Key Points
Question
What is the association between marital status and mortality outcomes in Asian populations?
Findings
In this cohort study of 623 140 individuals from 16 prospective cohorts participating in the Asia Cohort Consortium, a pooled analysis found that being unmarried was associated with a higher risk of all-cause and cause-specific mortality, compared with being married. The excess risks of death persisted across health conditions and were particularly pronounced among men and people younger than 65 years.
Meaning
These findings highlight that being unmarried substantially increases the risk of death among Asian individuals.
This cohort study examines the association of marital status with total and cause-specific mortality in Asian populations.
Abstract
Importance
Marital status has been shown to be associated with mortality, but evidence in Asian populations is limited.
Objective
To examine the association of marital status with total and cause-specific mortality.
Design, Setting, and Participants
This cohort study included individual participant data from 16 prospective studies in the Asia Cohort Consortium conducted between 1963 and 2015. Asian participants with complete information on marital and vital status were included. Study-specific hazard ratios (HRs) and 95% CIs were estimated using Cox proportional hazards model and then pooled using a random-effects meta-analysis. The analysis began in February 2021 and ended in August 2021.
Exposures
Marital status.
Main Outcomes and Measures
All-cause and cause-specific mortality.
Results
Of 623 140 participants (326 397 women [52.4%] and 296 743 men [47.6%]; mean [SD] age, 53.7 [10.2] years; mean [SD] follow-up time, 15.5 [6.1] years), 123 264 deaths were ascertained. Compared with married individuals, those who were unmarried had pooled HRs of 1.15 (95% CI, 1.07-1.24) for total mortality, 1.12 (95% CI, 1.03-1.22) for cerebrovascular disease mortality, 1.20 (95% CI, 1.09-1.31) for coronary heart disease mortality, 1.17 (95% CI, 1.07-1.28) for circulatory system diseases mortality, 1.06 (95% CI, 1.01-1.11) for cancer mortality, 1.14 (95% CI, 1.05-1.23) for respiratory diseases mortality, and 1.19 (95% CI, 1.05-1.34) for external causes of death. Positive associations with total mortality were also observed for those who were single (HR, 1.62; 95% CI, 1.41-1.86), separated (HR, 1.35; 95% CI, 1.13-1.61), divorced (HR, 1.38; 95% CI, 1.13-1.69), and widowed (HR, 1.09; 95% CI, 1.04-1.13). In subgroup analyses, the positive association persisted across baseline health conditions, and the risk of death was more pronounced among men or people younger than 65 years.
Conclusions and Relevance
This large pooled cohort study of individual participant data provides strong evidence that being unmarried, as well as belonging to the unmarried subcategories, was positively associated with total and cause-specific mortality. Investment of targeted social support services might need to be considered in light of the mortality differences between married and unmarried individuals.
Introduction
Globally, the marriage rate has decreased over the last decades.1 There is broad agreement on the association of marital status with mortality.2,3,4 A recent meta-analysis3 showed that individuals who were unmarried had a higher risk of all-cause and cause-specific mortality than their married counterparts. Achieving socioeconomic support and health-promoting behaviors have been implicated to be the factors contributing to these protective associations of marriage.5,6,7,8,9 Physiologically, a higher level of cortisol and a flatter diurnal cortisol slope are found in unmarried individuals,10 which are linked to an increased risk of carotid atherosclerosis,11 poor glycemic control in patients with diabetes,12 metabolic syndrome,13 and shorter survival time in patients with cancer.14,15
Although the pattern of marriage differs among societies, few studies have reported the linkage between marriage and mortality in non-Western populations.16,17,18,19,20 Marriages in East Asia have distinct features, including a strong tradition of extended family coresidence, an emphasis on family lineage that stabilizes the institution of marriage, and strong family ties,21 which have been associated with lower mortality risk.22 In addition, the pronounced marital selection outcomes and financial burden of single-earner households in Asian society have been suggested as factors associated with higher mortality among single Asian individuals.23 Together, we hypothesized that being married would be associated with survival benefits in Asian populations. Nevertheless, previous studies16,17,18,19,20 of Asian cohorts have published inconsistent results. It is also noteworthy that, in previous investigations, there were concerns regarding the potential effects of reverse causation, where initial presentation of undiagnosed diseases may influence the likelihood of marriage dissolution.24 In addition, the association may differ across participant subgroups. Prior studies investigating potential modifying effects of age and sex demonstrated mixed results.3,25,26,27,28,29 With most studies focused on the generally healthy population,3 less is known regarding the mortality differences by marital status among individuals with chronic diseases. Given the increasing prevalence of noncommunicable diseases in Asian countries,30 it is imperative to understand whether the association between marital status and mortality differs among people with underlying comorbidity. We therefore conducted a cohort study using individual-level data from the Asia Cohort Consortium (ACC), with more than 1 million participants, to ascertain the association between marital status and cause-specific mortality.
