Abstract
Objective
The involvement of salivary glands in primary SS (pSS) can be assessed in different ways: histopathology, salivary flow and ultrasonography. To understand the relative value of these different approaches, it is crucial to understand the relationship between them. As we routinely perform these three modalities in the parotid gland for disease evaluation, our aim was to investigate the construct validity between these modalities in one and the same gland.
Methods
Consecutive sicca patients underwent a multidisciplinary diagnostic workup including parotid gland biopsy, collection of parotid gland–specific saliva and parotid gland ultrasonography. Patients who were classified as pSS according to the ACR-EULAR criteria were included. Construct validity was assessed using Spearman’s correlation coefficients.
Results
The 41 included pSS patients completed a full workup within a mean time interval of 2.6 months. Correlations between histopathological features and stimulated parotid salivary flow were fair (ρ = −0.123 for focus score and ρ = −0.259 for percentage of CD45+ infiltrate). Likewise, poor correlations were observed between stimulated parotid salivary flow and parotid ultrasonography (ρ = −0.196). Moderate to good associations were found between the histopathological items focus score and the percentage of CD45+ infiltrate, with parotid US scores (total US score: ρ = 0.510 and ρ = 0.560; highest for homogeneity: ρ = 0.574 and ρ = 0.633).
Conclusion
Although pSS-associated ultrasonographic findings did correlate with histopathological features, the three modalities that evaluate salivary gland involvement assess different (or at best partly related) constructs. Therefore histopathology, salivary flow and ultrasonography are complementary measurements and cannot directly replace each other in the workup of pSS.
Keywords: primary Sjögren’s syndrome, parotid gland, biopsy, histopathology, salivary flow, ultrasonography
Rheumatology key messages.
Parotid gland histopathology, salivary flow and ultrasonography assess different constructs in primary SS (pSS) patients.
Parotid salivary flow is not related to parotid histopathology or parotid ultrasonography in pSS.
The three different modalities cannot directly replace each other in the workup of pSS.
Introduction
Primary SS (pSS) is a chronic, systemic autoimmune disease characterized by oral and ocular sicca complaints [1]. Inflammation of the salivary and lacrimal glands is a hallmark of the disease and plays a central role in the current classification criteria [2]. The involvement of salivary glands in the disease process can be assessed in different ways. The three following modalities are most commonly used: salivary gland biopsy, saliva collection and salivary gland ultrasonography. The histopathological assessment of salivary glands and collection of salivary secretions are included in the current classification criteria as separate items and it has recently been proposed to add ultrasonography as an item [2–4].
The inflammatory process in salivary glands of pSS patients is characterized by periductal clusters of ≥50 lymphocytes, called foci. The number of foci per 4 mm2 glandular parenchyma can be calculated into a focus score (FS) [5, 6]. For classification of pSS, in which histopathology of salivary glands is one of the major items, biopsies with an FS ≥1 are considered positive [2]. Other histopathological features are the presence of lymphoepithelial lesions and germinal centres and a relative increase of IgG and IgM plasma cells compared with the number of IgA plasma cells (plasma cell shift) [7–11]. Furthermore, salivary glands of pSS patients contain higher proportions of fibrosis and acinar atrophy than controls [12, 13]. Whether fatty infiltration is specific for pSS or an age-associated condition remains to be determined [14, 15]. During the diagnostic workup of pSS, biopsies are mostly taken from labial glands. However, taking biopsies from parotid glands offers several advantages, such as increased specificity for diagnosing pSS, the possibility to take multiple biopsies of the same gland and the advantage of early detection of pSS-associated lymphomas localized in the parotid gland [16, 17]. For these reasons, we routinely perform parotid gland biopsies in patients suspected of pSS.
The second tool to evaluate salivary gland involvement in pSS is the assessment of saliva secretion. Unstimulated whole salivary flow (UWSF) is currently included in the ACR-EULAR criteria as an item [2]. Unstimulated whole saliva (UWS) is composed of contributions of all minor and major glands, although UWS contains minor amounts of saliva from the parotid glands, since the parotid glands only contribute significantly to whole saliva after stimulation [18]. Saliva can also be collected under stimulated conditions, such as masticatory (chewing) or gustatory (citric acid solution) stimulation. Stimulated whole salivary flow (SWSF) is also a mixture of saliva from all minor and major salivary glands. In addition to collecting saliva from all glands together it is possible to collect saliva exclusively from the parotid glands [18]. Therefore parotid flow rates can be used for direct functional assessment of the parotid glands.
The third tool to assess salivary gland involvement in pSS is salivary gland ultrasonography (SGUS). SGUS evaluates major salivary glands, i.e. parotid and submandibular glands. This upcoming tool is non-invasive, well-tolerated, inexpensive, increasingly available in the outpatient clinic and can be performed repeatedly [19, 20]. Multiple scoring systems of SGUS are in use, of which the Hocevar scoring system is most commonly applied [21]. We previously showed that scoring hypoechogenic areas suffices for classification, which further increases the feasibility of SGUS [22].
To understand the relative value of these different modalities in the workup of SS, it is crucial to understand the relationship between them. Although patients secreting <0.1 ml/min UWS were two times more likely to have an FS ≥1 [23], correlations between histopathological findings, such as FS and the amount of fibrosis, and UWSF are poor [24–26]. When comparing SGUS scores (from major salivary glands) with labial gland FS and UWSF, correlation coefficients appear to be higher [27–29]. However, interpretation of these findings is complicated since histopathology, collection of saliva and ultrasonography were not assessed in the same salivary gland. Furthermore, there were differences in methods of saliva collection and SGUS scoring systems. Since we routinely perform parotid gland biopsies, collect parotid gland–specific saliva and perform parotid gland ultrasonography in the diagnostic workup of pSS, we are in the unique position to analyse the relationship between these three modalities in the same gland. In the work presented here we aim to explore this relationship by assessing construct validity between histopathology, salivary secretion and ultrasonography of the same parotid gland in pSS patients.
Materials and methods
Patients
In this cross-sectional study, we included consecutive patients ≥18 years of age who were referred to the Sjögren’s expertise centre at the University Medical Center Groningen (UMCG) for suspicion of pSS and were classified as pSS according to the ACR-EULAR criteria [2]. All patients of this inception cohort underwent a full diagnostic workup, including a parotid gland biopsy, collection of parotid gland–specific saliva and ultrasonography. Informed consent was not required by the Dutch Law for Medical Research and by institutional guidelines. No objection against the use of redundant diagnostic material was recorded from patients in the institutional record of objection. Patient material was handled according to the Code of Conduct for Health Research of the Dutch Federation of Biomedical Scientific Societies [30].
