Abstract
Background
Perinatal cannabis use is increasing, and clinician counselling is an important aspect of reducing the potential harm of cannabis use during pregnancy and lactation. To understand current counselling practices, we conducted a systematic review and integrative mixed-methods synthesis to determine “how do perinatal clinicians respond to pregnant and lactating patients who use cannabis?”
Methods
We searched 6 databases up until 2021-05-31. Eligible studies described the attitudes, perceptions, or beliefs of perinatal clinician about cannabis use during pregnancy or lactation. Eligible clinicians were those whose practice particularly focusses on pregnant and postpartum patients. The search was not limited by study design, geography, or year. We used a convergent integrative analysis method to extract relevant findings for inductive analysis.
Results
Thirteen studies were included; describing perspectives of 1,366 clinicians in 4 countries. We found no unified approach to screening and counselling. Clinicians often cited insufficient evidence around the effects of perinatal cannabis use and lacked confidence in counselling about use. At times, this meant clinicians did not address cannabis use with patients. Most counselled for cessation and there was little recognition of the varied reasons that patients might use cannabis, and an over-reliance on counselling focussed on the legal implications of use.
Conclusion
Current approaches to responding to cannabis use might result in inadequate counselling. Counselling may be improved through increased education and training, which would facilitate conversations to mitigate the potential harm of perinatal cannabis use while recognizing the benefits patients perceive.
Keywords: cannabis, counselling, delivery of health care, lactation, perception, pregnancy
Key Messages.
Rates of cannabis use during pregnancy and lactation continue to increase.
We conducted a systematic review to determine current counselling approaches.
There was no unified counselling approach due lacking knowledge and confidence.
Counselling may be improved with more training to support harm reduction.
Introduction
Cannabis use has increased over time in many populations, particularly when recreational cannabis is legalized or decriminalized.1–3 Cannabis use among pregnant and lactating people has shown a corresponding increase.4–6 Rates of cannabis use during pregnancy reported in current literature vary greatly (2%–36%)5,6 and actual use is often under-reported or under-detected.7 Cannabis use among lactating people is likely higher, as individuals who stopped during pregnancy may reinitiate postpartum.8,9
Addressing cannabis use during pregnancy and lactation is a complex counselling issue for perinatal clinicians, or health care providers whose clinical practice focusses on care for pregnant and/or postpartum patients. These clinicians may struggle with discussing risk and safety when evidence about the harm of cannabis use during pregnancy is equivocal, and in some instances, contradictory.10–13 Some studies show a decrease in birth weight with cannabis use,12,14,15 while others report no association.10,11 There is some association between substance use (cannabis and other illicit drugs) and pregnancy loss, but the impact of cannabis remains unclear.11 There are also inconsistencies as to whether cannabis use poses a risk for preterm delivery,11,12,15–17 or an increased risk of neonatal intensive care unit admission.11,12,16 Some studies of cognitive function suggest that prenatal exposure to cannabis may result in problems with executive functioning, emotion, and behaviour in early childhood17,18 but this evidence base also has limitations.19 Literature on the potential for harm from cannabis exposure during lactation is also conflicting, with some studies reporting decreased infant motor development while others report no effect.10,20,21
While it may be reasonable to follow the precautionary principle and counsel cessation for recreational users, there is evidence that pregnant and lactating people are using cannabis for a wide variety of therapeutic reasons.4,22–27 When a pregnant or lactating patient is using cannabis to provide relief from preexisting conditions (e.g. chronic pain, mental illness, sleep quality, and seizure control4,22–26), pregnancy-related symptoms (e.g. vomiting, nausea, pain, and fatigue24,25,28) or to decrease use of more harmful substances,29 the counselling encounter becomes more complex. When cannabis is being used for these reasons, clinicians may wish to help patients take a harm reduction approach,10 but with cannabis there is no clinical evidence to support risk mitigation through type, timing, or dose.30
A trusting, supportive relationship between patients and clinicians is an essential foundation for ensuring high quality perinatal care.31 Counselling about cannabis should seek to build the patient–clinician relationship through the provision of information and nonjudgemental support. To inform clinicians in their counselling approach, it is important to understand the current range of clinician responses to cannabis use, what influences these responses, and any potential gaps. We therefore conducted a systematic review to determine “how do perinatal clinicians respond to pregnant and lactating patients who use cannabis?”
Methods
We conducted a mixed-methods systematic review using a convergent integrated approach to synthesis and integration,32 following the Joanna Briggs Institute guidance.32,33 This review was conducted according to the PRISMA guidelines34 in conjunction with a separate review on the perspectives of pregnant and lactating people about cannabis use and is registered with PROSPERO (CRD42020180038).
Screening and sources
An initial search of published literature was conducted by a medical librarian on 1 April 2020, using the following databases: MEDLINE (via Ovid), APA PsycINFO (via Ovid), Cumulative Index to Nursing and Allied Health Literature (CINAHL, via EBSCOhost), Social Science Citation Index (SSCI, via Web of Science) Social Work Abstracts (via EBSCOhost), ProQuest Sociology Collection (including Sociological Abstracts). The final search update was completed on 31 May 2021. Grey literature searching was limited to academic theses and conducted within the ProQuest Dissertation Abstracts database.
The search strategy (Supplementary Material 1) consisted of both controlled vocabulary (e.g. Medical Subject Headings) and keywords, and was peer reviewed using PRESS (Peer Review of Electronic Search Strategies) guidelines. The search was limited to English language publications; however, no date limits, no geographic limits, and no study design filters were applied. A hand search of relevant journals was also conducted. See Supplementary Material 2 for eligibility criteria.
Two reviewers (of JP, ST, and AP) independently screened each citation to determine eligibility. When it was impossible to reach consensus on inclusion or exclusion via the title and abstract, full text articles were reviewed. Disagreements between reviewers were resolved through discussion with the senior author (MV) until consensus was reached.
