Groups 3 and 4 which were led by the newly trained CHC staff) and evaluated by the Project Manager to assess fidelity to the S&S sessions. Recordings (256 sessions) from 128 group leaders were assessed and a percentage of achieved fidelity score ranging from 85%–100% = A, 70%–84% = B, 60%–69% = C and below 60% = D was awarded to each group leader, including OJT trainers. Feedback to the trainee was provided by the Project Manager in the same week regarding the gaps identified or the needed areas for improvement.
RESULTS
Enrollment and retention
A total of 45,630 men (n = 23,236) and women (n = 22,394) were enrolled in the S&S intervention. Participants who completed all four sessions received a Certificate of Attendance; no other incentives were provided. The S&S intervention was provided as a service program by the CHCs and the evaluation of S&S efficacy was measured at the community level, i.e. only group attendance and overall historic and current clinic VMMC data were collected from the S&S clinics and compared to “observation only” clinics offering VMMC only.
Training of spear & shield group leaders
Eight training workshops were conducted, of which four trainings were conducted immediately upon activation of the province, and four conducted after a delay of six months; each province received two trainings. A total of 192 counselors were trained as group leaders; of these, 62 were government counselors and 130 were lay counselors. All were trained to lead the group for the S&S interventions at their respective facilities.
Logistics
All community health facilities received a 10-day surgical training to provide VMMC following guidelines from Zambia’s Ministry of Health as well as the WHO VMMC training manual. S&S VMMC trainings were conducted by study investigators and consultants. After the VMMC training, each facility was provided with four or more MC kits based on the needs assessment conducted during facility selection. VMMC trainees were also provided with VMMC Certificates of Training.
After the training, the trainees were given materials for their facilities to use during group sessions: female reproductive charts, penile models, male and female condoms, voice recorders, and Attendance Certificates. Group leaders, clinic in-charge, and the clinic facility were compensated by S&S as an addition to typical clinic obligations. Compensation included the following: Group Leader $8 per session × 4 sessions = $32 per group, VMMC room/providers = $40 per month, and Clinic In-Charge = $30 per month. The health facility In-Charge ensured that Group Leaders had space to conduct sessions and that VMMC was available as a clinical service to the general public as well as group attendees. VMMC aggregate data were provided to the S&S Data Manager on a monthly basis for the duration of the study.
Clients attending
The four group sessions were structured such that female and male attendees met separately to encourage group members to express themselves freely during the sessions. Both men and women were expected to attend all four S&S sessions. Upon completion of the four sessions, participants were awarded attendance certificates. Refreshments, e.g., biscuits and drinks, and the awarding of attendance certificates were pivotal to retention. In rural areas, for example, refreshments made a substantial impact on attendance due to the need to walk long distances to health facilities. At the completion of the study, both refreshments and certificates of attendance were discontinued due to budgetary restrictions. Feedback regarding attendance suggested that refreshments were thought to have a substantial impact. During the study, however, no monetary incentives were provided to S&S attendees.
Successes
Overall, the S&S program activated 96 health facilities in the four provinces from 2016 to 2019 in accordance with the project’s timeline. During the period under review, N = 124 VMMC providers were trained in all four provinces. A total of 192 GRZ and Lay Counselors were trained on how to conduct S&S sessions. A total of 5,313 group sessions (2,736 men and 2,582 female partners) were conducted over the 4.5 years of study activities. Remarkably, both men and women’s groups achieved 97% retention, indicating that the majority of men and women returned to subsequent sessions following the first S&S group. Of these, 256 recordings from 128 group leaders were assessed and scored for intervention fidelity; fidelity was 80%–90% at the majority of clinics. At clinics in which trainers were transferred or dropped out, replacement trainers were successfully trained using ToT/ToF strategies. Sustainment of the program exceeded expectations; the program was sustained across the duration the study by 85% of clinics in all four provinces (82/96).
Challenges
Space
Structural issues were a concern in most facilities, particularly in rural areas. The S&S project was widely accepted and as the project was implemented, the popularity of the program resulted in space scheduling for multiple groups competing for scarce meeting space during regular clinic hours. Group leaders and the In-Charge typically resolved the space issues by scheduling sessions on weekends or late afternoon when the facilities were typically less busy.
