Abstract
Rationale and Objectives:
Engaging medical students and radiology residents in research during clinically focused training in residency can be challenging. We investigated extending a substantial degree of supervised autonomy to qualified residents to engage, mentor, and manage teams of medical students and other residents in research projects, fostering a system of laddered mentoring, referred to as “Resident Managed Peer Mentoring Program”. The structure is as follows: a resident with research experience (preceptor) first identifies small-scale hypothesis driven projects which different novice learner-researchers at different levels of research background and training can undertake. The learner and preceptor then outline the learner’s deliverables and set deadlines for outcomes, with regular faculty check-ins and oversight.
Materials and Methods:
This observational study assessed the outcomes of our “Resident Managed Peer Mentoring Program” beginning November 2019. Primary outcomes were numbers of peer-reviewed publications. Secondary outcomes were: numbers of radiology physicians who participated in publication and academic rank-based analysis of publication numbers for attending radiologists before and after the intervention.
Results:
Number of peer-reviewed PubMed publications increased after our intervention (47.8%, in year-1; 167.4% in year-2). Increases also occurred in the number of radiology physicians who authored publications. The effect was largest for early career physicians.
Conclusion:
The “Resident managed peer-mentoring program” was a productive method that proved especially beneficial for students, residents, and early career physicians in our clinically focused training program. This approach may be transferable to other programs where an increase in research participation and productivity are valued.
Keywords: Education, Graduate Medical Education, Mentorship, Medical Student, Radiology, Resident, Research
BACKGROUND:
“Vertical Advisory” systems encourage medical students and resident physicians to become active as mentees and mentors. These create an effective system for providing mentorship and feedback by using an intermediate-level learner (1). Encouraging radiology research among medical students and residents can enhance their interest in radiology and increase the academic productivity of the resident and faculty mentors and the department (2, 3). Studies have shown that research trainees benefit greatly from being given clear responsibility, close supervision, timely feedback, and a degree of autonomy by their research mentor (2). Time constraints of faculty members in a clinically busy residency program can make cultivating effective faculty-student and faculty-resident collaborations challenging for scholarly activity (4). Studies have shown that many residents, especially those without aspirations for academic radiology, may only participate in a single project to fulfill the program’s and American College of Graduate Medical Education (ACGME) minimal requirements. Residents’ choice to participate in additional projects beyond minimal requirements can be greatly influenced by their relationship with their mentor on their first project (4).
Small mentoring groups composed of residents and faculty members have been shown to be valuable additions to residency training, especially in mentoring medical students with career choices (5). Winter et al. conducted an internal survey of their radiology residents and found the following barriers to resident research: time constraints, lack of interest, inadequate mentorship, and limited research training. Addressing those constraints by implementing a six-step resident-led strategic framework, residents’ research experience improved, based on their internal survey results. No research outcomes in scholarly activity were reported in this study (6). Som and colleagues at Massachusetts General Hospital implemented a resident-led medical student radiology research group. In their model, they standardized the system of recruitment for medical students as novice learners, residents as intermediate-level learners and faculty members as supervisors. They created an efficient laddered-mentoring program which required less of the faculty advisor’s time and supervision by introducing resident physicians as intermediate-level learners and mentors. In the first-six months following implementation, they saw a large enrollment with 38 participating members (14 medical students, three undergraduate students, five resident physicians and 16 faculty advisors). Through this model, students authored more than seven peer-reviewed manuscripts. The impact of this robust model on overall academic productivity of their radiology department was not studied (7). It is to be noted that this study was conducted in a “resource-rich” setting within a state-of-the art research institution, robust National Institution of Health (NIH) funding, Information technology backup, strong research interests amongst students-residents-faculty advisors and large number of research track faculty-advisors available, which may not be not be available at smaller university and community residency programs.
The classroom lecture remains the predominant model for teaching medical students and residents, which is an efficient and cost-effective way to teach large numbers of learners. Although a large volume of information can be transmitted in a 60-min didactic lecture, the learner is the passive recipient of this information. Studies have shown superior learning outcomes when students are presented with active (student-centered) lessons as compared to passive (teacher-centered) lessons, in-terms of recall and retention (8–11), emphasizing the fact that we learn best by “doing”. “Doing” a research project teaches research with active learning. Hence, taking responsibility in an actual research project would be better for learning about research than reading a text or attending a didactic presentation on research methods (5–7). Our intention was for novice researchers to learn the whole process of a research project culminating in a publication, rather than simply doing small disconnected tasks like data entry.
In this study we implemented a model of research training that used resident physicians (intermediate-level learners) as mentors, which can be easily implemented in a clinically-focused residency training program with less research funding and infrastructure. This model is referred to as “Resident-managed peer-mentoring program” in this manuscript. We hypothesize that “Resident managed peer-mentoring program” is an effective method to increase scholarly outcomes in clinically busy residency programs that value research participation and productivity.