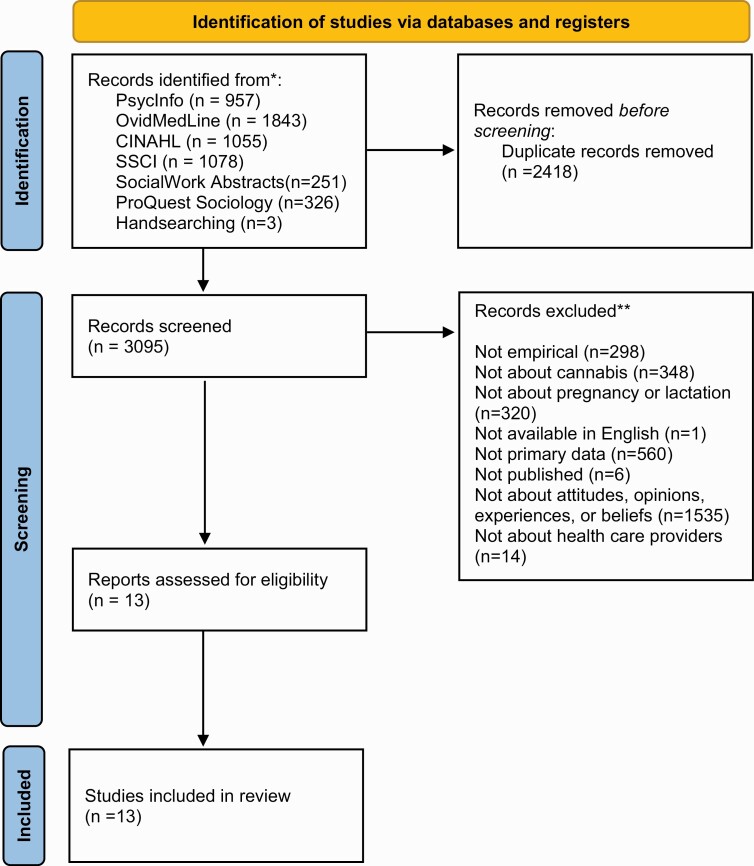
After identifying eligible articles, we engaged in citation chaining, searching the reference lists of included articles as well as those who cited our included articles. After determining our final list of included articles, we engaged 2 topic experts to review the list and to suggest additional publications which we may have missed. See Fig. 1 for PRISMA diagram.
Fig. 1.
PRISMA flow diagram of systematic review of perinatal clinicians’ responses to pregnant and lactating patients who use cannabis.
Critical appraisal
We critically appraised included articles using the Mixed Methods Appraisal Tool (MMAT).35 The MMAT was designed to appraise studies with diverse designs and is validated and reliability tested.35,36 Articles were appraised independently by 2 reviewers (JP, MV, ED, and a research assistant) who rated each aspect of the study as “yes,” “no,” or “can’t tell.” Disagreements were resolved through discussion (results in Table 1). All eligible studies were included, as long as they presented data in evidence of their conclusions.35
Table 1.
Critical appraisal results—quality evaluation of included studies using the Mixed Methods Appraisal Tool (2018 version).
| Qualitative | Quantitative descriptive | Mixed methods | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1.1 | 1.2 | 1.3 | 1.4 | 1.5 | 2.1 | 2.2 | 2.3 | 2.4 | 2.5 | 3.1 | 3.2 | 3.3 | 3.4 | 3.5 | |
| Bergeria37 | Y | C | Y | Y | N | ||||||||||
| Brooks38 | Y | N | Y | C | Y | ||||||||||
| Geraghty39 | Y | Y | Y | Y | Y | Y | N | Y | C | Y | Y | Y | Y | Y | C |
| Gérardin40 | Y | Y | N | Y | Y | ||||||||||
| Gotham41 | Y | Y | Y | N | N | ||||||||||
| Gray42 | Y | Y | Y | Y | Y | C | Y | Y | Y | N | Y | Y | Y | Y | C |
| Herzig43 | Y | Y | Y | Y | Y | ||||||||||
| Holland44 | Y | Y | Y | Y | Y | ||||||||||
| Holland45 | C | N | Y | Y | Y | ||||||||||
| Northrup46 | Y | Y | Y | N | Y | ||||||||||
| Petersen Williams47 | Y | Y | Y | Y | Y | ||||||||||
| Salisbury48 | Y | Y | Y | N | N | ||||||||||
| Young-Wolff49 | Y | Y | Y | Y | Y | Y | C | Y | N | Y | N | C | Y | Y | C |
Y = yes; N = No; C = Can’t Tell. Detailed descriptions of each criterion are published elsewhere.
Data extraction and collation
We obtained study characteristics and results relevant to the research question from each included study and extracted this descriptive data into a standardized electronic form. There are a variety of analytic approaches used in integrative reviews of studies.50,51 We used Sandelowski’s method of “qualitizing data,” 51 which consists of identifying and extracting findings and subsequently rewriting each finding into a declarative statement that can stand alone. These declarative statements were constructed in a way such that the findings were integrated with study information that was determined to be most relevant to characterizing those findings. Statements were composed by 1 reviewer and independently verified by a second, with disagreements resolved through discussion, and consultation with a third reviewer where necessary.
Data analysis
The results from all included studies were analyzed using the convergent integrated approach in Hong’s typology.32 The data from the “qualitized” declarative statements were treated as qualitative data and analysed via a staged comparative coding strategy similar to that in Grounded Theory.52 This analytic approach involves the comparison of research findings across studies, categories, and analysts including the identification of negative or discrepant findings. Analytic comparisons included attention to the drug of focus (cannabis only or general substance use), whether the patient population was pregnant, lactating or both, clinicians’ professional designations, time of publication, and jurisdictional legality of cannabis. Analysis was led by JP, MV, AP, and ST. Analytic interpretations were negotiated during regular meetings with the whole research team.
Results
We searched 6 databases and screened 3,095 records (see PRISMA diagram in Fig. 1). Thirteen eligible papers were included in this review (Table 2). As recommended for MMAT quality appraisal, rather than provide a global judgment of quality, the ratings for each criterion are provided in Table 1 for the purposes of evaluating the strength of the conclusions of this synthesis.35
Table 2.