Methods
Study Population
The ACC was established to foster collaborative epidemiological research in Asian countries using pooled multicenter cohort data. The ACC currently contains individual-level data from more than 1 million participants. Of 23 prospective cohort studies in the ACC, we used data from 16 cohorts with available data on marital status. The study designs of the included cohorts have been described elsewhere.31 Participating cohorts from 5 countries were included: Mainland China, Shanghai Cohort Study, Shanghai Men’s Health Study, and Shanghai Women’s Health Study; Japan, Japan Collaborative Cohort Study, Japan Public Health Center-Based Prospective Study, Miyagi Cohort Study, Ohsaki National Health Insurance Cohort Study, Life Span Study Cohort–Radiation Effects Research Foundation, and Takayama Study; Republic of Korea, Korea Multi-Center Cancer Cohort Study, Korea National Cancer Center Cohort, and Seoul Male Cancer Cohort; Singapore, Singapore Chinese Health Study; and Taiwan, Community-Based Cancer Screening Project and Cardiovascular Disease Risk Factor Two-Township Study. Of the 681 533 potential participants, we excluded those with missing information on marital status (37 600 individuals) or vital status (20 793 individuals). This study was approved by the ethics committees of each cohort study and by the institutional review board of the ACC coordinating center. Informed consent (either written or oral, depending on the cohort) was obtained from all participants per study cohort. This study follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Assessment of Exposure and Other Covariates
Cohort questionnaires at baseline assessed information on lifestyle factors, sociodemographic characteristics, diet, and medical history of type 2 diabetes, hypertension, cancer, coronary heart disease, and cerebrovascular disease. Among 16 cohorts included, participants from Korea National Cancer Center Cohort, Korea Multi-Center Cancer Cohort Study, Community-Based Cancer Screening Project, and Cardiovascular Disease Risk Factor Two-Township Study were interviewed by trained interviewers, whereas the other cohorts used self-administered questionnaires. Brief descriptions of participating cohorts are presented in eTable 1 in the Supplement. Information on marital status from each cohort was harmonized and classified into 5 categories: married, single, separated, widowed, and divorced. Analyses for subcategories of unmarried status (single, separated, widowed, and divorced) were performed where data were available (eAppendix in the Supplement).
Outcome Ascertainment
Our primary end point was death from all causes. Deaths were ascertained via linkage to the death certificates or active follow-up. The causes of death were classified using the International Classification of Diseases, Ninth Revision or International Classification of Diseases, Tenth Revision (eAppendix in the Supplement).
Statistical Analysis
In this study, we performed a 2-stage meta-analysis of individual participant data to estimate the pooled hazard ratios (HRs) and 95% CIs.32 First, a Cox proportional hazards regression model with age as the time scale was used to estimate HRs and 95% CIs across marital status categories by cohorts. Married individuals were the reference group. Time of entry was age at the baseline interview, and exit time was age at death or last follow-up, whichever came first. The multivariable model was adjusted for potential confounders, including sex, age at baseline (year, continuous), education (no formal education or primary education, secondary education, trade or technical education, university education or above, and missing), smoking status (never, former, current, and missing), alcohol intake (nondrinker, drinker, and missing), physical activity (none or almost none, low, intermediate, high, and missing), and baseline health conditions (cerebrovascular disease, coronary heart disease, cancer, hypertension, and diabetes). We used missing indicator variables to code missing values for potential confounders. Second, we obtained the overall estimates using random-effects meta-analysis. To minimize the bias due to reverse causation, we repeated the analyses and excluded deaths occurring within the first 5 years of follow-up.
We performed prespecified stratified analysis according to age at baseline (<65 and ≥65 years), sex (men and women), health status (prior diagnosis of cancer, cerebrovascular disease, or coronary heart disease; prior diagnosis of type 2 diabetes or hypertension but not cancer, cerebrovascular disease, or coronary heart disease; and healthy participants with none of the aforementioned diseases), birth year (before and after 1940), and country. Metaregression was used to test for effect modification. We used Stata statistical software version 16.0 (StataCorp) for analysis. All reported P values were 2-sided, and P < .05 was considered to be significant. Data analysis was performed from February to August 2021.
Results
A total of 623 140 participants were included in the analyses: 296 743 men (47.6%) and 326 397 women (52.4%). The mean (SD) age at baseline was 53.7 (10.2) years. During a mean (SD) follow-up of 15.5 (6.1) years, 123 264 deaths were ascertained, of which 37 394 were classified as death from circulatory system diseases, 8013 were from coronary heart disease, 14 563 were from cerebrovascular disease, 41 362 were from cancer, 13 583 were from respiratory diseases, and 7795 were from external causes. The mean prevalence of being married was 86.4% (538 377 individuals), ranging from 76.4% (36 046 individuals) in the Life Span Study Cohort–Radiation Effects Research Foundation to 98.7% (13 777 individuals) in the Seoul Male Cancer Cohort. Baseline characteristics of participants of each cohort are shown in Table 1 and eTable 2 in the Supplement.
