Abstract
Objective
The aim was to assess rheumatology clinicians’ perceptions of telemedicine and their experiences before and during the coronavirus disease 2019 (COVID-19) pandemic.
Methods
We conducted a cross-sectional online survey and collected responses from rheumatology clinicians worldwide, between November 2020 and February 2021, regarding use and perceptions of telemedicine in rheumatology. We summarized data with descriptive statistics and qualitative analysis for free-text responses.
Results
The survey was completed by 349 rheumatology clinicians from 49 countries; 59% were female and about two-thirds were in the 30–50 years age group. Academic affiliations were held by 55% of participants, and 44% were from North America. Before the pandemic, 24% of participants had experience with telemedicine, whereas about three-quarters used telemedicine for the first time during the pandemic. Overall, 56% thought they provided less adequate care with telemedicine. More than half of clinicians felt that telemedicine was adequate for evaluating crystalline arthritis, inflammatory arthritis and lupus flares. Telemedicine was felt to be inadequate for flares of myositis, vasculitis and scleroderma. Technical problems were reported in 29% of telemedicine encounters and were most commonly related to patient-encountered difficulties.
Conclusion
Most rheumatology clinicians used telemedicine for the first time during the pandemic. The quality of care provided was thought to be inferior to that provided in person for specific clinical situations. Additional efforts are needed to address barriers to effective telemedicine, such as patient-related technology issues, challenges with building rapport and performing a physical examination, and to define the appropriate scope of clinical scenarios conducive to telemedicine.
Keywords: telemedicine, clinical practice
Key messages.
This was among the earliest surveys assessing telemedicine experiences of rheumatology clinicians during the coronavirus disease 2019 (COVID-19) pandemic.
Results of this study may help to inform the future role of telemedicine in routine care models within rheumatology practice.
Telemedicine in rheumatology practice may be effective in clinical cases without multi-system involvement.
Introduction
Telemedicine, the use of communications technology to enable health care without being physically located with the patient, was widely adopted when physical interactions were reduced during the coronavirus disease 2019 (COVID-19) pandemic [1–5]. Before the COVID-19 pandemic, telemedicine in rheumatology was rarely used and generally reserved for providing care to patients geographically remote from rheumatologists [6–8]. The role of telemedicine in improving rheumatological care and disease activity had been explored but not widely applied [9]. In a pragmatic randomized controlled trial evaluating the effectiveness of telemedicine in the care of patients with RA, disease control could be achieved in patients with low disease activity or in remission [10]. A pre-pandemic survey of German clinicians had overall positive perspectives on the application of telemedicine in rheumatology, specifically patient counselling [11]. Despite the favourability of telemedicine in rheumatology clinical practices, the use of this technology was not widespread before the COVID-19 pandemic [12]. The COVID-19 pandemic resulted in rapid, widespread use of telemedicine in rheumatology and other specialties, with the inability to plan in advance [13, 14]. In the wake of the Omicron variant spread worldwide, the use of telemedicine once again becomes relevant and important in reducing exposure within communities [15, 16].
Examples of telemedicine use during the COVID-19 pandemic include the national-level state health department teleconsultation service initiative, e-sanjeevani, in India [3], and the locally deployed TELEA telemedicine tool in the Spanish region of Lugo [13]. Similar tools were used in Saudi Arabia, Taiwan and various countries around the world [2, 17, 18]. Indeed, in a survey of physicians in the Veterans Affairs health-care system in the USA, the majority had not used telemedicine before the pandemic [19]. In a nationwide survey of German rheumatologists and general practitioners performed at the height of the COVID-19 pandemic, the majority rated their knowledge of telemedicine as unsatisfactory, poor or very poor, but many ended up having a positive view of the experience as the pandemic evolved [2]. Likewise, a survey of rheumatologists in The Netherlands also found positive perceptions of telemedicine, with the majority likely to continue use of telemedicine and recommend telemedicine to their colleagues [20]. Given the unique aspects of rheumatic diseases and the specialized care provided by rheumatologists, we aimed to describe the use and perceptions of telemedicine for rheumatology care before and during the COVID-19 pandemic in an international sample of rheumatologists, further building on surveys administered in a single country.
Methods
The COVID-19 Global Rheumatology Alliance (GRA) launched a cross-sectional online survey, conducted between 6 November 2020 and 2 February 2021, which was available to rheumatology care providers globally. The study was reviewed and approved by the Johns Hopkins Institutional Review Board (IRB00263536).
Survey instrument and administration
In addition to questions about demographics, the survey explored three main topics: clinical practice characteristics before the pandemic, telemedicine adoption and use during the pandemic, and perceived adequacy of telemedicine in different clinical scenarios in rheumatology practice (Appendix S1, available at Rheumatology Advances in Practice online). Statements with Likert scales for response were used to assess the adequacy of telemedicine in different clinical scenarios. Free-text responses were used to gather perspectives on future barriers and enablers of telemedicine in rheumatology. For the purposes of the survey, a ‘visit’ referred to in-person clinic attendance pre-pandemic and to a telemedicine event during the pandemic.
