Abstract
Objectives
This study assesses how American life expectancy compares to other high-income countries and identifies key age groups and causes of death responsible for the U.S. life expectancy shortfall.
Methods
Data from the Human Mortality Database, World Health Organization Mortality Database, and vital statistics agencies for 18 high-income countries are used to examine trends in U.S. life expectancy gaps and how American age-specific death rates compare to other countries. Decomposition is used to estimate the contribution of 19 age groups and 16 causes to the U.S. life expectancy shortfall.
Results
In 2018, life expectancy for American men and women was 5.18 and 5.82 years lower than the world leaders and 3.60 and 3.48 years lower than the average of the comparison countries. Americans aged 25–29 experience death rates nearly 3 times higher than their counterparts. Together, injuries (drug overdose, firearm-related deaths, motor vehicle accidents, homicide), circulatory diseases, and mental disorders/nervous system diseases (including Alzheimer’s disease) account for 86% and 67% of American men’s and women’s life expectancy shortfall, respectively.
Discussion
American life expectancy has fallen far behind its peer countries. The U.S.’s worsening mortality at the prime adult ages and eroding old-age mortality advantage drive its deteriorating performance in international comparisons.
Keywords: Age patterns, Causes of death, Demography, International comparisons, Mortality
Life expectancy in the United States lags well behind that of other high-income countries. In the quarter century between 1980 and the mid-2000s, U.S. life expectancy dropped from being ranked around the middle to near the bottom of a set of peer countries (Institute of Medicine & National Research Council, 2013). This poor performance is particularly surprising given the country’s robust economic growth, high levels of health care spending, and rapid adoption of medical innovations.
The U.S. health and life expectancy disadvantage has been the focus of two National Academy of Sciences panels convened roughly a decade ago that focused on older (ages 50+) and younger (ages below 50) ages, respectively (Institute of Medicine & National Research Council, 2013; National Research Council, 2011). These reports and a number of prior studies have documented various aspects of the U.S. mortality disadvantage, including its elevated infant mortality rates (even accounting for cross-national differences in the reporting of live births or infant deaths; MacDorman et al., 2014); very high burden of young-age and injury-related mortality (Fenelon et al., 2016; Ho, 2013, 2019; Preston & Vierboom, 2021); high levels of smoking-attributable mortality at ages 50 and older (Preston et al., 2010); and slower progress in reducing cardiovascular disease mortality (Mehta et al., 2020). Although the United States performs poorly on an overwhelming number of fronts, this does not mean there are no areas in which American mortality performs better than in other high-income countries. The United States has experienced faster reductions from screenable and treatable cancers like breast, colorectal, and prostate cancers (Garcia & Crimmins, 2013; Preston & Ho, 2011) and enjoys a mortality advantage at the oldest ages (Ho & Preston, 2010; Manton & Vaupel, 1995; Palloni & Yonker, 2016). The majority of these studies are restricted to specific age ranges (e.g., ages below 50 or ages 50+) or causes of death (e.g., cardiovascular disease, smoking-related deaths, drug overdose), and many do not use data covering trends since 2010.
Since 2010, life expectancy trends in the United States have been particularly adverse both in an absolute sense and compared to trends in other high-income countries (Ho & Hendi, 2018). U.S. life expectancy increased only minimally between 2010 and 2013, declined for three consecutive years between 2014 and 2017, and increased slightly between 2017 and 2018. The end result has been that life expectancy in the United States did not increase between 2010 and 2018—in both years, it was 78.7 years (Xu et al., 2020). In contrast, several other high-income countries—including countries like Japan and Switzerland, which have achieved among the highest observed levels of life expectancy—have continued to enjoy robust life expectancy gains since 2010 (Ho, 2020). Thus, it is likely that this unprecedented stagnation in U.S. life expectancy coupled with continued gains experienced in other countries will have resulted in a substantial widening of the U.S. life expectancy shortfall.
This study is the first to provide a comprehensive, recent assessment of the American mortality disadvantage relative to a large set of high-income comparison countries. It considers the entire age range and covers a period spanning the alarming post-2010 developments in U.S. life expectancy. This article evaluates how key dimensions of the U.S. life expectancy shortfall have changed between 1958 and 2018, examines how age variations in American mortality performance have changed between 2008 and 2018, and identifies the key age groups and causes of death responsible for why the United States has lower life expectancy than its peer countries in 2016.
Method
The analysis focuses on a set of 18 high-income countries consisting of the United States and 17 comparison countries: Australia, Austria, Belgium, Canada, Denmark, Finland, France, Germany, Italy, Japan, the Netherlands, Norway, Portugal, Spain, Sweden, Switzerland, and the United Kingdom. The comparison countries are all developed nations with fairly large population sizes (upwards of 5 million in 2018) that underwent their mortality transitions over roughly the same time period as the United States. The set of countries overlaps with those used in prior cross-national studies of the U.S. life expectancy disadvantage (Ho, 2013; Ho & Hendi, 2018; Institute of Medicine & National Research Council, 2013; National Research Council, 2011; Verguet & Jamison, 2013).
Data
This study uses data from the Human Mortality Database (HMD), the World Health Organization (WHO) Mortality Database, and the vital statistics agencies of Austria, Germany, and Italy (Federal Statistical Office of Germany, 2021; Italian National Institute of Statistics, 2021; Statistik Austria, 2021; University of California, Berkeley (USA) & Max Planck Institute for Demographic Research (Germany), 2021; World Health Organization, 2021). Life table death rates were extracted from the HMD for each of the 18 countries for each year between 1958 and 2018. (For 1958–1989, life tables for Germany were produced using the population-weighted life table death rates for East and West Germany.) For three countries whose 2018 data are not yet available through the HMD (Austria, Germany, and Italy), I obtained data from these countries’ vital statistics agencies and constructed life tables using graduation to obtain values (Preston et al., 2001). I also produced life tables for the average of the 17 comparison countries based on their population-weighted death rates.