Table 1. Characteristics of Participating Cohorts in the Asia Cohort Consortium.
| Country and cohort | Follow-up duration, mean (SD), y | Years of study entry | Participants, No. (%) | Age at entry, mean (SD), y | Married individuals, No. (%) | Cause of death, No. of individuals | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | All-cause | Circulatory system diseases | Cancer | Respiratory diseases | External | |||||
| Mainland China | |||||||||||
| SCS (n = 16 751) | 22.4 (8.2) | 1986-1989 | 16 751 (100.0) | 0 | 55.9 (5.7) | 15 853 (94.6) | 10 181 | 3768 | 3533 | 1210 | 269 |
| SMHS (n = 53 205) | 9.5 (1.7) | 2001-2006 | 53 205 (100.0) | 0 | 55.7 (9.7) | 51 761 (97.3) | 4558 | 1487 | 2020 | 331 | 104 |
| SWHS (n = 74 743) | 14.9 (2.2) | 1996-2000 | 0 | 74 743 (100.0) | 52.6 (9.1) | 66 345 (88.8) | 7458 | 2432 | 3134 | 303 | 207 |
| Japan | |||||||||||
| JACC (n = 74 989) | 12.8 (3.2) | 1988-1990 | 31 337 (41.8) | 43 652 (58.2) | 57.1 (10.0) | 65 829 (87.8) | 10 270 | 3096 | 3842 | 1157 | 733 |
| JPHC1 (n = 42 587) | 21.1 (4.2) | 1990-1992 | 20 352 (47.8) | 22 235 (52.2) | 49.6 (6.0) | 33 042 (77.6) | 7324 | 1807 | 2881 | 596 | 683 |
| JPHC2 (n = 55 841) | 17.8 (4.0) | 1992-1995 | 26 407 (47.3) | 29 434 (52.7) | 54.2 (8.8) | 47 112 (84.4) | 12 505 | 3150 | 4608 | 1436 | 846 |
| Miyagi (n = 37 921) | 22.5 (4.8) | 1990 | 18 919 (49.9) | 19 002 (50.1) | 51.9 (7.5) | 34 259 (90.3) | 11 549 | 2184 | 2809 | 862 | 2494 |
| Ohsaki (n = 26 950) | 11.7 (3.2) | 1995 | 14 609 (54.2) | 12 341 (45.8) | 58.0 (10.8) | 22 365 (83.0) | 7435 | 2177 | 2415 | 1007 | 203 |
| RERF (n = 47 200) | 22.0 (10.2) | 1963-1993 | 18 691 (39.6) | 28 509 (60.4) | 52.1 (13.6) | 36 046 (76.4) | 24 400 | 9007 | 6619 | 3210 | 667 |
| Takayama (n = 30 574) | 13.8 (3.8) | 1992 | 13 961 (45.7) | 16 613 (54.3) | 55.8 (12.8) | 25 076 (82.0) | 5818 | 1930 | 1698 | 810 | 372 |
| Republic of Korea | |||||||||||
| KMCC (n = 19 337) | 13.9 (4.5) | 1993-2004 | 7718 (39.9) | 11 619 (60.1) | 53.9 (14.5) | 14 920 (77.2) | 3577 | 835 | 1108 | 317 | 357 |
| KNCC (n = 37 638) | 9.3 (3.3) | 2001-2015 | 19 113 (50.8) | 18 525 (49.2) | 49.8 (9.2) | 33 946 (90.2) | 553 | 48 | 207 | 6 | 57 |
| Seoul-Male (n = 13 957) | 15.6 (1.8) | 1992-1993 | 13 957 (100.0) | 0 | 49.2 (5.2) | 13 777 (98.7) | 901 | 150 | 498 | 29 | 101 |
| Singapore, SCHS/SGC (n = 62 658) | 14.0 (3.6) | 1993-1999 | 27 593 (44.0) | 35 065 (56.0) | 56.4 (8.0) | 52 177 (83.3) | 13 238 | 4500 | 4715 | 2033 | 361 |
| Taiwan | |||||||||||
| CBCSP (n = 23 670) | 15.3 (2.5) | 1991-1992 | 11 883 (50.2) | 11 787 (49.8) | 47.3 (10.0) | 21 771 (92.0) | 2688 | 537 | 994 | 160 | 276 |
| CVDFACTS (n = 5119) | 15.0 (2.9) | 1990-1993 | 2247 (43.9) | 2872 (56.1) | 47.5 (15.6) | 4098 (80.1) | 809 | 213 | 214 | 83 | 55 |
| Total (N = 623 140) | 15.5 (6.1) | 1963-2015 | 296 743 (47.6) | 326 397 (52.4) | 53.7 (10.2) | 538 377 (86.4) | 123 264 | 37 321 | 41 295 | 13 550 | 7785 |
Abbreviations: CBCSP, Community-based Cancer Screening Project; CVDFACTS, Cardiovascular Diseases Risk Factor Two-Township Study; JACC, Japan Collaborative Cohort Study; JPHC, Japan Public Health Center-based prospective Study; KMCC, Korean Multi-center Cancer Cohort Study; KNCC, Korea National Cancer Center Cohort; Miyagi, Miyagi Cohort Study; Ohsaki, Ohsaki National Health Insurance Cohort Study; RERF, Life Span Study Cohort–Radiation Effects Research Foundation; SCHS/SGC, Singapore Chinese Health Study; SCS, Shanghai Cohort Study; Seoul-Male, Seoul Male Cancer Cohort; SMHS, Shanghai Men’s Health Study; SWHS, Shanghai Women’s Health Study; Takayama, Takayama Study.
Marital Status and Total Mortality
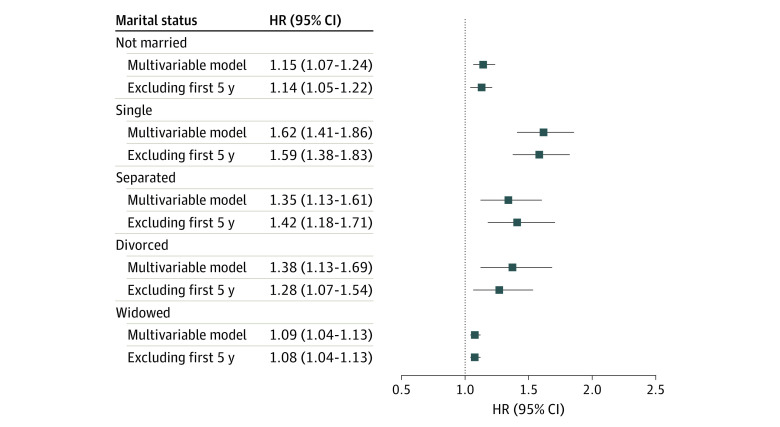
In multivariable analyses, being unmarried was associated with a 15% greater risk of all-cause mortality (pooled multivariable HR, 1.15; 95% CI, 1.07-1.24) compared with being married (Figure and eTable 3 in the Supplement). We further examined associations of subcategories of unmarried status with mortality. Compared with married participants, positive associations for death from all causes were found among those who were single (pooled HR, 1.62; 95% CI, 1.41-1.86), separated (pooled HR, 1.35; 95% CI, 1.13-1.61), divorced (pooled HR, 1.38; 95% CI, 1.13-1.69), and widowed (pooled HR, 1.09; 95% CI, 1.04-1.13). The associations remained positive when we excluded participants who died during the first 5 years of follow-up (Figure and eTable 3 in the Supplement).
Figure. Association of Marital Status With All-Cause Mortality Compared With Married Individuals in Asian Populations.
Multivariable Cox regression model was adjusted for sex, age at baseline (year, continuous), smoking status (never, former, current, and missing), education (no formal education or primary education, secondary education, trade or technical education, university education or above, and missing), physical activity (none or almost none, low, intermediate, high, and missing), alcohol intake (nondrinker, drinker, and missing), and baseline health conditions (cerebrovascular disease, coronary heart disease, cancer, hypertension, and diabetes). HR indicates hazard ratio.