Histochemical and immunohistochemical staining
Parotid gland biopsies were formalin fixed, paraffin embedded and sectioned at 3 µm thickness. On consecutive slides, haematoxylin and eosin (H&E) and Masson staining were performed. Immunohistochemical staining for CD45, IgA/IgG and IgM was performed on an automated staining platform, following the manufacturer’s protocols. For the Bcl-6 staining, tissue sections were deparaffinized and antigen retrieval was performed (EDTA pH 8, 15 min at 98°C). After blocking of endogenous peroxidase, slides were incubated with anti-Bcl6 for 75 min. Sections were incubated with anti-mouse Ig horseradish peroxidase polymer for 40 min. Staining was visualized with diaminobenzidine and slides were counterstained with haematoxylin. For further details see Supplementary Table S1, available at Rheumatology online.
Histological analysis
FS and the presence of lymphoepithelial lesions were assessed on H&E-stained sections (Fig. 1A). An arbitrary maximum FS of 12 was given to confluent foci. Lymphoepithelial lesions were determined by the presence of lymphocytes within the ductal epithelium with concurrent epithelial hyperplasia (Fig. 1A and B). A cluster of five or more Bcl6+ cells lying next to each other within a focus was classified as a germinal centre (Fig. 1C) [31, 32]. The presence of a plasma cell shift was assessed using IgA/IgG double staining and IgM staining (Fig. 1D). A relative decrease of ≤70% IgA+ plasma cells in relation to the total plasma cell population (present in foci and unaffected parenchyma) was considered as abnormal [11]. Biopsies were independently scored by two pathologists (E.A.H. and B.v.d.V.). Inconsistencies were resolved during a consensus meeting.
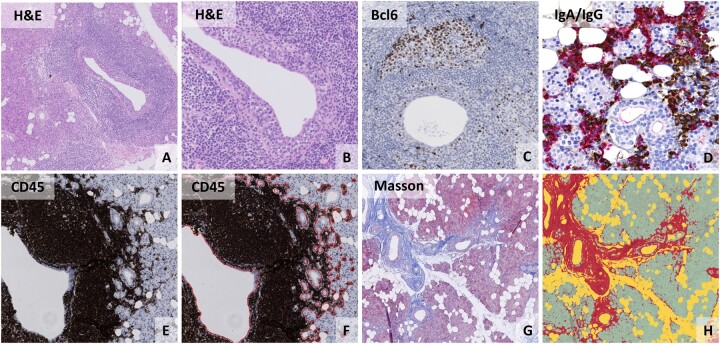
Fig. 1.
(Immuno-)histological analysis of parotid gland tissue from pSS patients
Parotid gland biopsies from pSS patients showing (A) a periductal focus on H&E staining with a centrally located lymphoepithelial lesion. (B) High-resolution image of the same lymphoepithelial lesion showing hyperplastic epithelium with intra-epithelial lymphocytes. (C) The presence of a germinal centre, as shown by a cluster of five or more Bcl6+ cells. (D) Dual staining for IgA (red) and IgG (brown) plasma cells showing an influx of IgG+ plasma cells. (E) CD45 staining of parotid gland tissue. (F) Digital image analysis of the relative area of CD45+ infiltrate by using QuPath. (G) Parotid gland tissue stained with a modified Masson stain in which dense connective tissue is coloured blue. (H) Digital image analysis of the modified Masson staining by using QuPath, in which red represents fibrotic tissue, yellow represents fat cells and green represents glandular parenchyma.
The relative area of CD45+ infiltrate in relation to the total area of glandular parenchyma (including intervening fat cells) was evaluated on CD45-stained slides and the relative areas of fatty and fibrotic tissue were evaluated on the modified Masson staining. Digital image analyses (DIA) of both slides were performed by using QuPath version 0.2.3 (Fig. 1F and H).
Salivary secretion
UWS and chewing stimulated whole saliva (SWS) were collected. UWS secretion rates of ≤1.5 ml/15 min and SWS secretion rates of ≤3.5 ml/5 min were considered abnormal [33]. Unstimulated parotid salivary flow (UPF) and 2% citric acid stimulated parotid salivary flow (SPF) were measured using Lashley cups using a standardized assessment protocol [18].
Ultrasonography
SGUS was performed using an ultrasonographic scanner (Esaote MyLabSeven, Genova, Italy) equipped with a high-resolution probe (4–13 MHz) by three well-trained ultrasonographers (A.J.S., K.D., J.F.N.), with good to excellent inter- and intra-observer reliability [34]. Patients were examined in a supine position with their head turned towards the opposite side and neck slightly extended. The scoring system of Hocevar et al. [21] was used in both the parotid and submandibular glands (Supplementary Fig. S1, available at Rheumatology online). Separate analyses were performed for one-sided parotid gland ultrasonography (PGUS), with emphasis on the components ‘hypoechogenic areas’ and ‘hyperechogenic reflections’ [22]. For the total Hocevar score, which includes all four major glands, a score ≥15 was considered positive [35].
Statistical analysis
Descriptive parameters were expressed as number (%), mean (s.d.) or median (IQR) as appropriate. Construct validity was assessed using Spearman’s correlation coefficients (ρ) between histopathological parameters and parotid salivary secretion, between histopathological parameters and PGUS scores and between parotid salivary flow and PGUS scores; all three modalities were assessed in the same parotid gland. Spearman’s correlation coefficient (ρ) was interpreted as poor (0.0–0.2), fair (0.2–0.4), moderate (0.4–0.6), good (0.6–0.8) or excellent agreement (0.8–1.0) [35]. Hypotheses for assessing construct validity were predefined, as recommended in construct validity research [37]. Since fair correlations were found between histopathology and salivary flow in previous studies [24–26], it was hypothesized that there would be fair to moderate correlations between parotid histopathological parameters and parotid salivary secretion, as they assess related but different types of outcomes. Furthermore, it is known that intra-individual variation of parotid salivary flow is ∼24% [38] and that salivary flow fluctuates with circadian rhythm and age [39, 40]. The relatively high measurement variation in salivary flow rates will lower the expected level of correlation with histopathological parameters. As parotid gland biopsies are always taken in the same region of the gland, representing only a small part of the parotid gland that is analysed by US, abnormalities that are detected by US can be missed in the salivary gland biopsy. Therefore correlations between histopathological parameters and PGUS scores were hypothesized to be moderate, as they only partly assess the same construct. Finally, it was hypothesized that there would be fair correlations between parotid salivary flow and PGUS, as they assess different outcomes within the same construct, and the measurement variation in parotid salivary flow was also taken into account.