The survey was developed by the GRA Physician Telemedicine Working Group. Members of the working group were from North America, Europe and New Zealand. The members were practising rheumatologists (academic and non-academic) or rheumatology trainees. Team leads of this working group drafted the survey, gathered feedback from working group members and refined questions iteratively to provide clarity and reduce ambiguity. The survey was then piloted with working group members and finalized by working group leads. The survey was administered electronically via the Qualtrics platform (Supplementary Data S1, available at Rheumatology Advances in Practice online).
Participants and recruitment
Participants completed the survey anonymously. Our target study participants were clinical practitioners in rheumatology clinics worldwide. Participants were able to complete the online survey if they responded affirmatively to a screening question (‘Are you a rheumatology provider taking care of patients?’) and consented to the survey. This wording allowed for inclusion of rheumatologists, rheumatology trainees and rheumatology practitioners (nurse practitioners and physician assistants), to include all practitioners who might provide rheumatology care in different parts of the world. The format of the survey was such that participants who completed the survey in its entirety had used telemedicine during the COVID-19 pandemic. The survey link was promoted online and via email by professional rheumatology societies internationally to their members, including the ACR, EULAR, ILAR, Argentinian Society of Rheumatology, Brazilian Society of Rheumatology, German Society of Rheumatology, Kuwait Association of Rheumatology, Portuguese League Against Rheumatic Diseases, and Mexican College of Rheumatology. Regional leads of the GRA were asked to distribute invitation letters electronically and disseminate the survey link among local members. We also used social media to promote and distribute the survey.
Statistical analysis
Descriptive statistics were used to summarize participant characteristics and the survey responses. Comparisons and associations between participant characteristics and telemedicine use were examined using Student’s paired t-tests, χ2 tests or analysis of variance, where appropriate. A two-sided test P-value of <0.05 was considered statistically significant for differences between groups. All analyses were performed using Stata IC, v.15.1 (StataCorp, College Station, TX, USA) and R v.4.1.1.
Qualitative analysis
Free-text responses to questions on enablers and barriers to telemedicine during and after the COVID-19 pandemic were analysed by content analysis. Data were managed in Microsoft Excel. A conventional approach to content analysis was used, whereby categories were derived inductively from the data to identify overarching themes within the texts [9]. Two authors (R.G. and N.U.) made notes of their impressions of these texts and independently generated codes based on texts of survey responses. After a consensus meeting to confirm code categories, coding of data was completed and organized into themes. The final themes and sub-themes were confirmed at a consensus meeting of the working group.
Patient and public involvement
No patients were involved in the implementation of this study.
Results
The survey was opened by 771 individuals, with 349 rheumatology clinicians completing the survey. Of the 422 who were excluded from analysis, 247 did not qualify to participate because they did not identify themselves as rheumatology clinicians in the survey and 175 did not complete the survey (Fig. 1). Participants who completed the survey after question 21 (see Supplementary Data S1, available at Rheumatology Advances in Practice online), which contained questions regarding care provided via telemedicine during the COVID-19 pandemic, were sufficiently regarded as telemedicine users in our analysis.
Fig. 1.
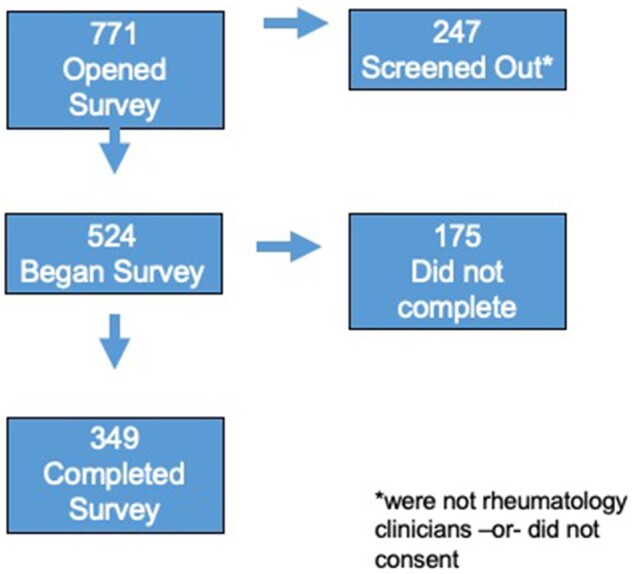
Flow chart of survey patients
Demographics and clinical practice characteristics of participants
Table 1 summarizes the characteristics of participants. The majority of respondents were in the age range of 30–50 years (220 of 349, 63%), and 59% (206 of 349) were female. Clinicians from 49 countries participated, with 55% of participants practising in academically affiliated institutions in North America, while 23% were from Europe. The majority of participants were rheumatology physicians (300 of 349, 86%), followed by rheumatology clinical providers such as nurse practitioners and physician assistants (49 of 349, 14%). Excluding trainee physicians, 79% (237 of 300) had been in practice for >5 years.