METHODS:
Study Design:
This was an observational study designed to assess departmental research outcomes following implementation of our Resident-managed peer mentoring program. Peer-reviewed PubMed indexed publications by radiology residents and radiology faculty members were collected for four academic years, 2017 – 2021. Academic year 2017 – 2018 was defined as July 01, 2017 to June 30, 2018, and so forth. The program was implemented in November 2019 (Figure 2). We compared the PubMed indexed publications (outcomes) in academic years 2019–2020 and 2020–2021 with baseline data from academic years 2017–2018 and 2018–2019.
Figure 2:
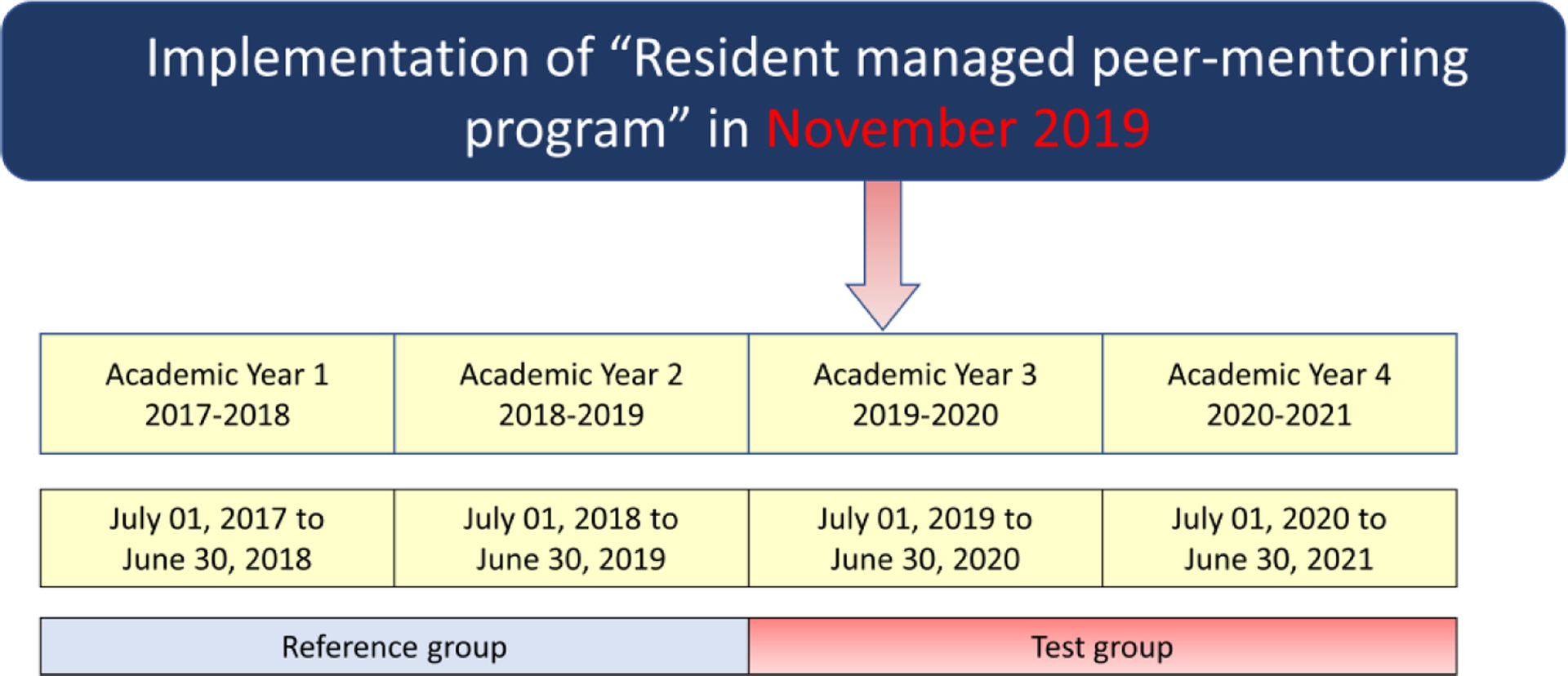
Timeline of the study outcomes.
The inclusion criteria included: Peer-reviewed PubMed Indexed publications by radiology residents and faculty members were studied for a total of four academic years, beginning before and after the intervention (Figure 2). We were able to obtain complete records of publications for radiology residents and radiology faculty members but could not get complete records of peer-reviewed publications for physicians outside of radiology and students for pre-intervention academic year. Therefore, the publication numbers by participants from outside the department of radiology were excluded from the quantitative analysis reported in this study, to avoid introducing bias.