Data on mortality by cause of death come from the WHO Mortality Database. The most recent year cause-specific data are available for all countries is 2016. Causes of death are coded into 16 mutually exclusive and exhaustive categories: alcohol-induced deaths, Alzheimer’s disease, circulatory diseases, diabetes, drug overdose, firearm-related deaths, homicide, infectious and parasitic diseases, lung cancer, mental/behavioral disorders and diseases of the nervous system (excluding Alzheimer’s disease), motor vehicle accidents, perinatal conditions and congenital anomalies, respiratory diseases, screenable/treatable cancers (breast, cervical, colorectal, and prostate cancers), suicide, and a residual category consisting of all remaining causes of death. Alcohol-induced deaths include deaths from mental/behavioral disorders and diseases of the nervous system, circulatory diseases, injuries, and the residual category, which are thus excluded from these overlapping categories. Drug overdose, alcohol-induced deaths, firearm-related deaths, and motor vehicle accidents are defined following the standard definitions used by the U.S. National Center for Health Statistics (Murphy et al., 2021). The International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) codes corresponding to these 16 cause of death categories are provided in Supplementary Table 1. Using broad cause of death categories helps to address issues of comparability of cause of death coding across countries.
Analysis
I assess trends in the gap in life expectancy at ages 0, 65, and 85 between the United States and the world leader, the average of the comparison countries, and the country with the lowest life expectancy value between 1958 and 2018. When the United States is either the world leader or the worst performer, the comparison is made between the United States and the second-ranked country (for the world leader comparison) or the 17th ranked country (for the worst performer comparison).
Next, I examine the age patterns of the American mortality disadvantage and how they have changed between 2008 and 2018. I compare the rankings of U.S. death rates at each age among the set of comparison countries (where the country with the lowest death rate is ranked first and the country with the highest death rate is ranked 18th) and the ratios of U.S. death rates to the population-weighted average of the comparison countries at each age.
Arriaga’s decomposition is used to apportion the difference in life expectancy at birth between the United States and each of the 17 comparison countries, as well as between the United States and the average of the comparison countries, into age and cause of death contributions (Arriaga, 1984). Within each age group, the cause of death contributions sum to the total contribution of that age group. The sum of the age group contributions across all ages equals the difference in life expectancy at birth between the United States and each country. All analyses are performed separately for men and women.
Results
Long-Run Trends in the U.S. Life Expectancy Shortfall
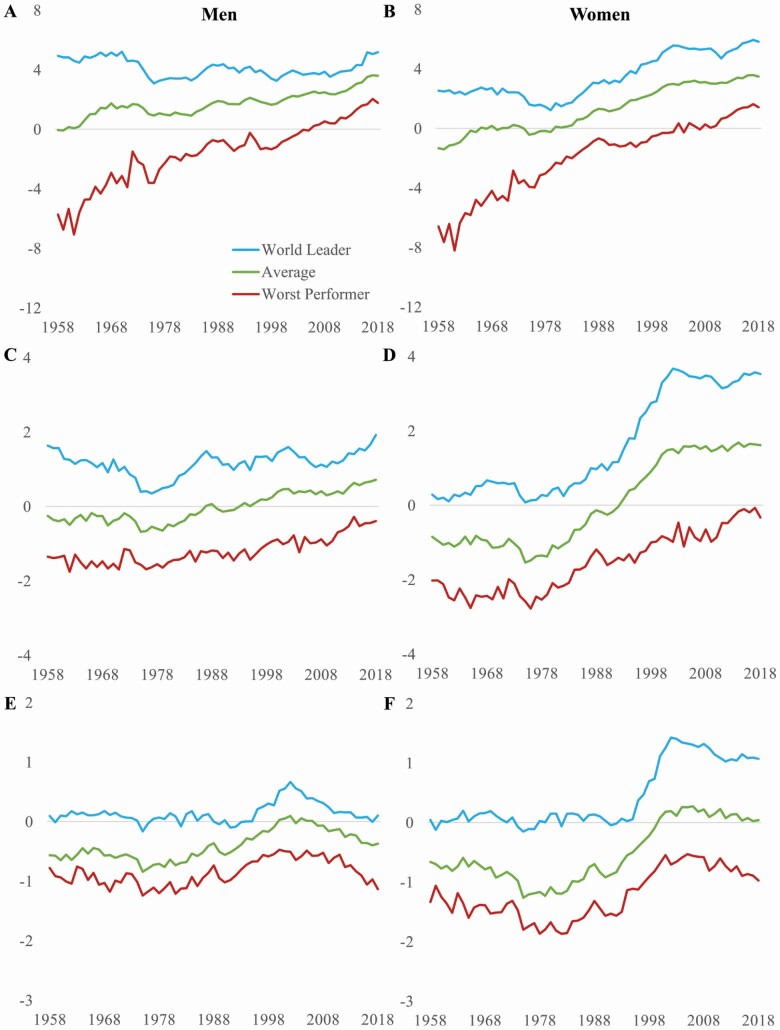
Figure 1 shows how the United States has performed relative to its peer countries in terms of life expectancy at birth, at age 65, and at age 85 between 1958 and 2018. Beginning with life expectancy at birth (Figure 1A and B), we can see that the United States performed very well in the early part of this period. Its life expectancy levels were close to (for men) or above (for women) the average, and they were well above the country with the lowest life expectancy. Starting in the late 1970s, however, the United States started to fall further and further behind its peer countries. Gaps between the United States and both the average and the world leaders have grown steadily. The United States fell into last place, becoming the country with the lowest life expectancy at birth, for the first time in 2003 for women and in 2006 for men. In every year of the past decade, U.S. life expectancy has remained in last place, falling well behind even the worst performer among the comparison countries.
Figure 1.
U.S. life expectancy shortfall (years) at birth (A and B), age 65 (C and D), and age 85 (E and F) compared to the world leader, average of the comparison countries, and worst performer, men and women, 1958–2018.
The U.S. life expectancy gaps are now the largest they have ever been. In 2018, American men and women could expect to live 5.18 and 5.82 fewer years than the world leaders, Swiss men and Japanese women. The gaps between the United States and the average of the other countries reached 3.60 and 3.48 fewer years for men and women, respectively. One of the most striking indicators of how far the United States now lags behind its peer countries is the comparison with the country with the lowest life expectancy level. In 1961, life expectancy at birth in the United States was 7.07 and 8.21 years higher than that of Portuguese men and women, respectively. Today, American men can expect to live 1.78 fewer years than Portuguese men, while American women can expect to live 1.42 years fewer years than British women.
