Abstract
Background:
Youth e-cigarette use is associated with initiation of combustible cigarette smoking, but prior studies have rarely accounted for time-varying measures of e-cigarette exposure or time-dependent confounding of e-cigarette use and smoking initiation.
Methods:
Using five waves of the Population Assessment of Tobacco and Health (2013-2019), we estimated marginal structural models with inverse probability of treatment and censoring weights to examine the association between time-varying e-cigarette initiation and subsequent cigarette smoking initiation among e-cigarette- and cigarette-naïve youth (12-17y) at baseline. Time-dependent confounders used as predictors in inverse probability weights included tobacco-related attitudes or beliefs, mental health symptoms, substance use, and tobacco-marketing exposure.
Results:
Among 9,584 youth at baseline, those who initiated e-cigarettes were 2.4 times as likely to subsequently initiate cigarette smoking as youth who did not initiate e-cigarettes (risk ratio [RR]=2.4, 95% CI: 2.2-2.7), after accounting for time-dependent confounding and selection bias. Among youth who initiated e-cigarettes, more frequent vaping was associated with greater risk of smoking initiation (RR ≥3 days/month=1.8, 95% CI: 1.4-2.2; 1-2 days/month=1.2, 95% CI: 0.93-1.6 vs. 0 days/month). Weighted marginal structural model estimates were moderately attenuated compared to unweighted estimates adjusted for baseline-only confounders. At the United States population-level, we estimated over half a million youth initiated cigarette smoking because of prior e-cigarette use over follow-up.
Conclusions:
The association between youth vaping and combustible cigarette smoking persisted after accounting for time-dependent confounding. We estimate that e-cigarette use accounts for a considerable share of cigarette initiation among US youth.
Keywords: E-cigarettes, Smoking, Youth, Marginal Structural Models, Confounding
Introduction
Electronic cigarettes (e-cigarettes) are the most popular tobacco product used by youth in the United States (US).1 Based on National Youth Tobacco Survey data from the first 2 months of 2020, approximately 1 in 5 high school students were current e-cigarette users.2,3 E-cigarette liquids often contain high levels of nicotine, a highly addictive compound that can negatively affect attention, memory, learning, and impulse control among youth.4-6 E-cigarette liquid and aerosol also contain other potentially harmful constituents including solvents,7 flavoring compounds,8 ultrafine particles,9 heavy metals,10 polycyclic aromatic hydrocarbons,11 and volatile organic compounds,11which may negatively affect the heart, brain, and lungs of youth. In addition to the direct harm of e-cigarette exposures on youth health, vaping nicotine might predispose youth to initiate combustible cigarette smoking.12
E-cigarette use could cause youth to initiate cigarette smoking through a variety of pathways, such as development of nicotine dependence, accessibility of e-cigarettes through the same source as cigarettes, modeling substance use norms, or social influences.13 Three meta-analyses reported adjusted odds ratios (OR) for the association between ever vaping and subsequent cigarette smoking among youth to be between 2.9 and 3.8.14-16 However, there are arguments against the theory that e-cigarettes are a cause of cigarette smoking initiation. For example, while youth vaping has increased over time in the US, youth cigarette smoking has consistently declined among most demographics.17 In addition, several sources of systematic error may produce a spurious association between youth vaping and smoking initiation, including time-dependent confounding, selection bias, and misclassification.
Most prior studies on youth e-cigarette use and smoking initiation measure e-cigarette exposure at baseline only. However, adolescence is characterized by experimentation, and youth who never vaped at study baseline could initiate e-cigarettes at a subsequent time point. Similarly, youth might experiment with vaping at baseline and not use e-cigarettes again over follow-up. Studies that measure e-cigarette exposure at baseline only are akin to estimating the intention-to-treat effect in a randomized trial, in which outcomes are compared between baseline treatment arms without consideration of adherence over-follow-up.18 Treating e-cigarette use as a time-varying exposure captures non-adherence to baseline reported e-cigarette use, and can be used to estimate effects analogous to per-protocol or as-treated effects, whereby outcomes are compared between treatment received over follow-up (as-treated effect), or between treatment groups as assigned (per-protocol effect).18,19
When modeling time-varying exposures, one must account for confounders that vary over time to estimate a valid effect.20 If time-varying confounders simultaneously act as causal intermediates of vaping and smoking initiation or if treatment-confounder feedback exists in other forms (i.e., time-dependent confounding),19 use of traditional regression methods may bias effect estimates by conditioning on causal intermediates or inducing collider stratification bias.20 Time-dependent confounding may be an important unaccounted-for source of bias in studies on time-varying e-cigarette use and youth cigarette smoking initiation. Factors such as alcohol use, mental health issues, and certain attitudes or beliefs could affect e-cigarette use and smoking initiation but also be affected by prior e-cigarette use, i.e., function as both confounders and causal intermediates. To appropriately adjust for such time-dependent confounding, researchers can employ analytic techniques called g-methods, which include marginal structural models.19
Cohort studies on vaping and smoking initiation are also vulnerable to selection bias due to differential loss-to-follow-up (i.e., informative censoring). If study continuation (or discontinuation) is directly or indirectly related to the occurrence of the outcome, estimates of the association between vaping and smoking may be biased.21,22 Marginal structural models can be used to address selection bias induced by differential loss-to-follow-up. In addition, survey-based studies rely on self-reported accounts of youth vaping and cigarette smoking which may be misreported. Exposure and outcome misclassification can induce substantial bias,23 yet no prior studies have quantified the impact of misclassification on the association between self-reported vaping and smoking initiation.
The present study examines the association between time-varying e-cigarette use and combustible cigarette smoking initiation among US youth, accounting for time-dependent confounding, selection bias, and exposure and outcome misclassification.
METHODS
Study Population and Study Design
This study uses five waves of data from the Population Assessment of Tobacco and Health (PATH), a prospective cohort study on tobacco use established by the National Institutes of Health and Federal Drug Administration. We used de-identified data from the youth public use files at wave 1 (2013-2014), wave 2 (2014-2015), wave 3 (2015-2016), wave 4 (2016-2018), and wave 5 (2018-2019). At wave 1, 13,651 youth (12-17y) were enrolled using a four-stage stratified area probability sample design.24 Youth who turned 18 years of age over follow-up “age out” of the PATH youth survey and are subsequently included in the PATH adult cohort. Rather than censoring youth when they turned 18 over follow-up, youth who aged into the adult cohort are retained for this analysis (i.e., by using data collected in follow-up waves from the adult cohort study).