The primary outcomes were numbers of peer-reviewed publications indexed in PubMed with authorship by radiology residents and radiology faculty members before and after the intervention. Secondary outcomes of the study included: 1) Numbers of radiology physicians (residents and faculty) who participated in publication before and after the intervention; 2) academic rank-based analysis of publication numbers for faculty advisors before and after the intervention.
Resident Managed Peer-Mentoring Program:
Our proposed model is illustrated in Figure 1. Medical students and resident physicians who are new to research, with interest in radiology research projects would be referred as novice learners. Radiology resident physician with prior research experience and expertise would be referred to as resident preceptor (intermediate-level learner). Radiology faculty physicians collaborating with and supervising the resident preceptor are referred to as faculty advisor.
Figure 1:
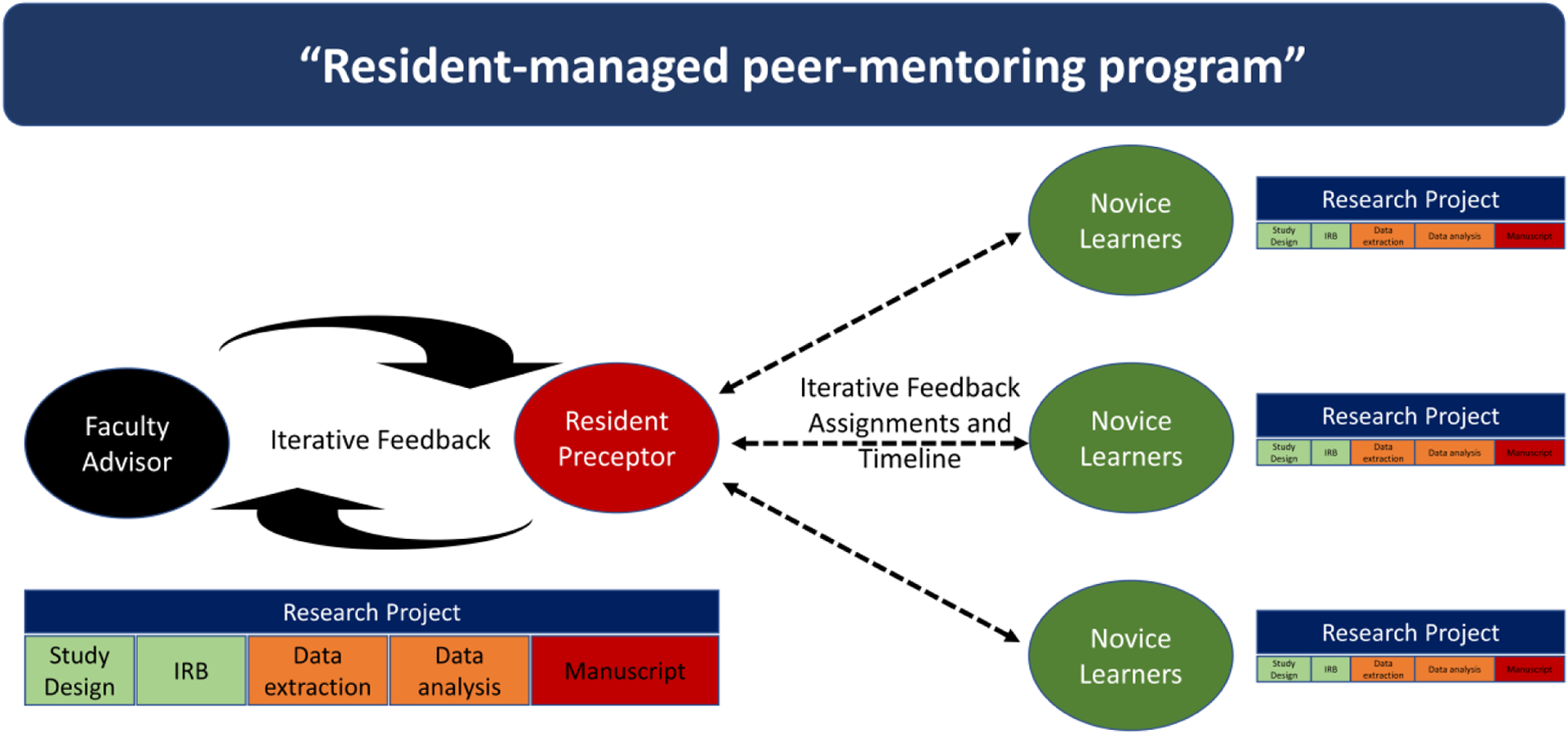
Resident-managed peer mentoring model.
