Abstract
Body composition algorithms are typically validated using multi-ethnic populations without accounting for ethnicity. This might be problematic when using multi-frequency bioimpedance analysis (MF-BIA) for Hispanics. Group error (i.e., constant error [CE]), individual error (i.e., 95% limits of agreement [LOAs]), and proportional bias of MF-BIA were determined in Hispanic men and women (n = 84 and 97, respectively) when using dual energy X-ray absorptiometry (DXA) as a reference method. Due to the lack of an ethnic-specific impedance equation for Hispanics, it was hypothesized that MF-BIA would be biased when compared to DXA. For body fat percent (BF%), MF-BIA displayed similar CE±95% LOA for the sample (−3.17±5.45%), males (−3.2±5.5%), and females (−3.2±5.4%) compared to DXA. However, moderate proportional bias was present for females (r=0.48). The sample (r=0.22) and males (r=−0.04) had trivial-to-no proportional bias. Regarding fat mass (FM), MF-BIA exhibited CE±95% LOA values of −1.4±4.2 kg for the sample, −1.9±4.6 kg for males, and −0.9±3.6 kg for females. There was strong proportional bias for females (=0.68) and moderate bias for the sample (r=0.36). No proportional bias was observed for males (r=−0.02). For fat-free mass (FFM), males demonstrated the largest CE±95% LOA (1.6±4.6), compared to the sample (1.2±3.9 kg) and females (0.9±3.4 kg) when MF-BIA was compared to DXA. No proportional biases existed for the sample (r=−0.01) or males (r=−0.10). However, females exhibited a moderate, negative bias (r=−0.38). Due to the observed moderate-to-strong proportional biases within body composition estimates, the need for ethnic-specific algorithms is warranted, particularly for the Hispanic female population.
Keywords: Body Fat, DEXA, dual-energy x-ray absorptiometry, bioelectrical impedance analysis, BIA
Visual Abstract
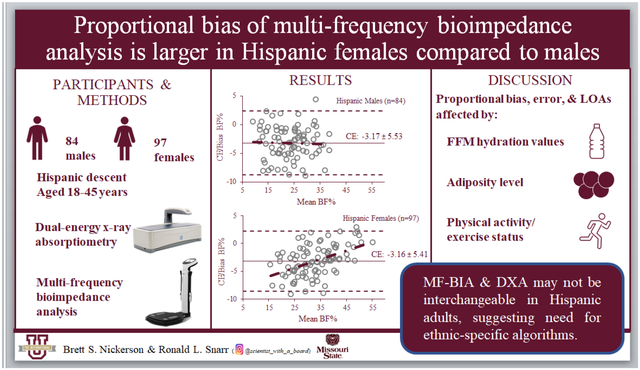
DXA = Dual-energy x-ray absorptiometry; MF-BIA = Multi-frequency bioimpedance analysis; FFM = Fat-free mass; BF% = Body fat percentage; CE = Constant Error; The middle solid lines on the scatterplots indicate CE. The dashed lines represent the upper and lower limits of agreement (± 1.96 SD). The dashed-dotted regression lines represent the proportional bias.
1. Introduction
Dual energy X-ray absorptiometry (DXA) is an imaging-based body composition method that has traditionally served as the “reference standard” for diagnosis of osteoporosis [1–3]. Nonetheless, the ability of DXA to quantify fat-free mass (FFM), fat mass (FM), and body fat (BF%) has led to widespread use in clinical and research settings [4–6]. Despite the multiple body composition metrics computed by DXA, issues may arise when attempting to complete body composition assessments with the device. For instance, the use of DXA in females that are pregnant or seeking to become pregnant should be avoided due to the small quantity of radiation exposure. Radiation, albeit small, also limits the number of scans that should be conducted via DXA in a year, especially when considering recent radiation exposure from other clinical devices such as magnetic resonance imaging and computed tomography [7]. Finally, the cost of acquiring and maintaining a DXA machine can be problematic for clinics and laboratories operating with a limited budget. Consequently, alternative methods such as multi-frequency bioimpedance analysis (MF-BIA) can be used as a surrogate of DXA in these circumstances.
Bioimpedance devices are designed to estimate the water content of FFM, which can then be used to solve for other body composition metrics such as FM and BF%. One limitation of bioimpedance technology is that it assumes the water content of FFM is constant (73%) for all individuals, regardless of race/ethnicity [8]. This might be problematic when testing a Hispanic population since previous research has shown that Hispanic males and females possess less water content in their FFM (72.00 and 71.88%, respectively) than the assumed constant of 73% [9], which was observed over 5 decades ago in cadavers [10]. In addition, many of the commercially available bioimpedance devices have been developed with proprietary algorithms. Consequently, study sample characteristics are not disclosed. Notably, commercial devices require inputting descriptive variables such as height and weight, but do not include a measure of race/ethnicity. This serves as an area of concern since the water content of FFM is significantly different between Hispanics and non-Hispanic Caucasians as previously referenced [9, 11]. Due to previous findings, it was hypothesized that MF-BIA (InBody 570) would be biased when compared to DXA. Therefore, the purpose of this study was to determine the agreement between DXA and MF-BIA for estimating BF%, FM, and FFM in a Hispanic population.