Summary of included studies in systematic review of clinician responses to perinatal cannabis use (no date—05/31/2021).
| Lead author | Date (dates of data collection) | Country (location) | Legal statusa (recreational) | Legal statusa (medical) | Methodology | Focus of paper | N | Study purpose/objective |
|---|---|---|---|---|---|---|---|---|
| Bergeria37 | 2015 (April 2014) | United States of America (Vermont) | Illegal | Legal | Quantitative | Lactation | 74 | To identify, (i) what recommendations lactation professionals are making to clients who use marijuana and breastfeed, and (ii) what professional guidelines, statements, or other sources lactation professionals cite as the basis for their recommendations. |
| Brooks38 | 2017 (2015) | United States of America (Colorado) | Legal | Legal | Quantitative | Pregnancy and lactation | 114 | To survey Colorado-based providers to determine: (i) their knowledge of current state laws, and marijuana health and safety risks; (ii) clinical practices surrounding marijuana assessment and patient communication; (iii) needs and preferences for additional training opportunities; and (iv) the impact of educational resources and outreach to change provider behaviour. |
| Geraghty39 | 2019 (N/A) | Australia (Perth) | Illegal | Legal | Mixed methods | Pregnancy and lactation | 14 | To identify midwives’ attitudes towards women using substances during pregnancy, which will inform the development of an integrated care pathway for the provision of optimal care. |
| Gérardin40 | 2011 (N/A) | France (Loire-Atlantique) | Illegal | Illegal | Quantitative | Pregnancy | 204 | To survey health care professionals in order to evaluate practices of detection and care for pregnant women who use cannabis. |
| Gotham41 | 2019 (N/A) | United States of America | b | b | Qualitative | Pregnancy | 34 | To use focus groups of family planning providers to explore barriers and facilitators to “screening, brief intervention, and referral to treatment” (SBIRT) for substance use. |
| Gray42 | 2017 (2015) | United States of America (Michigan) | Illegal | Legal | Mixed methods | Pregnancy | 12 | To evaluate, among pregnant women and prenatal care providers, the acceptability of an electronic brief intervention and text messaging plan for marijuana use in pregnancy. |
| Herzig43 | 2006 (2003–2004) | United States of America (San Francisco) | Illegal | Legal | Qualitative | Pregnancy | 49 | To explore prenatal care providers’ methods for addressing 4 behavioural risks in their pregnant patients: alcohol use, smoking, drug use, and domestic violence. |
| Holland44 | 2016 (2011–2015) | United States of America (Pennsylvania) | Illegal | Illegal | Qualitative | Pregnancy | 51 | To describe obstetric provider attitudes, beliefs, approaches, concerns, and needs about addressing perinatal marijuana use with their pregnant patients. |
| Holland45 | 2016 (2011–2014) | United States of America (Pennsylvania) | Illegal | Illegal | Mixed methods | Pregnancy | 47 | To describe obstetric health care providers’ responses and counselling approaches to patients’ disclosures of marijuana use during first prenatal visits. |
| Northrup46 | 2017 (February 2016–March 2016) | United States of America | b | b | Quantitative | Pregnancy | 417 | To assess and describe perceptions of prevalence and safety/risk, as well as current screening practices related to cigarettes, second-hand smoke exposure, marijuana, and synthetic marijuana, e-cigarettes, nicotine- replacement therapy, and smoking-cessation medications during pregnancy among prenatal care providers giving obstetric care within academic settings. |
| Petersen Williams47 | 2015 (August 2011– September 2011) | South Africa (Cape Town) | Illegal | Illegal | Qualitative | Pregnancy | 43 | To explore health care workers’ attitudes and perceptions about screening, brief intervention, and referral to treatment among substance-using women presenting for antenatal care. |
| Salisbury48 | 2017 (April 2016– June 2016) | United States of America (Washington) | Legal | Legal | Qualitative | Lactation | 30 | To examine medical provider perceptions of breastfeeding women who use recreational marijuana and identify common themes in provider responses. |
| Young-Wolff49 | 2020 (March 2011– January 2017) | United States of America | b | b | Mixed methods | Pregnancy and lactation | 277 | To analyze publicly posted questions on perinatal cannabis use on an online anonymous digital health platform and licensed US health care provider responses. |
| 1,366 |
aLegal status at time of data collection or date of journal submission/publication.
bMultiple jurisdictions—legal status unclear.
These studies represent the perspectives of 1,366 health care clinicians, mainly general practitioners/family physicians and obstetrician–gynaecologists (Table 3). Included studies were conducted in the United States,37,38,41–46,48,49 as well as France,40 Australia,39 and South Africa.47 At the time of study data collection or publication, recreational cannabis was only legal in 2 jurisdictions in the United States (Colorado and Washington).38,48 Medical cannabis was legal in Australia39 and in 6 jurisdictions within the United States.37,38,42,43,48 State-level cannabis legality is complicated by ongoing federal criminalization. The legal status of cannabis was unspecified for 3 studies41,46,49 where data collection occurred across multiple unidentified US jurisdictions (see Table 2). Cannabis was full illegal in South Africa47 and France.40 No study specified whether cannabis use was for medical or recreational purposes—although 1 study did mention considerations around providing patients with medical cannabis authorizations.48 Five studies were conducted with a qualitative methodology, 4 with quantitative and 3 with mixed methods (Table 2 and Supplementary Material 3). Eight studies focussed on cannabis or substance use in pregnancy, 2 focussed on lactation, and 3 focussed on both (Table 2). Nine studies specifically discussed cannabis, while the remaining 4 described cannabis as one of multiple substances of interest.39,41,43,47 Our analysis, depicted in Fig. 2, describes current evidence on how perinatal clinicians were observed or self-reported becoming aware that their pregnant and lactating patients were using cannabis, and how they responded to this awareness.
Table 3.
