Abstract
Background
Unconditional cash transfers (UCTs) are a common social protection intervention that increases income, a key social determinant of health, in disaster contexts in low‐ and middle‐income countries (LMICs).
Objectives
To assess the effects of UCTs in improving health services use, health outcomes, social determinants of health, health care expenditure, and local markets and infrastructure in LMICs. We also compared the relative effectiveness of UCTs delivered in‐hand with in‐kind transfers, conditional cash transfers, and UCTs paid through other mechanisms.
Search methods
We searched 17 academic databases, including the Cochrane Public Health Group Specialised Register, the Cochrane Database of Systematic Reviews (The Cochrane Library 2014, Issue 7), MEDLINE, and EMBASE between May and July 2014 for any records published up until 4 May 2014. We also searched grey literature databases, organisational websites, reference lists of included records, and academic journals, as well as seeking expert advice.
Selection criteria
We included randomised and quasi‐randomised controlled trials (RCTs), as well as cohort, interrupted time series, and controlled before‐and‐after studies (CBAs) on UCTs in LMICs. Primary outcomes were the use of health services and health outcomes.
Data collection and analysis
Two authors independently screened all potentially relevant records for inclusion criteria, extracted the data, and assessed the included studies' risk of bias. We requested missing information from the study authors.
Main results
Three studies (one cluster‐RCT and two CBAs) comprising a total of 13,885 participants (9640 children and 4245 adults) as well as 1200 households in two LMICs (Nicaragua and Niger) met the inclusion criteria. They examined five UCTs between USD 145 and USD 250 (or more, depending on household characteristics) that were provided by governmental, non‐governmental or research organisations during experiments or pilot programmes in response to droughts. Two studies examined the effectiveness of UCTs, and one study examined the relative effectiveness of in‐hand UCTs compared with in‐kind transfers and UCTs paid via mobile phone. Due to the methodologic limitations of the retrieved records, which carried a high risk of bias and very serious indirectness, we considered the body of evidence to be of very low overall quality and thus very uncertain across all outcomes.
Depending on the specific health services use and health outcomes examined, the included studies either reported no evidence that UCTs had impacted the outcome, or they reported that UCTs improved the outcome. No single outcome was reported by more than one study. There was a very small increase in the proportion of children who received vitamin or iron supplements (mean difference (MD) 0.10 standard deviations (SDs), 95% confidence interval (CI) 0.06 to 0.14) and on the child's home environment, as well as clinically meaningful, very large reductions in the chance of child death (hazard ratio (HR) 0.26, 95% CI 0.10 to 0.66) and the incidence of severe acute malnutrition (HR 0.44, 95% CI 0.24 to 0.80). There was also a moderate reduction in the number of days children spent sick in bed (MD − 0.36 SDs, 95% CI − 0.62 to − 0.10). There was no evidence for any effect on the proportion of children receiving deworming drugs, height for age among children, adults' level of depression, or the quality of parenting behaviour. No adverse effects were identified. The included comparisons did not examine several important outcomes, including food security and equity impacts.
With regard to the relative effectiveness of UCTs compared with a food transfer providing a relatively high total caloric value, there was no evidence that a UCT had any effect on the chance of child death (HR 2.27, 95% CI 0.69 to 7.44) or severe acute malnutrition (HR 1.15, 95% CI 0.67 to 1.99). A UCT paid in‐hand led to a clinically meaningful, moderate increase in the household dietary diversity score, compared with the same UCT paid via mobile phone (difference‐in‐differences estimator 0.43 scores, 95% CI 0.06 to 0.80), but there was no evidence for an effect on social determinants of health, health service expenditure, or local markets and infrastructure.
Authors' conclusions
Additional high‐quality evidence (especially RCTs of humanitarian disaster contexts other than droughts) is required to reach clear conclusions regarding the effectiveness and relative effectiveness of UCTs for improving health services use and health outcomes in humanitarian disasters in LMICs.
Plain language summary
Unconditional cash transfers in disasters: effect on use of health services and health outcomes in low‐ and middle‐income countries
Unconditional cash transfers (UCTs) for humanitarian assistance during disasters may improve health in low‐ and middle‐income countries (LMICs) by giving recipients additional income.
This review sought to assess the effect of UCTs on health services use, health outcomes, social determinants of health, health care expenditure, and local markets and infrastructure in LMICs. We also assessed the effects of UCTs paid in‐hand compared with grants of other goods (e.g., food) and types of cash transfers.
We sought expert advice, looked for different study types that investigated how UCTs affected the use of health services or health outcomes, and searched academic databases, organisational websites, bibliographies of included studies, and academic journals.
We included three studies on a total of 13,885 participants (9640 children and 4245 adults) and 1200 households in Nicaragua and Niger. They examined five programmes by governmental, non‐governmental or research organisations that gave recipients cash handouts worth USD 145 to USD 250 (or more, depending on household characteristics) as part of a disaster response (in these cases, to droughts). The studies had some serious methodological limitations, so we considered the evidence to be of very low quality and very uncertain.
UCTs appeared to contribute to a very small increase in the proportion of children who received vitamin or iron supplements and a beneficial effect on children's home environment. They may have resulted in a very large reduction in the chance of dying, a moderate reduction in the number of days spent sick in bed, and a large reduction in children's risk of acute malnutrition. UCTs had no clear effect on the proportion of children who received deworming drugs, children's height for age, adults' level of depression, or the quality of parenting behaviour. No adverse effects were identified.The included studies did not examine several important outcomes, including food security and equity impacts.
Compared with grants of food, there was no evidence that a UCT influenced the chance of child death or severe acute malnutrition. Compared with the same UCT paid via mobile phone, a UCT paid in‐hand led to a moderate increase in household dietary diversity, but there was no evidence for any effect on social determinants of health, health service expenditure, or local markets and infrastructure.
Additional research is required to reach clear conclusions regarding the effectiveness and relative effectiveness of UCTs in improving health services use and health outcomes in humanitarian disasters in LMICs.
Summary of findings
Background
Description of the condition
This review synthesises available evidence on the effect of one‐time or short duration unconditional cash transfers (UCTs) for assistance in humanitarian disasters on health services utilisation and health outcomes in low‐ and middle‐income countries (LMICs). The review was conducted in tandem with a forthcoming systematic review on the second broad type of UCTs, regular and ongoing UCTs for reducing poverty and vulnerabilities, on the same health outcomes in the same country setting (Pega 2014a).
Humanitarian assistance is defined as short‐term, material or logistical assistance provided for humanitarian purposes (saving lives, alleviating suffering, and maintaining dignity) just before, during or immediately after a natural or man‐made disaster, or as a means to shore up resilience and preparedness for future disasters (GHA 2014). Lack of financial resources is a key barrier that prevents people affected by disasters from accessing goods and services essential to maintaining health and well‐being (Bornemesiza 2010). UCTs for humanitarian assistance provide their recipients with additional, rapidly available income, to enable them to better manage the negative consequences of disasters, including on health.
From an economics perspective, disasters can reduce the supply, increase the demand, or disrupt the supply chain for certain goods and services required for restoring or maintaining good health, including food and health services. The result may be reduced access or quality of the goods and services for the population. Therefore, the specific economic environment in which a UCT is provided can profoundly influence the effect of the UCT on the use of health services and health outcomes.
Natural disasters
Natural disasters include climate‐related events such as extreme heat events, floods, droughts, storms and wildfires, as well as geophysical events such as earthquakes, tsunamis and volcanoes. Every year from 2001 to 2011, approximately 107,000 people died and 268 million people were affected by a natural disaster (Guha‐Sapir 2013). Over the same period, natural disasters cost economies about USD 143 billion annually (Guha‐Sapir 2013). LMICs and especially disadvantaged populations within these countries are disproportionately affected by (climatic) natural disasters because of their relative lack of protective infrastructure and resources (Stocker 2013).
The Intergovernmental Panel on Climate Change predicts that the frequency and intensity of climate‐related disasters will only increase (Stocker 2013). Indeed, three times as many natural disasters were observed from 2000 to 2009 compared to the period from 1980 to 1989, with an estimated 80% of this increase due to global climate change (Leaning 2013). Moreover, the impact of natural disasters has intensified as climate‐related events have become more extreme, with higher temperatures, higher precipitation, and more intense storms, combined with a loss of coping capabilities due to deforestation, environmental degradation, and urbanisation (Leaning 2013).
Natural disasters have a profound effect on health, including direct, immediate mortality and morbidity, as well as communicable disease outbreaks in their aftermath (Leaning 2013; McMichael 2006). Natural disasters can also displace the affected population internally and profoundly affect the environmental and social determinants of health, impairing agricultural, livestock, and fishery production and disrupting health service provision and livelihoods (e.g., loss of food security, proper shelter, and income) (Leaning 2013; McMichael 2006).
Man‐made disasters
Man‐made disasters encompass industrial accidents, man‐made environmental emergencies, and armed conflict, including civil and interstate war. These disasters have both immediate and delayed health effects, with direct consequences on immediate mortality and morbidity (e.g., from combat in an armed conflict) (Leaning 2013) as well as disruptions on health service provision and livelihoods (e.g., through loss of food security, proper shelter, and income). Indeed, the latter often have a greater impact on mortality and morbidity than the disaster itself (Leaning 2013; Spiegel 2010). Man‐made disasters have also been found to increase the unequal distribution of environmental and social determinants of health and undermine health equity (Bornemesiza 2010; Leaning 2013).
Armed conflict in particular leads to forced displacement, with increasing numbers of people fleeing internally to informal urban settings, rather than seeking international refuge in dedicated camps, which may be overcrowded and under‐serviced (Bornemesiza 2010; Spiegel 2010). Although communicable diseases (e.g., cholera and measles) associated with these camps are still the largest cause of mortality in low‐income countries experiencing armed conflicts (Spiegel 2010), the changing patterns of displacement have contributed to reducing the burden (Spiegel 2010). However, there are other indirect, negative effects for those that flee to informal urban settings, and these may be more difficult to address due to the unclear organisational responsibilities in terms of both mandate and funding. Moreover, these populations are particularly hard to reach and service (Leaning 2013; Spiegel 2010). As a result, mortality and morbidity rates among internally displaced populations are disproportionately high compared with both people who are not displaced and international refugees (Bornemesiza 2010; Leaning 2013). In medium‐income countries, where armed conflicts increasingly occur, non‐communicable diseases gain importance, reflecting the relatively older age of the affected population (Spiegel 2010). All in all, an estimated 300 million people live in an insecure or violent environment globally (Guha‐Sapir 2010).
Description of the intervention
Social protection
According to the United Nations Research Institute for Social Development, social protection means “protecting individuals and households during periods when they cannot engage in gainful employment or obtain enough income to secure their livelihoods—due to unemployment, sickness, chronic ill health or disability, old age or care responsibilities” (UNRISD 2010). LMICs are increasingly developing a social protection floor to foster human development, including increasing community resilience (Barrientos 2008; UNCEB 2009). Social protection comprises social assistance, labour market and social insurance interventions (Arnold 2011). Social assistance interventions aim to ensure an adequate standard of living through “noncontributory transfer programs targeted in some manner to the poor and those vulnerable to poverty and shocks” (World Bank 2011a). Social assistance interventions can be further differentiated into cash transfers, in‐kind transfers, fee waivers, subsidies, and public works programmes.
Global health leaders and the World Health Organization (WHO) have argued that some social protection interventions, including cash transfers, are policy tools for addressing the social determinants of health (such as income before, during or after a disaster) to improve individual and population health and health equity in LMICs (CSDH 2008; Marmot 2012; WHO 2008; WHO 2011). According to the WHO Commission on Social Determinants of Health, “governments, where necessary with help from donors and civil society organisations, and where appropriate in collaboration with employers, [should] build universal social protection systems and increase their generosity towards a level that is sufficient for healthy living” (CSDH 2008). Similarly, the World Bank has also argued that “social protection programmes … are a powerful tool to reduce poverty and vulnerability … [and] can have a direct, positive effect on poor families by building human capital through better health, more schooling, and greater skills” (World Bank 2014a). However, some experts contend that empirical evidence relating to the effect of social protection in the context of (man‐made) disasters on the use of health services and health outcomes is limited and of low quality (Carpenter 2012). And, again, the economic context of a social protection intervention (i.e., the access and quality of health‐relevant goods and services that the intervention provides) may determine its effect on the use of health services and health outcomes.
Cash transfers
Cash transfers are defined as cash payments that are provided by formal institutions (governmental, international, or non‐governmental organisations) to selected recipients, generally to enable them to meet their minimum consumption needs (Garcia 2012). Cash transfers are sometimes used as a one‐time or short duration disaster response because they are easier to distribute than in‐kind commodities and hence more rapid in reaching the target population (Harvey 2011). While their intended impacts are often targeted towards short‐term objectives (e.g., relief from a disaster), they may have long‐term health and well‐being effects by preventing disaster‐related health shocks (e.g., psychological trauma or stress) that may develop into a chronic condition (e.g., clinical depression) (Harvey 2011). Furthermore, from an economics perspective, markets for goods and services usually require steady demand to continue to function, so cash transfers can help keep underlying economic and institutional supply structures intact, which may have positive spin‐off effects on health. Further economic rationale for cash transfers is provided elsewhere (Arnold 2011; Fiszbein 2009).
Although cash transfers are diverse in terms of their objectives, designs, and implementations, two broad types can be distinguished. The first type (and the focus of this review) are one‐time or short duration cash transfers provided to smooth consumption before, during or after disasters as a form of humanitarian assistance (Arnold 2011; Garcia 2012; GHA 2014). The second type (and the focus of our forthcoming review (Pega 2014a)) are regular and ongoing cash transfers for reducing poverty and vulnerabilities (Arnold 2011; Garcia 2012). In terms of geographic spread, Garcia 2012 have argued that disaster‐related UCTs are more frequently used in low‐income countries, whereas poverty‐reduction transfers are more common in middle‐income countries, at least in Sub‐Saharan Africa.
Health experts have argued the case for using cash transfers to tackle key social determinants of health (especially income) to improve health and health equity in LMICs (CSDH 2008; Forde 2012). Furthermore, in line with the finding that income presents a key health determinant for people affected by disasters (Bornemesiza 2010), cash transfer interventions have been promoted as tools for preventing negative effects (including on health) of disasters (Harvey 2011). However, the effectiveness of cash transfers as a disaster response in improving health and its (equitable) distribution is not well established.
Unconditional cash transfers for humanitarian assistance
Cash transfers for humanitarian assistance can be differentiated by their degree of conditionality. While UCTs do not have any conditions attached to them, with the exception of broadly defined eligibility categories (i.e., only a defined subpopulation such as victims of a disaster are eligible) (Garcia 2012), conditional cash transfers (CCTs) require recipients to fulfil specific prescribed criteria (sometimes also called co‐responsibilities), such as using a specific health service or attending an educational institution (Garcia 2012). CCTs can further be typified into CCTs with 'hard' conditions (where non‐compliance with conditions results in penalties) and CCTs with 'soft' conditions (where non‐compliance does not result in penalties) (Garcia 2012). There are also what Baird 2013 have called 'fuzzy' cash transfers, which do not neatly fit into the classic UCT or CCT classification. For example, some transfers may be designed to be unconditional, but they are administered by organisations (e.g., the ministry of health) that create de facto conditions (e.g., enrolment for the cash transfer is linked to enrolment into a vaccination programme). On the contrary, some transfers may have a conditional design but no monitoring or enforcement mechanisms, resulting in unconditional transfers on a practical level. The focus of this review are cash transfers for humanitarian assistance that are distributed—by design or in practice—on unconditional terms.
As with cash transfers in general, UCTs for humanitarian assistance are used to pursue diverse objectives. One objective can be to prevent malnutrition among targeted individuals or groups by reducing food insecurity. Another common goal is to facilitate access to fee‐based health and social services, common in LMICs, and research has confirmed that at least part of the additional income from UCTs is consistently spent on health services (Devereux 2005; Harvey 2006). Another objective of UCTs that has emerged relatively recently is to manage disasters related to climate change (Pega 2015). UCTs can be used to support, protect, and rebuild livelihoods after a disaster has occurred. For example, they may prevent recipients from engaging in unfavourable coping strategies such as the selling of productive assets and investments (e.g., livestock or land) that may reduce future earning potential. Some UCTs facilitate the return or resettlement of internally displaced people or international refugees by covering their transportation costs and asset purchases. From an economic perspective, if supply chains have remained sufficiently intact, UCTs may stimulate and contribute to maintaining local markets in disaster situations by maintaining demand for goods and services (e.g., food and health services) which may keep the supply of these goods and services commercially viable for the providers.
There are several alternatives to UCTs, each with its own advantages and disadvantages. The most popular alternative are in‐kind transfers of goods and services, most commonly in the form of direct food aid. In‐kind transfers may have several potential advantages over UCTs. Unlike UCTs, they do not require a functioning market to satisfy demand, and they are unlikely to drive up inflation, which could decrease the relative purchasing power of non‐recipients, generating (health) inequalities. Moreover, whereas goods received from in‐kind transfers are likely to be consumed, receivers of UCTs might be forced to repay debts instead of promptly increasing (health promoting) consumption. In‐kind transfers may also have a more beneficial effect on health than UCTs if the quality of a good provided in‐kind exceeds that of the good available for purchase. For example, direct food aid may be more nutritionally beneficial than a UCT payment if the food aid is fortified with required minerals or vitamins, and the food available in the local market is not. Finally, providing an in‐kind transfer during a disaster response may require less preparation or knowledge of the local circumstances than establishing effective administrative systems for UCTs, so they may be more feasible and time‐efficient, potentially leading to a faster receipt of goods and services by the target population.
On the other hand, UCTs have other advantages. First, they stimulate local production and sale of key goods and services, whereas direct transfers may make producing and selling them less attractive, thereby potentially curbing their future supply. Second, UCTs may provide relatively more utility to recipients than in‐kind transfers of goods with limited demand. For example, a recent study found that recipients of cash transfers equivalent in value to pre‐packaged, non‐food transfers (e.g., pots, plastic sheeting, blankets, and tools) spent very little on these items (Bailey 2007). A third advantage of UCTs over in‐kind transfers is that, under certain circumstances, such as extremely inaccessible geographic regions, UCTs are much more rapidly delivered because they do not require the production, transport or delivery of commodities. Fourth, the World Bank has observed UCTs to be less prone to loss from corruption than in‐kind transfers in the context of disasters (Heltberg 2007). Finally, UCTs are not at risk of spoilage. It remains unclear whether and under which conditions UCTs lead to better health outcomes or are more cost‐effective, or both, than in‐kind transfers of good and services.
Another potential alternative to UCTs are CCTs for humanitarian assistance. Some experts have hypothesised that UCTs may more effectively improve social outcomes (including health) than CCTs, at least in low‐income African countries (Schubert 2006), where UCTs for humanitarian assistance are relatively common (Garcia 2012). Unlike CCTs, UCTs do not require their recipients to adhere to prescribed conditions, potentially making them less stigmatising, more empowering, more individually and socially transformative, and therefore more beneficial to health (Popay 2008). While quality and access of health‐relevant services is important in terms of health effect for both UCTs and CCTs, conditioning a cash transfer on uptake of services that are low quality or inaccessible is unlikely to add health benefits. Similarly, building the administrative and monitoring frameworks for a CCT during a disaster is challenging and may be so time‐consuming that it undermines the objective of extending access to essential health services. UCTs may also be more cost‐effective in design for LMICs (Schubert 2006). CCTs may have additional direct, indirect, and opportunity costs for both administrators and recipients, including monitoring costs and costs associated with compliance to the attached conditions. However, CCTs may have a lower net cost if the savings from not paying all eligible people exceeds the additional administrative expenses (Baird 2010). The relative effectiveness (and cost‐effectiveness) of UCTs versus CCTs in improving the use of health services and health outcomes in LMICs—in general and in the case of a disaster—is currently also unknown (Baird 2010; Robertson 2012).
Data is also scarce on the relative effectiveness of different payment mechanisms for UCTs. For example, it is theoretically plausible that UCTs provided in‐hand differ from those paid into a bank account or via mobile phone in terms of their health impacts. This might be caused by different payment mechanisms resulting in differential transaction costs for the recipient in obtaining the cash transfer or different perceived or actual barriers to accessing the cash transfer. Recipients may also view different payment mechanisms of a UCT as encouraging different uses of the UCT. For example, payment into a bank account may be perceived as an expression of the disbursement agent's expectation that the UCT be used for long‐term savings, whereas in‐hand payment may be perceived as intended for more immediate consumption.
How the intervention might work
The main causal pathway through which UCTs for humanitarian assistance influence health is through providing additional income (all pathways operating through A in Figure 1 taken from Pega 2014b). A second, but likely weaker causal pathway is a direct pathway (arrow I).
1.
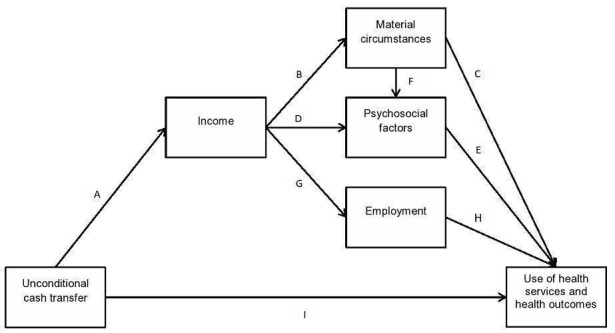
Conceptual framework of the causal relationship between an unconditional cash transfer and the use of health services and health outcomes (Pega 2014a)
Income pathway
There is a lack of specific empirical evidence on the effect of UCTs for humanitarian assistance on income in people affected by disasters. However, cash transfer interventions in LMICs have generally been shown to increase income over the short‐term (Arnold 2011; Barrientos 2006). Although the specific causal pathways between UCTs for humanitarian assistance and health have not previously been theorised, there are four hypothesised types of general causal effects between cash transfers and individual health: direct consumption effects (pathway A‐B‐C in Figure 1); direct status effects (pathway A‐D‐E); combined consumption and status effects (pathway A‐B‐F‐E); and employment effects (pathway A‐G‐H) (Borjas 2013; Lundberg 2010). We have provided a detailed description of these pathways elsewhere (Pega 2014a). In short, in direct consumption effects, income determines health through material conditions (e.g., the ability to purchase healthy food), and in turn, physical factors (e.g., the availability of healthy food in the household) (Lundberg 2010). Direct status effects influence psychosocial factors like relative income position or social status, which have an impact on health (Lundberg 2010). For their part, combined consumption and status effects operate through both physical and psychosocial mechanisms (Lundberg 2010). For example, recipients may spend income from UCTs on goods and services that facilitate their inclusion in a health‐promoting social group, which may improve their health. Finally, employment effects are at play when additional income from a UCT influences health through employment mechanisms (Borjas 2013). More specifically, labour economic theory predicts that additional income reduces recipients' number of working hours or motivates recipients to change to a lower‐paid occupation (Borjas 2013), which could impact health (Benach 2010a; Benach 2010b). In addition to taking recipients of UCTs as starting points for the income pathway, the uninterrupted or additional demand in the local market allows the continuation of an existing, commercially viable supply structure of goods and services, which may have health spin‐offs.
