Abstract
Portal vein recanalization-transjugular intrahepatic portosystemic shunt (PVR-TIPS) is a valuable technique in the treatment cirrhosis and portal vein (PV) thrombosis. Only a few studies have reported cases of utilizing the transmesenteric approach in the procedure's initial portal access. Here, we report the successful utilization of a CT-guided percutaneous puncture of the superior mesenteric vein (SMV) for PVR-TIPS in a patient with splenic vein thrombosis. A 54-year-old male with a history of morbid obesity (BMI: 44.67), hepatitis C, NASH cirrhosis, esophageal varices, and complete PV thrombosis presented for PVR-TIPS. An initial percutaneous transplenic approach was attempted, but was aborted due to the discovery of a splenic vein thrombosis. Subsequently, the patient was brought back into the hybrid-angio CT suite, and the SMV was accessed percutaneously with a 21-gauge needle under 4D CT-guidance. A 5-Fr micropuncture sheath was then placed. Additional portal venogram confirmed PV thrombosis. Right internal jugular vein (IJV) access was then obtained, and the right hepatic vein was catheterized. A loop snare was advanced from the SMV access into the right PV. A Colapinto needle was later positioned in the right hepatic vein, and the right PV was accessed using the loop snare as a target. A wire was then advanced and captured by the snare, and brought down through the PV. The tract was dilated with a 10 mm balloon, and a Viatorr stent was deployed. Balloon embolectomy of the SMV, splenomesenteric vein, and TIPS were then performed with a CODA balloon with improvement in flow through the TIPS on final portal venogram. Portosystemic gradient was 11 mmHg initially and 10 mmHg post-TIPS. Follow-up TIPS venogram in 3 weeks showed a widely patent TIPS. CT-guided percutaneous SMV access may serve as valuable technique in PVR-TIPS when traditional modes of initial portal access for recanalization are unobtainable.
Keywords: Portal Vein Recanalization, TIPS, CT, Transmesenteric Access, Transhepatic Access, Transplenic Access
Background
Portal vein recanalization-transjugular intrahepatic portosystemic shunt (PVR-TIPS) is an indispensable technique in the treatment of portal vein (PV) thrombosis and cirrhosis. By restoring portal venous flow and facilitating the placement of a portohepatic shunt, PVR-TIPS provides an effective bridge to liver transplantation [1]. Over the past few years, the percutaneous transplenic access of the PV has gained immense popularity over the percutaneous transhepatic approach in regards to technical success of PVR-TIPS [2], [3]. However, in cases where neither the transplenic or transhepatic routes are accessible another avenue is certainly warranted.
Previous literature has explored transmesenteric access via minilaparotomy, but also cautiously warned us of the extreme surgical risks associated with this option [4]. Recently, a study has observed the successful completion of PVR-TIPS via a percutaneous transmesenteric approach [5]. However, these attempts were solely conducted through ultrasound (US) guidance, which at times can be limited by factors such as operator experience and patient BMI [6]. In these instances, computed tomography (CT) remains a viable approach. To the authors’ knowledge, the feasibility of CT in guiding transabdominal access has not been applied to PVR-TIPS. Here, we report the utilization of a CT-guided percutaneous puncture of the superior mesenteric vein (SMV) for PVR-TIPS in a patient with a splenic vein thrombosis.
Case Presentation
A 54-year-old male with a history of morbid obesity (BMI: 44.67), hepatitis C, NASH cirrhosis, esophageal varices, and complete PV thrombosis presented for PVR-TIPS. An initial percutaneous transplenic approach was attempted, but was aborted due to the discovery of a splenic vein thrombosis (Fig. 1). After a multidisciplinary discussion ensued, the patient was brought back into a 4D CT or hybrid angio-CT suite (Canon, Tustin, CA) to undergo percutaneous transmesenteric access.
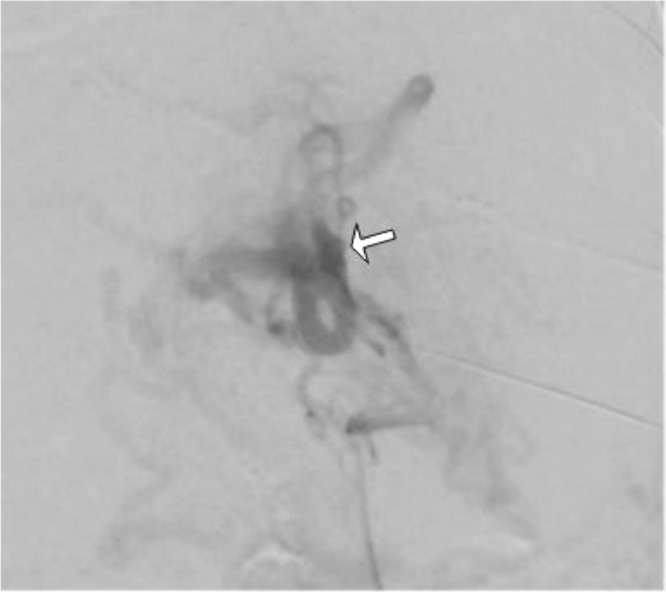
Fig. 1.