As exploratory analyses, Kruskal–Wallis tests were used to compare histopathological parameters between various groups based on PGUS-hypo and PGUS-hyper scores. Mann–Whitney U tests were used to compare variables between groups based on the presence of histopathological features and between groups based on the presence of multiple hypoechogenic areas (PGUS-hypo ≥2) vs limited or no hypoechogenic areas (PGUS-hypo ≤1).
The percentages of absolute agreement between the different methods were calculated, based on the cut-off values that are used for classification of pSS: FS ≥1, UWSF ≤0.1 ml/min, SGUS ≥15. Furthermore, the associations between FS, UWSF and SGUS were explored using Spearman’s correlation coefficients (ρ). Statistical analyses were executed using SPSS Statistics 23 (IBM, Armonk, NY, USA). P-values <0.05 were considered statistically significant.
Results
Patients and time interval between methods
Forty-six consecutive pSS patients were evaluated for eligibility. Four patients had to be excluded because of insufficient biopsy material (surface area <4 mm2) and one patient because of the presence of a parotid gland mucosa-associated lymphoid tissue lymphoma. Patient characteristics are presented in Table 1. The median time interval between the biopsy and saliva collection was 2.3 months (range 0.0–16.8), between the biopsy and SGUS 1.6 months (range 0.0–11.0) and between SGUS and saliva collection 1.2 months (range 0.0–14.7). In 90% and 73% of pSS patients the parotid biopsy was performed after saliva collection or after SGUS, respectively.
Table 1.
Patient characteristics of the included pSS patients (n = 41)
| Characteristics | Values |
|---|---|
| Age, years, mean (s.d.) | 50.4 (13.6) |
| Female, n (%) | 40 (97.6) |
| ACR-EULAR items, n (%) | |
| Anti-SSA antibodies | 37 (90.2) |
| FS ≥1, parotid gland | 25 (61.0) |
| UWSF ≤0.1 ml/mina | 27 (65.9) |
| Schirmer’s test ≤5 mm/5 min | 32 (78.0) |
| OSS ≥5a | 23 (56.1) |
| SGUS ≥15b | 25 (61.0) |
| Parotid histology | |
| FS, median (IQR) | 1.1 (0.4–2.3) |
| CD45+ infiltrate, %, median (IQR) | 5.3 (2.2–18.9) |
| Fat, %, median (IQR) | 37.9 (24.2–45.8) |
| Fibrosis, %, median (IQR) | 19.8 (6.8–26.1) |
| Presence of lymphoepithelial lesions, n (%) | 20 (48.8) |
| ≤70% IgA plasma cells, n (%) | 15 (36.6) |
| Presence of germinal centres, n (%) | 14 (34.1) |
| Parotid saliva (biopsy side), median (IQR) | |
| UPF, ml/min | 0.00 (0.00–0.03) |
| SPF, ml/min | 0.06 (0.02–0.11) |
| Parotid ultrasonography (biopsy side), median (IQR) | |
| PGUS total score (range 0–13) | 4.0 (2.0–7.5) |
| PGUS-homogeneity (range 0–3) | 1.0 (0.0–2.0) |
| PGUS-hypo (range 0–3) | 1.0 (1.0–3.0) |
| PGUS-hyper (range 0–3) | 1.0 (1.0–1.0) |
<5% missing data. bSGUS is not (yet) included in the ACR-EULAR criteria, but a score of ≥15 has been proposed.
OSS: ocular staining score.
Parotid salivary flow vs parotid histology
UPF showed poor to fair associations with FS, percentages of CD45+ infiltrate and percentages of fat and fibrosis within the parotid gland (Table 2; Supplementary Fig. S2A and C, available at Rheumatology online). Correlation coefficients between SPF and histological parameters were slightly higher, but associations were still fair (Table 2; Supplementary Fig. S2B and D, available at Rheumatology online). No significant differences in parotid flow (UPF or SPF) were found between pSS patients with presence of lymphoepithelial lesions (UPF P = 0.27 and SPF P = 0.39) or presence of a plasma cell shift (UPF P = 0.83 and SPF P = 0.75) compared with pSS patients without these histopathological features. Although SPF levels seemed to be lower in pSS patients with presence of germinal centres compared with pSS patients without germinal centres, no significant differences were found (median 0.02 vs 0.07; P = 0.08). Overall there is no clear relation between histological features within parotid gland biopsies and parotid salivary flow rates in this diagnostic cohort.
Table 2.
Spearman correlations between parotid histological parameters, parotid salivary flow and parotid gland ultrasonography
| Characteristics | Parotid gland histopathology |
Parotid salivary flow (biopsy side) |
||||
|---|---|---|---|---|---|---|
| FS | CD45 (%) | Fat (%) | Fibrosis (%) | UPF (ml/min) | SPF (ml/min) | |
| Parotid salivary flow (biopsy side) | ||||||
| UPF (ml/min) | 0.095 | −0.226 | 0.228 | −0.045 | – | – |
| SPF (ml/min) | −0.123 | −0.259 | 0.239 | −0.133 | – | – |
| Parotid gland ultrasonography (biopsy side) | ||||||
| PGUS total score (biopsy side) (0–13) | 0.510* | 0.560* | −0.110 | 0.077 | 0.069 | −0.196 |
| PGUS subscores of individual US components | ||||||
| Parenchymal echogenicity (range 0–1) | 0.219 | 0.346* | −0.186 | 0.177 | 0.134 | 0.015 |
| Homogeneity (range 0–3) | 0.574* | 0.633* | 0.197 | 0.156 | −0.002 | −0.224 |
| Hypoechogenic areas (range 0–3) | 0.523* | 0.540* | −0.114 | 0.034 | 0.042 | −0.227 |
| Hyperechogenic reflections (range 0–3) | 0.274 | 0.170 | 0.173 | 0.061 | 0.226 | 0.157 |
| Salivary gland posterior border (range 0–3) | 0.091 | 0.231 | 0.028 | −0.069 | −0.027 | −0.159 |
P < 0.05.
