BACKGROUND
Subcuticular suture is an important technique for achieving optimum wound closure, and there has been no comprehensive summary of subcuticular sutures to date.
OBJECTIVE
To summarize the origin and development of interrupted subcuticular suture to help clinicians improve their wound closure skills.
MATERIALS AND METHODS
A comprehensive review of subcuticular suture techniques was conducted in PubMed to summarize the advantages and disadvantages of various methods and clinical indications.
RESULTS
Buried suture is the oldest subcuticular suture technique, followed by buried vertical mattress suture, intracutaneous butterfly suture, modified/variant buried vertical mattress suture, intradermal buried vertical mattress suture, buried horizontal mattress suture, wedge-section and modified buried vertical mattress suture, set-back suture, and modified buried horizontal mattress suture, which have gradually been applied in clinical practice. Buried vertical mattress suture is currently the most widely used subcuticular suture technique.
CONCLUSION
Patients can certainly benefit from the appropriate application of subcuticular suture. There is also no single ideal method for achieving optimal results in all cases. Fully understanding the history of subcuticular suture can help doctors improve their wound closure technique.
Wound closure techniques are important for skin and soft tissue repair after trauma and surgery, and suture is still the most widely used closure method for all wound types.1–3 Suture techniques can be divided into percutaneous and subcuticular suture techniques. The percutaneous suture is a transdermal suture where the suture pierces the skin completely and the knot is on the skin surface, while the subcuticular suture is an intradermal suture where the sutures are placed under the epidermis.1,4 Compared with other wound closure techniques, the subcuticular suture can improve the aesthetic outcomes of scars without increasing the wound infection rate.5–7 However, most of the subcuticular suture techniques reported in clinical studies are traditional basic techniques with minimal tension-reduction effects, such as the simple buried suture or continuous intradermal suture techniques.6–9 The technical details are not even very well-known by professional dermatologists and plastic surgeons.4
There has been no comprehensive summary of subcuticular sutures to date; in this study, we systematically summarize the origin and development of interrupted subcuticular sutures (Table 1).
TABLE 1.
List of Classic Subcuticular Suture Technique
| Category | Suture Techniques | Advantages | Disadvantages |
| Planar suture | Halsted's buried suture; Intradermal buried vertical mattress suture | • Easy mastery • Precise apposition • No suture marks |
• Less firmly anchored • Wound dehiscence risk • No wound eversion |
| Eversion suture | Buried vertical mattress suture; Intracutaneous butterfly suture; Modified/variant vertical mattress suture; Buried horizontal mattress suture | • Prolonged wound edge eversion • Stable anchored • Long-term tension reduction • Strong stability |
• Practice to master • Limited to needle size incidentally • Occasional suture marks |
| Super-tension-reduction suture | Double butterfly suture; WE-MBVMS; Set-back suture; Modified buried horizontal mattress suture | • Broadly anchored • Great tension relief • Prominent wound eversion • No suture marks |
• Complex operation • Limitation in thin dermis or tiny wounds • Prolonged surgery time |
The subcuticular suture techniques we discussed above can be divided into 3 categories: planar sutures, eversion sutures, and super-tension-reduction sutures. The table shows a summary of their main advantages and disadvantages.
WE-MBVMS, wedge-shaped excision and modified buried vertical mattress suture.
Methods
A comprehensive search of PubMed was conducted to identify articles related to subcuticular suture techniques. The search terms included interrupted subcuticular suture, buried suture, and tension-reduction suture. The non-English language was the only exclusion criteria. The bibliographies of relevant articles were searched for additional references.
Origin of the Subcuticular Suture Technique
The subcuticular suture was invented at the end of the 19th century to reduce wound infection and promote wound healing.10,11 William S. Halsted first proposed the concept of buried sutures for treating inguinal hernias.12,13 Halsted's suture technique for skin closure over the repaired hernia cord involved burying interrupted sutures of fine silk in dogs, and these buried silk sutures were placed entirely within the lower layer of the skin without contacting contaminants on the skin surface10(Figure 1A, B). During the experiment, Halsted found that wound infection rates decreased notably with buried sutures. Until 1895, the subcuticular suture remained the same. Gradually, the subcuticular suture has been proven to reduce the width of scars because of their tension-reducing effects on wound edges, and doctors have started trying to use absorbable sutures instead of nonabsorbable sutures for subcuticular suture.14,15
Figure 1.