Table 1.
Demographics and clinical practice characteristics of participants
| Variable (N = 349) | n (%) |
|---|---|
| Age group, years | |
| <30 | 4 (1.1) |
| 30–40 | 115 (33) |
| 41–50 | 105 (30.1) |
| 51–60 | 88 (10.6) |
| >60 | 37 (10.6) |
| Sex | |
| Female | 206 (59) |
| Male | 141 (40.4) |
| Prefer not to say | 2 (0.6) |
| Region | |
| North America | 154 (44.3) |
| Europe | 81 (23.3) |
| Othera | 113 (32.5) |
| Type of rheumatology clinician | |
| Physician | 289 (83.8) |
| Trainee physician | 11 (3.2) |
| Non-physician (nurse practitioners, physician assistants) | 49 (14.0) |
| Practice settings | |
| Academic affiliation (>50% of time spent) | 193 (55.3) |
| Private practice/otherb | 156 (44.7) |
| Time in independent practice, years (N = 300)c | |
| 0–5 | 63 (21.0) |
| 6–10 | 65 (21.7) |
| 11–15 | 49 (16.3) |
| 16–20 | 42 (14.0) |
| >20 | 81 (27.0) |
| Pre-COVID-19, tTtal patients/week seen in office | |
| 0–5 | 20 (5.7) |
| 6–20 | 80 (22.9) |
| 21–50 | 144 (41.3) |
| >50 | 105 (30.1) |
Other regions include Africa, Asia, Australasia, Middle East and South America.
Non-governmental organizations, research facilities.
Excluding trainees and incorrect responses.
COVID-19: coronavirus disease 2019.
Characteristics of telemedicine use before and during COVID-19
About one-quarter (82 of 349, 24%) of participants had used telemedicine before the pandemic, most with use only once a week (34 of 82, 41%). Most rheumatology clinicians (298 of 349, 85%) continued to see patients in person during the pandemic; however, 72% (252 of 349) saw fewer patients compared with their pre-pandemic practice (Supplementary Table S1, available at Rheumatology Advances in Practice online). Since the implementation of telemedicine in their clinical practices, 36% (124 of 349) did not experience any change in the volume of patients, and volume did not increase for 48% (168 of 349) of participants. About half of telemedicine visits during the pandemic (177 of 349, 51%) were telephone only; 33% (116 of 349) used the Zoom video conference platform. Other modalities, such as WhatsApp and Attend Everywhere, were each used by <5% of participants. Telemedicine platforms integrated into the institution’s electronic medical record system were felt best to meet the needs of 44% (152 of 349) of respondents. Overall, 41% (144 of 349) of participants reported receiving reimbursements for both audio-only and audiovisual telemedicine encounters.
Perceived adequacy of telemedicine for different purposes
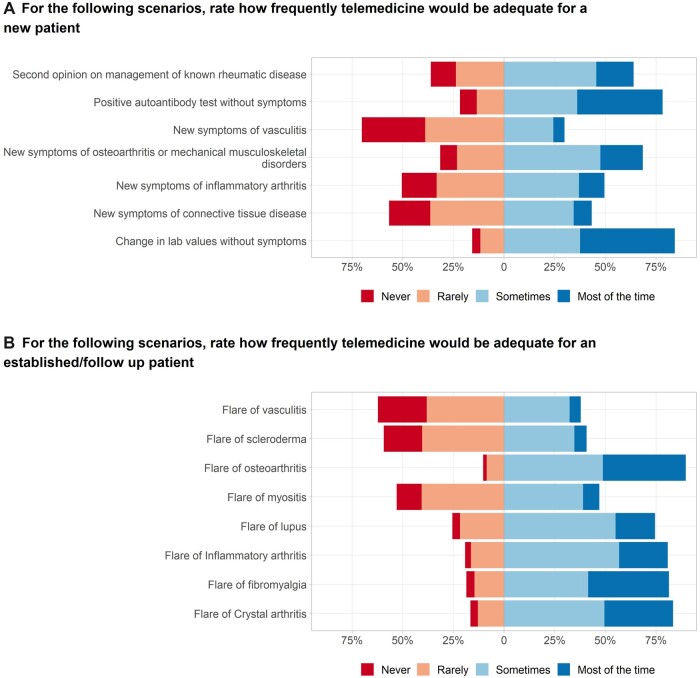
More than half of participants (56%, 198 of 349) reported they provided care via telemedicine that they rated as ‘worse care’ compared with in-person care. Most respondents (64%, 223 of 349) also reported that telemedicine would be adequate ‘sometimes’ or ‘most of the time’ for new patient visits when the patient was being seen for a second opinion, had OA or a non-inflammatory musculoskeletal complaint, or had a positive ANA or other laboratory abnormality without symptoms (Fig. 2A; the frequencies are provided in Supplementary Table S2, available at Rheumatology Advances in Practice online). The majority of respondents thought that telemedicine would ‘rarely’ or ‘never’ be adequate for new patients with symptoms of vasculitis or of a CTD (Fig. 2A). For established/follow-up patient visits, the majority indicated that telemedicine would be adequate ‘sometimes’ or ‘most of the time’ for flare of OA, lupus, inflammatory arthritis, FM or crystalline arthritis; and was ‘rarely’ or ‘never’ adequate to for patients with flare of vasculitis, myositis and scleroderma (Fig. 2B; the frequencies are provided in Supplementary Table S3, available at Rheumatology Advances in Practice online).