In this model, the novice learners with interest in pursuing a research project typically contact a radiology faculty advisor. Radiology faculty members in roles highly visible to medical students serve as conduits of interested medical students (future novice researchers). Highly visible roles include radiology faculty members who teach radiology to preclinical and clerkship medical students, radiology faculty members who serve as formal academic advisors, and radiology faculty members who have educational administrative roles like directors of medical student education or residency program directors.
Novice learners approached us for several reasons, based on our two-year experience with this model. Medical students wanted to learn about radiology as a career, to conduct research, to enhance their academic writing, and to enhance their curriculum vitae for residency applications. Resident physicians have approached us for completing program requirements for research projects, gaining research experience and enhancing their curriculum vitae for fellowship applications. Our experience aligns with the motivations of novice learners to engage in a radiology research project as reported by Som and Winter (6,7).
Following enrollment of novice learners, they meet with the resident preceptor, and faculty advisor, to discuss multiple potential research projects that might be pursued. Based on the novice researcher’s interest, they would choose a clinical research project, which is subsequently divided into small tasks which are appropriate for a beginner in research, such as, filing a research proposal, designing the study, getting Institutional Review Board (IRB) approval, data extraction, data analysis, collaboration with statistician, drafting the manuscript and cover letter, journal selection, submitting it through the journal portal, responding to reviewers comments, proofreading the final file, and creating a strategy to present preliminary data at national meetings. In our process, the novice learners are given iterative supervision and feedback and introduced to all steps involved in going from a research question to a published manuscript.
The meetings between the novice and intermediate-level learner were informal and mostly scheduled via email or text messages. Meetings with faculty advisors were scheduled through email as needed during the process. Existing institutional email accounts were used for scheduling. During the pandemic, the majority of the meetings were conducted virtually via Zoom video conference (Zoom Video Communications Inc), access to which was supported by the institution for all the employees and students. No additional costs were incurred to the institution for our intervention in scheduling the meetings.
As a part of West Virginia Clinical and Translational Science Institute initiative for promoting research, the following resources were made available at no cost to the employees and students: Biostatistical consultation (including study design, sample size calculation, statistical analysis and interpretation of results), online anonymized health-care database (TriNetX), REDCap and Integrated Data Repository (IDR). The institutional library was utilized at no cost to access journals with subscriptions. Online storage drive (OneDrive) and REDCap were utilized for data storage and collection, with password protected user identity authenticated institutional access. The residency program provided up to USD 1000.00 travel reimbursement for each radiology resident who presented as first author at each national or international meeting for the accepted abstracts.
All these resources had been available before the intervention. None were added as a result of or as part of the intervention we describe.
The Resident managed peer mentoring program was initiated by a single radiology resident (who was the resident preceptor) in collaboration with a single senior radiology faculty member. We did not have a formal steering committee. The resident preceptor had a strong background and expertise in conducting clinical and translational research. A total of 21 radiology residents participated and a total of 26 radiology faculty members participated in this program. The participation of novice learners was on a volunteer basis, with an emphasis on inclusiveness with no strict criteria for their selection. All the participants including novice learners, residents and faculty members who expressed a desire to join a working group were accommodated. Project roles were assigned or created based on their future interest and goals of the novice learner. After a novice learner, resident preceptor and senior faculty advisor developed project ideas, faculty members with content expertise were approached and invited to a project working group (novice learner + resident preceptor + invited faculty member) by the resident preceptor.
Statistics:
The results are described as numbers and percentages. Percent change is used to assess the difference in outcomes. Bar diagrams are used for illustration.
RESULTS:
Peer-reviewed publications on PubMed by radiology faculty and residents
After our intervention, we see large increases in publications reported by both radiology residents and radiology faculty members, going from 48 and 44 before the intervention to 68 and 123 publications in the first and second years after the intervention, representing a 47.83% increase in the first academic year and 167.39% increase in the second academic year after the intervention (Figure 3A).