Parotid histology vs parotid ultrasonography
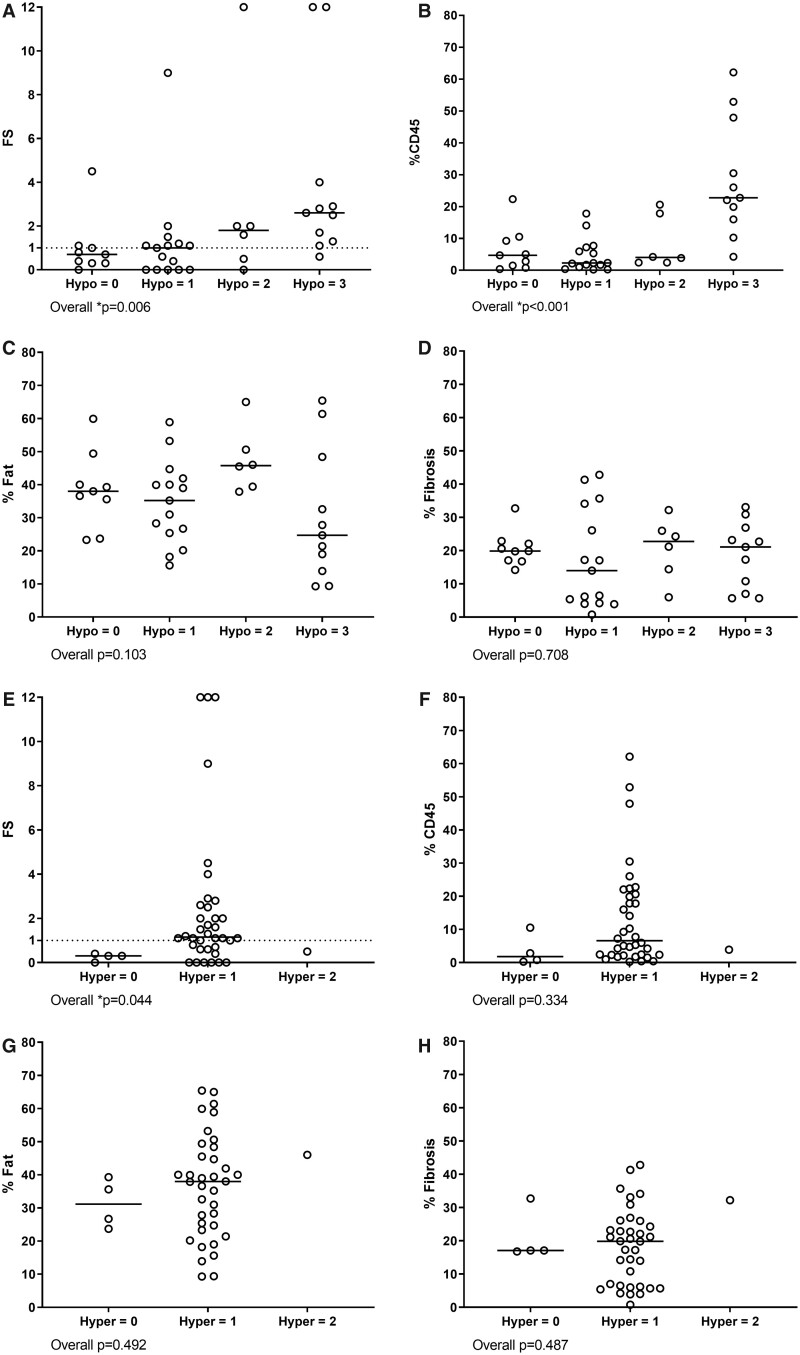
Moderate associations were found between FS, the percentage of CD45+ infiltrate and PGUS total scores (Table 2). For the individual US components PGUS-homogeneity and PGUS-hypo, moderate to good associations were found with FS and the percentage of CD45+ infiltrate (Table 2). Remarkably, three patients with a positive FS (i.e. FS ≥1) had no hypoechogenic areas within the parotid gland (i.e. PGUS-hypo = 0) and three patients with a negative FS did have hypoechogenic areas (i.e. PGUS-hypo ≥2) (Fig. 2). In other words, FS ≥1 was not always reflected by the presence of hypoechogenic areas and the presence of hypoechogenic areas was not always reflected by a positive FS. The percentages of fat and fibrosis did not differ significantly between the different PGUS-hypo and PGUS-hyper scores (Fig. 2), which was also reflected by poor associations between these parameters (Table 2).
Fig. 2.
Comparison between parotid US and parotid biopsy features
Hypoechogenic areas in the parotid gland compared with (A) the FS, (B) percentage of CD45+ infiltrate, (C) percentage of fat and (D) percentage of fibrosis. Hyperechogenic reflections in the parotid gland compared with (E) the FS, (F) percentage of CD45+ infiltrate, (G) percentage of fat and (H) percentage of fibrosis. Hypoechogenic areas were scored as follows: 0 = absent, 1 = a few (<25%), 2 = several (25–50%) and 3 = numerous (>50%). Hyperechogenic reflections were scored as follows: 0 = absent; 1 = a few, scattered (<25%); 2 = several (25–50%) and 3 = numerous (>50%). Dotted lines represent FS = 1. *P < 0.05.
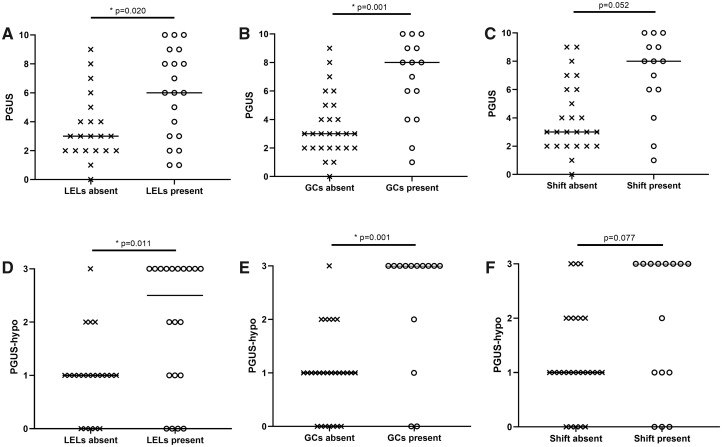
Patients with presence of lymphoepithelial lesions and patients with presence of germinal centres had significantly higher PGUS total scores compared with patients without these features (Fig. 3A–C). The two individual components that contributed most to this difference were homogeneity and hypoechogenic areas. Scores for these two components were significantly higher in patients with lymphoepithelial lesions and germinal centres (P = 0.014 for PGUS-homogeneity and P = 0.004 for PGUS-hypo). However, patients with lymphoepithelial lesions and germinal centres did not always show hypoechogenic areas on US, as four patients with lymphoepithelial lesions (20%) and two patients with germinal centres (14%) had a PGUS-hypo score of 0 (Fig. 3D–F). In conclusion, pSS-associated ultrasonographic findings (PGUS-hypo and PGUS-homogeneity) correlated to some extent with glandular histological parameters of inflammation and were also associated with typical histopathological features.
Fig. 3.