2. Methods and materials
2.1. Participants
One-hundred eighty-one individuals (males: n=84; females: n=97) of Hispanic descent had body composition estimated via DXA and MF-BIA. Recruitment occurred via flyers, word of mouth, and classroom recruitment. Inclusion criteria consisted of Hispanic females and males that were: 1). 18 – 45 years of age and apparently healthy (i.e., free from orthopedic disorders and who had no known signs or symptoms of cardiovascular, pulmonary, or metabolic diseases); 2). < 158.76 kg due to DXA table restrictions; and 3). did not have conditions or take medications that may affect body composition. Participants were asked to complete an overnight fasting protocol, which consisted of not eating or drinking 8 hours prior to participation and to also avoid exercise 24 h before testing. Prior to testing, participants provided written informed consent and a completed a self-reported medical history questionnaire to ensure inclusion criteria were met. Institutional review board approval for subject participation was approved by the host university (IRB # 2016-10-16).
2.2. Procedures
Upon completion of the informed consent and medical history questionnaire, participants’ hydration status was assessed from a urine sample using a handheld refractometer. Urine specific gravity (USG) values < 1.029 were required for inclusion in this analysis [12]. After assessing hydration, height was measured (to the nearest 0.1cm) with a stadiometer that has a maximum capacity of 205 cm (SECA 213, Seca Ltd., Hamburg, Germany).
2.3. Multi-Frequency Bioimpedance Analysis
Subjects first had BF%, FFM, and FM measured with MF-BIA based upon manufacturer’s instructions (InBody 570, InBodyUSA, Cerritos, CA). The MF-BIA device employed in the current study utilized a tetrapolar 8-point tactile electrode system, which sends three frequencies (i.e., 5, 50, and 500 kHz) of alternating currents through the body. For testing, subjects’ feet were centered on the electrodes and the hand electrodes were grasped with arms being held wide enough so there was no contact between the arms and torso. The position was held for the duration of the test (approximately 45 seconds). Once the assessment was completed, participants were prompted to return the hand electrodes and step off the device.
2.4. Dual Energy X-ray Absorptiometry
Next, subjects had their BF%, FFM, and FM measured with DXA (GE Lunar Prodigy, Madison, WI). The DXA machine was calibrated according to the manufacturer’s instructions via a standard calibration block prior to each scan. The DXA quality control procedures were followed according to manufacturer guidelines. All subjects reported to the laboratory and were asked to remove any metal objects (e.g., jewelry, coins, etc.). Volunteers wore light cotton clothing free from metal during the scan and were instructed to lie supine on the scanning bed with hands by their sides in a neutral position. During body scans, subjects were asked to remain motionless, while Velcro straps were situated around the ankles and knees. Scans lasted approximately 6 to 10 min. The same researcher positioned all participants on the DXA scanning bed. In addition, the trained researcher analyzed each scan to adjust software-determined regions of interest prior to producing the body composition reports.
2.5. Statistical Analyses
All statistical analyses were performed using IBM SPSS Statistics v. 28.0 (IBM Corp., Armonk, NY) and data visualizations created using Microsoft Excel (Microsoft Corp., Redmond, WA). Prior to analysis, normality of the data were assessed using Shapiro-Wilks tests, skewness, kurtosis, and histogram analyses. BF%, FM, and FFM values obtained from DXA and MF-BIA were compared via paired samples t-tests. The magnitude of the mean differences were assessed using Cohen’s d statistics [13] and evaluated with Hopkins’ effect size scale [14]. The scale for effect sizes was 0 to <0.2 for trivial, 0.2 to <0.6 for small, 0.6 to <1.2 for moderate, 1.2 to <2.0 for large, and ≥2.0 for very large.
Agreement within BF%, FM, and FFM, between lab measures, was assessed using intraclass correlation coefficients (ICC), standard error of the estimate (SEE), and constant error (CE). Additionally, Bland-Altman analyses [15] and linear regression modeling (enter method) were used to identify the 95% limits of agreement (LOA) and proportional bias for BF%, FM, and FFM. Proportional biases were determined by the estimated slope of the regression line. A slope of 0 would indicate no proportional bias. The strength of association between outcome variables (ICC), as estimated by DXA and MF-BIA, used a scale of 0 to 0.19 as very weak-to-no association, 0.20 to 0.39 as weak, 0.40 to 0.59 as moderate, 0.60 to 0.79 as strong, and 0.80 to 1.00 as very strong-to-perfect [14, 15]. All analyses were performed for the entire sample, as well as factored by sex. Alpha levels were set a priori at a value of <0.05. Values for all outcome variables are displayed as mean ± standard deviation
3. Results
All individuals completed both the DXA and MF-BIA measurements (n = 181). After checks for normality, data were deemed parametric. No data were excluded prior to analysis for any group or by sex comparisons.
3.1. Body Fat Percentage
MF-BIA mean values for BF% showed a range in CE from −3.16% (females [d=1.14]) to −3.17% (both the group [d =1.14] and males [d=1.12]) when compared to DXA (Table 1). Correlation analyses indicated near-perfect associations between both methods for the group (ICC=0.95), males (ICC=0.92), and females (ICC=0.92). The SEEs for MF-BIA ranged from 2.23% (females) to 2.81% (males), while 95% LOAs ranged from ±5.41% (females) to ±5.53% (males). Bland Altman analysis indicated a moderate proportional bias for females (r=0.48), with trivial-to-no proportional bias for the group (r=0.22) and males (r=−0.04) (Fig. 1a–c).