The study design, data collection methods, and response rates for PATH have been described in detail previously.24 Briefly, interview data were collected using household computer-assisted interview methods, and participants provided information at each study visit on tobacco-use behaviors, attitudes and beliefs, and socio-demographic and physical/mental health factors. The WESTAT Institutional Review Board obtained parental permission and youth assent for participation.
In this study, wave 1 provides data on prior confounders and exposure history. Wave 2 serves as study baseline, and waves 3,4, and 5 are follow-up assessments. We restricted our analysis to youth who had never smoked a combustible cigarette at wave 2 (baseline) and had never used an e-cigarette at wave 1 (prior to baseline; Figure 1). We excluded youth who used e-cigarettes at wave 1 to avoid prevalent exposure bias.25,26
Figure 1.
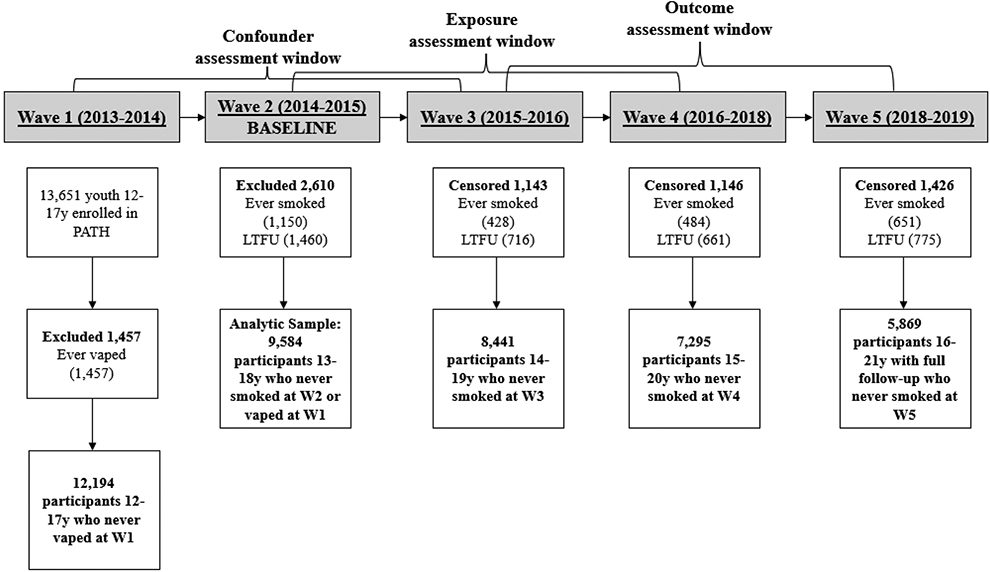
Exclusions, Censoring, and Measurement Assessment Windows.
Measures
Exposure: E-cigarette Initiation
The exposure was time-varying e-cigarette use, measured at waves 2, 3, and 4. We examined four specifications of e-cigarette use.
First, we examined any initiation of e-cigarettes (yes/no), defined as having ever used e-cigarettes, even once or twice, compared to never initiating e-cigarettes (reference). Once a youth ever used an e-cigarette, they remained an ever-user at the subsequent wave.
Second, among those who reported any e-cigarette initiation, we further distinguished recency of e-cigarette use (current/former use) at a given wave. Current use was defined as using e-cigarettes in the past 30-days at a given follow-up wave, and former use was defined as initiated use of e-cigarettes, but having not used e-cigarettes in the past 30-days at a given wave. Participants were allowed to switch between current and former use status (or vice versa) if they changed behavior between waves.
Third, among those who reported any e-cigarette initiation, we examined flavor use at initiation (non-tobacco flavor/tobacco flavor). Initiation with non-tobacco flavor was defined as a positive report of first using an e-cigarette flavored to taste like “menthol, mint, clove, spice, fruit, chocolate, alcoholic drinks, candy, or other sweets”; those who responded negatively were classified as initiating with tobacco-flavored e-cigarettes.
Fourth, among participants who reported any e-cigarette initiation, we created an exposure for frequency of past 30-day e-cigarette use at a given wave. More than 60% of youth reported vaping <3 days in the past 30-days. To avoid practical positivity issues resulting from too many exposure categories (i.e., non-zero probability of exposure within strata of covariates), vaping frequency was trichotomized as 0-days (reference), 1-2 days, and ≥3 days in the past 30-days. The reference group included youth who ever initiated e-cigarettes but reported vaping 0 days in the past 30-days. Participants were allowed to switch between vaping frequency categories between waves.
Outcome: Cigarette Smoking Initiation
The primary outcome was combustible cigarette smoking initiation measured at waves 3, 4 and 5, defined as having ever smoked a cigarette, even one or two puffs. A secondary outcome was first report of current combustible smoking, defined as smoking in the past 30 days. We used current smoking to capture initiation of more regular smoking, as in prior studies.27,28
Confounders
We measured time-invariant confounders at wave 1 and time-varying confounders were measured at waves 1, 2, and 3. Confounders were variables associated with both e-cigarette use and cigarette smoking initiation in prior literature, including socio-demographic,29 behavioral,30-32 and environmental factors.30
Confounders measured at wave 1 only and used as predictors in inverse probability of treatment and censoring weights included age (12-14 years, 15-17 years), biologic sex (male, female), parent’s educational attainment as a proxy for socio-economic status (<high school graduate or GED, ≥ high school graduate), living with a user of any tobacco product (yes/no), past 12-month grade performance (Mostly A’s or B’s, all other grades), and a measure of sensation-seeking collected via the Brief Sensation Seeking Scale (continuous score with natural cubic spline).33
We incorporated self-reported race and ethnicity as a proxy for social and/or structural racism which may influence substance use.34 Participants were asked, “What is your race?” with 14 response categories (select all that apply), and “Are you Hispanic, Latino/Latina, or of Spanish origin?” In public use datasets, race was available as a categorical variable (Black, White, all other races). We combined race and ethnicity for analysis (non-Hispanic Black, non-Hispanic White, Non-Hispanic Asian, Non-Hispanic other races, Hispanic). We included age, living with a tobacco user, grades, and sensation-seeking as wave 1 measures because they were either collected only at wave 1 (sensation-seeking), only asked on the youth survey (grades), or the change over time was minimal (age, living with a tobacco user).