Type and number of participants.
| Type of participants | N |
|---|---|
| Family Planning Cliniciansa | 34 |
| OB-GYN (including obstetricians, gynaecologists, faculty OB-GYN, OB-GYN resident) | 219 |
| Midwives | 95 |
| Nurses (including RN, RPN, nurse midwife, nurses with a Bachelor of Nursing, mental health nurse) | 126 |
| Physicians (not otherwise specified) | 13 |
| Paediatrician | 4 |
| Lactation Specialists (breastfeeding medicine specialists and lactation consultants) | 36 |
| HIV counsellor | 8 |
| Physician Assistant | 5 |
| General Practitioners/Family Physicians | 623 |
| Public health/WIC personnel | 11 |
| Nutritionist | 5 |
| Psychiatrists/Psychologists | 63 |
| Other (medical assistants, dietitians/nutrition counsellors, counsellors, social workers, reception staff, La Leche League affiliate, unknown) | 145 |
| 1,387 |
Fig. 2.
Depiction of how clinician awareness of patient perinatal cannabis use can impact response type.
Awareness of cannabis use
Clinicians became aware of or screened for, patient cannabis use in a variety of ways that included previsit questionnaires,38,46 structured or informal discussions between the patient and clinician (where the clinician asked about use or the patient disclosed use),38,40,44,46 and biochemical screening as part of routine blood testing.46 When asking patients about their consumption of substances, some American clinicians described needing to ask directly about cannabis use, as patients did not always include it when talking about general substance use.44 Clinicians reasoned this may be because patients do not view cannabis as similarly harmful to other drugs.44 French clinicians did not always attempt to identify specific substances pregnant patients were consuming, considering all illicit drug use to be equivalently harmful.40
Clinicians in multiple studies expressed a lack of confidence about how to respond after becoming aware a patient was using cannabis.38,40,43,45 A lack of research evidence and knowledge about perinatal cannabis use also made it a challenge to fit cannabis into standard assessment or counselling procedures.43 This lack of knowledge and confidence often contributed to clinician avoidance of screening for or asking about cannabis use38,40 and some clinicians waited for patients to spontaneously disclose their use.45 This finding was different in studies where cannabis was considered alongside other substances; clinicians were more likely to express comfort and confidence identifying and counselling pregnant patients about general substance use than cannabis use specifically.41,43,47
Response to cannabis use
Comparative analysis identified common factors that influenced clinicians’ responses to patient cannabis use—including counselling approaches.
Understanding of risks and benefits
Perceptions that cannabis posed a risk to fetal health were cited as influencing clinicians’ decisions to counsel about ceasing cannabis use. Specific risks mentioned by clinicians were the impacts of tetrahydrocannabinol (THC) (a component of cannabis) on cognitive development,37,38,48 the addictive potential of cannabis,48 and the potential negative impact of cannabis on a patient’s parenting abilities.37,48 In several of the included studies, clinicians described cannabis use as unsafe but did not describe specific risks.40,42,44,46,49
The 2 studies that focussed only on cannabis use during lactation noted that clinicians weighed the benefits of breastfeeding against the risks of cannabis use when considering how to counsel.37,48 One article discussed clinician hesitancy in providing medical authorization of cannabis for lactating patients who desired relief from migraines, seizures, chronic pain, or chemotherapy.48 Benefits of cannabis use were seldom mentioned in other studies. One study mentioned the use of cannabis for relief of pregnancy-associated nausea, but beyond this mention there was no discussion of potential therapeutic reasons for which patients may wish to use cannabis during pregnancy or lactation.43
Confidence in knowledge and skills
In some studies, clinicians expressed a lack of knowledge about the risks of cannabis use during pregnancy and lactation.40,43,44,48 This lack of knowledge contributed to reluctance counselling about anything beyond the legal risks of cannabis use.44 In contrast, clinicians who felt more informed about the evidence that exists about the risks of cannabis use during pregnancy were more likely to screen for use and engage in discussions with their patients and make additional referrals for consultation.40 This link between knowledge and comfort counselling was made explicit by clinicians in 1 study who emphasized the need for more education and resources to increase their comfort in counselling.38 Clinicians based their knowledge and recommendations on information from colleagues,40 textbooks, and professional college policy statements or personal experiences.37 They expressed a desire for additional information about the health risks of cannabis38 and strategies for counselling patients.40
Professional designation
Professional designation affected the way that clinicians responded to the issue of cannabis use in pregnancy, and a number of studies offered comparative insights into interprofessional variation on counselling and consultation. In France, compared with gynaecologists and general practitioners, midwives and obstetricians see a higher volume of pregnant patients and so encounter more pregnant patients using cannabis. This additional clinical exposure resulted in midwives and obstetricians describing more difficulties in supporting these patients, but also feeling more informed than colleagues with less clinical exposure.40 This finding of clinical exposure increasing both comfort and identification was echoed with different groups of providers in the United States.45 One study from Washington found that most family physicians, breastfeeding medicine specialists, and some paediatricians were less likely to authorize medical cannabis to a breastfeeding mother than obstetricians and midwives.48 It is difficult to draw conclusive comparisons given the differences in national and clinical context, but this evidence suggests that clinicians who specialize in perinatal care and have higher levels of clinical exposure to pregnant and lactating patients who use cannabis are more likely to address cannabis use during pregnancy and breastfeeding than generalist clinicians.
Cannabis considered alone or as one of a number of substances
Studies which included cannabis as one of multiple substances described clinicians as more likely to encourage cessation than studies that addressed clinician responses to cannabis only. Clinicians in 1 US state expressed that with the limited time they have during a patient’s first perinatal appointment, they do not prioritize discussing cannabis but will focus on other substances.44 Patients who disclosed using both cannabis and tobacco often only received tobacco counselling from clinicians,45 and counselling about cannabis smoking was notably tied with tobacco smoking in 1 study.46
Studies which included cannabis as one of multiple substances used in pregnancy were more likely to offer suggestions for improvements to current systems to better address substance use. Comparatively, studies which considered cannabis alone focussed more on clinician experiences, describing clinician perceptions of a lack of knowledge, training and, consequently, lower confidence in counselling.