Table 1.
Comparison of body composition values between multi-frequency bioelectrical impedance and dual-energy x-ray absorptiometry for all subjects (n = 181).
| 95% Limits of Agreement | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | (Mean ± SD) | d | ICC | R2 | SEE | CE ± 1.96 SD | Upper | Lower | Trend |
| DXA BF% | 30.25 ± 9.06 | --- | |||||||
| InBody BF% | 27.08 ± 9.68 | 1.14 | 0.95 | 0.92 | 2.60 | −3.17 ± 5.45 | 2.28 | −8.62 | 0.22 |
| DXA FM | 21.71 ± 9.98 | --- | |||||||
| InBody FM | 20.33 ± 10.75 | 0.65 | 0.99 | 0.98 | 2.04 | −1.38 ± 4.16 | 2.78 | −5.54 | 0.36 |
| DXA FFM | 51.50 ± 12.51 | --- | |||||||
| InBody FFM | 52.72 ± 12.49 | 0.60 | 0.99 | 0.96 | 1.90 | 1.22 ± 3.99 | 5.21 | −2.77 | −0.01 |
DXA = Dual-energy x-ray absorptiometry; InBody 570 = Multi-frequency bioelectrical impedance; BF% = body fat percentage; FFM = fat-free mass; SEE = standard error of estimate; CE = constant error.
Figure 1.
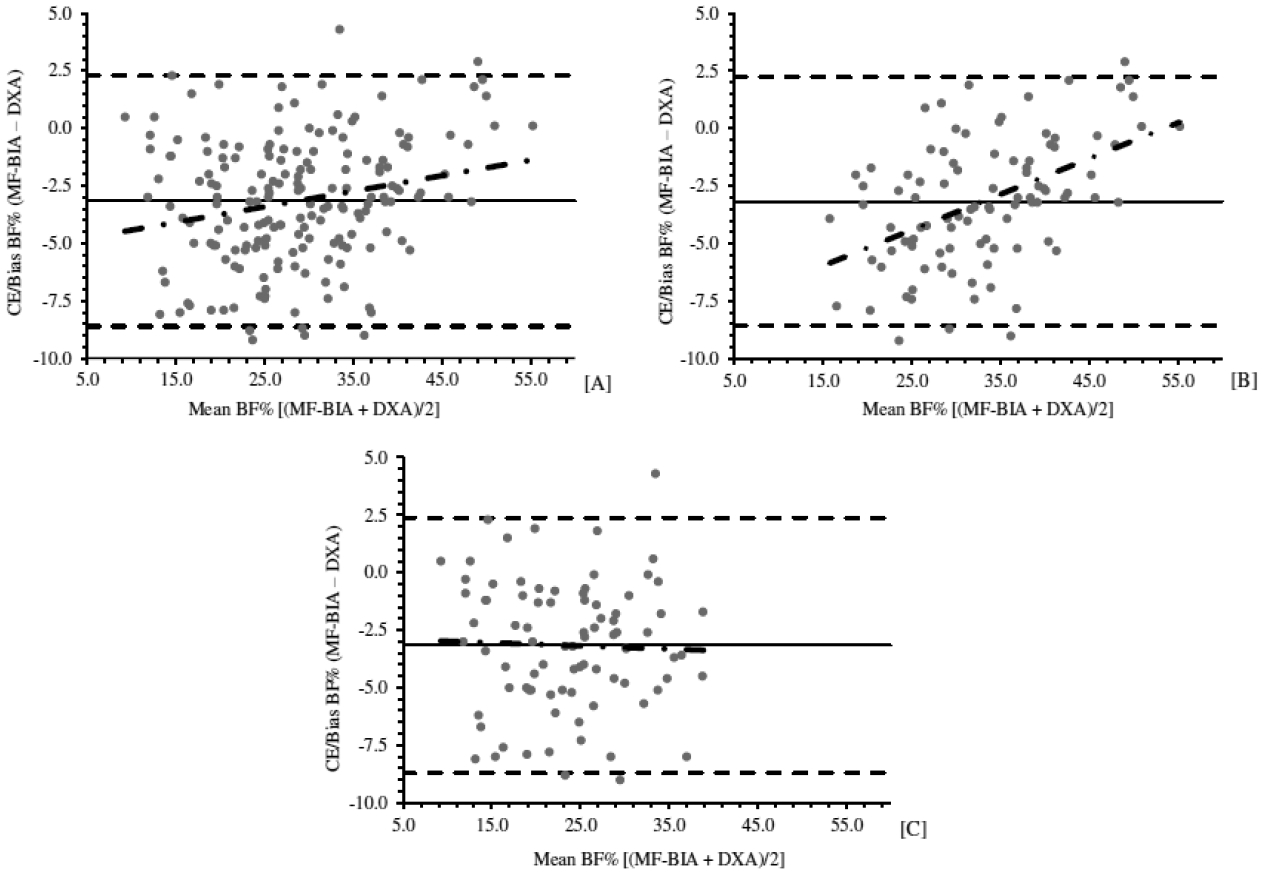
Bland and Altman plots comparing body fat percentage (BF%) between multi-frequency bioelectrical impedance analysis (MF-BIA) and dual energy x-ray absorptiometry (DXA) in Hispanic adults. [A] Entire group (n=181); [B] Females (n=97); and [C] Males (n=84). The middle solid lines indicate the constant error. The dashed lines represent the upper and lower limits of agreement (± 1.96 SD). The dashed-dotted regression lines represent the proportional bias
3.2. Fat Mass
Regarding FM, MF-BIA mean values demonstrated a range in CE from −0.98kg (females [d=0.53]) to −1.86kg (males [d=0.80]) when compared to DXA (Table 2). The 95% LOAs ranged from ±3.61kg for females to ±4.55kg for males. Correlation analyses indicated near-perfect associations between both methods for the group (ICC=0.99), males (ICC=0.97), and females (ICC=0.98). The SEEs for MF-BIA ranged from 1.28kg (females) to 2.32 kg (males). Trend analyses determined a strong proportional bias for females (r=0.68), moderate bias for the group (r=0.36), and no bias for males (r=−0.02) (Fig. 2a–c).