Time-varying confounders used as predictors in weight models included externalizing mental health problems measured via the Global Appraisal of Individual Needs Short Screener (GAIN-SS) (low or moderate vs. high problems);35 past 12-month use of alcohol, marijuana, or other tobacco product use (yes/no); having been talked to by parents about not using tobacco in the past 12 months (yes/no); having a favorite tobacco advertisement (yes/no); and perceived harm of e-cigarettes compared to cigarettes (less harmful vs. equally harmful, more harmful, don’t know). We included a dichotomous measure of cigarette susceptibility, with non-susceptible defined as responding negatively to each question: (1) being curious about smoking a cigarette, (2) thinking about smoking in the next year, and (3) would smoke if a friend offered a cigarette.36
Analysis
We restricted data as one observation per exposure wave (up to three observations per participant). Follow-up began at wave 2, and we censored youth at cigarette smoking initiation, or the first wave lost to follow-up. We calculated the exposure prevalence, rate of smoking initiation (i.e., events per person–waves), and distribution of covariates stratified by exposure and loss to follow-up status.
Marginal Structural Models (MSMs)
We used marginal structural models to adjust for time-dependent confounding. These models incorporate inverse probability of treatment weights (IPTW) to create a pseudopopulation in which participants with low probability for the e-cigarette exposure they received are given higher weights so that exposure appears random with respect to measured covariates.20
IPTW estimation (exposure model)
For each participant and wave for which exposure was measured, we estimated a stabilized weight equal to the inverse probability that a participant received the e-cigarette exposure history they received, given past exposure and covariates. Stabilized weights reduce probability of extreme weights and increase precision.20,37 To estimate the weight denominator for the dichotomous exposure of ever vs. never e-cigarette initiation, we used pooled logistic regression to estimate the probability of never vaping at each time point. Independent variables included all time-invariant covariates, time-varying covariates measured at the prior wave, and a variable for visit to allow for a time-specific intercept.38 The same model estimated the weight numerator, excluding time-varying values of covariates. We fitted weight models on the subsample of observations for which no e-cigarette initiation had yet occurred.
Predicted probabilities were used to derive the probability of observed e-cigarette exposure at each time point. For participants that used e-cigarettes, their probability of observed exposure was equal to 1 minus the predicted probability from the above regression. For those who had not initiated e-cigarettes, their probability of observed exposure was equal to the predicted probability. To estimate the probability of e-cigarette history up to each time point, we multiplied probabilities over time (e.g., at wave 4, the denominator was equal to the product of the probabilities at wave 2, 3, and 4).
The same approach but with pooled multinomial logistic regression was used to estimate weights for the remaining three categorical exposures. For current, former, and never e-cigarette use and vaping frequency exposures, we did not restrict models to the subsample of observations for which no e-cigarette initiation had yet occurred, as participants were able to switch between exposure categories.
We used a similar process to estimate stabilized inverse probability of censoring weights (IPCW) representing the probability of remaining non-censored at each observation conditional on past covariates and exposure among the full sample at baseline. Incorporation of IPCW accounts for selection bias due to dropout by creating a pseudopopulation that would have been observed had loss-to-follow-up been random with respect to prior exposure and covariates.22 The final weights were equal to the product of the IPTW and IPCW. See eAppendix 1 for SAS code, calculation, and distribution of the final weights. All stabilized weights had a mean of 1.0.
Marginal Structural Model (outcome model)
We estimated the parameters of the following marginal structural model: log (pr[Ya = 1∣ν]) = β0(t) + β1a(t) + β2ν; β0(t) represents the time-specific intercept, a(t) is e-cigarette exposure at wave t, and v is a vector of wave 1 covariates. We fitted weighted discrete-time Poisson regression models for each exposure specification, using the SAS procedure PROC GENMOD and a repeated statement with an independent correlation matrix for robust standard errors. Under assumptions of exchangeability, positivity, consistency, and correct model specification,37 β1 is interpreted as the causal risk ratio (RR) for the effect of initiating e-cigarettes, comparing participants’ risk of smoking initiation if they initiated e-cigarettes at or before wave t with their risk of smoking initiation if they never initiated e-cigarettes at or before wave t. The interpretation changes slightly for the current, former, or never initiating e-cigarettes and vaping frequency exposures as the effect of most recent exposure at wave t. See eAppendix 2 for discussion of corresponding causal estimands.
For each exposure–outcome pair, we additionally estimated the association using traditional regression models adjusting for wave 1 values of confounders. We expect these estimates to be biased and they serve as a comparison for the magnitude of residual time-dependent confounding after baseline.
Secondary and Sensitivity Analyses
We conducted a simple quantitative bias analysis to assess the magnitude and direction of bias due to potential non-differential exposure and differential outcome misclassification. Informed by internal and external validation studies, we re-estimated marginal structural models using a range of sensitivity and specificity values for self-reported e-cigarette use and cigarette smoking and record-level Bernoulli trials (eAppendix 3).39 40
We multiplied inverse probability weights by PATH wave 2 sample weights to produce estimates representative of the US population at study baseline. Sample-weighted associations were estimated using logistic regression with PROC SURVEYLOGISTIC to accommodate the Balanced Repeated Replication method and Fay adjustment (ρ = 0.3) for robust standard errors, as recommended in the PATH user guide.24
We calculated the population attributable fraction (PAF) for ever e-cigarette initiation using the sample-weighted marginal structural model odds ratio (OR) and vaping prevalence among youth who initiated smoking (Pr(Ed)) with the following equation:41 Pr(Ed)*OR-1/OR. Sample-weighted ORs approximate RRs under the rare disease assumption. The PAF 95% confidence interval was calculated using the method proposed by Greenland (1999).42 We used SAS survey procedures and PATH sample weights to estimate the number of youths in the US who initiated cigarette smoking between waves 2 and 5 (2014-2019). We then multiplied the total number of youths who initiated cigarette smoking by the PAF percentage to estimate the number of youths who initiated cigarette smoking attributable to prior e-cigarette initiation over the study period.
Missing Data
We used the Markov Monte Carlo method of multiple imputation with 10 imputed datasets to simulate values for missing data. Data were missing for <3% of participants for all variables except: wave 1 other tobacco use (4.4%), wave 3 flavor of first e-cigarette (8.7%), wave 4 ever cigarette smoking (4.4%), and wave 4 ever e-cigarette use (4.4%).
Results
The 9,584 cigarette and e-cigarette naïve youth at wave 1 contributed 23,167 person–waves. Over the study period, 1,763 initiated e-cigarettes (12% exposed person–waves, 593 at wave 2, 783 at wave 3, and 385 at wave 4), 1,563 initiated combustible cigarette smoking (7% per person–wave), 917 reported current cigarette smoking (4% per person–wave), and 2,152 (22%) were lost to follow-up.