Fig. 2.
Perceived adequacy of telemedicine visits for new and follow-up visits
Barriers and facilitators to telemedicine use in rheumatology care
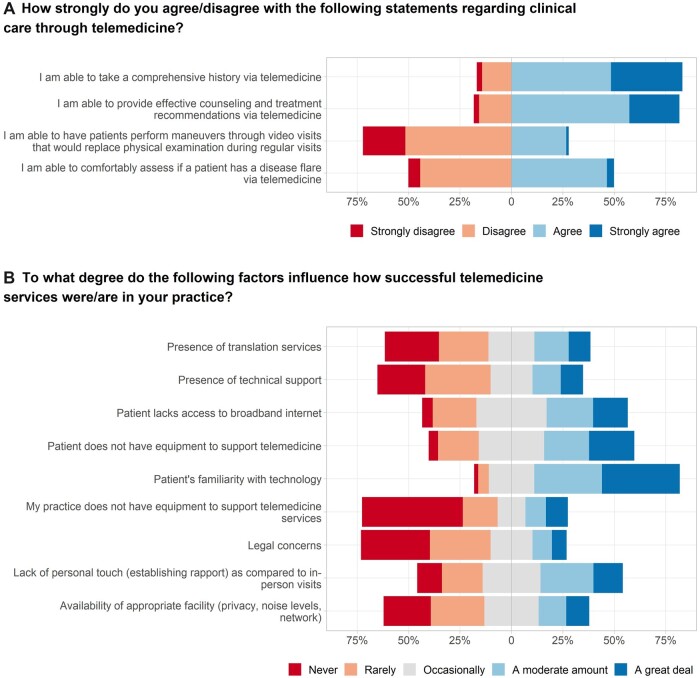
Technical issues were commonly reported by the survey respondents (Table 2); the median percentage of encounters reported to have technical issues was 29% (interquartile range: 11%, 40%). Patient-related technical issues were cited as more common by 59% (205 of 349) of clinicians, while 22% (78 of 349) thought that technical issues were equally common for clinicians and patients. The majority of participants (82%) agreed or strongly agreed that they could take a history or provide counselling via telemedicine. In contrast, the majority of respondents (72%) disagreed or strongly disagreed that patients could carry out a physical assessment that substituted for an in-person examination (Fig. 3A; the frequencies are provided in Supplementary Table S4, available at Rheumatology Advances in Practice online). Patient familiarity with telemedicine technology was rated ‘to a moderate amount’ and ‘a great deal’ as factors in the success of telemedicine by 71% (247 of 349) of participants (Fig. 3B; the frequencies are provided in Supplementary Table S5, available at Rheumatology Advances in Practice online). In addition, 40% (140 of 349) rated that the inability to build rapport reduced the success of telemedicine ‘a moderate amount’ and ‘a great deal’ (Fig. 3B). Legal concerns were rated as impeding use of telemedicine ‘occasionally’, in ‘a moderate amount’ and ‘a great deal’ by 37% (129 of 349) of respondents.
Table 2.
Technical difficulties encountered during telemedicine visits
| Variable | Summary value, n (%) |
|---|---|
| Reimbursement of telemedicine visits | |
| Both telephone and video visits | 144 (41.3) |
| Video visits only | 34 (9.7) |
| Telephone visits only | 11 (3.2) |
| Not reimbursed | 37 (10.6) |
| Not relevant in my country | 54 (15.5) |
| Do not know/do not have this information | 30 (8.6) |
| Frequency of technical difficulties in telemedicine encounters | Median: 29% (11, 40) |
| Percentages of clinicians reporting lack of patient technical support to participate in telemedicine visits | Median: 61% (40, 81) |
| Physician or patient factors contributing to technical difficulties | |
| Unable to discern | 23 (6.6) |
| Technical difficulties from both | 78 (22.4) |
| More often from the patient | 205 (58.7) |
| More often from the physician | 21 (6.0) |
| Do not experience technical difficulties | 22 (6.3) |
Fig. 3.
