Abstract
Poor healing of cutaneous wounds is a common medical problem in the field of traumatology. Due to the intricate pathophysiological processes of wound healing, the use of conventional treatment methods, such as chemical molecule drugs and traditional dressings, have been unable to achieve satisfactory outcomes. Within recent years, explicit evidence suggests that mesenchymal stem cells (MSCs) have great therapeutic potentials on skin wound healing and regeneration. However, the direct application of MSCs still faces many challenges and difficulties. Intriguingly, exosomes as cell-secreted granular vesicles with a lipid bilayer membrane structure and containing specific components from the source cells may emerge to be excellent substitutes for MSCs. Exosomes derived from MSCs (MSC-exosomes) have been demonstrated to be beneficial for cutaneous wound healing and accelerate the process through a variety of mechanisms. These mechanisms include alleviating inflammation, promoting vascularization, and promoting proliferation and migration of epithelial cells and fibroblasts. Therefore, the application of MSC-exosomes may be a promising alternative to cell therapy in the treatment of cutaneous wounds and could promote wound healing through multiple mechanisms simultaneously. This review will provide an overview of the role and the mechanisms of MSC-derived exosomes in cutaneous wound healing, and elaborate the potentials and future perspectives of MSC-exosomes application in clinical practice.
Keywords: Mesenchymal stem cells, Extracellular vesicles, Exosomes, Wound healing, Skin regeneration
Core Tip: The promotion of wound healing is an important obstacle in the treatment of trauma in clinic. Exosomes derived from mesenchymal stem cells (MSCs) may provide a novel remedy with advantages and prospects. Herein, we discuss the role and the underlying mechanisms via which MSC-derived exosomes improve cutaneous wound healing, and elaborate the potentials and future perspectives of MSC-exosome application in clinical practice.
INTRODUCTION
The skin, as our body’s barrier to the external environment, plays a crucial role in defense against surrounding challenges, such as ultraviolet rays in sunlight and pathogens. Additionally, the skin is crucial to our mental health due to its sensory perception and aesthetic maintenance functions. However, our skin is very vulnerable to trauma or burns and is prone to develop chronic wounds or ulcers under certain pathological conditions, such as diabetes mellitus[1]. Currently, the standard therapeutic strategy to promote wound healing is application of biologics, including growth factors and cytokines[2]. Nonetheless, since wound healing is a dynamic and complex process involving various cell types and crosstalk between cells and the extracellular matrix (ECM), the therapeutic effects of biologics are limited and unsatisfactory[2,3]. Therefore, novel curative paradigms for acute and chronic cutaneous wounds need to be explored.
Intriguingly, stem cell-based therapies emerge to show great potential for regeneration of damaged tissues in both preclinical and clinical trials[4-8]. Remedies based on stem cells have many advantages over conventional therapies based on growth factors or cytokine biologicals, as stem cells possess a higher ability of regeneration, and promote the healing process and regeneration in multifactorial ways. Particularly, mesenchymal stem cells (MSCs) are the major stem cell types that have shown definite therapeutic effects on a variety of tissue injuries[9]. MSCs are multipotent mesenchymal stromal cells with the capabilities of self-renewal and multi-lineage differentiation. They exist extensively in the body and can be obtained from many tissues such as bone marrow, adipose tissue, dental tissue, umbilical cord, etc. A large body of evidence has shown that MSCs derived from several tissues exhibit great therapeutic potentials for enhancing cutaneous wound healing and regeneration via the regulation of multiple processes, including cell migration and proliferation, angiogenesis, inflammation resolution, and ECM remodeling[10]. Nevertheless, the direct application of MSCs as a cellular therapy for tissue injuries still involves many limitations and obstacles. A non-negligible limitation is the risk of teratoma occurrence and immunogenicity, of which the incidence increases with the culture expansion or cryopreservation of cells[1,11]. Moreover, the extraction, transportation, and expansion of MSCs are invasive or time-consuming procedures that are also difficult to perform in clinic. From the cell delivery point of view, the majority of MSCs via systemic delivery (intravenous infusion) are entrapped in the lungs, resulting in few cells migrating through the pulmonary capillaries and reaching the target sites[9,11]. Also, the survival, retention, and engraftment of MSCs in local application are limited. Notably, recent studies of the MSC therapeutic mechanism have revealed that the positive effects of MSCs on cutaneous wounds are predominantly mediated via paracrine actions rather than differentiation[12-14]. Thus, the application of MSC extracts may be a more feasible and practical paradigm than direct cellular delivery treatment. Recently, with advances in research on MSC-based therapy, MSC-derived extracellular vesicles (EVs), especially exosomes, have demonstrated promising results in cutaneous wound healing and skin regeneration. The application of exosomes has become a novel and cell-free therapeutic paradigm and been given high expectations due to their convenience in clinical practice.
In this review, we summarize the applications of MSC-derived exosomes in cutaneous regeneration and expound the underlying cellular and molecular mechanisms. We also explicate the future perspectives for their application in clinic, as well as latent problems to be solved.
EVs AND EXOSOMES
EVs are a heterogeneous population of lipid bilayer particles with different sizes, biogenesis, composition, and functions. They are secreted from most types of cells in the body and contain the components of the donor cells, including a variety of specific proteins, lipids, and nucleic acid molecules[15]. Thus, to a certain extent, they inherit the functional properties of the parental cells and are considered important constituents in intercellular communication, as they are loaded with signal biomolecules and shuttle from donor cells to recipient cells[16-18]. According to their diameters or biogenesis, EVs are usually divided into three main subtypes, i.e. exosomes, microvesicles, and apoptotic bodies. Microvesicles and apoptotic bodies are vesicles derived from budding and pinching out of the surface of plasma membrane, while exosomes are vesicles derived from intracellular endosomes. Within recent years, exosomes as a special category of EVs, are more widely and deeply studied.
Exosomes are spherical lipid bilayer vesicles with distributed diameters ranging from 30-150 nm. The biogenesis of exosomes is through a series of membrane-trafficking processes[19]. Firstly, invagination of the plasma membrane or budding of intracellular organelle membranes gives rise to early endosomes. Secondly, intraluminal vesicles (ILVs) are generated as early endosomes invaginate inward, generating the so-called multivesicular bodies (MVBs). ILVs within MVBs can either degrade in the lysosome or undergo exocytosis when transporting with MVBs to fuse with the plasma membrane. Exosomes are generated when ILVs are secreted to the extracellular space[20]. The released exosomes can arrive at their target cells in a paracrine way or through the circulation and then be internalized by the recipient cells in the following ways: Ligand-receptor interaction; surface molecule-mediated endocytosis, micropinocytosis, or phagocytosis; or plasmatic membrane fusion with the recipient cells[21]. Following the release of exosome enclosed contents in the recipient cytoplasm, alterations of intracellular signaling pathways occur in recipient cells to modulate cellular processes and functions. Thus, the basic biology of exosomes indicates that MSC-exosomes may contain MSC-specific components to exert specific effects on recipient cells, which are somewhat equivalent to the therapeutic effects of MSCs.
TRANSLATIONAL POTENTIALS AND REGULATORY ASPECTS OF MSC-EXOSOMES
Cell therapy has made great progress in clinical practice and a growing number clinical trials involving MSC-based therapy have reported therapeutic efficacy[22]. However, the application of exosomes as therapeutic biologics takes on many advantages over the whole MSCs[19,23]. Firstly, exosomes can be stored and transported at low temperatures for a longer duration without significant loss in bioactivity than whole cells. Secondly, exosomes have better penetrating abilities to cross biological barriers, such as the blood brain barrier, and avoid entrapment in filter organs or tissues. Also, their lipid bilayer membranes can protect the bioactivity of content molecules in a sophisticated physiological environment. Thirdly, exosomes can be engineered to obtain specific properties and can be quantitatively administered to patients in clinic to obtain better clinical effects. Lastly, they are safer than cell transplantation therapy, with less risk of neoplastic transformation[24] and immune response activation[25].