PGUS total scores and PGUS-hypo scores compared with the presence of lymphoepithelial lesions, germinal centres and plasma cell shift
PGUS total scores in pSS patients with and without presence of (A) LELs, (B) GCs and (C) plasma cell shift. PGUS-hypo scores in pSS patients with and withou presence of (D) LELs, (E) GCs and (F) plasma cell shift. Horizontal bars represent medians. *P < 0.05. GC: germinal centre; LEL: lymphoepithelial lesion.
Parotid salivary flow vs parotid ultrasonography
Reduced parotid flow was poorly reflected by abnormal PGUS scores, as UPF and SPF both showed poor associations with PGUS total scores and PGUS components (Table 2; Supplementary Fig. S2E and F, available at Rheumatology online). UPF and SPF levels were not significantly lower in pSS patients with multiple hypoechogenic areas in the parotid gland (PGUS-hypo ≥2) compared with patients with limited or no hypoechogenic areas (PGUS-hypo ≤1) (P = 0.62 and P = 0.29, respectively). Apparently, typical PGUS abnormalities and parotid salivary secretion are not directly related to each other.
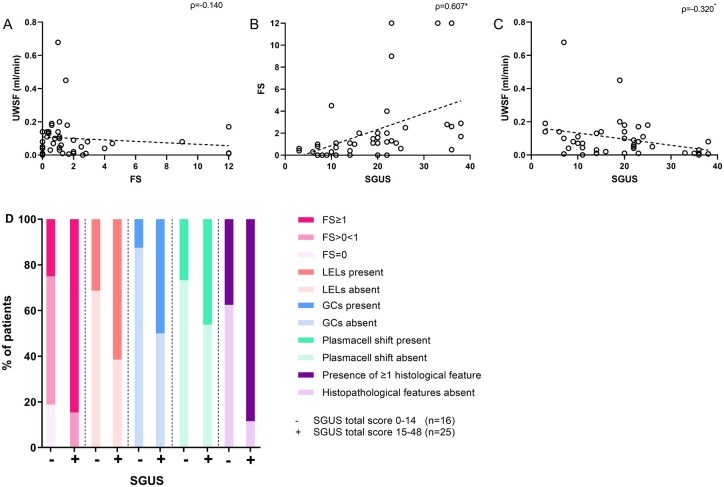
Agreement of the three modalities used for pSS classification
The items FS and UWSF that are included in the current 2016 ACR-EULAR classification criteria for pSS are not parotid gland specific. FS can be measured in both labial and parotid gland biopsies and UWS is a mixture of contributions of all minor and major salivary glands. Furthermore, the item ultrasonography, which has recently been proposed to be included in these criteria, evaluates the submandibular glands in addition to the parotid glands. To compare the three different modalities as used in the classification criteria, we analysed the agreement based on their cut-off values (FS ≥1, UWSF ≤0.1 ml/min, SGUS score ≥15). Absolute agreement between FS and UWSF was 61%, between FS and SGUS was 80% and between UWSF and SGUS was 56%. The highest correlation was found between FS and SGUS (ρ = 0.607, P < 0.001). Correlation between FS and UWSF was poor (ρ = −0.140, P = 0.38), and between UWSF and SGUS fair (ρ = −0.320, P = 0.042) (Fig. 4A–C). As shown in Fig. 4D, all SGUS-positive patients had foci in the parotid gland (i.e. FS >0) and >80% had an FS ≥1. Furthermore, almost all SGUS-positive patients (89%) showed at least one histological feature associated with pSS (FS ≥1, presence of lymphoepithelial lesions, germinal centres, plasma cell shift) within their biopsy. However, 38% of SGUS-negative patients also showed one or more histopathological features within their parotid gland biopsy, indicating that the presence of specific histopathological features of pSS is not always associated with a positive US.
Fig. 4.
Comparison of items as used in the 2016 ACR-EULAR classification criteria for pSS
Correlations between (A) UWSF and FS, (B) FS and SGUS and (C) UWSF and SGUS. (D) Percentages of SGUS-positive and SGUS-negative patients with the presence of histopathological features within the parotid gland biopsy. *P < 0.05. GC: germinal centre; LEL: lymphoepithelial lesion.
Discussion
The present study showed that evaluations of the same parotid gland by histopathology, salivary flow and ultrasonography assess different (or at best partly related) constructs. We showed that in patients with pSS, correlations between parotid gland salivary flow and parotid gland histopathological parameters were poor to fair. Likewise, no clear relation was found between parotid salivary flow and abnormalities found by parotid gland ultrasonography. Apparently, salivary flow does not assess the same construct as parotid gland histopathology, nor parotid gland ultrasonography. On the other hand, we showed moderate to good correlations between the histopathological parameters FS and the amount of infiltrate and the US parameters PGUS-total, PGUS-homogeneity and PGUS-hypo (Table 2). Thus typical US findings in pSS patients seem to be related to the amount of inflammatory infiltrate in the salivary gland biopsy. However, this was not seen in all pSS patients, as there are still some patients with a positive US and FS <1, as well as patients with histological lymphocytic foci without typical ultrasonographic abnormalities.
Recently Izzetti et al. [41] compared US and histopathology of labial salivary glands. They found a moderate correlation (ρ = 0.532) between labial gland FS and labial gland US scores in patients suspected of pSS [41]. We found a comparable correlation (ρ = 0.510) between FS and PGUS total score of the parotid glands and an even better correlation between the amount of infiltrate and PGUS total scores. From these results we can conclude that the inflammatory infiltrates are somehow related to US scores, both in the labial and parotid salivary gland. In the present study, the highest correlations were found between FS and the amount of CD45 infiltrate and the US scores PGUS-hypo and PGUS-homogeneity. This implies that hypoechogenic areas and inhomogeneity are linked to histopathological lymphocytic infiltrates. Previously it was suggested that hypoechogenic areas represent lymphocytic infiltrates [42, 43]. However, as hypoechogenic areas are significantly larger in size compared with foci seen in tissue sections of biopsies, these hypoechogenic areas cannot directly represent foci. Therefore an indirect association between hypoechogenic areas and infiltrates is more likely.