Perceptions of factors affecting clinical care and success of telemedicine
Exploration of survey responses by demographic groups
An exploratory analysis of responses to survey questions by participant characteristics revealed differences in reporting of technical difficulties by several characteristics (provided in Supplementary Data S2, available at Rheumatology Advances in Practice online). There was a significant difference in reported technical difficulty by age group, with people in the youngest age category on the survey reporting more technical difficulty on a scale (with 0 representing no difficulty and 100 indicating highest level of difficulty), compared with any of the older age groups [mean technical difficulty rating 35/100 (CI: 31–39) for ages 30–40 vs 28/100 (CI: 24–31) in ages 41–50 years, 27/100 (CI: 23–31) in ages 51–60 years, and 25/100 (CI: 17–32) in ≥ 61 years, P < 0.01]. Those who identified as female [mean rating of 33/100 (CI: 30–36) for females vs mean rating 26/100 (CI: 23–29) for males, P < 0.01] and non-physician clinicians [mean rating of 43/100 (CI: 30–59) vs 29/100 in physicians (CI: 26–31), P = 0.04] reported higher levels of technical difficulties.
In overall ratings of the ability to provide quality clinical care by telemedicine (categorical question with options better, same or worse quality in comparison to in-person visits), there were no significant differences by sex (P = 0.1), type of clinician (P = 0.96) or age group (P = 0.9). There were no significant differences in ratings of technical difficulty between those who worked in an academic centre and those who were in private practice (P = 0.6) or between trainees and non-trainees (P = 0.2).
Qualitative analysis
Free-text responses to prompts about barriers and enablers to telemedicine during and beyond the pandemic were provided by 190 respondents (54%) (see Supplementary Data S2, available at Rheumatology Advances in Practice online). The major factors driving telemedicine use during the pandemic were necessity for patient care when in-person care was precluded by the need for physical distancing and patient preferences. The widespread uptake of communications technology and remote working were viewed as enablers of telemedicine. A number of factors were reported to act as enablers or barriers for telemedicine during and after the pandemic, depending on their presence or absence. These were categorized as patient related, provider/organization related or wider system factors. Patient-related factors that could enable or be a barrier to telemedicine included technology competence, acceptance of telemedicine, access to a computer or smartphone, and internet access. Provider/organizational factors that could enable or be a barrier to telemedicine included availability of suitable hardware, video conferencing or scheduling software, internet access, ability to access patient laboratory and imaging studies, and staff for patient support. System factors that could enable or be a barrier to telemedicine included financial reimbursement and regulations for telemedicine. A barrier to telemedicine during and after the pandemic was lack of physical examination. Enablers to telemedicine post-pandemic included perceived increased patient acceptance and preference for telemedicine (e.g. to reduce travel); however, ongoing adequate reimbursement would be required, reflecting the increased time required for telemedicine and organizational support for telemedicine.
Discussion
In this survey of rheumatology clinicians, widespread use of telemedicine occurred internationally during the COVID-19 pandemic. Our study demonstrated that telemedicine is a useful tool to deliver care during the COVID-19 pandemic for patients with rheumatic diseases, who otherwise might not receive medical attention. Most clinicians had not used telemedicine frequently before the pandemic. A large proportion of rheumatology clinicians still continued to see patients in person during the pandemic, but reported a reduced volume of in-person patient visits. Overall, rheumatology clinicians perceived that their patients faced several barriers during telemedicine use, including lack of internet access, low familiarity with technology, and lack of equipment as main barriers to telemedicine. This finding parallels the perspectives of patients in a recent study of patient experience in telemedicine use [14].
Clinicians also experienced barriers to telemedicine use. Women, non-physician clinicians and younger respondents reported more technical difficulties. Why this occurred was unclear, especially given that younger people grew up with more forms of technology and tend to have fewer technical difficulties. This report of more technical difficulties might reflect a higher expectation for telemedicine platform performance in certain demographic groups rather than a real difference in how platforms performed technically. To our knowledge, other studies have not evaluated how provider demographics influence satisfaction with telemedicine. Understanding why this was the case provides a future research opportunity and could be helpful in informing future telemedicine implementation. In addition to patient-related factors, provider, organizational and system-wide factors were identified as influencing the success of telemedicine.
Most respondents preferred using telemedicine applications embedded into their electronic medical record system. Although the reasons for this preference were not elicited, it could be attributable to a more seamless integration with clinical workflows. Respondents also view reimbursements of telemedicine visits as an important enabling factor in ensuring long-term use of telemedicine in rheumatology practice. Hence, longevity of telemedicine use might depend on reimbursement policies regulated by government and insurance agencies. History and provision of counselling and treatment recommendations via telemedicine were undertaken satisfactorily by telemedicine. Clinicians reported feeling less able to assess a flare of rheumatic disease accurately owing to the absence of physical examination, particularly in conditions with multi-system involvement. The finding is consistent with other studies that identified the limitation of telemedicine in providing diagnostic accuracy among patients with rheumatic and musculoskeletal diseases [12, 21–23]. This suggests that rheumatic conditions with complex presentations are less easy to assess via telemedicine, potentially owing to challenges around the performance of accurate physical examination. Based on our survey findings, our group provided recommendations to guide the triaging of visits suitable for telemedicine visits in rheumatology practices in Table 3. To encourage the continued use of telemedicine in rheumatology, integration of advanced technology, such as remote auscultation of heart and lung sounds, and validation of other means of remote clinical assessment of disease activity might be needed in caring for patients with multi-organ involvement.