Direct pathway
Welfare security is defined as a sense of psychological security from the knowledge that a cash transfer (or cash transfers) provides a basic income in times of financial hardship (Pega 2012; Sjöberg 2010). By increasing welfare security, UCTs may have a direct and beneficial effect on health (Pega 2012; Sjöberg 2010), especially considering the considerable psychological stresses associated with disasters.
Why it is important to do this review
A scoping paper of the International Initiative for Impact Evaluation published in 2014 found that stakeholders viewed systematic review evidence on heath and cash transfer interventions as the top priority for systematic review evidence on humanitarian disasters (Clarke 2014). Researchers have also called for systematic review evidence on the effects of different types of cash transfers on social outcomes (including health) in LMICs (Arnold 2011). Systematic reviews on UCTs in LMICs are particularly important for two reasons. Firstly, UCT interventions are increasingly common responses to disasters, raising global interest in and stimulating research on the effects of these transfers. Secondly, UCTs may be relatively more effective and less costly than alternative interventions (e.g., in‐kind transfers and CCTs). To date, no previous systematic review has specifically examined the effect of UCTs for humanitarian assistance on the use of health services and health outcomes before, during or after a disaster, or as a way to build resilience for future disasters. Nor are we aware of any previous reviews on the relative effectiveness of UCTs compared to in‐kind transfers or CCTs as disaster responses, or the relative effectiveness of payment mechanisms of such UCTs.
Previous reviews have synthesised evidence on the effect of CCTs on the use of health services and health outcomes in LMICs (Gaarder 2010; Lagarde 2009) and of in‐work tax credits (CCTs provisional on uptake or retention of employment) on health status in adults (Pega 2013). However, these three reviews did not include UCTs. Eight reviews have compared the effects of various financial credit interventions, including UCTs, in terms of their impact on health. Boccia 2011 reviewed the effect of UCTs, CCTs, and micro‐finance interventions on risk factors for tuberculosis, while Bassani 2013 reviewed the effect of UCTs, CCTs, voucher programmes, and removal of user fees on the use of health services and health outcomes in children. Manley 2013 reviewed the effect of UCTs, CCTs, and public works programmes on nutrition, and Adato 2009, Heise 2013, and Pettifor 2012 conducted reviews of the effects of UCTs and CCTs on the incidence of HIV in LMICs. Finally, two non‐systematic reviews assessed the effect of UCTs and CCTs on the use of several health services and health outcomes (Arnold 2011; Sridhar 2006). UCTs, CCTs, and other financial interventions may differ in their effect on health in LMICs (Baird 2010; Robertson 2012); therefore, the evidence should be reviewed separately for each of these types of interventions. We are aware of one ongoing review of the effectiveness of cash‐based approaches in disasters (Doocy 2014), and our forthcoming review will focus on the effect of the second broad type of UCTs, as poverty‐reduction interventions in LMICs (Pega 2014a).
The present review is broadly comparable with this parallel work (Pega 2014a) as well as with the Lagarde 2009 review on CCTs. We provide systematic review evidence on the effectiveness of humanitarian UCTs aiming to improve health services use, health outcomes, social determinants of health, health service expenditure, and local markets and infrastructure in diaster contexts. We also synthesise evidence on the relative effectiveness of UCTs compared with in‐kind transfers, CCTs, and UCTs paid through different mechanisms. Therefore, this review aids governments, international organisations, non‐governmental organisations, and communities in identifying, planning, and implementing the most suitable and effective types of cash transfers for improving health‐related outcomes in the context of recent or ongoing disasters in LMICs.
Objectives
To assess the effects of UCTs in improving health services use, health outcomes, social determinants of health, health care expenditure, and local markets and infrastructure in LMICs. We also compared the relative effectiveness of UCTs delivered in‐hand with in‐kind transfers, conditional cash transfers, and UCTs paid through other mechanisms.
Methods
Criteria for considering studies for this review
Types of studies
The review protocol published prior to this review guided our work (Pega 2014b). We included randomised controlled trials (RCTs) and quasi‐RCTs, as well as controlled before‐and‐after studies (CBAs), interrupted time‐series studies, and cohort studies. We only included CBAs that fulfilled the following minimum criteria: two or more sites per intervention group, contemporaneous collection of data from the intervention and control group, and comparable intervention and control sites (as per EPOC 2012 recommendations). We included (but did not find any) interrupted time‐series studies that had three or more time points before and after the intervention along with a clearly defined intervention point (as per Cochrane PHG 2011 recommendations). Finally, we included (but did not find any) cohort studies that fulfilled the following criteria: three or more repeated measurements and controls for either confounding or reverse causation (as per our previous and forthcoming reviews; Pega 2013 and Pega 2014a). All other study types, including qualitative studies, were excluded.
Types of participants
Children (0 to 17 years) and adults (over 17 years) residing in a country defined by the World Bank as low‐ or middle‐income (World Bank 2014b).
Types of interventions
This review included UCTs for assistance in humanitarian disasters, defined as:
a cash payment provided in‐hand, into a bank account, via mobile phone or on a value card;
unconditional (i.e., eligibility for a cash transfer may be restricted to certain groups, but its receipt has neither soft nor hard conditions attached);
non‐contributory (i.e., the cash transfer is not paid through a social insurance system to which recipients previously contributed);
provided by a formal institution or as part of a scientific study;
provided for humanitarian assistance (i.e., UCTs for reducing poverty and vulnerabilities are excluded from this review);
granted to individuals or households (not communities); and
provided as a one‐time lump sum or short duration (within a period of months) payment just before, during or immediately after a disaster, or as a means to strengthen preparedness for a future disaster (i.e., not a regular and ongoing cash transfer).
We included both UCTs paid exclusively to women and those paid to both sexes. We also included studies on both stand‐alone UCTs and UCTs provided in combination with or alongside another intervention). For each UCT plus co‐intervention we documented the co‐intervention in the 'Characteristics of included studies' table. We excluded UCTs paid via vouchers because they generally limit the goods and services that can be purchased with them, whereas the included payment mechanisms do not.
The review included fuzzy (Baird 2013) UCTs, which we define as any cash transfer that was unconditional in practice. For example, if the conditions that were initially attached to a cash transfer were not monitored or enforced, then we included it. On the other hand, if a cash transfer was designed to be unconditional, but its implementation could have produced de facto or perceived conditions (e.g., major administrative linking of the cash transfer or major messaging around the cash transfer), then it was excluded. For the fuzzy UCTs included, we describe the specific intervention context that 'deactivated' the attached conditions, such as a lack of monitoring or enforcement, in the 'Characteristics of included studies' table.
UCTs for humanitarian assistance differ from UCTs for reducing poverty and vulnerability (Pega 2014a) in terms of intervention objectives (humanitarian assistance versus poverty or vulnerability reduction); frequency and duration of provision (payment at one point in time or over a short duration versus regular payments over an extended time period); and context (presence or absence of an emergency situation). These differences are substantial enough to potentially change effects on health. Consequently, UCTs for reducing poverty and vulnerability are excluded here and covered in a second systematic review (Pega 2014a).
To assess the effectiveness of UCTs for humanitarian assistance, different types of comparators were included in the review. The first was a control group receiving either no UCT or the co‐intervention (e.g., in‐kind transfer) only, because these comparators could in principle isolate the effectiveness of UCT‐only interventions or of a UCT plus co‐intervention, respectively. Potential limitations for applicability of including as comparators control groups who received a co‐intervention only are discussed in the section 'Overall completeness and applicability of evidence'. We excluded comparisons where UCTs combined with co‐interventions were compared with a control group who received anything other than the co‐intervention alone, as such comparisons did not enable us to robustly isolate the effectiveness of the UCT, since any observed effects could be due to the cash transfer, the co‐intervention, or the interaction between the cash transfer and the co‐intervention. The second type of comparator for assessing the effectiveness of UCTs was a control group receiving a UCT with a significantly lower value. Only one included study compared UCTs with different values. To assess the relative effectiveness of UCTs compared with CCTs, control groups who received a CCT only were included as comparators. We excluded control groups receiving more than one kind of co‐intervention (e.g., in‐kind transfers and CCTs) because again such comparators would not have enabled us to robustly isolate the relative effectiveness of the UCTs.
Finally, to assess the relative effectiveness of different payment mechanisms, we also included as a comparator control groups who received the same UCT paid through different mechanisms. For example, we included pair‐wise comparisons of a UCT paid in‐hand and the same UCT paid into a bank account, via mobile phone, or on a value card.
Types of outcome measures
To guarantee the comparability of systematic review evidence across relevant reviews, this review used the same types of outcomes as the Lagarde 2009 review and our forthcoming review on UCTs for reducing poverty and vulnerabilities (Pega 2014a). We only included studies that reported primary outcomes at the individual or household level. If a study reported several outcomes, then we included one measure for each outcome in the review. If a study reported multiple measures for the same outcome, then we prioritised the measure most consistent with the measure reported in the other included studies.
We included studies reporting effects over any time period. If a study provided treatment effect estimates for two or more time periods (e.g., after a three‐month intervention period, after a six‐month intervention period, and three months after a five‐month intervention period), then we prioritised the time‐point with the largest follow‐up period during the intervention (i.e., in the example, after a six‐month intervention period). However, to assess whether intervention effects persisted after the intervention had stopped, we also briefly report post‐intervention effects in the section 'Effects of interventions' (e.g., in the example, the effect three months after a five‐month long intervention period).
Primary outcomes
Use of health services
We included objective measures (e.g., from administrative records or surveys) and subjective measures (e.g., ratings by clinicians, patients, or caregivers) of the final use of any health facilities or services. This included, for example, the proportion of participants who used preventive health services facilities or who received vaccinations. We excluded measures of the distance travelled and travel time required to access the facility or service.
Health outcomes
We included objective and subjective measures of any health outcomes. This included mortality, anthropometric measures, food security, mental health, child cognitive development, and nutrition. We extracted and reported on any negative health and non‐health outcomes documented in the included studies.
Secondary outcomes
Social determinants of health
We included all relevant social determinants of health. These included asset ownership, income, education, employment, and social cohesion.
Health service expenditure
We included direct and indirect costs of health services borne by the recipient and excluded all other health service costs.
Local markets and infrastructure
We included all relevant measures of local markets and infrastructure, such as agricultural productivity, entrepreneurship, and spending of the cash transfers at local markets.
Search methods for identification of studies
Electronic searches
Academic databases
We searched the following databases for relevant records.
Cochrane Public Health Group Specialised Register.
Cochrane Central Register of Controlled Trial (CENTRAL) (The Cochrane Library, 2014, issue 7).
Ovid MEDLINE with Daily Update (1946 to May 2014).
EMBASE (1947 to May 2014).
Academic Search Premier (1990 to May 2014).
Business Source Complete (1990 to May 2014).
CINAHL (1937 to May 2014).
EconLit (1969 to May 2014).
3IE database (1990 to June 2014).
PsycINFO (1920 to May 2014).
PubMed (1920 to June 2014).
Scopus (1995 to July 2014).
Social Sciences Citation Index (1955 to May 2014).
Sociological Abstracts (1952 to May 2014).
The Campbell Library: The Campbell Collaboration (The Campbell Library, 2014, issue 10).
TRoPHI (1920 to June 2014).
WHOLIS (1948 to June 2014).
We used the strategy presented in Appendix 1 to search Ovid MEDLINE and the modified versions of this search strategy presented in Appendix 2 to search other electronic databases for records written in any year and any language. When we were near to finalising the review, we searched the PubMed database for the most recent publications (from January 2015 to June 2015), such as electronic publications ahead of print.
Grey literature databases
We searched the following grey literature databases.
ProQuest Dissertations and Theses Database.
System for Information on Grey Literature in Europe ‐ Open‐Grey (www.opengrey.eu).
The Directory of Open Access Repositories ‐ OpenDOAR (www.opendoar.org).
EconPapers (www.econpapers.repec.org).
Social Science Research Network ‐ SSRN eLibrary (www.ssrn.com).
National Bureau of Economic Research (www.nber.org).
Internet search engines
We screened the first 30 hits on Google Scholar, Scirus, and ReliefWeb.
Targeted internet searching of key organisational websites
We searched the websites of eight key international, governmental, and non‐governmental organisations.
African Development Bank (www.afdb.org).
Asian Development Bank (www.adb.org).
European Bank for Reconstruction and Development (www.ebrd.com).
Inter‐American Development Bank (www.iadb.org).
World Bank (www.worldbank.org).
United Kingdom Department for International Development (www.gov.uk/government/organisations/department‐for‐international‐development).
Cash Transfer Projects in Humanitarian Aid (www.sdc‐cashprojects.ch).
Save the Children (www.savethechildren.org.uk).
We did not conduct a targeted search of the WHO website because we searched WHOLIS, which comprehensively indexes publications from this organisation.
Searching other resources
Previous reviews, academic journals, and reference lists of included records
We handsearched for eligible studies and records:
the eight previous reviews on the effect of cash transfers (potentially including unconditional ones) on health service use and health outcomes (Adato 2009; Arnold 2011; Bassani 2013; Boccia 2011; Heise 2013; Manley 2013; Pettifor 2012; Sridhar 2006);
all issues published in the previous year (October 2013 to September 2014) in the three journals with the highest number of included studies; and
the reference lists of all included records.
Advisory group and other experts
The review advisory group, who guided the development of our protocol (Pega 2014b), were also convened to consult on this review. When we identified comparisons of an intervention group receiving a UCT with a control group receiving a smaller UCT, we contacted an advisory group member by email and asked the member to judge whether the difference in income from the UCTs that were compared was 'significant' in size. Once we had completed the search and screening phases, we sent the advisory group members a list of included studies and asked them to identify any additional, potentially eligible studies and records, regardless of publication status or degree of completion. We also asked other experts on cash transfers and their effect on the use of health services and health outcomes to identify additional, potentially eligible studies and records.
Data collection and analysis
Selection of studies
A reference librarian searched the electronic academic databases. One author (either FP, SYL, or SW) conducted the other searches. Duplicate articles were eliminated. The end product of these searches was a list of the titles and abstracts (if available) of all unique records identified in the various searches.
One of three authors (FP, SYL, or SW) first screened the titles of all records for potentially relevant records, and two or more authors (out of FP, SYL, SW) then independently screened the abstracts of the identified records for the inclusion criteria. We eliminated records deemed irrelevant based on the title and abstract, and then screened the full text of records without an abstract or identified as potentially relevant. When potentially relevant records had been written in languages other than those spoken by the authors (Dutch, German, English, French, Italian, and Spanish), we had them translated into English.
One author retrieved the records selected for full‐text screening (FP or SW). Two authors then independently applied the criteria outlined above to establish inclusion or exclusion of the record in the review (out of FP, SYL, SW, or SKL). A third author resolved any disagreements between the two authors (FP or SW). We documented the reason for the exclusion of studies that had undergone full‐text screening in the 'Characteristics of excluded studies' table. The results of each stage of study selection were described in a PRISMA flowchart.
Data extraction and management
Two contributors independently extracted data for each included study, using the Cochrane Public Health Group's data extraction form (Cochrane PHG 2011), expanded for the complex intervention perspective we adopt in this review and including the Cochrane & Campbell Methods Group Equity Checklist (CCEMG 2011). To ensure standardised data extraction, the data extractors received specialised training and then piloted the form before commencing extraction tasks. A review author (FP) checked all data extraction sheets and resolved discrepancies between the forms, and a second author independently double‐checked the extracted data (either SYL, SW, or SKL).
We extracted data in the following categories: study eligibility (e.g., type of study, participant, and intervention); funding sources; intervention design (including, for fuzzy UCTs, the contexts such as lack of monitoring or enforcement, which created the unconditionality in practice); context (including co‐interventions); implementation; cost and sustainability; intervention groups; sociodemographic characteristics of participants along the PROGRESS framework at baseline and at the endpoint; outcomes; measured potential confounders and method of confounder control; comparator; and results. We also collected relevant information on the comparator intervention, including its design, context, implementation, cost, and sustainability. If a study record did not provide information on these criteria in the record, but referred to other records or sources for this information, we extracted the information from these other records or sources whenever feasible. We described the context, implementation, cost, and sustainability of the intervention in the 'Characteristics of included studies' table. We did not extract qualitative data, which were excluded from the review. We entered, stored, and managed extracted data in the Review Manager software (RevMan).
Assessment of risk of bias in included studies
We conducted risk of bias assessments at the outcome level (for each outcome and for each study) and at the study level. Two authors independently assessed the risk of bias in the included outcomes and studies, and a third resolved disagreements. To guide our risk assessment, we applied the Cochrane 'Risk of bias' tool for the included cluster‐RCT (Higgins 2011a). To assess the risk of bias in the included CBAs, we used the Cochrane Effective Practice and Organisation of Care's 'Risk of Bias' criteria (EPOC 2012).
Measures of treatment effect
The included studies reported treatment effects of UCTs for humanitarian assistance on dichotomous or ordinal health outcomes, either as relative measures (i.e., hazard ratios (HRs) for the Langendorf 2013 study) or as absolute measures (mean differences (MDs) for the Aker 2011 and Macours 2008 studies, as well as difference‐in‐differences estimators (DDs) in Aker 2011).
In some cases, the Langendorf 2013 study calculated HRs as the relative effect of the group we considered as our control (i.e. the effect of the co‐interventions only relative to the UCTs plus co‐intervention). For these comparisons, we calculated the reciprocal of each HR (i.e. 1/HR) and its 95% confidence interval limits, so that the reciprocal HRs estimated the treatment effect of the intervention, compared with the comparator. For meta‐analyses, we calculated the log[HR] and its standard error, using the methods (Tierney 2007) recommended by The Cochrane Collaboration (Higgins 2011b). These log[HR] and their standard errors were the treatment effect measures entered in RevMan. This was not required for the comparisons of UCTs only with the co‐interventions only, as the HRs were calculated as we required.
The MDs in the Aker 2011 study were simple differences in means between the intervention and comparator group for outcomes, for which only post‐intervention measures were available. These MDs were calculated by subtracting the post‐intervention mean in the comparator group from the post‐intervention mean in the intervention group. The DDs in the Aker 2011 study were reported for outcomes for which both pre‐ and post‐intervention measures were available. DDs were calculated by subtracting the difference in the outcome between the mean measured pre‐intervention and the mean measured post‐intervention among the comparator group (i.e., the underlying time trend in the outcome variable) from the difference in the outcome between pre‐intervention and post‐intervention means among the intervention group (i.e., the treatment effect plus the underlying time trend in the outcome variable). Thus, whereas the simple MDs from this study are not adjusted for potential differential trends between intervention and control groups in the outcome over time, DDs provide treatment effect estimates adjusted for potential underlying time trends.
The MDs reported in the Macours 2008 study were MDs of outcomes that had been standardised by subtracting the sample mean and dividing by the standard deviation (SD) of the control group. For example, an MD of 0.05 indicated an increase in the mean in the intervention group by 0.05 SDs of the control group, compared with the control group. Because the absolute measures (the MDs) could not be converted into relative measures, we reported these in the review. Since the SDs used to standardise the MDs were unclear, we were unable to convert the MDs into natural units.
Like the included studies themselves, we also reported effects on continuous outcomes as MDs between intervention and control groups. We prioritised treatment effect measures from intention‐to‐treat analyses (rather than, for example, the average treatment effect in the treated analyses) that were adjusted for the largest set of potential confounders (rather than unadjusted). Treatment effect measures were presented with their 95% confidence intervals.
Unit of analysis issues
Unit of analysis issues can occur due to randomising clusters of participants rather than individuals, implementing two or more interventions on the same participants, and collecting several measures for an outcome over time. We screened all studies for unit of analysis issues but did not identify any, as all studies had adjusted treatment effects for clustering. We did not combine pair‐wise comparisons that shared the same participants in meta‐analyses (e.g., we did not combine comparisons of Group A and Group B with another comparison that included Groups A or B).
Dealing with missing data
We requested missing data from the principal study authors via email. Specifically, we requested missing information on the type of study and type of population for Langendorf 2013, and we requested missing mean values at baseline for the treatment and control groups, along with missing treatment effect estimates for all relevant outcomes for the included comparison for Macours 2008. We received the requested missing data for the Macours 2008 study. However, we did not receive the requested data for the Langendorf 2013 study. Therefore, we only presented the available data for this study and described any potential effects of these missing data on the findings of the review in the 'Discussion' section.
Assessment of heterogeneity
We were unable to perform meta‐analyses for the outcomes because no two included studies were sufficiently comparable across population, intervention, comparator and outcome (PICO) elements. However, as recommended by The Cochrane Collaboration, for RCTs with two or more eligible pair‐wise comparisons (Higgins 2011e), we combined two pair‐wise comparisons from one study that were comparable across PICO elements in meta‐analyses. The statistical heterogeneity in these meta‐analyses was estimated with the I2 statistic, which we calculated using RevMan. We did not meta‐analyse comparisons with a heterogeneity of 75% or more (Higgins 2011b).
Assessment of reporting biases
To judge the presence (or not) of publication bias, if the review included at least 10 studies of the same outcome, we planned to produced a funnel plot and test for funnel plot asymmetry. We planned to follow Cochrane Collaboration guidelines in selecting the appropriate statistical test for funnel plot asymmetry (Higgins 2011c). However, since the review included less than 10 studies of the same outcome, we did not carry out these tasks.
Data synthesis
As explained above, we did not perform meta‐analyses of the included studies in this review, instead reporting results separately for each outcome, without putting emphasis on any one study, and synthesising all findings narratively. However, as noted above, in line with The Cochrane Collaboration's recommendation (Higgins 2011e), we meta‐analysed two heterogeneous comparisons, both from Langendorf 2013, applying a random‐effects model to address statistical heterogeneity, making no adjustments to treatment effect measures, and using RevMan. For each of the comparisons that we combined in a meta‐analysis, we entered the log[hazard ratio] and its standard error in RevMan.