Youth who initiated e-cigarettes on average were older, more likely to live with a tobacco user, had a higher sensation-seeking score, were more likely to have externalizing mental health problems, to have used alcohol, marijuana, and other tobacco products, had worse grade performance, were more susceptible to cigarette smoking, and were more likely to believe e-cigarettes are less harmful than cigarettes than youths who never initiated e-cigarettes (Table 1). There were few differences in confounders or baseline e-cigarette use between youths retained versus lost to follow-up (eTable 1).
Table 1.
Wave 1 covariates by e-cigarette initiation over follow-up among 9,584 cigarette naive youth at baseline
| Covariates measured at wave 1 | Ever e-cigarette use (n=1,763) |
Never e-cigarette use (n=7,821) |
|---|---|---|
| 12-14 years old, N (%) | 829 (47) | 4,719 (60) |
| 15-17 years old, N (%) | 934 (53) | 3,102 (40) |
| Female sex, N (%) | 829 (47) | 3,892 (50) |
| Race/ethnicity, N (%) | ||
| non-Hispanic Black | 206 (12) | 1,172 (15) |
| non-Hispanic white | 874 (50) | 3,665 (47) |
| non-Hispanic Asian or other race | 147 (8) | 721 (9) |
| Hispanic | 536 (30) | 2,263 (29) |
| Parental Education, N (%) | ||
| < High School or equivalent | 639 (36) | 3013 (39) |
| Some college or Associates degree | 586 (33) | 2,385 (31) |
| ≥Bachelors degree | 539 (31) | 2423 (31) |
| Lives with tobacco user, N (%) | 668 (38) | 2,274 (29) |
| Brief Sensation Seeking Scale, median (interquartile range) | 3.0 (2.7-3.7) | 3.7 (3.0-4.3) |
| Externalizing mental health problems, N (%) | ||
| Low | 436 (25) | 3,314 (42) |
| Medium | 619 (35) | 2,474 (32) |
| High | 708 (40) | 2,033 (40) |
| Past 12-month alcohol use, N (%) | 326 (19) | 515 (7) |
| Past 12-month marijuana use, N (%) | 113 (6) | 143 (2) |
| Past 12-month other tobacco use, N (%) | 125 (7) | 142 (2) |
| Parent talked to youth about not using tobacco, N (%) | 954 (54) | 3,924 (50) |
| Grades, N (%) | ||
| Mostly As | 411 (23) | 2,314 (30) |
| Mostly As and Bs | 633 (36) | 2,763 (35) |
| Mostly Bs | 168 (10) | 675 (9) |
| Mostly Bs and Cs or lower | 551 (31) | 2,069 (27) |
| Susceptible to cigarette smoking, N (%) | 813 (46) | 2,061 (26) |
| Believe e-cigarettes are less harmful tshan cigarettes, N (%) | 910 (52) | 1,914 (37) |
| Has a favorite tobacco advertisement, N (%) | 164 (9) | 459 (6) |
E-cigarette use and Smoking Initiation: Ever Smoking Outcome
Table 2 presents results from marginal structural models and traditional baseline-adjusted models for the ever-smoking outcome. Prior to accounting for time-dependent confounding, baseline-adjusted RRs for the association between e-cigarette use and cigarette smoking initiation were 2.7 (95% CI: 2.4–3.0) for ever e-cigarette use, 3.5 (95% CI: 2.9–4.1) for current e-cigarette use, and 2.5 (95% CI: 2.2–2.9) for former e-cigarette use relative to never e-cigarette use. After accounting for time-dependent confounding and selection bias using marginal structural models, RRs for cigarette smoking initiation attenuated to 2.4 (95% CI: 2.2–2.7) for ever e-cigarette use, 3.1 (95% CI: 2.6–3.7) for current e-cigarette use, and 2.2 (95% CI: 2.0–2.5) for former e-cigarette use. In marginal structural models, there was no difference in risk of smoking initiation by flavor use at initiation. Among youth who ever initiated e-cigarettes, marginal structural model-adjusted RRs for smoking initiation were 1.8 (95% CI: 1.4–2.2) for vaping ≥3 days and 1.2 (95% CI: 0.93–1.6) for vaping 1–2 days compared to vaping 0 days in the past 30 days.
Table 2.
Youth e-cigarette use and ever cigarette smoking initiation: Baseline-adjusted and marginal structural model discrete-time regression results
| Crudea | Unweighted Baseline- Adjustedb |
MSMb,c | ||||||
|---|---|---|---|---|---|---|---|---|
| Time-varying e-cigarette use | No. youth initiating smoking |
Total person- waves |
RR | 95% CI | RR | 95% CI | RR | 95% CI |
| Never use | 1,001 | 20,368 | 1.0 | REF | 1.0 | REF | 1.0 | REF |
| Ever use | 562 | 2,799 | 3.8 | 3.4-4.2 | 2.7 | 2.4-3.0 | 2.4 | 2.1-2.7 |
| Former used | 378 | 2,101 | 3.4 | 3.0-3.8 | 2.5 | 2.2-2.9 | 2.2 | 2.0-2.5 |
| Current usee | 184 | 698 | 4.9 | 4.2-5.8 | 3.5 | 2.9-4.1 | 3.1 | 2.6-3.7 |
| Tobacco flavored | 41 | 241 | 3.5 | 2.6-4.8 | 2.5 | 1.8-3.5 | 2.4 | 1.7-3.3 |
| Non-Tobacco flavored | 521 | 2,558 | 3.8 | 3.4-4.2 | 2.8 | 2.5-3.1 | 2.4 | 2.2-2.7 |
| E-cigarette frequencyf | ||||||||
| 0 days | 399 | 2,204 | 1.0 | REF | 1.0 | REF | 1.0 | REF |
| 1-2 days | 72 | 315 | 1.2 | 0.96-1.6 | 1.2 | 0.92-1.5 | 1.2 | 0.93-1.6 |
| ≥3 days | 91 | 280 | 1.8 | 1.4-2.3 | 1.7 | 1.3-2.1 | 1.8 | 1.4-2.2 |
CI indicates confidence interval, MSM marginal structural model, RR risk ratio.
Model includes time-varying exposure and time-specific intercept
Model includes time-varying exposure, time-specific intercept, and wave 1 values of age, sex, race/ethnicity, parental education, living with tobacco user, grades, externalizing mental health, alcohol, marijuana, and other tobacco use (past 12-months), cigarette susceptibility, perceived harm of vaping, having a favorite tobacco ad.
Weighted by inverse probability of treatment and censoring weights to adjust for bias due to time-dependent confounding and selection bias due to lost to follow-up.
Former use defined as ever using e-cigarettes, but not in the past 30-days at the wave immediately prior to the outcome.