The U.S. shortfalls in life expectancy at age 65 are smaller in magnitude but follow similar patterns to those observed for life expectancy at birth (Figure 1C and D). Since the late 1970s, these gaps have grown larger, and the increases have been particularly sharp for women. For example, the gap in life expectancy at age 65 between the United States and the world leader increased from 1.64 to 1.92 years between 1958 and 2016 among men, but from 0.28 to 3.53 years—a 12 and a half fold increase—among women. Initially, U.S. life expectancy at age 65 was higher than the average, but has fallen below the average since 1993 (women) and 1994 (men). The main difference from the patterns observed for life expectancy birth is that to date, the United States has never ranked in the last place for life expectancy at age 65, although American women have been in second to last place in every year since 2009. Life expectancy at age 65 for American men has ranked in 12th or 13th place in every year since 2014. The U.S. advantage relative to the lowest-performing country has shrunk dramatically over time.
The patterns for life expectancy at age 85 (Figure 1E and F) are quite different from those observed for ages 0 and 65. Until the mid-1990s, differences between the United States and the world leader were negligible. In fact, the United States ranked among the top five countries in life expectancy at age 85 in 55 years (90% of the period) and 50 years (82% of the period) for men and women, respectively, between 1958 and 2018. Aside from a brief deterioration in their relative performance around the 2000s, American men have generally maintained their advantage in life expectancy at age 85. Their levels stayed fairly close to that of the world leaders and were nearly always higher than the average and substantially higher than the worst performing country. In contrast, American women’s advantage has eroded over the past two decades. Between 1958 and the early 1990s, U.S. female life expectancy at age 85 was very similar to that of the world leaders and well above the average of the comparison countries. Subsequently, however, a large gap has opened between the world leaders and American women, and life expectancy at age 85 for American women has not exceeded the average since 2000. American men and women have continued to maintain an advantage in life expectancy at age 85 over the worst-performing country, which is not the case for either life expectancy at birth or age 65.
How American Mortality Performs by Age
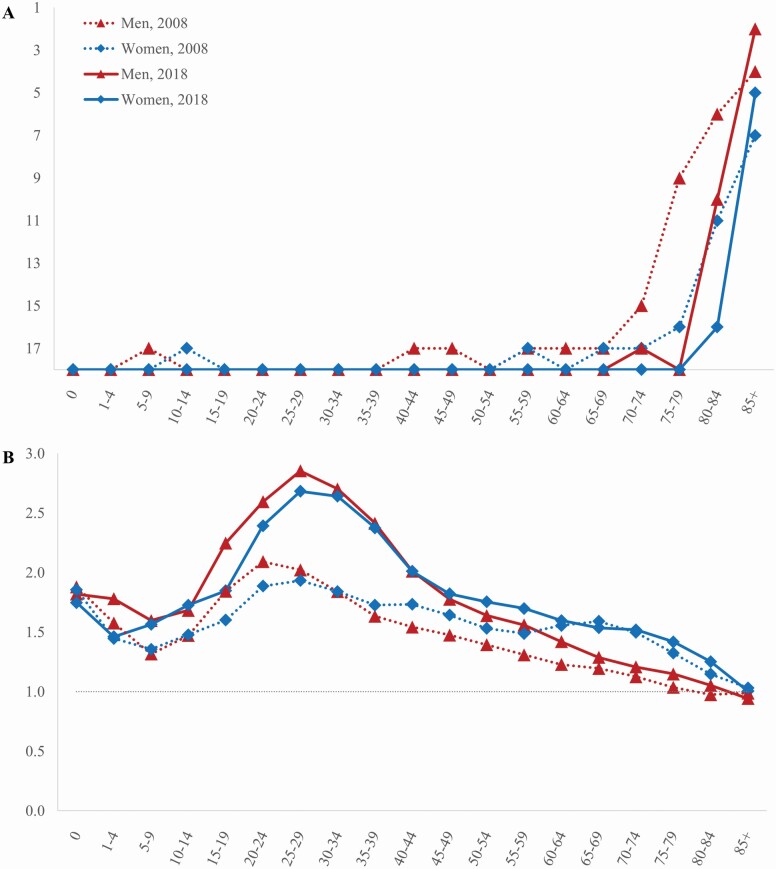
Mortality is strongly patterned by age, and we would like to know whether the U.S. mortality disadvantage is uniform across age and at which ages it has become more or less pronounced over time. Figure 2A shows the rankings of U.S. death rates by age in 2008 and 2018. Within each age group, the 18 countries are ranked from lowest to highest death rate, so that the country with the lowest (most favorable) death rate receives a rank of 1 and the country with the highest (least favorable) death rate receives a rank of 18. The age pattern of U.S. mortality rankings bears the characteristic J-shape documented by Ho and Preston (2010). For both men and women, U.S. death rates were the highest or second highest among the comparison countries in every age group until age 70–74 (in 2008) or age 80–84 (in 2018). At the older ages (70+), we observe a jump in the rankings, indicating that the United States performs very well at these ages compared to other countries. These low death rates at older ages are consistent with the U.S.’s generally favorable performance in life expectancy at age 85 seen in Figure 1. However, there has been a distinct deterioration in the rankings over the past decade. The age at which Americans begin experiencing a mortality advantage relative to other countries has been pushed back to progressively older ages. For example, in 2008, American men aged 75–79 had mortality rates near the median—they had a rank of 9. By 2018, the ranking for American men aged 75–79 dropped to 18. American women experienced a similar deterioration in their rankings over this decade. These findings demonstrate that the erosion of the U.S. old-age mortality advantage has continued in the post-2010 period.
Figure 2.
Ranking of U.S. death rates among 18 countries (A) and the ratio of U.S. death rates to the average of comparison countries (B), men and women, 2008 and 2018.