We assessed the quality of the evidence for each outcome. Following Cochrane Public Health Group guidelines (Cochrane PHG 2011), we applied to the randomised and non‐randomised evidence the GRADE Working Group criteria (Balshem 2011), which assesses quality of evidence on the basis of study design, risk of bias, inconsistency, indirectness, imprecision, presence of publication bias and (for non‐randomized studies only)presence of large effects, plausibility that confounding could change the effect, and presence of a dose response gradient. We provided a GRADE rating (high, moderate, low, or very low) for the quality of each primary outcome in the review and justified the rating with reference to the GRADE criteria.
For each of the two primary outcomes domains (that is, the use of health services and health outcomes), we reported the prioritised treatment effect measure or measures from the narrative analysis in the 'Summary of findings' tables (Higgins 2011d). We presented a summary table for two comparisons: UCT compared with no UCT (or co‐intervention only), and UCT compared with in‐kind transfer. At a minimum, these tables presented the treatment effect measure or measures, the total number of studies and participants that each measure was based on, and the GRADE Working Group grades (Balshem 2011) for the overall quality of the body of evidence on each outcome. We did not present a summary table for one comparison with evidence included in the review (that is, UCT compared with the same UCT paid through a different mechanism), because we judged the outcome measured and the applicability of the comparison insufficient to make an additional table helpful.
Subgroup analysis and investigation of heterogeneity
The small number of included studies, in most cases only one study per subgroup of interest (i.e., age, disaster type, gender, and WHO region), prohibited meaningful subgroup analyses in this review.
Sensitivity analysis
We planned to conduct sensitivity analyses to determine the robustness of the treatment effect measures produced in meta‐analyses. We planned to conduct sensitivity analyses of each meta‐analysis by re‐running each meta‐analysis with only high‐quality studies with low risk of bias. In the case of meta‐analyses of parallel and cross‐over randomised trials, we planned to re‐run the meta‐analysis with only parallel trials included. Considering that some studies suggest that even small amounts of income from (conditional) cash transfers have a large effect (at least on educational outcomes) (Baird 2011; Filmer 2011), we planned to also determine whether studies with different comparators (i.e., no UCT and a UCT with a 'significantly smaller' amount) provide consistent results. However, since we neither meta‐analysed two or more studies, nor found studies that used a 'significantly smaller' amount of the UCT as the comparator, none of the planned sensitivity analyses were feasible. Consequently, we did not conduct any sensitivity analyses.
Results
Description of studies
Results of the search
Figure 2 presents a PRISMA flowchart of the study selection, including a detailed breakdown of the search results by individual database and other searched sources, respectively. Our search of the 17 electronic academic databases identified a total of 26,802 records. After removal of duplicates, a total of 16,288 records remained. After title screening, 379 records were considered potentially eligible for study inclusion, and after detailed abstract screening, 80 records of 77 studies were still considered potentially eligible. After full‐text screening of these records, three records of two studies, that is the Langendorf 2013 and Macours 2008 studies, were found to fulfil the inclusion criteria and, hence, these studies were included in the review. We became aware of an additional (third) record from the Langendorf 2013 study published in an academic journal during the course of the review.
2.
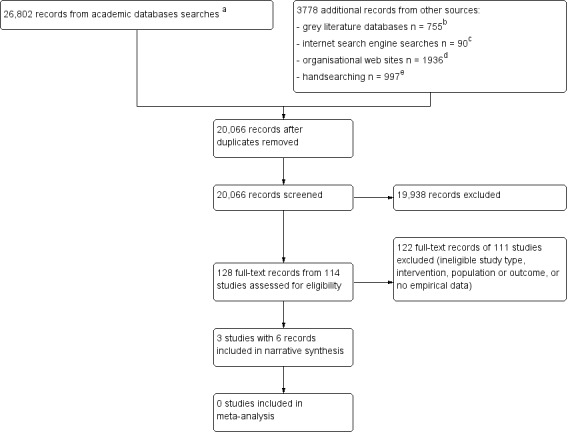
Flowchart of study selection.
Footnotes: aCochrane Public Health Group Specialised Register, n = 37; Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library, 2014, issue 7), n = 105; Ovid MEDLINE 1946 to May 2014 with Daily Update, n = 4950; EMBASE, n = 5210; Academic Search Premier, n = 2002; Business Source Complete, n = 1592; CINAHL, n = 527; EconLit ,n = 1329; 3IE database, n = 5; PsycINFO, n = 962; PubMed, n = 4626; Scopus, n = 692; Social Science Citation Index, n = 2569; Sociological Abstracts, n = 1852; The Campbell Library: The Campbell Collaboration (The Campbell Library, 2014, issue 10), n = 318; TRoPHI, n = 20; and WHOLIS, n =6. bProQuest Dissertations & Theses Database, n = 48; Open‐Grey, n = 317; OpenDOAR, n = 100; EconPapers, n = 100; Social Science Research Newtork eLibrary, n = 90; and National Bureau of Economic Research, n = 100. cGoogleScholar, n = 30; Scirus, n = 30; and ReliefWeb, n = 30. dAfrican Development Bank, n = 643; Asian Development Bank, n = 173; European Bank for Reconstruction and Development, n = 88; Inter‐American Development Bank, n = 184; World Bank, n = 437; United Kingdom Department for International Development, n = 411; Cash Transfer Projects in Humanitarian Aid, n = 29; and Save the Children, n = 34. eTwo hundred ninety‐four records published in the three academic journals with an included record, 151 records referenced in included records identified through handsearching, and 552 records of the eight relevant previous reviews of cash transfers.
Our searches of other sources retrieved a total of 3778 additional unique records. Searches of the six electronic grey literature databases generated 755 records, searches of the two Internet search engines identified 90 records, and searches of the eight websites of key international, governmental, and non‐governmental organisations resulted in 1936 records. After title and abstract screening, 48 records of 47 studies were considered potentially eligible and underwent full‐text screening. One additional record of the Macours 2008 study and one record of an additional study (Aker 2011) met the inclusion criteria for the review. We also identified two ongoing studies (REFANI‐P; REFANI‐N).
We found no additional eligible records from handsearching the 151 references of the 6 records of the three included studies, nor in the 294 records published over the previous 12 months (from October 2013 to September 2014) in the three academic journals with records of an included study (Annals of Nutrition and Metabolism, PLoS Medicine, andAmerican Economic Journal: Applied Economics). Neither did we identify any additional records from the 552 references of the eight previous health‐focused reviews of cash transfers that may potentially have included UCTs (Adato 2009; Arnold 2011; Bassani 2013; Boccia 2011; Heise 2013; Manley 2013; Pettifor 2012; Sridhar 2006), nor from the review advisory group or other experts.
Included studies
Three studies, with a total of six records, 13,885 participants (9640 children and 4245 adults), and 1200 households fulfilled the inclusion criteria (Aker 2011; Langendorf 2013; Macours 2008). The study characteristics, including sources of funding, study type and methods, participants, interventions, comparisons, intervention context, and outcomes are summarised in the 'Characteristics of included studies' table.
Funding
Concern Worldwide, the European Commission, Hitachi Center, Irish Aid, and Tufts University funded the Aker 2011 study. Médecins Sans Frontiéres and the World Food Programme funded the Langendorf 2013 study, while the World Bank and the BASIS Assets and Market Access Collaborative Research Support Program financed the Macours 2008 study. In the Langendorf 2013 and Macours 2008 studies, the funding bodies contributed to the study design and the preparation of publications, suggesting potential conflicts of interest.
Study types and methods
Study types
Cluster‐randomised controlled trials
Macours 2008 was a cluster‐randomised controlled trial (C‐RCT). Intervention allocation occurred in four stages. First, 106 communities (clusters) in six rural municipalities in Nicaragua were enumerated. Second, 56 clusters were randomly allocated to intervention groups and 50 clusters to a pure control group. Third, each of the clusters allocated to intervention groups was randomly allocated to one of three interventions. Fourth, all households in intervention groups that were living in poverty received their respective intervention.
The three intervention groups received:
UCT only (number of clusters and participants unclear);
UCT plus vocational scholarship (number of clusters and participants unclear); or
UCT plus a lump sum payment that was partially conditional on non‐agricultural entrepreneurship (number of clusters and participants unclear).
This study provided evidence on the effectiveness of UCTs compared with no UCTs, and this was the only pair‐wise comparison from the study that we included in our review. We excluded all other comparisons because they studied the effect of UCTs provided alongside major, complex co‐interventions and were therefore less able to isolate the effect of the UCT component.
Controlled before‐and‐after studies
The other two included studies were CBAs. Both of these studies randomly allocated some clusters to some interventions, as would be done in a C‐RCT. However, they also non‐randomly allocated some clusters to other interventions, and therefore we classified them as CBAs.
In the Aker 2011 study, interventions were allocated in three stages. First, 116 food deficit villages (clusters) in six communes in the Tahoua region in Niger were enumerated. Food deficit villages were defined as villages that were officially classified as producing less than 50% of their consumption needs in the 2009 harvest. Second, 20 clusters were non‐randomly allocated to one intervention group (to avoid interfering with existing programmes), and 96 clusters were randomly allocated to one of three intervention groups. Third, in the intervention groups the respective intervention was provided to poor households with one or more children aged four or under.
The study had three intervention groups and no control group.
UCT provided in‐hand (32 clusters, number of participants unclear).
UCT paid in‐hand, with recipients also receiving a mobile phone (32 clusters, number of participants unclear).
UCT paid via mobile phone, with recipients receiving a mobile phone (52 clusters, number of participants unclear).
This study provided evidence on the relative effectiveness of different payment mechanisms (that is, payment in‐hand compared with payment via mobile phone). We included one pair‐wise comparison from this study: the UCT paid in‐hand plus mobile phone with the UCT paid via mobile phone plus mobile phone (items 2 and 3 from the above list). All other comparisons were excluded.
In the Langendorf 2013 study, interventions were also allocated in three stages. First, 48 rural villages or hamlets (clusters) located within 15 km of a health centre in the Madarounfa health district in Niger were enumerated. Second, the clusters were allocated to seven intervention groups (four non‐randomly and three randomly), with no control group.
UCT only (7 clusters, 680 participants), unclear allocation method.
UCT plus food transfer* 1 (6 clusters, 766 participants), unclear allocation method.
UCT plus food transfer 2 (5 clusters, 657 participants), unclear allocation method.
UCT plus food transfer 4 (11 clusters, 1089 participants), non‐random allocation method.
food transfer 1 (5 clusters, 951 participants), unclear allocation method.
food transfer 2 (6 clusters, 733 participants), unclear allocation method.
food transfer 3 (8 clusters, 680 participants), unclear allocation method.
*Food transfers 1, 2, and 3 were relevant for this review, because they were either provided as a co‐intervention alongside an included UCT intervention or were a comparator group. Food transfer 1 had the relatively lowest total caloric value, providing a nutritional supplement of 500 kcal/day (92 g of Supplementary Plumpy per day). Food transfer 2 provided a nutritional supplement of 820 kcal/day (i.e., 200 g/day of Super Cereal Plus), and food transfer 3 had the highest caloric value, providing a nutritional supplement of 820 kcal/day (i.e., 200 g/day of Super Cereal Plus), as well as a monthly family food ration (i.e., 50 kg cereals, 7.5 kg pulses, and 2.5 kg oil). Food transfer 4, which provided 250 kcal/day (46 g/day of Plumpy’Doz), was excluded from this review, because it was not part of an eligible comparison.
Finally, the third stage of allocation consisted of providing the interventions to mothers or primary caregivers in households with at least one child measuring > 60.0 cm and ≤ 80.0 cm in length.
This study provided evidence on the effectiveness of UCTs and on the relative effectiveness of UCTs compared with in‐kind transfers. To assess the effectiveness of UCTs, we included the two pair‐wise comparisons that compared a UCTs plus co‐intervention with the co‐intervention only. The first of these comparison was the UCT plus food transfer 1 intervention group compared with the food transfer 1 intervention group (interventions 2 and 5 in the above list). The second comparison was the UCT plus food transfer 2 intervention group compared with the food transfer 2 comparison group (interventions 3 and 6). To assess the relative effectiveness of UCTs compared with in‐kind transfers, we included the three pair‐wise comparisons of the UCT only intervention group compared with the food transfers 1, 2, and 3 intervention groups.
No other pair‐wise comparisons fulfilled the inclusion criteria, including three pair‐wise comparisons of a UCT valued at USD 59 (i.e., the UCT only intervention) with UCTs valued at USD 52 (i.e., the UCT plus food transfer interventions). A review advisory group member determined that the less generous UCT was not 'significantly smaller' than the more generous UCT.
Study methods
All three of the included studies conducted intention‐to‐treat analyses, using allocation to the UCT or eligibility for the UCT as the intervention or exposure. Analytical methods included difference‐in‐differences models (Aker 2011), survival analytic models (i.e., Cox proportional hazards modelling with propensity scores; Langendorf 2013), and regression analytic models (Macours 2008).
Treatment effects were estimated with either relative measures (HRs in the Langendorf 2013) or absolute measures (MDs and DDs in the Aker 2011 study and MDs in the Macours 2008 study). All three studies adjusted treatment effect estimates for potential baseline differences in outcome measurements and characteristics (see 'Risk of bias in included studies'). Subgroup analyses were conducted in one study (Aker 2011) for one secondary outcome (the proportion of participants who used their UCT to pay for health services) along one PROGRESS category (ethnicity) for two subgroups (Fulani or Touareg, and Hausa, respectively).
Two studies assessed the effectiveness of UCTs by comparing a UCT with no UCT (or with the co‐intervention only). The Macours 2008 study compared the UCT‐only intervention group with the pure control group, and Langendorf 2013 compared two intervention groups receiving the UCTs plus co‐intervention (i.e., food transfers 1 and 2, respectively) with the intervention groups who received the co‐interventions only.
No study provided evidence on the relative effectiveness of UCTs compared with CCTs. Langendorf 2013 examined the effectiveness of UCTs relative to in‐kind transfers, comparing the UCT‐only intervention group with the intervention groups who received different levels of food transfers. In addition, Aker 2011 provided evidence on the relative effectiveness of different payment mechanisms by comparing a UCT paid in‐hand with the same UCT paid via mobile phone.
Participants
Overall, the three included studies comprised a total of 13,885 participants as well as about 1200 households. The included participants were 9640 children aged 0 to 15 years and 4245 adults (the children's mothers) aged over 17 years. The Aker 2011 study interviewed 1200 poor households with one or more children aged 0 to 4 years who resided in a food deficit village twice in 2010 in six communes in the Tahoua region in Niger. The Langendorf 2013 study assessed 5395 children aged 6 to 23 months and measuring between 60.0 cm and 80.0 cm in length, and living in poor households within 15km of a health centre in the rural Madarounfa health district, in the Maradi region in Niger, on five occasions in 2011. The Macours 2008 study evaluated 4245 children aged 0 to 15 years, as well as 4245 adults (the children's mothers) three times between 2005 and 2009, in six rural municipalities in Nicaragua.
Interventions
Overall, the three included studies investigated a total of five UCTs eligible for inclusion in this review. Table 3 presents a more detailed description of these interventions.
1. Comparisons of interventions in included studies.
| Comparison | Intervention | Comparator | Study | ||||||
| Type | Name | ||||||||
| Name | UCT | Co‐intervention | Type | Description | |||||
| Type | Description | Type | Description | ||||||
| UCT compared with no UCT (or co‐intervention only) | Comparison 1 | Intervention 1 | UCT only | Between USD 145 and USD 235 plus USD 25 per child paid in‐handa | — | — | No UCT | — | Macours 2008 |
| Comparison 2b | Intervention 2 | UCT plus co‐intervention | USD 59 paid in‐hand | In‐kind transfer | Food transfer 1c | Co‐intervention | Food transfer 1c | Langendorf 2013 | |
| Intervention 3 | UCT plus co‐intervention | USD 59 paid in‐hand | In‐kind transfer | Food transfer 2d | Co‐intervention | Food transfer 2d | Langendorf 2013 | ||
| UCT compared with in‐kind transfer | Comparison 3 | Intervention 4 | UCT only | USD 52 paid in‐hand | — | — | In‐kind transfer | Food transfer 1c | Langendorf 2013 |
| Comparison 4 | In‐kind transfer | Food transfer 2d | Langendorf 2013 | ||||||
| Comparison 5 | In‐kind transfer | Food transfer 3e | Langendorf 2013 | ||||||
| UCT compared with sameUCT paid through different mechanism | Comparison 6 | Intervention 5 | UCT plus co‐intervention | USD 45 paid in‐hand | In‐kind transfer | Mobile phone | Same UCT paid through different mechanism | Intervention 5 paid via mobile phone | Aker 2011 |
aUSD 145 for families without children or with children aged 0 to 6 years, and USD 235 plus USD 25 per child paid in‐hand for families with children aged 7 to 15 years and enrolled in primary school, respectively. bComparison 2 combined two individual comparisons in meta‐analysis. cNutritional supplement of 500 kcal/day through 92 g/day of Supplementary Plumpy. dNutritional supplement of 820 kcal/day through 200 g/day of Super Cereal Plus. eNutritional supplement of 820 kcal/day through 200 g/day of Super Cereal Plus plus monthly family food ration of 50 kg cereals, 7.5 kg pulses, and 2.5 kg oil.
Intervention 1
Macours 2008 implemented UCTs with a total value of USD 145 (approximately USD 24 every 2 months for 12 months) for families without children or with children aged 6 and under, and USD 235 plus USD 25 per child for families with children aged 7 to 15 years and enrolled in primary school (about USD 43 every 2 months for 12 months for a family with one eligible child). In terms of intervention design, the intervention aimed to reduce the impact of shocks on human and physical capital investments after a drought (World Bank 2011b); it was targeted to children in poor households in rural areas, and it was paid in‐hand to mothers. The intervention had a fuzzy design (Baird 2013): it was conditional on regular preventive health check‐ups for children aged up to 6 years old, but these conditions were neither monitored nor enforced with penalties. However, for households with children aged 7 to 15 years, there were conditions related to children's school enrolment and regular attendance, and these conditions were monitored, with penalties for non‐compliance. In addition, there was messaging to all recipients that transfers were intended to improve the diversity and nutrient content of children’s diets and to buy school material. However, we judged this messaging to be too minor to create de facto conditions.
Intervention 2
The Langendorf 2013 study's UCT plus food transfer 1 had a total value of USD 208 (USD 52 per month for four months). All interventions in Langendorf 2013 study used the same design and aimed to prevent acute malnutrition among children aged between 6 and 23 months after droughts. They were targeted to children measuring > 60.0 cm and ≤ 80.0 cm in length and paid in‐hand to the children's mothers, who received educational material that aimed to ensure nutritional value and dietary diversity of the food that parents purchased for their children.
Intervention 3
The Langendorf 2013 study's UCT plus food transfer 2 had a total value of USD 208 (USD 52 per month for four months).
Intervention 4
The Langendorf 2013 study's UCT only had a total value of USD 236 (USD 59 per month for four months).
Intervention 5
The Aker 2011 study's UCT of USD 225 (USD 45 per month for five months) was paid in‐hand, and recipients also received a mobile phone. The intervention aimed to reduce malnutrition and prevent asset depletion in households during and after droughts. It was targeted to poor households with at least one child aged zero to four years, and it was paid to either parent.
Pair‐wise comparisons
The effects of these five interventions on the use of health services, health outcomes or both were examined in a total of six pair‐wise comparisons. Of the included comparisons, two compared a UCT with no UCT (or the co‐intervention only), three a UCT with an in‐kind transfer, and one a UCT with the same UCT paid through a different mechanism. Again, Table 3 presents a more detailed description of the included comparisons.
Comparison 1
The Macours 2008 study's intervention 1, compared with a pure control group who received no UCT.
Comparison 2
This comparison was a meta‐analysis of two individual pair‐wise comparisons from the Langendorf 2013 study. Here, we combined interventions 2 and 3 compared with their co‐interventions only, that is food transfers 1 and 2, respectively.
Comparison 3
The Langendorf 2013 study's intervention 4 (UCT only) compared with an in‐kind transfer, that is food transfer 1.
Comparison 4
The Langendorf 2013 study's intervention 4 compared with an in‐kind transfer, that is food transfer 2.
Comparison 5
The Langendorf 2013 study's intervention 4 compared with an in‐kind transfer, that is food transfer 3.
Comparison 6
The Aker 2011 study's intervention 5 compared with the same UCT paid via mobile phone.
Intervention context
The included UCTs were provided by governmental, non‐governmental or research organisations in experiments or pilot programmes. Two studies examined UCT experiments conducted by a non‐governmental organisation (Concern Worldwide in the Aker 2011 study) and a research organisation (Epicentre in the Langendorf 2013 study). On the other hand, Macours 2008 examined UCTs that were part of a pilot programme of the Nicaraguan government called Atención a Crisis. While this review intended to find evidence on the effect of UCTs in the context of natural and man‐made humanitarian disasters in general, the setting for all included interventions was the same type of natural disaster: droughts.
Intervention uptake was not reported in the Aker 2011 and Langendorf 2013 studies, but it was high in the Macours 2008 study, with over 95% of eligible participants receiving the UCT. In the Langendorf 2013 study, participants did not receive the same number of cash transfer payments across intervention and comparator groups, partially because enrolment was continuous over the study period. On average, 69% of the participants received four or five of the total of five payments, but this percentage ranged from 62% to 74% across intervention groups. Likewise, an average of 95% of participants were present at all their payment meetings, but this percentage ranged from 93% to 99% across intervention groups. Total programme costs for the UCTs were not reported in either of the studies.
Outcomes
Primary outcomes
Overall, the review included a total of 10 primary outcomes. Two related to health services use, comprising the domains of preventive health services and receipt of treatment for an existing condition. The other eight were health outcomes from the domains of mortality, anthropometric measures, disease prevalence, mental health, child development, and nutrition. Nine of these outcomes were measured at the individual level (eight among children and one among adults), and one was measured at the household level.
Use of health services
Two health services use outcomes among children were examined in the Macours 2008 study. The first outcome was the use of preventive health services, and it was measured by the proportion of children who received a vitamin or iron supplement in the previous six months. The second outcome, receipt of treatment for an existing condition, was measured using the proportion of participants who received deworming drugs in the previous six months. These were subjective measures derived from participants' self reports. Both outcomes were followed up 8 to 9 months after the intervention had begun to assess immediate effectiveness, as well as 8 to 29 months after the 12‐month intervention had ceased, to assess whether effects persisted.
