Abstract
Depression involves a heterogenous collection of symptoms. Network perspective views depressive symptoms as an interrelated network. The current study aimed to replicate network analyses on adolescent depression in three samples assessed with three instruments to examine the consistency of network structures and also examine the variance of networks between genders. Three samples of adolescents (total N = 4375, mean age = 15, 49.1% boys) were assessed with PHQ-9, SMFQ and CDI, respectively. Network analyses were carried out on depression symptoms. Network stability, node centrality and network comparisons between genders were examined. Three networks were reliably stable. Sadness and self-hatred were unanimously identified to be central symptoms of adolescent depression in three networks. In addition, fatigue, no good, everything wrong and loneliness also appeared to be central in specific networks. Among three depression networks, PHQ-9 network demonstrated gender difference in network structure. The current study is exploratory in nature. The differences in three networks can be due to various samples or different node inclusions. Further, the study is cross-sectional precluding causal interpretation and the samples are nonclinical. Besides “hallmark” symptom sadness, self-hatred was also identified unanimously in three networks, which demonstrated the significant role self-worth played in adolescent depression. The results also suggested that differences in node inclusion may have influence on the network structure.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12144-022-03201-z.
Keywords: Depression, Network analysis, Adolescent, Depression scales
Introduction
Depression is one of the most prevalent mental health problems occurred among adolescents in China as well as worldwide (Avenevoli et al., 2015; Tang et al., 2019). As a challenging developmental phase with physical and psychological changes and school transition, adolescence is marked with drastic increase in depression incidence (Benner, 2011; Costello et al., 2011). Epidemiological studies done in mainland China suggested that among children and adolescents aged 5–19, approximately 1.3% have experienced major depressive disorder (MDD; Xu et al., 2018) and the prevalence of depressive symptoms was 24.3% among adolescents attending secondary schools (Tang et al., 2019). Adolescent depression is demonstrated to be associated with a myriad of disrupting psychosocial consequences that can expand across the lifespan, including compromised educational attainment and employment opportunities, impaired intimate relationships and social networks (Clayborne et al., 2019).
Since depression is pervasive and debilitating, it’s been extensively researched. In regard to assessment, more than 280 various depression instruments have been developed and published over the past century to measure depression severity (Santor et al., 2006). These scales were developed with different theoretical conceptualizations in mind and to serve different purposes so their content also varied vastly (Fried, 2017). For example, Patient Health Questionnaire (PHQ-9) was developed for criteria-based diagnoses of depression, and thus includes nine items directly corresponding to the nine DSM-5 criteria symptoms for MDD (Kroenke et al., 2001). Beck Depression Inventory (BDI) was developed based on Beck’s conceptualization of depression and accordingly characterizes several cognitive symptoms central to Beck’s theory (Beck, 2002). Fried (2017) compared seven frequently used depression scales (encompassing a total of 125 items) and found that the content overlap among the scales was low.
Depression studies routinely employed particular scales and used total scores of all items to measure depression severity, without specifically demonstrating the rationale for scale selection. This practice was suggestive of the traditional entity perspective on psychopathology, which emphasizes on the underlying depression entity, and views depressive symptoms only as equivalent and interchangeable indicators of the depression entity (Brown & Barlow, 2005; Schmittmann et al., 2013). Inspired by this perspective, various studies revolving depression used the sum scores of certain depression instruments as the assessment of depression severity in a general sense, without delving into the symptom-level differences or explaining the rationale for scale selection (Fried, 2017; Fried & Nesse, 2015).
In fact, individual depressive symptoms varies in important properties such as risk factors (Lux & Kendler, 2010), predictive value (McKenzie et al., 2011) and impairment of functioning (Fried & Nesse, 2014; Tweed, 1993). Furthermore, both clinical theory (Beck, 2002) and empirical research (e.g., Bringmann et al., 2015) provided substantial evidence that depressive symptoms influence each other. For example, in Beck’s descriptive model of depression, negative beliefs about the self, the world and the future serves to exacerbate negative mood and in turn maintain depression (Beck, 2002). Studies conducted in the U.S. healthy adult samples demonstrated that hopelessness predicts suicidal ideation over time (Kuo et al., 2004). This suggested that various symptoms of depression are not equivalent and interchangeable and it may be beneficial to study depression at the symptom level (Fried & Nesse, 2015). Also, it may be advantageous to be more aware of the symptoms included in the instruments in use.
The recently proposed network perspective of psychopathology views disorders as constituted by the causal interplay between specific symptoms (Wasil et al., 2020). The network perspective focuses on symptom-level associations that form a complex system described as depression (Beard et al., 2016). Developed under this perspective, network analysis helps to visualize the interrelated system of depression. In depression networks, symptoms are represented as “nodes” and relationships between them are represented as “edges”. Central nodes which share stronger relationships with other nodes are integral to the network structure and play a crucial role in the development and maintenance of mental disorders (Barrat et al., 2007).
Burgeoning studies have been conducted using network analysis to understand symptom-level structure of psychopathology. Previous research of depression networks primarily revolved around depression in clinical samples of adults. Among adult samples diagnosed with MDD and other psychiatric conditions, sad mood, low energy, and anhedonia were identified to be highly central symptoms of depression networks measured with PHQ-9, BDI-II and QIDS-SR, respectively (Beard et al., 2016; Bos et al., 2018; McNally et al., 2017). Several studies have also explored the network structure of depressive symptoms in adolescent samples. In a study conducted in an American community sample of adolescents, sadness, pessimism, self-hatred and loneliness were identified as the central symptoms of depression measured with CDI (Mullarkey et al., 2019). Feeling like a failure and depressed mood were indicated to be the most central depressive symptoms in the depression network assessed with PHQ-9 among non-clinical adolescents from Sub-Sahara Africa and India (Osborn et al., 2020; Wasil et al., 2020). In summary, among nonclinical adolescents, in addition to sad mood, feeling like a failure (or self-hatred and self-blame) was also central in the depression network, which is consistent with the cognitive features associated with developmental period of adolescence (Carlson, 2000). Above-mentioned studies all used single instruments to investigate interrelations between depressive symptoms without specifying the rationale for scale selection. Though network approach performs on symptom-level and is supposed to be less susceptible to the bias resulted from using various measures, the inclusion of different symptoms in the network still has substantial impact on the network structure (Fried & Cramer, 2017; Jones et al., 2017). Network structure is determined based on the partial correlations between nodes included in the network. Thus, the inclusion of redundant nodes and even more so the exclusion of relevant variables that are strongly associated with other nodes pose serious challenge to network accuracy and interpretation (Fried & Cramer, 2017). Since depression involves heterogenous symptoms as well as numerous related cognitive and behavioral factors, it’s impractical to create a depression network with all-inclusive variables. Therefore, the current study chose to select three widely-used depression measures to replicate the network estimation and examine if important network properties (e.g., node centrality) hold across three networks.