Recently Wang et al. [44] hypothesized that the presence of hypoechogenic areas could be caused by leakage of saliva into the periductal infiltrate and eventually into the salivary gland parenchyma, due to dysfunction of tight junctions between striated ductal cells [44]. Although this hypothesis may explain why hypoechogenic areas are much larger than infiltrates, intraparenchymal saliva and concurrent reactive changes were not observed in this series (nor in clinical practice). Therefore the most likely explanation would be that hypoechogenic areas represent areas with a higher density of periductal foci with relatively little unaffected glandular tissue between these foci, which is also supported by the good correlation between the amount of CD45+ infiltrate and hypoechogenic areas (ρ = 0.540) in this study. Furthermore, we showed that pSS patients with histopathological features (lymphoepithelial lesions and germinal centres), which are associated with inflammatory foci, had higher PGUS-hypo scores. Nevertheless, the presence of hypoechogenic areas does not predict whether the biopsy contains any of these features (Fig. 3D–F) and not all pSS patients with these histopathological features show hypoechogenic areas on US. This is in line with previous findings, as Hammenfors et al. [45] showed that only 67% of pSS patients with germinal centre–like structures in the labial gland had an abnormal US score. Although Wernicke et al. [42] hypothesized that hyperechogenic reflections consist of areas of fibrosis, we did not find a correlation between hyperechogenic reflections and any histological parameter (including fat and fibrosis). However, the analysis of ultrasonographic images may suffer from inter- and intra-observer differences and is based on a categorical scale, which will also lower the level of correlation in this study. Several initiatives, like the European Union–funded Horizon 2020 project called HarmonicSS and a sub-task force of the OMERACT working group, aim to develop more objective US scoring systems to overcome the risk of inter- and intra-observer differences [46–48].
Furthermore, as described earlier, a parotid gland biopsy represents only a small part of the gland, while the whole gland is analysed by ultrasonography. Therefore a biopsy might be taken from non-affected salivary gland tissue and result in a false-negative outcome (sampling error). A technique that could help to better understand the relationship between hyper- and hypoechogenic areas and histopathological features is US-guided core needle biopsy. Recently this technique has proven to be useful in the evaluation of suspected salivary gland lymphoma in pSS [49]. Although less tissue is collected compared with an open biopsy, core needle biopsy also provides biopsies with a preserved architecture. Thus a biopsy can be taken specifically from the location of hyper- or hypoechogenic areas.
Despite the notion that there is a relationship between parotid histology and ultrasonography, parotid salivary flow rates do not correlate well with histopathological features, nor with ultrasonography. In line with our results, Bookman et al. [24] also found poor agreement between UWSF and labial gland FS and fair agreement between SWSF and labial gland FS. Likewise, Daniels et al. [23] found an absolute agreement of 60% between UWSF and labial gland FS in the large Sjögren’s International Collaborative Clinical Alliance cohort. Yalcinkaya et al. [50] recently showed that patients with UWSF ≤0.1 ml/min had significantly higher PGUS scores compared with patients with a UWSF above the threshold. In our study, UPF did not differ significantly between patients with high (≥2) and low (<2) PGUS-hypo scores. However, in unstimulated conditions, whole saliva mainly consists of the contributions of submandibular and sublingual glands [18]. For this reason, analyses containing either UWSF or UPF cannot be equally compared with each other. In our cohort, the correlation between UWSF and UPF was ρ = 0.600, compared with ρ = 0.832 between SWSF and SPF. Furthermore, the parotid glands appear to be the last salivary gland to show a functional decline in pSS patients [51]. As we evaluated newly diagnosed pSS patients in a diagnostic cohort, the parotid glands were still relatively spared, which can partly explain the poor correlations of SGUS and histopathology with parotid salivary flow in this cohort. The time lag between the saliva collection, US and biopsy reflects the diagnostic pathway in daily clinical practice but may have somewhat underestimated the observed associations between the three modalities. In a minority of pSS patients, the parotid gland biopsy was performed prior to saliva collection or US (n = 4 and n = 11, respectively), which might affect the results. For these subgroups of patients, the median time intervals between the modalities were relatively large (5.9 months between biopsy and saliva collection and 4.6 months between biopsy and PGUS). Furthermore, right- and left-sided salivary flow rates and right- and left-sided US scores were highly associated (ρ = 0.815 and ρ = 0.943, respectively). Therefore the impact of the previous biopsy on salivary flow rates or US scores are expected to be negligible in this cohort.
Together, parotid gland salivary flow was not related to parotid gland histopathology nor to parotid gland US scores. Parotid gland histopathology was partly related to parotid gland US, as we found moderate to good correlations between histopathological inflammatory parameters and PGUS scores. In conclusion, histopathology, salivary flow and ultrasonography are three complementary measurements that cannot directly replace each other in the workup of pSS.
Funding: No specific funding was received from any bodies in the public, commercial or not -for- profit sectors to carry out the work described in this article.
Disclosure statement: The authors have declared no conflicts of interest. The authors state that the study complies with the Declaration of Helsinki. Informed consent and local ethical approval was not required by the Dutch Law for Medical Research and by institutional guidelines. No objection against the use of redundant diagnostic material was recorded from patients in the institutional record of objection. Patient material was handled according to the Code of Conduct for Health Research of the Dutch Federation of Biomedical Scientific Societies. In addition, patients were included in one of our research cohorts: REgistry of Sjögren syndrome in UMCG LongiTudinal (RESULT) cohort (METc 2014.491), Biomarker cohort (METc 2013.066) and Abatacept Sjögren Active Patients phase III (ASAPIII) cohort (METc 2014.118).
Data availability statement
All data underlying this article are included in the article and in its online supplementary material. The data that support this study are available on a reasonable request to the corresponding author.
Supplementary data
Supplementary data are available at Rheumatology online.
Supplementary Material
Contributor Information
Esther Mossel, Department of Rheumatology and Clinical Immunology.
Martha S van Ginkel, Department of Rheumatology and Clinical Immunology.
Erlin A Haacke, Department of Rheumatology and Clinical Immunology; Department of Pathology and Medical Biology.
Suzanne Arends, Department of Rheumatology and Clinical Immunology.
Silvia C Liefers, Department of Rheumatology and Clinical Immunology.
Konstantina Delli, Department of Oral and Maxillofacial Surgery, University of Groningen and University Medical Center Groningen, Groningen, The Netherlands.
Jolien F van Nimwegen, Department of Rheumatology and Clinical Immunology.
Alja J Stel, Department of Rheumatology and Clinical Immunology.
Fred K L Spijkervet, Department of Oral and Maxillofacial Surgery, University of Groningen and University Medical Center Groningen, Groningen, The Netherlands.
Arjan Vissink, Department of Oral and Maxillofacial Surgery, University of Groningen and University Medical Center Groningen, Groningen, The Netherlands.
Bert van der Vegt, Department of Pathology and Medical Biology.
Frans G M Kroese, Department of Rheumatology and Clinical Immunology.
Hendrika Bootsma, Department of Rheumatology and Clinical Immunology.