Exosomes are natural bi-layered lipid spheres possessing high skin penetration efficiency, similar to liposomal nanoparticles[26,27]. This enables topical administration of exosomes, rendering wound areas more receptive to the therapeutic exosomes[28]. Furthermore, delivered exosomes can also be chemotactic to the inflammatory or injured site when a distance exists between the administered area and the lesion center[29]. Additionally, with a variety of bioactive molecules inside, exosomes can exert their curative benefits through many different therapeutic mechanisms simultaneously, which leads to better biological effects than small molecular compounds.
Nevertheless, when we consider exosomes as biological agents in clinical application, there are a series of nonnegligible challenges in the regulatory and quality control aspects of exosome manufacturing. Due to the lack of standardizations in the methodology or procedures for the collection and isolation of exosomes, exosome products often differ in safety and quality aspects. Regarding the challenge of safety considerations, exosome manufacturing should follow clinical good manufacturing practice protocols like other pharmaceutical preparations to obtain clinical-grade exosome preparations. Besides, with the successful development and use of various serum-free media, the medium that do not contain animal serum is recommended for MSC culturing to avoid mixing of exogenous exosomes derived from animal serum. Also, bioengineering technology may be applied to modify exosome phenotypes or contents, which can add or subtract specific biological molecules possessed by exosomes to increase efficacy or reduce undesirable effects during the therapeutic course[30,31].
Homogeneity and quality control are also important considerations or challenges in the regulatory aspect. Exosome homogeneity cannot be attained with certainty as with chemically defined drugs, even exosomes from the same cell are heterogeneous. However, exosome heterogeneity does not preclude adoption of exosome products in clinical practice. A variety of experimental techniques can be used to determine the mechanism of action of exosomes in therapy. We can subsequently regulate the major active ingredients within exosomes related to the mechanism of action to assure quality and potency[32]. With a better understanding of the mechanism of action, we can identify the exact active ingredients and overexpress them to improve homogeneity and determine the quality control strategy of manufacturing. Moreover, screening exosomes with biomarkers, such as surface receptors, is also a method to obtain more homogenous exosomes and to enrich exosomes with higher efficacy[33]. Although the lack of standardizations in the methodology for the collection, isolation, and analysis of exosomes can affect the exosome contents and potency, we can still determine the mainly active contents responsible for therapeutic efficacy by inactivation assay. Additionally, once active contents are identified, we can use them to establish quality control as described above and determine the best methodology for the collection, isolation, and purification of exosomes[34].
The regulation and quality control of exosome products need further development, so there is still a long way to go before they can be authentically used in clinical practice. Yet this course needs to be based on in-depth exploration of the underlying mechanisms of action. Thus, in the following part of this review, we elaborate on the underlying mechanisms of MSC-derived exosomes in cutaneous wound healing and regeneration.
MECHANISMS OF MSC-EXOSOMES IN CUTANEOUS WOUND HEALING AND REGE NERATION
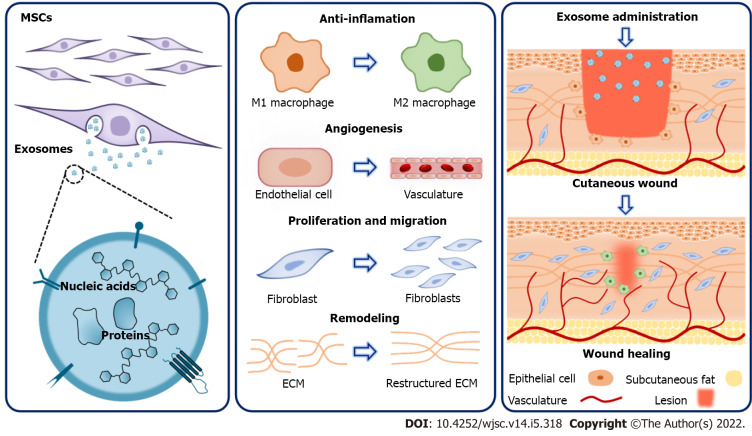
Cutaneous wound healing is a dynamic physiological process which is initiated when the normal anatomical structure or integrity of the skin are destructed. It is an intrinsic protective mechanism of the skin itself to ameliorate damage, restrain infection, and restore the anatomical structure and function. The typical cutaneous wound healing process can be summarized as a series of overlapping phases: Hemostatic phase, inflammation phase, proliferation phase, and remodeling phase[35]. During these phases, a series of orchestrated biological events sequentially occur: The damaged cutaneous tissue is activated to recruit various cell types involved in the following events; immune cells are chemoattracted to clear pathogens and damaged tissues; fibroblasts proliferate and produce ECM to support re-epithelization; the newly produced ECM is remodeled to stabilize the wound sites[36]. It has been demonstrated in multiple wound healing models that exosomes obtained from various cell types exert beneficial effects on the whole process of wound healing, particularly in the inflammation, proliferation, and remodeling phases (Figure 1).
Figure 1.
Mechanisms underlying the therapeutic effects of mesenchymal stem cell-derived exosomes on cutaneous wound healing. Mesenchymal stem cell (MSC)-derived exosomes contain a variety of proteins and nucleic acids and hold great potential for promoting cutaneous wound healing. Specifically, MSC-derived exosomes exert therapeutic effects through multiple mechanisms. They can inhibit inflammation via modulating macrophage polarization. Besides, during the proliferation phase, MSC-exosomes promote angiogenesis, as well as the proliferation and migration of fibroblasts. Furthermore, MSC-exosomes can improve extracellular matrix remodeling. As a result, MSC-derived exosomes have offered a new paradigm in the treatment of cutaneous wounds. ECM: Extracellular matrix; MSC: Mesenchymal stem cell.