Table 2.
Comparison of body composition values between multi-frequency bioelectrical impedance and dual-energy x-ray absorptiometry for females (n = 97).
| 95% Limits of Agreement | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Value | (Mean ± SD) | d | ICC | R2 | SEE | CE ± 1.96 SD | Upper | Lower | Trend |
| DXABF% | 34.63 ± 8.03 | --- | |||||||
| InBody BF% | 31.47 ± 9.35 | 1.15 | 0.94 | 0.92 | 2.23 | −3.16 ± 5.41 | 2.25 | −8.57 | 0.48 |
| DXA FM | 22.61 ± 10.75 | --- | |||||||
| InBody FM | 21.64 ± 12.01 | 0.53 | 0.97 | 0.98 | 1.28 | −0.98 ± 3.61 | 2.63 | −4.59 | 0.68 |
| DXA FFM | 42.56 ± 6.84 | --- | |||||||
| InBody FFM | 43.50 ± 6.20 | 0.55 | 0.98 | 0.94 | 1.66 | 0.94 ± 3.35 | 4.29 | −2.41 | −0.38 |
DXA = Dual-energy x-ray absorptiometry; InBody 570 = Multi-frequency bioelectrical impedance; BF% = body fat percentage; FFM = fat-free mass; SEE = standard error of estimate; CE = constant error.
Figure 2.
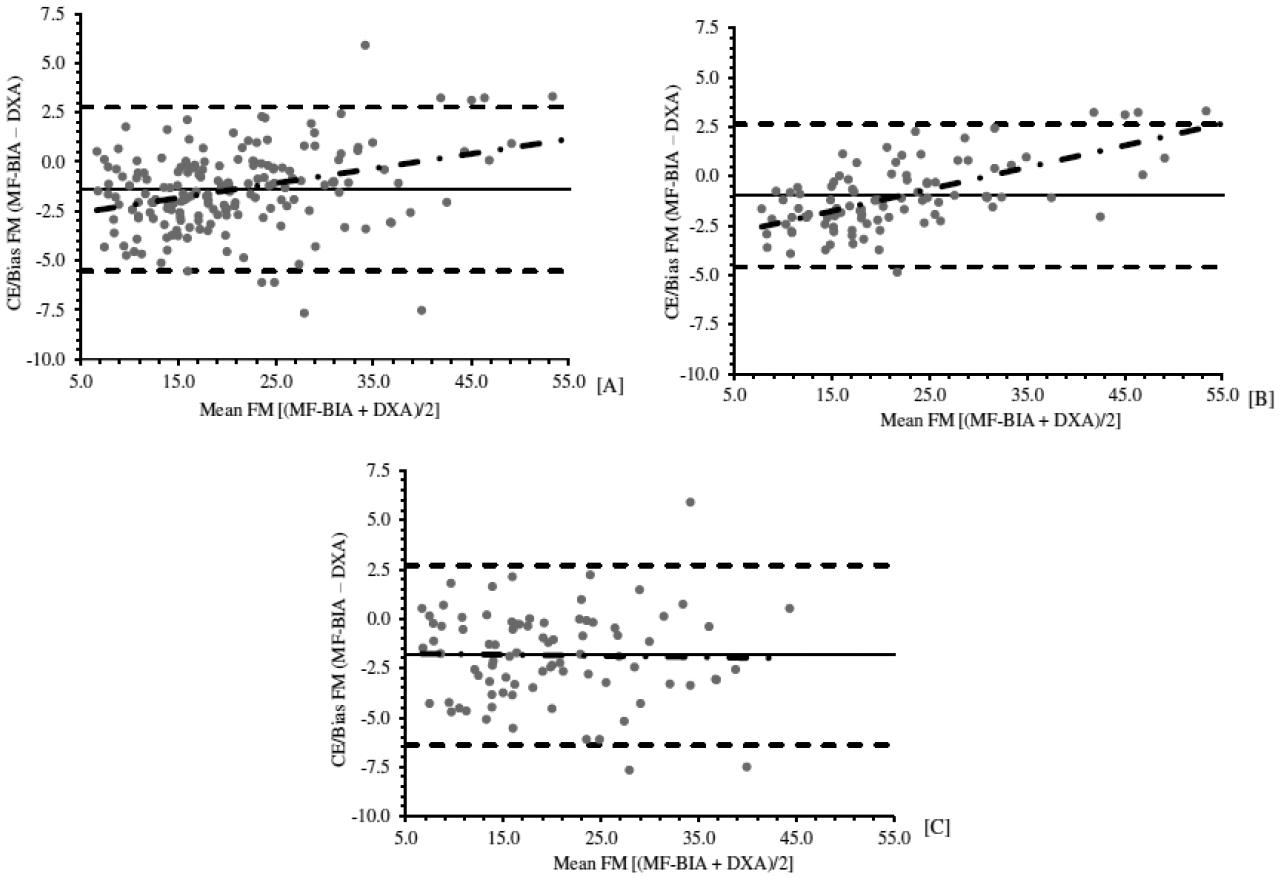
Bland and Altman plots comparing fat mass (kg) between multi-frequency bioelectrical impedance analysis (MF-BIA) and dual energy x-ray absorptiometry (DXA) in Hispanic adults. [A] Entire group (n=181); [B] Females (n=97); and [C] Males (n=84). The middle solid lines indicate the constant error. The dashed lines represent the upper and lower limits of agreement (± 1.96 SD). The dashed-dotted regression lines represent the proportional bias.