Table 3.
Guidance for telemedicine visits for rheumatology clinicians
| New patient visits | Follow-up patient visits |
|---|---|
| Favourable for telemedicine: | Favourable for telemedicine: |
| Laboratory abnormalities, including positive autoantibodies without symptoms | Flare of certain rheumatic and musculoskeletal diseases, such as OA, FM, inflammatory arthritis and crystalline-induced arthritis |
| Second opinion managing an existing rheumatic condition | |
| Musculoskeletal complaints | |
| Less favourable for telemedicine: | Less favourable for telemedicine: |
| New symptoms of CTDs and vasculitis | Flare of myositis or vasculitis |
Our study is novel as the first rheumatology telemedicine study with international participation and included all persons providing rheumatological care. However, the effectiveness of telemedicine use in rheumatology practices is not clear [9, 24, 25]. A report of rheumatology clinician experiences on using telemedicine during the beginning of the COVID-19 pandemic highlighted the need to incorporate pre-consultation preparations, use of consultation templates and better documentation practices in order for telemedicine to replace in-person visits [23].
A small study done within the Alaska Tribal Health System noted no significant differences in disease activity and functional status between RA patients who were evaluated via telemedicine vs in person [26]. Systematic reviews of the outcomes of telemedicine use in the management of geriatric and intensive care unit patients, however, identified few studies with discordant results and that clinical outcomes might be better than in-person evaluations [24, 27]. The lack of consensus from current published data underscores the importance of appropriately conducted evaluation of different methods of health-care delivery. Further studies are needed to assess long-term outcomes of people with rheumatic diseases cared for via telemedicine compared with in person. In the face of evolving COVID-19 variants and surges, leveraging telemedicine in certain groups of patients with rheumatic diseases might be strategic and reasonable. We also do not know the impact of telemedicine use on clinic wait times when it is safe to resume in-person visits; the continuation of care with telemedicine during COVID-19 restrictions might have reduced such wait times. On the contrary, wait times might not be impacted significantly if clinicians were unable accurately to diagnose or manage a condition via telemedicine.
There are several inherent limitations to this cross-sectional survey study. First, although our distribution strategy was effective in reaching a reasonably large number of rheumatologists in many countries globally, this strategy is likely to have sampling bias because participants who responded were likely to be members of rheumatology associations that received the survey and to have an interest in this particular topic. Second, the responses received were subject to recall bias, and with self-reported surveys, participants can provide socially favourable responses. However, our intent was to provide a snapshot of the status of telemedicine practice, with particular attention to the challenges that rheumatology clinicians experienced in using telemedicine, in order to determine ways to improve telemedicine practice in the future. Non-response bias is also possible because one-third of people did not complete the survey. There is likely to be selection bias because most respondents were likely to be fluent in English, from the USA and worked in academic centres. They also might have had better technological support and infrastructure for telemedicine visits during the time of survey. Given that 85% (298 of 349) of surveyed clinicians continued to see patients in person during the pandemic, with 72% (252 of 349) reporting that they saw fewer patients than pre-pandemic, this seemed to indicate that there was not a dire need to convert all visits to telemedicine for most participants in this survey. Therefore, their telemedicine experience will be likely to differ from clinicians who were fully using telemedicine in practice locations where in-person visits were prohibited during the pandemic. As our survey did not include patient participation, we were unable to corroborate whether the technical difficulties perceived to be originating from the patients’ end were impacted by technical limitations at the clinicians’ end, such as lack of equipment (Fig. 3B). To expand and innovate the use of telemedicine in rheumatology post-pandemic, we need better technical support for both clinicians and patients with respect to equipment availability, training in both groups, and ensuring a conducive environment with consistent internet connection [28]. We also note that perceptions of telemedicine by clinicians will be likely to fluctuate over time as public health measures and telemedicine technology evolve after the survey was administered.
In conclusion, this study of rheumatology clinicians with appreciable global reach found that rheumatology clinicians commonly adopted telemedicine for the first time in the COVID-19 pandemic, and they were able to deliver quality clinical care in certain clinical scenarios, but not all. Concrete barriers to telemedicine identified by the survey are targets for innovation and improvement in future efforts. Additionally, the areas of clinical practice where telemedicine has been deemed adequate for patient management can be used further to define the appropriate scope of telemedicine in rheumatological care. These might include adequate training in and ongoing support in technical aspects of telemedicine for both patients and providers, embedding of telemedicine processes in health-provider software and workflows, appropriate processes of patient triage to ensure clinical suitability for telemedicine, and adequate financial reimbursement.