Marital Status and Cause-Specific Mortality
The pooled multivariable HRs for unmarried compared with married individuals were 1.12 (95% CI, 1.03-1.22) for cerebrovascular disease mortality, 1.20 (95% CI, 1.09-1.31) for coronary heart disease mortality, 1.17 (95% CI, 1.07-1.28) for circulatory system diseases mortality, 1.06 (95% CI, 1.01-1.11) for cancer mortality, 1.14 (95% CI, 1.05-1.23) for respiratory diseases mortality, and 1.19 (95% CI, 1.05-1.34) for external causes of death (Table 2). Compared with those who were married, being single was associated with a greater risk of death from cerebrovascular disease, coronary heart disease, circulatory system diseases, cancer, respiratory diseases, and external causes (Table 2). Being widowed was associated with higher risks of death from cerebrovascular disease, coronary heart disease, circulatory system diseases, and external causes. There were higher risks of coronary heart disease mortality and external causes of death among separated participants. Being divorced was positively associated with risk of death from cerebrovascular disease, with similar magnitude of associations observed with risk of death from circulatory system diseases, respiratory diseases, and external causes (Table 2). Similar patterns were observed after the exclusion of mortality cases with the first 5 years of follow-up.
Table 2. Association of Marital Status With Risk of Cause-Specific Mortality in Asian Populations.
| Model and cause of death | Married (n = 538 377) | Not married (n = 84 763) | Single (n = 13 159) | Separated (n = 1168) | Divorced (n = 4671) | Widowed (n = 33 997) |
|---|---|---|---|---|---|---|
| Multivariable model | ||||||
| Cerebrovascular disease | ||||||
| Deaths, No. | 11 699 | 2864 | 339 | 18 | 99 | 1688 |
| HR (95% CI)a | 1 [Reference] | 1.12 (1.03-1.22) | 1.59 (1.22-2.06) | 1.01 (0.63-1.60) | 1.45 (1.18-1.79) | 1.08 (1.00-1.17) |
| Coronary heart disease | ||||||
| Deaths, No. | 6461 | 1552 | 188 | 15 | 49 | 882 |
| HR (95% CI)a | 1 [Reference] | 1.20 (1.09-1.31) | 1.72 (1.31-2.27) | 2.21 (1.32-3.71) | 1.40 (0.85-2.30) | 1.13 (1.01-1.26) |
| Circulatory system diseases | ||||||
| Deaths, No. | 29 721 | 7673 | 937 | 49 | 212 | 4348 |
| HR (95% CI)a | 1 [Reference] | 1.17 (1.07-1.28) | 1.68 (1.37-2.07) | 1.31 (0.98-1.74) | 1.56 (1.12-2.17) | 1.11 (1.04-1.17) |
| Cancer | ||||||
| Deaths, No. | 34 692 | 6670 | 877 | 55 | 213 | 3179 |
| HR (95% CI)a | 1 [Reference] | 1.06 (1.01-1.11) | 1.31 (1.17-1.45) | 1.25 (0.96-1.64) | 1.10 (0.93-1.30) | 1.04 (0.99-1.08) |
| Respiratory diseases | ||||||
| Deaths, No. | 10 845 | 2738 | 362 | 12 | 63 | 1429 |
| HR (95% CI)a | 1 [Reference] | 1.14 (1.05-1.23) | 1.80 (1.39-2.35) | 2.28 (0.82-6.37) | 1.42 (1.11-1.83) | 1.05 (0.98-1.13) |
| External causes of death | ||||||
| Deaths, No. | 6565 | 1230 | 217 | 12 | 45 | 403 |
| HR (95% CI)a | 1 [Reference] | 1.19 (1.05-1.34) | 1.63 (1.28-2.06) | 2.09 (1.18-3.71) | 1.56 (1.16-2.11) | 1.12 (1.00-1.25) |
| Excluding first 5 y of follow-up | ||||||
| Cerebrovascular disease | ||||||
| Deaths, No. | 9905 | 2328 | 277 | 15 | 83 | 1374 |
| HR (95% CI)a | 1 [Reference] | 1.10 (1.01-1.21) | 1.47 (1.11-1.95) | 1.16 (0.70-1.94) | 1.47 (1.18-1.83) | 1.07 (0.99-1.16) |
| Coronary heart disease | ||||||
| Deaths, No. | 5491 | 1255 | 154 | 13 | 40 | 697 |
| HR (95% CI)a | 1 [Reference] | 1.16 (1.05-1.28) | 1.76 (1.29-2.40) | 2.35 (1.35-4.10) | 1.35 (0.78-2.32) | 1.09 (0.99-1.22) |
| Circulatory system diseases | ||||||
| Deaths, No. | 25 414 | 6342 | 788 | 41 | 165 | 3529 |
| HR (95% CI)a | 1 [Reference] | 1.15 (1.05-1.26) | 1.67 (1.35-2.06) | 1.41 (1.03-1.95) | 1.42 (1.03-1.96) | 1.09 (1.03-1.15) |
| Cancer | ||||||
| Deaths, No. | 28 822 | 5449 | 707 | 44 | 159 | 2522 |
| HR (95% CI)a | 1 [Reference] | 1.05 (0.99-1.12) | 1.27 (1.12-1.43) | 1.27 (0.95-1.72) | 1.04 (0.87-1.24) | 1.04 (1.00-1.09) |
| Respiratory diseases | ||||||
| Deaths, No. | 9664 | 2415 | 319 | 11 | 55 | 1240 |
| HR (95% CI)a | 1 [Reference] | 1.15 (1.05-1.25) | 1.72 (1.31-2.26) | 2.39 (1.12-5.14) | 1.47 (1.12-1.93) | 1.08 (0.99-1.18) |
| External causes of death | ||||||
| Deaths, No. | 5631 | 1006 | 177 | 10 | 35 | 292 |
| HR (95% CI)a | 1 [Reference] | 1.16 (1.03-1.29) | 1.52 (1.25-1.86) | 2.76 (1.47-5.18) | 1.75 (1.15-2.67) | 1.08 (0.95-1.24) |
Abbreviation: HR, hazard ratio.