3.3. Fat-Free Mass
For FFM, males demonstrated the largest CE±95% LOA (1.6±4.6 kg), compared to the sample (1.2±3.9 kg) and females (0.9±3.4 kg) when MF-BIA was compared to DXA (Table 3). Effect sizes for mean comparisons were classified as moderate for the group (d=0.60) and males (d=0.66), while females showed a small effect (d=0.55) Near-perfect correlations were observed for the group (ICC=0.99), males (ICC=0.98), and females (ICC=0.94). Additionally, SEEs ranged from 1.66kg for females to 2.34kg for males. There was no proportional bias present within the group (r=−0.01) or males (r=−0.10); however, females exhibited a moderate, negative bias (r=−0.38) (Fig. 3a–c).
Table 3.
Comparison of body composition values between multi-frequency bioelectrical impedance and dual-energy x-ray absorptiometry for males (n = 84).
| 95% Limits of Agreement | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Value | (Mean ± SD) | d | ICC | R2 | SEE | CE ± 1.96 SD | Upper | Lower | Trend |
| DXA BF% | 25.19 ± 7.42 | --- | |||||||
| InBody BF% | 22.02 ± 7.33 | 1.12 | 0.92 | 0.86 | 2.81 | −3.17 ± 5.53 | 2.16 | −8.70 | −0.04 |
| DXA FM | 20.67 ± 8.96 | --- | |||||||
| InBody FM | 18.81 ± 8.90 | 0.80 | 0.97 | 0.93 | 2.32 | −1.86 ± 4.55 | 2.69 | −6.41 | −0.02 |
| DXA FFM | 61.81 ± 9.18 | --- | |||||||
| InBody FFM | 63.36 ± 8.95 | 0.66 | 0.98 | 0.94 | 2.34 | 1.55 ± 4.57 | 6.12 | −3.02 | −0.10 |
DXA = Dual-energy x-ray absorptiometry; InBody 570 = Multi-frequency bioelectrical impedance; BF% = body fat percentage; FFM = fat-free mass; SEE = standard error of estimate; CE = constant error
Figure 3.
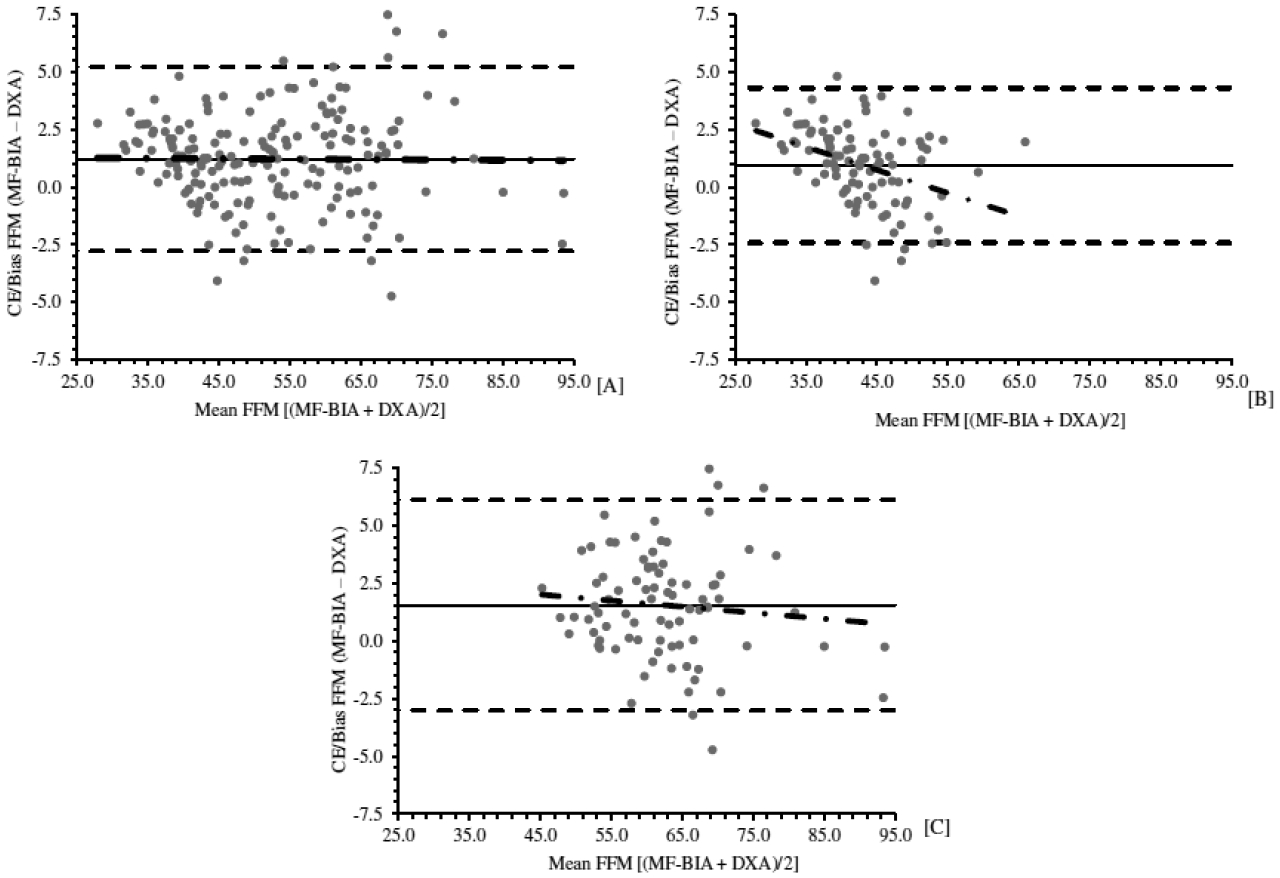
Bland and Altman plots comparing fat-free mass (kg) between multi-frequency bioelectrical impedance analysis (MF-BIA) and dual energy x-ray absorptiometry (DXA) in Hispanic adults. [A] Entire group (n=181); [B] Females (n=97); and [C] Males (n=84). The middle solid lines indicate the constant error. The dashed lines represent the upper and lower limits of agreement (± 1.96 SD). The dashed-dotted regression lines represent the proportional bias.
4. DISCUSSION
The purpose of this study was to determine the agreement between DXA and MF-BIA for estimating BF%, FM, and FFM in a Hispanic population. The current study findings demonstrate that MF-BIA systematically underestimated BF% by more than 3%, as indicated by the CEs, when compared to DXA. In contrast, the CEs revealed that MF-BIA slightly overestimates FFM values (0.9 to 1.6 kg) in a group of Hispanic adults. In addition, the proportional bias for all comparisons revealed larger correlation coefficients when evaluating Hispanic females. For instance, the moderate proportional bias of BF% for Hispanic females suggest that MF-BIA underestimates BF% in leaner individuals, when compared to DXA, and overestimates as level of body fatness increases. Altogether, the observed systematic and proportional bias suggest caution should be employing when assessing body composition with MF-BIA in Hispanics, adults, particularly when being utilized in females. Consequently, these findings support the authors original hypothesis that MF-BIA would be biased when compared to DXA.