Supplementary Material
Acknowledgements
All authors met the criteria of authorship as outlined in the ICMJE and approved this manuscript for submission. Specific contributions were as follows: conceptualization: E.C., L.C. and B.H.; methodology: E.C., L.C., R.G. and B.H.; original survey design: E.C., L.C. and B.H.; all authors were involved with providing comments and further development of survey; data curation and analysis: E.C., L.C. and M.P.; writing original draft: E.C. and L.C.; writing, reviewing, editing: E.C., L.C., R.G. and Z.S.W. All authors were involved in revision and review of the original draft.
Funding: No specific funding was received from any bodies in the public, commercial or not-for-profit sectors to carry out the work described in this article.
Disclosure statement: R.G. reports personal fees from AbbVie New Zealand, Cornerstones, Janssen New Zealand, and personal fees and non-financial support Pfizer New Zealand, (all <$10,000) outside the submitted work. P.M.M. has received consulting/speaker’s fees from Abbvie, BMS, Celgene, Eli Lilly, Galapagos, Janssen, MSD, Novartis, Pfizer, Roche and UCB, all unrelated to this study. P.M.M. is supported by the National Institute for Health Research (NIHR) University College London Hospitals (UCLH) Biomedical Research Centre (BRC). N.S. reports research funding support from Rheumatology Research Foundation and the American Heart Association. E.H. reports research funding from NIH/Fogarty International Center K01TW009995 and Rheumatology Research Foundation. J.a.L. reports receiving consultancy and/or speaker fees and/or travel reimbursements unrelated to the topic covered in this publication: Abbvie, BMS, EUSA Pharma, Janssen-Cilag, Gilead, Lilly, Mylan, Novartis, Roche/Chugai, Sanofi UCB. He also has scientific support not related to the topic covered in this publication from Abbott, Gilead, Novartis and federal state Baden-Württemberg. P.C.R. reports personal fees from Abbvie, Atom Biosciences, Eli Lilly, Gilead, Janssen, Novartis, UCB, Roche, Pfizer; meeting attendance support from BMS, Eli Lilly, Pfizer and UCB Pharma and grant funding from Janssen, Novartis, Pfizer and UCB Pharma. M.I.D. has received research support from Amgen, Horizon, Genentech, Radius, Boehringer Ingelheim, Pfizer for unrelated work. M.I.D. has received consulting fees from Amgen, Abbvie, Novartis. S.-A.Y. reports research grant funding from National Institute for Health Research (NIHR) University College London Hospitals Biomedical Research Centre/UCLH Charities, Royal College of Physicians, Rosetrees Trust, Versus Arthritis, all unrelated to this work. Z.S.W. reports grant support from BMS, Sanofi/Principia; consulting fees from Zena BioPharma, Sanofi/Principia, MedPace, Viela Bio. L.C.C. reports grant and consulting funding from Bristol-Myers Squibb. L.C.C. also reports consulting fees with Mallinckrodt. The remaining authors have declared no conflicts of interest.
Disclaimer: The views expressed here are those of the authors and the participating members of the COVID-19 Global Rheumatology Alliance and do not necessarily represent the views of the American College of Rheumatology (ACR), the European Alliance of Associations for Rheumatology (EULAR), the (UK) National Health Service (NHS), the National Institute for Health Research (NIHR) or the (UK) Department of Health, or any other organization.
Data availability statement
The data underlying this article are available in the article and in its online supplementary material.
Supplementary data
Supplementary data are available at Rheumatology Advances in Practice online.