Current use defined as ever using e-cigarettes and used in the past 30-days at the wave immediately prior to the outcome.
Frequency defined as the number of days e-cigarette were used in the past 30-days at the wave immediately prior to the outcome. Models restricted to youth who ever initiated e-cigarettes.
E-cigarette use and Smoking Initiation: Current Smoking Outcome
Table 3 presents results from marginal structural models and traditional models for the current smoking outcome. Prior to accounting for time-dependent confounding, baseline-adjusted RRs were 2.9 (95% CI: 2.5–3.3) for ever e-cigarette use, 3.8 (95% CI: 3.1–4.6) for current e-cigarette use, and 2.6 (95% CI: 2.2–3.1) for former e-cigarette use relative to never e-cigarette use. In weighted marginal structural models, RRs attenuated to 2.5 (95% CI: 2.2–2.9) for ever e-cigarette use, 3.4 (95% CI: 2.8–4.2) for current e-cigarette use, and 2.3 (95% CI: 1.9–2.7) for former e-cigarette use. In marginal structural models, initiating non-tobacco flavored e-cigarettes was associated with 2.6 (95% CI: 2.2–3.0) times the risk, and initiating tobacco-flavored e-cigarettes was associated with 2.3 (95% CI: 1.5–3.5) times the risk of initiating current smoking, relative to never e-cigarette use. Among youth who ever initiated e-cigarettes, marginal structural model-adjusted RRs for current smoking initiation were 1.9 (95% CI: 1.5–2.6) for vaping ≥3 days and 1.3 (95% CI: 0.92–1.8) for vaping 1-2 days compared to vaping 0 days in the past 30-days.
Table 3.
Youth e-cigarette use and current cigarette smoking initiation: Baseline-adjusted and marginal structural model discrete-time regression results
| Crudea | Unweighted Baseline- Adjustedb |
MSMb,c | ||||||
|---|---|---|---|---|---|---|---|---|
| Time-varying e-cigarette use | No. youth initiatingcurrent smoking |
Total person- waves |
RR | 95% CI | RR | 95% CI | RR | 95% CI |
| Never use | 546 | 20,569 | 1.0 | REF | 1.0 | REF | 1.0 | REF |
| Ever use | 371 | 3,117 | 4.0 | 3.5-4.6 | 2.9 | 2.5-3.3 | 2.5 | 2.2-2.9 |
| Former used | 243 | 2,310 | 3.6 | 3.1-4.2 | 2.6 | 2.2-3.1 | 2.3 | 1.9-2.7 |
| Current usee | 128 | 807 | 5.3 | 4.4-6.5 | 3.8 | 3.1-4.6 | 3.4 | 2.8-4.2 |
| Tobacco flavored | 25 | 256 | 3.7 | 2.5-5.5 | 2.6 | 1.7-3.9 | 2.3 | 1.5-3.5 |
| Non-Tobacco flavored | 346 | 2,861 | 4.1 | 3.5-4.7 | 3.0 | 2.6-3.4 | 2.6 | 2.2-3.0 |
| E-cigarette frequencyf | ||||||||
| 0 days | 257 | 2,431 | 1.0 | REF | 1.0 | REF | 1.0 | REF |
| 1-2 days | 51 | 352 | 1.4 | 1.0-1.9 | 1.4 | 1.0-1.9 | 1.3 | 0.92-1.8 |
| ≥3 days | 63 | 334 | 1.8 | 1.4-2.4 | 1.7 | 1.3-2.3 | 1.9 | 1.5-2.6 |
CI indicates confidence interval, MSM marginal structural model, RR risk ratio.
Model includes time-varying exposure and time-specific intercept
Model includes time-varying exposure, time-specific intercept, and wave 1 values of age, sex, race/ethnicity, parental education, living with tobacco user, grades, externalizing mental health, alcohol, marijuana, and other tobacco use (past 12-months), cigarette susceptibility, perceived harm of vaping, having a favorite tobacco ad.
Weighted by inverse probability of treatment and censoring weights to adjust for bias due to time-dependent confounding and selection bias due to lost to follow-up.
Former use defined as ever using e-cigarettes, but not in the past 30-days at the wave immediately prior to the outcome.
Current use defined as ever using e-cigarettes and used in the past 30-days at the wave immediately prior to the outcome.
Frequency defined as the number of days e-cigarette were used in the past 30-days at the wave immediately prior to the outcome. Models restricted to youth who ever initiated e-cigarettes.
Secondary and Sensitivity Analyses
Sample-weighted marginal structural model estimates did not change appreciably compared to estimates without PATH survey sample weights (Table 4). The absolute number of cigarette-naïve youths at wave 2 who initiated cigarette smoking by wave 5 at the US population level was estimated to be 3,228,524. Assuming internal validity, the estimated number of youths who initiated cigarette smoking attributable to prior e-cigarette initiation over the two-year follow-up period was 554,153 (95% CI: 395,366-704,040; PAF=17%, 95% CI: 12%-22%).
Table 4.
Youth e-cigarette use and cigarette smoking initiation: Adjusted and marginal structural model discrete-time logistic regression results weighted by PATH wave 2 survey sample weights
| Sample-weighted Baseline-Adjusteda | Sample-weighted MSMb | |||
|---|---|---|---|---|
| Time-varying e-cigarette use | OR | 95% CI | OR | 95% CI |
| Never use | 1.0 | REF | 1.0 | REF |
| Ever use | 3.2 | 2.7-3.7 | 2.8 | 1.8-4.3 |
| Former usec | 2.8 | 2.4-3.3 | 2.4 | 1.6-3.8 |
| Current used | 4.3 | 3.5-5.4 | 4.6 | 3.7-5.8 |
| Tobacco flavored | 2.8 | 1.8-4.3 | 2.7 | 1.7-4.2 |
| Non-Tobacco flavored | 3.2 | 2.7-3.8 | 2.8 | 1.7-4.4 |
| E-cigarette frequencye | ||||
| 0 days | 1.0 | REF | 1.0 | 1.0 |
| 1-2 days | 1.4 | 1.0-1.8 | 1.3 | 0.98-1.8 |
| ≥3 days | 1.9 | 1.3-2.7 | 2.1 | 1.4-3.2 |
CI indicates confidence interval, MSM marginal structural model, OR odds ratio.
All models include time-varying exposure, time-specific intercept, and wave 1 values of age, sex, race/ethnicity, parental education, living with tobacco user, grades, externalizing mental health, alcohol, marijuana, and other tobacco use (past 12-months), cigarette susceptibility, perceived harm of vaping, having a favorite tobacco ad. Sample-weighted odds ratios approximate sample-weighted risk ratios under the rare disease assumption (risk of smoking initiation=7%).