Next, we examine the ratio of U.S. death rates to the average of the comparison countries (Figure 2B). This is a complementary measure to rankings that allows us to examine the degree to which the American mortality disadvantage has worsened or improved over time. For nearly the entire age range, the ratios were above 1, indicating that the United States experienced higher mortality at each age compared to other countries. The ratios fell below 1 only at ages 80–84 for men in 2008 and at age 85 and older for men in 2018 and were close to but did not fall below 1 for women in either year. While Americans experienced elevated mortality rates for most of the age range, the largest differences were observed at the younger adult ages. The ratios peaked in the 20s for both men and women. Examining change between 2008 and 2018, we see that the ratios in 2018 were above those in 2008 for almost every age group. In other words, the United States is now worse off at just about every age compared to a decade earlier. The deepening of the U.S. mortality disadvantage at the young and prime adult ages over the past decade is striking. For both men and women, the ratios increased at every age group between 15 and 64 over the past decade. This increase was particularly dramatic for Americans aged 25–29. In 2008, Americans in this age group experienced death rates about twice as high as their counterparts in other countries. The ratios peaked at 2.02 for men and 1.93 for women. A decade later, these ratios had increased to 2.85 and 2.68 for men and women, respectively, indicating that Americans in their mid-20s now have death rates that are nearly three times higher on average than people in their mid-20s living in other high-income countries.
Age Groups Contributing to the U.S. Life Expectancy Shortfall
Next, we examine which age groups contribute most to the U.S. life expectancy shortfall and whether these contributions have changed over time. Table 1 presents the age decomposition results for the difference in life expectancy at birth between the United States and the average of the comparison countries and between the United States and the world leader. How much of the shortfall comes from ages below 50 is one metric that has been used in prior studies. Ages below 50 accounted for 56%–60% of the gap between the American men and the average and for 46%–47% of the gap between American men and the world leaders. The corresponding percentages for women relative to the average and world leaders were 31%–34% (average) and 21%–24% (world leaders), respectively.
Table 1.
Contribution of Specific Age Groups (%) to the U.S. Shortfall in Life Expectancy at Birth, Men and Women, 2008 and 2018
| Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|
| Average | World leader | Average | World leader | |||||
| Age group (years) | 2008 | 2018 | 2008 | 2018 | 2008 | 2018 | 2008 | 2018 |
| 0 | 11% | 6% | 6% | 4% | 8% | 5% | 6% | 5% |
| 1–4 | 1% | 1% | 1% | 1% | 1% | 1% | 0% | 0% |
| 5–9 | 0% | 0% | 0% | 0% | 0% | 0% | 0% | 0% |
| 10–14 | 1% | 1% | 1% | 1% | 0% | 1% | 0% | 0% |
| 15–19 | 4% | 3% | 3% | 2% | 1% | 1% | 1% | 1% |
| 20–24 | 8% | 6% | 6% | 5% | 2% | 3% | 1% | 2% |
| 25–29 | 7% | 8% | 5% | 6% | 2% | 4% | 1% | 2% |
| 30–34 | 6% | 8% | 5% | 7% | 3% | 4% | 1% | 3% |
| 35–39 | 6% | 8% | 5% | 7% | 3% | 5% | 2% | 3% |
| 40–44 | 7% | 7% | 7% | 6% | 5% | 5% | 3% | 3% |
| 45–49 | 8% | 8% | 8% | 7% | 6% | 6% | 5% | 4% |
| 50–54 | 9% | 9% | 10% | 9% | 7% | 7% | 6% | 6% |
| 55–59 | 9% | 10% | 10% | 11% | 7% | 9% | 6% | 8% |
| 60–64 | 8% | 10% | 9% | 11% | 10% | 9% | 9% | 9% |
| 65–69 | 8% | 8% | 8% | 9% | 13% | 10% | 12% | 10% |
| 70–74 | 6% | 6% | 8% | 7% | 13% | 12% | 12% | 12% |
| 75–79 | 2% | 5% | 6% | 7% | 11% | 11% | 12% | 12% |
| 80–84 | −1% | 1% | 2% | 3% | 5% | 7% | 10% | 10% |
| 85+ | −1% | −4% | −1% | −3% | 3% | 1% | 12% | 9% |
| U.S. shortfall (years) | 2.49 | 3.60 | 3.87 | 5.18 | 3.11 | 3.48 | 5.32 | 5.82 |
Notes: U.S. shortfall refers to the difference in life expectancy at birth between the United States and the average of the comparison countries or between the United States and the world leader in life expectancy. The world leader for men is Switzerland and the world leader for women is Japan. Positive (negative) percentages indicate that mortality differences between the United States and other countries in a specific age group widened (narrowed) the U.S. life expectancy shortfall.
In general, mortality differences at the younger ages contributed more to the U.S. life expectancy shortfall for men than for women and more in 2008 than in 2018. For example, the largest contributions were concentrated between ages 50 and 64 among men, with each 5-year age group in this range accounting for around 10% of the U.S. life expectancy shortfall. Among women, the largest contributions (ranging between 10% and 13%) were concentrated at ages 65–79. The oldest ages (80–84 and 85+) did not add to the life expectancy shortfall among American men because they had lower mortality at these ages than men in other countries; in fact, mortality differences at ages 85 and older mean the U.S. shortfall was smaller than it would be otherwise. Among women, these age groups only recently started contributing to the U.S. life expectancy shortfall and were more important for the shortfall relative to the world leaders than relative to the average.