Counselling approaches
With respect to counselling specifically for cannabis use, most studies described clinicians focussing on encouraging cessation of cannabis use during pregnancy or lactation—with the implication or direct statement that use was harmful.37,38,40,42,44–46,48,49 In most of these studies, however, there were clinicians who chose to respond in other ways,37,40,44,48,49 did not respond at all when patients disclosed use,45 or expressed uncertainty about how to respond to cannabis use.40,43,44 When cannabis was studied alongside other substances, there was a clearer focus on counselling to encourage cessation of substance use39,41,43,47 than when cannabis was considered alone.37,38,40,42,44–46,48,49
When clinicians counselled with the goal of encouraging pregnant and lactating patients to cease cannabis use,42,44–46,48,49 they most frequently reported or were observed doing so by sharing the medical risks of use.40,45 Two studies noted that in these counselling sessions many clinicians used a “punitive counselling style” 45—threatening involvement of child protective services,44,45 which study authors identified as the only leverage clinicians felt they had to motivate cessation, given their limited knowledge about medical risks of perinatal use.
Other clinicians took an empathetic or encouraging approach to counselling when trying to get pregnant patients to stop using cannabis.42,45,49 Some described making case-by-case decisions on their approaches to counselling their lactating patients—considering the individuality of the patient’s situation48 such as lifestyle factors, the severity of cannabis use, and parenting situation.37,48 While the studies addressing responses to “substance use” more generally identified a common approach or consensus about how to respond to disclosures about substance use,41,43,47 the studies examining cannabis only did not identify a consensus or preference for how to respond to awareness of cannabis use.37,38,40,42,44–46,48,49
Discussion
This review highlights the relationship between clinician comfort regarding counselling about cannabis use during pregnancy or lactation and clinicians’ likelihood of eliciting and responding to information about cannabis use. Across multiple jurisdictions and professional designations, there were no standardized approaches for screening for cannabis use. Clinicians acknowledged the underdevelopment of the clinical evidence about the potential harms of perinatal cannabis use, and strategies to mitigate those risks. Accordingly, some clinicians adopted a variety of screening methods and counselling approaches based on past experience and advice from their professional networks or colleagues. Therefore, we suspect that newer, less experienced, and less connected clinicians may encounter more challenges when attempting to determine how to screen for and address cannabis use. While these studies indicate the need for more clinician education, they also point to a greater need for clear research evidence to inform that education and the resulting clinical strategies.
Also noteworthy was a lack of discussion about the reasons why pregnant and lactating people might use cannabis, perhaps related to the grouping of cannabis with other substances that do not have known therapeutic benefits.53,54 Medical authorization and counselling about medical cannabis was not mentioned in most papers, and was described as an area of confusion for clinicians.30 Given that many pregnant and lactating people consume cannabis to treat specific conditions and symptoms including some related to pregnancy,55 this is an important area to address with patients in order to provide information, guidance, and support. Clinical practice guidelines in multiple jurisdictions are clear that there is no evidence of a safe level for cannabis consumption in pregnancy or lactation, and cessation is recommended.10,56–58 However, these statements do not provide adequate guidance to assist clinicians in nuanced counselling with patients who perceive therapeutic benefits from cannabis. Where pregnant or lactating people identify specific reasons for using cannabis, clinicians should seek to assist by identifying alternative solutions including acceptable substitutions.59 Patients who use cannabis therapeutically will also require guidance on when and how to restart their use after pregnancy or lactation ends.
We also found that counselling approaches varied considerably, with an over-reliance on what Holland et al. title a “punitive style” 45 of counselling that emphasized the potential sociolegal consequences of cannabis use. Clinicians noted confusion about how to counsel about the issue, indicating the need for guidance. Recent literature on counselling for cannabis use during pregnancy and lactation suggests that a nonpunitive, harm reduction approach might be more suitable.10,53,60–62 A harm reduction approach typically entails strategies and perspectives directed at reducing the negative consequences of substance use, while respecting the autonomy of the person using substances and the complexity of the phenomenon of substance use.63 Likely due to a focus on abstinence,64 there is not much research describing harm reduction approaches employed with pregnant or lactating patients. Past studies have focussed on harm reduction approaches for pregnant and postpartum persons using tobacco,65–67 cocaine,68 and methamphetamine.64 Adopting from the strategies employed in these studies, a harm reduction approach for managing cannabis use during pregnancy or lactation would include establishing perinatal care environments and interactions that are supportive, judgement-free, and conducive to open and honest conversations between clinicians and patients about cannabis use.64 The counselling foci should be to improve birth and neonatal outcomes; provide education to not only patients but all clinicians and staff involved on how to counsel for cannabis use in a judgement-free way; provide educational resources to the community for those looking for more information on the potential impact of cannabis use during pregnancy and lactation; suggest alternative therapies for patients using cannabis therapeutically (for existing and pregnancy-related symptoms), and be involved in, or promote further research on the effects of cannabis to advance the current evidence base.64,67
Areas for future research
The results of this study point to the need for more clinical research on the risks of cannabis use during pregnancy and lactation, and strategies for mitigating those harms. In the domain of counselling, future research might include feasibility and pilot tests of cannabis harm reduction programmes and strategies for clinician behaviour change as they were suggested above. Clinical guidelines to inform patient-centred approaches on screening and counselling for cannabis use should be developed or modified to acknowledge the varied reasons that patients might be using cannabis during pregnancy or breastfeeding10 and the implications these reasons might have for cessation.
Strengths and limitations
To our knowledge, this is the first systematic review to describe perinatal clinicians’ approaches to counselling for cannabis use. Our search approach was extensive—and including citation list searching and hand searching, resulted in 13 eligible studies. These studies were also a mix of studies focussed on pregnancy and those on lactation. This analysis is limited, however, by the fact that we only included studies published in English and only included published empirical studies, potentially missing valuable research published in other languages, nonempirical reports of experience and opinion, and important content in the grey literature. The literature retrieved comes primarily from industrialized, high-income countries and transferability to other clinical contexts may be limited.