The present study sought to expand on the existing literature by pursuing three primary goals. Firstly, this study intended to estimate the depression network in a sample of Chinese adolescents. It has long been recognized that mental disorders are expressed, perceived and described quite differently across different age groups (Nardi et al., 2013) and among diverse cultures (Wilk & Bolton, 2002). For instance, as a turbulent period of life, adolescence appears to be associated with specific features of depression such as low self-esteem (Carlson, 2000). In addition, Chinese individuals tend to report more somatic symptoms of depression than their western counterparts (Ryder et al., 2008). Also, depression was more closely associated with peer problems among western adolescents and more strongly linked with academic difficulties in Chinese adolescents (Ryder et al., 2012). Therefore, applying network analyses to different age groups in different cultures has the potential to deepen our understanding of the patterns of depression networks. Secondly, the current study aimed to replicate the network analyses with three different depression instruments in three samples. Symptoms with high centrality would be identified in each network. Since node inclusion has significant influence on the network model, the current study would estimate depression networks using different scales and samples to examine if centrality of nodes remains relatively invariable across three networks. Thirdly, the present study proposed to investigate the differences of depression networks between genders. Gender differences in depression severity becomes evident since adolescence (e.g., Hankin & Abramson, 2001). Epidemiological studies conducted in the U.S. reported that MDD is nearly twice as prevalent in girls than in boys (Merikangas et al., 2010). Previous network analyses found differences in both network structure (Mullarkey et al., 2019) and network connectivity (Kim et al., 2021) between genders in samples of children and adolescents. The present study aimed to replicate network comparisons between genders in three Chinese adolescent samples with three depression instruments.
Methods
Participants and Procedures
Data from three samples of Chinese adolescents were utilized in the current study. Sample 1 (N = 1610, age = 16.03 ± 1.72, 46.5% girls and 53.4% boys) was a convenience sample of adolescents from three public secondary schools in Henan, Sichuan and Shaanxi Provinces in China. Sample 2 (N = 2194, age = 14.33 ± 3.60, 47.0% girls, 47.5% boys and 5.5% not reported) was recruited in three secondary schools in Beijing. Sample 3 (N = 571, 14.70 ± 1.72, 56.7% girls and 43.3% boys) consisted of adolescents from two secondary schools in Shanxi Province. The data collection of the three samples were carried out before the COVID-19 pandemic. Demographic information is provided in Table 1.
Table 1.
Participant demographic information (N = 4375)
| Grades | Parents’ marital status | Place of residence | ||||
|---|---|---|---|---|---|---|
| Middle school | High school | Married | Othera | Village | City | |
| Sample 1 | 605 | 1005 | 1468 | 142 | 1059 | 551 |
| Sample 2 | 1062 | 1132 | 1950 | 244 | 77 | 2117 |
| Sample 3 | 284 | 287 | 510 | 61 | 283 | 288 |
| Total | 1951 | 2424 | 3928 | 447 | 1419 | 2956 |
a The Other category includes separated, divorced and widowed status
The present study was approved by the local Ethics Committee and the process of data collection was conducted with the permission of the principals of the participating schools. Questionnaires were handed out on school days in classes and completed in paper–pencil format. After explaining the purpose and the nature of the study, informed consent was obtained from classroom teachers and participants. The present researchers provided clarification and ensured independent response from participants.
Measures
Depressive symptoms were assessed with three scales in three samples. Sample 1 was measured with PHQ-9, Sample 2 with SMFQ and Sample 3 with CDI.
Patient Health Questionnaire (PHQ-9; Kroenke et al., 2001) is a self-report measure designed for criteria-based diagnoses of depression in primary care. It consists of 9 items that are rated on a 4-point scale (0 = not at all to 3 = nearly every day). The original and Chinese version of PHQ-9 have been shown to be well-validated in previous research (Kroenke et al., 2001; Yu et al., 2012). In our present study, Cronbach’s alpha was 0.84.
Short Mood and Feelings Questionnaire (SMFQ; Angold et al., 1995) was developed for the purpose of rapid evaluation of depressive symptoms in youths aged 8–16 years old. The scale mainly revolves around affective and cognitive symptoms. It comprises 13 items, each rated on a 3-point scale (0 = never, 1 = sometimes, 2 = always). The Chinese version of SMFQ demonstrated good internal consistency and test–retest reliability (Cheng et al., 2009). In the present study, Cronbach’s alpha was 0.88.
Children’s Depression Inventory, (CDI; Kovacs, 1992) was adapted from Beck’s Depression Inventory to assess depression in children and adolescents aged 7–17. It includes 27 items measuring cognitive, affective and behavioral symptoms, respectively. The participants were asked to select one out of three statements for each item (0 = absence of symptoms, 1 = mild presence of symptoms, 2 = definite presence of symptoms). The Chinese version of the CDI has evidenced good internal consistency (Wu et al., 2010). In the current study, Cronbach’s alpha was 0.83.
Data Analysis Plan
Descriptive analyses of variables were performed in SPSS version 26 and R version 4.0.2. Missing data accounted for 0.36% of the data, with 213 missing values out of 58,429 possible values. The Full Information Maximum Likelihood (FIML) estimation via the Expectation Maximization (EM) algorithm was used to impute the missing values (Dempster et al., 1977; Wang & Deng, 2016).
Item Selection
It’s suggested that if redundant nodes were included in the network at the same time, it will obscure the real relationships between nodes (Levinson et al., 2018). To address that concern, the goldbricker function in the R package networktools (Jones, 2020) was used to detect each pair of nodes for high correlation between them and compare their correlation pattern with the remaining nodes. The results indicated that there were no redundant nodes in three node collections and thus all items were included in the corresponding networks.
Network Estimation
Network analysis and visualization were conducted in R using the bootnet and qgraph packages (Epskamp et al., 2012, 2017). The networks were estimated using a Gaussian Graphical Model (GGM; Costantini et al., 2015) regularized by glasso algorithm, creating a sparse graph containing significant partial correlations between nodes (Epskamp & Fried, 2018; Simon et al., 2011). Spearman correlation was used to account for the ordinal data and the dense networks. Glasso algorithm was implemented in combination with Extended Bayesian Information Criterion (EBIC) to select the optimal degree of shrinkage (Chen & Chen, 2008). The default hyperparameter value (γ = 0.5)1 was used in the networks (Epskamp & Fried, 2018).