Figure 3:
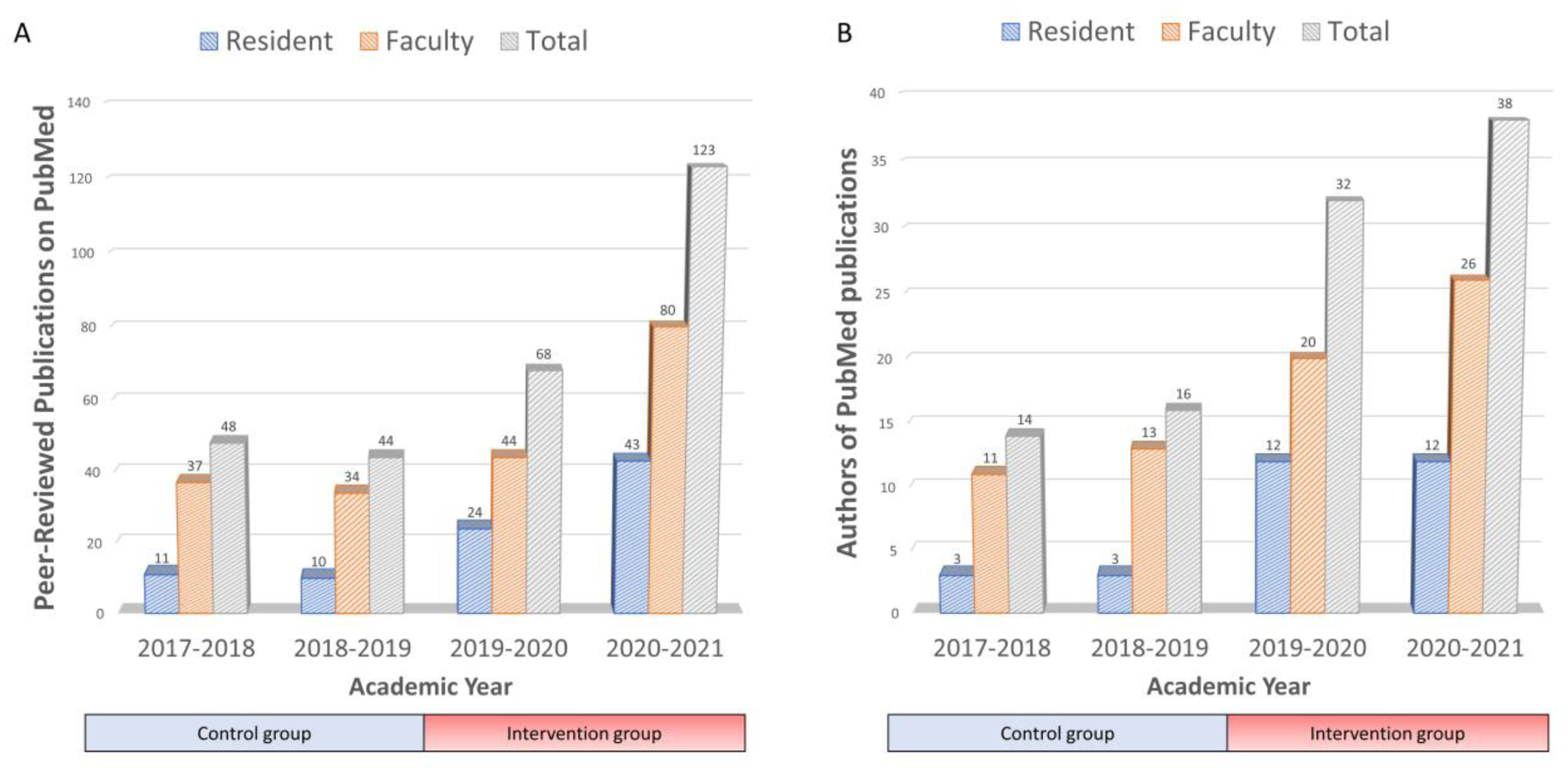
Study Outcomes. 3A. Publications by radiology faculty and residents before and after the intervention, X axis illustrates academic year and Y axis illustrates Peer-reviewed PubMed indexed publications reported by radiology physicians. 3B: Radiologists (faculty and residents) who authored PubMed indexed publications. Blue column = Radiology residents, Orange column = Radiology faculty members and Gray column = Radiology physicians includes residents and faculty members.
Historically, at our program the majority of the scholarly activity was faculty driven, with some resident physician participation. As illustrated in Figure 3A, in the pre-intervention year, radiology resident physicians had authorship in 11 and 10 publications in the 2 years before the intervention. By comparison, faculty members had authorship in 37 and 34 publications, accounting for 77% of the total departmental publications. After our intervention, increased resident participation and more resident authorship of publications occurred, going from 11 and 10 before the intervention to 24 and 43 publications with resident authors in the two academic years studied after the intervention, representing a 140% increase in the first year and 330% increase in the second year after the intervention.
Increased participation of resident physicians in scholarly activities was accompanied also by a large increase in faculty member authorship in publications. These increased from 37 and 34 before the intervention to 44 and 80 publications in each year studied after the intervention, representing a 23.94% increase in the first year and 125.35% increase in the second year after the intervention.
Authors of PubMed Publication - Number of radiology residents and faculty with authorship
The number of radiology residents and faculty members authoring PubMed Indexed publications also increased, along with overall publication numbers (Figure 3B). The number of residents participating in authorship of publications also increased by 300% in the first year, going from three residents to 12 residents reporting participation in PubMed indexed publications. The total participation by both radiology residents and faculty members increased from 14 and 16 pre-intervention to 32 and 38 annually, reporting a 113.33% increase in the first year and 153.33% increase in the second year following intervention. This illustrates broader department research involvement compared to pre-intervention years.