Although research has yet to compare MF-BIA vs DXA in Hispanic adults, numerous studies have been conducted in other populations with both methods. For instance, Antonio et al. [16] revealed that MF-BIA (InBody 770) underestimated BF% and FFM in a similar fashion as the current study when compared to DXA in exercise-trained men and women. Similarly, Shafer et al. [17] found that MF-BIA underestimates BF% in men and women with a BMI classification as normal weight, but overestimates when compared to obese individuals. In addition, researchers stated the error of MF-BIA (Inbody 320) increased at higher adiposity levels [17], which may explain why proportional bias was more profound for Hispanic females than males in the current study sample, particularly when estimating FM and BF%. Collectively, the current study findings seem to be consistent with findings from Antonio et al. [16] and Shafer et al. [17].
Additional reasons for discrepancies between MF-BIA and DXA are worth further consideration. Specifically, the mean differences (CE) observed between both methods could be related to the reference method used for analysis. For instance, Nickerson et al. [18] revealed that DXA systematically overestimates BF% approximately 4% in young adults when compared to a 5-compartment model. Similarly, Moon et al. [19] also revealed that DXA overestimated adiposity by 3.71% when compared to a 5-compartment model in female collegiate athletes. The DXA-based error in the aforementioned studies is similar to the CE values observed in the current study. Therefore, it is plausible the mean body composition values of MF-BIA are similar as a multi-compartment model. For instance, both DXA and MF-BIA quantify body composition assuming hydration comprises 73% of FFM [9]. These principles make it difficult to determine which method is more affected by the employed assumptions of soft tissue hydration. As a result, additional research is warranted in a Hispanic population.
The larger proportional bias in Hispanic females is also worth consideration. For example, Tinsley [20] revealed that single-frequency BIA exhibited larger proportional bias in women than men when compared to DXA. These findings are consistent with current study results, which observed larger proportional bias when using MF-BIA in Hispanic females. In contrasts, proportional bias was not observed between MF-BIA and DXA when evaluated in previous research by Ling et al. [21]. The discrepancies between the current study and previous findings of Ling et al. [21] could be multi-factorial. First, the current study consisted of young Hispanic adults whereas Ling et al. [21] utilized middle-aged non-Hispanic Caucasian adults. As previously mentioned, the hydration of FFM for Hispanics is lower than values observed in non-Hispanic Caucasians, which bioimpedance principles are based upon. Moreover, body composition is known to alter due to aging [22, 23]. Consequently, this may lead to different outcomes when evaluating populations that differ from the assumed hydration constants and that have varying age ranges. Secondly, the DXA model used by Ling et al. [21] differed from that of the current study. This is important to consider since previous research has shown differences in body composition measurements when using DXA devices from different manufacturers [24]. Thus, the type of DXA scanner used in past research should also be taken into consideration when comparing and contrasting results. Finally, it is possible the algorithms between the current study and Ling et al. [21] were different. Notably, the race/ethnicity of subjects does not have to entered into the MF-BIA software when calculating body composition with the current study device. As a result, there may be a need to develop an improved algorithm in the future with a larger more heterogenous sample that accounts for different races/ethnicities.