Network Stability
The stability of the network was examined with the bootnet package using both nonparametric bootstrapping and case-dropping bootstrapping (Epskamp et al., 2017). The nonparametric bootstrapping repeatedly resamples subsets of the data to construct bootstrapped confidence intervals (CI) around edge estimates. Wider CIs indicates lower accuracy of the edge values. To test the stability of centrality indices, case-dropping bootstrapping was employed to calculate a correlation-stability (CS) coefficient.
Centrality and Difference Test
In addition to visual inspection, the centrality indices were computed in the qgraph package to infer the structural importance of nodes in the network (Opsahl et al., 2010). There’re three centrality indices that have been used in previous research employing network analysis (e.g., Olatunji et al., 2018). The current study didn’t examine betweenness and closeness indices as they demonstrated poor replicability (Epskamp et al., 2017) and appeared to be not suitable in psychopathology networks (Bringmann et al., 2019). Hence, the analyses and interpretations of centrality would focus on strength index. Strength refers to the sum of the absolute edge values between a given node and all other nodes to which the node is connected (McNally, 2016).
The node centrality difference tests were also employed to determine which nodes were significantly more central than other nodes (Levinson et al., 2018).
Network Comparison Tests by Genders
We also tested whether three depression networks varied with genders. First, t-tests were performed on the mean sum scores of depression measures between genders. Then the network comparison tests (NCT) were conducted with the R package NetworkComparisonTest (van Borkulo et al., 2017) to determine whether significant gender differences existed in global strength and network structure. Global strength referred to the overall network connectivity and can be calculated as the weighted absolute sum of all edges. The calculation of differences in network structure involved absolute maximum differences among all edge strengths.
Results
Participant Characteristics and Descriptive Statistics
The complete sample included three datasets totaling 4375 adolescents, aged 11–18 years old (mean age = 15), with approximately even gender proportion (48.1% girls, 49.1% boys and 2.8% not reported).
The mean sum scores on the PHQ-9, SMFQ and CDI were 8.27, 6.28 and 16.69, respectively. According to the cut-off values of the three depression instruments (Kroenke et al., 2001; McKenzie et al., 2011; Bang et al., 2015), approximately 32.8% of Sample 1, 19.55% of Sample 2 and 31.9% of Sample 3 were above the clinical threshold of depression.
Descriptive information for each item in the three depression scales are provided in Table 2.
Table 2.
Items included in three networks
| Node | Mean | SD | Presence in % of participantsa | Skewness | Kurtosis |
|---|---|---|---|---|---|
| PHQ-9 (Sample 1) | |||||
| Anhedonia | 1.16 | 0.76 | 85.8% | 0.77 | 0.68 |
| Depressed | 0.94 | 0.73 | 74.7% | 0.75 | 0.91 |
| Sleep problems | 1.07 | 0.97 | 67.6% | 0.63 | -0.56 |
| Fatigue | 1.15 | 0.81 | 81.2% | 0.61 | 0.12 |
| Poor Appetite | 0.89 | 0.88 | 62.5% | 0.83 | 0.06 |
| Self-blame | 1.15 | 0.90 | 75.9% | 0.53 | -0.40 |
| Poor concentration | 0.96 | 0.94 | 62.8% | 0.74 | -0.34 |
| Motor problems | 0.57 | 0.80 | 41.2% | 1.40 | 1.34 |
| Suicidal ideation | 0.39 | 0.68 | 29.6% | 1.94 | 3.68 |
| SMFQ (Sample 2) | |||||
| Miserable | 0.91 | 0.64 | 74.4% | 0.09 | -0.58 |
| Not enjoy | 0.50 | 0.66 | 40.3% | 0.98 | -0.20 |
| Tired | 0.91 | 0.72 | 69.7% | 0.13 | -1.05 |
| Restless | 0.45 | 0.65 | 36% | 1.15 | 0.13 |
| No good | 0.36 | 0.61 | 29.3% | 1.52 | 1.14 |
| Cried a lot | 0.24 | 0.53 | 19.3% | 2.13 | 3.55 |
| Poor concentration | 0.61 | 0.67 | 50.1% | 0.66 | -0.66 |
| Self-hatred | 0.28 | 0.57 | 22.3% | 1.89 | 2.50 |
| Bad person | 0.22 | 0.51 | 17% | 2.34 | 4.54 |
| Loneliness | 0.62 | 0.74 | 46.1% | 0.75 | -0.81 |
| Unloved | 0.30 | 0.59 | 22.8% | 1.84 | 2.19 |
| Never as good | 0.52 | 0.69 | 40.5% | 0.97 | -0.31 |
| Everything wrong | 0.38 | 0.62 | 30.8% | 1.39 | 0.76 |
| CDI (Sample 3) | |||||
| Sadness | 0.32 | 0.58 | 25.7% | 1.67 | 1.7 |
| Pessimism | 0.99 | 0.28 | 95.8% | -0.25 | 10.06 |
| Self-deprecation | 1.22 | 0.45 | 98.8% | 0.90 | -0.07 |
| Anhedonia | 0.67 | 0.56 | 62.2% | 0.10 | -0.69 |
| Misbehavior | 0.26 | 0.55 | 20.5% | 2.03 | 3.07 |
| Worry | 0.48 | 0.70 | 35.9% | 1.13 | -0.09 |
| Self-hatred | 0.45 | 0.62 | 38.5% | 1.04 | 0.02 |
| Self-blame | 0.42 | 0.60 | 35.7% | 1.15 | 0.28 |
| Suicidal | 0.56 | 0.57 | 52.7% | 0.36 | -0.82 |
| Crying | 0.26 | 0.55 | 20.7% | 2.02 | 3.07 |
| Irritable | 0.56 | 0.71 | 43.6% | 0.86 | -0.56 |
| Withdrawal | 0.35 | 0.60 | 28.2% | 1.53 | 1.20 |
| Indecisiveness | 0.97 | 0.71 | 73.2% | 0.04 | -1.03 |
| Negative body image | 0.77 | 0.61 | 67.3% | 0.17 | –0.54 |
| School difficulty | 1.00 | 0.69 | 76.2% | 0.00 | -0.90 |
| Sleep problems | 0.49 | 0.73 | 34.9% | 1.14 | -0.19 |
| Fatigue | 0.64 | 0.74 | 48.5% | 0.68 | -0.88 |
| Poor appetite | 0.43 | 0.64 | 34.9% | 1.20 | 0.27 |
| Somatic concern | 0.44 | 0.62 | 36.8% | 1.11 | 0.17 |
| Loneliness | 0.64 | 0.72 | 49.6% | 0.66 | -0.83 |
| School dislike | 0.81 | 0.66 | 67.3% | 0.22 | -0.74 |
| Lack of friends | 0.68 | 0.53 | 64.4% | -0.11 | -0.76 |
| School performance | 0.90 | 0.74 | 67.6% | 0.16 | -1.14 |
| Low self-esteem | 1.04 | 0.46 | 91.4% | 0.16 | 1.64 |
| Unloved | 0.46 | 0.63 | 38.9% | 1.03 | -0.02 |
| Disobedience | 0.68 | 0.50 | 66.0% | -0.34 | -0.94 |
| Fights | 0.18 | 0.42 | 17.0% | 2.18 | 4.06 |
a Presence of symptoms was indicated if participants responded with “1” or greater on the item
Network Stability
The three depression networks all robust to stability tests. Centrality stability coefficients for strength were investigated for three networks. CS coefficients were excellent for Network 1(CS coefficient = 0.75) and Network 2(CS coefficient = 0.75) and acceptable for Network 3(CS coefficient = 0.36) based on the values suggested by Epskamp et al. (2017) (See Fig. S1-S3). Edges values were estimated to be with moderate confidence intervals (Fig. S4-S6). The strength indices of central nodes were estimated to be significantly higher than other nodes in a bootstrapped difference test which aids in demonstrating stability and accuracy in network interpretation (Fig. S7-S9; Epskamp et al., 2017).