References
- 1. Brito-Zerón P, Baldini C, Bootsma H et al. Sjögren syndrome. Nat Rev Dis Primers 2016;2:16047. [DOI] [PubMed] [Google Scholar]
- 2. Shiboski CH, Shiboski SC, Seror R et al. 2016 American College of Rheumatology/European League Against Rheumatism classification criteria for primary Sjögren’s syndrome: a consensus and data-driven methodology involving three international patient cohorts. Ann Rheum Dis 2017;76:9–16. [DOI] [PubMed] [Google Scholar]
- 3. van Nimwegen J, Mossel E, Delli K et al. Incorporation of salivary gland ultrasonography into the ACR-EULAR criteria for primary Sjögren’s syndrome. Arthritis Care Res 2020;72:583–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jousse-Joulin S, Gatineau F, Baldini C et al. Weight of salivary gland ultrasonography compared to other items of the 2016 ACR/EULAR classification criteria for primary Sjögren’s syndrome. J Intern Med 2020;287:180–8. [DOI] [PubMed] [Google Scholar]
- 5. Chisholm DM, Mason DK. Labial salivary gland biopsy in Sjögren’s disease. J Clin Pathol 1968;21:656–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fisher BA, Jonsson R, Daniels T et al. Standardisation of labial salivary gland histopathology in clinical trials in primary Sjögren’s syndrome. Ann Rheum Dis 2017;76:1161–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kroese FGM, Haacke EA, Bombardieri M. The role of salivary gland histopathology in primary Sjögren’s syndrome: promises and pitfalls. Clin Exp Rheumatol 2018;36:S222–33. [PubMed] [Google Scholar]
- 8. Risselada AP, Looije MF, Kruize AA, Bijlsma JWJ, van Roon JAG. The role of ectopic germinal centers in the immunopathology of primary Sjögren’s syndrome: a systematic review. Semin Arthritis Rheum 2013;42:368–76. [DOI] [PubMed] [Google Scholar]
- 9. Ihrler S, Zietz C, Sendelhofert A, Riederer A, Löhrs U. Lymphoepithelial duct lesions in Sjogren-type sialadenitis. Virchows Arch 1999;434:315–23. [DOI] [PubMed] [Google Scholar]
- 10. Zandbelt M, Wentink J, de Wilde P et al. The synergistic value of focus score and IgA% score of sublabial salivary gland biopsy for the accuracy of the diagnosis of Sjögren’s syndrome: a 10-year comparison. Rheumatology (Oxford) 2002;41:819–23. [DOI] [PubMed] [Google Scholar]
- 11. Bodeutsch C, de Wilde PCM, Kater L et al. Quantitative immunohistologic criteria are superior to the lymphocytic focus score criterion for the diagnosis of Sjögren’s syndrome. Arthritis Rheum 1992;35:1075–87. [DOI] [PubMed] [Google Scholar]
- 12. Llamas-Gutierrez FJ, Reyes E, Martínez B, Hernández-Molina G. Histopathological environment besides the focus score in Sjögren’s syndrome. Int J Rheum Dis 2014;17:898–903. [DOI] [PubMed] [Google Scholar]
- 13. Leehan K, Pezant N, Rasmussen A et al. Minor salivary gland fibrosis in Sjögren’s syndrome is elevated, associated with focus score and not solely a consequence of aging. Clin Exp Rheumatol 2018;36(Suppl 112):80–8. [PMC free article] [PubMed] [Google Scholar]
- 14. Leehan K, Pezant N, Rasmussen A et al. Fatty infiltration of the minor salivary gland is a selective feature of aging but not Sjögren’s syndrome. Autoimmunity 2017;50:451–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Skarstein K, Aqrawi L, Øijordsbakken G, Jonsson R, Jensen J. Adipose tissue is prominent in salivary glands of Sjögren’s syndrome patients and appears to influence the microenvironment in these organs. Autoimmunity 2016;49:338–46. [DOI] [PubMed] [Google Scholar]
- 16. Pijpe J, Kalk WWI, van der Wal JE et al. Parotid gland biopsy compared with labial biopsy in the diagnosis of patients with primary Sjogren’s syndrome. Rheumatology (Oxford) 2007;46:335–41. [DOI] [PubMed] [Google Scholar]
- 17. Delli K, Vissink A, Spijkervet FKL. Salivary gland biopsy for Sjögren’s syndrome. Oral Maxillofac Surg Clin North Am 2014;26:23–33. [DOI] [PubMed] [Google Scholar]
- 18. Jensen SB, Vissink A. Salivary gland dysfunction and xerostomia in Sjögren’s syndrome. Oral Maxillofac Surg Clin North Am 2014;26:35–53. [DOI] [PubMed] [Google Scholar]
- 19. Delli K, Dijkstra PU, Stel AJ et al. Diagnostic properties of ultrasound of major salivary glands in Sjögren’s syndrome: a meta-analysis. Oral Dis 2015;21:792–800. [DOI] [PubMed] [Google Scholar]
- 20. Jousse-Joulin S, Milic V, Jonsson M. V et al. Is salivary gland ultrasonography a useful tool in Sjögren’s syndrome? A systematic review. Rheumatology (Oxford) 2016;55:789–800. [DOI] [PubMed] [Google Scholar]
- 21. Hocčevar A, Ambrožič A, Rozman B, Kveder T, Tomšič M. Ultrasonographic changes of major salivary glands in primary Sjögren’s syndrome. Diagnostic value of a novel scoring system. Rheumatology (Oxford) 2005;44:768–72. [DOI] [PubMed] [Google Scholar]
- 22. Mossel E, Arends S, van Nimwegen JF et al. Scoring hypoechogenic areas in one parotid and one submandibular gland increases feasibility of ultrasound in primary Sjögren’s syndrome. Ann Rheum Dis 2018;77:556–62. [DOI] [PubMed] [Google Scholar]
- 23. Daniels TE, Cox D, Shiboski CH et al. Associations between salivary gland histopathologic diagnoses and phenotypic features of Sjögren’s syndrome among 1,726 registry participants. Arthritis Rheum 2011;63:2021–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bookman AAM, Shen H, Cook RJ et al. Whole stimulated salivary flow: correlation with the pathology of inflammation and damage in minor salivary gland biopsy specimens from patients with primary Sjögren’s syndrome but not patients with sicca. Arthritis Rheum 2011;63:2014–20. [DOI] [PubMed] [Google Scholar]
- 25. Fisher BA, Brown RM, Bowman SJ, Barone F. A review of salivary gland histopathology in primary Sjögren’s syndrome with a focus on its potential as a clinical trials biomarker. Ann Rheum Dis 2015;74:1645–50. [DOI] [PubMed] [Google Scholar]
- 26. Atkinson J, Travis W, Pillemer S et al. Major salivary gland function in primary Sjögren’s syndrome and its relationship to clinical features. J Rheumatol 1990;17:318–22. [PubMed] [Google Scholar]
- 27. Kim JW, Lee H, Park SH et al. Salivary gland ultrasonography findings are associated with clinical, histological, and serologic features of Sjögren’s syndrome. Scand J Rheumatol 2018;47:303–10. [DOI] [PubMed] [Google Scholar]
- 28. Caraba A, Babalic FC, Iurciuc S, Iurciuc M, Mynbaev OA. The utility of major salivary gland ultrasonographic parameters in the diagnosis of Sjögren syndrome. Dis Markers 2019;2019:1716848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cornec D, Jousse-Joulin S, Costa S et al. High-grade salivary-gland involvement, assessed by histology or ultrasonography, is associated with a poor response to a single rituximab course in primary Sjögren’s syndrome: data from the TEARS randomized trial. PLoS One 2016;11:e0162787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Federation of Dutch Medical Scientific Societies. Human Tissue and Medical Research: Code of Conduct for responsible use. 2011. https://www.bbmri.nl/sites/bbmri/files/styles/Federa_code_of_conduct_english.pdf.