Health outcomes
The chance of child death was examined by the Langendorf 2013 study. This outcome was measured objectively by medically trained study personnel through verbal autopsy conducted with household members, followed up after five months. One anthropometric measure, height for age, was examined among children in the Macours 2008 study, and the measure was followed up at 8 to 9 months and 8 to 29 months after the intervention of 12 months. It was unclear whether this outcome was measured objectively or subjectively. Macours 2008 subjectively measured disease prevalence among children, through the participant‐reported number of days spent in bed sick, at 8 to 9 months and 8 to 29 months after the cessation of the intervention. Macours 2008 also examined mental health in adults, specifically the level of depression as measured using the Center for Epidemiological Studies Depression Scale (Eaton 2004), a subjective measure derived from participants' self reports, followed up at 8 to 9 months and 8 to 29 months after the start of the intervention.
Macours 2008 also tracked four subjective measures of child development outcomes, which were measured using standardised tests: language development, measured using the language subscale of the Denver Developmental Screening Test (DDST; Frankenberg 1996); memory development, measured using the short‐term memory subscale of the McCarthy Scales of Children's Abilities (McCarthy 1972); motor development, measured using the fine motor subscale of the DDST; and social development, measured using the social‐personal subscale of the DDST. Like the other outcomes assessed in Macours 2008, these were followed up at 8 to 9 months and 8 to 29 months after the 12‐month intervention.
Langendorf 2013 and Aker 2011 examined two nutritional outcomes among children and the household, respectively. Langendorf 2013 assessed the incidence of severe acute malnutrition at five months, based on measures of weight, length, mid‐upper arm circumference, and the presence of bipedal edema, as taken by two independent medically trained study personnel using standardised methods and measurement instruments, with disagreements resolved by a third assessor. Aker 2011 examined household dietary diversity using the Household Diet Diversity Score, a subjective measure derived from self reports by one household member, followed up three months after a five‐month long intervention.
Secondary outcomes
Overall, nine secondary outcomes were included in the review: three social determinants of health (children's home environment, quality of parenting, and asset ownership), one health service expenditure outcome, and five local market and infrastructure outcomes (investment in agricultural business, production of agricultural goods, sale of the goods, location of spending of cash transfer, and timing of the spending). Two outcomes were measured at the individual level (one each among children and adults) and seven at the household level.
Social determinants of health
The Aker 2011 and Macours 2008 studies examined the three social determinants of health outcomes among children, adults, and households. Macours 2008 assessed children's home environment by measuring the proportion of children who had a pen and paper in the home, and the quality of maternal parenting behaviour using the Home Observation for Measurement of the Environment (HOME) Scale. Both of these measures were subjective, participant‐reported, and followed up 8 to 9 months into the intervention and 8 to 29 months after it had ceased. Aker 2011 examined asset ownership in households by measuring the total number of asset categories owned, a subjective, participant‐reported measure, followed up three months after five months of the intervention.
Health service expenditure
Aker 2011 examined one household‐level health service expenditure: the proportion of households who used the cash transfer to pay for health services. This measure was also subjective and participant‐reported, followed up three months after five months of the intervention.
Local markets and infrastructure
The Aker 2011 study also examined five household outcomes related to local markets and infrastructure. The proportion of households who had cultivated land in the last growing season was the measure of investment in agricultural business, while production and sale of agricultural goods was examined through measures of the number of crop types grown and the proportion of participants who sold millet, respectively. Researchers also examined the location and timing of spending of the cash transfer, using the proportions of participants who spent the cash transfer at a kiosk in the village and those who spent the cash transfer all at once, respectively. All these outcomes were measured using subjective, participant‐reported measures, followed up three months after the intervention.
Excluded studies
A total of 122 records from 111 studies underwent full‐text screening but did not fulfil the inclusion criteria. The reasons for excluding the 30 studies closest to the inclusion criteria are presented in the 'Characteristics of excluded studies' table. We excluded 59 studies because they did not study an eligible UCT for assistance in humanitarian disasters. For example, Ahmed 2009 investigated the effects of a multi‐component intervention that included a UCT for residents of flood‐ and famine‐prone Bangladesh, but it could not isolate the effects of the cash transfer intervention, and the cash transfer was only a minor component within the broader intervention under study. Similarly, we excluded the Pellerano 2014 study because it could not isolate the effect of a UCT for assistance in humanitarian disasters called the Emergency Food Grant from a poverty‐reduction UCT called the Child Grant Programme that was provided alongside it. We also excluded studies that examined UCTs for reducing poverty or vulnerabilities, which will be covered in a parallel review (Pega 2014a). We excluded 17 studies for not examining one or more primary health outcomes, 4 studies for not examining populations in LMICs, 22 studies for using an ineligible study type, 2 studies for using an ineligible comparator, and 7 studies for not reporting any empirical data.
Ongoing studies
The characteristics of the two ongoing studies identified by the review are presented in detail in the 'Characteristics of ongoing studies' table.
Research on Food Assistance for Nutritional Impact ‐ Niger 2014 study
The Research on Food Assistance for Nutritional Impact ‐ Niger 2014, or REFANI‐N, is a C‐RCT that will interview 7500 participants from 2000 households in the Affala and Takanamatt communes (clusters) of the Tahoua district in Niger twice over a seven‐month period (March to September 2015) of expected food insecurity resulting from unspecified natural disasters.
The C‐RCT will have two intervention groups and no control group.
UCT only (number of clusters and participants unclear).
Earlier and extended (by two months) UCT only (number of clusters and participants unclear).
Although the C‐RCT will not include a control group, the wider REFANI‐N study will also randomly sample non‐recipient households, who may be used as a comparison group.
The UCT interventions will provide an unclear amount (expected to cover about 75% of a household's total energy needs) per month for either four months (standard UCT only intervention group) or six months (earlier and extended UCT only intervention group), respectively. Co‐interventions will provide nutritional supplements, as well as health, hygiene, and nutrition education messages to both intervention groups.
Primary outcomes will be the use of health services outcomes and health outcomes in the domains of anthropometric measures and nutrition. Secondary outcomes will be social determinants of health in the domain of asset ownership.
Research on Food Assistance for Nutritional Impact ‐ Pakistan 2015 study
The Research on Food Assistance for Nutritional Impact ‐ Pakistan 2015 study (REFANI‐P) is a C‐RCT that will interview 11,360 participants from 2580 poor or very poor households in 78 villages (clusters) of the Sindh Province in Pakistan three times over a 12‐month period beginning in April 2015, when food insecurity is expected to occur due to natural disasters, especially floods.
The study will have three intervention groups and one control group.
Smaller UCT only (number of clusters and participants unclear).
Larger UCT only (number of clusters and participants unclear).
Food voucher (number of clusters and participants unclear).
Control group (number of clusters and participants unclear).
The UCT interventions will provide USD 87.00 (about USD 14.50 per month for six months) and USD 174.00 (about USD 29.00 per month for six months), respectively.The ACF Women and Children/Infant Improved Nutrition in Sindh (EU‐WINS) programme will be provided as a co‐intervention to all intervention groups and the control group (i.e., the control group will not be pure).
Primary outcomes will be health outcomes in the domains of anthropometric measures, disease prevalence, and nutrition.
Risk of bias in included studies
For each study, the risk of bias is described in detail in the 'Characteristics of included studies' table. All three included studies carried an overall high risk of selection bias. One study ensured random sequence generation, whereas two did not. Two studies did not conceal allocation, whereas allocation concealment was unclear in the third study. All studies had low risk of bias from differences in outcome measurements at baseline. The risk of bias from baseline differences in characteristics was high in one study, but unclear in the other two studies. All studies carried a high risk of bias from blinding. The risk of performance bias was high for all studies, and the risk of detection bias was low in two studies, but unclear in the third study. All three studies carried a high risk of contamination. Attrition bias was low in two studies and high in one study. All studies carried an unclear risk of reporting bias. Consequently, the risk of bias in this review was considered high overall (see 'Risk of bias' graph in Figure 3).
3.
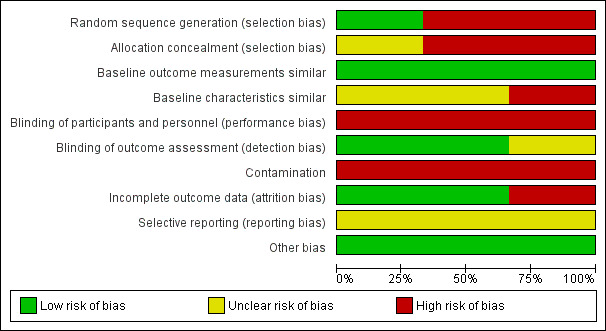
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
We analysed the risk of selection bias on the basis of the risks of bias from random sequence generation, allocation concealment, baseline differences in outcomes measurements, and baseline differences in characteristics (EPOC 2012). Regarding random sequence generation, the Macours 2008 C‐RCT ensured random sequence generation and thus carried low risk from this selection bias. In contrast, the two CBAs, the Aker 2011 and Langendorf 2013 studies, did not randomly allocate all clusters and participants to the intervention groups, so we judged them to carry a high risk of selection bias from lack of random sequence generation.
Regarding allocation concealment, neither the Langendorf 2013 study nor the Macours 2008 study concealed allocation of clusters and participants to intervention or control groups, so there was a high risk of this selection bias. The risk of selection bias from allocation concealment was unclear for the Aker 2011 study.
In terms of the similarity of baseline outcomes measurements, the Aker 2011 study reported no baseline differences (confidence level: P < 0.05) between the intervention and control groups in outcomes measurements. In contrast, both the Langendorf 2013 and the Macours 2008 studies reported such differences. In the Langendorf 2013 study, there were baseline differences between the intervention groups in two outcome measurements. The proportion of children with severe acute malnutrition ranged between 0.03 and 0.07 (P = 0.01). In the Macours 2008 study, baseline differences (P < 0.05) were reported between the intervention group and the control group in one outcome measurement. The proportion of children in the intervention groups who had received deworming drugs in the last six months was lower than the proportion in the control group (0.59 compared with 0.51, P = 0.04). However, all three studies comprehensively adjusted for any baseline differences in outcome measurements using regression analysis. In summary, we judged the risk of selection bias due to differences in outcome measurements at baseline to be low for all three studies.
In terms of the similarity of baseline characteristics, the Aker 2011 study reported differences (confidence level: P < 0.05) between the intervention group and the control group in one characteristic. The proportion of participants with some education in the intervention group was lower than that in the control group (0.07 compared with 0.15, P < 0.05). Langendorf 2013 reported baseline differences (P < 0.05) between the intervention groups in two characteristics. The proportion of children who were stunted ranged from 0.58 to 0.67 (P = 0.04), and the proportion of girls ranged from 0.46 to 0.56 (P = 0.00). Macours 2008 reported no baseline differences in characteristics. However, all three studies comprehensively adjusted any baseline differences in key measured characteristics using regression analytic methods. On the other hand, investigators could not assess baseline differences in some unmeasured characteristics, such as presence and magnitude of local natural disasters, man‐made disasters, epidemics, and economic shocks, despite considering their presence possible in the Aker 2011 and Macours 2008 studies. Such differences likely occurred in the Langendorf 2013 study, considering that, for example, the death rates observed across intervention groups were highly differential, ranging between 0.2% and 2.3%. None of the three studies adjusted for such potential or likely differences in characteristics. In summary, we deemed the risk of selection bias to be high for the Langendorf 2013 study and unclear for the other two studies. Overall, we thought each study carried an overall high risk of selection bias.
Blinding
We judged the risk of lack of blinding on the basis of risk of performance bias (i.e., blinding of participants and personnel), detection bias (i.e., blinding of outcome assessors), and contamination. Regarding risk of performance bias, it is not possible to blind participants to cash transfer interventions and difficult on a practical level to blind personnel to these interventions. Therefore, all studies were judged to have a high risk of performance bias.
Regarding the risk of detection bias, we considered that Aker 2011 carried an unclear risk due to lack of reporting, while the other two studies carried a low risk. While the Langendorf 2013 study did not blind outcome assessors, all its outcomes were measured objectively. The Macours 2008 study also did not blind outcome assessors, and its outcomes were subjective. Nevertheless, we judged the study's risk of detection bias as low because the statistical analysis was adjusted for the identity of the outcome assessors and the month of the outcome assessment, and the subjective measures were validated with objective measures from administrative data. In summary, however, all studies carried some risk of bias from lack of blinding.
Allocation was by cluster for all three included studies (i.e., community, village, or hamlet). However, additional income from the UCT provided to participants in the intervention groups may have been transferred to participants in the control group (e.g., between family members). Therefore, all three studies carried a high risk of contamination. Overall, we judged all three studies to carry an overall high risk of bias from blinding.
Incomplete outcome data
We judged the risk of attrition bias on the basis of the level of initial survey non‐response (or, in other words, missing participants in the baseline survey), the level of attrition over the study period, whether attrition was differential between the intervention group and control group (or between intervention groups), the reasons for missing data, and the potential impact of missing data on treatment effect estimates. The risk of attrition bias in two studies, that is the Aker 2011 and Macours 2008 studies, was judged to be low. The only noteworthy potential risk in these studies was that the initial survey non‐response and the numbers of missing participants per outcome were unclear. We considered the missing data unlikely to have impacted effect estimates because there was missing data for only a small percentage of participants in these two studies.
We considered the risk of attrition bias to be high in the Langendorf 2013 study. The study's initial survey non‐response rate was unclear. Although the level of attrition was moderate (7%), it differed by intervention group, ranging from 3% to 18%. The exact number of missing participants per outcome was unclear. Analyses of severe acute malnutrition excluded 230 participants (5.5% of all participants) with this condition at baseline. However, since the incidence of severe acute malnutrition was studied, the exclusion of participants with prevalent malnutrition was unlikely to have introduced attrition bias. We considered the missing data to potentially have impacted effect estimates, because a moderate percentage of participants missed data (7%) and the chance of the events occurring was low (mortality was 0.33 per 100 child‐months, and diagnosis of severe acute malnutrition was 1.56 per 100 child‐months). Overall, two studies had a low risk of attrition bias, and one study carried a high risk.
Selective reporting
Because no trial registrations or study protocols were available for any of the studies, we could not assess the risk of reporting bias with confidence, and we judged it to be unclear.
Other potential sources of bias
None identified.
Effects of interventions
for the main comparison.
| Unconditional cash transfer in humanitarian disasters compared with no unconditional cash transfer (or co‐intervention only) for improving use of health services and health outcomes | ||||||
|
Population: children and adults in low‐ and middle‐income countries Settings: drought Intervention: unconditional cash transfer Comparison: no unconditional cash transfer (or co‐intervention only) | ||||||
| Outcomes | Illustrative comparative risks (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk No unconditional cash transfer (or co‐intervention only) | Corresponding risk Unconditional cash transfer a | |||||
| Received vitamin or iron supplements Z‐score of proportion (follow‐up: 8 to 9 months) | The mean proportion of participants who received vitamin or iron supplements in the control group was 0.75 |
The mean proportion of participants who received vitamin or iron supplements in the intervention group was 0.10 SDs higher (0.06 to 0.14 higher) (very small effect) |
— | 3326 children (1 study) |
⊕⊝⊝⊝ very low |
Better indicated by higher values Quality of evidence downgraded due to risk of bias (minus one grade)b and very serious indirectness (minus two grades)c |
| Received deworming drugs Z‐score of proportion (follow‐up: 8 to 9 months) | The mean proportion of participants who received deworming drugs in the control group was 0.59 |
The mean proportion of participants who received deworming drugs in the intervention group was 0.04 SDs higher (0.01 lower to 0.09 higher) (small effect) |
— | 3326 children (1 study) |
⊕⊝⊝⊝ very low |
Better indicated by higher values Quality of evidence downgraded due to risk of bias (minus one grade)b, very serious indirectness (minus two grades)c and serious imprecision (minus one grade)d |
| Died Mortality rate per 10,000 child‐months (follow‐up: 4 months) | 57 per 10,000 |
15 per 10,000 (6 to 37) |
HR 0.26 (0.10 to 0.66) |
2885 children (1 study) |
⊕⊝⊝⊝ very low |
Better indicated by lower values Quality of evidence downgraded due to observational evidence (minus two grades), serious risk of bias (minus one grade)b and very serious indirectness (minus two grades)c |
| Height for age Z‐score of number (follow‐up: 8 to 9 months) | The mean height for age z‐score in the control group was − 1.08 |
The mean height for age z‐score in the intervention group was 0.06 SDs higher (0.01 lower to 0.13 higher) |
— | 3326 children (1 study) |
⊕⊝⊝⊝ very low |
Better indicated by higher values Quality of evidence downgraded due to risk of bias (minus one grade)b, very serious indirectness (minus two grades)c, and serious imprecision (minus one grade)e |
| Number of days sick in bed Z‐score of number (follow‐up: 8 to 9 months) | The mean number of days sick in bed in the control group was 0.62 |
The mean number of days sick in bed in the intervention group was 0.36 SDs lower (0.62 to 0.10 lower) (moderate effect) |
— | 3326 children (1 study) |
⊕⊝⊝⊝ very low |
Better indicated by lower values Quality of evidence downgraded due to risk of bias (minus one grade)b and very serious indirectness (minus two grades)c |
| Became severely acutely malnourished Incidence of first event per 1000 child months (follow‐up: 4 months) | 23 per 1000 |
10 per 1000 (6 to 19) |
HR 0.44 (0.24 to 0.80) |
2885 children (1 study) |
⊕⊝⊝⊝ very low |
Better indicated by lower values Quality of evidence downgraded due to observational evidence (minus two grades), serious risk of bias (minus one grade)b and very serious indirectness (minus two grades)c |
| Level of depression Z‐score of Center for Epidemiological Studies Depression score. Scale: from 0 to 80. (follow‐up: 8 to 9 months) | The mean level of depression score in the control group was 11.88 points (Center for Epidemiological Studies Depression score) |
The mean level of depression score in the intervention group was 0.48 SDs lower (1.84 lower to 0.88 higher) |
— | 3326 adults (1 study) |
⊕⊝⊝⊝ very low |
Better indicated by higher values Quality of evidence downgraded due to serious risk of bias (minus two grades)b, very serious indirectness (minus two grades)c and very serious imprecision (minus two grades)f |
| CI: confidence interval; HR: hazard ratio; MD: mean difference; SDs: standard deviations. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
aCalculated using the formulas provided in the GRADE handbook (Schünemann 2009). bAllocation not concealed, unblinded, and potential contamination. cThe only evidence found was conducted in a single type of humanitarian disaster setting (i.e., droughts) and among only one type of participants (i.e., either children or adults). dLower confidence limit indicates a potential non‐meaningful effect. eLower confidence limit indicates potentially no effect, whereas upper confidence limit indicates a potential small beneficial effect. fLower confidence limit indicates a potential large adverse effect, whereas upper confidence limit indicates a potential moderate beneficial effect.
2.
| Unconditional cash transfer compared with in‐kind transfer for improving use of health services and health outcomes | ||||||
|
Population: children and adults in low‐ and middle‐income countries Settings: droughts Intervention: unconditional cash transfer Comparison: in‐kind transfer | ||||||
| Outcomes | Illustrative comparative risks (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk In‐kindtransfer | Corresponding risk Unconditional cash transfer a | |||||
| Received vitamin or iron supplements | — | — | — | — | — | No evidence available on this outcome |
| Received deworming drugs | — | — | — | — | — | No evidence available on this outcome |
| Died Mortality rate per 10,000 child‐months (follow‐up: 4 months) | 26 per 10,000b |
58 per 10,000 (18 to 189) |
HR 2.27 (0.69 to 7.44)b, c |
3044 children (1 study) |
⊕⊝⊝⊝ very low |
Better indicated by lower values Quality of evidence downgraded due to observational evidence (minus two grades), serious risk of bias (minus one grade)d, very serious indirectness (minus two grades)e, and very serious imprecision (minus two grades)f |
| Height for age | — | — | — | — | — | No evidence available on this outcome |
| Number of days sick in bed | — | — | — | — | — | No evidence available on this outcome |
| Became severely acutely malnourished Incidence of first event per 1000 child months (follow‐up: 4 months) | 17 per 1000b |
20 per 1000 (11 to 34) |
HR 1.15 (0.67 to 1.99)b, g |
3044 children (1 study) |
⊕⊝⊝⊝ very low |
Better indicated by lower values Quality of evidence downgraded due to observational evidence (minus two grades), serious risk of bias (minus one grade)d, very serious indirectness (minus two grades)e, and very serious imprecision (minus two grades)f |
| Level of depression | — | — | — | — | — | No evidence available on this outcome |
| CI: confidence interval; HR: hazard ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
aCalculated using the formulas provided in the GRADE handbook (Schünemann 2009). bThese estimates are from comparison 5 of the unconditional cash transfer with the most generous in‐kind transfer (see Table 3 for description of comparison) (Langendorf 2013). cThe alternative treatment effect estimates from comparisons 3 and 4 (see Table 3 for description of comparisons) were HRs of 0.81 (95% CI 0.40 to 1.66) and 1.74 (95% CI 0.88 to 3.47), respectively (Langendorf 2013). dAllocation not concealed, unblinded, and potential contamination. eThe only evidence found was conducted in only one type of humanitarian disaster setting (i.e., droughts) and among only one type of participants (i.e., children). fLower confidence limits indicate potential beneficial effects, whereas upper confidence limits indicate potential adverse effects. gThe alternative treatment effect estimates from comparisons 3 and 4 (see Table 3 for description of comparisons) were HRs of 0.84 (95% CI 0.49 to 1.44) and 0.78 (95% CI 0.46 to 1.35), respectively (Langendorf 2013).
We now present the evidence on the effects of UCTs, first by comparing UCTs with no UCTs (or co‐intervention only), then comparing them with in‐kind transfers and with the same UCTs paid through a mechanism other than cash in‐hand. We did not identify any evidence on the relative effectiveness of UCTs compared with CCTs. For each outcome included in the three comparisons identified in this review, the evidence came from only one study, and according to GRADE criteria (Balshem 2011), it was of very low overall quality due to a combination of observational evidence, serious risk of bias, very serious indirectness, and serious or very serious imprecision (see section 'Quality of the evidence'). Consequently, we are very uncertain of the evidence.