Health centre facility deactivation
A protocol for deactivation of sites was developed to respond to the failure of some sites to recruit any men over a period of two months. Numerous attempts were made to engage both the group leaders and facility before a warning regarding nonrecruitment and potential deactivation was given to the group leader, and the clinic In-Charge was asked to consider replacing the group leader. If no improvement in recruitment was observed over an additional four months, sites were deactivated. During this period, problem solving sessions by the S&S Program Coordinator with the Group Leader and site leadership were proffered prior to formal deactivation. Only 14 of 96 sites were deactivated in the provinces for the following reasons: five sites in Lusaka (e.g., inability to recruit male participants and conduct sessions), six in Central (e.g., no MC provider, inability to recruit male participants), and three in the Copperbelt (e.g., inability to recruit male participants or OJT trainers). Some facilities were unable to kick start the OJT sessions due to the transfer of trained VMMC providers that were never replaced by the Ministry of Health, at some, staff were overwhelmed with other duties causing them to fail to conduct sessions or perform VMMCs, and some failed to recruit men despite replacement of male group leaders several times. Once deactivated, sites were replaced, and training was provided to the new group leader and other CHC staff.
Stipends
Following the completion of this service program in May of 2020, facility group leader stipends were discontinued. Facility In-Charges encouraged group leaders to continue to provide S&S sessions as part of their day-to-day services in their quest to increase demand for VMMC and reduce new cases of sexually transmitted infections (STIs).
Retention of group leaders
Of the 192 trained group leaders, 28 dropped out (14.5%), many of whom were GRZ counselors who described conflicts with other facility duties or transfers to other facilities. GRZ counselors also received guaranteed monthly payments from the government, potentially creating less incentive to provide sessions. In the case of dropout, an assistant group leader of the same sex was immediately asked to take over leading the sessions, and support was provided to ensure continuity.
DISCUSSION
This study presents the successful implementation and dissemination of the S&S program using a staged roll out of the ToT/ToF model with implementation science strategies to maximize the number of CHCs providing VMMC and the S&S intervention and to optimize sustainment of the program. The implementation program applied intensive training that emphasized fidelity monitoring in combination with strategies that included attention to planning, organization, scheduling, and logistics that were tailored to the local climate. Ongoing feedback loops were used to monitor, identify, and resolve challenges as they arose to ensure the sustainability of the program. The ToT model was used to train new leaders when group leaders dropped out of the program, and retention of both trainees and clients attending the program was high. Similarly, sustainment of the program at the sites was extremely high, and only a minority of sites were deactivated and replaced. Modest stipends and incentives in the forms of certificates were valuable in retaining healthcare workers, and as were modest incentives in the form of certificates of attendance and snacks to retain clients. Results from this study provide valuable guidance for future healthcare worker task shifting interventions in Zambia.
Over the past 20 years, the Zambia/US research team has focused its efforts on various findings supporting HIV prevention strategies and how to improve the acceptability of condoms, microbicides, maternal feeding practices, sexual partner reduction, high-risk sexual practices, among others. Within the past 15 years, a compelling body of evidence, including over 40 observational studies and at least six major clinical trials have consistently demonstrated the effectiveness of male circumcision in reducing HIV risk for men. For the purpose of this study, we accepted the extant data as an evidence-based finding and therefore accepted the body of evidence as conclusive. However, the question of VMMC acceptability at the population level was obvious: to conduct a “dissemination and implementation” population study using the findings from our clinical trial [1] as the foundation for designing this implementation and dissemination study, an innovative, community-based, provider training approach to roll out a VMMC demand generation program to implement and disseminate S&S. Previous research has supported the efficacy of the ToT/ToF model in the establishment of cost-effective and sustainable HIV prevention programs [17]. The ToT/ToF model has been utilized in Voluntary Counseling and Testing (VCT) for HIV prevention in the Caribbean and have shown sustainment in the post-implementation period [16]. The S&S Program had several unique characteristics; implementation was activated in provinces sequentially, providing valuable lessons to inform the implementation of subsequent provinces; VCT counselors were trained following a protocol checklist to ensure fidelity to the intervention; facilities were encouraged to integrate S&S sessions as a service program and part of their clinical enterprise to increase sustainability beyond duration of the study. Finally, monitoring protocols established criteria to deactivate facilities that were facing challenges to maximize use of funding at clinics with strong potential for recruitment and retention of clinic attendees.