Academic rank-based analysis of Faculty outcomes before and after the intervention
We observed a large increase in publications by assistant professor faculty members, going from six and seven before the intervention to 15 and 35 publications in the first and second years after the intervention, representing a 130.77% increase in the first year after and 438.46% increase in the second year following intervention (Figure 4). Similarly large increases were noted among full professor faculty members, increasing by 24.14% in the first year and increasing by 106.90% in the second year after intervention. Interestingly, the effect was notably more modest with our associate professor faculty members. Our study did not specifically examine the factors for why this may be.
Figure 4:
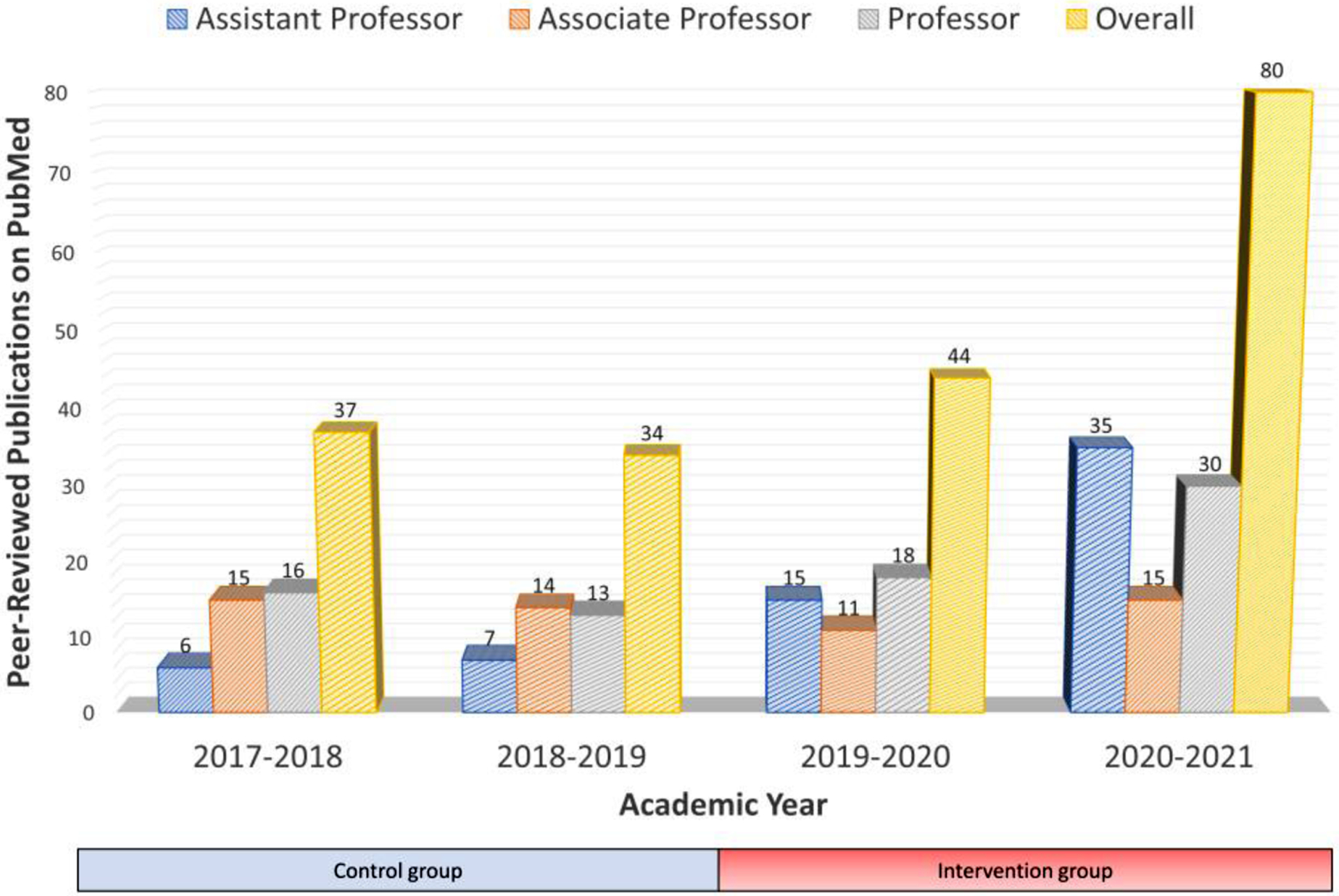
Academic rank-based analysis of Faculty outcomes before and after the intervention. X axis illustrates academic year and Y axis illustrates Peer-reviewed PubMed indexed publications reported by radiology faculty members. Blue column = Assistant professor, orange column = Associate professor, gray column = Professor and yellow column = total publications with radiology faculty member authorship.