References
- 1. Rabuñal R, Suarez-Gil R, Golpe R. et al. Usefulness of a telemedicine tool TELEA in the management of the COVID-19 pandemic. Telemed e-Health 2020; 26:1332–5. [DOI] [PubMed] [Google Scholar]
- 2. Peine A, Paffenholz P, Martin L. et al. Telemedicine in Germany during the COVID-19 pandemic: multi-professional national survey. J Med Internet Res 2020;22:e19745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mahajan V, Singh T, Azad C.. Using telemedicine during the COVID-19 pandemic. Indian Pediatr 2020;57:652–7. [PubMed] [Google Scholar]
- 4. North S. Telemedicine in the time of COVID and beyond. J Adolesc Health 2020;67:145–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. El Miedany Y. E-rheumatology: are we ready? Clin Rheumatol 2015;34:831–7. [DOI] [PubMed] [Google Scholar]
- 6. Jong M, Kraishi M.. A comparative study on the utility of telehealth in the provision of rheumatology services to rural and northern communities. Int J Circumpolar Health 2004;63:415–21. [DOI] [PubMed] [Google Scholar]
- 7. Roberts LJ, Lamont EG, Lim I, Sabesan S, Barrett C.. Telerheumatology: an idea whose time has come. Intern Med J 2012;42:1072–8. [DOI] [PubMed] [Google Scholar]
- 8. Lockwood MM, Wallwork RS, Lima K. et al. Telemedicine in adult rheumatology: in practice and in training. Arthritis Care Res (Hoboken) 2021;0:1–7. [DOI] [PubMed] [Google Scholar]
- 9. McDougall JA, Ferucci ED, Glover J, Fraenkel L.. Telerheumatology: a systematic review. Arthritis Care Res (Hoboken) 2017;69:1546–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. de Thurah A, Stengaard-Pedersen K, Axelsen M. et al. Tele-health followup strategy for tight control of disease activity in rheumatoid arthritis: results of a randomized controlled trial. Arthritis Care Res (Hoboken) 2018;70:353–60. [DOI] [PubMed] [Google Scholar]
- 11. Muehlensiepen F, Knitza J, Marquardt W. et al. Acceptance of telerheumatology by rheumatologists and general practitioners in Germany: nationwide cross-sectional survey study. J Med Internet Res 2021;23:e23742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Matsumoto RA, Barton JL.. Telerheumatology: before, during, and after a global pandemic. Curr Opin Rheumatol 2021;33:262–9. [DOI] [PubMed] [Google Scholar]
- 13. Hollander JE, Carr BG.. Virtually perfect? Telemedicine for Covid-19. N Engl J Med 2020; 382:1679–81. [DOI] [PubMed] [Google Scholar]
- 14. Webster P. Virtual health care in the era of COVID-19. Lancet 2020;395:1180–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kimball S, Rattner N, Kim Constantino A. ‘We’re heartbroken. We’re overwhelmed’ — U.S. hospitals grapple with delta outbreak as omicron takes root. CNBC. https://www.cnbc.com/2021/12/15/covid-delta-drives-surge-of-us-infections-hospitalizations-amid-omicron-fears.html. Updated 2021 (13 January 2022, date last accessed).
- 16. Gov’t gears up for optimizing telemedicine services amid spike in omicron cases. Gov’t Gears Up for Optimizing Telemedicine Services Amid Spike in Omicron Cases Web site. Office of Assistant to Deputy Cabinet Secretary for State Documents & Translation. https://setkab.go.id/en/govt-gears-up-for-optimizing-telemedicine-services-amid-spike-in-omicron-cases/. Published 12 January 2022. Updated 2022 (13 January 2022, date last accessed).
- 17. Alsaffar H, Almamari W, Al Futaisi A.. Telemedicine in the era of COVID-19 and beyond: a new horizon. Sultan Qaboos Univ Med J 2020; 20:e277–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yen YF, Tsai YF, Su VY. et al. Use and cost-effectiveness of a telehealth service at a centralized COVID-19 quarantine center in Taiwan: cohort study. J Med Internet Res 2020;22:e22703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Matsumoto RA, England BR, Mastarone G. et al. Rheumatology clinicians' perceptions of telerheumatology within the Veterans Health Administration: a national survey study. Mil Med 2020;185:e2082–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bos WH, van Tubergen A, Vonkeman HE.. Telemedicine for patients with rheumatic and musculoskeletal diseases during the COVID-19 pandemic; a positive experience in the Netherlands. Rheumatol Int 2021;41:565–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bateman J, Cleaton N.. Managing patients using telerheumatology: lessons from a pandemic. Best Pract Res Clin Rheumatol 2021;35:101662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hall AG, Kim DH, Rainey C, Singh JA.. Telemedicine including video-based visits in rheumatology in COVID-19 pandemic: not yet ideal. J Clin Rheumatol 2022;28:e292–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chan A, Suarez A, Kitchen J, Bradlow A.. Teleclinics in rheumatology introduced during the first lockdown phase of the COVID-19 pandemic of 2020. Future Healthc J 2021;8:e27–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Batsis JA, DiMilia PR, Seo LM. et al. Effectiveness of ambulatory telemedicine care in older adults: a systematic review. J Am Geriatr Soc 2019;67:1737–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Solomon DH, Rudin RS.. Digital health technologies: opportunities and challenges in rheumatology. Nat Rev Rheumatol 2020;16:525–35. [DOI] [PubMed] [Google Scholar]
- 26. Ferucci ED, Holck P, Day GM, Choromanski TL, Freeman SL.. Factors associated with use of telemedicine for follow-up of rheumatoid arthritis. Arthritis Care Res (Hoboken) 2020;72(10):1404–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chen J, Sun D, Yang W. et al. Clinical and economic outcomes of telemedicine programs in the intensive care unit: a systematic review and meta-analysis. J Intensive Care Med 2018;33:383–93. [DOI] [PubMed] [Google Scholar]
- 28. Sloan M, Lever E, Harwood R. et al. Telemedicine in rheumatology: a mixed methods study exploring acceptability, preferences and experiences among patients and clinicians. Rheumatology (Oxford) 2021. doi: 10.1093/rheumatology/keab796. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.