Causes of Death Contributing to the U.S. Life Expectancy Shortfall
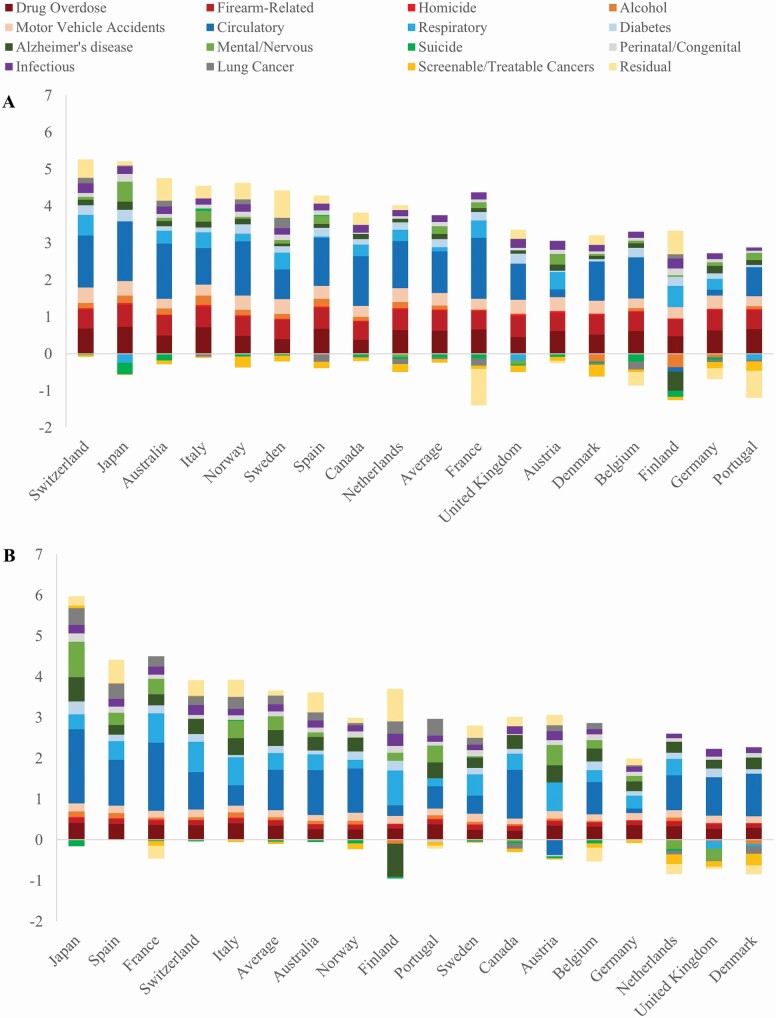
Figure 3 shows the contribution of 16 causes of death to the U.S. life expectancy shortfall in 2016, the latest year cause-specific mortality data are available for all of the countries. I decompose the difference in life expectancy at birth between the United States and each of the comparison countries and between the United States and the average of the comparison countries (numeric values are provided in Supplementary Table 2). Bars above the x-axis add to the U.S. life expectancy shortfall (i.e., the United States performs less favorably in terms of mortality from a specific cause of death than the comparison country), while bars below the x-axis reduce the U.S. life expectancy shortfall (i.e., the United States performs more favorably in terms of mortality from a specific cause of death than the comparison country). The contributions of the 16 causes of death sum to the total difference in life expectancy between the United States and each country, and the countries are ranked from largest to smallest difference with the United States. Thus, the world leaders—Swiss men and Japanese women—are the leftmost bars, while the countries with the lowest life expectancy levels—Portuguese men and Danish women—are the rightmost bars.
Figure 3.
Contribution of 16 causes of death (years) to the U.S. shortfall in life expectancy at birth, men (A) and women (B), 2016.
The U.S. mortality disadvantage is wide-ranging and not restricted to a single specific cause of death. Causes as diverse as drug overdose, perinatal conditions/congenital anomalies, circulatory disease, and Alzheimer’s disease all contribute to the U.S. life expectancy shortfall. While the United States experiences a mortality disadvantage for many different types of causes of death, some groups clearly contribute more than others. Injuries (in red) and diseases related to cardiovascular, respiratory, and metabolic diseases (in blue) account for the lion’s share of the U.S. life expectancy shortfall among men (Figure 3A). Among injuries, a fairly diverse set of causes—drug overdose, firearm-related deaths, and motor vehicle accidents—tend to make the largest contributions. On average, they account for 18%, 15%, and 10% of American men’s life expectancy shortfall, respectively. Circulatory diseases, diabetes, and respiratory diseases account for 32%, 6%, and 3%, respectively. Causes of death that reduce the male U.S. life expectancy shortfall include lung cancer, suicide, and screenable/treatable cancers.
For American women, circulatory disease and respiratory disease are the main contributors to the U.S. life expectancy shortfall, accounting for 28% and 12% on average. Injuries are also important, although they make relatively smaller contributions than for men, while mental/behavioral disorders and diseases of the nervous system (in green) are relatively more important for women than for men. Drug overdose accounts for 10% of the female U.S. life expectancy shortfall compared to the average, while Alzheimer’s disease and other mental/behavioral disorders and diseases of the nervous system account for 11% and 10%, respectively. Similar to the case for men, American women also perform more favorably in terms of mortality from screenable/treatable cancers and suicide—but not lung cancer—than the comparison countries.
While there is some variation across countries, the patterns observed for the breakdown of the life expectancy difference between the United States and the average of the comparison countries generally apply to the individual country comparisons as well. The main exceptions are that Alzheimer’s disease does not contribute to the gap in life expectancy between the United States and Finland, and that circulatory disease either does not contribute to or makes smaller contributions to the gap in life expectancy between the United States and Austria and Germany than it does to the gap between the United States and the other countries. In these cases, this results from Finland, Austria, and Germany having relatively high mortality rates from these two causes of death.
Discussion
U.S. life expectancy has fallen far behind its peer countries. The U.S. life expectancy shortfall is larger than it has ever been before, with Americans living over 5 and 3 fewer years compared to the world leaders and the average of the comparison countries, respectively, in 2018. These life expectancy differentials are substantial. The following thought experiment provides a sense of just how large these gaps are. Best-practice life expectancy—the highest life expectancy observed in a given year—has been found to increase by about 2.5 years per decade (Oeppen & Vaupel, 2002). If we froze all other countries at their current life expectancy levels and allowed the United States to increase its life expectancy at a rate of 2.5 years per decade, it would take over a decade—about 14 years—for Americans to catch up to the average of the other countries. To catch up to the world leaders would require over two decades (21 years for men and 23 years for women). Again, this is assuming other countries make no further life expectancy gains and that the United States could achieve a rate of increase of 2.5 years per decade. In fact, between 2008 and 2018, life expectancy increased by only 0.78 years for American men and 0.89 years for American women. If those rates were to continue, it would take around four decades for the United States to match the average life expectancy levels of the other countries. A particularly dismal indicator of the U.S.’s worsening performance is that where it once used to experience life expectancy levels far higher than the worst-performing country, U.S. life expectancy levels now fall well below even the worst performer among its peer countries. American men and women have had the lowest life expectancy at birth for over a decade and are perilously close to ranking in last place for life expectancy at age 65.