Percutaneous transplenic venogram displays occlusion (indicated by white arrow) of the splenic vein
Using CT-guidance, a 21-gauge needle (Cook, Bloomington, IN) was advanced trans-abdominally into the SMV (Fig. 2). A 5-Fr micropuncture sheath (Cook, Bloomington, IN) was then later placed. A subsequent portal venogram confirmed portal vein thrombosis (Fig. 3). A right internal jugular vein (IJV) access was then obtained, and the right hepatic vein was catheterized. A loop snare (Argon, Frisco, TX) was advanced from the SMV access into the right portal vein (Fig. 4). A Colapinto needle (Cook, Bloomington, IN) was then positioned in the right hepatic vein, and the right portal vein was accessed using the loop snare as a target (Fig. 5). A wire was then advanced and captured by the snare, and later brought down through the portal vein. The tract was subsequently dilated with a 10 mm balloon, and a 10 mm x 70 mm Viatorr stent (W.L Gore & Associates, Flagstaff, Arizona) was deployed. Balloon embolectomy of the SMV, splenomesenteric vein, and TIPS was then performed with a CODA balloon (Cook, Bloomington, IN). A final portal venogram revealed a patent TIPS as well as an improvement in flow through the portal vasculature (Fig. 6). The portosystemic gradient was 11 mmHg initially, and was 10 mmHg post-TIPS. After 3 weeks from initial placement, a follow-up venogram still demonstrated a widely patent TIPS (Fig. 7).
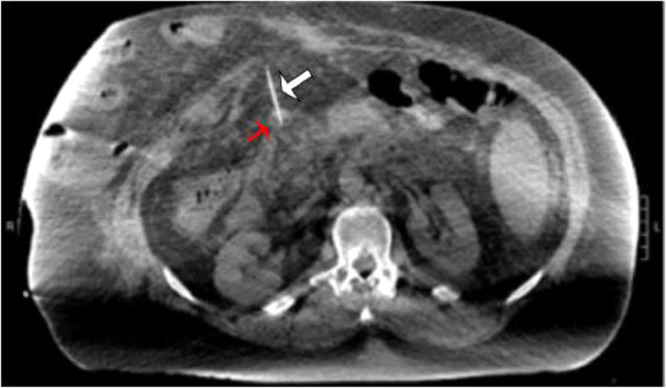
Fig. 2.
Axial CT fluoroscopy shows direct percutaneous access of the SMV (red arrow) using a 21-gauge needle (white arrow). (Color version of figure is available online.)
Fig. 3.
Direct portal vein injection shows PV thrombosis (white arrow)
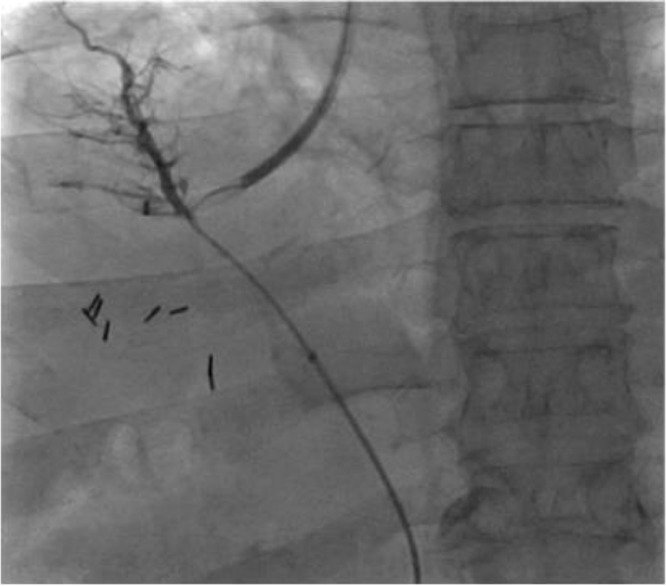
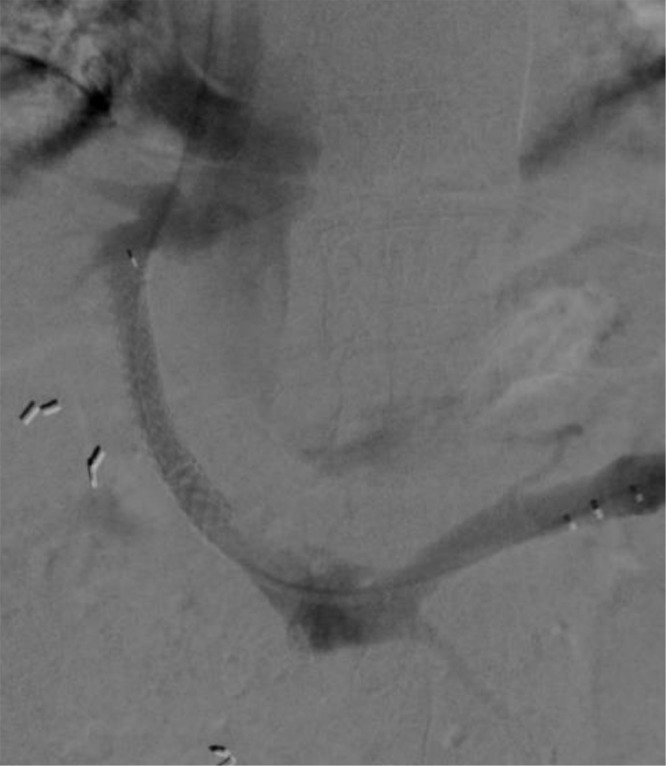
Fig. 4.
Right hepatic venogram was performed from right IJV access. A loop snare was positioned in the PV from the SMV access