Conclusion
This systematic review and synthesis of 13 studies described clinician responses to cannabis use by pregnant or lactating patients. Findings indicated that many clinicians felt uncertain about their knowledge and skills in addressing cannabis use with patients and this uncertainty acted as a barrier to eliciting information about cannabis use. The lack of clear research evidence on safety, adequate substitutions, and strategies to mitigate harm by changing the timing, dose, type, or amount contributed to clinician discomfort in counselling. Amongst the included papers, there were no unified approaches to screening and counselling. Clinicians who did counsel focussed on encouraging cannabis cessation but there was little discussion of the varied reasons a patient might use cannabis during pregnancy or lactation. These findings highlighted the opportunity for clinicians to change their counselling to an approach that reduces the potential harm of cannabis use while ensuring that the other needs of the pregnant or lactating person are met and the patient–clinician relationship remains strong.
Supplementary Material
Acknowledgements
Caroline Higgins (a medical librarian) designed and conducted the literature search. Meera Mahmud assisted with critical appraisal.
Funding
This study was funded by the Canadian Institutes of Health Research (grant number 167972), who played no role in the design, conduct, or reporting of the research.
Ethical approval
All data were in the public domain so ethical approval was not required.
Conflict of interest
From April to December 2019, J. Panday was employed as a Research Analyst at PureSinse Inc (a licensed cannabis producer). She does not hold any remaining financial or personal connection to PureSinse, which is no longer in operation. From May 2021 - February 2022, J. Panday was employed as a freelance research coordinator by Avail Cannabis Clinics, a privately owned network of medical clinics, to prepare and submit ethics applications for research related to the use of cannabis to alleviate PTSD symptoms in military populations. Ms. Panday was compensated hourly for this work, which has concluded. She does not hold any remaining financial or personal connection to Avail.
Data availability
All data were publicly available and a list of papers is available in Table 2. Data collection and extraction forms used in this review are available by contacting the corresponding author.
References
- 1. Brown QL, Sarvet AL, Shmulewitz D, Martins SS, Wall MM, Hasin DS. Trends in marijuana use among pregnant and nonpregnant reproductive-aged women, 2002–2014. JAMA. 2017;317(2):207–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Petrangelo A, Czuzoj-Shulman N, Balayla J, Abenhaim HA. Cannabis abuse or dependence during pregnancy: a population-based cohort study on 12 million births. J Obstet Gynaecol Can. 2019;41(5):623–630. [DOI] [PubMed] [Google Scholar]
- 3. Young-Wolff KC, Tucker LY, Alexeeff S, Armstrong M, Conway A, Weisner C, Goler N. Trends in self-reported and biochemically tested marijuana use among pregnant females in California from 2009–2016. JAMA. 2017;318(24):2490–2491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mark K, Gryczynski J, Axenfeld E, Schwartz RP, Terplan M. Pregnant women’s current and intended cannabis use in relation to their views toward legalization and knowledge of potential harm. J Addict Med. 2017;11(3):211–216. [DOI] [PubMed] [Google Scholar]
- 5. Cerdá M, Wall M, Keyes KM, Galea S, Hasin D. Medical marijuana laws in 50 states: investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug Alcohol Depend. 2012;120(1–3):22–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Statistics Canada. National Cannabis Survey. Ottawa (ON): Statistics Canada; 2019. [Google Scholar]
- 7. Roncero C, Valriberas-Herrero I, Mezzatesta-Gava M, Villegas JL, Aguilar L, Grau-López L. Cannabis use during pregnancy and its relationship with fetal developmental outcomes and psychiatric disorders. A systematic review. Reprod Health. 2020;17(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Astley SJ, Little RE. Maternal marijuana use during lactation and infant development at one year. Neurotoxicol Teratol. 1990;12(2):161–168. [DOI] [PubMed] [Google Scholar]
- 9. Crume TL, Juhl AL, Brooks-Russell A, Hall KE, Wymore E, Borgelt LM. Cannabis use during the perinatal period in a state with legalized recreational and medical marijuana: the association between maternal characteristics, breastfeeding patterns, and neonatal outcomes. J Pediatr. 2018;197:90–96. [DOI] [PubMed] [Google Scholar]
- 10. Badowski S, Smith G. Cannabis use during pregnancy and post-partum. Can Fam Physician. 2020;66:98–103. [PMC free article] [PubMed] [Google Scholar]
- 11. Thompson R, DeJong K, Lo J. Marijuana use in pregnancy: a review. Obstet Gynecol Surv. 2019;74(7):415–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gunn JK, Rosales CB, Center KE, Nuñez A, Gibson SJ, Christ C, Ehiri JE. Prenatal exposure to cannabis and maternal and child health outcomes: a systematic review and meta-analysis. BMJ Open. 2016;6(4):e009986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Stickrath E. Marijuana use in pregnancy: an updated look at marijuana use and its impact on pregnancy. Clin Obstet Gynecol. 2019;62(1):185–190. [DOI] [PubMed] [Google Scholar]
- 14. Bailey BA, Wood DL, Shah D. Impact of pregnancy marijuana use on birth outcomes: results from two matched population-based cohorts. J Perinatol. 2020;5(10):1477-1482. [DOI] [PubMed] [Google Scholar]
- 15. Alharbi FF, el-Guebaly N. Exploring the management of cannabis use among women and during pregnancy. Addict Disord Their Treat. 2014;13(2):93–100. [Google Scholar]
- 16. Metz TD, Borgelt LM. Marijuana use in pregnancy and while breastfeeding. Obstet Gynecol. 2018;132(5):1198–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Braillon A, Bewley S. Committee opinion no. 722: marijuana use during pregnancy and lactation. Obstet Gynecol. 2018;131(1):164. [DOI] [PubMed] [Google Scholar]