Estimates weighted by the PATH wave 2 sample weights.
Estimates weighted by the product of PATH wave 2 sample weights and inverse probability of treatment and censoring weights.
Former use is defined as ever using e-cigarettes, but not in the past 30-days at the wave immediately prior to the outcome.
Current use defined as ever using e-cigarettes and used in the past 30-days at the wave immediately prior to the outcome.
Frequency defined as the number of days e-cigarette were used in the past 30-days at the wave immediately prior to the outcome. Models restricted to youth who ever initiated e-cigarettes.
RRs corrected for non-differential exposure misclassification ranged from 2.4 (<1% bias) to 5.2 (54% bias) (eTable 5). RRs corrected for differential outcome misclassification ranged from 1.6 (50% bias) to 4.3 (56% bias) when outcome specificity was set to 1.0 in both exposed and unexposed (eTable 6), and 2.4 (<1% bias) to 5.4 (56% bias) when specificity was reduced to 0.95 for exposed and unexposed (eTable 7). When correcting for exposure and outcome misclassification simultaneously, corrected ORs ranged from 2.3 (<5% bias) to 6.4 (63% bias) (eTables 8-9). Bias analyses indicated that most scenarios of non-differential exposure and differential outcome misclassification expect to bias observed associations towards the null. Imperfect specificity induced more bias than imperfect sensitivity.
Discussion
In the current study, we estimated the association between time-varying e-cigarette initiation and subsequent cigarette smoking initiation among US youth who had never used e-cigarettes or combustible cigarettes at baseline. Our study confirmed that youth who initiated e-cigarettes were more likely to subsequently initiate combustible cigarette smoking than youth who never initiated e-cigarettes. The association persisted after adjustment for time-dependent confounding, selection bias, and exposure/outcome misclassification, and was slightly stronger for more recent e-cigarette use and greater vaping frequency. There was little difference in risk of smoking initiation between youth who initiated non-tobacco flavored vs. tobacco-flavored e-cigarettes. Models that did not adjust for time-dependent confounding yielded slightly overestimated associations.
The association between vaping and cigarette smoking initiation appeared stronger for youth who vaped ≥3 days/month (versus <3 days/month). Frequency is an important consideration when studying the effect of vaping on tobacco use, as well as other substance use behaviors. More frequent vaping is associated not only with more frequent cigarette smoking43,44 but also greater risk of binge drinking and cannabis use in youth.45 Few studies have examined the differential association of vaping frequency with smoking initiation among youth. Among adults, vaping daily (vs. non-daily) may be more effective for cigarette smoking cessation,46,47 but also contribute to longer-term vaping dependence.48 Data from this and prior studies43-47 highlight the importance of distinguishing between frequency of e-cigarette use in epidemiologic studies on vaping.
E-cigarette flavorings were not meaningfully associated with risk of cigarette smoking initiation in this study. Availability of flavored e-liquids increases the appeal of e-cigarettes to youth.49 Youth who vape flavored e-cigarettes are more susceptible to continued regular vaping and report greater susceptibility to cigarette smoking than those who vape tobacco flavors.50 However, a recent PATH study similarly found that flavored e-cigarette use (vs. tobacco flavored e-cigarette use) was not associated with increased risk of cigarette smoking initiation.51 While this and prior studies did not find differences in smoking initiation by e-cigarette flavors, flavored e-liquids may increase initiation of youth vaping,50 and have additional implications for product toxicity.8
We estimated approximately 550,000 youth in the US initiated cigarette smoking as a result of e-cigarette initiation over three-years of follow-up during the study period (2014–2019). In a prior PATH study, Berry et al. estimated 180,000 youth initiated cigarette smoking after e-cigarette initiation between 2013–2016.52 Given that population-level absolute estimates are a function of the total number of youth who initiated cigarette smoking over the time period, and thus highly influenced by length of follow-up and other study design decisions (e.g., sample inclusion criteria), the PAF percentage value is more comparable across studies. Berry et al. estimated a PAF of 21%, which falls within the PAF confidence limit range of the current study (12%-22%). It is reassuring that the two sets of results are highly consistent, and both the current study and that by Berry et al. indicate that a substantial proportion of cigarette smoking initiation among US youth may be attributable to prior nicotine vaping. It is important to consider that e-cigarettes may have prevented some youth from initiating cigarette smoking (i.e., acted as a substitute among youth interested in tobacco). Whether vaping caused a greater number of new smokers compared to a counterfactual world with no e-cigarettes would likely depend on several factors, including the vaping prevalence among youth who would otherwise not have used any tobacco products in their absence.
There are limitations to our study. Results should only be interpreted causally under assumptions of exchangeability, consistency, positivity, and correct model specification (and assuming no other sources of bias).37 Although models adjusted for a number of time-invariant and time-varying confounders, the possibility of unmeasured confounding (i.e., non-exchangeability) cannot be ruled out, for example by factors such as peer influence that were not measured in PATH.53 Similarly, the population-level estimate assumes a causal relationship and no bias. Although weights accounted for selection bias due to dropout, if youth who were included in the study at baseline were more or less likely to initiate e-cigarettes and cigarette smoking than youth not included at baseline, this may be a source of selection bias not accounted for in the analysis.21 Misclassification probabilities addressed in the bias analysis were assumed to be independent; however, exposure and outcome data were collected from the same survey and dependent misclassification is possible.54,55 Incorrect misclassification assumptions can lead to bias-corrected estimates further from the truth than the original misclassified estimate.56 There may be e-cigarette device characteristics that differentially affect likelihood of smoking initiation that were not investigated. For example, concentration and type of nicotine (e.g., free-base vs. nicotine salts) likely plays an important role in nicotine dependence among youth. Finally, results do not provide information on whether youth become regular cigarette smokers after initiation.
Conclusion
A strong association between e-cigarette use and combustible cigarette smoking in the PATH survey population persisted after adjustment for time-dependent confounding and selection bias due to dropout using marginal structural models with inverse probability of treatment and censoring weights. The association between e-cigarette initiation and smoking initiation appeared strongest for more recent and frequent users. Results from bias analyses indicate misclassification may be a bigger concern to study validity than time-dependent confounding. However, even the most extreme bias analysis results supported a strong positive association. The findings are therefore consistent with the preponderance of evidence that vaping nicotine may be one cause of subsequent combustible cigarette smoking initiation among US youth.