As life expectancy levels and survivorship increase, mortality at the oldest ages will become increasingly important determinants of cross-national life expectancy differences. Thus, it is instructive to consider patterns in life expectancy at age 85, an age to which 36% and 50% of American men and women could expect to survive, respectively, according to the 2018 U.S. life table. The comparable figures for men and women for the average of the other high-income countries were 44% and 62%, respectively, and a remarkable 70% for Japanese women. While the United States has managed to maintain a favorable performance in terms of life expectancy at age 85, it has lost ground over time, particularly for women. In 2018, mortality differences at the oldest ages no longer acted to reduce the U.S. life expectancy shortfall for women, although they continued to do so for men.
This study has demonstrated the continued importance of younger age (below 50) mortality for the U.S. life expectancy shortfall. Mortality below age 50 accounts for over half of American men’s life expectancy shortfall and about a third of American women’s life expectancy shortfall, on average. Over the past decade, the U.S.’s relative mortality disadvantage at the prime adult ages (25–64) has deepened. Trends have been particularly adverse between ages 25 and 44. At these ages, Americans experienced death rates two to three times higher than their counterparts living in other high-income countries in 2018.
These elevated death rates at the prime adult ages are related to a high burden of injury-related deaths in the United States. Deaths from drug overdose, firearms, and car accidents make large contributions to the U.S. life expectancy shortfall, particularly for men. Among women, we see a growing contribution of Alzheimer’s disease and other mental disorders and diseases of the nervous system. We also see lung cancer and respiratory diseases playing a greater role for women. This is related to cross-national and gender differences in smoking epidemics. The United States had an earlier and more severe smoking epidemic compared to other high-income countries, and men started (and eventually quit) smoking earlier than women (Ho & Fenelon, 2015; National Research Council, 2011; Preston et al., 2010). As a result, American men’s smoking-attributable mortality peaked in the 1990s and has been declining since then. Men in other countries, who began smoking slightly later, are now benefiting from reductions in smoking-attributable mortality. In contrast, American women’s smoking-attributable mortality peaked in the mid-2000s and remains higher than in many of the comparison countries. In other high-income countries, women generally began smoking later than American women, so smoking-attributable mortality currently remains at lower levels but is expected to continue to rise in the coming decades. Circulatory diseases are an important contributor to the U.S. life expectancy shortfall among both men and women. Mehta et al. (2020) found that stalled progress in reducing cardiovascular disease mortality has been an important contributor to the post-2010 U.S. life expectancy stagnation. Prior studies have found that several other high-income countries are also experiencing slowdowns in cardiovascular disease mortality declines, although to a lesser degree than the United States (Ho, 2020; Raleigh, 2019). The reasons for these slowdowns have yet to be fully identified, although potential explanations include smaller gains from reductions in smoking-attributable mortality, rising levels of obesity, and slowing expansions in the use of drugs and other treatments for cardiovascular disease in high-income countries.
This study provides a foundation for understanding the broader determinants of and policy targets for addressing the U.S. life expectancy shortfall. One perennial question asks whether behavioral or structural factors are predominantly responsible for Americans’ mortality disadvantage. The causes of death identified as key contributors to the U.S. life expectancy shortfall underscore that a combination of behavioral factors and structural and organizational factors (and interactions between the two groups of factors) are involved. Both types of factors matter, and they are not easily separable. For example, high rates of homicide are related to inequality and residential segregation, high rates of firearm-related deaths are influenced by both behavioral factors and the greater availability of guns in the United States, and motor vehicle fatalities are driven by risky behaviors like drunk driving as well as structural factors like long commutes and lower population density (Evans, 2014; Hemenway & Miller, 2000; Massey, 1995; Peterson & Krivo, 1993, 1999; Richardson & Hemenway, 2011; Siegel et al., 2013; Transportation Research Board, 2011). In other words, Americans are highly exposed to risky conditions and a high prevalence of negative behavioral factors, the consequences of which may be exacerbated by poor structural and organizational conditions including a lack of universal access to health care.
Another question relates to how inequality within the United States contributes to its low life expectancy ranking. Large life expectancy differentials along racial/ethnic, socioeconomic, and geographic dimensions exist within the United States (Dwyer-Lindgren et al., 2017; Elo et al., 2019; Harper et al., 2012; Hendi, 2015, 2017; Vierboom et al., 2019; Wang et al., 2013), and these differentials tend to be larger in the United States than in other high-income countries (Hendi et al., 2021; Mackenbach et al., 2008; Martikainen et al., 2013). Prior studies have found that while educational disparities account for part of the U.S. life expectancy shortfall (van Hedel et al., 2015), it is also the case that even the most advantaged groups in American society (e.g., the college-educated and those in the top wealth tertile) have worse health than their counterparts in other high-income countries (Avendano et al., 2009; Banks et al., 2006, 2010). Thus, it seems likely that reducing mortality inequalities within the United States would narrow but not eliminate the U.S. life expectancy shortfall.
Given the U.S.’s dismal performance in international rankings of life expectancy, it may come as a surprise that increasingly, researchers and policymakers are looking to American life expectancy trends for lessons that may translate to other countries. This interest is underpinned by the growth in global connectedness (Berry et al., 2014; Guillén, 2020)—increasingly, health insults faced by one nation are shared by others (Ho & Hendi, 2018), as the coronavirus disease 2019 pandemic demonstrated all too well. It is also the case that the United States often acts as a vanguard nation or cautionary tale. The country tends to be at the forefront of emerging health threats such as the opioid epidemic and a sudden slowing in improvements in cardiovascular disease mortality. While other countries may not experience the same degree of exposure or vulnerability to such threats, the United States tends to provide a particularly effective illustration of their possible impacts on life expectancy.
Supplementary Material
Funding
Funding for this research was provided by the National Institute on Aging (P30AG012846 and R01AG060115) and the Eunice Kennedy Shriver National Institute of Child Health & Human Development (R00HD083519). This paper was published as part of a supplement sponsored by the University of Michigan with support from the National Institute on Aging (P30AG012846).
Conflict of Interest
None declared.
Acknowledgments
An earlier version of this paper was presented at the 2021 Annual Meeting of the TRENDS Network, May 13–14. The views expressed are those of the author alone and do not represent those of their employers or any funding agency.