Network Visualization and Interpretation
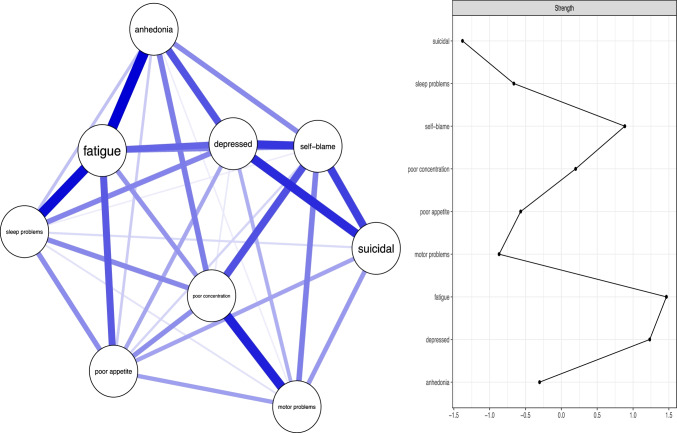
Network 1 (PHQ-9)
The resultant network with 9 nodes and the strength centrality plot of all nodes were presented in Fig. 1. Nodes that appeared central in the network were fatigue (Strength = 1.47), depressed (Strength = 1.23) and self-blame (Strength = 0.88), which, as stated above, appeared to be significantly more central than 62.5% of the other nodes. There have been suggestions that differential variability of symptom severity could distort the results about node centrality (Terluin et al., 2016). Following prior research (Heeren et al., 2018), the correlation between strength of nodes and variance of symptom severity ratings was calculated. In this network, the strength of the nodes was not significantly related to the variance (rs = 0.82, p = 0.835). Hence, the differential variability didn’t present a problem for interpreting the centrality indices in this network. Some pairwise associations that stood out were anhedonia—feeling fatigued, feeling fatigued—sleep problems, and depressed mood—suicidal ideation.
Fig. 1.
The left part shows the estimated network of depression (measured by PHQ-9) and the right panel shows the strength scores (centrality indices) of Network 1, shown as z scores
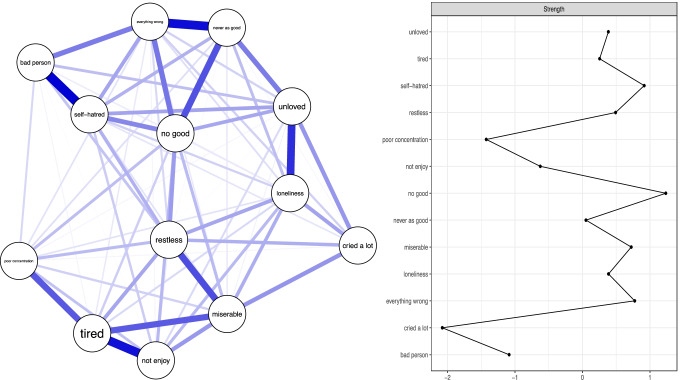
Network 2 (SMFQ)
The estimated depression network measured with SMFQ and the corresponding plot of strength index was shown in Fig. 2. No good (Strength = 1.23) stood out to be the most central symptom in the network, with its strength significantly higher than 75% of other symptoms. Self-hatred (Strength = 0.91), Everything wrong (Strength = 0.77) and Miserable (Strength = 0.72) appeared as relatively central in the network. The correlation between strength and variance of symptom severity was rs = 0.30 (p = 0.33), ruling out the influence of differential variability on centrality estimation. There existed strong associations between self-hatred—bad person, never as good—everything wrong, and not enjoy—tired symptom pairs.
Fig. 2.
The left part depicts the estimated network of depression (measured by SMFQ) and the right panel presents the strength scores (centrality indices) of Network 2, shown as z scores
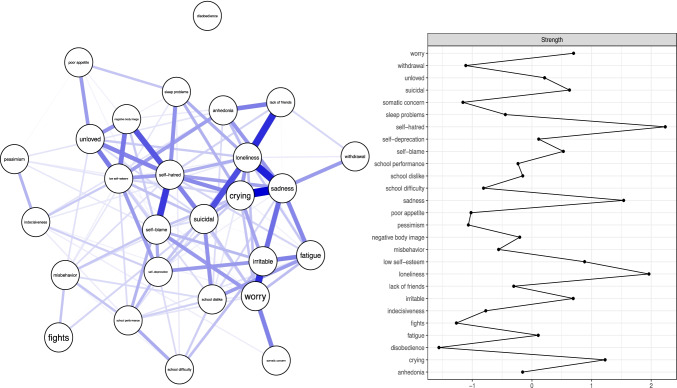
Network 3 (CDI)
Network 3 was relatively sparse compared to the previous two networks due to more nodes and smaller sample size (see Fig. 3). Self-hatred (Strength = 2.24), loneliness (Strength = 1.96), and sadness (Strength = 1.54) were highly central symptoms in the network, significantly more central than 76% of other symptoms as indicated by strength. Strength scores and variance of the symptoms weren’t significantly correlated (rs = 0.23, p = 0.26), so centrality calculation wasn’t biased by variability differences. Strong partial correlations existed between crying—sadness, sadness—loneliness, loneliness—lack of friends.
Fig. 3.