Supplementary Material
Source of funding:
This work was supported by grant U54HL120163 from the National Heart, Lung and Blood Institute and FDA Center for Tobacco Products.
Footnotes
Conflicts of Interest: None declared
Data availability:
SAS code is provided in the supplementary material. The data used in this study are publicly available through the University of Michigan National Addiction and HIV Data Archive Program (NAHDAP).
References
- 1.Gentzke AS, Creamer M, Cullen KA, et al. Vital Signs: Tobacco Product Use Among Middle and High School Students — United States, 2011–2018. MMWR Morbidity and Mortality Weekly Report. 2019;68(6):157–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang TW, Neff LJ, Park-Lee E, Ren C, Cullen KA, King BA. E-cigarette Use Among Middle and High School Students — United States, 2020. MMWR Morbidity and Mortality Weekly Report. 2020;69(37):1310–1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cullen KA, Ambrose BK, Gentzke AS, Apelberg BJ, Jamal A, King BA. Notes from the Field: Use of Electronic Cigarettes and Any Tobacco Product Among Middle and High School Students — United States, 2011–2018. MMWR Morbidity and Mortality Weekly Report. 2018;67(45):1276–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.England LJ, Bunnell RE, Pechacek TF, Tong VT, McAfee TA. Nicotine and the Developing Human: A Neglected Element in the Electronic Cigarette Debate. American Journal of Preventive Medicine. 2015;49(2):286–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jacobsen LK, Krystal JH, Mencl WE, Westerveld M, Frost SJ, Pugh KR. Effects of smoking and smoking abstinence on cognition in adolescent tobacco smokers. Biological Psychiatry. 2005;57(1):56–66. [DOI] [PubMed] [Google Scholar]
- 6.Musso F, Bettermann F, Vucurevic G, Stoeter P, Konrad A, Winterer G. Smoking impacts on prefrontal attentional network function in young adult brains. Psychopharmacology. 2007;191(1):159–169. [DOI] [PubMed] [Google Scholar]
- 7.Kosmider L, Sobczak A, Fik M, et al. Carbonyl compounds in electronic cigarette vapors: Effects of nicotine solvent and battery output voltage. Nicotine and Tobacco Research. 2014;16(10):1319–1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fetterman JL, Weisbrod RM, Feng B, et al. Flavorings in Tobacco Products Induce Endothelial Cell Dysfunction. Arteriosclerosis, Thrombosis, and Vascular Biology. 2018;38(7):1607–1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fernández E, Ballbè M, Sureda X, Fu M, Saltó E, Martínez-Sánchez JM. Particulate Matter from Electronic Cigarettes and Conventional Cigarettes: a Systematic Review and Observational Study. Current environmental health reports. 2015;2(4):423–429. [DOI] [PubMed] [Google Scholar]
- 10.Zhao D, Aravindakshan A, Hilpert M, et al. Metal/Metalloid Levels in Electronic Cigarette Liquids, Aerosols, and Human Biosamples: A Systematic Review. Environmental Health Perspectives. 2020;128(3):036001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheng T Chemical evaluation of electronic cigarettes. Tobacco control. 2014;23(suppl 2):ii11–ii17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Academies of Sciences Engineering and Medicine. Public Health Consequences of E-Cigarettes. (Stratton K, Kwan LY, Eaton DL, eds.). National Academies Press; 2018. [PubMed] [Google Scholar]
- 13.Schneider S, Diehl K. Vaping as a Catalyst for Smoking? An Initial Model on the Initiation of Electronic Cigarette Use and the Transition to Tobacco Smoking Among Adolescents. Nicotine & Tobacco Research. 2016;18(5):647–653. [DOI] [PubMed] [Google Scholar]
- 14.Soneji S, Barrington-Trimis JL, Wills TA, et al. Association Between Initial Use of e-Cigarettes and Subsequent Cigarette Smoking Among Adolescents and Young Adults. JAMA Pediatrics. 2017;171(8):788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chan GCK, Stjepanović D, Lim C, et al. Gateway or common liability? A systematic review and meta-analysis of studies of adolescent e-cigarette use and future smoking initiation. Addiction. 2021;116(4):743–756. [DOI] [PubMed] [Google Scholar]
- 16.Khouja JN, Suddell SF, Peters SE, Taylor AE, Munafò MR. Is e-cigarette use in non-smoking young adults associated with later smoking? A systematic review and meta-analysis. Tobacco Control. 2021;30(1):8–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levy DT, Warner KE, Michael Cummings K, et al. Examining the relationship of vaping to smoking initiation among US youth and young adults: A reality check. Tobacco Control. 2019;28(6):629–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hernán MA, Hernández-Díaz S. Beyond the intention to treat in comparative effectiveness research. Clinical trials (London, England). 2012;9(1):48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hernán MA, Robins JM. Causal Inference: What If. Published online 2020. Accessed January 4, 2022. https://www.hsph.harvard.edu/miguel-hernan/causal-inference-book/
- 20.Robins JM, Hernán MA, Brumback B. Marginal Structural Models and Causal Inference in Epidemiology. Epidemiology. 2000;11(5):550–60. [DOI] [PubMed] [Google Scholar]
- 21.Hernán M, Hernandez-Diaz S, Robins J. A Structural Approach to Selection Bias. Epidemiology. 2004;15(5):615–625. [DOI] [PubMed] [Google Scholar]
- 22.Howe CJ, Cole SR, Lau B, Napravnik S, Eron JJ Jr. Selection bias due to loss to follow up in cohort studies. Epidemiology (Cambridge, Mass). 2016;27(1):91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jurek AM, Greenland S, Maldonado G. How far from non-differential does exposure or disease misclassification have to be to bias measures of association away from the null? International Journal of Epidemiology. 2008;37(2):382–385. [DOI] [PubMed] [Google Scholar]
- 24.Hyland A, Ambrose BK, Conway KP, et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tobacco control. 2017;26(4):371–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Applebaum KM, Malloy EJ, Eisen EA. Left truncation, susceptibility, and bias in occupational cohort studies. Epidemiology. 2011;22(4):599–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hazelbag CM, Klungel OH, van Staa TP, de Boer A, Groenwold RHH. Left truncation results in substantial bias of the relation between time-dependent exposures and adverse events. Annals of Epidemiology. 2015;25(8):590–596. [DOI] [PubMed] [Google Scholar]