During the inflammation phase, neutrophils first infiltrate into the injury site to remove microbial pathogens and then undergo apoptosis, followed by macrophages infiltration, which engulf cellular debris, apoptotic neutrophils, and other apoptotic cells. Of note, macrophages play a distinctive and important role in the cutaneous regeneration process. Recent evidence has suggested that macrophages present two anti-functional phenotypes: Pro-inflammatory M1 phenotype and anti-inflammatory M2 phenotype. Following injury, M1 macrophages can promote pro-inflammatory activities which are necessary for the protective actions of inflammation and eliminating damaged tissue and cells, while M2 macrophages elicit anti-inflammatory activities, which facilitate tissue repair and regeneration[37]. However, excessive pro-inflammation activities, as well as inadequate anti-inflammatory activities, can lead to risks of developing chronic wounds or fibrosis. Evidence suggests that exosomes can elicit M2 polarization through transferring microRNAs (miRNAs). He et al[38] reported that exosomes derived from bone marrow MSCs (BMMSCs) induced macrophage polarization toward the M2 phenotype; they further reported that the polarization was regulated by miR-223 derived from exosomes of MSCs, which targets pknox1. Additionally, human umbilical cord MSCs (hUCMSCs)-derived exosomes can regulate the inflammatory reaction of macrophages in burned rats through miR-181c[39]. The study showed that miR-181c could effectively suppress the toll-like receptor 4 (TLR4) signaling pathway, preserving the increased levels of tumor necrosis factor α (TNF-α) and interleukin-1β (IL-1β) and the decreased levels of IL-10 in macrophages, which indicates M2 polarization. Particularly, the polarization effects of MSC-exosomes can be enhanced under preconditioning by lipopolysaccharide (LPS). A study exploring the curative effects of exosomes derived from LPS pre-treated MSCs (LPS pre-exosomes) on wound healing inflammation has confirmed that LPS pre-exosomes have better immunotherapeutic potential and ability than untreated MSC-derived exosomes to promote M2 macrophage activation[40]. The enhanced effect is associated with the unique expression of let-7b in LPS pre-exosomes and the let-7b/TLR4/NF-κB/STAT3/AKT regulatory signaling pathway in macrophages. Moreover, exosomes derived from adipose-derived MSCs (ADMSCs) have been proven to exert similar effects on macrophage polarization. In the study by Zhao et al[41], treatment of obese mice with ADMSC-derived exosomes lead to significant attenuation in adipose inflammation and obesity through M2 macrophage polarization. ADMSC-derived exosomes can promote M2 polarization through the transactivation of arginase-1 by exosome-carried active STAT3. Although this effect of ADMSC-derived exosomes was not expressed in the skin wound healing model, the results still indicate the promising role of ADMSC-derived exosomes in the inflammation process of wound healing. Generally, macrophages are major inflammatory mediators in cutaneous repair, whereas some observations show that T-cells also play an important role in the inflammation modulating process[42]. Evidence suggested that MSC-exosomes can switch activated T-cells into the T-regulatory phenotype to suppress the inflammatory response[43]. Recently, studies have revealed that local application of exosomes can regulate the innate and adaptive immune networks as a whole, and better promote wound healing[44]. These indicate that MSC-exosomes can exert multiple effects in the inflammation phase of wound healing. Yet, more detailed mechanisms underlying exosome-mediated inflammation modulation need to be clarified by future studies.
During the proliferation phase, mainly four regenerative episodes occur: Fibroblast proliferation, production of ECM components, re-epithelization and angiogenesis. Under permitted conditions created by the prior inflammation phase, the four episodes are orchestrated to regenerate new tissues and restore the morphology and function of the skin. A substantial body of evidence has shown that exogenetic exosomes have positive therapeutic effects on these four processes. In the in vitro study by Shabbir et al[45], MSC-exosomes could enhance the proliferation and migration of fibroblasts and increase tube formation by human umbilical vein endothelial cells, both in a dose-dependent manner. The effects were proven to be triggered by activations of intracellular signaling pathways involving AKT, ERK, and STAT3, which are known to be important in wound healing. The same results of human ADMSC-derived exosomes were verified in experiments by Choi et al[46] and Zhang et al[47]. In the study by Zhang et al[47], ADMSC-derived exosomes were shown to have positive actions on fibroblasts, which promote collagen deposition and expression of growth factors, such as basic fibroblast growth factor (bFGF) and transforming growth factor-β1 (TGF-β1), both in vitro and in vivo via modulating the PI3K/AKT signaling pathway. Apart from fibroblasts, BMSC-derived exosomes could also repress apoptosis of HaCaT cells (human immortalized epidermal cells) induced by hydrogen peroxide via the miR-93-3p/APAF1 axis[48]. Also, research demonstrated that ADMSC-derived exosomes could prompt proliferation and migration of HaCaT cells via Wnt/β-catenin signaling[49]. These indicate that MSC-exosomes can accelerate the process of re-epithelization in the proliferation phase. In a more extensive study by Ren et al[50], the effects of ADMSC-derived microvesicles (ADMSC-MVs) were examined on fibroblasts, keratinocytes, and endothelial cells both in vitro and in vivo. Their research revealed that ADMSC-MVs promoted the proliferation, migration of these cells via AKT and ERK signaling pathways, resulting in upregulations of growth factors, such as vascular endothelial growth factor A, platelet derived growth factor A, epidermal growth factor, and FGF2, and enhancement of re-epithelialization, collagen deposition and neovascularization. Additionally, exosomes derived from other MSCs were also verified to be bioactive in the proliferation phase. Zhang et al[51] reported that hUCMSCs-derived exosomes could enhance re-epithelialization and cell proliferation in rat skin burn model via the activation of the Wnt/β-catenin pathway. Meanwhile, heat stress-induced apoptosis was reduced by hUCMSC-derived exosomes via activation of the AKT pathway. Another study by Zhang et al[52] reported that exosomes derived from human induced pluripotent stem cell-derived MSCs (hiPSC-MSCs) had similar effects with MSC-derived exosomes on the proliferation of fibroblasts and angiogenesis of endothelial cells. In a later study by Kim et al[53], hiPSC-MSC-derived exosomes could also promote re-epithelization by stimulating the ERK1/2 pathway. Other than exosomes derived from MSCs, Zhao et al[54] reported that exosomes derived from human amniotic epithelial cells (hAEC-exosomes) could promote the proliferation and function of fibroblasts via miRNAs so as to accelerate wound healing. Although the results mentioned above highlight the therapeutic roles of exosomes derived from MSCs, the exact content of the exosomes that mediate these effects in the proliferation phase remains to be further identified.
As for the remodeling phase, the newly produced ECM is restructured and reorganized: The ECM is degraded by matrix metalloproteases (MMPs) and replaced by new ECM proteins; collagen Ⅲ is converted to collagen I; fibroblasts differentiate into myofibroblasts; and then scar tissue forms. Research have demonstrated that exosomes play an intriguing role in optimizing this process. For example, ADMSC-derived exosomes increase the expression of MMP-3 and the ratio of collagen III to collagen I so as to promote ECM remodeling in murine incisional wounds[55]. Moreover, ADMSC-derived exosomes can inhibit the differentiation of fibroblasts into myofibroblasts to mitigate scar formation. Additionally, hUCMSC-derived exosomes were demonstrated to inhibit the differentiation of fibroblasts to myofibroblasts by inhibiting the TGF-β2/SMAD2 pathway through the transfer of miRNAs (miR-21, -23a, -125b, and -145), resulting in reduced scar formation in a skin-defect mouse model[56,57]. The same effects were observed in the study using exosomes derived from human amniotic fluid stem cells (hAFSCs), which showed that hAFSC-derived exosomes suppressed the excessive aggregation of myofibroblasts and ECM via inhibiting the TGF-β pathway[58]. Taken together, exosomes not only promote ECM synthesis in the proliferation phase, but also improve ECM remodeling in the late phase of wound healing to inhibit scar tissue formation.
Collectively, exosomes derived from a variety of MSCs, including BMMSCs, ADMSCs, hUCMSCs, hiPSC-MSCs, and hAECs, are demonstrated to have beneficial therapeutic effects on cutaneous wound healing through reducing inflammation, promoting re-epithelization and angiogenesis, and promoting proliferation and migration of fibroblasts, as well as enhancing ECM formation and remodeling. The above preclinical studies of MSC-exosomes in cutaneous wound are listed in Table 1.
Table 1.