The left part presents the estimated network of depression (measured by SMFQ) and the right panel shows the strength scores (centrality indices) of Network 3, shown as z scores
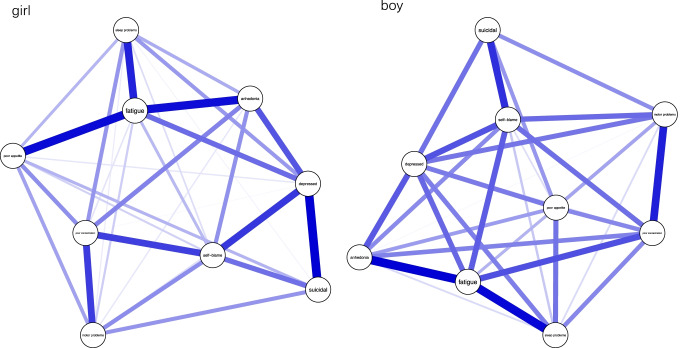
Network Comparison Between Genders
Differences between genders in the three depression networks were investigated with t-tests and NCTs. According to the results of t-tests, whereas the mean levels of depression in Sample 1 (measured with PHQ-9; t = -3.43, p = 0.001) and Sample 2 (measured with SMFQ; t = -2.31, p = 0.021) showed significant differences between boys and girls, depression level didn’t significantly differ between genders in Sample 3 (measured with CDI; t = 0.30, p = 0.77). In both Sample 1 and Sample 2, girls reported higher level of depressive symptoms than boys. Whereas the results of network comparison tests indicated no significant differences between gender in global strength in Network 1 (p = 0.85), Network 2 (p = 0.13), and Network 3 (p = 0.08), the network structures appeared to be significantly different between boys and girls for Network 1 (p = 0.005), but not for Network 2 (p = 0.06) and Network 3 (p = 0.73). Since Network 1 demonstrated significant difference in network structure between boys and girls, specific edges were further compared to elucidate gender differences. Four edges turned out to be significantly different. Fatigue—poor appetite (p = 0.00) and depressed—suicidal (p = 0.001) appeared to be more strongly connected in girls than in boys, whereas fatigue—poor concentration (p = 0.02) and depressed—motor problems (p = 0.05) were more closely related in boys than in girls (Fig. 4).
Fig. 4.
Estimated Network 1 (PHQ-9) in girl (n = 749) and boy (n = 861) participants
Discussion
The present study replicated network analyses on adolescent depression in three samples measured with three different depression instruments.
Our results revealed that sadness (depressed or miserable) and self-hatred were unanimously identified to be two of the most central symptoms of depression in the three networks among three samples of Chinese adolescents. Consistent with the results of previous network analyses (Mullarkey et al., 2019; Osborn et al., 2020; Wasil et al., 2020), this finding spoke to the stability and generalizability of the centrality of sadness and self-hatred in adolescent depression. Sad mood is usually recognized as the “hallmark” symptom of depression (American Psychiatric Association, 2013), and the centrality of sad mood is in line with the theoretical conceptualization of depression (Beck, 2002) as well as previous research of depression network in both adults and adolescents (Beard et al., 2016; Wasil et al., 2020). It’s notable that self-hatred (self-blame) was also identified as a central symptom, which was found before in adolescent samples (e.g., Wasil et al., 2020) but not in adult samples (e.g., Beard et al., 2016). During adolescence, individuals are prompted to introspect who they are and how they are perceived by others (Steinberg, 2005) and are in turn vulnerable to develop low self-esteem and form negative self-referent thinking style (Neff & Mcgehee, 2010). According to Beck’s cognitive theory of depression (Beck, 2002), negative self-referent thinking puts individuals at greater risk for developing depression, as corroborated by substantial empirical evidence (e.g., Franck et al., 2007; Orth et al., 2009). Low self-worth was also found to have high predictive value for adolescent depression (McKenzie et al., 2011). Along with previous network analyses (e.g., Mullarkey et al., 2019), our research supported self-hatred as a central symptom in depression among adolescents in diverse cultural backgrounds.
Apart from shared central symptoms (i.e., sadness and self-hatred), network analyses of three depression instruments also identified unique central nodes in their respective networks. Fatigue emerged as a central symptom in Network 1 (measured with PHQ-9), no good and everything wrong appeared to be central in Network 2 (measured with SMFQ) and Network 3 (measured with CDI) features loneliness as a central symptom. Fatigue as a central node was previously found in clinical adult samples but not in nonclinical adolescent samples (Fried et al., 2016). A probable explanation is that, somatic symptoms such as fatigue or headache are characteristic of Chinese presentation of depression (Ryder et al., 2008). Secondary school students in China are faced with exhausting academic pressure that could add to the symptom of fatigue. These contextual factors may partially account for the high centrality of fatigue in the current study. It’s also noticeable that fatigue was identified in the PHQ-9 network but not in the CDI network which also included tired as a symptom. It could be due to that PHQ-9 composed of a variety of physical behavioral symptoms such as motor problems, poor appetite and sleep problems, which had closer relationship with fatigue and increased the connectivity and strength of fatigue in the network. Cognitive characteristics common for adolescent depression, such as everything wrong and no good, emerged as central nodes in SMFQ network. This could be attributed to the focus on cognitive factors in the SMFQ and its close relationship with negative self-referent thinking style and low self-worth, which was integral to adolescent depression (McKenzie et al., 2011). Loneliness appeared to be central in the CDI network rather than in the SMFQ network. It could partially be explained by the emphasis of CDI on school life and interpersonal relationships with the inclusion of items such as lack of friends and withdrawal.
The t-test results showed that the mean scores of PHQ-9 and SMFQ showed significant gender differences, which was supportive of the widely recognized findings that girls experienced higher level of depression than boys (e.g., Hankin & Abramson, 2001). The NCT results revealed that only PHQ-9 network demonstrated significant network structure difference between boys and girls. Fatigue was more strongly related with poor appetite in girls and more closely associated with poor concentration in boys. Depressed shared stronger relationships with motor problems in boys and with suicidal ideation in girls. These results suggested that gender differences in adolescent depression may be more manifest in somatic and behavioral aspects, which was consistent with previous findings in adults (e.g., Silverstein et al., 2013).