Notwithstanding this success, there were some challenges to implementation. Although overall retention was 97%, 28 trained group leaders discontinued their participation due to competing work responsibilities, transfers, or competitive salaries received from the government for their clinical duties. Additionally, 14 sites were deactivated due to unsuccessful recruitment of participants. These are consistent with similar program implementation challenges in resource-limited settings [18]. Jones et al. reported that increasing workload associated with new programs often fell to lower-level staff members because higher level staff were not readily available to provide services [10], posing barriers to sustainable implementation and the potential for burnout. Also, some staff believed that their monetary compensation did not reflect the effort and workload associated with working on weekends to train and recruit men for the S&S program, given that work schedules could not accommodate weekdays-only operating hours [10].
Increasing acceptability of VMMC through programs like S&S has significant implications for HIV prevention efforts. The current study targeted high HIV prevalence provinces to maximize preventative benefits, focusing on Lusaka (capital of Zambia and where S&S is based) and the Copper Belt provinces with 15.4% and 15.1% HIV prevalence, respectively [19]. VMMC scale-up to reach 10,000 men and women in Lusaka alone through S&S has been estimated to avert 504 cases of HIV [12], and substantially reduce other STIs, including HPV, HSV-2, syphilis and related cervical cancers (Cook, 2016 [5, 20–25];. With an HIV prevalence of 11.3%, Zambia is one of the 14 priority countries identified by the WHO for VMMC scale-up [26], making interventions like S&S that improve uptake of VMMC crucial to reaching country and global targets. Current estimates in Zambia suggest that seven VMMCs could avert one case of HIV [27], with fewer VMMCs needed in high HIV prevalence provinces, where VMMC scale-up has played a significant role in HIV prevention. In Zambia, 80% scale-up was reached in 2018 with 1.9 million circumcisions completed [28]. Increased VMMC uptake is reflected in decreases in HIV infection across Zambia by 14% between 2010 and 2018 [16, 29]. Similar trends are noted at the sub-Saharan regional level with a 33% decrease in HIV infection between 2005 and 2013 [30].
VMMC scale-up is a proven effective strategy part of regional and global efforts to increase awareness and prevent HIV infection. Notwithstanding these advances, significant challenges remain, especially at the subnational level. Overall declines in HIV prevalence in Zambia at the national level mask wide variation and striking within-country differences [31, 32]. Moreover, many subregions have not met the 80% VMMC targets [31], which may be a contributory factor to continued high HIV prevalence in these regions. Efforts focused on closing these gaps through programs like S&S are necessary to achieve true VMMC scale-up and reduce HIV infection at both provincial and national levels.
Our findings demonstrate that the S&S ToT/ToF model is acceptable and feasible even in severely resource-limited settings. Though important challenges to increasing governmental support, resources, and sustainability remain, S&S program retention was promising and demonstrates that this intensive ToT/ToF model is an approach that may be effective in scaling up VMMC in this region. Future efforts must focus on finding solutions to these challenges as well as targeting within-country disparities in both VMMC scale-up and HIV prevalence.
Acknowledgements
This study was funded by National Institutes of Health/National Institute of Mental Health (NIH/NIMH) (R01MH095539), with support from the University of Miami Miller School of Medicine Center for AIDS Research funded by NIH/National Institute of Allergy and Infectious Diseases (NIAID) (P30AI073961). VJR’s work on this study was supported by a Ford Foundation Fellowship, administered by the National Academies of Sciences, Engineering, and Medicine (NASEM), a PEO Scholar Award from the PEO Sisterhood, and NIMH R36MH127838.