Preclinical studies of mesenchymal stem cell-exosomes in cutaneous wound healing phases
|
Wound healing phase
|
Exosome cellular origin
|
Model
|
Functional effects
|
Pathways
|
Ref.
|
| Inflammation | hBMMSCs; hJMMSCs | Mice dorsal skin defects | Macrophage M2 polarization | miR-223 via pknox1 | [38] |
| hUCMSCs | Rat severe burn | M2 polarization. Inflammation alleviation | miR-181c via TLR4 | [39] | |
| LPS-pretreated hUCMSCs | Rat diabetic cutaneous wound | M2 polarization | Let-7b via TLR4/NF-κB/STAT3/AKT | [40] | |
| mBMMSCs | Mice skin excision wound | Promote beneficial regulatory T cell responses and M2 polarization | M2/Th2/Treg responses | [44] | |
| Proliferation | hADMSCs | Mice full-thickness incision wound | Promote fibroblast proliferation and migration; optimize collagen deposition | PI3K/Akt | [47] |
| hUCMSCs | Rat skin burn | Enhance re-epithelialization and cell proliferation; reduce heat stress-induced apoptosis | Wnt/β-catenin; AKT | [51] | |
| hiPSC-MSCs | Rat dorsal skin wound | Accelerate skin cell proliferation and migration; promote collagen synthesis and angiogenesis | ERK1/2 | [52,53] | |
| Remodeling | hADMSCs | Mice skin incisional wound | Mitigating scar formation; promote ECM reconstruction | ERK/MAPK | [55] |
| hUCMSCs | Mice full-thickness skin defects | Suppress myofibroblast differentiation and scar formation | TGF-β/SMAD2 | [56,57] | |
| hAFSCs | Rat full-thickness skin wound | Anti-fibrotic scarring; suppress the excessive aggregation of myofibroblasts and ECM | TGF-β | [58] |
BMMSCs: Bone marrow MSCs; ECM: Extracellular matrix; hADMSCs: Human adipose-derived MSCs; hAFSCs: Human amniotic fluid stem cells; hBMMSCs: Human BMMSCs; hiPSC-MSCs: Human induced pluripotent stem cell-derived MSCs; hJMMSCs: Human jaw bone marrow MSCs; hUCMSCs: Human umbilical cord MSCs; LPS: Lipopolysaccharide; mBMMSCs: Mice BMMSCs; MSCs: Mesenchymal stem cells; TGF-β1: Transforming growth factor-β1; TLR4: Toll-like receptor 4.
EFFECTS OF MSC-EXOSOMES ON CUTANEOUS REGENERATION IN AGING AND DISEASE
Skin anti-aging
Another application of MSC-derived exosome in cutaneous regeneration is skin anti-aging. hUCMSC-derived exosomes were tested on human skin tissues by Kim et al[59]. They discovered that the administrated exosomes were absorbed by the epidermis after 18 h and lead to increased collagen I and elastin expression levels in human skin after 3 days of treatment. In another study, iPSC-derived exosomes were used to treat aged human dermal fibroblasts (HDFs) induced by UVB (315 nm) irradiation or over passage, which reduced the damages of HDFs with increased expression of collagen I and reduced expression of natural senescence marker senescence-associated-β-galactosidase[60]. Moreover, exosomes derived from three-dimensional human dermal fibroblast spheroids (3D HDFSs) were compared with those derived from the monolayer culture of HDFs (2D HDFs)[61]. Furthermore, 3D HDFS-derived exosomes demonstrated better efficacy than 2D HDF-derived exosomes in collagen synthesis induction and decreasing MMP-1 expression by up-regulating the TGF-β/TNF-α ratio. Also, 3D HDFS-derived exosomes exhibited skin anti-aging properties in the nude mouse photoaging model. Similarly, at the molecular level, Bae et al[62] made an array analysis of mouse embryonic stem cell-derived extracellular miRNAs that are enclosed in exosomes. They screened out mmu-miR-291a-3p and proved it could inhibit cellular senescence via the TGF-β receptor 2 signaling pathway. Taken together, the evidence corroborates the positive effects of MSC-derived exosomes on skin rejuvenation and the potential application of MSC-derived exosomes in cosmetics.
Diabetic wound healing
Due to the high glucose environment and chronic inflammation conditions, patients with diabetes mellitus are often confronted with impaired wound healing, resulting in limb loss and disability. Considering their anti-inflammation and pro-proliferation properties, the application of MSC-derived exosomes in diabetic wound healing is a promising therapeutic strategy. It has been reported that the delayed healing of diabetic foot ulcers (referred to as DFUs) partly results from impaired function of endothelial progenitor cells (EPCs) in patients with diabetes mellitus. However, ADMSC-derived exosomes could promote the proliferation of EPCs and angiogenesis in a high glucose environment in vitro, and reduce the ulcerated area in DFU rats via increasing angiogenesis and growth factor expression, as well as reducing inflammation[63]. Geiger et al[64] reported that exosomes derived from human circulating fibrocytes could induce the proliferation and migration of keratinocytes and fibroblasts in diabetic mice, and accelerate diabetic wound closure in vivo. In the study performed by Dalirfardouei et al[65], exosomes derived from menstrual blood-derived MSCs were applied to full thickness excisional wounds in a diabetic mouse model, which reduced inflammation via promoting M2 macrophage polarization, strengthened angiogenesis through upregulating VEGF-A expression, enhanced re-epithelialization via activation of the NF-κB signaling pathway, and reduced scar formation via decreasing the collagen I: Collagen Ⅲ ratio. Recently, Han et al[66] reported that BMSC-derived exosomes contained lncRNA KLF3-AS1, which could induce angiogenesis to promote wound healing in diabetic condition[66]. Above all, based on the beneficial effects of MSC-derived exosomes on wound healing, MSC-derived exosomes hold great potentials in diabetic wound therapy.
Ischemic wound healing
Chronic ischemic wounds are another challenging problem in trauma clinic with delayed wound healing and therapeutic difficulties. Due to ischemia and hypoxia, the healing process of ischemic wounds is inhibited, resulting in the inadequate curative effects of conventional treatments. Thus, exosome-based therapies, with multiple therapeutic benefits, have been tentatively applied in this disease area. In the study performed by Shi et al[67], exosomes loaded with TGF-β have been proven to enhance ischemic wound healing, which suggests a promising regenerative therapy. Another study by Cooper et al[68] showed that human ADMSC-derived exosomes could stimulate HDFs migration and enhance ischemic cutaneous wound healing. All these results provide prospects and theoretical basis for clinical trials of exosomes in ischemic wounds.
Taken together, these data suggest that MSC-derived exosomes not only promote healing of cutaneous wounds in normal condition, but also in diabetic and ischemic conditions, as well as skin regeneration in the aging process. To make MSC-derived exosomes more effective in treating cutaneous wounds in special conditions, exosomes isolated from pretreated MSCs were studied. For instance, exosomes isolated from pioglitazone-pretreated BMMSCs and hypoxia ADMSCs were both confirmed to induce high-quality healing of diabetic wounds[69,70]. These experiments expand the available scope of application of exosomes in cutaneous wounds and suggest better sources of MSC-exosomes.
PERSPECTIVES FOR APPLICATION OF EXOSOMES IN CUTANEOUS WOUND HEALING AND REGENERATION
Notwithstanding the large body of evidence in the preceding sections that MSC-exosomes have positive effects on cutaneous wound healing in animal studies and preclinical trials, the data of exosomes in cutaneous wound healing from clinical studies is still inadequate. Exhilaratingly, a lot of meta-analyses demonstrate MSC-exosomes to be a potential and promising remedy for many acute and chronic diseases, including cutaneous wounds in pre-clinical studies[71-73], revealing the therapeutic effects of MSC-exosomes on inflammation and injury. These make successful clinical translation of MSC-exosomes more hopeful in cutaneous wound healing. Moreover, a randomized double-blind controlled clinical trial by Kwon et al[74] demonstrated acne scars treated with human ADMSC-exosomes and fractional CO2 laser exhibited better improvement than the control treated group, which gave a broad hint that ADMSC-exosomes provide synergistic therapeutic effects on atrophic acne scar clinical treatments[74]. Therefore, there are positive prospects of MSC-exosomes for a promising future in clinical translation.