Study Limitations and Strengths
The present study has several limitations. First, the current study raised no formal hypotheses and was exploratory in nature. Network analysis of psychopathology was a strongly exploratory and data-driven field. Especially, no study that we know has compared network models with nodes from different measuring instruments. Second, the three network analyses were conducted in three different samples varying in demographic characteristics, depression levels. Also, the sample sizes of the three studies varied considerably. Though we tried to control for the differences in sample sizes by statistical methods (i.e., using different γ), it still had the potential to skew the results. Therefore, the differences in network structure could be argued to result from differences in samples rather than node inclusions. However, for the very reason of the heterogenous samples, the results indicated the generalizability of the central role that sadness and self-hatred played in the development and maintenance of adolescent depression. Third, given the cross-sectional nature of the data, the present study can only draw conclusions about simultaneous associations among symptoms, precluding strong inference of causal interplay. Fourth, the sample of this study were nonclinical and convenient, so the structure of the present network analyses may not be completely generalizable to clinical adolescent samples. Previous research suggested that the connectivity among symptoms within the network is likely to differ between clinical and nonclinical samples (Santos et al., 2017). Future studies could examine the depression network in clinically diagnosed adolescents and compare the networks of clinical and nonclinical groups. Fifth, the current study only investigated the general network structure of depression in common samples of Chinese adolescents. However, the structures of depression can be different for adolescents faced with specific risk factors (e.g., sexual minority) (Forbes et al., 2021; Lucassen et al., 2017). Future research examining the network structures of depression in relation to different predisposing factors would broaden our understanding of the relationships within symptoms of depression as well as with other correlates (e.g., Choi et al., 2017).
These limitations notwithstanding, the current study helped to deepen our understanding of the structure of depression network in adolescent in the background of Chinese culture. In combination of previous studies (McKenzie et al., 2011), sad mood and self-hatred demonstrated to be significant in adolescent depression. Targeting self-worth in adolescents with elevated level of depression may have beneficial cascading effects on the depression network (McNally, 2016; Valente, 2012). Network structure differences in three networks indicated that researchers should be more aware of the generalizability challenge of psychopathology network derived from single scales. The network comparison tests implied that gender differences in adolescent depression was more evident in somatic and behavioral aspects.
Supplementary Information
Below is the link to the electronic supplementary material.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethical approval
The present study was approved by the relevant Ethics Committee.
Conflict of interest
The authors declare they have no financial interests.
Footnotes
= 0.25 was used in Network 3 for the sparsity of the network, following the suggestion by Epskamp and Fried (2017).
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders (DSM-5®) American Psychiatric Pub; 2013. [Google Scholar]
- Angold A, Costello EJ, Messer SC, Pickles A. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research. 1995;5(4):237–249. [Google Scholar]
- Avenevoli S, Swendsen J, He J-P, Burstein M, Merikangas KR. Major depression in the national comorbidity survey-adolescent supplement: Prevalence, correlates, and treatment. Journal of the American Academy of Child and Adolescent Psychiatry. 2015;54(1):37–44.e2. doi: 10.1016/j.jaac.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bang YR, Park JH, Kim SH. Cut-off scores of the children's depression inventory for screening and rating severity in Korean adolescents. Psychiatry Investigation. 2015;12(1):23. doi: 10.4306/pi.2015.12.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrat, A., Barthelemy, M., & Vespignani, A. (2007). The architecture of complex weighted networks: Measurements and models. In Large scale structure and dynamics of complex networks: from information technology to finance and natural science (pp. 67–92). World Scientific.
- Beard C, Millner AJ, Forgeard MJC, Fried EI, Hsu KJ, Treadway MT, Leonard CV, Kertz SJ, Björgvinsson T. Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychological Medicine. 2016;46(16):3359–3369. doi: 10.1017/S0033291716002300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT. Cognitive models of depression. Clinical Advances in Cognitive Psychotherapy: Theory and Application. 2002;14(1):29–61. [Google Scholar]
- Benner AD. The transition to high school: Current knowledge, future directions. Educational Psychology Review. 2011;23(3):299. doi: 10.1007/s10648-011-9152-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bos FM, Fried EI, Hollon SD, Bringmann LF, Dimidjian S, DeRubeis RJ, Bockting CLH. Cross-sectional networks of depressive symptoms before and after antidepressant medication treatment. Social Psychiatry and Psychiatric Epidemiology. 2018;53(6):617–627. doi: 10.1007/s00127-018-1506-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bringmann LF, Elmer T, Epskamp S, Krause RW, Schoch D, Wichers M, Wigman JTW, Snippe E. What do centrality measures measure in psychological networks? Journal of Abnormal Psychology. 2019;128(8):892–903. doi: 10.1037/abn0000446. [DOI] [PubMed] [Google Scholar]
- Bringmann LF, Lemmens L, Huibers MJH, Borsboom D, Tuerlinckx F. Revealing the dynamic network structure of the Beck Depression Inventory-II. Psychological Medicine. 2015;45(4):747–757. doi: 10.1017/S0033291714001809. [DOI] [PubMed] [Google Scholar]
- Brown TA, Barlow DH. Dimensional versus categorical classification of mental disorders in the fifth edition of the Diagnostic and statistical manual of mental disorders and beyond: Comment on the special section. Journal of Abnormal Psychology. 2005;114(4):551–556. doi: 10.1037/0021-843X.114.4.551. [DOI] [PubMed] [Google Scholar]
- Carlson GA. The challenge of diagnosing depression in childhood and adolescence. Journal of Affective Disorders. 2000;61:S3–S8. doi: 10.1016/S0165-0327(00)00283-4. [DOI] [PubMed] [Google Scholar]
- Chen J, Chen Z. Extended Bayesian information criteria for model selection with large model spaces. Biometrika. 2008;95(3):759–771. doi: 10.1093/biomet/asn034. [DOI] [Google Scholar]
- Cheng, P.-X., Cao, F.-L., & Su, L.-Y. (2009). Reliability and validity of the Short Mood and Feelings Questionnaire in Chinese adolescents. In Chinese Mental Health Journal (vol. 23, issue 1, pp. 60–62,72). Chinese Mental Health.