- 31. Haacke EA, van der Vegt B, Vissink A et al. Germinal centres in diagnostic labial gland biopsies of patients with primary Sjogren’s syndrome are not predictive for parotid MALT lymphoma development. Ann Rheum Dis 2017;76:1781–6. [DOI] [PubMed] [Google Scholar]
- 32. Nakshbandi U, Haacke EA, Bootsma H et al. Bcl6 for identification of germinal centres in salivary gland biopsies in primary Sjögren’s syndrome. Oral Dis 2020;26:707–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Pedersen AM, Bardow A, Beier Jensen S, Nantofte B. Saliva and gastrointestinal functions of taste, mastication, swallowing and digestion. Oral Dis 2002;8:117–29. [DOI] [PubMed] [Google Scholar]
- 34. Delli K, Arends S, van Nimwegen JF et al. Ultrasound of the major salivary glands is a reliable imaging technique in patients with clinically suspected primary Sjögren’s syndrome. Ultraschall Med 2018;39:328–33. [DOI] [PubMed] [Google Scholar]
- 35. Mossel E, Delli K, van Nimwegen JF et al. Ultrasonography of major salivary glands compared with parotid and labial gland biopsy and classification criteria in patients with clinically suspected primary Sjögren’s syndrome. Ann Rheum Dis 2017;76:1883–9. [DOI] [PubMed] [Google Scholar]
- 36. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–74. [PubMed] [Google Scholar]
- 37. Terwee CB, Bot SDM, de Boer MR et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007;60:34–42. [DOI] [PubMed] [Google Scholar]
- 38. Burlage FR, Pijpe J, Coppes RP, Hemels MEW et al. Variability of flow rate when collecting stimulated human parotid saliva. Eur J Oral Sci 2005;113:386–90. [DOI] [PubMed] [Google Scholar]
- 39. Baum BJ. Salivary gland fluid secretion during aging. J Am Geriatr Soc 1989;37:453–8. [DOI] [PubMed] [Google Scholar]
- 40. Kariyawasam AP, Dawes C. A circannual rhythm in unstimulated salivary flow rate when the ambient temperature varies by only about 2°C. Arch Oral Biol 2005;50:919–22. [DOI] [PubMed] [Google Scholar]
- 41. Izzetti R, Ferro F, Vitali S et al. Ultra-high frequency ultrasonography (UHFUS)-guided minor salivary gland biopsy: a promising procedure to optimize labial salivary gland biopsy in Sjögren’s syndrome. J Oral Pathol Med 2021;50:485–91. [DOI] [PubMed] [Google Scholar]
- 42. Wernicke D, Hess H, Gromnica-Ihle E, Krause A, Schmidt WA. Ultrasonography of salivary glands— a highly specific imaging procedure for diagnosis of Sjögren’s syndrome. J Rheumatol 2008;35:285–93. [PubMed] [Google Scholar]
- 43. Takashima S, Morimoto S, Tomiyama N et al. Sjogren syndrome: comparison of sialography and ultrasonography. J Clin Ultrasound 1992;20:99–109. [DOI] [PubMed] [Google Scholar]
- 44. Wang X, Bootsma H, Terpstra J et al. Progenitor cell niche senescence reflects pathology of the parotid salivary gland in primary Sjögren’s syndrome. Rheumatology (Oxford) 2020;59:3003–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hammenfors DS, Brun JG, Jonsson R, Jonsson M. V. Diagnostic utility of major salivary gland ultrasonography in primary Sjögren’s syndrome. Clin Exp Rheumatol 2015;33:56–62. [PubMed] [Google Scholar]
- 46. Jousse-Joulin S, D’Agostino MA, Nicolas C et al. Video clip assessment of a salivary gland ultrasound scoring system in Sjögren’s syndrome using consensual definitions: an OMERACT ultrasound working group reliability exercise. Ann Rheum Dis 2019;78:967–73. [DOI] [PubMed] [Google Scholar]
- 47. Fisher BA, Emery P, Pitzalis C, Bombardieri M, Bowman SJ. Response to: can ultrasound of the major salivary glands assess histopathological changes induced by treatment with rituximab in primary Sjögren’s syndrome? Ann Rheum Dis 2019;78:e28. [DOI] [PubMed] [Google Scholar]
- 48.Zabotti A, Zandonella Callegher S, Tullio A et al. Salivary gland ultrasonography in Sjögren’s syndrome: a European multicenter reliability exercise for the HarmonicSS project. Front Med 2020;7:e581248. [DOI] [PMC free article] [PubMed]
- 49. Baer AN, Grader-Beck T, Antiochos B, Birnbaum J, Fradin JM. Ultrasound-guided biopsy of suspected salivary gland lymphoma in Sjögren’s syndrome. Arthritis Care Res 2021;73:849–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Yalcinkaya Y, Mumcu G, Özdemir FT et al. Are salivary gland ultrasonography scores associated with salivary flow rates and oral health-related quality of life in Sjögren syndrome? J Rheumatol 2020;47:1774–9. [DOI] [PubMed] [Google Scholar]
- 51. Pijpe J, Kalk WWI, Bootsma H et al. Progression of salivary gland dysfunction in patients with Sjögren’s syndrome. Ann Rheum Dis 2006;66:107–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data underlying this article are included in the article and in its online supplementary material. The data that support this study are available on a reasonable request to the corresponding author.