Once MSC-exosomes are translated into clinical practice, improving their therapeutic efficacy is an issue to be prospected. One of the methods is combining exosomes and biomaterials to exert synergistic functions. Recently, Wang and colleagues[75] reported the application of exosome-loaded biocompatible natural-based methylcellulose-chitosan hydrogels in severe wound models under diabetic conditions. The hydrogels acted as three-dimensional porous scaffolds to provide a favorable environment for cell proliferation and ECM remodeling. Specifically, based on the hydrogels, exosomes could be sustainably released for a long period of time and exert lasting curative functions for better effects. The transformation of biomaterials provides a more flexible form for the application of exosomes. For instance, MSC-exosome combined hydrogel[76] and adhesive ultraviolet shielding exosome-releasing dressing[77] were applied on diabetic wound models and elicited better therapeutic effects on wound healing and skin reconstruction. Another method is bioengineering the properties of exosomes, such as their cargos or surface molecular functions. The selected molecules with therapeutic value (such as miRNAs or drugs) can be loaded in exosomes to endow exosomes with exogenous efficacy[78]. Also, the surface of exosome can be modified with some functional molecules, such as aptamers to enable the transfer of engineered exosomes to target sites when administered systematically or locally, which can improve therapeutic efficiency. Together, these above strategies will enhance the therapeutic efficacy of exosomes in cutaneous wound healing and regeneration.
Despite many exciting prospects, we need to recognize that the clinical use of exosomes is still hampered by many safety concerns and consistent regulatory issues. The clinical translation process of MSC-exosomes is still in a long way and far from the foreseeable prospect. Thus, the use of exosomes in clinic is still far from being applied until these problems are better solved and perfected.
CONCLUSION
Taken together, MSC-derived exosomes, as a cell-free therapeutic paradigm, provide a novel promising option for cutaneous regeneration. Yet, more research is needed to further excavate the curative potentials of exosomes and make them more available and suitable for clinical application.
Footnotes
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: December 31, 2021
First decision: March 13, 2022
Article in press: May 21, 2022
Specialty type: Cell and tissue engineering
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Jeyaraman M, India; Kang D, South Korea; Prasetyo EP, Indonesia; Sallustio F, Italy; Ventura C, Italy A-Editor: Flores AI, Spain S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR
Contributor Information
Jia-Chen Hu, State Key Laboratory of Military Stomatology and National Clinical Research Center for Oral Diseases and Shaanxi International Joint Research Center for Oral Diseases, Center for Tissue Engineering, School of Stomatology, The Fourth Military Medical University, Xi’an 710032, Shaanxi Province, China.
Chen-Xi Zheng, State Key Laboratory of Military Stomatology and National Clinical Research Center for Oral Diseases and Shaanxi International Joint Research Center for Oral Diseases, Center for Tissue Engineering, School of Stomatology, The Fourth Military Medical University, Xi’an 710032, Shaanxi Province, China.
Bing-Dong Sui, State Key Laboratory of Military Stomatology and National Clinical Research Center for Oral Diseases and Shaanxi International Joint Research Center for Oral Diseases, Center for Tissue Engineering, School of Stomatology, The Fourth Military Medical University, Xi’an 710032, Shaanxi Province, China.
Wen-Jia Liu, National and Local Joint Engineering Research Center of Biodiagnosis and Biotherapy, Precision Medicine Institute, Institute for Stem Cell and Regenerative Medicine, The Second Affiliated Hospital, Xi’an Jiaotong University, Xi’an 710032, Shaanxi Province, China.
Yan Jin, State Key Laboratory of Military Stomatology and National Clinical Research Center for Oral Diseases and Shaanxi International Joint Research Center for Oral Diseases, Center for Tissue Engineering, School of Stomatology, The Fourth Military Medical University, Xi’an 710032, Shaanxi Province, China. yanjin@fmmu.edu.cn.
References
- 1.Cabral J, Ryan AE, Griffin MD, Ritter T. Extracellular vesicles as modulators of wound healing. Adv Drug Deliv Rev. 2018;129:394–406. doi: 10.1016/j.addr.2018.01.018. [DOI] [PubMed] [Google Scholar]
- 2.Zielins ER, Atashroo DA, Maan ZN, Duscher D, Walmsley GG, Hu M, Senarath-Yapa K, McArdle A, Tevlin R, Wearda T, Paik KJ, Duldulao C, Hong WX, Gurtner GC, Longaker MT. Wound healing: an update. Regen Med. 2014;9:817–830. doi: 10.2217/rme.14.54. [DOI] [PubMed] [Google Scholar]
- 3.Boateng J, Catanzano O. Advanced Therapeutic Dressings for Effective Wound Healing--A Review. J Pharm Sci. 2015;104:3653–3680. doi: 10.1002/jps.24610. [DOI] [PubMed] [Google Scholar]
- 4.Kucharzewski M, Rojczyk E, Wilemska-Kucharzewska K, Wilk R, Hudecki J, Los MJ. Novel trends in application of stem cells in skin wound healing. Eur J Pharmacol. 2019;843:307–315. doi: 10.1016/j.ejphar.2018.12.012. [DOI] [PubMed] [Google Scholar]
- 5.Fukutake M, Ochiai D, Masuda H, Abe Y, Sato Y, Otani T, Sakai S, Aramaki-Hattori N, Shimoda M, Matsumoto T, Miyakoshi K, Kanai Y, Kishi K, Tanaka M. Human amniotic fluid stem cells have a unique potential to accelerate cutaneous wound healing with reduced fibrotic scarring like a fetus. Hum Cell. 2019;32:51–63. doi: 10.1007/s13577-018-0222-1. [DOI] [PubMed] [Google Scholar]
- 6.Aboulhoda BE, Abd El Fattah S. Bone marrow-derived vs adipose-derived stem cells in wound healing: value and route of administration. Cell Tissue Res. 2018;374:285–302. doi: 10.1007/s00441-018-2879-x. [DOI] [PubMed] [Google Scholar]
- 7.Yu J, Wang MY, Tai HC, Cheng NC. Cell sheet composed of adipose-derived stem cells demonstrates enhanced skin wound healing with reduced scar formation. Acta Biomater. 2018;77:191–200. doi: 10.1016/j.actbio.2018.07.022. [DOI] [PubMed] [Google Scholar]
- 8.Guo J, Hu H, Gorecka J, Bai H, He H, Assi R, Isaji T, Wang T, Setia O, Lopes L, Gu Y, Dardik A. Adipose-derived mesenchymal stem cells accelerate diabetic wound healing in a similar fashion as bone marrow-derived cells. Am J Physiol Cell Physiol. 2018;315:C885–C896. doi: 10.1152/ajpcell.00120.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kosaric N, Kiwanuka H, Gurtner GC. Stem cell therapies for wound healing. Expert Opin Biol Ther. 2019;19:575–585. doi: 10.1080/14712598.2019.1596257. [DOI] [PubMed] [Google Scholar]