Unconditional cash transfers compared with no unconditional cash transfers (or co‐intervention only)
Use of health services
Received vitamin or iron supplements, previous six months
Information on this outcome came from comparison 1 from the Macours 2008 study, covered more comprehensively in Table 3. Compared to a pure control group, the UCT moderately increased the proportion of children who received vitamin or iron supplements in the previous 6 months, followed up 8 to 9 months into the intervention (MD 0.10 SDs, 95% CI 0.06 to 0.14, Analysis 1.1). Judging the clinical meaningfulness and effect size of standard mean differences (SMDs) was not straightforward, as there are no internationally agreed standards on which level of change is clinically meaningful or even which can be considered 'small' or 'large' in size. Consequently, we could not judge the clinical meaningfulness of the change in this outcome. However, considering the high mean proportion in the control group at baseline (75%), we considered the treatment effect to be very small in size. However, this small, beneficial effect was still apparent 8 to 29 months after 12‐month intervention (MD 0.06 SDs, 95% CI 0.01 to 0.12, Analysis 1.1).
1.1. Analysis.
Comparison 1 Unconditional cash transfer compared with no unconditional cash transfer (or co‐intervention only), Outcome 1 Use of health service outcomes.
| Use of health service outcomes | ||||
|---|---|---|---|---|
| Study | Outcome | Mean in control group | Mean in intervention group | Number of participants |
| Macours 2008 |
Received vitamin or iron supplements, previous 6 months Z‐score of proportion (follow‐up: 8 to 9 months) |
75% |
0.10 SDs higher (0.06 to 0.14 higher) |
3326 children |
| Macours 2008 | (follow‐up: 8 to 29 months after 12 months of intervention) | — |
0.06 SDs higher (0.01 to 0.12 higher) |
4245 children |
| Macours 2008 |
Received deworming drugs, previous 6 months Z‐score of proportion (follow‐up: 8 to 9 months) |
59% |
0.04 SDs higher (0.01 lower to 0.09 higher) |
3326 children |
| Macours 2008 | (follow‐up: 8 to 29 months after 12 months of intervention) | — |
0.07 SDs higher (0.02 to 0.11 higher) |
4245 children |
Received deworming drugs, previous six months
Comparison 1 from the Macours 2008 study did not yield any evidence that the UCT intervention impacted the proportion of children who had received deworming drugs in the previous 6 months, when followed up after 8 to 9 months (MD 0.04 SDs, 95% CI − 0.01 to 0.09, Analysis 1.1). However, the UCT did increase this outcome after the intervention had ceased, that is 8 to 29 months after 12‐month intervention (MD 0.07 SDs, 95% CI 0.02 to 0.11, Analysis 1.1). We could not judge the clinical meaningfulness of this level of change in this outcome due to a lack of international standards. However, considering the high mean baseline proportion in the control group (59%), we considered this treatment effect to be small.
Health outcomes
Died, previous three months
In comparison 2 from the Langendorf 2013 study, when combined in meta‐analysis, the two UCTs reduced the chance of death among children in the previous three months, compared with their co‐intervention only and followed up after four months of the intervention (HR 0.26, 95% CI 0.10 to 0.66, Figure 4). In absolute terms, 15 children died per 10,000 child months among those receiving the UCT plus co‐intervention (95% CI 6 to 37), compared with 57 children per 10,000 child months among those receiving the co‐intervention only. The HR of 0.26 indicates that participants receiving the UCTs had a 74% reduced death rate, compared with participants receiving the co‐interventions only. Considering that Mayo‐Wilson 2011 have previously deemed a reduction in all‐cause mortality among children of 24% to be clinically meaningful, we judged the reduction from UCTs found in this review by 74% as clinically meaningful and very large in size.
4.
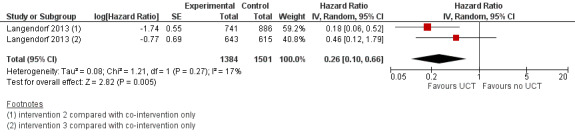
Forest plot of comparison: 1 Unconditional cash transfer compared with no unconditional cash transfer (or co‐intervention only), outcome: 1.2 Died, previous three months.
Height for age, current
Comparison 1 from the Macours 2008 study provided no evidence that the UCT had any effect on height for age among children, when compared with no UCT. No evidence for an effect was found at 8 to 9 months (MD 0.06 SDs, 95% CI − 0.01 to 0.13, Analysis 1.3), consistent with either no effect or a small beneficial effect. There was also no evidence for an intervention effect 8 to 29 months after the 12‐month intervention had ceased (MD 0.01 SDs, 95% CI − 0.06 to 0.09, Analysis 1.3).
1.3. Analysis.
Comparison 1 Unconditional cash transfer compared with no unconditional cash transfer (or co‐intervention only), Outcome 3 Anthropometric measures, disease prevalence, and level of depression.
| Anthropometric measures, disease prevalence, and level of depression | ||||
|---|---|---|---|---|
| Study | Outcome | Mean in control group | Mean in treatment group | Number of participants |
| Macours 2008 |
Height for age, current Z‐score of number (follow‐up: 8 to 9 months) |
−1.08 |
0.06 SDs higher (0.01 lower to 0.13 higher) |
1500 children |
| Macours 2008 | (follow‐up: 8 to 29 months after 12 months of the intervention) | — |
0.01 SDs higher (0.06 lower to 0.09 higher) |
1994 children |
| Macours 2008 |
Number of days sick in bed, previous month Z‐score of number (follow‐up: 8 to 9 months) |
unclear |
0.36 SDs lower (0.62 to 0.10 lower) |
3326 children |
| Macours 2008 | (follow‐up: 8 to 29 months after 12 months of the intervention) | — |
0.10 SDs lower (0.33 lower to 0.13 higher) |
4245 children |
| Macours 2008 |
Level of depression, current Z‐score of Center for Epidemiological Studies Depression score. Scale: from 0 to 80. (follow‐up: 8 to 9 months) |
11.88 |
0.48 SDs lower (1.84 lower to 0.88 higher) |
3326 adults |
| Macours 2008 | (follow‐up: 8 to 29 months after 12 months of the intervention) | — |
0.04 SDs lower (1.58 lower to 1.50 higher) |
4245 adults |
Number of days sick in bed, last month
The UCT in comparison 1 from the Macours 2008 study reduced the number of days that children were sick in bed in the previous month, compared with no UCT and followed up at 8 to 9 months of the intervention (MD − 0.36 SDs, 95% CI − 0.62 to − 0.10, Analysis 1.3). We could not judge the clinical meaningfulness of this level of change due to the lack of international standards. The mean proportion in the control group at baseline was also unclear, but we judged this treatment effect to probably be of moderate size. This comparison provided no evidence that the moderately beneficial effect persisted after the intervention had ceased, that is when followed up 8 to 29 months after the 12‐month intervention had ceased (MD − 0.10 SDs, 95% CI − 0.33 to 0.13, Analysis 1.3).
Level of depression, current
Comparison 1 from the Macours 2008 study provided no evidence that the UCT impacted the level of depression among adults, when when compared with receiving no UCT and followed up at 8 to 9 months (MD − 0.48 SDs, 95% CI − 1.84 to 0.88, Analysis 1.3), consistent with either a large adverse effect or a potential moderate beneficial effect. There was also no evidence for an effect 8 to 29 months after the 12‐month intervention had ceased (MD − 0.04 SDs, 95% CI − 1.58 to 1.50, Analysis 1.3).
Level of language development, current
In comparison 1 from the Macours 2008 study, the UCT increased the level of language development, compared with no UCT and when followed up after 8 to 9 months (MD 0.17 SDs, 95% CI 0.05 to 0.29, Analysis 1.4). We cannot judge its clinical meaningfulness due to the absence of international standards. The mean score in the control group at baseline was also unclear, but we judged this treatment effect to be of moderate size. This comparison provided no evidence that this moderate beneficial effect persisted after the intervention had ceased (MD 0.10 SDs, 95% CI − 0.01 to 0.21, Analysis 1.4).
1.4. Analysis.
Comparison 1 Unconditional cash transfer compared with no unconditional cash transfer (or co‐intervention only), Outcome 4 Level of child development, current.
| Level of child development, current | |||||
|---|---|---|---|---|---|
| Study | Outcome | Mean in control group | Mean in treatment group | Number of participants | Comments |
| Macours 2008 |
Level of language development, current Z‐score of Denver Developmental Screening Test (general language sub‐scale) score. Scale: unclear. (follow‐up: 8 to 9 months) |
unclear |
0.17 SDs higher (0.05 to 0.29 higher) |
1577 children | Better indicated by higher values |
| Macours 2008 | (follow‐up: 8 to 29 months after 12 months of the intervention) | — |
0.10 SDs higher (0.01 lower to 0.21 higher) |
1469 children | — |
| Macours 2008 |
Level of short‐term memory development, current Z‐score of McCarthy Scales of Children's Abilities score. Scale: unclear. (follow‐up: 8 to 9 months) |
unclear |
0.18 SDs higher (0.05 to 0.30 higher) |
885 children | Better indicated by higher values |
| Macours 2008 | (follow‐up: 8 to 29 months after 12 months of the intervention) | — |
0.07 SDs higher (0.04 lower to 0.17 higher) |
1454 children | — |
| Macours 2008 |
Level of fine motor development, current Z‐score of Denver Developmental Screening Test (fine motor sub‐scale) score. Scale: unclear. (follow‐up: 8 to 9 months) |
unclear |
0.09 SDs higher (0.04 lower to 0.23 higher) |
1568 children | Better indicated by higher values |
| Macours 2008 | (follow‐up: eight to 29 months after 12 months of the intervention) | — |
0.15 SDs higher (0.06 to 0.25 higher) |
1467 children | — |
| Macours 2008 |
Level of social‐personal development, current Z‐score of Denver Developmental Screening Test (social‐personal sub‐scale) score. Scale: unclear. (follow‐up: 8 to 9 months) |
unclear |
0.11 SDs higher (0.01 lower to 0.22 higher) |
1585 children | Better indicated by higher values |
| Macours 2008 | (follow‐up: 8 to 29 months after 12 months of the intervention) | — |
0.09 SDs higher (0.03 lower to 0.22 higher) |
1473 children | — |
Level of memory development, current
In comparison 1 from the Macours 2008 study, the UCT increased the level of development of short‐term memory, compared with no UCT and when followed up at 8 to 9 months (MD 0.18 SDs, 95% CI 0.05 to 0.30, Analysis 1.4). We could not judge the clinical meaningfulness of this level of change due to the lack of relevant standards. The mean score in the control group at baseline was also unclear, but we judged this treatment effect to be of moderate size. This comparison provided no evidence that the moderate beneficial effect persisted after the intervention had ceased (MD 0.07 SDs, 95% CI − 0.04 to 0.17, Analysis 1.4).
Level of motor development, current
In comparison 1 from the Macours 2008 study, compared with no UCT and followed‐up at 8 to 9 months, there was no evidence that the UCT had any effect on development of fine motor skills (MD 0.09, 95% CI − 0.04 to 0.23, Analysis 1.4). When followed up 8 to 29 months after the 12‐month intervention had ceased, the UCT had increased the development of fine motor skills (MD 0.15, 95% CI 0.06 to 0.25, Analysis 1.4). We could not judge the clinical meaningfulness of this level of change due to the lack of relevant standards. The mean score in the control group at baseline was also unclear, but we judged this treatment effect to be of moderate size.
Level of social‐personal development, current
Comparison 1 from the Macours 2008 study provided no evidence that the UCT had any effect on social‐personal development among children, when compared with no UCT, whether followed up at 8 to 9 months (MD 0.11 SDs, 95% CI − 0.01 to 0.22, Analysis 1.4) or 8 to 29 months after 12 months of the intervention (MD 0.09 SDs, 95% CI − 0.03 to 0.22, Analysis 1.4).
Became acutely malnourished, previous three months
In comparison 2 from the Langendorf 2013 study, the meta‐analysed UCTs reduced the incidence of severe acute malnutrition (HR 0.44, 95% CI 0.24 to 0.80, Figure 5) in the previous three months among children, compared with their co‐interventions only and followed up after four months of the intervention. In absolute terms, 10 children per 1000 child months became acutely malnourished among those receiving the UCT plus co‐intervention (95% CI 6 to 19), compared with 23 children per 1000 child months among those receiving the co‐intervention only. We are not aware of international standards for judging the clinical meaningfulness of change in this outcome. However, we nevertheless felt confident that this 56% reduction in incidence was both large and clinically meaningful.
5.
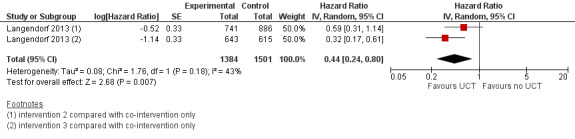
Forest plot of comparison: 1 Unconditional cash transfer compared with no unconditional cash transfer (or co‐intervention only), outcome: 1.5 Became severely acutely malnourished, previous three months.
Social determinants of health
Has pen and paper in home, current
The UCT in comparison 1 from the Macours 2008 study increased the proportion of children who had pen and paper in their home at the time of the interview, compared with no UCT and followed up at 8 to 9 months of the intervention's commencement (MD 0.11 SDs, 95% CI 0.05 to 0.16, Analysis 1.6). We could not judge the clinical meaningfulness of this level of change due to a lack of international standards. However, considering the high mean proportion in the control group with the outcome at baseline (68%), we judged this beneficial effect to be small in size. However, the comparison provided no evidence suggesting that the benefit persisted 8 to 29 months after the intervention of 12 months duration had ceased (MD 0.04 SDs, 95% CI − 0.01 to 0.09, Analysis 1.6).
1.6. Analysis.
Comparison 1 Unconditional cash transfer compared with no unconditional cash transfer (or co‐intervention only), Outcome 6 Social determinants of health.
| Social determinants of health | |||||
|---|---|---|---|---|---|
| Study | Outcome | Mean in control group | Mean in intervention group | Number of participants | Comments |
| Macours 2008 |
Has pen and paper in home, current Z‐score of proportion (follow‐up: 8 to 9 months) |
The mean proportion in the control group was 68% |
0.11 standard deviations (SDs) higher (0.05 SDs to 0.16 SDs higher) |
3326 children | — |
| Macours 2008 | (follow‐up: 8 to 29 months after 12 months of the intervention) | — |
0.04 SDs higher (0.01 lower to 0.09 higher) |
4245 children | — |
| Macours 2008 |
Quality of parenting Z‐score of Home Observation for Measurement of the Environment score. Scale: unclear. (follow‐up: 8 to 9 months) |
The mean score in the control group was 4.02 units |
0.20 SDs lower (0.81 lower to 0.40 higher) |
3326 adults | Better indicated by lower values |
| Macours 2008 | (follow‐up: 8 to 29 months after 12 months of the intervention) | — |
0.13 SDs lower (0.39 lower to 0.14 higher) |
4245 children | — |
Quality of parenting, current
There was no evidence from comparison 1 from the Macours 2008 study that the UCT had any effect on the quality of maternal parenting as measured by the Home Observation Measurement of the Environment (HOME) Scale after 8 to 9 months of the intervention (MD − 0.20 SDs, 95% CI − 0.81 to 0.40, Analysis 1.6) or 8 to 29 months after the intervention had ceased (MD − 0.13 SDs, 95% CI − 0.39 to 0.14, Analysis 1.6).
Unconditional cash transfers compared with in‐kind transfers
Health outcomes
Died, previous three months
Comparisons 3, 4, and 5 from the Langendorf 2013 study provided no evidence for reductions of the chance of death among children when the UCT was compared with three in‐kind transfers and followed up after four months of the intervention (food transfer 1: HR 0.81, 95% CI 0.40 to 1.66; food transfer 2: HR 1.74, 95% CI 0.88 to 3.47; food transfer 3: HR 2.27, 95% CI 0.69 to 7.44; Analysis 2.1).
2.1. Analysis.
Comparison 2 Unconditional cash transfer compared with in‐kind transfer, Outcome 1 Health outcomes.
| Health outcomes | ||||||
|---|---|---|---|---|---|---|
| Study | Outcome | Comparison |
Hazard rate in control group (95% confidence interval) |
Hazard rate in treatment group (95% confidence interval) |
Hazard ratio (95% CI) |
Number of participants |
| Langendorf 2013 |
Died, previous three monts Number of events per 100 child‐months (follow‐up: four months) |
Comparison 3 | 0.70 (0.46 to 1.07) |
0.61 (0.36 to 1.03) |
HR 0.81 (0.40 to 1.66) |
1140 children |
| Langendorf 2013 | Comparison 4 | 0.37 (0.18 to 0.74) |
0.61 (0.36 to 1.03) |
HR 1.74 (0.88 to 3.47) |
943 children | |
| Langendorf 2013 | Comparison 5 | 0.26 (0.13 to 0.51) |
0.61 (0.36 to 1.03) |
HR 2.27 (0.69 to 7.44) |
1082 children | |
| Langendorf 2013 |
Became severely acutely malnourished, last three months Number of events per child‐months (follow‐up: four months) |
Comparison 3 | 2.24 (1.73 to 2.89) |
1.79 (1.27 to 2.51) |
HR 0.84 (0.49 to 1.44) |
1140 children |
| Langendorf 2013 | Comparison 4 | 2.29 (1.68 to 3.12) |
1.79 (1.27 to 2.51) |
HR 0.78 (0.46 to 1.35) |
943 children | |
| Langendorf 2013 | Comparison 5 | 1.73 (1.28 to 2.33) |
1.79 (1.27 to 2.51) |
HR 1.15 (0.67 to 1.99) |
— | |
Became acutely malnourished, previous three months
Comparisons 3, 4, and 5 from the Langendorf 2013 study also provided no evidence for reductions of the incidence of severe acute malnutrition among children receiving the UCT, compared with children receiving an in‐kind transfer and followed up after four months of the intervention (food transfer 1: HR 0.84, 95% CI 0.49 to 1.44; food transfer 2: HR 0.78, 95% CI 0.46 to 1.35; food transfer 3: HR 1.15, 95% CI 0.67 to 1.99; Analysis 2.1).
Unconditional cash transfer compared with the same unconditional cash transfer paid through a different mechanism
Health outcomes
Level of dietary diversity, current
In comparison 6 from the Aker 2011 study, compared with the same UCT paid via mobile phone, the UCT paid in‐hand led to an increase in dietary diversity among households, when measured using the 12‐unit Household Dietary Diversity Score and followed up three months after the five‐month intervention had ceased (DD 0.43 scores, 95% CI 0.06 to 0.80, Analysis 3.1). We are not aware of international standards for judging the clinical meaningfulness of change in this outcome. However, considering the relatively low mean score in the control group at baseline (3.07 units), we nevertheless felt confident that the increase of 0.43 units was both large and clinically meaningful.
3.1. Analysis.
Comparison 3 Unconditional cash transfer compared with same unconditional cash transfer paid through different mechanism, Outcome 1 Health outcomes.
| Health outcomes | |||||
|---|---|---|---|---|---|
| Study | Outcome | Mean in control group | Mean in treatment group | Number of participants | Comment |
| Aker 2011 |
Level of dietary diversity, current Household Dietary Diversity score. Scale: 0 to 12. (follow‐up: 3 months after 5 months of intervention) |
3.07 scores |
0.43 scores higher (0.06 to 0.80 higher) |
1200 households | Measure of treatment effect: difference‐in‐differences estimator |
Social determinants of health
Number of asset categories owned, current
Comparison 6 from the Aker 2011 study reported that the UCT paid in‐hand increased the total numbers of asset categories owned among households, compared with the same UCT paid via mobile phone and followed up three months after five months of the intervention (DD 0.46 categories, 95% CI 0.20 to 0.72, Analysis 3.2). We could not judge the clinical meaningfulness of this level of change in this outcome due to a lack of international standards. However, considering the small mean number in the control group at baseline (3.59 categories), we considered this treatment effect to be moderate in size.
3.2. Analysis.
Comparison 3 Unconditional cash transfer compared with same unconditional cash transfer paid through different mechanism, Outcome 2 Social determinants of health.
| Social determinants of health | |||||
|---|---|---|---|---|---|
| Study | Outcome | Mean in control group | Mean in intervention group | Number of participants | Comments |
| Aker 2011 |
Number of asset categories owned, current Number (follow‐up: 3 months after 5 months of intervention) |
3.59 categories |
0.46 categories higher (0.20 to 0.72 higher) |
1200 households | Measure of treatment effect: difference‐in‐differences estimator |
Health service expenditure
Used cash transfer to pay for health services, reporting period unclear
Comparison 6 from the Aker 2011 study provided no evidence that the UCT paid in‐hand impacted the proportion of households who used the cash transfer to pay for health services, compared with the same UCT paid via mobile phone and when followed up three months after five months of the intervention (MD − 0.05, 95% CI − 0.13 to 0.03, Analysis 3.3). Subgroup analyses reported similar relative effectiveness of in‐hand and mobile phone payments on this outcome among the Fulani and Touareg ethnic groups (MD − 0.03, 95% CI − 0.17 to 0.11) and the Hausa ethnic group (MD 0.06, 95% CI − 0.02 to 0.14). Our formal test found no evidence of any subgroup differences by these ethnic groups (P = 0.26).
3.3. Analysis.
Comparison 3 Unconditional cash transfer compared with same unconditional cash transfer paid through different mechanism, Outcome 3 Health service expenditure.
| Health service expenditure | |||||
|---|---|---|---|---|---|
| Study | Outcome | Mean in control group | Mean in intervention group | Number of participants | Comments |
| Aker 2011 |
Used cash transfer to pay for health services, reporting period unclear Proportion (follow‐up: 3 months after 5 months of intervention) |
29% |
0.05 lower (0.13 lower to 0.03 higher) |
1200 households | Measure of treatment effect: mean difference. No evidence for any difference in treatment effect between the Fulani or Touareg ethnic group and the Hausa ethnic group (P = 0.26). |
Local markets and infrastructure
Cultivated land, previous growing season
Comparison 6 from the Aker 2011 study suggested no effect on the proportion of households who had cultivated land in the previous growing season, when the UCT paid in‐hand was compared with the same UCT paid via mobile phone, measured three months after five months of the intervention (DD 0.01, 95% CI − 0.01 to 0.03, Analysis 3.4).