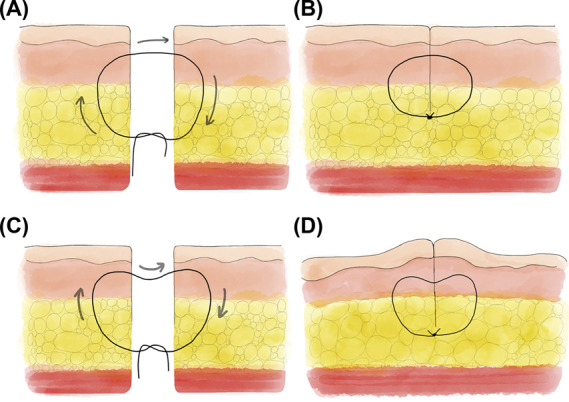
Comparison of everted and plane sutures. (A) Suture path of Halsted's buried sutures; (B) side view after buried suture with a planar wound; (C) suture path of buried vertical sutures; (D) ridge-like side view after buried vertical suture with wound edge eversion.
Evolution of the Subcuticular Suture Technique
Buried sutures are essentially planar closures with minimal skin edge eversion and tension-reduction effects.16 This is far from ideal for doctors who insist on avoiding “cosmetically unappealing scars.”17 Since then, the development of the subcuticular suture technique is mainly to change the needle entry point, exit point, and the rivet point of the skin, in return for better effect of tension-reduction and skin edge eversion effects.18
Buried Vertical Mattress Suture
In 1989, Zitelli and Moy19 proposed the buried vertical mattress suture, combining the advantages of the vertical mattress suture and the buried intradermal suture, which could be considered a milestone in subcuticular suture. The most significant technical change was that the suture was placed snugly against the epidermis, 3 to 4 mm from the skin edge, and brought out in the deeper dermis (Figure 1C). This was the first breakthrough in the transformation of the subcuticular suture from planar closure to everted closure (Figure 1D). The modified technique offers prolonged dermal support and prolonged wound eversion. Since their development, buried vertical mattress suture has been the most widely used subcuticular suture, especially among dermatologists and plastic surgeons.20
Intracutaneous Butterfly Suture
Aiming at obtaining a suture with greater stability and convenience, Dr. Breuninger21 invented a new technique named the intracutaneous butterfly suture in 1993. As shown in Figure 2A, B, scalpel excision was performed not perpendicularly to the skin surface but rather obliquely (or horizontally) to increase the contact area of the wound edge and thus gain better wound eversion. Compared with buried vertical mattress suture, it provides greater tension relief, and the inflammatory response produced by the suture material is theoretically less, with almost no suture material at the wound surface. Tying the knot is reportedly easier because the knot lies not underneath but besides the loop of the suture. Based on Breuninger's 6-year experience involving 18,000 procedures, intracutaneous butterfly suture provides maximum skin eversion with exact epidermal apposition and achieves appealing cosmetic results.21
Figure 2.
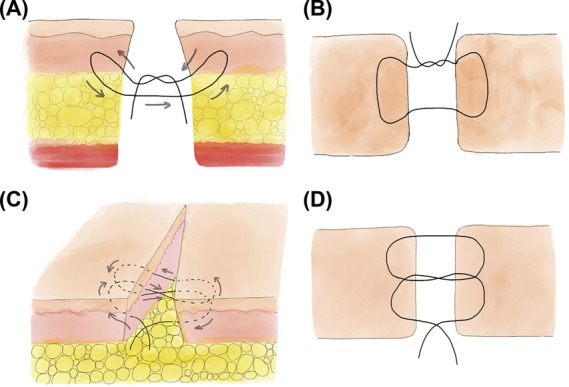
Intradermal butterfly suture. (A) Suture path of a single intradermal butterfly suture; (B) view from above, with the suture arcs as the wings and the knot as the head of a butterfly; (C) suture path of a double butterfly suture; (D) the 2 mirrored “S,” view from above.