DISCUSSION:
We report results of a “Resident-managed peer mentoring program” studied over 4 academic years designed to increase engagement of novice researchers (medical students and radiology residents) in research (Figure 1). Laddered mentorship helped novice researchers gain experience and proficiency in clinical research through active learning. After implementing this approach, substantial departmental increases in the number of PubMed indexed publications (Figure 3A) and the number of radiology physicians included in authorship of these publications (Figure 3B) were observed.
Before starting this model, it was difficult for faculty members to mentor more than 2–3 novice researchers simultaneously. When more made requests for mentorship in research, they were referred to other faculty members, some of whom had little time, experience, or interest in mentoring a novice researcher. Results were mixed, consisting mostly of Case reports or posters at meetings. Time constraints of faculty members limited access of novice researchers to research projects. We speculate that these circumstances limited education of novice researchers in basics like study design, methods, and precluded a holistic immersion in research. These observations reflect a similar experience to that described in the study by Winter and colleagues (6). These circumstances resulted in fewer novice learners getting research opportunities and fewer radiology residents participating in academic publication in the two pre-intervention years we studied when the total number of publications from the department with resident authorship was 11 and 10, and only 3 radiology residents were authors in each pre-intervention year (Figure 3).
Our resident managed peer mentoring program is analogous to Teaching Assistants (TA) widely used in college courses as a “force multiplier” for instruction. Using the resident preceptor allows faculty to supervise more novice researchers while also helping develop leadership and educator skills (elements needed to fulfill ACGME requirements) in the supervised resident preceptors through active learning. These measures improve the faculty advisor’s ability to engage more novice learners and conduct more hypothesis driven projects, based on the research outcomes we observed in this study. Additionally, we speculate that this approach provides more supervision and coaching to the novice learners for each research task to deliver completed projects, allowing them to function at higher levels and gain a rich, holistic, and more favorable research experience, improving their ability to publish and present their projects. These speculations align with the observations reported in the study by Winter and Som (4,7). The fourfold increase of residents who authored publications (3 each year before and 12 each year after intervention) and the increase in number of publications (11 and 10 before and 24 and 43 after intervention) is similar to the effect reported by Som and colleagues in which they observed a large enrollment, with 38 active research members, 14 medical students, three undergraduate students, five residents and 16 faculty members within the first six-months of resident-managed research mentoring model implementation (7). It may be worthwhile to note that Som and his colleagues did their work in the resource rich environment of the radiology department with the highest 2021 Radiology Department Research Ranking, based on NIH RePORTER (https://reporter.nih.gov/). Our investigation took place in a more clinically focused state university setting with fewer research faculty, less research infrastructure, and little NIH funding. Our work suggests that it is possible to increase research productivity and participation in departments that value these outcomes by implementing effective strategies to do so, even if departmental research resources are more modest. Our program may be particularly helpful for smaller academic centers and community programs where well-developed research infrastructure is not readily available, and where research faculty and NIH funding are scarce.
Benefits offered by this approach for novice researchers include: 1) improved access to research opportunities, 2) step-by-step instructions, constructive feedback, critical analysis, and team skills 3) scholarly outcomes (publications) that support their careers and satisfies their creativity and perhaps most important, 4) gaining research skills through active learning.
Benefits of this approach for resident preceptors (intermediate level learners) include: 1) cultivation of collaboration, leadership, and coaching skills supervised by faculty 2) longitudinal experience with iterative development of educator skills (supervision, giving feedback, managing time, assessing work, etc) with faculty supervision. Similarly, Som and colleagues observed in their model that supervising residents were able to engage in clinical research directly relevant to patient care while still allowing time to explore other basic science or translational research interests (7).
Sustainability of a program of resident managed peer mentoring may be more challenging for smaller academic or community-based residency programs than for large academic programs with long standing well-developed research programs. We believe a crucial element to sustain such a program is the intentional recruitment of resident applicants who have a demonstrated interest and ability in academic research and writing. It is desirable to have at least one resident in each training year who can be groomed to be the champion of a resident managed peer mentoring program. In some programs, a chief resident for research is formally appointed, but success may follow good efforts without that formal title. The key element is to have a resident who is focused on the desirability of extending academic success to peer residents and to medical students. Finding candidates with these values can be done by interviewing some who have achieved successes in academic writing and then discussing those works during the interview to identify candidates who are genuinely enthused and excited about pursuing research questions during residency training. Those candidates are ones who can become future resident research preceptors.
