Dear editor,
Quetiapine is a dibenzothiazepine derivative atypical anti-psychotic and has been suggested to have a lower risk of movement disorder adverse effects. Few reports of myoclonus induced by quetiapine are available in the literature, especially at therapeutic dosages [1].
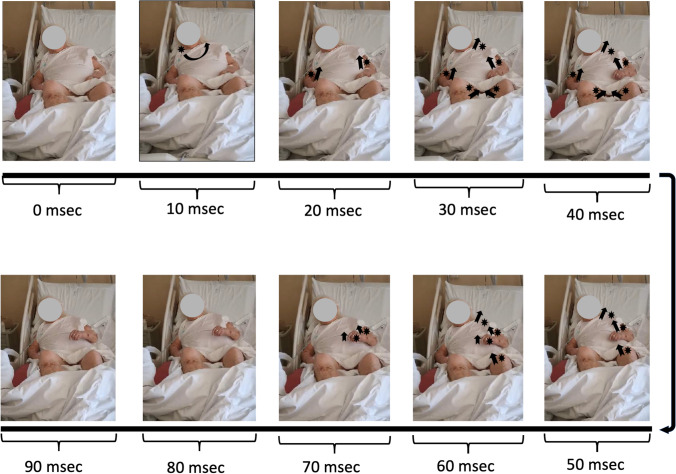
We report the case of an 85-year-old woman with a diagnosis of vascular dementia and behavioral disorder, who was admitted for respiratory distress in heart failure. After few days of hospitalization, she displayed generalized, sudden jerks of the trunk and extremities, leading to the request for a neurological bedside evaluation. Through the accurate analysis of the video made with a simple smartphone during the bedside examination, we were able to disclose the progression of the myoclonic jerks. To do that, we used a free editing software (Wondershare filmora 9) that allowed to analyze the video with a time frame of 10 ms. We found that jerks started at rest in the right sternocleidomastoid muscle and caudally spread to bilateral arm and leg muscles, being clinically compatible with subcortical generalized myoclonus (Video, segment 1; Fig. 1) [1]. Brain-TC showed mild atrophy. Blood tests and electroencephalography were normal. An evaluation of the current therapy highlighted an incorrect dosage of quetiapine (from 300 to 600 mg/day) even if within therapeutic dosages. The restoration of the correct dosage led to progressive disappearance of involuntary jerks (Video, segment 2).
Fig. 1.
Timeline of myoclonic jerks obtained after analyzing the video with a time frame of 10 ms. Jerks started at rest in the right sternocleidomastoid muscle and caudally spread to bilateral biceps followed by left trapezius, bilateral adductor muscles, left quadriceps muscle, and extensor muscle of the left hand. Muscles are highlighted with a black eight-pointed star, while the direction of movement was highlighted with the black arrows
Myoclonus is a sudden, brief, shock-like involuntary movement caused by muscular contractions or inhibitions. A comprehensive history and examination are critical in defining the type and etiology of myoclonus [2]. Possible etiologies include neurodegenerative disorders, metabolic disorders, and central nervous system infections. Moreover, myoclonus may occur as an effect of certain drug overdose or discontinuation, including antipsychotic agents [1, 2]. Quetiapine fumarate belongs to the class of antipsychotic drugs known as the dibenzothiazepine derivatives. Compared to the first generation of antipsychotic medications, it is characterized by an improved safety profile, particularly a decrease in the frequency of extrapyramidal symptoms and tardive dyskinesia [3]. Myoclonus is rarely induced by quetiapine, especially at therapeutic dosages. However, although maximum doses of quetiapine are known to be around 800 mg/day, in our case the reduction of the quetiapine dosage from 600 to 300 mg/day led to the disappearance of myoclonus, supporting our hypothesis regarding the role of this drug in the genesis of the movement disorder.
Moreover, this case highlights that even in an acute setting, a simple smartphone videoclip, if analyzed in depth by using a video editing software, could be of a great help in the description and understanding of hyperkinetic movement disorders. This is particularly true during the COVID-19 outbreak that has strongly limited the possibility to move patients from one hospital (spoke) to another (hub) only to perform second-rate expert medical advice or “ancillary” instrumental investigations. In this way, with a minimum need for resources, a short lead time and above all without taking risks to the patient, good diagnostic results can still be obtained.
Supplementary Information
Below is the link to the electronic supplementary material.
Declarations
Ethical approval
All authors have approved the final article.
Informed consent
Written informed consent was obtained from the patient to be videoed for publication.
Conflict of interest
The authors do not have any conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Velayudhan L, Kirchner V. Quetiapine-induced myoclonus. Int Clin Psychopharmacol. 2005;20(2):119–120. doi: 10.1097/00004850-200503000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Caviness JN. Myoclonus. Contin Lifelong Learn Neurol. 2019;25(4):1055–1080. doi: 10.1212/CON.0000000000000750. [DOI] [PubMed] [Google Scholar]
- 3.Strachan PM, Benoff BA. Mental status change, myoclonus, electrocardiographic changes, and acute respiratory distress syndrome induced by quetiapine overdose. Pharmacother J Hum Pharmacol Drug Ther. 2006;26(4):578–582. doi: 10.1592/PHCO.26.4.578. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.