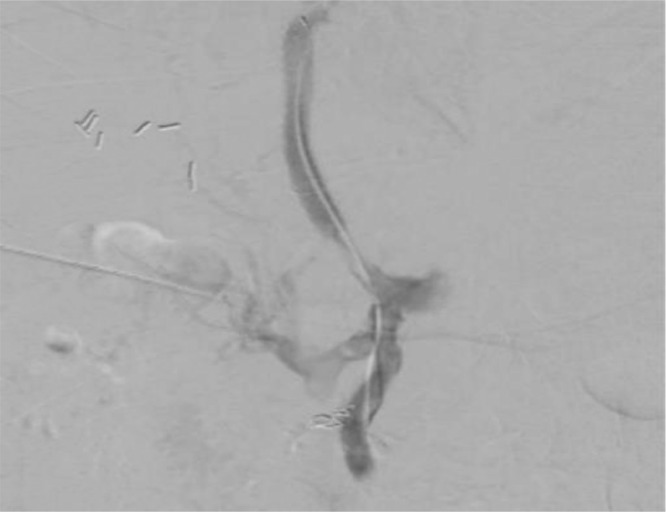
Fig. 5.
Through and through wire access from the right hepatic vein to the right PV was obtained using the loop snare as a target
Fig. 6.
Final portal venogram directly after the procedure showcased a widely patent TIPS
Fig. 7.
TIPS venogram 3 weeks after initial placement also demonstrated a widely patent TIPS
Conclusion
PVR-TIPS remains a valuable technique in the treatment of PV thrombosis and cirrhosis. In regards to accessing the PV for reconstruction in this procedure, the traditional percutaneous transhepatic method comes with a couple drawbacks. First, the approach is predicated on the PV not being occluded, and the PV intrahepatic branches being sufficiently patent [7], [8]. Second, transhepatic access increases the risk of tumor seeding in the event of a largely infiltrated tumor in the path of puncture [9]. Similar to the transhepatic approach, the percutaneous transplenic method also has its limitations such as being inaccessible in splenic vein thrombosis (like this case) or asplenia. In instances where neither of the above routes are feasible, percutaneous SMV access remains a worthwhile option, especially considering its early success [5]. One particular highlight to this approach centers on the anatomy of the SMV in relation to the PV. Unlike the splenic vein in transplenic access or many of the intrahepatic PV branches in transhepatic access, the SMV is nearly vertically in line with the PV [4]. This allows operators to obtain portal access in a hypothetically efficient way, potentially contributing to lower fluoroscopy use, quicker turnaround for PVR-TIPS, and easier maneuverability within the portal system to conduct related procedures (ie, occluding gastroesophageal varices). Nonetheless, a large clinical trial is necessary to confirm whether transmenteric access truly possesses these advantages over transhepatic and/or transplenic access.