3.4. Analysis.
Comparison 3 Unconditional cash transfer compared with same unconditional cash transfer paid through different mechanism, Outcome 4 Local markets and infrastructure.
| Local markets and infrastructure | |||||
|---|---|---|---|---|---|
| Study | Outcome | Mean in control group | Mean in treatment group | Number of participants | Comments |
| Aker 2011 |
Cultivated land, previous growing season Proportion (follow‐up: 3 months after 5 months of intervention) |
98% |
0.01 higher (0.01 lower to 0.03 higher) |
1200 households | Measure of treatment effect: difference‐in‐differences estimator (DD) |
| Aker 2011 |
Number of crop types grown, previous growing season Number (follow‐up: 3 months after 5 months of intervention) |
4.44 types |
0.36 types higher (0.05 lower to 0.77 higher) |
1200 households | Measure of treatment effect: DD |
| Aker 2011 |
Sold millet, previous growing season Proportion (follow‐up: 3 months after 5 months of intervention) |
4% |
0.04 higher (0.04 lower to 0.12 higher) |
1200 households | Measure of treatment effect: DD |
| Aker 2011 |
Spent cash transfer at kiosk in village, reporting period unclear Proportion (follow‐up: 3 months after 5 months of intervention) |
43% |
0.09 higher (0.03 lower to 0.21 higher) |
1200 households | Measure of treatment effect: mean difference (MD) |
| Aker 2011 |
Spent cash transfer all at once, reporting period unclear Proportion (follow‐up: 3 months after 5 months of intervention) |
54% |
0.00 higher (0.08 lower to 0.08 higher) |
1200 households | Measure of treatment effect: MD |
Number of crop types grown, last growing season
Comparison 6 from the Aker 2011 study provided no evidence for any effect on the number of crop types grown among households, when the UCT paid in‐hand was compared with the same UCT paid via mobile phone, followed up after five months of the intervention (DD 0.36 types, 95% CI − 0.05 types to 0.77 types, Analysis 3.4).
Sold millet, previous growing season
Comparion 6 from the Aker 2011 study also provided no evidence for any effect of the UCT paid in‐hand on the proportion of households who sold millet in the previous growing season, compared with the same UCT paid via mobile phone and followed up after five months of the intervention (DD 0.04, 95% CI − 0.04 to 0.12, Analysis 3.4).
Spent cash transfer at kiosk in village, reporting period unclear
In comparison 6 from the Aker 2011 study, no evidence was found for any effect of the UCT paid in‐hand on the proportion of households who spent the cash transfer at a kiosk in their village, when compared with the same UCT paid via mobile phone at five months follow‐up (MD 0.09, 95% CI − 0.03 to 0.21, Analysis 3.4).
Spent cash transfer all at once, reporting period unclear
Finally, comparison 6 from the Aker 2011 study reported no evidence for any impact of the UCT paid in‐hand on the proportion of households who spent the cash transfer all at once, compared with the same UCT paid via mobile phone at five months follow‐up (MD 0.00, 95% CI − 0.08 to 0.08, Analysis 3.4).
Discussion
Summary of main results
Three studies (one cluster‐RCT and two CBAs) comprising a total of 13,885 participants (9640 children and 4245 adults) and 1200 households in two LMICs (Nicaragua and Niger) fulfilled the inclusion criteria and were narratively synthesised. These studies examined five short‐term UCTs that were worth between USD 145 and 250 (or more, depending on household characteristics) and were provided by governmental, non‐governmental or research organisations in experiments or pilot programmes. Although this review covered disaster contexts in general, the only studies found were conducted in response to droughts. Two studies examined the effectiveness of UCTs, and one study examined the relative effectiveness of UCTs paid in‐hand compared with in‐kind transfers and UCTs paid through a different mechanism. Due to the body of evidence's methodologic limitations, serious risk of bias and very serious indirectness, it was considered to be of very low overall quality and thus very uncertain.
Depending on the specific health services use and health outcomes examined, the included studies either reported no evidence that UCTs had impacted the outcome or they reported that UCTs had improved the outcome. One study reported that a UCT led to a very small increase in the proportion of children who received vitamin or iron supplements after eight to nine months. One study examined the proportion of children receiving deworming drugs, but it found no evidence for any effect of a UCT on this outcome after eight to nine months. One study showed that UCTs led to clinically meaningful, very large reductions in the chance of child death and a clinically meaningful, large reduction in the incidence of acute severe malnutrition after four months. One study reported no evidence for any effect of a UCT on children's height for age. In one study, a UCT resulted in a moderate reduction in the number of days children spent sick in bed after eight to nine months. The one study that examined adults' level of depression found no evidence for any effect after eight to nine months. One study reported a beneficial effect on a social determinant of health (i.e., the child home environment) but did not find evidence for an effect on another determinant (i.e., the quality of parenting behaviour). The included comparisons did not examine several other important outcomes, including food security and equity impacts.
Evidence on the relative effectiveness of in‐hand UCTs compared with in‐kind transfers and with UCTs paid through a different mechanism was also of very low quality and uncertain. Compared with in‐kind transfers, there was no evidence from one study that a UCT had any effect on the chance of child death and severe acute malnutrition after four months. In one study, a UCT paid in‐hand led to a clinically meaningful, moderate increase in the household dietary diversity score, compared with the same UCT paid via mobile phone, but the study found no evidence for an effect on social determinants of health, health service expenditure, or local markets and infrastructure, three months after the five‐month intervention had ceased.
Overall completeness and applicability of evidence
The current body of evidence is insufficient in size and scope to address the objectives of this review. Existing evidence is limited in participant type (i.e., limited mostly to children) and to a small number of LMICs (i.e., two countries from different WHO regions). Evidence on UCT effects in adults is sparse, and it is missing altogether for adult men. There is a profound lack of evidence on UCTs for assistance in natural disasters other than droughts, and for assistance in man‐made disasters. Evidence on health services use is limited to only a few outcomes on a limited range of mostly preventive services. While evidence on health outcomes achieves a better coverage of more diverse, relevant outcomes from several relevant domains, it could be improved, especially in outcome domains such as anthropometric measures (e.g., stunting, wasting, and underweight) and food security (e.g., the Household Food Insecurity Access Scale score). The two ongoing studies included in this review will provide evidence on some of the required anthropometric measures (REFANI‐N; REFANI‐P). Secondary outcomes are limited to a small number of social determinants of health, health care expenditure, and local markets and infrastructure outcomes. Subgroup analyses along PROGRESS categories are missing, meaning that evidence to determine equity impacts of UCTs is currently unavailable.
We identified two limitations to the applicability of evidence from the Langendorf 2013 study. First, because the study excluded 12 eligible village clusters with access concerns (e.g., more remote villages), evidence from this study may not be applicable to inaccessible geographic areas. Second, comparison 2 from the Langendorf 2013 study, where two UCTs provided in combination with co‐interventions were compared with their co‐intervention only (for details see Table 3), may also have limited applicability. In this comparison the observed net treatment effect of the two UCTs plus co‐interventions may have interacted to produce an additional effect, beyond what the UCT and the co‐intervention would have had if they had been implemented as standalone interventions. For example, while neither the UCT nor the co‐intervention (i.e., a food transfer) may be effective, the combination of both (i.e., additional income together with food) may be. Therefore, comparison 2 may not robustly isolate the effectiveness of the UCT component alone, and evidence from this comparison may not necessarily be applicable for planning and implementing standalone UCT interventions.
Quality of the evidence
Additional, high‐quality evidence is required to reach conclusions regarding the effectiveness and relative effectiveness of UCTs for improving health services use and health outcomes in humanitarian disasters in LMICs. The number of studies and, to a lesser degree, the number of interventions included in this review were small. The included studies comprised a large number of participants (13,885 participants and 1200 households). However, these participants came from only two LMICs. Only two studies provided evidence on the effectiveness of UCT interventions in improving health services use and health outcomes. Only one study was a RCT, whereas two studies were CBAs and thus methodologically limited.
The assessment of the quality of the evidence on each primary outcome in primary analyses (i.e., UCT compared with no UCT or with the co‐intervention only) was based on the GRADE criteria (Balshem 2011). All primary outcomes carried a serious risk of bias from lack of allocation concealment, lack of blinding, and potential contamination (minus one grade). Because all included primary outcomes were reported in one study only, the consistency of study findings could not be assessed for any outcome. All primary outcomes were very seriously indirect (minus two grades), because the only evidence found on them was conducted in only one type of humanitarian disaster setting (i.e., droughts) and among only one type of participants (i.e., either children or adults). Most primary outcomes were estimated with a good level of precision, but some primary outcomes were seriously imprecise (i.e., weight, height for age, weight for age, gross motor development, social‐personal development; minus one grade) or very seriously imprecise (i.e., level of depression; minus two grades). Due to all included primary outcomes being reported in one study only, the risk of publication bias could not be assessed for any outcome. There was no evidence that all plausible confounding would tend to reduce the observed effect, rather than explain it, and no evidence was found for dose response gradients. Thus, we judged the overall quality of the evidence to be very low for all primary outcomes.
Potential biases in the review process
We have some confidence that the review identified all completed eligible studies. However, evaluations of existing UCT programmes are commonly published in inaccessible grey literature, and the review may have missed some such programme evaluations. However, our search strategy was designed to be very broad in order to ensure that all potentially relevant records were identified from the several academic and grey literature databases, as well as other relevant sources such as websites of key international, governmental, and non‐governmental organisations. We also asked several leading experts to identify any missing studies. Moreover, the review methodology was designed with the goal of ensuring that review processes would not introduce bias. All academic and several grey literature database searches were conducted by an independent reference librarian. Two review authors independently selected, extracted, quality‐assessed, and interpreted the existing evidence. We extracted all eligible primary outcomes reported for each study and listed alternative measurements for included outcomes that we did not report in this review in the 'Characteristics of included studies' table. However, we excluded studies that did not report any primary outcomes of this review in their study records without checking these studies for any unreported outcomes, and this may have introduced reporting bias. Furthermore, we excluded non‐randomised study designs other than cohort studies, CBAs, and interrupted time‐series studies to reduce bias, but this decision may have reduced the applicability and completeness of the results of the review. Finally, changes between the protocol and the review (described in the section 'Differences between protocol and review') may have introduced bias. However, major changes such as the addition of a secondary review objective were made in agreement with the editors, which should have prevented the introduction of reporting bias.
Agreements and disagreements with other studies or reviews
We are not aware of any previous systematic reviews that have synthesised evidence specifically on the effect of UCTs for assistance in humanitarian disasters on the use of health services and health outcomes. A number of previous reviews on the effect of cash transfers on the use of health services, health outcomes or both in LMICs generally included either CCTs only (Gaarder 2011; Lagarde 2009; Pega 2013) or a broader set of cash transfers that combined UCTs with CCTs and sometimes even also with other financial interventions such as microfinance interventions or public works programmes (Adato 2009; Arnold 2011; Bassani 2013; Boccia 2011; Heise 2013; Manley 2013; Pettifor 2012; Sridhar 2006). They also generally included a broader set of study types, often including cross‐sectional studies that Cochrane Reviews exclude due to their high risk of bias. Therefore, previous review findings are not comparable with those of this review.
Authors' conclusions
Implications for practice.
Given the low quality of the available evidence to date, we cannot make any clear conclusions regarding the effectiveness of UCTs for improving health services use and health outcomes in humanitarian disaster contexts in LMICs.
Implications for research.
Further high‐quality studies of the effect of UCTs for assistance in humanitarian disasters on use of health services and health outcomes in LMICs are required. The International Initiative for Impact Evaluation has recently published best practice guidelines for conducting impact evaluations in disaster contexts that aim to ensure the highest feasible quality of impact evaluations in these contexts (Puri 2014). Future studies should apply RCT designs, if feasible. In studies that compare participants receiving a UCT with those not receiving a UCT, risk of performance bias is perhaps unavoidable, because participants cannot be blinded to the receipt of a UCT. Previous studies have often not ensured allocation concealment, risked contamination or both, but to improve the quality of the body of evidence, future studies should conceal allocation and reduce the risk of contamination (e.g., by sampling geographically disconnected clusters). Also, future studies should develop and publish study protocols and rigorously report missing data so that reviewers can fully judge the risks of publication and attrition bias. In terms of scope, additional research is particularly needed to determine the effects of UCTs in adults, including especially adult men, and on outcome domains with relatively little or no existing evidence such as anthropometric measures and food security. Studies examining a range of disaster contexts other than droughts are paramount. Finally and importantly, studies that determine the equity impacts of UCTs along key PROGRESS categories are needed.
Acknowledgements
We are thankful to: Jodie Doyle, Miranda Cumpston, Dr Rob Anderson, and Professor Elizabeth Waters (all Cochrane Public Health Group) and Toby Lasserson (Cochrane Editorial Unit) for editorial guidance; Dr Paul Bain (Harvard Medical School) for searching electronic academic and grey literature databases; Dr Roman Pabayo (University of Nevada, Reno and Harvard School of Public Health) for contributing to the search of key organisational websites; Carolin Henning and Tatjana Paeck (both University of Bremen) for contributing to data extraction; Kate Sloane (University of Otago) for proof‐reading this review; Meggan Harris (The Cochrane Collaboration) for copy‐editing this review; Dr Karen Macours (Paris School of Economics) for providing additional data on an included study; Carmel Dolan (Emergency Nutrition Network) and Ellyn Yakowenko (Action Against Hunger) for providing information on ongoing studies; Gordon Purdie and Dr James Stanley (both University of Otago) for statistical advice; the review advisory group members Dr Sarah Baird (University of Washington) and Dr Bayard Roberts (London School of Hygiene and Tropical Medicine) and the other experts Aneil Jaswal (Oxford University) and Dr Luca Pellerano (Oxford Policy Mangement) for their advice; and Patrick Condron (University of Melbourne), Dr David Warren (World Bank), and an anonymous reviewer for their external peer review.
Appendices
Appendix 1. Search strategy for Ovid MEDLINE 1946 to Present with Daily Update
This search strategy is identical to that used in our forthcoming review of UCTs for reducing poverty and vulnerabilities (Pega 2014a), which is being conducted in tandem with this review. Because specific keywords or MeSH heading terms for UCTs in electronic academic databases are lacking, and different terms for UCTs are used within and across relevant disciplines (e.g., medicine, epidemiology, economics, social policy and political science), any search strategy for UCTs is necessarily broad and encompasses both UCTs for assistance in humanitarian disasters and UCTs for reducing poverty and vulnerabilities.
Intervention terms
1. maternal welfare/ 2. public policy/ 3. social welfare/ 4. exp social security/ 5. (social adj (assistance or polic$ or welfare or insurance$ or protection)).ti,ab. 6. public assistance.ti,ab. 7. family policy.mp. 8. ((financial or cash or pay$ or monetary or money) adj3 (transfer$ or measure$ or incentive$ or allowance$ or exclu$ or reform$ or gain$ or credit$1 or benefit$1)).ti,ab. 9. or/1‐8
Study terms
10. randomised controlled trial/ 11. random$.ti,ab. 12. random allocation/ 13. placebos/ 14. placebo$.ti,ab. 15. single‐blind method/ 16. double‐blind method/ 17. ((single or double or triple or treble) adj blind$).ti,ab. 18. control groups/ 19. exp clinical trial/ 20. comparative Study/ 21. intervention studies/ 22. exp cohort studies/ 23. evaluation studies/ 24. program evaluation/ 25. (time adj series).ti,ab. 26. quasi‐experiment$.ti,ab. 27. (pre test or pretest or pre‐intervention or post test or posttest or post‐intervention).ti,ab. 28. controlled before.ti,ab. 29. independent panel.ti,ab. 30. panel stud$.ti,ab. 31. intervention$ stud$.ti,ab. 32. “before and after”.ti,ab. 33. repeat$ measure$.ti,ab. 34. evaluat$ stud$.ti,ab. 35. compari$ stud$.ti,ab. 36. (trial or follow‐up assessment$ or follow up assessment$ or groups).ti,ab. 37. ((intervention or interventional or process or program) adj8 (evaluat$ or effect$ or outcome$)).ti,ab. 38. (program or programme or secondary analys$).ti,ab. 39. ((evaluat$ or intervention$ or treatment$) and (control$ or study or program$ or comparison or comparative)).ti,ab. 40. or/10‐39