Later, in 2000, Dr. Breuninger modified his single butterfly suture to be a double butterfly suture to provide high-tension wound closure (Figure 2C, D).22 In this way, the length of the wound closed in a single suture is equivalent to that closed with 3 vertical mattress sutures. With the suture knot anchored deep beneath the corium, it will achieve greater tension support and a lower rate of knot perforation.23
Modified/Variant Buried Vertical Mattress Suture
To enhance suture efficiency, Neil Sadick24 modified the buried vertical mattress suture and published their results in 1994. The mattress suture was not placed under the epidermis but directly punctured the skin, and there was no need for superficial sutures (Figure 3A). This method has been proven to be easier technically, reduce operation time, and avoid the need for stitch removal. Similarly, in late 2002, Berry25 proposed the variant vertical mattress suture, which is quite similar to Sadick's modified vertical mattress suture. The difference is that it starts in the subcutaneous layer, but not the reticular dermis. The benefits include ease of placement, successful eversion, firm anchoring, and being especially suitable for narrow and superficial wounds.26,27 According to the results of a double-blind randomized study conducted by Sadick, the modified buried vertical mattress suture produced less hypertrophic scar/keloid formation (2% vs 16%), less wound scar spread (6% vs 24%), and a higher degree of patient satisfaction (96%).24 However, occasional residual thread on the skin surface suture creates potential hazards for fraying, suture breakage, local tissue necrosis, infection, and reactive fibrosis at the exposed suture points.24,28–30 The techniques may be more suited for thick dermal cutaneous anatomic areas, such as truncal and extremity sites, than the face.24
Figure 3.
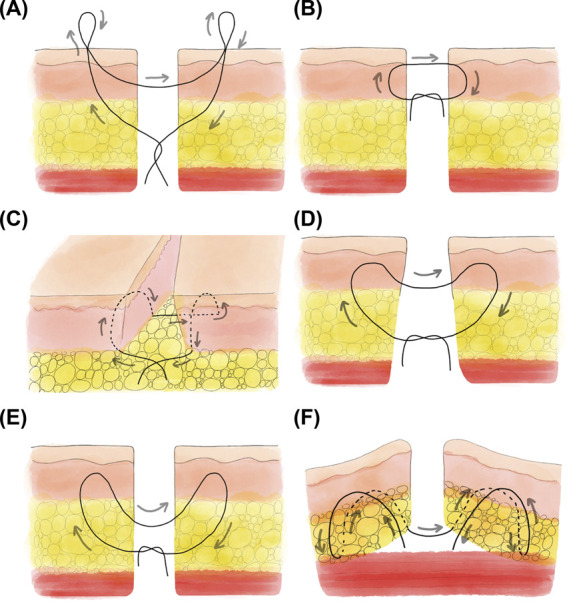
Suture path of developed subcuticular suture techniques. (A) Modified buried vertical mattress suture; (B) intradermal buried vertical mattress suture; (C) buried horizontal mattress suture; (D) WE-MBVMS; (E) set-back suture; (F) modified buried horizontal mattress suture. WE-MBVMS, wedge-shaped excision and modified buried vertical mattress suture.
Intradermal Buried Vertical Mattress Suture
In 2000, Hohenleutner29 slightly modified the standard buried vertical mattress suture, advocating that the superior arc of the suture should be extremely superficial to the epidermis to achieve perfect apposition of the wound edges (Figure 3B). Hohenleutner applied his modified technique as a sole skin closure method in 149 procedures in 126 patients. As the results showed, additional sutures could be omitted in most cases without worsening the cosmetic result or increasing the frequency of complications (14.7% rate of the need of additional superficial sutures). Notably, the cosmetic outcomes in the face achieved excellent and good results in 89.1% and were even better than those in any other anatomical region.29 Taking this into account, Hohenleutner suggested that this technique can be used safely in areas with relatively thin skin, but not in areas with very fine, thin skin, such as the lips, periorbital areas, or ears. In 2018, Yang and colleagues31 compared this method with traditional running subcuticular sutures for cesarean sections and showed that the former was cosmetically superior (lower scar assessment score and higher overall satisfaction, p < .01).
Buried Horizontal Mattress Suture
Buried vertical mattress sutures are not the best choice for regions where the dermis is extremely thin or for shallow wounds because angling the suture upward in the dermis may be less practical for inducing eversion.19,26,32 In 2004, Alam and Goldberg26 invented the buried horizontal mattress suture. The procedures of the 2 methods are almost the same, while the latter changes the needle direction from vertical to horizontal (Figure 3C). Technically, this method is particularly useful for small apertures or narrow defects where a deep stitch is required but where it is difficult to insert the needle.