Compliance with Ethical Standards
Conflict of Interest: None declared.
Primary Data: Findings reported have not been previously published and this manuscript is not being simultaneously submitted elsewhere. Data have not been previously reported elsewhere. The authors have full control of all primary data and agree to allow the Journal to review data if requested.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
Transparency StatementThis study was not preregistered. No analytic plan was needed in the development of this manuscript; thus, no code is available. Materials (e.g., attendance data) is available upon request from the authors.
References
- 1. Weiss SM, Zulu R, Jones DL, Redding CA, Cook R, Chitalu N. The Spear and Shield intervention to increase the availability and acceptability of voluntary medical male circumcision in Zambia: A cluster randomised controlled trial. Lancet HIV, 2015; 2(5): e181–e189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: The ANRS 1265 trial. PLoS Med. 2005; 2(11): e298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gray RH, Kigozi G, Serwadda D, Makumbi F, Watya S, Nalugoda F, Wawer MJ. Male circumcision for HIV prevention in men in Rakai, Uganda: A randomised trial. Lancet 2007; 369(9562): 657–666. [DOI] [PubMed] [Google Scholar]
- 4. Kripke K, Njeuhmeli E, Samuelson J, et al. Assessing progress, impact, and next steps in rolling out voluntary medical male circumcision for HIV prevention in 14 priority countries in eastern and southern Africa through 2014. PLoS One. 2016; 11(7): e0158767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Weiss HA, Thomas SL, Munabi SK, Hayes RJ. Male circumcision and risk of syphilis, chancroid, and genital herpes: A systematic review and meta-analysis. Sex Transm Infect. 2006; 82(2): 101–9; discussion 110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Castellsagué X, Bosch FX, Muñoz N, Meijer CJ, Shah KV, De Sanjosé S, Franceschi S. Male circumcision, penile human papillomavirus infection, and cervical cancer in female partners. N Engl J Med. 2002; 346(15): 1105–1112. [DOI] [PubMed] [Google Scholar]
- 7. Alanis MC, Lucidi RS. Neonatal circumcision: A review of the world’s oldest and most controversial operation. Obstetr Gynecol Survey 2004; 59(5): 379–395. [DOI] [PubMed] [Google Scholar]
- 8. Joint United Nations Program on HIV/AIDS. (2013). Zambia country report. Monitoring the declaration of commitment on HIV and AIDS and the universal access.2013. https://www.unaids.org/sites/default/files/country/documents/ZMB_narrative_report_2015.pdf
- 9. Morris BJ, Wamai RG, Henebeng EB, et al. Estimation of country-specific and global prevalence of male circumcision. Population Health Metrics 2016; 14(1): 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jones DL, Rodriguez VJ, Butts SA, et al. Increasing acceptability and uptake of voluntary male medical circumcision in Zambia: Implementing and disseminating an evidence-based intervention. Transl Behav Med. 2018; 8(6): 907–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rodriguez VJ, Chahine A, de la Rosa A, Lee TK, Cristofari NV, Jones DL, Weiss SM. Identifying factors associated with successful implementation and uptake of an evidence-based voluntary medical male circumcision program in Zambia: The Spear and Shield 2 Program. Transl Behav Med. 2020; 10(4): 970–977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cook R, Jones D, Redding CA, Zulu R, Chitalu N, Weiss SM. Female partner acceptance as a predictor of men’s readiness to undergo voluntary medical male circumcision in Zambia: The Spear and Shield Project. AIDS Behav. 2016; 20(11): 2503–2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mundeva H, Snyder J, Ngilangwa DP, Kaida A. Ethics of task shifting in the health workforce: Exploring the role of community health workers in HIV service delivery in low-and middle-income countries. BMC Med Ethics. 2018; 19(1): 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Curran K, Njeuhmeli E, Mirelman A, et al. Voluntary medical male circumcision: strategies for meeting the human resource needs of scale-up in southern and eastern Africa. PLOS Med. 2011; 8(11): e1001129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ford N, Chu K, Mills EJ. Safety of task-shifting for male medical circumcision: A systematic review and meta-analysis. AIDS. 2012; 26(5): 559–566. [DOI] [PubMed] [Google Scholar]