Author Contributions
J. Y. Ho conceptualized and planned the study, performed the data analysis, and wrote and revised the manuscript.
References
- Arriaga, E. E. (1984). Measuring and explaining the change in life expectancies. Demography, 21(1), 83–96. doi: 10.2307/2061029 [DOI] [PubMed] [Google Scholar]
- Avendano, M., Glymour, M. M., Banks, J., & Mackenbach, J. P. (2009). Health disadvantage in US adults aged 50 to 74 years: A comparison of the health of rich and poor Americans with that of Europeans. American Journal of Public Health, 99(3), 540–548. doi: 10.2105/AJPH.2008.139469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banks, J., Marmot, M., Oldfield, Z., & Smith, J. P. (2006). Disease and disadvantage in the United States and in England. Journal of the American Medical Association, 295(17), 2037–2045. doi: 10.1001/jama.295.17.2037 [DOI] [PubMed] [Google Scholar]
- Banks, J., Muriel, A., & Smith, J. P. (2010). Disease prevalence, disease incidence, and mortality in the United States and in England. Demography, 47, S211–S231. doi: 10.1353/dem.2010.0008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry, H., Guillen, M. F., & Hendi, A. S. (2014). Is there convergence across countries? A spatial approach. Journal of International Business Studies, 45, 387–404. doi: 10.1057/jibs.2013.72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwyer-Lindgren, L., Bertozzi-Villa, A., Stubbs, R. W., Morozoff, C., Mackenbach, J. P., van Lenthe, F. J., Mokdad, A. H., & Murray, C. J. L. (2017). Inequalities in life expectancy among US counties, 1980 to 2014: Temporal trends and key drivers. JAMA Internal Medicine, 177(7), 1003–1011. doi: 10.1001/jamainternmed.2017.0918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elo, I. T., Hendi, A. S., Ho, J. Y., Vierboom, Y. C., & Preston, S. H. (2019). Trends in non-Hispanic White mortality in the United States by metropolitan–nonmetropolitan status and region, 1990–2016. Population and Development Review, 45(3), 549–583. doi: 10.1111/padr.12249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans, L. (2014). Traffic fatality reductions: United States compared with 25 other countries. American Journal of Public Health, 104(8), 1501–1507. doi: 10.2105/AJPH.2014.301922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal Statistical Office of Germany . (2021). GENESIS—Online Database.https://www-genesis.destatis.de/genesis/online/logon?language=en
- Fenelon, A., Chen, L. H., & Baker, S. P. (2016). Major causes of injury, death and the life expectancy gap between the United States and other high-income countries. Journal of the American Medical Association, 315(6), 609–611. doi: 10.1001/jama.2015.15564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia, K., & Crimmins, E. M. (2013). Cancer screening in the U.S. and Europe: Policies, practices, and trends in cancer incidence and mortality. In Hoque N., McGehee M. A., & Bradshaw B. S. (Eds.), Applied demography and public health (pp. 125–154). Springer. doi: 10.1007/978-94-007-6140-7_9 [DOI] [Google Scholar]
- Guillén, M. F. (2020). 2030: How today’s biggest trends will collide and reshape the future of everything. St. Martin’s Press. [Google Scholar]
- Harper, S., Rushani, D., & Kaufman, J. S. (2012). Trends in the black–white life expectancy gap, 2003–2008. Journal of the American Medical Association, 307(21), 2257–2259. doi: 10.1001/jama.2012.5059 [DOI] [PubMed] [Google Scholar]
- Hemenway, D., & Miller, M. (2000). Firearm availability and homicide rates across 26 high-income countries. The Journal of Trauma, 49(6), 985–988. doi: 10.1097/00005373-200012000-00001 [DOI] [PubMed] [Google Scholar]
- Hendi, A. S. (2015). Trends in U.S. life expectancy gradients: The role of changing educational composition. International Journal of Epidemiology, 44(3), 946–955. doi: 10.1093/ije/dyv062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendi, A. S. (2017). Trends in education-specific life expectancy, data quality, and shifting education distributions: A note on recent research. Demography, 54(3), 1203–1213. doi: 10.1007/s13524-017-0574-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendi, A. S., Elo, I. T., & Martikainen, P. (2021). The implications of changing education distributions for life expectancy gradients. Social Science & Medicine (1982), 272, 113712. doi: 10.1016/j.socscimed.2021.113712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho, J. Y. (2013). Mortality under age 50 accounts for much of the fact that US life expectancy lags that of other high-income countries. Health Affairs (Project Hope), 32(3), 459–467. doi: 10.1377/hlthaff.2012.0574 [DOI] [PubMed] [Google Scholar]
- Ho, J. Y. (2019). The contemporary American drug overdose epidemic in international perspective. Population and Development Review, 45(1), 7–40. doi: 10.1377/hlthaff.2012.0574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho, J. Y. (2020). Causes of gains and losses in life expectancy in OECD countries. In OECD/The King’s Fund (Ed.), Cardiovascular disease slowing improvements in life expectancy?: OECD and the King’s Fund Workshop proceedings (pp. 39–52). OECD Publishing. doi: 10.1787/47a04a11-en [DOI] [Google Scholar]
- Ho, J. Y., & Fenelon, A. (2015). The contribution of smoking to educational gradients in U.S. life expectancy. Journal of Health and Social Behavior, 56(3), 307–322. doi: 10.1177/0022146515592731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho, J. Y., & Hendi, A. S. (2018). Recent trends in life expectancy across high income countries: Retrospective observational study. BMJ (Clinical Research Ed.), 362, k2562. doi: 10.1136/bmj.k2562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho, J. Y., & Preston, S. H. (2010). US mortality in an international context: Age variations. Population and Development Review, 36(4), 749–773. doi: 10.1111/j.1728-4457.2010.00356.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine & National Research Council . (2013). U.S. health in international perspective: Shorter lives, poorer health. The National Academies Press. doi: 10.17226/13497 [DOI] [PubMed] [Google Scholar]
- Italian National Institute of Statistics . (2021). I.Stat.https://www.istat.it/en/
- MacDorman, M. F., Mathews, T. J., Mohangoo, A. D., & Zeitlin, J. (2014). International comparisons of infant mortality and related factors: United States and Europe, 2010. National Vital Statistics Reports, 63(5), 1–6. [PubMed] [Google Scholar]