Wedge-Section and Modified Buried Vertical Mattress Suture
To further enhance the wound tension-reduction effect, Mao-Guo Shu and colleagues proposed a subcuticular suture referred to as wedge-shaped excision and modified buried vertical mattress suture (WE-MBVMS).33 The premise of WE-MBVMS is that wedge-shaped excision is performed first and then the needle is inserted in the subcutaneous tissue obliquely, enters the middermis repeatedly along an arc track, and involves the dermis as much as possible (Figure 3D).34 Current clinical trials have verified its good cosmetic effect and safety in high-tension wound closure. Liu's split-scar model showed that WE-MBVMS significantly increased wound eversion both immediately and postoperatively and performed significantly better on the scar assessment at the end of the 3-month follow-up period than intradermal buried sutures.34,35 Similar to other subcuticular sutures, it is not useful for extremely thin dermis or tiny wounds.19–21
Set-Back Suture
Another super-tension-reduction suture was invented by Kantor in 2010, namely, the set-back suture.36 Unlike previous suture techniques, there is no suture through the dermis of the incision with this technique (Figure 3E). Kantor identified the following advantages of his method: ease of use, dramatic wound eversion, decreased risk of suture spitting, minimization of dead space, and no limitation of the needle radius.36 Compared with that of the buried vertical suture, the tension vector of the tied set-back suture results in an upward push on the suture line, leading to dramatic wound eversion. Increased bulk of the tissue in the dermis helps to achieve greater tension reduction.37 This technique is especially beneficial for larger defects with a thicker dermis, such as the trunk, scalp, and extremities. Audrey included 42 split wounds to compare the cosmetic outcomes and wound eversion achieved with set-back suture and buried vertical mattress suture.20 They found that the set-back suture yielded significant wound eversion. Both patient and observer total patients and observer assessment scale scores were significantly lower on the set-back suture side. Wang combined set-back suture with radiotherapy to treat chest keloids and successfully decreased the rate of keloid relapse to 2.2%.37 Despite its great performance, further studies about whether it significantly reduces wound tension remain to be performed.
Modified Buried Horizontal Mattress Suture
To achieve an improved and longer-lasting effect of tension reduction, Meng proposed a new suture technique called the modified subcutaneous buried horizontal mattress suture in 2017.32 Meng made 2 subcutaneous buried horizontal mattress sutures through sole intermittent suture (Figure 3F). The in vitro trial showed that the modified technique greatly decreased tension on the dermis and subcutaneous tissue compared with buried vertical mattress suture. As Meng described, its 4 arc segments provide a much more active area than traditional suture loops, and the thread catches more tissue from both the dermal and subcutaneous layers, so the pressure on the affected tissue is lower and has little chance of causing ischemia.18
Conclusion
As Gregory T. Fisher10 wrote, “The subcuticular suture has its origins not in the work of one individual but in that of generations of surgeons interested in obtaining the best wound healing possible.” In general, the subcuticular suture technique can avoid the transverse scars because of the additional damage to skin tissue caused by traditional interrupted sutures and alleviate the pain of removing the sutures for patients.38 At the same time, the subcuticular suture can obtain better cosmetic outcomes because of their tension-reduction and skin edge eversion effects. Buried vertical mattress suture is currently the most widely used subcuticular suture technique, while the set-back suture is easier to perform and permits aggressive minimization of dead space. Appropriate application of subcuticular suture can certainly benefit patients, but this does not mean that they can completely replace traditional suture. Compared with that of percutaneous suture, the learning curve of the subcuticular suture is longer, and intraoperative sutures take more time.19–21,26 Thin skin and fragile skin are not suitable for subcuticular suture, with risks of suture extrusion to the epidermal surface, and surgical sutures left in the skin may increase the risk of infection.
Realizing the best wound healing, avoiding pathological scars, and achieving an “invisible scar” is an ongoing challenge for all surgeons, and it is an important task that we need to work together to address.
Footnotes
The authors have indicated no significant interest with commercial supporters.
W. Zhang and J. Xie contributed equally to this work.
Contributor Information
WenChao Zhang, Email: 13051159771@163.com.
Ang Zeng, Email: xiejiangmiao@163.com.