- Choi KW, Batchelder AW, Ehlinger PP, Safren SA, O’Cleirigh C. Applying network analysis to psychological comorbidity and health behavior: Depression, PTSD, and sexual risk in sexual minority men with trauma histories. Journal of Consulting and Clinical Psychology. 2017;85(12):1158–1170. doi: 10.1037/ccp0000241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clayborne ZM, Varin M, Colman I. Systematic review and meta-analysis: Adolescent depression and long-term psychosocial outcomes. Journal of the American Academy of Child & Adolescent Psychiatry. 2019;58(1):72–79. doi: 10.1016/j.jaac.2018.07.896. [DOI] [PubMed] [Google Scholar]
- Costantini G, Epskamp S, Borsboom D, Perugini M, Mõttus R, Waldorp LJ, Cramer AOJ. State of the aRt personality research: A tutorial on network analysis of personality data in R. Journal of Research in Personality. 2015;54:13–29. doi: 10.1002/cpp.2360. [DOI] [Google Scholar]
- Costello EJ, Copeland W, Angold A. Trends in psychopathology across the adolescent years: What changes when children become adolescents, and when adolescents become adults? Journal of Child Psychology and Psychiatry. 2011;52(10):1015–1025. doi: 10.1111/j.1469-7610.2011.02446.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dempster AP, Laird NM, Rubin DB. Maximum likelihood from incomplete data via the EM algorithm. Journal of the Royal Statistical Society: Series B (Methodological) 1977;39(1):1–22. [Google Scholar]
- Epskamp, S., Borsboom, D., & Fried, E. I. (2017). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods, 195–212. 10.3758/s13428-017-0862-1. [DOI] [PMC free article] [PubMed]
- Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, Borsboom D. qgraph: Network visualizations of relationships in psychometric data. Journal of Statistical Software. 2012;48(4):1–18. doi: 10.18637/jss.v048.i04. [DOI] [Google Scholar]
- Epskamp S, Fried EI. A tutorial on regularized partial correlation networks. Psychological Methods. 2018;23(4):617–634. doi: 10.1037/met0000167. [DOI] [PubMed] [Google Scholar]
- Forbes EE, Eckstrand KL, Rofey DL, Silk JS. A social affective neuroscience model of risk and resilience in adolescent depression: Preliminary Evidence and application to sexual and gender minority adolescents. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging. 2021;6(2):188–199. doi: 10.1016/j.bpsc.2020.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franck E, De Raedt R, De Houwer J. Implicit but not explicit self-esteem predicts future depressive symptomatology. Behaviour Research and Therapy. 2007;45(10):2448–2455. doi: 10.1016/j.brat.2007.01.008. [DOI] [PubMed] [Google Scholar]
- Fried EI. The 52 symptoms of major depression: Lack of content overlap among seven common depression scales. Journal of Affective Disorders. 2017;208:191–197. doi: 10.1016/j.jad.2016.10.019. [DOI] [PubMed] [Google Scholar]
- Fried EI, Cramer AOJ. Moving forward: Challenges and directions for psychopathological network theory and methodology. Perspectives on Psychological Science. 2017;12(6):999–1020. doi: 10.1177/1745691617705892. [DOI] [PubMed] [Google Scholar]
- Fried EI, Epskamp S, Nesse RM, Tuerlinckx F, Borsboom D. What are “good” depression symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. Journal of Affective Disorders. 2016;189:314–320. doi: 10.1016/j.jad.2015.09.005. [DOI] [PubMed] [Google Scholar]
- Fried EI, Nesse RM. The Impact of Individual Depressive Symptoms on Impairment of Psychosocial Functioning. PLoS One. 2014;9(2):e90311. doi: 10.1371/journal.pone.0090311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried EI, Nesse RM. Depression sum-scores don’t add up: Why analyzing specific depression symptoms is essential. BMC Medicine. 2015;13(1):1–11. doi: 10.1186/s12916-015-0325-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY. Development of gender differences in depression: An elaborated cognitive vulnerability-transactional stress theory. Psychological Bulletin. 2001;127(6):773–796. doi: 10.1037/0033-2909.127.6.773. [DOI] [PubMed] [Google Scholar]
- Heeren A, Jones PJ, McNally RJ. Mapping network connectivity among symptoms of social anxiety and comorbid depression in people with social anxiety disorder. Journal of Affective Disorders. 2018;228:75–82. doi: 10.1016/j.jad.2017.12.003. [DOI] [PubMed] [Google Scholar]
- Jones, P. J. (2020). networktools: Tools for identifying important nodes in networks. R package version 1.2.3.https://cran.r-project.org/package=networktools
- Jones PJ, Heeren A, McNally RJ. Commentary: A network theory of mental disorders. Frontiers in Psychology. 2017;8:1305. doi: 10.3389/fpsyg.2017.01305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D, Kwon H-J, Ha M, Lim MH, Kim KM. Network analysis for the symptom of depression with Children’s Depression Inventory in a large sample of school-aged children. Journal of Affective Disorders. 2021;281:256–263. doi: 10.1016/j.jad.2020.12.002. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Children’s depression inventory: Manual. Multi-Health Systems North Tonawanda; 1992. [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo WH, Gallo JJ, Eaton WW. Hopelessness, depression, substance disorder, and suicidality–a 13-year community-based study. Social Psychiatry & Psychiatric Epidemiology. 2004;39(6):497–501. doi: 10.1007/s00127-004-0775-z. [DOI] [PubMed] [Google Scholar]
- Levinson CA, Brosof LC, Vanzhula I, Christian C, Jones P, Rodebaugh TL, Langer JK, White EK, Warren C, Weeks JW, Menatti A, Lim MH, Fernandez KC. Social anxiety and eating disorder comorbidity and underlying vulnerabilities: Using network analysis to conceptualize comorbidity. International Journal of Eating Disorders. 2018;51(7):693–709. doi: 10.1002/eat.22890. [DOI] [PubMed] [Google Scholar]
- Lucassen MFG, Stasiak K, Samra R, Frampton CMA, Merry SN. Sexual minority youth and depressive symptoms or depressive disorder: A systematic review and meta-analysis of population-based studies. Australian & New Zealand Journal of Psychiatry. 2017;51(8):774–787. doi: 10.1177/0004867417713664. [DOI] [PubMed] [Google Scholar]
- Lux V, Kendler KS. Deconstructing major depression: A validation study of the DSM-IV symptomatic criteria. Psychological Medicine. 2010;40(10):1679–1690. doi: 10.1017/S0033291709992157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie DP, Toumbourou JW, Forbes AB, Mackinnon AJ, McMorris BJ, Catalano RF, Patton GC. Predicting future depression in adolescents using the Short Mood and Feelings Questionnaire: A two-nation study. Journal of Affective Disorders. 2011;134(1):151–159. doi: 10.1016/j.jad.2011.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally RJ. Can network analysis transform psychopathology? Behaviour Research and Therapy. 2016;86:95–104. doi: 10.1016/j.brat.2016.06.006. [DOI] [PubMed] [Google Scholar]