- Mackenbach, J. P., Stirbu, I., Roskam, A. J., Schaap, M. M., Menvielle, G., Leinsalu, M., & Kunst, A. E.; European Union Working Group on Socioeconomic Inequalities in Health . (2008). Socioeconomic inequalities in health in 22 European countries. The New England Journal of Medicine, 358(23), 2468–2481. doi: 10.1056/NEJMsa0707519 [DOI] [PubMed] [Google Scholar]
- Manton, K. G., & Vaupel, J. W. (1995). Survival after the age of 80 in the United States, Sweden, France, England, and Japan. The New England Journal of Medicine, 333(18), 1232–1235. doi: 10.1056/NEJM199511023331824 [DOI] [PubMed] [Google Scholar]
- Martikainen, P., Ho, J. Y., Preston, S., & Elo, I. T. (2013). The changing contribution of smoking to educational differences in life expectancy: Indirect estimates for Finnish men and women from 1971 to 2010. Journal of Epidemiology and Community Health, 67(3), 219–224. doi: 10.1136/jech-2012-201266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massey, D. S. (1995). Getting away with murder: Segregation and violent crime in urban America. University of Pennsylvania Law Review, 143(5), 1203–1232. doi: 10.2307/3312474 [DOI] [Google Scholar]
- Mehta, N. K., Abrams, L. R., & Myrskylä, M. (2020). US life expectancy stalls due to cardiovascular disease, not drug deaths. Proceedings of the National Academy of Sciences of the United States of America, 117(13), 6998–7000. doi: 10.1073/pnas.1920391117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy, S. L., Xu, J., Kochanek, K. D., Arias, E., & Tejada-Vera, B. (2021). Deaths: Final data for 2018. National Vital Statistics Reports, 69(13), 1–82. [PubMed] [Google Scholar]
- National Research Council . (2011). Explaining divergent levels of longevity in high-income countries. The National Academies Press. doi: 10.17226/13089 [DOI] [PubMed] [Google Scholar]
- Oeppen, J., & Vaupel, J. W. (2002). Demography. Broken limits to life expectancy. Science (New York, N.Y.), 296(5570), 1029–1031. doi: 10.1126/science.1069675 [DOI] [PubMed] [Google Scholar]
- Palloni, A., & Yonker, J. A. (2016). Is the US old-age mortality advantage vanishing?1. Population and Development Review, 42(3), 465–489. doi: 10.1111/j.1728-4457.2016.00157.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson, R. D., & Krivo, L. J. (1993). Racial segregation and black urban homicide. Social Forces, 71(4), 1001–1026. doi: 10.1093/sf/71.4.1001 [DOI] [Google Scholar]
- Peterson, R. D., & Krivo, L. J. (1999). Racial segregation, the concentration of disadvantage, and black and white homicide victimization. Sociological Forum, 14(3), 465–493. doi: 10.1023/A:1021451703612 [DOI] [Google Scholar]
- Preston, S. H., Glei, D. A., & Wilmoth, J. R. (2010). A new method for estimating smoking-attributable mortality in high-income countries. International Journal of Epidemiology, 39(2), 430–438. doi: 10.1093/ije/dyp360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston, S. H., Heuveline, P., & Guillot, M. (2001). Demography: Measuring and modeling population processes. Wiley-Blackwell. [Google Scholar]
- Preston, S. H., & Ho, J. Y. (2011). Low life expectancy in the United States: Is the health care system at fault? In Crimmins E. M., Preston S. H., & Cohen B. (Eds.), International differences in life expectancy at older ages: Dimensions and sources (pp. 259–298). The National Academies Press. [PubMed] [Google Scholar]
- Preston, S. H., & Vierboom, Y. C. (2021). Excess mortality in the United States in the 21st century. Proceedings of the National Academy of Sciences of the United States of America, 118(16). doi: 10.1073/pnas.2024850118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raleigh, V. S. (2019). Trends in life expectancy in EU and other OECD countries. OECD Health Working Papers. OECD Publishing. https://www.oecd-ilibrary.org/content/paper/223159ab-en [Google Scholar]
- Richardson, E. G., & Hemenway, D. (2011). Homicide, suicide, and unintentional firearm fatality: Comparing the United States with other high-income countries, 2003. The Journal of Trauma, 70(1), 238–243. doi: 10.1097/TA.0b013e3181dbaddf [DOI] [PubMed] [Google Scholar]
- Siegel, M., Ross, C. S., & King, C.3rd. (2013). The relationship between gun ownership and firearm homicide rates in the United States, 1981–2010. American Journal of Public Health, 103(11), 2098–2105. doi: 10.2105/AJPH.2013.301409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistik Austria . (2021). STATcube.https://www.statistik.at/web_de/services/statcube/index.html
- Transportation Research Board . (2011). Achieving traffic safety goals in the United States: Lessons from other nations. The National Academies Press. doi: 10.17226/13046 [DOI] [Google Scholar]
- University of California, Berkeley (USA), & Max Planck Institute for Demographic Research (Germany) . (2021). Human mortality database.www.mortality.org
- van Hedel, K., Avendano, M., Berkman, L. F., Bopp, M., Deboosere, P., Lundberg, O., Martikainen, P., Menvielle, G., van Lenthe, F. J., & Mackenbach, J. P. (2015). The contribution of national disparities to international differences in mortality between the United States and 7 European countries. American Journal of Public Health, 105(4), e112–e119. doi: 10.2105/AJPH.2014.302344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verguet, S., & Jamison, D. T. (2013). Improving life expectancy: How many years behind has the USA fallen? A cross-national comparison among high-income countries from 1958 to 2007. BMJ Open, 3(7), 1-8. doi: 10.1136/bmjopen-2013-002814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vierboom, Y. C., Preston, S. H., & Hendi, A. S. (2019). Rising geographic inequality in mortality in the United States. SSM—Population Health, 9, 100478. doi: 10.1016/j.ssmph.2019.100478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, H., Schumacher, A. E., Levitz, C. E., Mokdad, A. H., & Murray, C. J. (2013). Left behind: Widening disparities for males and females in US county life expectancy, 1985–2010. Population Health Metrics, 11(1), 8. doi: 10.1186/1478-7954-11-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2021). WHO mortality database.https://www.who.int/data/data-collection-tools/who-mortality-database
- Xu, J., Murphy, S. L., Kochanek, K. D., & Arias, E. (2020). Mortality in the United States, 2018. NCHS Data Brief, 355, 1-8. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.