Previously reported cases on percutaneous transmesenteric access centered on ultrasound technology, which is not always the ideal form of guidance. Ultrasound use is entirely operator-dependent, and poses significant technical challenges in obese patients [6]. Meanwhile, CT is a readily available alternative that is not as highly skill dependent, and can easily accommodate larger individuals such as our individual in this case [6]. In addition, CT has been shown to provide better visualization than US in some hepatoportal anatomy in TIPS candidates [10]. In one study, CT scored higher than US in detecting PV branches and the splenic vein [10]. Also, CT was shown to be more sensitive than US in detecting varices, and spontaneous shunts [10]. By improving hepatoportal visualization, CT can increase the technical success rate of PVR-TIPS, and optimize operator decision-making skills in procedure. Like US, CT has its own limitations such as increased radiation exposure, and the inability to capture real-time vessel flow (ie, PV). Nonetheless, CT, whenever appropriate, can serve as a valuable modality in the interventional radiologists’ arsenal for PVR-TIPS via percutaneous SMV access.
Patient consent
We declare that the patient described in this study gave informed consent prior to inclusion in this study.
Compliance with Ethical Standards Yes
Consent for Publication Consent for publication was obtained for every individual person's data included in the study.
IRB Status IRB Exempt
Footnotes
Acknowledgments: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Salem R., Vouche M., Baker T. Pretransplant portal vein recanalization—transjugular intrahepatic portosystemic shunt in patients with complete obliterative portal vein thrombosis. Transplantation. 2015;99(11):2347–2355. doi: 10.1097/TP.0000000000000729. [DOI] [PubMed] [Google Scholar]
- 2.Kallini J.R., Gabr A., Kulik L. Noncirrhotic complete obliterative portal vein thrombosis: novel management using trans-splenic transjugular intrahepatic portosystemic shunt with portal vein recanalization. Hepatology. 2016;63(4):1387–1390. doi: 10.1002/hep.28429. [DOI] [PubMed] [Google Scholar]
- 3.Habib A., Desai K., Hickey R. Portal vein recanalization–transjugular intrahepatic portosystemic shunt using the transsplenic approach to achieve transplant candidacy in patients with chronic portal vein thrombosis. J Vasc Interv Radiol. 2015;26(4):499–506. doi: 10.1016/j.jvir.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 4.Rozenblit G, Del Guercio Louis R.N. Combined transmesenteric and transjugular approach for intrahepatic portosystemic shunt placement. J Vasc Interv Radiol. 1993;4(5):661–666. doi: 10.1016/s1051-0443(93)71942-9. [DOI] [PubMed] [Google Scholar]
- 5.Entezari P., Riaz A., Thornburg B. Percutaneous ultrasound-guided superior and inferior mesenteric vein access for portal vein recanalization–transjugular intrahepatic portosystemic shunt: a case series. Cardiovasc Intervent Radiol. 2021;44:496–499. doi: 10.1007/s00270-020-02713-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Modica M.J., Kanal K.M., Gunn M.L. The obese emergency patient: imaging challenges and solutions. RadioGraphics. 2011;31(3):811–823. doi: 10.1148/rg.313105138. [DOI] [PubMed] [Google Scholar]
- 7.Cheng Y.F., Ou H.Y., Tsang L.C. Vascular stents in the management of portal venous complications in living donor liver transplantation. Am J Transplant. 2010;10:1276–1283. doi: 10.1111/j.1600-6143.2010.03076.x. [DOI] [PubMed] [Google Scholar]
- 8.Han G.H., Qi X.H., He C.Y. Transjugular intrahepatic portosystemic shunt for portal vein thrombosis with symptomatic portal hypertension in liver cirrhosis. J Hepatol. 2011;54:78–88. doi: 10.1016/j.jhep.2010.06.029. [DOI] [PubMed] [Google Scholar]
- 9.Silva M.A., Hegab B., Hyde C., Guo B., Buckels J.A., Mirza D.F. Needle tract seeding following biopsy of liver lesions in the diagnosis of hepatocellular cancer: a systematic review and meta-analysis. Gut. 2008;57:1592–1596. doi: 10.1136/gut.2008.149062. [DOI] [PubMed] [Google Scholar]
- 10.Kraus B.B., Ros P.R., Abbitt P.L. Comparison of ultrasound, CT, and MR imaging in the evaluation of candidates for TIPS. J Magn Reson Imaging. 1995;5(5):571–578. doi: 10.1002/jmri.1880050517. [DOI] [PubMed] [Google Scholar]