- McNally RJ, Mair P, Mugno BL, Riemann BC. Co-morbid obsessive–compulsive disorder and depression: A Bayesian network approach. Psychological Medicine. 2017;47(7):1204–1214. doi: 10.1017/S0033291716003287. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He J-P, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullarkey MC, Marchetti I, Beevers CG. Using network analysis to identify central symptoms of adolescent depression. Journal of Clinical Child and Adolescent Psychology. 2019;48(4):656–668. doi: 10.1080/15374416.2018.1437735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nardi B, Francesconi G, Catena-Dell’osso M, Bellantuono C. Adolescent depression: Clinical features and therapeutic strategies. European Review for Medical and Pharmacological Sciences. 2013;17(11):1546–1551. [PubMed] [Google Scholar]
- Neff KD, Mcgehee P. Self-compassion and psychological resilience among adolescents and young adults. Self & Identity. 2010;9(3):225–240. doi: 10.1080/15298860902979307. [DOI] [Google Scholar]
- Olatunji BO, Levinson C, Calebs B. A network analysis of eating disorder symptoms and characteristics in an inpatient sample. Psychiatry Research. 2018;262:270–281. doi: 10.1016/j.psychres.2018.02.027. [DOI] [PubMed] [Google Scholar]
- Opsahl T, Agneessens F, Skvoretz J. Node centrality in weighted networks: Generalizing degree and shortest paths. Social Networks. 2010;32(3):245–251. doi: 10.1016/j.socnet.2010.03.006. [DOI] [Google Scholar]
- Orth U, Robins RW, Trzesniewski KH, Maes J, Schmitt M. Low self-esteem is a risk factor for depressive symptoms from young adulthood to old age. Journal of Abnormal Psychology. 2009;118(3):472–478. doi: 10.1037/a0015922. [DOI] [PubMed] [Google Scholar]
- Osborn, T. L., Campbell, S., Ndetei, D., & Weisz, J. (2020). Network Analysis Reveals Central Symptoms of Adolescent Depression and Anxiety in Sub-Saharan Africa. 10.31234/osf.io/dv6c9
- Ryder AG, Sun J, Zhu X, Yao S, Chentsova-Dutton YE. Depression in China: Integrating developmental psychopathology and cultural-clinical psychology. Journal of Clinical Child & Adolescent Psychology. 2012;41(5):682–694. doi: 10.1080/15374416.2012.710163. [DOI] [PubMed] [Google Scholar]
- Ryder AG, Yang J, Zhu X, Yao S, Yi J, Heine SJ, Bagby RM. The cultural shaping of depression: Somatic symptoms in China, psychological symptoms in North America? Journal of Abnormal Psychology. 2008;117(2):300–313. doi: 10.1037/0021-843X.117.2.300. [DOI] [PubMed] [Google Scholar]
- Santor DA, Gregus M, Welch A. FOCUS ARTICLE: Eight decades of measurement in depression. Measurement: Interdisciplinary Research and Perspectives. 2006;4(3):135–155. doi: 10.1207/s15366359mea0403_1. [DOI] [Google Scholar]
- Santos JH, Fried EI, Asafu-Adjei J, Ruiz RJ. Network structure of perinatal depressive symptoms in Latinas: Relationship to stress and reproductive biomarkers. Research in Nursing & Health. 2017;40(3):218–228. doi: 10.1002/nur.21784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmittmann VD, Cramer AOJ, Waldorp LJ, Epskamp S, Kievit RA, Borsboom D. Deconstructing the construct: A network perspective on psychological phenomena. New Ideas in Psychology. 2013;31(1):43–53. doi: 10.1016/j.newideapsych.2011.02.007. [DOI] [Google Scholar]
- Silverstein B, Edwards T, Gamma A, Ajdacic-Gross V, Rossler W, Angst J. The role played by depression associated with somatic symptomatology in accounting for the gender difference in the prevalence of depression. Social Psychiatry and Psychiatric Epidemiology. 2013;48(2):257–263. doi: 10.1007/s00127-012-0540-7. [DOI] [PubMed] [Google Scholar]
- Simon N, Friedman J, Hastie T, Tibshirani R. Regularization paths for Cox’s proportional hazards model via coordinate descent. Journal of Statistical Software. 2011;39(5):1. doi: 10.18637/jss.v039.i05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L. Cognitive and affective development in adolescence. Trends in Cognitive Sciences. 2005;9(2):69–74. doi: 10.1016/j.tics.2004.12.005. [DOI] [PubMed] [Google Scholar]
- Tang X, Tang S, Ren Z, Wong DFK. Prevalence of depressive symptoms among adolescents in secondary school in mainland China: A systematic review and meta-analysis. Journal of Affective Disorders. 2019;245:498–507. doi: 10.1016/j.jad.2018.11.043. [DOI] [PubMed] [Google Scholar]
- Terluin B, De Boer MR, De Vet HCW. Differences in connection strength between mental symptoms might be explained by differences in variance: Reanalysis of network data did not confirm staging. PLoS One. 2016;11(11):e0155205. doi: 10.1371/journal.pone.0155205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tweed DL. Depression-related impairment: Estimating concurrent and lingering effects. Psychological Medicine. 1993;23(2):373–386. doi: 10.1017/S0033291700028476. [DOI] [PubMed] [Google Scholar]
- Valente TW. Network interventions. Science. 2012;337(6090):49–53. doi: 10.1126/science.1217330. [DOI] [PubMed] [Google Scholar]
- van Borkulo, C., van Bork, R., Boschloo, L., Kossakowski, J., Tio, P., Schoevers, R., Borsboom, D., & Waldorp, L. (2017). Comparing network structures on three aspects: A permutation test. 10.13140/RG.2.2.29455.38569. [DOI] [PubMed]
- Wang M-C, Deng Q. The mechanism of auxiliary variables in full information maximum likelihood–based structural equation models with missing data. Acta Psychologica Sinica. 2016;48(11):1489. doi: 10.3724/SP.J.1041.2016.01489. [DOI] [Google Scholar]
- Wasil AR, Venturo-Conerly KE, Shinde S, Patel V, Jones PJ. Applying network analysis to understand depression and substance use in Indian adolescents. Journal of Affective Disorders. 2020;265:278–286. doi: 10.1016/j.jad.2020.01.025. [DOI] [PubMed] [Google Scholar]
- Wilk CM, Bolton P. Local perceptions of the mental health effects of the Uganda acquired immunodeficiency syndrome epidemic. Journal of Nervous & Mental Disease. 2002;190(6):394–397. doi: 10.1097/00005053-200206000-00008. [DOI] [PubMed] [Google Scholar]
- Wu, W.-F., Lu, Y.-B., Tan, F.-R., & Yao, S.-Q. (2010). Reliability and validity of the Chinese version of Children’s Depression Inventory. In Chinese Mental Health Journal (vol. 24, issue 10, pp. 775–779). Chinese Mental Health.
- Xu D-D, Rao W-W, Cao X-L, Wen S-Y, Che W-I, Ng CH, Ungvari GS, Du Y, Zhang L, Xiang Y-T. Prevalence of major depressive disorder in children and adolescents in China: A systematic review and meta-analysis. Journal of Affective Disorders. 2018;241:592–598. doi: 10.1016/j.jad.2018.07.083. [DOI] [PubMed] [Google Scholar]
- Yu X, Tam W, Wong P, Lam T, Stewart S. The Patient Health Questionnaire-9 for measuring depressive symptoms among the general population in Hong Kong. Comprehensive Psychiatry. 2012;53(1):95–102. doi: 10.1016/j.comppsych.2010.11.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.