- 10.Ding DC, Shyu WC, Lin SZ. Mesenchymal stem cells. Cell Transplant. 2011;20:5–14. doi: 10.3727/096368910X. [DOI] [PubMed] [Google Scholar]
- 11.Kim N, Cho SG. New strategies for overcoming limitations of mesenchymal stem cell-based immune modulation. Int J Stem Cells. 2015;8:54–68. doi: 10.15283/ijsc.2015.8.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gnecchi M, He H, Liang OD, Melo LG, Morello F, Mu H, Noiseux N, Zhang L, Pratt RE, Ingwall JS, Dzau VJ. Paracrine action accounts for marked protection of ischemic heart by Akt-modified mesenchymal stem cells. Nat Med. 2005;11:367–368. doi: 10.1038/nm0405-367. [DOI] [PubMed] [Google Scholar]
- 13.Chen B, Li Q, Zhao B, Wang Y. Stem Cell-Derived Extracellular Vesicles as a Novel Potential Therapeutic Tool for Tissue Repair. Stem Cells Transl Med. 2017;6:1753–1758. doi: 10.1002/sctm.16-0477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bjørge IM, Kim SY, Mano JF, Kalionis B, Chrzanowski W. Extracellular vesicles, exosomes and shedding vesicles in regenerative medicine - a new paradigm for tissue repair. Biomater Sci. 2017;6:60–78. doi: 10.1039/c7bm00479f. [DOI] [PubMed] [Google Scholar]
- 15.Jeppesen DK, Fenix AM, Franklin JL, Higginbotham JN, Zhang Q, Zimmerman LJ, Liebler DC, Ping J, Liu Q, Evans R, Fissell WH, Patton JG, Rome LH, Burnette DT, Coffey RJ. Reassessment of Exosome Composition. Cell. 2019;177:428–445.e18. doi: 10.1016/j.cell.2019.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schatz D, Vardi A. Extracellular vesicles - new players in cell-cell communication in aquatic environments. Curr Opin Microbiol. 2018;43:148–154. doi: 10.1016/j.mib.2018.01.014. [DOI] [PubMed] [Google Scholar]
- 17.Bang C, Thum T. Exosomes: new players in cell-cell communication. Int J Biochem Cell Biol. 2012;44:2060–2064. doi: 10.1016/j.biocel.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 18.van Niel G, D'Angelo G, Raposo G. Shedding light on the cell biology of extracellular vesicles. Nat Rev Mol Cell Biol. 2018;19:213–228. doi: 10.1038/nrm.2017.125. [DOI] [PubMed] [Google Scholar]
- 19.Riazifar M, Pone EJ, Lötvall J, Zhao W. Stem Cell Extracellular Vesicles: Extended Messages of Regeneration. Annu Rev Pharmacol Toxicol. 2017;57:125–154. doi: 10.1146/annurev-pharmtox-061616-030146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tkach M, Théry C. Communication by Extracellular Vesicles: Where We Are and Where We Need to Go. Cell. 2016;164:1226–1232. doi: 10.1016/j.cell.2016.01.043. [DOI] [PubMed] [Google Scholar]
- 21.Colombo M, Raposo G, Théry C. Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Annu Rev Cell Dev Biol. 2014;30:255–289. doi: 10.1146/annurev-cellbio-101512-122326. [DOI] [PubMed] [Google Scholar]
- 22.Krampera M, Le Blanc K. Mesenchymal stromal cells: Putative microenvironmental modulators become cell therapy. Cell Stem Cell. 2021;28:1708–1725. doi: 10.1016/j.stem.2021.09.006. [DOI] [PubMed] [Google Scholar]
- 23.Hu P, Yang Q, Wang Q, Shi C, Wang D, Armato U, Prà ID, Chiarini A. Mesenchymal stromal cells-exosomes: a promising cell-free therapeutic tool for wound healing and cutaneous regeneration. Burns Trauma. 2019;7:38. doi: 10.1186/s41038-019-0178-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ben-David U, Benvenisty N. The tumorigenicity of human embryonic and induced pluripotent stem cells. Nat Rev Cancer. 2011;11:268–277. doi: 10.1038/nrc3034. [DOI] [PubMed] [Google Scholar]
- 25.Zakrzewski JL, van den Brink MR, Hubbell JA. Overcoming immunological barriers in regenerative medicine. Nat Biotechnol. 2014;32:786–794. doi: 10.1038/nbt.2960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bi Y, Xia H, Li L, Lee RJ, Xie J, Liu Z, Qiu Z, Teng L. Liposomal Vitamin D3 as an Anti-aging Agent for the Skin. Pharmaceutics. 2019;11 doi: 10.3390/pharmaceutics11070311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carita AC, Eloy JO, Chorilli M, Lee RJ, Leonardi GR. Recent Advances and Perspectives in Liposomes for Cutaneous Drug Delivery. Curr Med Chem. 2018;25:606–635. doi: 10.2174/0929867324666171009120154. [DOI] [PubMed] [Google Scholar]
- 28.Desmet E, Van Gele M, Lambert J. Topically applied lipid- and surfactant-based nanoparticles in the treatment of skin disorders. Expert Opin Drug Deliv. 2017;14:109–122. doi: 10.1080/17425247.2016.1206073. [DOI] [PubMed] [Google Scholar]
- 29.Guo S, Perets N, Betzer O, Ben-Shaul S, Sheinin A, Michaelevski I, Popovtzer R, Offen D, Levenberg S. Intranasal Delivery of Mesenchymal Stem Cell Derived Exosomes Loaded with Phosphatase and Tensin Homolog siRNA Repairs Complete Spinal Cord Injury. ACS Nano. 2019;13:10015–10028. doi: 10.1021/acsnano.9b01892. [DOI] [PubMed] [Google Scholar]
- 30.Ferreira D, Moreira JN, Rodrigues LR. New advances in exosome-based targeted drug delivery systems. Crit Rev Oncol Hematol. 2022;172:103628. doi: 10.1016/j.critrevonc.2022.103628. [DOI] [PubMed] [Google Scholar]
- 31.Tran PHL, Xiang D, Tran TTD, Yin W, Zhang Y, Kong L, Chen K, Sun M, Li Y, Hou Y, Zhu Y, Duan W. Exosomes and Nanoengineering: A Match Made for Precision Therapeutics. Adv Mater. 2020;32:e1904040. doi: 10.1002/adma.201904040. [DOI] [PubMed] [Google Scholar]
- 32.Aheget H, Tristán-Manzano M, Mazini L, Cortijo-Gutierrez M, Galindo-Moreno P, Herrera C, Martin F, Marchal JA, Benabdellah K. Exosome: A New Player in Translational Nanomedicine. J Clin Med. 2020;9 doi: 10.3390/jcm9082380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen J, Li P, Zhang T, Xu Z, Huang X, Wang R, Du L. Review on Strategies and Technologies for Exosome Isolation and Purification. Front Bioeng Biotechnol. 2021;9:811971. doi: 10.3389/fbioe.2021.811971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Maia J, Batista S, Couto N, Gregório AC, Bodo C, Elzanowska J, Strano Moraes MC, Costa-Silva B. Employing Flow Cytometry to Extracellular Vesicles Sample Microvolume Analysis and Quality Control. Front Cell Dev Biol. 2020;8:593750. doi: 10.3389/fcell.2020.593750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guo S, Dipietro LA. Factors affecting wound healing. J Dent Res. 2010;89:219–229. doi: 10.1177/0022034509359125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carrasco E, Soto-Heredero G, Mittelbrunn M. The Role of Extracellular Vesicles in Cutaneous Remodeling and Hair Follicle Dynamics. Int J Mol Sci. 2019;20 doi: 10.3390/ijms20112758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Koh TJ, DiPietro LA. Inflammation and wound healing: the role of the macrophage. Expert Rev Mol Med. 2011;13:e23. doi: 10.1017/S1462399411001943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.He X, Dong Z, Cao Y, Wang H, Liu S, Liao L, Jin Y, Yuan L, Li B. MSC-Derived Exosome Promotes M2 Polarization and Enhances Cutaneous Wound Healing. Stem Cells Int. 2019;2019:7132708. doi: 10.1155/2019/7132708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li X, Liu L, Yang J, Yu Y, Chai J, Wang L, Ma L, Yin H. Exosome Derived From Human Umbilical Cord Mesenchymal Stem Cell Mediates MiR-181c Attenuating Burn-induced Excessive Inflammation. EBioMedicine. 