Multivariable Cox regression model was adjusted for sex, age at baseline (year, continuous), smoking status (never, former, current, and missing), education (no formal education or primary education, secondary education, trade or technical education, university education or above, and missing), physical activity (none or almost none, low, intermediate, high, and missing), alcohol intake (nondrinker, drinker, and missing), and baseline health conditions (cerebrovascular disease, coronary heart disease, cancer, hypertension, and diabetes).
Subgroup Analyses
We further evaluated the association between marital status and mortality risk stratified by health status at baseline (Table 3). In subgroup analyses defined by variables (e.g. disease status at baseline), there were positive associations between unmarried and total mortality in each subgroup (Table 3). An insignificant P value for interaction indicated that there was no difference between 3 groups: (1) cancer, coronary heart disease, or cerebrovascular disease; (2) diabetes or hypertension only; and (3) healthy. We found that being single was associated with higher risk of mortality among healthy participants than among those with a history of cancer, cerebrovascular disease, or coronary heart disease (P for interaction = .01). The association for the separated was also modified by health status (P for interaction = .01). In subgroup analyses, we found that the associations between being unmarried, widowed, or divorced and risk of death from all causes were modified by sex (Table 3). Positive associations were found among unmarried (P for interaction = .003), widowed (P for interaction =. 049), and divorced (P for interaction = .047) men, but no association was found among women. The associations between marital status (unmarried or single) and risk of total mortality were modified by age (P for interaction < .001) (Table 3). The HRs were higher among single participants younger than 65 years (HR, 1.79; 95% CI, 1.54-2.08) than those who were aged 65 years and older (HR, 1.11; 95% CI, 1.02-1.22) (P for interaction < .001). Subgroup analyses according to birth year and country are presented in eTable 4 in the Supplement.
Table 3. All-Cause Mortality Associated With Marital Status Stratified by Individual Characteristics in Asian Populations.
| Variable | Married | Not married | Single | Separated | Divorced | Widowed | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | P for interaction | HR (95% CI) | P for interaction | HR (95% CI) | P for interaction | HR (95% CI) | P for interaction | HR (95% CI) | P for interaction | ||
| Disease status at baselinea | |||||||||||
| Cancer, coronary heart disease, or cerebrovascular disease | 1 [Reference] | 1.10 (1.05-1.16) | .26 | 1.28 (1.10-1.49) | .01 | 1.91 (1.33-2.74) | .01 | 1.45 (0.98-2.16) | .42 | 1.10 (1.03-1.18) | .62 |
| Deaths, No. | 9132 | 2316 | 178 | 30 | 79 | 1440 | |||||
| Diabetes or hypertension only | 1 [Reference] | 1.10 (1.02-1.19) | 1.39 (1.18-1.63) | 2.03 (1.25-3.29) | 1.20 (1.02-1.42) | 1.10 (1.04-1.16) | |||||
| Deaths, No. | 30 123 | 7078 | 784 | 42 | 153 | 3667 | |||||
| Healthyb | 1 [Reference] | 1.19 (1.09-1.30) | 1.77 (1.51-2.08) | 1.18 (0.96-1.45) | 1.51 (1.19-1.93) | 1.09 (1.03-1.14) | |||||
| Deaths, No. | 60 994 | 13 621 | 2110 | 92 | 409 | 6544 | |||||
| Sexc | |||||||||||
| Male | 1 [Reference] | 1.23 (1.12-1.35) | .003 | 1.67 (1.43-1.94) | .11 | 1.62 (1.23-2.13) | .09 | 1.48 (1.28-1.75) | .047 | 1.13 (1.06-1.21) | .049 |
| Deaths, No. | 63 594 | 9405 | 1799 | 51 | 355 | 3313 | |||||
| Female | 1 [Reference] | 1.03 (0.97-1.10) | 1.39 (1.18-1.62) | 1.21 (1.00-1.46) | 1.22 (0.91-1.62) | 1.03 (0.97-1.10) | |||||
| Deaths, No. | 36 655 | 13 610 | 1273 | 113 | 286 | 8338 | |||||
| Age at baselined | |||||||||||
| <65 y | 1 [Reference] | 1.26 (1.14-1.38) | <.001 | 1.79 (1.54-2.08) | <.001 | 1.67 (1.25-2.22) | .05 | 1.53 (1.22-1.92) | .06 | 1.09 (1.03-1.15) | .19 |
| Deaths, No. | 68 812 | 12 182 | 2308 | 89 | 449 | 4235 | |||||
| ≥65 y | 1 [Reference] | 1.00 (0.94-1.07) | 1.11 (1.02-1.22) | 1.12 (0.89-1.40) | 1.06 (0.84-1.35) | 1.04 (0.99-1.09) | |||||
| Deaths, No. | 31 437 | 10 833 | 764 | 75 | 192 | 7416 | |||||
Abbreviation: HR, hazard ratio.
Multivariable Cox regression model was adjusted for sex, age at baseline (year, continuous), smoking status (never, former, current, and missing), education (no formal education or primary education, secondary education, trade or technical education, university education or above, and missing), physical activity (none or almost none, low, intermediate, high, and missing), and alcohol intake (nondrinker, drinker, and missing).
Refers to participants who had no history of cancer, cerebrovascular disease, coronary heart disease, diabetes, or hypertension.
Multivariable Cox regression model was adjusted for age at baseline (year, continuous), smoking status (never, former, current, and missing), education (no formal education or primary education, secondary education, trade or technical education, university education or above, and missing), physical activity (none or almost none, low, intermediate, high, and missing), alcohol intake (nondrinker, drinker, and missing), and baseline health conditions (cerebrovascular disease, coronary heart disease, cancer, hypertension, and diabetes).