- 16. Hiner CA, Mandel BG, Weaver MR, Bruce D, McLaughlin R, Anderson J. Effectiveness of a training-of-trainers model in a HIV counseling and testing program in the Caribbean Region. Human Resources Health, 2009; 7(1): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. UNICEF, UNICEF: Evaluation of UNICEF learning strategy to strengthen staff competencies for humanitarian response, 2000–2004. 2005. [Google Scholar]
- 18. Breimaier HE, Heckemann B, Halfens RJ, Lohrmann C. The Consolidated Framework for Implementation Research (CFIR): A useful theoretical framework for guiding and evaluating a guideline implementation process in a hospital-based nursing practice. BMC Nurs. 2015; 14(1): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zambia Statistics Agency, Ministry of Health (MOH) Zambia, and ICF. 2019. Zambia Demographic and Health Survey 2018. Lusaka, Zambia, and Rockville, Maryland, USA: Zambia Statistics Agency, Ministry of Health, and ICF.https://dhsprogram.com/pubs/pdf/FR361/FR361.pdf [Google Scholar]
- 20. Auvert B, Sobngwi-Tambekou J, Cutler E, et al. Effect of male circumcision on the prevalence of high-risk human papillomavirus in young men: Results of a randomized controlled trial conducted in Orange Farm, South Africa. J Infect Dis. 2009; 199(1): 14–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Davis MA, Gray RH, Grabowski MK, et al. Male circumcision decreases high‐risk human papillomavirus viral load in female partners: A randomized trial in Rakai, Uganda. Int J Cancer. 2013; 133(5): 1247–1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gray RH, Serwadda D, Kong X, et al. Male circumcision decreases acquisition and increases clearance of high-risk human papillomavirus in HIV-negative men: A randomized trial in Rakai, Uganda. J Infect Dis. 2010; 201(10): 1455–1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hallett TB, Alsallaq RA, Baeten JM, et al. Will circumcision provide even more protection from HIV to women and men? New estimates of the population impact of circumcision interventions. Sex Transm Infect. 2011; 87(2): 88–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Larke N. Male circumcision, HIV and sexually transmitted infections: A review. Br J Nurs. 2010; 19(10): 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tobian AA, Serwadda D, Quinn TC, et al. Male circumcision for the prevention of HSV-2 and HPV infections and syphilis. N Engl J Med. 2009; 360(13): 1298–1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. UNAIDS, Country fact sheets 2019: Zambia.2019. https://www.unaids.org/sites/default/files/media_asset/2019-UNAIDS-data_en.pdf
- 27. Republic of Zambia Ministry of Health. Country Operational Plan for the Scale-up of Voluntary Medical Male Circumcision in Zambia, 2012-2015. 2012. https://www.malecircumcision.org/sites/default/files/document_library/Zambia_VMMC_operational_plan.pdf
- 28. World Health Organization, Regional Office for Africa. WHO Progress Brief: Voluntary Medical Male Circumcision for HIV Prevention. 2018. https://www.afro.who.int/sites/default/files/2018-10/29%20Oct_18145_Progress%20Brief_VMMC%202018.pdf?ua=1
- 29. UNAIDS, The Gap Report. 2014. https://www.unaids.org/sites/default/files/media_asset/UNAIDS_Gap_report_en.pdf
- 30. Kharsany AB, Karim QA. HIV infection and AIDS in sub-Saharan Africa: Current status, challenges and opportunities. Open AIDS J. 2016;10: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cork MA, Wilson KF, Perkins S, Collison ML, Deshpande A, Eaton JW, Dwyer-Lindgren L. Mapping male circumcision for HIV prevention efforts in sub-Saharan Africa. BMC Med. 2020; 18(1): 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nakazwe C, Michelo C, Sandøy IF, Fylkesnes K. Contrasting HIV prevalence trends among young women and men in Zambia in the past 12 years: Data from demographic and health surveys 2002–2014. BMC Infect Dis. 2019; 19(1): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]