Limitations of our study design include that we 1) lacked pre-intervention baseline data for medical student publications and participation prior to our intervention, so we excluded peer-reviewed publications by medical students from our analysis. 2) our intervention was started in November 2019, not in July 2019 at the beginning of the academic year. This may result in under-reporting the true outcomes, since less than a full academic year was included in the initial post-intervention year. 3) Outcomes of abstracts and conference presentations were not available for pre-intervention years, so these were not included in our study that ultimately looked only at PubMed indexed publications. These exclusions will predictably result in under-reporting of the outcomes.
This proposed model promotes active learning amongst novice researchers, illustrating the path and training them to tackle a research project from start to finish, while providing them with explanatory narrative, sufficient autonomy, and oversight. Strong advantages of utilizing a resident preceptor are that it reduces the time constraints of faculty advisors in a clinically busy program, promotes leadership and teaching by residents, and allows faculty advisors to effectively mentor more trainees, extending their reach similar to the way Teaching Assistants function in college courses. This approach is transferable and can be replicated to other programs where an increase in research productivity and participation are valued.
Acknowledgement:
The preliminary results of this work were presented as oral presentation at American University of Radiology (AUR) 2021 annual meeting. The study was exempted under protocol #2103266667 by West Virginia University Office of Research Integrity and Compliance, Institutional Review Board (IRB).
Funding:
Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number 5U54GM104942-05. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health
Abbreviation:
- ACGME
American College of Graduate Medical Education
- NIH
National Institution of Health
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: None
Financial disclosure: None
REFERENCES:
- 1.Magid D Building a Vertical Advisory system: how to succeed as an educator and mentor without going insane. Acad Radiol 2007;14(8):992–997. doi: 10.1016/j.acra.2007.05.004 [DOI] [PubMed] [Google Scholar]
- 2.Whitworth PW, Agarwal A, Colucci A, Sherry SJ, Subramaniam RM. Radiology research and medical students. Acad Radiol 2013;20(12):1506–1510. doi: 10.1016/j.acra.2013.09.013 [DOI] [PubMed] [Google Scholar]
- 3.Shah P, Sheng M, Mankoff DA, Trerotola SO, Galperin-Aizenberg M, Katz SI, Barbosa EJM, Nachiappan AC. Impact of Early Radiology Research Experiences on Medical Student Perceptions of Radiology and Research. Curr Probl Diagn Radiol 2019;48(5):423–426. doi: 10.1067/j.cpradiol.2018.05.011 [DOI] [PubMed] [Google Scholar]
- 4.Taylor CS, Vijayakumar V. Effective Research Mentoring of Radiology Residents. J Am Coll Radiol 2018;15(4):667–668. doi: 10.1016/j.jacr.2017.12.003 [DOI] [PubMed] [Google Scholar]
- 5.Wazen J, Goldstein AJ, Kim HH, Tai R, Watts GJ, DeBenedectis CM. Tales of Mentoring in Radiology: The Experience of Residents and Mentors at a Single Academic Program. Curr Probl Diagn Radiol 2021;50(3):374–378. doi: 10.1067/j.cpradiol.2020.01.004 [DOI] [PubMed] [Google Scholar]
- 6.Winter AM, Parikh R, Hardy AK, Akduman EI, Osman M, Brown J. A roadmap of resident-led initiatives to promote research within the radiology department. Clin Imaging 2021;72:58–63. doi: 10.1016/j.clinimag.2020.11.032 [DOI] [PubMed] [Google Scholar]
- 7.Som A, Lang M, Di Capua J, Chonde DB, Cochran RL. Resident-Led Medical Student Radiology Research Interest Group: An Engine for Recruitment, Research, and Mentoring-Radiology In Training. Radiology 2021;300(1):E290–E292. doi: 10.1148/radiol.2021204518 [DOI] [PubMed] [Google Scholar]
- 8.Phelps A, Fritchle A, Hoffman H. Passive vs. active virtual reality learning: the effects on short- and long-term memory of anatomical structures. Stud Health Technol Inform 2004;98:298–300. [PubMed] [Google Scholar]
- 9.Lawal O, Ramlaul A, Murphy F. Problem based learning in radiography education: A narrative review. Radiography (Lond) 2021;27(2):727–732. doi: 10.1016/j.radi.2020.11.001 [DOI] [PubMed] [Google Scholar]
- 10.Bucklin BA, Asdigian NL, Hawkins JL, Klein U. Making it stick: use of active learning strategies in continuing medical education. BMC Med Educ 2021;21(1):44. doi: 10.1186/s12909-020-02447-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Riddell J, Jhun P, Fung CC, Comes J, Sawtelle S, Tabatabai R, Joseph D, Shoenberger J, Chen E, Fee C, Swadron SP. Does the Flipped Classroom Improve Learning in Graduate Medical Education? J Grad Med Educ 2017;9(4):491–496. doi: 10.4300/JGME-D-16-00817.1 [DOI] [PMC free article] [PubMed] [Google Scholar]