Multivariable Cox regression model was adjusted for sex, smoking status (never, former, current, and missing), education (no formal education or primary education, secondary education, trade or technical education, university education or above, and missing), physical activity (none or almost none, low, intermediate, high, and missing), alcohol intake (nondrinker, drinker, and missing), and baseline health conditions (cerebrovascular disease, coronary heart disease, cancer, hypertension, and diabetes).
Discussion
In this cohort study using pooled data for 623 140 Asian individuals from 16 prospective cohorts, we demonstrated that unmarried individuals had a 15% increased risk of total mortality, after adjusting for potential confounders. Compared with married participants, those who were single, separated, widowed, and divorced had a greater risk of death from all causes. The results were similar after excluding deaths occurring within the first 5 years, which confirmed the robustness of our findings. This pooled analysis further showed that being unmarried was associated with a greater risk of death from 6 specific causes. The large sample size of the ACC allowed us to examine whether the association between marital status and mortality risks differed across subgroups of sex, age, and health condition at baseline.
Our results confirmed the findings in a recent meta-analysis,3 which reported pooled risk ratios (RRs) of 1.33 (95% CI, 1.24-1.43) for death from all causes, 1.37 (95% CI, 1.21-1.55) for cancer, and 1.11 (95% CI, 1.07-1.15) for circulatory system diseases for unmarried vs married individuals. The evidence for respiratory disease mortality has been sparse, however. In accordance with our findings, data from the Japan Collaborative Cohort Study16 and the National Cohort Study in Denmark25 showed a greater risk of death from respiratory diseases among those who were unmarried compared with married individuals.
Although the association between unmarried subcategories with mortality has been extensively investigated, the results are inconclusive.2,3,4 An early meta-analysis2 found that the positive association was greater among divorced or separated individuals (RR, 1.16; 95% CI, 1.09-1.23) than among widowed individuals (RR, 1.11; 95% CI, 1.08-1.14) or those who were never married (RR, 1.11; 95% CI, 1.07-1.15); however, only 5 of the 53 included studies were from Asian populations, and they were limited by small samples. More studies have been conducted since but with conflicting results (HR for single individuals, 1.54; 95% CI, 1.46-1.63; HR for divorced or separated individuals, 1.43; 95% CI, 1.34-1.52; HR for widowed individuals, 1.23; 95% CI, 1.19-1.26).3 In our study of 623 140 Asian individuals with a mean follow-up of 15.5 years, we found that, among all unmarried subcategories, being single was most associated with death from all causes. These findings could be explained by self-selection of single individuals with less favorable socioeconomic and psychosocial status to enter into marriage33 and by the disparity in social support across subgroups of unmarried individuals. The duration of living with a spouse may also play an important role in mortality risks, because individuals who were divorced, separated, or widowed had been cohabitating with a spouse for a time during marriage. Similar findings were seen for deaths from other major causes, except for coronary heart disease mortality and external causes of death, for which separation was associated with greater risks than other unmarried status. The observed associations may be a consequence of the reduction in the ability to cope with stress accrued from separation.4
Prior literature reported decreased survival for unmarried patients with known cardiovascular disease4,24 and cancer.34 Although marital status has been associated with the incidence of hypertension35 and type 2 diabetes,36 none of the previous studies has explored mortality outcomes by marital status after the onset of hypertension or diabetes, rendering interpretation of long-term outcomes difficult. To our knowledge, the current study is the first to examine the association between marital status and mortality risks among participants with various health statuses within the same cohort. Our results suggest that there is a survival advantage not only for married individuals with life-threatening diseases (cancer, coronary heart disease, and cerebrovascular disease) but also for those with diabetes or hypertension. The protective outcomes of marriage among people with chronic diseases may be associated with the encouragement from partners to seek medical help and adhere to treatment.37,38 Given the wealth of evidence indicating the positive association between marital status and mortality, the importance of adequate support to unmarried individuals with chronic diseases cannot be neglected.
The current analysis found a significant interaction between age and all-cause mortality among unmarried groups, especially for the single and the separated. Sorlie et al26 reported that unmarried participants younger than 65 years experienced a higher risk of mortality than those who were older. The smaller association in elderly populations may be due to extramarital support from relatives or community, diminished health-promoting outcomes of marriage, and reduction of social support disparity between married and unmarried groups.2,37 The exact reasons still need to be explored. Some previous studies found that sex is a modifier of the association of marriage with death,27,28 whereas others failed to demonstrate the disparity.25,29 One meta-analysis3 summarizing 3 studies from Asia and 12 studies from America and Europe reported a women-to-men relative RR of 0.86 (95% CI, 0.79-0.94) for total mortality associated with being unmarried. In our study, we found that being unmarried was associated with higher mortality among men but not among women, reflecting the possibility that, in Asian marriages, gender inequality in the division of domestic labor and high expectations of childcare for women21 may counteract the health benefits of marriage among women. Another possible explanation is that, compared with married women, a higher employment rate among unmarried women may have contributed to financial security and favorable health outcomes.16,39 Furthermore, unmarried men may receive less social support and financial protection from the government than unmarried women in Asia.16,39
Strengths and Limitations
The strength of our pooled analyses includes the prospective design of each study, which minimized potential recall bias and selection bias. In addition, to our knowledge, the present study is the largest pooled analysis of Asian populations from 16 cohorts, which allowed us to provide estimates with sufficient precision and to examine reverse causation.