2016;8:72–82. doi: 10.1016/j.ebiom.2016.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ti D, Hao H, Tong C, Liu J, Dong L, Zheng J, Zhao Y, Liu H, Fu X, Han W. LPS-preconditioned mesenchymal stromal cells modify macrophage polarization for resolution of chronic inflammation via exosome-shuttled let-7b. J Transl Med. 2015;13:308. doi: 10.1186/s12967-015-0642-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhao H, Shang Q, Pan Z, Bai Y, Li Z, Zhang H, Zhang Q, Guo C, Zhang L, Wang Q. Exosomes From Adipose-Derived Stem Cells Attenuate Adipose Inflammation and Obesity Through Polarizing M2 Macrophages and Beiging in White Adipose Tissue. Diabetes. 2018;67:235–247. doi: 10.2337/db17-0356. [DOI] [PubMed] [Google Scholar]
- 42.Nosbaum A, Prevel N, Truong HA, Mehta P, Ettinger M, Scharschmidt TC, Ali NH, Pauli ML, Abbas AK, Rosenblum MD. Cutting Edge: Regulatory T Cells Facilitate Cutaneous Wound Healing. J Immunol. 2016;196:2010–2014. doi: 10.4049/jimmunol.1502139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Monguió-Tortajada M, Roura S, Gálvez-Montón C, Pujal JM, Aran G, Sanjurjo L, Franquesa M, Sarrias MR, Bayes-Genis A, Borràs FE. Nanosized UCMSC-derived extracellular vesicles but not conditioned medium exclusively inhibit the inflammatory response of stimulated T cells: implications for nanomedicine. Theranostics. 2017;7:270–284. doi: 10.7150/thno.16154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Su N, Hao Y, Wang F, Hou W, Chen H, Luo Y. Mesenchymal stromal exosome-functionalized scaffolds induce innate and adaptive immunomodulatory responses toward tissue repair. Sci Adv. 2021;7 doi: 10.1126/sciadv.abf7207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shabbir A, Cox A, Rodriguez-Menocal L, Salgado M, Van Badiavas E. Mesenchymal Stem Cell Exosomes Induce Proliferation and Migration of Normal and Chronic Wound Fibroblasts, and Enhance Angiogenesis In Vitro. Stem Cells Dev. 2015;24:1635–1647. doi: 10.1089/scd.2014.0316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Choi EW, Seo MK, Woo EY, Kim SH, Park EJ, Kim S. Exosomes from human adipose-derived stem cells promote proliferation and migration of skin fibroblasts. Exp Dermatol. 2018;27:1170–1172. doi: 10.1111/exd.13451. [DOI] [PubMed] [Google Scholar]
- 47.Zhang W, Bai X, Zhao B, Li Y, Zhang Y, Li Z, Wang X, Luo L, Han F, Zhang J, Han S, Cai W, Su L, Tao K, Shi J, Hu D. Cell-free therapy based on adipose tissue stem cell-derived exosomes promotes wound healing via the PI3K/Akt signaling pathway. Exp Cell Res. 2018;370:333–342. doi: 10.1016/j.yexcr.2018.06.035. [DOI] [PubMed] [Google Scholar]
- 48.Shen C, Tao C, Zhang A, Li X, Guo Y, Wei H, Yin Q, Li Q, Jin P. Exosomal microRNA⁃93⁃3p secreted by bone marrow mesenchymal stem cells downregulates apoptotic peptidase activating factor 1 to promote wound healing. Bioengineered. 2022;13:27–37. doi: 10.1080/21655979.2021.1997077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ma T, Fu B, Yang X, Xiao Y, Pan M. Adipose mesenchymal stem cell-derived exosomes promote cell proliferation, migration, and inhibit cell apoptosis via Wnt/β-catenin signaling in cutaneous wound healing. J Cell Biochem. 2019;120:10847–10854. doi: 10.1002/jcb.28376. [DOI] [PubMed] [Google Scholar]
- 50.Ren S, Chen J, Duscher D, Liu Y, Guo G, Kang Y, Xiong H, Zhan P, Wang Y, Wang C, Machens HG, Chen Z. Microvesicles from human adipose stem cells promote wound healing by optimizing cellular functions via AKT and ERK signaling pathways. Stem Cell Res Ther. 2019;10:47. doi: 10.1186/s13287-019-1152-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang B, Wang M, Gong A, Zhang X, Wu X, Zhu Y, Shi H, Wu L, Zhu W, Qian H, Xu W. HucMSC-Exosome Mediated-Wnt4 Signaling Is Required for Cutaneous Wound Healing. Stem Cells. 2015;33:2158–2168. doi: 10.1002/stem.1771. [DOI] [PubMed] [Google Scholar]
- 52.Zhang J, Guan J, Niu X, Hu G, Guo S, Li Q, Xie Z, Zhang C, Wang Y. Exosomes released from human induced pluripotent stem cells-derived MSCs facilitate cutaneous wound healing by promoting collagen synthesis and angiogenesis. J Transl Med. 2015;13:49. doi: 10.1186/s12967-015-0417-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kim S, Lee SK, Kim H, Kim TM. Exosomes Secreted from Induced Pluripotent Stem Cell-Derived Mesenchymal Stem Cells Accelerate Skin Cell Proliferation. Int J Mol Sci. 2018;19 doi: 10.3390/ijms19103119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhao B, Li X, Shi X, Zhang W, Wu G, Wang X, Su L, Hu D. Exosomal MicroRNAs Derived from Human Amniotic Epithelial Cells Accelerate Wound Healing by Promoting the Proliferation and Migration of Fibroblasts. Stem Cells Int. 2018;2018:5420463. doi: 10.1155/2018/5420463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang L, Hu L, Zhou X, Xiong Z, Zhang C, Shehada HMA, Hu B, Song J, Chen L. Exosomes secreted by human adipose mesenchymal stem cells promote scarless cutaneous repair by regulating extracellular matrix remodelling. Sci Rep. 2017;7:13321. doi: 10.1038/s41598-017-12919-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhang Y, Pan Y, Liu Y, Li X, Tang L, Duan M, Li J, Zhang G. Exosomes derived from human umbilical cord blood mesenchymal stem cells stimulate regenerative wound healing via transforming growth factor-β receptor inhibition. Stem Cell Res Ther. 2021;12:434. doi: 10.1186/s13287-021-02517-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fang S, Xu C, Zhang Y, Xue C, Yang C, Bi H, Qian X, Wu M, Ji K, Zhao Y, Wang Y, Liu H, Xing X. Umbilical Cord-Derived Mesenchymal Stem Cell-Derived Exosomal MicroRNAs Suppress Myofibroblast Differentiation by Inhibiting the Transforming Growth Factor-β/SMAD2 Pathway During Wound Healing. Stem Cells Transl Med. 2016;5:1425–1439. doi: 10.5966/sctm.2015-0367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhang Y, Yan J, Liu Y, Chen Z, Li X, Tang L, Li J, Duan M, Zhang G. Human Amniotic Fluid Stem Cell-Derived Exosomes as a Novel Cell-Free Therapy for Cutaneous Regeneration. Front Cell Dev Biol. 2021;9:685873. doi: 10.3389/fcell.2021.685873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kim YJ, Yoo SM, Park HH, Lim HJ, Kim YL, Lee S, Seo KW, Kang KS. Exosomes derived from human umbilical cord blood mesenchymal stem cells stimulates rejuvenation of human skin. Biochem Biophys Res Commun. 2017;493:1102–1108. doi: 10.1016/j.bbrc.2017.09.056. [DOI] [PubMed] [Google Scholar]