- 27.Sargent JD, Gabrielli J, Budney A, Soneji S, Wills TA. Adolescent smoking experimentation as a predictor of daily cigarette smoking. Drug and Alcohol Dependence. 2017;175:55–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Saddleson ML, Kozlowski LT, Giovino GA, Homish GG, Mahoney MC, Goniewicz ML. Assessing 30-day quantity-frequency of U.S. adolescent cigarette smoking as a predictor of adult smoking 14 years later. Drug and Alcohol Dependence. 2016;162:92–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Creamer MR, Everett Jones S, Gentzke AS, Jamal A, King BA. Tobacco Product Use Among High School Students — Youth Risk Behavior Survey, United States, 2019. MMWR Supplements. 2020;69(1):56–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kwon E, Seo DC, Lin HC, Chen Z. Predictors of youth e-cigarette use susceptibility in a U.S. nationally representative sample. Addictive Behaviors. 2018;82:79–85. [DOI] [PubMed] [Google Scholar]
- 31.Riehm KE, Young AS, Feder KA, et al. Mental health problems and initiation of e-cigarette and combustible cigarette use. Pediatrics. 2019;144(1):e20182935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lê Cook B, Wayne GF, Kafali EN, Liu Z, Shu C, Flores M. Trends in smoking among adults with mental illness and association between mental health treatment and smoking cessation. JAMA - Journal of the American Medical Association. 2014;311(2):172–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hoyle RH, Stephenson MT, Palmgreen P, Lorch EP, Donohew RL. Reliability and validity of a brief measure of sensation seeking. Personality and individual differences. 2002;32(3):401–414. [Google Scholar]
- 34.Jones CP. Invited Commentary: “Race,” Racism, and the Practice of Epidemiology. American Journal of Epidemiology. 2001;154(4):299–304. [DOI] [PubMed] [Google Scholar]
- 35.Stucky BD, Edelen MO, Ramchand R. A psychometric assessment of the GAIN Individual Severity Scale (GAIN-GISS) and Short Screeners (GAIN-SS) among adolescents in outpatient treatment programs. Journal of Substance Abuse Treatment. 2014;46(2):165–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nicksic NE, Barnes AJ. Is susceptibility to E-cigarettes among youth associated with tobacco and other substance use behaviors one year later? Results from the PATH study. Preventive Medicine. 2019;121:109–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cole SR, Hernán MA. Constructing Inverse Probability Weights for Marginal Structural Models. American Journal of Epidemiology. 2008;168(6):656–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hernán MÁ, Brumback B, Robins JM. Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men. Epidemiology. 2000;11(5):561–570. [DOI] [PubMed] [Google Scholar]
- 39.Lash T, Fox M, Fink A. Applying Quantitative Bias Analysis to Epidemiologic Data. Springer-Verlag; 2018. [Google Scholar]
- 40.Lash TL, Fox MP, MacLehose RF, Maldonado G, McCandless LC, Greenland S. Good practices for quantitative bias analysis. International Journal of Epidemiology. 2014;43(6):1969–1985. [DOI] [PubMed] [Google Scholar]
- 41.Hanley JA. A heuristic approach to the formulas for population attributable fraction. J Epidemiol Community Health. 2001;55:508–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Greenland S Re: “Confidence Limits Made Easy: Interval Estimation Using a Substitution Method”. American Journal of Epidemiology. 1999;149(9):884. [DOI] [PubMed] [Google Scholar]
- 43.Leventhal AM, Stone MD, Andrabi N, et al. Association of e-cigarette vaping and progression to heavier patterns of cigarette smoking. JAMA. 2016;316(18):1918–1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Doran N, Brikmanis K, Petersen A, et al. Does e-cigarette use predict cigarette escalation? A longitudinal study of young adult non-daily smokers. Preventive Medicine. 2017;100:279–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McCabe SE, West BT, Veliz P, Boyd CJ. E-cigarette Use, Cigarette Smoking, Dual Use, and Problem Behaviors Among U.S. Adolescents: Results From a National Survey. Journal of Adolescent Health. 2017;61(2):155–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Berry KM, Reynolds LM, Collins JM, et al. E-cigarette initiation and associated changes in smoking cessation and reduction: the Population Assessment of Tobacco and Health Study, 2013-2015. Tobacco control. 2019;28(1):42–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brose LS, Hitchman SC, Brown J, West R, McNeill A. Is the use of electronic cigarettes while smoking associated with smoking cessation attempts, cessation and reduced cigarette consumption? A survey with a 1-year follow-up. Addiction (Abingdon, England). 2015;110(7):1160–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Harlow A, Fetterman J, Robertson R, Ross C, Benjamin E, Stokes A. Association of Device Type, Flavours, and Vaping Behaviour with Tobacco Product Transitions among Adult Electronic Cigarette Users in the United States. Tobacco Control. 2021; Published Online First: 21 January 2021. doi: 10.1136/tobaccocontrol-2020-055999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cullen KA, Gentzke AS, Sawdey MD, et al. e-Cigarette Use among Youth in the United States, 2019. JAMA. 2019;322(21):2095–2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Leventhal AM, Goldenson NI, Cho J, et al. Flavored e-cigarette use and progression of vaping in adolescents. Pediatrics. 2019;144(5):e20190789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Friedman AS, Xu S. Associations of Flavored e-Cigarette Uptake With Subsequent Smoking Initiation and Cessation. JAMA Network Open. 2020;3(6):e203826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Berry KM, Fetterman JL, Benjamin EJ, et al. Association of Electronic Cigarette Use With Subsequent Initiation of Tobacco Cigarettes in US Youths. JAMA network open. 2019;2(2):e187794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Urberg KA, Luo Q, Pilgrim C, Degirmencioglu SM. A two-stage model of peer influence in adolescent substance use: Individual and relationship-specific differences in susceptibility to influence. Addictive Behaviors. 2003;28(7):1243–1256. [DOI] [PubMed] [Google Scholar]
- 54.Kristensen P Bias from nondifferential but dependent misclassification of exposure and outcome. Epidemiology (Cambridge, Mass). 1992;3(3):210–215. [DOI] [PubMed] [Google Scholar]
- 55.Brooks DR, Getz KD, Brennan AT, Pollack AZ, Fox MP. The Impact of Joint Misclassification of Exposures and Outcomes on the Results of Epidemiologic Research. Current Epidemiology Reports. 2018;5(2):166–174. [Google Scholar]
- 56.Johnson CY, Flanders WD, Strickland MJ, Honein MA, Howards PP. Potential Sensitivity of Bias Analysis Results to Incorrect Assumptions of Nondifferential or Differential Binary Exposure Misclassification. Epidemiology. 2014;25(6):902–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
SAS code is provided in the supplementary material. The data used in this study are publicly available through the University of Michigan National Addiction and HIV Data Archive Program (NAHDAP).