However, our study has limitations that merit further discussion. First, given the observational nature of the study and the lack of data on income, residual confounding could exist. Second, we excluded participants with missing information on marriage and vital status, and this may lead to selection bias if participants with complete information are not representative of the cohort population. Also, individuals with higher socioeconomic status may be more likely to participate in the study and less likely to be lost to follow-up. Third, information regarding cohabitation and changes in marital status was not captured in our data set, and misclassification is possible. However, later life marital dissolution may be more dominant than remarriage, which could diminish the observed associations. In addition, the rate of nonmarital cohabitation is likely to be small in the included countries of the present analysis.21 Such participants would be grouped as unmarried in the analyses and were expected to show better survival outcomes, which, in turn, biased the association toward the null. Fourth, the likelihood of alterations in marital status before the baseline survey may be influenced by initial symptoms of undiagnosed diseases. To minimize bias from reverse causation, we performed analysis excluding deaths within the first 5 years of follow-up. Similar results were observed, suggesting these biases could be minimal in our findings. Fifth, covariates were assessed at baseline; therefore, the changes in these variables over time were not considered. Although we have included 16 population-based cohorts in Asia, we acknowledge that the heterogeneity within the region may not be fully represented by this study. Sixth, the mean age of 53.7 years at baseline was young with regard to the outcome of mortality, despite the long follow-up of 15.5 years.
Conclusions
In this large-scale cohort study pooling data from multiple cohorts, being unmarried was associated with a higher risk of total and cause-specific mortality. The association persisted across baseline health conditions and was particularly evident in men and participants who were younger than 65 years at baseline. Our findings underscore the potential to reduce unfavorable mortality outcomes among unmarried individuals in Asia.
eAppendix. Supplemental Methods
eTable 1. Descriptions and Basic Characteristics of Participating Cohorts
eTable 2. Baseline Characteristics for 623,140 Participants According to Marital Status
eTable 3. Association of Marital Status With Risk of All-Cause Mortality in Asian Populations
eTable 4. All-Cause Mortality Associated With Marital Status by Birth Years and Countries in Asian Populations
References
- 1.Ortiz-Ospina E, Roser M. Marriages and divorces. Our World in Data. 2020. Accessed November 16, 2021. https://ourworldindata.org/marriages-and-divorces
- 2.Manzoli L, Villari P, M Pirone G, Boccia A. Marital status and mortality in the elderly: a systematic review and meta-analysis. Soc Sci Med. 2007;64(1):77-94. doi: 10.1016/j.socscimed.2006.08.031 [DOI] [PubMed] [Google Scholar]
- 3.Wang Y, Jiao Y, Nie J, et al. Sex differences in the association between marital status and the risk of cardiovascular, cancer, and all-cause mortality: a systematic review and meta-analysis of 7,881,040 individuals. Glob Health Res Policy. 2020;5(1):4. doi: 10.1186/s41256-020-00133-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wong CW, Kwok CS, Narain A, et al. Marital status and risk of cardiovascular diseases: a systematic review and meta-analysis. Heart. 2018;104(23):1937-1948. doi: 10.1136/heartjnl-2018-313005 [DOI] [PubMed] [Google Scholar]
- 5.Verbrugge LM. Marital status and health. J Marriage Fam. 1979;41(2):267-285. doi: 10.2307/351696 [DOI] [Google Scholar]
- 6.Waldron I, Hughes ME, Brooks TL. Marriage protection and marriage selection: prospective evidence for reciprocal effects of marital status and health. Soc Sci Med. 1996;43(1):113-123. doi: 10.1016/0277-9536(95)00347-9 [DOI] [PubMed] [Google Scholar]
- 7.Umberson D. Family status and health behaviors: social control as a dimension of social integration. J Health Soc Behav. 1987;28(3):306-319. doi: 10.2307/2136848 [DOI] [PubMed] [Google Scholar]
- 8.Umberson D. Gender, marital status and the social control of health behavior. Soc Sci Med. 1992;34(8):907-917. doi: 10.1016/0277-9536(92)90259-S [DOI] [PubMed] [Google Scholar]
- 9.Miller-Tutzauer C, Leonard KE, Windle M. Marriage and alcohol use: a longitudinal study of “maturing out”. J Stud Alcohol. 1991;52(5):434-440. doi: 10.15288/jsa.1991.52.434 [DOI] [PubMed] [Google Scholar]
- 10.Chin B, Murphy MLM, Janicki-Deverts D, Cohen S. Marital status as a predictor of diurnal salivary cortisol levels and slopes in a community sample of healthy adults. Psychoneuroendocrinology. 2017;78:68-75. doi: 10.1016/j.psyneuen.2017.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matthews K, Schwartz J, Cohen S, Seeman T. Diurnal cortisol decline is related to coronary calcification: CARDIA study. Psychosom Med. 2006;68(5):657-661. doi: 10.1097/01.psy.0000244071.42939.0e [DOI] [PubMed] [Google Scholar]
- 12.Joseph JJ, Wang X, Spanakis E, et al. Diurnal salivary cortisol, glycemia and insulin resistance: the multi-ethnic study of atherosclerosis. Psychoneuroendocrinology. 2015;62:327-335. doi: 10.1016/j.psyneuen.2015.08.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anagnostis P, Athyros VG, Tziomalos K, Karagiannis A, Mikhailidis DP. The pathogenetic role of cortisol in the metabolic syndrome: a hypothesis. J Clin Endocrinol Metab. 2009;94(8):2692-2701. doi: 10.1210/jc.2009-0370 [DOI] [PubMed] [Google Scholar]
- 14.Sephton SE, Sapolsky RM, Kraemer HC, Spiegel D. Diurnal cortisol rhythm as a predictor of breast cancer survival. J Natl Cancer Inst. 2000;92(12):994-1000. doi: 10.1093/jnci/92.12.994 [DOI] [PubMed] [Google Scholar]
- 15.Sephton SE, Lush E, Dedert EA, et al. Diurnal cortisol rhythm as a predictor of lung cancer survival. Brain Behav Immun. 2013;30(suppl):S163-S170. doi: 10.1016/j.bbi.2012.07.019 [DOI] [PubMed] [Google Scholar]