Country terms
41. Developing Countries/ 42. Medically Underserved Area/ 43. exp Africa/ or exp “Africa South of the Sahara”/ or exp Asia/ or exp South America/ or exp Latin America/ or exp Central America/ 44. (Africa or Asia or South America or Latin America or Central America).tw. 45. (American Samoa$ or Argentin$ or Beliz$ or Botswana$ or Brazil$ or Bulgaria$ or Chile$ or Comoro$ or Costa Rica$ or Croatia$ or Dominica$ or Equatorial Guinea$ or Gabon$ or Grenada$ or Hungar$ or Kazakh$ or Latvia$ or Leban$ or Libya$ or Lithuania$ or Malaysia$ or Mauriti$ or Mexic$ or Micronesia$ or Montenegr$ or Oman$ or Palau$ or Panama$ or Poland or Polish or Romania$ or Russia$ or Seychelles$ or Slovakia$ or South Africa$ or “Saint Kitts and Nevis” or Saint Lucia$ or “Saint Vincent and the Grenadines” or Turk$ or Urugua$ or Venezuel$ or Yugoslavia$).sh,tw. or Guinea$.tw. or Libia$.tw. or Mayotte.tw. or Northern Mariana Island$.tw. or Russian Federation.tw. or Samoa$.tw. or Serbia$.tw. or Slovak Republic$.tw. or “St Kitts and Nevis”.tw. or St Lucia$.tw. or “St Vincent and the Grenadines”.tw. 46. (Albania$ or Algeria$ or Angol$ or Armenia$ or Azerbaijan$ or Belarus$ or Bhutan$ or Bolivia$ or “Bosnia and Herzegovina” or Bosnian$ or Cameroon$ or China or Chinese or Colombia$ or Congo$ or Cuba$ or Djibouti$ or Dominican Republic$ or Ecuador$ or Egypt$ or El Salvador$ or Fiji$ or “Georgia (Republic)” or Goergian$ or Guam$ or Guatemal$ or Guyana$ or Hondur$ or Indian Ocean Island$ or Indonesia$ or Iran$ or Iraq$ or Jamaica$ or Jordan$ or Lesotho or “Macedonia (Republic)” or Marshall Island$ or Micronesia$ or Middle East$ or Moldova$ or Morocc$ or Namibia$ or Nicaragua$ or Paraguay$ or Peru$ or Philippin$ or Samoa$ or Sri Lanka$ or Suriname$ or Swaziland$ or Syria$ or Thai$ or Tonga$ or Tunisia$ or Turkmen$ or Ukrain$ or Vanuatu).sh,tw. or Bosnia$.tw. or Cape Verd$.tw. or Gaza.tw. or Georgia$.tw. or Kiribati$.tw. or Macedonia$.tw. or Maldives.tw. or Marshall Island$.tw. or Palestin$.tw. or Syrian Arab Republic$.tw. or West Bank.tw. 47. (Afghan$ or Bangladesh$ or Benin$ or Burkina Faso$ or Burundi$ or Cambodia$ or Central African Republic$ or Chad$ or Comoros or “Democratic Republic of the Congo” or Cote d’Ivoire or Eritrea$ or Ethiopia$ or Gambia$ or Ghana$ or Guinea$ or Guinea‐Bissau or Haiti$ or India$ or Kenya$ or Korea$ or Kyrgyz$ or Laos or Laot$ or Liberia$ or Madagascar or Malagasy or Malawi$ or Mali$ or Mauritania$ or Melanesia$ or Mongolia$ or Mozambi$ or Myanmar or Nepal$ or Niger$ or Nigeria$ or Pakistan$ or Papua New Guinea$ or Rwanda$ or Senegal$ or Sierra Leone$ or Somalia$ or Sudan$ or Tajikistan$ or Tanzania$ or East Timor$ or Togo$ or Uganda$ or Uzbek$ or Vietnam$ or Yemen$ or Zambia$ or Zimbabw$).sh,tw. or Burm$.tw. or Congo$.tw. or Lao.tw. or North Korea$.tw. or Solomon Island$.tw. or Sao Tome.tw. or Timor$.tw. or Viet Nam.tw. 48. ((developing or less$ developed or third world or under developed or middle income or low income or underserved or under served or deprived or poor$) adj (count$ or nation? or state? or population?)).tw. 49. (lmic or lmics).tw. 50. or/41‐49 51. 10 and 40 and 50
Appendix 2. Search strategies for electronic academic databases
Cochrane Central Register of Controlled Trial (CENTRAL)
9 May 2014
105 records
Intervention terms
TX ((social N1 (assistance OR polic* OR welfare OR insurance* OR protection)) OR "public assistance" OR "family policy" OR ((financial OR cash OR pay* OR monetary OR money) N3 (transfer* OR measure* OR incentive* OR allowance* OR exclu* OR reform* OR gain* OR credit OR credits OR benefit OR benefits)))
Countries terms
TX (Africa OR Asia OR "South America" OR "Latin America" OR "Central America" OR ((developing OR "less* developed" OR "third world" OR "under developed" OR "middle income" OR "low income" OR underserved OR "under served" OR deprived OR poor*) N1 (count* OR nation OR nations OR state OR states OR population OR populations)) OR lmic OR lmics)
OR
TI (Samoa* OR Argentin* OR Beliz* OR Botswana* OR Brazil* OR Bulgaria* OR Chile* OR Comoro* OR "Costa Rica*" OR Croatia* OR Dominica* OR Guinea* OR Gabon* OR Grenada* OR Hungar* OR Kazakh* OR Latvia* OR Leban* OR Libya* OR Lithuania* OR Malaysia* OR Mauriti* OR Mexic* OR Micronesia* OR Montenegr* OR Oman* OR Palau* OR Panama* OR Poland OR Polish OR Romania* OR Russia* OR Seychelles* OR Slovak* OR "Saint Kitts" OR Nevis OR "Saint Lucia*" OR "Saint Vincent" OR Grenadines OR Turk* OR Urugua* OR Venezuel* OR Yugoslavia* OR Libia* OR Mayotte OR "Mariana Island*" OR Serbia* OR "St Kitts" OR "St Lucia*" OR "St Vincent" OR Albania* OR Algeria* OR Angol* OR Armenia* OR Azerbaijan* OR Belarus* OR Bhutan* OR Bolivia* OR Bosnia* OR Herzegovin* OR Cameroon* OR China OR Chinese OR Colombia* OR Congo* OR Cuba* OR Djibouti* OR Ecuador* OR Egypt* OR "El Salvador*" OR Fiji* OR Georgia* OR Guam* OR Guatemal* OR Guyana* OR Hondur* OR "Indian Ocean Island*" OR Indonesia* OR Iran* OR Iraq* OR Jamaica* OR Jordan* OR Lesotho OR Macedonia* OR "Marshall Island*" OR Micronesia* OR "Middle East*" OR Moldova* OR Morocc* OR Namibia* OR Nicaragua* OR Paraguay* OR Peru* OR Philippin* OR "Sri Lanka*" OR Suriname* OR Swaziland* OR Syria* OR Thai* OR Tonga* OR Tunisia* OR Turkmen* OR Ukrain* OR Vanuatu* OR "Cape Verd*" OR Gaza OR Kiribati* OR Maldives OR Palestin* OR "West Bank" OR Afghan* OR Bangladesh* OR Benin* OR "Burkina Faso*" OR Burundi* OR Cambodia* OR "Central African Republic*" OR Chad* OR Comoros OR Congo* OR "Cote d Ivoire" OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea* OR "Guinea‐Bissau" OR Haiti* OR India* OR Kenya* OR Korea* OR Kyrgyz* OR Laos OR Laot* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Melanesia* OR Mongolia* OR Mozambi* OR Myanmar OR Nepal* OR Niger* OR Nigeria* OR Pakistan* OR "Papua New Guinea*" OR Rwanda* OR Senegal* OR "Sierra Leone*" OR Somalia* OR Sudan* OR Tajikistan* OR Tanzania* OR "East Timor*" OR Togo* OR Uganda* OR Uzbek* OR Vietnam* OR Yemen* OR Zambia* OR Zimbabw* OR Burm* OR Lao.tw. OR "North Korea*" OR "Solomon Island*" OR "Sao Tome" OR Timor* OR "Viet Nam*" OR "ivory coast")
OR
AB (Samoa* OR Argentin* OR Beliz* OR Botswana* OR Brazil* OR Bulgaria* OR Chile* OR Comoro* OR "Costa Rica*" OR Croatia* OR Dominica* OR Guinea* OR Gabon* OR Grenada* OR Hungar* OR Kazakh* OR Latvia* OR Leban* OR Libya* OR Lithuania* OR Malaysia* OR Mauriti* OR Mexic* OR Micronesia* OR Montenegr* OR Oman* OR Palau* OR Panama* OR Poland OR Polish OR Romania* OR Russia* OR Seychelles* OR Slovak* OR "Saint Kitts" OR Nevis OR "Saint Lucia*" OR "Saint Vincent" OR Grenadines OR Turk* OR Urugua* OR Venezuel* OR Yugoslavia* OR Libia* OR Mayotte OR "Mariana Island*" OR Serbia* OR "St Kitts" OR "St Lucia*" OR "St Vincent" OR Albania* OR Algeria* OR Angol* OR Armenia* OR Azerbaijan* OR Belarus* OR Bhutan* OR Bolivia* OR Bosnia* OR Herzegovin* OR Cameroon* OR China OR Chinese OR Colombia* OR Congo* OR Cuba* OR Djibouti* OR Ecuador* OR Egypt* OR "El Salvador*" OR Fiji* OR Georgia* OR Guam* OR Guatemal* OR Guyana* OR Hondur* OR "Indian Ocean Island*" OR Indonesia* OR Iran* OR Iraq* OR Jamaica* OR Jordan* OR Lesotho OR Macedonia* OR "Marshall Island*" OR Micronesia* OR "Middle East*" OR Moldova* OR Morocc* OR Namibia* OR Nicaragua* OR Paraguay* OR Peru* OR Philippin* OR "Sri Lanka*" OR Suriname* OR Swaziland* OR Syria* OR Thai* OR Tonga* OR Tunisia* OR Turkmen* OR Ukrain* OR Vanuatu* OR "Cape Verd*" OR Gaza OR Kiribati* OR Maldives OR Palestin* OR "West Bank" OR Afghan* OR Bangladesh* OR Benin* OR "Burkina Faso*" OR Burundi* OR Cambodia* OR "Central African Republic*" OR Chad* OR Comoros OR Congo* OR "Cote d Ivoire" OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea* OR "Guinea‐Bissau" OR Haiti* OR India* OR Kenya* OR Korea* OR Kyrgyz* OR Laos OR Laot* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Melanesia* OR Mongolia* OR Mozambi* OR Myanmar OR Nepal* OR Niger* OR Nigeria* OR Pakistan* OR "Papua New Guinea*" OR Rwanda* OR Senegal* OR "Sierra Leone*" OR Somalia* OR Sudan* OR Tajikistan* OR Tanzania* OR "East Timor*" OR Togo* OR Uganda* OR Uzbek* OR Vietnam* OR Yemen* OR Zambia* OR Zimbabw* OR Burm* OR Lao.tw. OR "North Korea*" OR "Solomon Island*" OR "Sao Tome" OR Timor* OR "Viet Nam*" OR "ivory coast")
OR
SU (Samoa* OR Argentin* OR Beliz* OR Botswana* OR Brazil* OR Bulgaria* OR Chile* OR Comoro* OR "Costa Rica*" OR Croatia* OR Dominica* OR Guinea* OR Gabon* OR Grenada* OR Hungar* OR Kazakh* OR Latvia* OR Leban* OR Libya* OR Lithuania* OR Malaysia* OR Mauriti* OR Mexic* OR Micronesia* OR Montenegr* OR Oman* OR Palau* OR Panama* OR Poland OR Polish OR Romania* OR Russia* OR Seychelles* OR Slovak* OR "Saint Kitts" OR Nevis OR "Saint Lucia*" OR "Saint Vincent" OR Grenadines OR Turk* OR Urugua* OR Venezuel* OR Yugoslavia* OR Libia* OR Mayotte OR "Mariana Island*" OR Serbia* OR "St Kitts" OR "St Lucia*" OR "St Vincent" OR Albania* OR Algeria* OR Angol* OR Armenia* OR Azerbaijan* OR Belarus* OR Bhutan* OR Bolivia* OR Bosnia* OR Herzegovin* OR Cameroon* OR China OR Chinese OR Colombia* OR Congo* OR Cuba* OR Djibouti* OR Ecuador* OR Egypt* OR "El Salvador*" OR Fiji* OR Georgia* OR Guam* OR Guatemal* OR Guyana* OR Hondur* OR "Indian Ocean Island*" OR Indonesia* OR Iran* OR Iraq* OR Jamaica* OR Jordan* OR Lesotho OR Macedonia* OR "Marshall Island*" OR Micronesia* OR "Middle East*" OR Moldova* OR Morocc* OR Namibia* OR Nicaragua* OR Paraguay* OR Peru* OR Philippin* OR "Sri Lanka*" OR Suriname* OR Swaziland* OR Syria* OR Thai* OR Tonga* OR Tunisia* OR Turkmen* OR Ukrain* OR Vanuatu* OR "Cape Verd*" OR Gaza OR Kiribati* OR Maldives OR Palestin* OR "West Bank" OR Afghan* OR Bangladesh* OR Benin* OR "Burkina Faso*" OR Burundi* OR Cambodia* OR "Central African Republic*" OR Chad* OR Comoros OR Congo* OR "Cote d Ivoire" OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea* OR "Guinea‐Bissau" OR Haiti* OR India* OR Kenya* OR Korea* OR Kyrgyz* OR Laos OR Laot* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Melanesia* OR Mongolia* OR Mozambi* OR Myanmar OR Nepal* OR Niger* OR Nigeria* OR Pakistan* OR "Papua New Guinea*" OR Rwanda* OR Senegal* OR "Sierra Leone*" OR Somalia* OR Sudan* OR Tajikistan* OR Tanzania* OR "East Timor*" OR Togo* OR Uganda* OR Uzbek* OR Vietnam* OR Yemen* OR Zambia* OR Zimbabw* OR Burm* OR Lao.tw. OR "North Korea*" OR "Solomon Island*" OR "Sao Tome" OR Timor* OR "Viet Nam*" OR "ivory coast")
Ovid MEDLINE 1946 to Present with Daily Update, plus Daily Update through May 5, 2014
6 May 2014
Total Records: 4950
Intervention terms
maternal welfare/ OR public policy/ OR social welfare/ OR exp social security/ OR (social adj (assistance or polic$ or welfare or insurance$ or protection)).ti,ab. OR public assistance.ti,ab. OR family policy.mp OR ((financial or cash or pay$ or monetary or money) adj3 (transfer$ or measure$ or incentive$ or allowance$ or exclu$ or reform$ or gain$ or credit$1 or benefit$1)).ti,ab
Study terms
randomised controlled trial/ OR random$.ti,ab. OR random allocation/ OR placebos/ OR placebo$.ti,ab. OR single‐blind method/ OR double‐blind method/ OR ((single or double or triple or treble) adj blind$).ti,ab. OR control groups/ OR exp clinical trial/ OR comparative Study/ OR intervention studies/ OR exp cohort studies/ OR evaluation studies/ OR program evaluation/ OR (time adj series).ti,ab. OR quasi‐experiment$.ti,ab. OR (pre test or pretest or pre‐intervention or post test or posttest or post‐intervention).ti,ab. OR controlled before.ab,ti. OR independent panel.ti,ab. OR panel stud$.ti,ab. OR intervention$ stud$.ti,ab. OR "before and after".ti,ab. OR repeat$ measure$.ti,ab. OR evaluat$ stud$.ti,ab. OR compari$ stud$.ti,ab. OR (trial or follow‐up assessment$ or follow up assessment$ or groups).ti,ab OR ((intervention or interventional or process or program) adj8 (evaluat$ or effect$ or outcome$)).ab,ti. OR (program or programme or secondary analys$).ti,ab OR ((evaluat$ or intervention$ or treatment$) and (control$ OR study OR program$ OR comparison OR comparative)).ab,ti.
Country terms
Developing Countries/ OR Medically Underserved Area/ OR exp Africa/ OR exp Asia/ OR exp South America/ OR exp Latin America/ OR exp Central America/ OR (Africa OR Asia OR South America OR Latin America OR Central America).tw OR ((developing OR less$ developed OR third world OR under developed OR middle income OR low income OR underserved OR under served OR deprived OR poor$) adj (count$ OR nation? OR state? OR population?)).tw OR (lmic OR lmics).tw
(American Samoa$ OR Argentin$ OR Beliz$ OR Botswana$ OR Brazil$ OR Bulgaria$ OR Chile$ OR Comoro$ OR Costa Rica$ OR Croatia$ OR Dominica$ OR Equatorial Guinea$ OR Gabon$ OR Grenada$ OR Hungar$ OR Kazakh$ OR Latvia$ OR Leban$ OR Libya$ OR Lithuania$ OR Malaysia$ OR Mauriti$ OR Mexic$ OR Micronesia$ OR Montenegr$ OR Oman$ OR Palau$ OR Panama$ OR Poland OR Polish OR Romania$ OR Russia$ OR Seychelles$ OR Slovakia$ OR South Africa$ OR "Saint Kitts and Nevis" OR Saint Lucia$ OR "Saint Vincent and the Grenadines" OR Turk$ OR Urugua$ OR Venezuel$ OR Yugoslavia$).sh,tw. OR Guinea$.tw. OR Libia$.tw. OR Mayotte.tw. OR Northern Mariana Island$.tw. OR Russian Federation.tw. OR Samoa$.tw. OR Serbia$.tw. OR Slovak Republic$.tw. OR "St Kitts and Nevis".tw. OR St Lucia$.tw. OR "St Vincent and the Grenadines".tw.
(Albania$ OR Algeria$ OR Angol$ OR Armenia$ OR Azerbaijan$ OR Belarus$ OR Bhutan$ OR Bolivia$ OR "Bosnia and Herzegovina" OR Bosnian$ OR Cameroon$ OR China OR Chinese OR Colombia$ OR Congo$ OR Cuba$ OR Djibouti$ OR Dominican Republic$ OR Ecuador$ OR Egypt$ OR El Salvador$ OR Fiji$ OR "Georgia (Republic)" OR Georgian$ OR Guam$ OR Guatemal$ OR Guyana$ OR Hondur$ OR Indian Ocean Island$ OR Indonesia$ OR Iran$ OR Iraq$ OR Jamaica$ OR Jordan$ OR Lesotho OR "Macedonia (Republic)" OR Marshall Island$ OR Micronesia$ OR Middle East$ OR Moldova$ OR Morocc$ OR Namibia$ OR Nicaragua$ OR Paraguay$ OR Peru$ OR Philippin$ OR Samoa$ OR Sri Lanka$ OR Suriname$ OR Swaziland$ OR Syria$ OR Thai$ OR Tonga$ OR Tunisia$ OR Turkmen$ OR Ukrain$ OR Vanuatu$).sh,tw. OR Bosnia$.tw. OR Cape Verd$.tw. OR Gaza.tw. OR Georgia$.tw. OR Kiribati$.tw. OR Macedonia$.tw. OR Maldives.tw. OR Marshall Island$.tw. OR Palestin$.tw. OR Syrian Arab Republic$.tw. OR West Bank.tw.
(Afghan$ OR Bangladesh$ OR Benin$ OR Burkina Faso$ OR Burundi$ OR Cambodia$ OR Central African Republic$ OR Chad$ OR Comoros OR "Democratic Republic of the Congo" OR Cote d Ivoire OR Eritrea$ OR Ethiopia$ OR Gambia$ OR Ghana$ OR Guinea$ OR Guinea‐Bissau OR Haiti$ OR India$ OR Kenya$ OR Korea$ OR Kyrgyz$ OR Laos OR Laot$ OR Liberia$ OR Madagascar OR Malagasy OR Malawi$ OR Mali$ OR Mauritania$ OR Melanesia$ OR Mongolia$ OR Mozambi$ OR Myanmar OR Nepal$ OR Niger$ OR Nigeria$ OR Pakistan$ OR Papua New Guinea$ OR Rwanda$ OR Senegal$ OR Sierra Leone$ OR Somalia$ OR Sudan$ OR Tajikistan$ OR Tanzania$ OR East Timor$ OR Togo$ OR Uganda$ OR Uzbek$ OR Vietnam$ OR Yemen$ OR Zambia$ OR Zimbabw$).sh,tw. OR Burm$.tw. OR Congo$.tw. OR Lao.tw. OR North Korea$.tw. OR Solomon Island$.tw. OR Sao Tome.tw. OR Timor$.tw. OR Viet Nam$.tw. OR vietnam$.tw. OR ivory coast.tw.
EMBASE
6 May 2014
5,210 records
Interventon terms
'maternal welfare'/de OR 'policy'/de OR 'social welfare'/de OR 'social security'/exp OR (social NEAR/1 (assistance OR polic* OR welfare OR insurance* OR protection)):ti,ab OR 'public assistance':ti,ab OR 'family policy':ti,ab OR ((financial OR cash OR pay* OR monetary OR money) NEAR/3 (transfer* OR measure* OR incentive* OR allowance* OR exclu* OR reform* OR gain* OR credit OR credits OR benefit OR benefits)):ti,ab
Study terms
'clinical trial'/exp OR 'placebo'/de OR 'single blind procedure'/de OR 'double blind procedure'/de OR 'control group'/de OR 'comparative study'/de OR 'intervention study'/de OR 'cohort analysis'/exp OR 'evaluation study'/exp OR random*:ti,ab OR 'random allocation':ti,ab OR placebo*:ti,ab OR ((single OR double OR triple OR treble) NEAR/1 blind*):ti,ab OR (time NEAR/1 series):ti,ab OR (quasi NEXT/1 experiment*):ti,ab OR ('pre test' OR pretest OR 'pre‐intervention' OR 'post test' OR posttest OR 'post‐intervention'):ti,ab OR 'controlled before':ti,ab OR 'independent panel':ti,ab OR ((panel OR intervention* OR evaluat* OR compari*) NEXT/1 stud*):ti,ab OR 'before and after':ti,ab OR (repeat* NEXT/1 measure*):ti,ab OR trial OR ('follow up' NEXT/1 assessment*):ti,ab OR groups:ti,ab OR ((intervention OR interventional OR process OR program) NEAR/8 (evaluat* OR effect* OR outcome*)):ti,ab OR program:ti,ab OR programme:ti,ab OR (secondary NEXT/1 analys*):ti,ab OR ((evaluat* OR intervention* OR treatment*) AND (control* OR study OR program* OR comparison OR comparative)):ti,ab
Countries terms
'developing country'/exp OR 'Africa'/exp OR 'Asia'/exp OR 'South and Central America'/exp OR (Africa OR Asia OR 'South America' OR 'Latin America' OR 'Central America'):ti,ab OR ((developing OR 'less developed' OR 'third world' OR 'under developed' OR 'middle income' OR 'low income' OR underserved OR 'under served' OR deprived OR poor*) NEXT/1 (count* OR nation? OR state? OR population?)):ti,ab OR (lmic OR lmics):ti,ab
OR
(Samoa* OR Argentin* OR Beliz* OR Botswana* OR Brazil* OR Bulgaria* OR Chile* OR Comoro* OR (Costa NEXT/1 Rica*) OR Croatia* OR Dominica* OR Guinea* OR Gabon* OR Grenada* OR Hungar* OR Kazakh* OR Latvia* OR Leban* OR Libya* OR Lithuania* OR Malaysia* OR Mauriti* OR Mexic* OR Micronesia* OR Montenegr* OR Oman* OR Palau* OR Panama* OR Poland OR Polish OR Romania* OR Russia* OR Seychelles* OR Slovak* OR South Africa* OR 'Saint Kitts' OR Nevis OR (Saint NEXT/1 Lucia*) OR (Saint NEXT/1 Vincent*) OR Grenada* OR Turk* OR Urugua* OR Venezuel* OR Yugoslavia* OR Libia* OR Mayotte OR 'Northern Mariana' OR mariana* OR Russia* OR Serbia* OR 'St Kitts' OR 'St Lucia' OR 'st lucian' OR 'St Vincent'):ab,de,ti
OR
(Albania* OR Algeria* OR Angol* OR Armenia* OR Azerbaijan* OR Belarus* OR Bhutan* OR Bolivia* OR Bosnia* OR Herzegovina* OR Cameroon* OR China OR Chinese OR Colombia* OR Congo* OR Cuba* OR Djibouti* OR Dominica* OR Ecuador* OR Egypt* OR Salvador* OR Fiji* OR Georgia OR georgian* OR Guam* OR Guatemal* OR Guyana* OR Hondur* OR Indonesia* OR Iran* OR Iraq* OR Jamaica* OR Jordan* OR Lesoth* OR Macedonia* OR (Marshall NEXT/1 Island*) OR Micronesia* OR (Middle NEXT/1 East*) OR Moldova* OR Morocc* OR Namibia* OR Nicaragua* OR Paraguay* OR Peru* OR Philippin* OR (Sri NEXT/1 Lanka*) OR Suriname* OR Swaziland* OR Syria* OR Thai* OR Tonga* OR Tunisia* OR Turkmen* OR Ukrain* OR Vanuatu OR (Cape NEXT/1 Verd*) OR Gaza OR Kiribati* OR Maldives OR (Marshall NEXT/1 Island*) OR Palestin* OR 'West Bank'):ab,de,ti
OR
(Afghan* OR Bangladesh* OR Benin* OR (Burkina NEXT/1 Faso*) OR Burundi* OR Cambodia* OR 'Central African Republic' OR Chad* OR Comoros OR Congo OR 'Cote d Ivoire' OR 'Ivory Coast' OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Haiti* OR India* OR Kenya* OR Korea* OR Kyrgyz* OR Laos OR Laot* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali OR Malian OR Mauritania* OR Melanesia* OR Mongolia* OR Mozambi* OR Myanmar OR Nepal* OR Niger* OR Nigeria* OR Pakistan* OR Rwanda* OR Senegal* OR (Sierra NEXT/1 Leone*) OR Somalia* OR Sudan* OR Tajikistan* OR Tanzania* OR Togo* OR Uganda* OR Uzbek* OR Vietnam* OR Yemen* OR Zambia* OR Zimbabw* OR Burm*.tw. OR (Salomon NEXT/1 Island*) OR 'Sao Tome' OR (Viet NEXT/1 Nam) OR vietnam*):ab,de,ti