- 18. El Marroun H, Bolhuis K, Franken IH, Jaddoe VW, Hillegers MH, Lahey BB, Tiemeier H. Preconception and prenatal cannabis use and the risk of behavioural and emotional problems in the offspring; a multi-informant prospective longitudinal study. Int J Epidemiol. 2019;48(1):287–296. [DOI] [PubMed] [Google Scholar]
- 19. Torres CA, Medina-Kirchner C, O’Malley KY, Hart CL. Totality of the evidence suggests prenatal cannabis exposure does not lead to cognitive impairments: a systematic and critical review. Front Psychol. 2020;11:816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ordean A, Kim G. Cannabis use during lactation: literature review and clinical recommendations. J Obstet Gynaecol Can. 2020;25(10):1248–1253. [DOI] [PubMed] [Google Scholar]
- 21. Tennes K, Avitable N, Blackard C, Boyles C, Hassoun B, Holmes L, Kreye M. Marijuana: prenatal and postnatal exposure in the human. NIDA Res Monogr. 1985;59:48–60. [PubMed] [Google Scholar]
- 22. Ko JY, Farr SL, Tong VT, Creanga AA, Callaghan WM. Prevalence and patterns of marijuana use among pregnant and nonpregnant women of reproductive age. Am J Obstet Gynecol. 2015;213(2):201.e201–201.e210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bayrampour H, Zahradnik M, Lisonkova S, Janssen P. Women’s perspectives about cannabis use during pregnancy and the postpartum period: an integrative review. Prev Med. 2019;119:17–23. [DOI] [PubMed] [Google Scholar]
- 24. Young-Wolff KC, Sarovar V, Tucker LY, Avalos LA, Conway A, Armstrong MA, Goler N. Association of nausea and vomiting in pregnancy with prenatal marijuana use. JAMA Intern Med. 2018;178(10):1423–1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Roberson EK, Patrick WK, Hurwitz EL. Marijuana use and maternal experiences of severe nausea during pregnancy in Hawai ‘i. Hawai’i J Med Public Health. 2014;73(9):283–287. [PMC free article] [PubMed] [Google Scholar]
- 26. Greyson D, Roosevelt L, Boyd CJ. Desistance, self-treatment, or substitution: decisions about cannabis use during pregnancy. J Midwifery Womens Health. 2021;66(1):96–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Weisbeck SJ, Bright KS, Ginn CS, Smith JM, Hayden KA, Ringham C. Perceptions about cannabis use during pregnancy: a rapid best-framework qualitative synthesis. Can J Public Health. 2021;112(1):49–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Barbosa-Leiker C, Burduli E, Smith CL, Brooks O, Orr M, Gartstein M. Daily cannabis use during pregnancy and postpartum in a state with legalized recreational cannabis. J Addict Med. 2020;14(6):467–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Benoit C, Magnus S, Phillips R, Marcellus L, Charbonneau S. Complicating the dominant morality discourse: mothers and fathers’ constructions of substance use during pregnancy and early parenthood. Int J Equity Health. 2015;14(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ng JY, Gilotra K, Usman S, Chang Y, Busse JW. Attitudes toward medical cannabis among family physicians practising in Ontario, Canada: a qualitative research study. CMAJ Open. 2021;9(2):E342–E348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sword W, Heaman MI, Brooks S, Tough S, Janssen PA, Young D, Kingston D, Helewa ME, Akhtar-Danesh N, Hutton E. Women’s and care providers’ perspectives of quality prenatal care: a qualitative descriptive study. BMC Pregnancy Childbirth. 2012;12(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hong QN, Pluye P, Bujold M, Wassef M. Convergent and sequential synthesis designs: implications for conducting and reporting systematic reviews of qualitative and quantitative evidence. Syst Rev. 2017;6(1):61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lizarondo L, Stern C, Carrier J, Godfrey C, Reiger K, Salmond S, Apostolo J, Kirkpatrick P, Loveday H. Mixed methods systematic reviews. In: Aromataris E, Munn Z, editors. Joanna Briggs Institute Reviewer’s Manual. Adelaide, Australia: The Joanna Briggs Institute; 2019. [Google Scholar]
- 34. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med. 2021;18(3):e1003583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, Gagnon MP, Griffiths F, Nicolau B, O’Cathain A, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34(4):285–291. [Google Scholar]
- 36. Pace R, Pluye P, Bartlett G, Macaulay AC, Salsberg J, Jagosh J, Seller R. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. Int J Nurs Stud. 2012;49(1):47–53. [DOI] [PubMed] [Google Scholar]
- 37. Bergeria CL, Heil SH. Surveying lactation professionals regarding marijuana use and breastfeeding. Breastfeed Med. 2015;10(7):377–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Brooks E, Gundersen DC, Flynn E, Brooks-Russell A, Bull S. The clinical implications of legalizing marijuana: are physician and non-physician providers prepared? Addict Behav. 2017;72:1–7. [DOI] [PubMed] [Google Scholar]
- 39. Geraghty S, Doleman G, De Leo A. Midwives’ attitudes towards pregnant women using substances: informing a care pathway. Women Birth. 2019;32(4):e477–e482. [DOI] [PubMed] [Google Scholar]
- 40. Gérardin M, Victorri-Vigneau C, Louvigné C, Rivoal M, Jolliet P. Management of cannabis use during pregnancy: an assessment of healthcare professionals’ practices. Pharmacoepidemiol Drug Saf. 2011;20(5):464–473. [DOI] [PubMed] [Google Scholar]
- 41. Gotham HJ, Wilson K, Carlson K, Rodriguez G, Kuofie A, Witt J. Implementing substance use screening in family planning. J Nurse Pract. 2019;15(4):306–310. [Google Scholar]
- 42. Gray J, Beatty JR, Svikis DS, Puder KS, Resnicow K, Konkel J, Rice S, McGoron L, Ondersma SJ. Electronic brief intervention and text messaging for marijuana use during pregnancy: initial acceptability of patients and providers. JMIR Mhealth Uhealth. 2017;5(11):e172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Herzig K, Huynh D, Gilbert P, Danley DW, Jackson R, Gerbert B. Comparing prenatal providers’ approaches to four different risks: alcohol, tobacco, drugs, and domestic violence. Women Health. 2006;43(3):83–101. [DOI] [PubMed] [Google Scholar]