- 16.Ikeda A, Iso H, Toyoshima H, et al. ; JACC Study Group . Marital status and mortality among Japanese men and women: the Japan Collaborative Cohort Study. BMC Public Health. 2007;7:73. doi: 10.1186/1471-2458-7-73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Va P, Yang WS, Nechuta S, et al. Marital status and mortality among middle age and elderly men and women in urban Shanghai. PLoS One. 2011;6(11):e26600. doi: 10.1371/journal.pone.0026600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nagata C, Takatsuka N, Shimizu H. The impact of changes in marital status on the mortality of elderly Japanese. Ann Epidemiol. 2003;13(4):218-222. doi: 10.1016/S1047-2797(02)00409-X [DOI] [PubMed] [Google Scholar]
- 19.Iwasaki M, Otani T, Sunaga R, et al. Social networks and mortality based on the Komo-Ise cohort study in Japan. Int J Epidemiol. 2002;31(6):1208-1218. doi: 10.1093/ije/31.6.1208 [DOI] [PubMed] [Google Scholar]
- 20.Hurt LS, Ronsmans C, Saha S. Effects of education and other socioeconomic factors on middle age mortality in rural Bangladesh. J Epidemiol Community Health. 2004;58(4):315-320. doi: 10.1136/jech.2003.007351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Raymo JM, Park H, Xie Y, Yeung WJ. Marriage and family in East Asia: continuity and change. Annu Rev Sociol. 2015;41:471-492. doi: 10.1146/annurev-soc-073014-112428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shor E, Roelfs DJ, Yogev T. The strength of family ties: a meta-analysis and meta-regression of self-reported social support and mortality. Soc Networks. 2013;35(4):626-638. doi: 10.1016/j.socnet.2013.08.004 [DOI] [Google Scholar]
- 23.Roelfs DJ, Shor E, Kalish R, Yogev T. The rising relative risk of mortality for singles: meta-analysis and meta-regression. Am J Epidemiol. 2011;174(4):379-389. doi: 10.1093/aje/kwr111 [DOI] [PubMed] [Google Scholar]
- 24.Floud S, Balkwill A, Canoy D, et al. ; Million Women Study Collaborators . Marital status and ischemic heart disease incidence and mortality in women: a large prospective study. BMC Med. 2014;12(1):42. doi: 10.1186/1741-7015-12-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Frisch M, Simonsen J. Marriage, cohabitation and mortality in Denmark: national cohort study of 6.5 million persons followed for up to three decades (1982-2011). Int J Epidemiol. 2013;42(2):559-578. doi: 10.1093/ije/dyt024 [DOI] [PubMed] [Google Scholar]
- 26.Sorlie PD, Backlund E, Keller JB. US mortality by economic, demographic, and social characteristics: the National Longitudinal Mortality Study. Am J Public Health. 1995;85(7):949-956. doi: 10.2105/AJPH.85.7.949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Breeze E, Sloggett A, Fletcher A. Socioeconomic and demographic predictors of mortality and institutional residence among middle aged and older people: results from the Longitudinal Study. J Epidemiol Community Health. 1999;53(12):765-774. doi: 10.1136/jech.53.12.765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Molloy GJ, Stamatakis E, Randall G, Hamer M. Marital status, gender and cardiovascular mortality: behavioural, psychological distress and metabolic explanations. Soc Sci Med. 2009;69(2):223-228. doi: 10.1016/j.socscimed.2009.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Johnson NJ, Backlund E, Sorlie PD, Loveless CA. Marital status and mortality: the National Longitudinal Mortality Study. Ann Epidemiol. 2000;10(4):224-238. doi: 10.1016/S1047-2797(99)00052-6 [DOI] [PubMed] [Google Scholar]
- 30.GBD 2015 Risk Factors Collaborators . Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1659-1724. doi: 10.1016/S0140-6736(16)31679-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zheng W, McLerran DF, Rolland BA, et al. Burden of total and cause-specific mortality related to tobacco smoking among adults aged ≥45 years in Asia: a pooled analysis of 21 cohorts. PLoS Med. 2014;11(4):e1001631. doi: 10.1371/journal.pmed.1001631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Burke DL, Ensor J, Riley RD. Meta-analysis using individual participant data: one-stage and two-stage approaches, and why they may differ. Stat Med. 2017;36(5):855-875. doi: 10.1002/sim.7141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goldman N. Marriage selection and mortality patterns: inferences and fallacies. Demography. 1993;30(2):189-208. doi: 10.2307/2061837 [DOI] [PubMed] [Google Scholar]
- 34.Aizer AA, Chen MH, McCarthy EP, et al. Marital status and survival in patients with cancer. J Clin Oncol. 2013;31(31):3869-3876. doi: 10.1200/JCO.2013.49.6489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lipowicz A, Lopuszanska M. Marital differences in blood pressure and the risk of hypertension among Polish men. Eur J Epidemiol. 2005;20(5):421-427. doi: 10.1007/s10654-005-1752-x [DOI] [PubMed] [Google Scholar]
- 36.Ramezankhani A, Azizi F, Hadaegh F. Associations of marital status with diabetes, hypertension, cardiovascular disease and all-cause mortality: a long term follow-up study. PLoS One. 2019;14(4):e0215593. doi: 10.1371/journal.pone.0215593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rendall MS, Weden MM, Favreault MM, Waldron H. The protective effect of marriage for survival: a review and update. Demography. 2011;48(2):481-506. doi: 10.1007/s13524-011-0032-5 [DOI] [PubMed] [Google Scholar]
- 38.Ikeda A, Iso H, Kawachi I, Yamagishi K, Inoue M, Tsugane S; JPHC Study Group . Living arrangement and coronary heart disease: the JPHC study. Heart. 2009;95(7):577-583. doi: 10.1136/hrt.2008.149575 [DOI] [PubMed] [Google Scholar]
- 39.Martire LM, Helgeson VS. Close relationships and the management of chronic illness: associations and interventions. Am Psychol. 2017;72(6):601-612. doi: 10.1037/amp0000066 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Supplemental Methods
eTable 1. Descriptions and Basic Characteristics of Participating Cohorts
eTable 2. Baseline Characteristics for 623,140 Participants According to Marital Status
eTable 3. Association of Marital Status With Risk of All-Cause Mortality in Asian Populations
eTable 4. All-Cause Mortality Associated With Marital Status by Birth Years and Countries in Asian Populations