References
- 1.Azmat CE, Council M. Wound Closure Techniques. In: StatPearls. Treasure Island, FL: StatPearls Publishing Copyright © 2021, StatPearls Publishing LLC.; 2021. [PubMed] [Google Scholar]
- 2.Ku D, Koo DH, Bae DS. A prospective randomized control study comparing the effects of dermal staples and intradermal sutures on postoperative scarring after thyroidectomy. J Surg Res 2020;256:413–21. [DOI] [PubMed] [Google Scholar]
- 3.Tandon S, Smale M, Pacilli M, Nataraja RM. Tissue adhesive and adhesive tape for pediatric wound closure: a systematic review and meta-analysis. J Pediatr Surg 2021;56:1020–9. [DOI] [PubMed] [Google Scholar]
- 4.Regula CG, Yag-Howard C. Suture products and techniques: what to use, where, and why. Dermatol Surg 2015;41(Suppl 10):S187–200. [DOI] [PubMed] [Google Scholar]
- 5.Chen ZS, Zhu SL, Qi LN, Li LQ. A combination of subcuticular suture and enhanced recovery after surgery reduces wound complications in patients undergoing hepatectomy for hepatocellular carcinoma. Sci Rep 2018;8:12942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berghella V, Baxter JK, Mackeen AD. Suture is still the gold standard for closure of the skin incision at caesarean delivery. BJOG 2019;126:511. [DOI] [PubMed] [Google Scholar]
- 7.Lima RJ, Schnaider TB, Francisco AMC, FrancescatoVeiga D. Absorbable suture. Best aesthetic outcome in cesarian scar1. Acta Cir Bras 2018;33:1027–36. [DOI] [PubMed] [Google Scholar]
- 8.Mahalingam S, Alatsatianos A, Pitkin L, D'Souza A. Does the technique of skin closure affect the cosmesis of cervical thyroidectomy and parathyroidectomy scars? A review of literature. Facial Plast Surg 2018;34:524–8. [DOI] [PubMed] [Google Scholar]
- 9.Shin TM, Bordeaux JS. How suture technique affects the cosmetic outcome of cutaneous repairs. J Drugs Dermatol 2014;13:967–9. [PubMed] [Google Scholar]
- 10.Fisher GT, Fisher JB, Stark RB. Origin of the use of subcuticular sutures. Ann Plast Surg 1980;4:144–8. [DOI] [PubMed] [Google Scholar]
- 11.Mashhadi SA, Loh CYY. Subcuticular suture—is it a misnomer? Eur J Plast Surg 2010;33:233. [Google Scholar]
- 12.Halsted WS, III. The radical cure of inguinal hernia in the male. Ann Surg 1893;17:542–56. [PMC free article] [PubMed] [Google Scholar]
- 13.William Stewart Halsted (1852–1922). CA Cancer J Clin 1973;23:94–5. [DOI] [PubMed] [Google Scholar]
- 14.Sanders RJ. Subcuticular skin closure—description of technique. J Dermatol Surg 1975;1:61–4. [DOI] [PubMed] [Google Scholar]
- 15.Winn HR, Jane JA, Rodeheaver G, Edgerton MT, et al. Influence of subcuticular sutures on scar formation. Am J Surg 1977;133:257–9. [DOI] [PubMed] [Google Scholar]
- 16.Ogawa R, Akaishi S, Huang C, Dohi T, et al. Clinical applications of basic research that shows reducing skin tension could prevent and treat abnormal scarring: the importance of fascial/subcutaneous tensile reduction sutures and flap surgery for keloid and hypertrophic scar reconstruction. J Nippon Med Sch 2011;78:68–76. [DOI] [PubMed] [Google Scholar]
- 17.Harn HI, Ogawa R, Hsu CK, Hughes MW, et al. The tension biology of wound healing. Exp Dermatol 2019;28:464–71. [DOI] [PubMed] [Google Scholar]
- 18.Meng F, Andrea S, Cheng S, Wang Q, et al. Modified subcutaneous buried horizontal mattress suture compared with vertical buried mattress suture. Ann Plast Surg 2017;79:197–202. [DOI] [PubMed] [Google Scholar]
- 19.Zitelli JA, Moy RL. Buried vertical mattress suture. J Dermatol Surg Oncol 1989;15:17–9. [DOI] [PubMed] [Google Scholar]