There are several limitations worth considering when interpreting results of the present study. First, the study consisted of young Hispanic adults. It’s unknown whether our results can be generalized to Hispanic children, middle-aged adults, or elderly. Secondly, the use of DXA may be viewed as a limitation due to the inability to account for variations in hydration of FFM. Accordingly, future research might seek to compare MF-BIA to a more advance multi-compartment model that is able to account for variations in FFM characteristics. Thirdly, the current study did not evaluate single-frequency bioimpedance (SF-BIA). Therefore, extrapolating present study results to SF-BIA should be avoided until further research is conducted. For instance, it is worth noting that MF-BIA devices measure impedance at 50 kHz, which is similar to SF-BIA devices. Thus, future research might seek to quantify body composition at 50 kHz for both MF-BIA and SF-BIA in order to determine if error is related to a device instead of an equation. Lastly, it is worth noting that the results of the current study should only be generalized to the MF-BIA model used in the current study (InBody 570). It is unknown whether these results would be observed in other MF-BIA devices.
In conclusion, the current study sought to determine whether MF-BIA can be used as a surrogate of DXA when compared to Hispanic males and females. Results revealed there was large group error and proportional bias when comparing MF-BIA to DXA in young Hispanic adults. In addition, the 95% LOAs were greater than ± 5.0% for males and females. Collectively, these findings suggest MF-BIA and DXA may not be interchangeable in young Hispanic adults. Moreover, the observed moderate-to-strong proportional biases, particularly for Hispanic females, suggests there may be a need for manufacturers and researchers to consider developing ethnic-specific algorithms in a Hispanic population.
Article Highlights.
Multi-frequency bioimpedance analysis (MF-BIA) has yet to be evaluated in a young Hispanic adult population
Previous research has shown the hydration of fat-free mass to differ from the constants employed in MF-BIA principles
The use of proprietary algorithms that do not account for race/ethnicity might introduce error when seeking to estimate body composition with MF-BIA
The mean differences between MF-BIA and dual energy X-ray absorptiometry were significantly different when comparing body fat percentage, fat mass, and fat-free mass
The proportional bias was largest for Hispanic females, which indicates the development of new algorithms with a more heterogenous sample of Hispanic adults may be necessary
Acknowledgement
The authors would like to extend thanks to the participants of this study and to Gabriel Perez, Andres Orozco, Isabel Delgado, Samantha Narvaez, Misael Duque and Joshua Carrillo for their efforts in the data collection of the current study.
Sources of Supports
Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number SC1GM135099. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviation List
- BF%
body fat percentage
- CE
constant error
- DXA
dual energy X-ray absorptiometry
- FFM
fat-free mass
- FM
fat mass
- LOAs
limits of agreement
- MF-BIA
multi-frequency bioelectrical impedance analysis
- SEE
standard error of estimate
- USG
urine specific gravity
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Declarations
The authors have no conflicts to declare.
REFERENCES
- [1].Nam HS, Kweon SS, Choi JS, Zmuda JM, Leung PC, Lui LY, et al. Racial/ethnic differences in bone mineral density among older women. J Bone Miner Metab 2013;31:190–8. 10.1007/s00774-012-0402-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Guijarro M, Valero C, Paule B, Gonzalez-Macias J, Riancho JA. Bone mass in young adults with Down syndrome. J Intellect Disabil Res 2008;52:182–9. 10.1111/j.1365-2788.2007.00992.x [DOI] [PubMed] [Google Scholar]
- [3].Coin A, Sergi G, Benincà P, Lupoli L, Cinti G, Ferrara L, et al. Bone mineral density and body composition in underweight and normal elderly subjects. Osteoporos Int 2000;11:1043–50. 10.1007/s001980070026 [DOI] [PubMed] [Google Scholar]
- [4].Nickerson BS, Fedewa MV, McLester CN, McLester JR, Esco MR. Development of a DXA-derived body volume equation in Hispanic adults for administering in a 4-compartment model. Br J Nutr 2020;123:1373–81. [DOI] [PubMed] [Google Scholar]
- [5].Nickerson BS, Tinsley GM, Esco MR. Validity of field and laboratory three-compartment models in healthy adults. Med Sci Sports Exerc 2019;51:1032–9. 10.1249/mss.0000000000001876 [DOI] [PubMed] [Google Scholar]