- 44. Holland CL, Nkumsah MA, Morrison P, Tarr JA, Rubio D, Rodriguez KL, Kraemer KL, Day N, Arnold RM, Chang JC. “Anything above marijuana takes priority”: obstetric providers’ attitudes and counseling strategies regarding perinatal marijuana use. Patient Educ Couns. 2016;99(9): 1446–1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Holland CL, Rubio D, Rodriguez KL, Kraemer KL, Day N, Arnold RM, Chang JC. Obstetric health care providers’ counseling responses to pregnant patient disclosures of marijuana use. Obstet Gynecol. 2016;127(4):681–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Northrup TF, Klawans MR, Villarreal YR, Abramovici A, Suter MA, Mastrobattista JM, Moreno CA, Aagaard KM, Stotts AL. Family physicians’ perceived prevalence, safety, and screening for cigarettes, marijuana, and electronic-nicotine delivery systems (ENDS) use during pregnancy. J Am Board Fam Med. 2017;30(6):743–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Petersen Williams P, Petersen Z, Sorsdahl K, Mathews C, Everett-Murphy K, Parry CD. Screening and brief interventions for alcohol and other drug use among pregnant women attending midwife obstetric units in Cape Town, South Africa: a qualitative study of the views of health care professionals. J Midwifery Womens Health. 2015;60(4):401–409. [DOI] [PubMed] [Google Scholar]
- 48. Salisbury KW. Medical provider perceptions of breastfeeding women who use recreational marijuana. School of Public Health University of Washington; 2017. [Google Scholar]
- 49. Young-Wolff KC, Gali K, Sarovar V, Rutledge GW, Prochaska JJ. Women’s questions about perinatal cannabis use and health care providers’ responses. J Womens Health (Larchmt). 2020;30(7):919–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–553. [DOI] [PubMed] [Google Scholar]
- 51. Sandelowski M, Leeman J, Knafl K, Crandell JL. Text-in-context: a method for extracting findings in mixed-methods mixed research synthesis studies. J Adv Nurs. 2013;69(6):1428–1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis. London, UK: Sage Publications; 2006. [Google Scholar]
- 53. Bartholomew ML, Lee M-J. Substance use in the breastfeeding woman. Contemporary OB/GYN. 2019;64(9):22–42. [Google Scholar]
- 54. Meffert BN, Morabito DM, Mosich MK, Loflin MJ, Sottile J, Heinz AJ. Navigating blind in the green rush: clinical considerations and harm reduction practices for cannabis. Curr Drug Res Rev. 2019;11(1):3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Chang JC, Tarr JA, Holland CL, De Genna NM, Richardson GA, Rodriguez KL, Sheeder J, Kraemer KL, Day NL, Rubio D. Beliefs and attitudes regarding prenatal marijuana use: perspectives of pregnant women who report use. Drug Alcohol Depend. 2019;196:14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. World Health Organization. Guidelines for the identification and management of substance use and substance use disorders in pregnancy. Geneva, Switzerland: World Health Organization; 2014. [PubMed] [Google Scholar]
- 57. Braillon A, Bewley S. Committee Opinion No. 722: marijuana use during pregnancy and lactation. Obstet Gynecol. 2018;131(1):164. [DOI] [PubMed] [Google Scholar]
- 58. Ordean A, Wong S, Graves L. No. 349-Substance Use in Pregnancy. J Obstet Gynaecol Can. 2017;39(10):938–956.e3. [DOI] [PubMed] [Google Scholar]
- 59. Piper BJ, DeKeuster RM, Beals ML, Cobb CM, Burchman CA, Perkinson L, Lynn ST, Nichols SD, Abess AT. Substitution of medical cannabis for pharmaceutical agents for pain, anxiety, and sleep. J Psychopharmacol. 2017;31(5):569–575. [DOI] [PubMed] [Google Scholar]
- 60. Davis E, Lee T, Weber JT, Bugden S. Cannabis use in pregnancy and breastfeeding: the pharmacist’s role. Can Pharm J (Ott). 2020;153(2):95–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Dennis CL, Vigod S. Cannabis use in pregnancy: a harm reduction approach is needed with a focus on prevention and positive intervention. Evid Based Nurs. 2021;24(2):58. [DOI] [PubMed] [Google Scholar]
- 62. Skelton KR, Benjamin-Neelon SE, Young-Wolff KC. Management of cannabis use in breastfeeding women: the untapped potential of International Board Certified Lactation Consultants. Breastfeed Med. 2020;15(2):117–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. National Harm Reduction Coalition. Harm Reduction Principles. National Harm Reduction Coalition; 2021. [Accessed September 1, 2021]. https://harmreduction.org/about-us/principles-of-harm-reduction/ [Google Scholar]
- 64. Wright TE, Schuetter R, Fombonne E, Stephenson J, Haning WF III. Implementation and evaluation of a harm-reduction model for clinical care of substance using pregnant women. Harm Reduct J. 2012;9(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Nichter M, Nichter M, Adrian S, Goldade K, Tesler L, Muramoto M. Smoking and harm-reduction efforts among postpartum women. Qual Health Res. 2008;18(9):1184–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Thomson R, McDaid L, Emery J, Phillips L, Naughton F, Cooper S, Dyas J, Coleman T. Practitioners’ views on nicotine replacement therapy in pregnancy during lapse and for harm reduction: a qualitative study. Int J Environ Res Public Health. 2019;16(23):4791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Kumar R, Gould GS. Tobacco harm reduction for women who cannot stop smoking during pregnancy—a viable option? JAMA Pediatr. 2019;173(7):615–616. [DOI] [PubMed] [Google Scholar]
- 68. Flavin J. A glass half full? Harm reduction among pregnant women who use cocaine. J Drug Issues. 2002;32(3):973–998. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data were publicly available and a list of papers is available in Table 2. Data collection and extraction forms used in this review are available by contacting the corresponding author.