- 20.Wang AS, Kleinerman R, Armstrong AW, Fitzmaurice S, et al. Set-back versus buried vertical mattress suturing: results of a randomized blinded trial. J Am Acad Dermatol 2015;72:674–80. [DOI] [PubMed] [Google Scholar]
- 21.Breuninger H, Keilbach J, Haaf U. Intracutaneous butterfly suture with absorbable synthetic suture material. Technique, tissue reactions, and results. J Dermatol Surg Oncol 1993;19:607–10. [DOI] [PubMed] [Google Scholar]
- 22.Breuninger H. Double butterfly suture for high tension: a broadly anchored, horizontal, buried interrupted suture. Dermatol Surg 2000;26:215–8. [DOI] [PubMed] [Google Scholar]
- 23.Kantor J. The running butterfly suture: a novel, everting alternative to the running subcuticular technique. J Am Acad Dermatol 2016;74:e19–20. [DOI] [PubMed] [Google Scholar]
- 24.Sadick NS, D'Amelio DL, Weinstein C. The modified buried vertical mattress suture. J Dermatol Surg Oncol 1994;20:735–9. [DOI] [PubMed] [Google Scholar]
- 25.Berry MG, Ion L. Variant mattress suture for skin closure. Br J Plast Surg 2002;55:178. [DOI] [PubMed] [Google Scholar]
- 26.Alam M, Goldberg LH. Utility of fully buried horizontal mattress sutures. J Am Acad Dermatol 2004;50:73–6. [DOI] [PubMed] [Google Scholar]
- 27.Collins SC, Whalen JD. Surgical pearl: percutaneous buried vertical mattress for the closure of narrow wounds. J Am Acad Dermatol 1999;41:1025–6. [DOI] [PubMed] [Google Scholar]
- 28.Justan I. New type of skin suture—fully buried running mattress suture. J Plast Reconstr Aesthet Surg 2010;63:e338–9. [DOI] [PubMed] [Google Scholar]
- 29.Hohenleutner U, Egner N, Hohenleutner S, Landthaler M. Intradermal buried vertical mattress suture as sole skin closure: evaluation of 149 cases. Acta Dermato-Venereologica 2000;80:344–7. [DOI] [PubMed] [Google Scholar]
- 30.Maher IA, Bingham J, Mellette R. A running modification of the percutaneous buried vertical mattress. Dermatol Surg 2012;38:1560–2. [DOI] [PubMed] [Google Scholar]
- 31.Yang J, Kim KH, Song YJ, Kim SC, et al. Cosmetic outcomes of cesarean section scar; subcuticular suture versus intradermal buried suture. Obstet Gynecol Sci 2018;61:79–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Epstein E. The buried horizontal mattress suture. Cutis 1979;24:104–6. [PubMed] [Google Scholar]
- 33.Zhang X, Diao JS, Guo SZ, Han Y, et al. Wedge-shaped excision and modified vertical mattress suture fully buried in a multilayered and tensioned wound closure. Aesthet Plast Surg 2009;33:457–60. [DOI] [PubMed] [Google Scholar]
- 34.Liu ZH, Tang ZS, Hao XY, Liu XY, et al. Modified buried vertical mattress suture versus buried intradermal suture: a prospective split-scar study. Dermatol Surg 2021;47:e75–e80. [DOI] [PubMed] [Google Scholar]
- 35.Liu Z, Liu X, He L, Yu X, et al. Different suturing techniques in thoracic incision: protocol for a feasibility randomised controlled trial. BMJ Open 2019;9:e021645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kantor J. The set-back buried dermal suture: an alternative to the buried vertical mattress for layered wound closure. J Am Acad Dermatol 2010;62:351–3. [DOI] [PubMed] [Google Scholar]
- 37.Wang LZ, Ding JP, Yang MY, Chen B. Forty-five cases of chest keloids treated with subcutaneous super-tension-reduction suture combined with postoperative electron-beam irradiation. Dermatol Surg 2014;40:1378–84. [DOI] [PubMed] [Google Scholar]
- 38.Pratsinis H, Mavrogonatou E, Kletsas D. Scarless wound healing: from development to senescence. Adv Drug Deliv Rev 2019;146:325–43. [DOI] [PubMed] [Google Scholar]