- [6].Oldroyd B, Treadgold L, Hind K. Cross Calibration of the GE Prodigy and iDXA for the Measurement of Total and Regional Body Composition in Adults. J Clin Densitom 2018;21:383–93. 10.1016/j.jocd.2017.05.009 [DOI] [PubMed] [Google Scholar]
- [7].Reinhardt M, Piaggi P, DeMers B, Trinidad C, Krakoff J. Cross calibration of two dual-energy X-ray densitometers and comparison of visceral adipose tissue measurements by iDXA and MRI. Obesity (Silver Spring) 2017;25:332–7. 10.1002/oby.21722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Moon JR. Body composition in athletes and sports nutrition: an examination of the bioimpedance analysis technique. Eur J Clin Nutr 2013;67:S54–9. 10.1038/ejcn.2012.165 [DOI] [PubMed] [Google Scholar]
- [9].Nickerson BS, Tinsley GM, Fedewa MV, Esco MR. Fat-free mass characteristics of Hispanic adults: Comparisons with non-Hispanic caucasians and cadaver reference values. Clin Nutr 2020;39:3080–5. 10.1016/j.clnu.2020.01.013 [DOI] [PubMed] [Google Scholar]
- [10].Brozek J, Grande F, Anderson JT, Keys A. Densitometric analysis of body composition: revision of some quantitative assumptions. Ann NY Acad Sci 1963;110:113–40. 10.1111/j.1749-6632.1963.tb17079.x [DOI] [PubMed] [Google Scholar]
- [11].Tinsley GM, Smith-Ryan AE, Kim Y, Blue MN, Nickerson BS, Stratton MT, et al. Fat-free mass characteristics vary based on sex, race, and weight status in US adults. Nutr Res 2020;81:58–70. 10.1016/j.nutres.2020.07.002 [DOI] [PubMed] [Google Scholar]
- [12].Armstrong LE. Assessing hydration status: the elusive gold standard. J Am Coll Nutr 2007;26:575S–84S. 10.1080/07315724.2007.10719661 [DOI] [PubMed] [Google Scholar]
- [13].Cohen J Statistical power analysis. Curr Dir Psychol Sci 1992;1:98–101. 10.1111/1467-8721.ep10768783 [DOI] [Google Scholar]
- [14].Hopkins W, Marshall S, Batterham A, Hanin J. Progressive statistics for studies in sports medicine and exercise science. Med Sci Sports Exer 2009;41:3. 10.1249/MSS.0b013e31818cb278 [DOI] [PubMed] [Google Scholar]
- [15].Bland JM, Altman D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;327:307–10. 10.1016/S0140-6736(86)90837-8 [DOI] [PubMed] [Google Scholar]
- [16].Antonio J, Kenyon M, Ellerbroek A, Carson C, Burgess V, Tyler-Palmer D, et al. Comparison of dual-energy X-ray absorptiometry (DXA) versus a multi-frequency bioelectrical impedance (InBody 770) device for body composition assessment after a 4-week hypoenergetic diet. J Funct Morphol Kinesiol 2019;4:23. 10.3390/jfmk4020023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Shafer KJ, Siders WA, Johnson LK, Lukaski HC. Validity of segmental multiple-frequency bioelectrical impedance analysis to estimate body composition of adults across a range of body mass indexes. Nutrition 2009;25:25–32. 10.1016/j.nut.2008.07.004 [DOI] [PubMed] [Google Scholar]
- [18].Nickerson B, Tinsley G. Utilization of BIA-derived bone mineral estimates exerts minimal impact on body fat estimates via multicompartment models in physically active adults. J Clin Densitom 2018;21:541–9. 10.1016/j.jocd.2018.02.003 [DOI] [PubMed] [Google Scholar]
- [19].Moon JR, Eckerson JM, Tobkin SE, Smith AE, Lockwood CM, Walter AA, et al. Estimating body fat in NCAA Division I female athletes: a five-compartment model validation of laboratory methods. Eur J Appl Physiol 2009;105:119–30. 10.1007/s00421-008-0881-9 [DOI] [PubMed] [Google Scholar]
- [20].Tinsley GM. Proportional bias between dual-energy x-ray absorptiometry and bioelectrical impedance analysis varies based on sex in active adults consuming high- and low-carbohydrate diets. Nutr Res 2017;42:85–100. 10.1016/j.nutres.2017.05.003 [DOI] [PubMed] [Google Scholar]
- [21].Ling CH, de Craen AJ, Slagboom PE, Gunn DA, Stokkel MP, Westendorp RG, et al. Accuracy of direct segmental multi-frequency bioimpedance analysis in the assessment of total body and segmental body composition in middle-aged adult population. Clin Nutr 2011;30:610–5. 10.1016/j.clnu.2011.04.001 [DOI] [PubMed] [Google Scholar]
- [22].Clark BC, Manini TM. Sarcopenia ≠ dynapenia. J Gerontol A Biol Sci Med Sci 2008;63:829–34. 10.1093/gerona/63.8.829 [DOI] [PubMed] [Google Scholar]
- [23].Proctor DN, O’Brien PC, Atkinson EJ, Nair KS. Comparison of techniques to estimate total body skeletal muscle mass in people of different age groups. Am J Physiol 1999;277:489–95. 10.1152/ajpendo.1999.277.3.E489 [DOI] [PubMed] [Google Scholar]
- [24].Soriano JM, Ioannidou E, Wang J, Thornton JC, Horlick MN, Gallagher D, et al. Pencil-beam vs fan-beam dual-energy X-ray absorptiometry comparisons across four systems: body composition and bone mineral. J Clin Densitom 2004;7:281–9. 10.1385/JCD:7:3:281 [DOI] [PubMed] [Google Scholar]