- 60.Oh M, Lee J, Kim YJ, Rhee WJ, Park JH. Exosomes Derived from Human Induced Pluripotent Stem Cells Ameliorate the Aging of Skin Fibroblasts. Int J Mol Sci. 2018;19 doi: 10.3390/ijms19061715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hu S, Li Z, Cores J, Huang K, Su T, Dinh PU, Cheng K. Needle-Free Injection of Exosomes Derived from Human Dermal Fibroblast Spheroids Ameliorates Skin Photoaging. ACS Nano. 2019;13:11273–11282. doi: 10.1021/acsnano.9b04384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bae YU, Son Y, Kim CH, Kim KS, Hyun SH, Woo HG, Jee BA, Choi JH, Sung HK, Choi HC, Park SY, Bae JH, Doh KO, Kim JR. Embryonic Stem Cell-Derived mmu-miR-291a-3p Inhibits Cellular Senescence in Human Dermal Fibroblasts Through the TGF-β Receptor 2 Pathway. J Gerontol A Biol Sci Med Sci. 2019;74:1359–1367. doi: 10.1093/gerona/gly208. [DOI] [PubMed] [Google Scholar]
- 63.Li X, Xie X, Lian W, Shi R, Han S, Zhang H, Lu L, Li M. Exosomes from adipose-derived stem cells overexpressing Nrf2 accelerate cutaneous wound healing by promoting vascularization in a diabetic foot ulcer rat model. Exp Mol Med. 2018;50:1–14. doi: 10.1038/s12276-018-0058-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Geiger A, Walker A, Nissen E. Human fibrocyte-derived exosomes accelerate wound healing in genetically diabetic mice. Biochem Biophys Res Commun. 2015;467:303–309. doi: 10.1016/j.bbrc.2015.09.166. [DOI] [PubMed] [Google Scholar]
- 65.Dalirfardouei R, Jamialahmadi K, Jafarian AH, Mahdipour E. Promising effects of exosomes isolated from menstrual blood-derived mesenchymal stem cell on wound-healing process in diabetic mouse model. J Tissue Eng Regen Med. 2019;13:555–568. doi: 10.1002/term.2799. [DOI] [PubMed] [Google Scholar]
- 66.Han ZF, Cao JH, Liu ZY, Yang Z, Qi RX, Xu HL. Exosomal lncRNA KLF3-AS1 derived from bone marrow mesenchymal stem cells stimulates angiogenesis to promote diabetic cutaneous wound healing. Diabetes Res Clin Pract. 2022;183:109126. doi: 10.1016/j.diabres.2021.109126. [DOI] [PubMed] [Google Scholar]
- 67.Shi A, Li J, Qiu X, Sabbah M, Boroumand S, Huang TC, Zhao C, Terzic A, Behfar A, Moran SL. TGF-β loaded exosome enhances ischemic wound healing in vitro and in vivo. Theranostics. 2021;11:6616–6631. doi: 10.7150/thno.57701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cooper DR, Wang C, Patel R, Trujillo A, Patel NA, Prather J, Gould LJ, Wu MH. Human Adipose-Derived Stem Cell Conditioned Media and Exosomes Containing MALAT1 Promote Human Dermal Fibroblast Migration and Ischemic Wound Healing. Adv Wound Care (New Rochelle) 2018;7:299–308. doi: 10.1089/wound.2017.0775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hu Y, Tao R, Chen L, Xiong Y, Xue H, Hu L, Yan C, Xie X, Lin Z, Panayi AC, Mi B, Liu G. Exosomes derived from pioglitazone-pretreated MSCs accelerate diabetic wound healing through enhancing angiogenesis. J Nanobiotechnology. 2021;19:150. doi: 10.1186/s12951-021-00894-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wang J, Wu H, Peng Y, Zhao Y, Qin Y, Zhang Y, Xiao Z. Hypoxia adipose stem cell-derived exosomes promote high-quality healing of diabetic wound involves activation of PI3K/Akt pathways. J Nanobiotechnology. 2021;19:202. doi: 10.1186/s12951-021-00942-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bailey AJM, Li H, Kirkham AM, Tieu A, Maganti HB, Shorr R, Fergusson DA, Lalu MM, Elomazzen H, Allan DS. MSC-Derived Extracellular Vesicles to Heal Diabetic Wounds: a Systematic Review and Meta-Analysis of Preclinical Animal Studies. Stem Cell Rev Rep. 2022;18:968–979. doi: 10.1007/s12015-021-10164-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tieu A, Hu K, Gnyra C, Montroy J, Fergusson DA, Allan DS, Stewart DJ, Thébaud B, Lalu MM. Mesenchymal stromal cell extracellular vesicles as therapy for acute and chronic respiratory diseases: A meta-analysis. J Extracell Vesicles. 2021;10:e12141. doi: 10.1002/jev2.12141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Liu C, Wang J, Hu J, Fu B, Mao Z, Zhang H, Cai G, Chen X, Sun X. Extracellular vesicles for acute kidney injury in preclinical rodent models: a meta-analysis. Stem Cell Res Ther. 2020;11:11. doi: 10.1186/s13287-019-1530-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kwon HH, Yang SH, Lee J, Park BC, Park KY, Jung JY, Bae Y, Park GH. Combination Treatment with Human Adipose Tissue Stem Cell-derived Exosomes and Fractional CO2 Laser for Acne Scars: A 12-week Prospective, Double-blind, Randomized, Split-face Study. Acta Derm Venereol. 2020;100:adv00310. doi: 10.2340/00015555-3666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wang C, Liang C, Wang R, Yao X, Guo P, Yuan W, Liu Y, Song Y, Li Z, Xie X. The fabrication of a highly efficient self-healing hydrogel from natural biopolymers loaded with exosomes for the synergistic promotion of severe wound healing. Biomater Sci. 2019;8:313–324. doi: 10.1039/c9bm01207a. [DOI] [PubMed] [Google Scholar]
- 76.Yang J, Chen Z, Pan D, Li H, Shen J. Umbilical Cord-Derived Mesenchymal Stem Cell-Derived Exosomes Combined Pluronic F127 Hydrogel Promote Chronic Diabetic Wound Healing and Complete Skin Regeneration. Int J Nanomedicine. 2020;15:5911–5926. doi: 10.2147/IJN.S249129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wang M, Wang C, Chen M, Xi Y, Cheng W, Mao C, Xu T, Zhang X, Lin C, Gao W, Guo Y, Lei B. Efficient Angiogenesis-Based Diabetic Wound Healing/Skin Reconstruction through Bioactive Antibacterial Adhesive Ultraviolet Shielding Nanodressing with Exosome Release. ACS Nano. 2019;13:10279–10293. doi: 10.1021/acsnano.9b03656. [DOI] [PubMed] [Google Scholar]
- 78.Li B, Luan S, Chen J, Zhou Y, Wang T, Li Z, Fu Y, Zhai A, Bi C. The MSC-Derived Exosomal lncRNA H19 Promotes Wound Healing in Diabetic Foot Ulcers by Upregulating PTEN via MicroRNA-152-3p. Mol Ther Nucleic Acids. 2020;19:814–826. doi: 10.1016/j.omtn.2019.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]