Academic Search Premier
13 May 2014
2,002 records
Intervention terms
SU ("PUBLIC welfare" OR "CONDITIONAL cash transfer programs" OR "SOCIAL security" OR "SUPPLEMENTAL security income program" OR "MATERNAL & infant welfare") OR TI ((social N1 (assistance OR polic* OR welfare OR insurance* OR protection)) OR "public assistance" OR "family policy" OR ((financial OR cash OR pay* OR monetary OR money) N3 (transfer* OR measure* OR incentive* OR allowance* OR exclu* OR reform* OR gain* OR credit OR credits OR benefit OR benefits))) OR AB ((social N1 (assistance OR polic* OR welfare OR insurance* OR protection)) OR "public assistance" OR "family policy" OR ((financial OR cash OR pay* OR monetary OR money) N3 (transfer* OR measure* OR incentive* OR allowance* OR exclu* OR reform* OR gain* OR credit OR credits OR benefit OR benefits)))
Study terms
SU ("RANDOMIZED controlled trials" OR "PLACEBOS (Medicine)" OR "BLIND experiment" OR "CONTROL groups (Research)" OR "CLINICAL trials" OR "COHORT analysis" OR "LONGITUDINAL method" OR "RETROSPECTIVE studies" OR "EVALUATION") OR TI (random* OR placebo* OR ((single OR double OR triple OR treble) N1 blind*) OR (time N1 series) OR "quasi‐experiment*" OR "pre test" OR pretest OR "pre‐intervention" OR "post test" OR posttest OR "post‐intervention" OR "controlled before" OR "independent panel" OR "panel stud* OR "intervention* stud*" OR "before and after" OR "repeat* measure* OR "evaluat* stud*" OR "compari* stud*" OR trial OR "follow‐up assessment*" OR groups OR ((intervention OR interventional OR process OR program) N8 (evaluat* OR effect* OR outcome*)) OR program OR programme OR "secondary analys*" OR ((evaluat* OR intervention* OR treatment*) and (control* OR study OR program* OR comparison OR comparative))) OR AB (random* OR placebo* OR ((single OR double OR triple OR treble) N1 blind*) OR (time N1 series) OR "quasi‐experiment*" OR "pre test" OR pretest OR "pre‐intervention" OR "post test" OR posttest OR "post‐intervention" OR "controlled before" OR "independent panel" OR "panel stud* OR "intervention* stud*" OR "before and after" OR "repeat* measure* OR "evaluat* stud*" OR "compari* stud*" OR trial OR "follow‐up assessment*" OR groups OR ((intervention OR interventional OR process OR program) N8 (evaluat* OR effect* OR outcome*)) OR program OR programme OR "secondary analys*" OR ((evaluat* OR intervention* OR treatment*) AND (control* OR study OR program* OR comparison OR comparative)))
Countries terms
SU ("Developing Countries" OR "Medically Underserved Area" OR "Africa" OR "Asia" OR "South America" OR "Central America" OR "Latin America") OR TI (Africa OR Asia OR "South America" OR "Latin America" OR "Central America" OR ((developing OR "less* developed" OR "third world" OR "under developed" OR "middle income" OR "low income" OR underserved OR "under served" OR deprived OR poor*) N1 (count* OR nation OR nations OR state OR states OR population OR populations)) OR lmic OR lmics) OR AB (Africa OR Asia OR "South America" OR "Latin America" OR "Central America" OR ((developing OR "less* developed" OR "third world" OR "under developed" OR "middle income" OR "low income" OR underserved OR "under served" OR deprived OR poor*) N1 (count* OR nation OR nations OR state OR states OR population OR populations)) OR lmic OR lmics)
OR
TI(Samoa* OR Argentin* OR Beliz* OR Botswana* OR Brazil* OR Bulgaria* OR Chile* OR Comoro* OR "Costa Rica*" OR Croatia* OR Dominica* OR Guinea* OR Gabon* OR Grenada* OR Hungar* OR Kazakh* OR Latvia* OR Leban* OR Libya* OR Lithuania* OR Malaysia* OR Mauriti* OR Mexic* OR Micronesia* OR Montenegr* OR Oman* OR Palau* OR Panama* OR Poland OR Polish OR Romania* OR Russia* OR Seychelles* OR Slovak* OR "Saint Kitts" OR Nevis OR "Saint Lucia*" OR "Saint Vincent" OR Grenadines OR Turk* OR Urugua* OR Venezuel* OR Yugoslavia* OR Libia* OR Mayotte OR "Mariana Island*" OR Serbia* OR "St Kitts" OR "St Lucia*" OR "St Vincent" OR Albania* OR Algeria* OR Angol* OR Armenia* OR Azerbaijan* OR Belarus* OR Bhutan* OR Bolivia* OR Bosnia* OR Herzegovin* OR Cameroon* OR China OR Chinese OR Colombia* OR Congo* OR Cuba* OR Djibouti* OR Ecuador* OR Egypt* OR "El Salvador*" OR Fiji* OR Georgia* OR Guam* OR Guatemal* OR Guyana* OR Hondur* OR "Indian Ocean Island*" OR Indonesia* OR Iran* OR Iraq* OR Jamaica* OR Jordan* OR Lesotho OR Macedonia* OR "Marshall Island*" OR Micronesia* OR "Middle East*" OR Moldova* OR Morocc* OR Namibia* OR Nicaragua* OR Paraguay* OR Peru* OR Philippin* OR "Sri Lanka*" OR Suriname* OR Swaziland* OR Syria* OR Thai* OR Tonga* OR Tunisia* OR Turkmen* OR Ukrain* OR Vanuatu* OR "Cape Verd*" OR Gaza OR Kiribati* OR Maldives OR Palestin* OR "West Bank" OR Afghan* OR Bangladesh* OR Benin* OR "Burkina Faso*" OR Burundi* OR Cambodia* OR "Central African Republic*" OR Chad* OR Comoros OR Congo* OR "Cote d Ivoire" OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea* OR "Guinea‐Bissau" OR Haiti* OR India* OR Kenya* OR Korea* OR Kyrgyz* OR Laos OR Laot* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Melanesia* OR Mongolia* OR Mozambi* OR Myanmar OR Nepal* OR Niger* OR Nigeria* OR Pakistan* OR "Papua New Guinea*" OR Rwanda* OR Senegal* OR "Sierra Leone*" OR Somalia* OR Sudan* OR Tajikistan* OR Tanzania* OR "East Timor*" OR Togo* OR Uganda* OR Uzbek* OR Vietnam* OR Yemen* OR Zambia* OR Zimbabw* OR Burm* OR Lao* OR "North Korea*" OR "Solomon Island*" OR "Sao Tome" OR Timor* OR "Viet Nam*" OR "ivory coast")
OR
AB(Samoa* OR Argentin* OR Beliz* OR Botswana* OR Brazil* OR Bulgaria* OR Chile* OR Comoro* OR "Costa Rica*" OR Croatia* OR Dominica* OR Guinea* OR Gabon* OR Grenada* OR Hungar* OR Kazakh* OR Latvia* OR Leban* OR Libya* OR Lithuania* OR Malaysia* OR Mauriti* OR Mexic* OR Micronesia* OR Montenegr* OR Oman* OR Palau* OR Panama* OR Poland OR Polish OR Romania* OR Russia* OR Seychelles* OR Slovak* OR "Saint Kitts" OR Nevis OR "Saint Lucia*" OR "Saint Vincent" OR Grenadines OR Turk* OR Urugua* OR Venezuel* OR Yugoslavia* OR Libia* OR Mayotte OR "Mariana Island*" OR Serbia* OR "St Kitts" OR "St Lucia*" OR "St Vincent" OR Albania* OR Algeria* OR Angol* OR Armenia* OR Azerbaijan* OR Belarus* OR Bhutan* OR Bolivia* OR Bosnia* OR Herzegovin* OR Cameroon* OR China OR Chinese OR Colombia* OR Congo* OR Cuba* OR Djibouti* OR Ecuador* OR Egypt* OR "El Salvador*" OR Fiji* OR Georgia* OR Guam* OR Guatemal* OR Guyana* OR Hondur* OR "Indian Ocean Island*" OR Indonesia* OR Iran* OR Iraq* OR Jamaica* OR Jordan* OR Lesotho OR Macedonia* OR "Marshall Island*" OR Micronesia* OR "Middle East*" OR Moldova* OR Morocc* OR Namibia* OR Nicaragua* OR Paraguay* OR Peru* OR Philippin* OR "Sri Lanka*" OR Suriname* OR Swaziland* OR Syria* OR Thai* OR Tonga* OR Tunisia* OR Turkmen* OR Ukrain* OR Vanuatu* OR "Cape Verd*" OR Gaza OR Kiribati* OR Maldives OR Palestin* OR "West Bank" OR Afghan* OR Bangladesh* OR Benin* OR "Burkina Faso*" OR Burundi* OR Cambodia* OR "Central African Republic*" OR Chad* OR Comoros OR Congo* OR "Cote d Ivoire" OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea* OR "Guinea‐Bissau" OR Haiti* OR India* OR Kenya* OR Korea* OR Kyrgyz* OR Laos OR Laot* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Melanesia* OR Mongolia* OR Mozambi* OR Myanmar OR Nepal* OR Niger* OR Nigeria* OR Pakistan* OR "Papua New Guinea*" OR Rwanda* OR Senegal* OR "Sierra Leone*" OR Somalia* OR Sudan* OR Tajikistan* OR Tanzania* OR "East Timor*" OR Togo* OR Uganda* OR Uzbek* OR Vietnam* OR Yemen* OR Zambia* OR Zimbabw* OR Burm* OR Lao* OR "North Korea*" OR "Solomon Island*" OR "Sao Tome" OR Timor* OR "Viet Nam*" OR "ivory coast")
OR
SU (Samoa* OR Argentin* OR Beliz* OR Botswana* OR Brazil* OR Bulgaria* OR Chile* OR Comoro* OR "Costa Rica*" OR Croatia* OR Dominica* OR Guinea* OR Gabon* OR Grenada* OR Hungar* OR Kazakh* OR Latvia* OR Leban* OR Libya* OR Lithuania* OR Malaysia* OR Mauriti* OR Mexic* OR Micronesia* OR Montenegr* OR Oman* OR Palau* OR Panama* OR Poland OR Polish OR Romania* OR Russia* OR Seychelles* OR Slovak* OR "Saint Kitts" OR Nevis OR "Saint Lucia*" OR "Saint Vincent" OR Grenadines OR Turk* OR Urugua* OR Venezuel* OR Yugoslavia* OR Libia* OR Mayotte OR "Mariana Island*" OR Serbia* OR "St Kitts" OR "St Lucia*" OR "St Vincent" OR Albania* OR Algeria* OR Angol* OR Armenia* OR Azerbaijan* OR Belarus* OR Bhutan* OR Bolivia* OR Bosnia* OR Herzegovin* OR Cameroon* OR China OR Chinese OR Colombia* OR Congo* OR Cuba* OR Djibouti* OR Ecuador* OR Egypt* OR "El Salvador*" OR Fiji* OR Georgia* OR Guam* OR Guatemal* OR Guyana* OR Hondur* OR "Indian Ocean Island*" OR Indonesia* OR Iran* OR Iraq* OR Jamaica* OR Jordan* OR Lesotho OR Macedonia* OR "Marshall Island*" OR Micronesia* OR "Middle East*" OR Moldova* OR Morocc* OR Namibia* OR Nicaragua* OR Paraguay* OR Peru* OR Philippin* OR "Sri Lanka*" OR Suriname* OR Swaziland* OR Syria* OR Thai* OR Tonga* OR Tunisia* OR Turkmen* OR Ukrain* OR Vanuatu* OR "Cape Verd*" OR Gaza OR Kiribati* OR Maldives OR Palestin* OR "West Bank" OR Afghan* OR Bangladesh* OR Benin* OR "Burkina Faso*" OR Burundi* OR Cambodia* OR "Central African Republic*" OR Chad* OR Comoros OR Congo* OR "Cote d Ivoire" OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea* OR "Guinea‐Bissau" OR Haiti* OR India* OR Kenya* OR Korea* OR Kyrgyz* OR Laos OR Laot* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Melanesia* OR Mongolia* OR Mozambi* OR Myanmar OR Nepal* OR Niger* OR Nigeria* OR Pakistan* OR "Papua New Guinea*" OR Rwanda* OR Senegal* OR "Sierra Leone*" OR Somalia* OR Sudan* OR Tajikistan* OR Tanzania* OR "East Timor*" OR Togo* OR Uganda* OR Uzbek* OR Vietnam* OR Yemen* OR Zambia* OR Zimbabw* OR Burm* OR Lao* OR "North Korea*" OR "Solomon Island*" OR "Sao Tome" OR Timor* OR "Viet Nam*" OR "ivory coast")
Business Source Complete
14 May 2014
1,592 records
Intervention terms
DE ("PUBLIC welfare" OR "INCOME maintenance programs" OR "SUPPLEMENTAL security income program" OR "SOCIAL security") OR TI ((social N1 (assistance OR polic* OR welfare OR insurance* OR protection)) OR "public assistance" OR "family policy" OR ((financial OR cash OR pay* OR monetary OR money) N3 (transfer* OR measure* OR incentive* OR allowance* OR exclu* OR reform* OR gain* OR credit OR credits OR benefit OR benefits))) OR AB ((social N1 (assistance OR polic* OR welfare OR insurance* OR protection)) OR "public assistance" OR "family policy" OR ((financial OR cash OR pay* OR monetary OR money) N3 (transfer* OR measure* OR incentive* OR allowance* OR exclu* OR reform* OR gain* OR credit OR credits OR benefit OR benefits)))
Study terms
TI (random* OR placebo* OR ((single OR double OR triple OR treble) N1 blind*) OR (time N1 series) OR "quasi‐experiment*" OR "pre test" OR pretest OR "pre‐intervention" OR "post test" OR posttest OR "post‐intervention" OR "controlled before" OR "independent panel" OR "panel stud* OR "intervention* stud*" OR "before and after" OR "repeat* measure* OR "evaluat* stud*" OR "compari* stud*" OR trial OR "follow‐up assessment*" OR groups OR ((intervention OR interventional OR process OR program) N8 (evaluat* OR effect* OR outcome*)) OR program OR programme OR "secondary analys*" OR ((evaluat* OR intervention* OR treatment*) and (control* OR study OR program* OR comparison OR comparative))) OR AB (random* OR placebo* OR ((single OR double OR triple OR treble) N1 blind*) OR (time N1 series) OR "quasi‐experiment*" OR "pre test" OR pretest OR "pre‐intervention" OR "post test" OR posttest OR "post‐intervention" OR "controlled before" OR "independent panel" OR "panel stud* OR "intervention* stud*" OR "before and after" OR "repeat* measure* OR "evaluat* stud*" OR "compari* stud*" OR trial OR "follow‐up assessment*" OR groups OR ((intervention OR interventional OR process OR program) N8 (evaluat* OR effect* OR outcome*)) OR program OR programme OR "secondary analys*" OR ((evaluat* OR intervention* OR treatment*) AND (control* OR study OR program* OR comparison OR comparative)))
Countries terms
DE ("Africa" OR "Asia" OR "South America" OR "Central America" OR "Latin America") OR TI (Africa OR Asia OR "South America" OR "Latin America" OR "Central America" OR ((developing OR "less* developed" OR "third world" OR "under developed" OR "middle income" OR "low income" OR underserved OR "under served" OR deprived OR poor*) N1 (count* OR nation OR nations OR state OR states OR population OR populations)) OR lmic OR lmics) OR AB (Africa OR Asia OR "South America" OR "Latin America" OR "Central America" OR ((developing OR "less* developed" OR "third world" OR "under developed" OR "middle income" OR "low income" OR underserved OR "under served" OR deprived OR poor*) N1 (count* OR nation OR nations OR state OR states OR population OR populations)) OR lmic OR lmics)
OR
TI(Samoa* OR Argentin* OR Beliz* OR Botswana* OR Brazil* OR Bulgaria* OR Chile* OR Comoro* OR "Costa Rica*" OR Croatia* OR Dominica* OR Guinea* OR Gabon* OR Grenada* OR Hungar* OR Kazakh* OR Latvia* OR Leban* OR Libya* OR Lithuania* OR Malaysia* OR Mauriti* OR Mexic* OR Micronesia* OR Montenegr* OR Oman* OR Palau* OR Panama* OR Poland OR Polish OR Romania* OR Russia* OR Seychelles* OR Slovak* OR "Saint Kitts" OR Nevis OR "Saint Lucia*" OR "Saint Vincent" OR Grenadines OR Turk* OR Urugua* OR Venezuel* OR Yugoslavia* OR Libia* OR Mayotte OR "Mariana Island*" OR Serbia* OR "St Kitts" OR "St Lucia*" OR "St Vincent" OR Albania* OR Algeria* OR Angol* OR Armenia* OR Azerbaijan* OR Belarus* OR Bhutan* OR Bolivia* OR Bosnia* OR Herzegovin* OR Cameroon* OR China OR Chinese OR Colombia* OR Congo* OR Cuba* OR Djibouti* OR Ecuador* OR Egypt* OR "El Salvador*" OR Fiji* OR Georgia* OR Guam* OR Guatemal* OR Guyana* OR Hondur* OR "Indian Ocean Island*" OR Indonesia* OR Iran* OR Iraq* OR Jamaica* OR Jordan* OR Lesotho OR Macedonia* OR "Marshall Island*" OR Micronesia* OR "Middle East*" OR Moldova* OR Morocc* OR Namibia* OR Nicaragua* OR Paraguay* OR Peru* OR Philippin* OR "Sri Lanka*" OR Suriname* OR Swaziland* OR Syria* OR Thai* OR Tonga* OR Tunisia* OR Turkmen* OR Ukrain* OR Vanuatu* OR "Cape Verd*" OR Gaza OR Kiribati* OR Maldives OR Palestin* OR "West Bank" OR Afghan* OR Bangladesh* OR Benin* OR "Burkina Faso*" OR Burundi* OR Cambodia* OR "Central African Republic*" OR Chad* OR Comoros OR Congo* OR "Cote d Ivoire" OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea* OR "Guinea‐Bissau" OR Haiti* OR India* OR Kenya* OR Korea* OR Kyrgyz* OR Laos OR Laot* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Melanesia* OR Mongolia* OR Mozambi* OR Myanmar OR Nepal* OR Niger* OR Nigeria* OR Pakistan* OR "Papua New Guinea*" OR Rwanda* OR Senegal* OR "Sierra Leone*" OR Somalia* OR Sudan* OR Tajikistan* OR Tanzania* OR "East Timor*" OR Togo* OR Uganda* OR Uzbek* OR Vietnam* OR Yemen* OR Zambia* OR Zimbabw* OR Burm* OR Lao* OR "North Korea*" OR "Solomon Island*" OR "Sao Tome" OR Timor* OR "Viet Nam*" OR "ivory coast")
OR
AB(Samoa* OR Argentin* OR Beliz* OR Botswana* OR Brazil* OR Bulgaria* OR Chile* OR Comoro* OR "Costa Rica*" OR Croatia* OR Dominica* OR Guinea* OR Gabon* OR Grenada* OR Hungar* OR Kazakh* OR Latvia* OR Leban* OR Libya* OR Lithuania* OR Malaysia* OR Mauriti* OR Mexic* OR Micronesia* OR Montenegr* OR Oman* OR Palau* OR Panama* OR Poland OR Polish OR Romania* OR Russia* OR Seychelles* OR Slovak* OR "Saint Kitts" OR Nevis OR "Saint Lucia*" OR "Saint Vincent" OR Grenadines OR Turk* OR Urugua* OR Venezuel* OR Yugoslavia* OR Libia* OR Mayotte OR "Mariana Island*" OR Serbia* OR "St Kitts" OR "St Lucia*" OR "St Vincent" OR Albania* OR Algeria* OR Angol* OR Armenia* OR Azerbaijan* OR Belarus* OR Bhutan* OR Bolivia* OR Bosnia* OR Herzegovin* OR Cameroon* OR China OR Chinese OR Colombia* OR Congo* OR Cuba* OR Djibouti* OR Ecuador* OR Egypt* OR "El Salvador*" OR Fiji* OR Georgia* OR Guam* OR Guatemal* OR Guyana* OR Hondur* OR "Indian Ocean Island*" OR Indonesia* OR Iran* OR Iraq* OR Jamaica* OR Jordan* OR Lesotho OR Macedonia* OR "Marshall Island*" OR Micronesia* OR "Middle East*" OR Moldova* OR Morocc* OR Namibia* OR Nicaragua* OR Paraguay* OR Peru* OR Philippin* OR "Sri Lanka*" OR Suriname* OR Swaziland* OR Syria* OR Thai* OR Tonga* OR Tunisia* OR Turkmen* OR Ukrain* OR Vanuatu* OR "Cape Verd*" OR Gaza OR Kiribati* OR Maldives OR Palestin* OR "West Bank" OR Afghan* OR Bangladesh* OR Benin* OR "Burkina Faso*" OR Burundi* OR Cambodia* OR "Central African Republic*" OR Chad* OR Comoros OR Congo* OR "Cote d Ivoire" OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea* OR "Guinea‐Bissau" OR Haiti* OR India* OR Kenya* OR Korea* OR Kyrgyz* OR Laos OR Laot* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Melanesia* OR Mongolia* OR Mozambi* OR Myanmar OR Nepal* OR Niger* OR Nigeria* OR Pakistan* OR "Papua New Guinea*" OR Rwanda* OR Senegal* OR "Sierra Leone*" OR Somalia* OR Sudan* OR Tajikistan* OR Tanzania* OR "East Timor*" OR Togo* OR Uganda* OR Uzbek* OR Vietnam* OR Yemen* OR Zambia* OR Zimbabw* OR Burm* OR Lao* OR "North Korea*" OR "Solomon Island*" OR "Sao Tome" OR Timor* OR "Viet Nam*" OR "ivory coast")
OR
SU(Samoa* OR Argentin* OR Beliz* OR Botswana* OR Brazil* OR Bulgaria* OR Chile* OR Comoro* OR "Costa Rica*" OR Croatia* OR Dominica* OR Guinea* OR Gabon* OR Grenada* OR Hungar* OR Kazakh* OR Latvia* OR Leban* OR Libya* OR Lithuania* OR Malaysia* OR Mauriti* OR Mexic* OR Micronesia* OR Montenegr* OR Oman* OR Palau* OR Panama* OR Poland OR Polish OR Romania* OR Russia* OR Seychelles* OR Slovak* OR "Saint Kitts" OR Nevis OR "Saint Lucia*" OR "Saint Vincent" OR Grenadines OR Turk* OR Urugua* OR Venezuel* OR Yugoslavia* OR Libia* OR Mayotte OR "Mariana Island*" OR Serbia* OR "St Kitts" OR "St Lucia*" OR "St Vincent" OR Albania* OR Algeria* OR Angol* OR Armenia* OR Azerbaijan* OR Belarus* OR Bhutan* OR Bolivia* OR Bosnia* OR Herzegovin* OR Cameroon* OR China OR Chinese OR Colombia* OR Congo* OR Cuba* OR Djibouti* OR Ecuador* OR Egypt* OR "El Salvador*" OR Fiji* OR Georgia* OR Guam* OR Guatemal* OR Guyana* OR Hondur* OR "Indian Ocean Island*" OR Indonesia* OR Iran* OR Iraq* OR Jamaica* OR Jordan* OR Lesotho OR Macedonia* OR "Marshall Island*" OR Micronesia* OR "Middle East*" OR Moldova* OR Morocc* OR Namibia* OR Nicaragua* OR Paraguay* OR Peru* OR Philippin* OR "Sri Lanka*" OR Suriname* OR Swaziland* OR Syria* OR Thai* OR Tonga* OR Tunisia* OR Turkmen* OR Ukrain* OR Vanuatu* OR "Cape Verd*" OR Gaza OR Kiribati* OR Maldives OR Palestin* OR "West Bank" OR Afghan* OR Bangladesh* OR Benin* OR "Burkina Faso*" OR Burundi* OR Cambodia* OR "Central African Republic*" OR Chad* OR Comoros OR Congo* OR "Cote d Ivoire" OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea* OR "Guinea‐Bissau" OR Haiti* OR India* OR Kenya* OR Korea* OR Kyrgyz* OR Laos OR Laot* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Melanesia* OR Mongolia* OR Mozambi* OR Myanmar OR Nepal* OR Niger* OR Nigeria* OR Pakistan* OR "Papua New Guinea*" OR Rwanda* OR Senegal* OR "Sierra Leone*" OR Somalia* OR Sudan* OR Tajikistan* OR Tanzania* OR "East Timor*" OR Togo* OR Uganda* OR Uzbek* OR Vietnam* OR Yemen* OR Zambia* OR Zimbabw* OR Burm* OR Lao* OR "North Korea*" OR "Solomon Island*" OR "Sao Tome" OR Timor* OR "Viet Nam*" OR "ivory coast")
CINAHL
07 May 2014
527 records
Intervention terms
MH ("Maternal Welfare" OR " Social Welfare +" OR "Economic and Social Security") OR TI ((social N1 (assistance OR polic* OR welfare OR insurance* OR protection)) OR "public assistance" OR "family policy" OR ((financial OR cash OR pay* OR monetary OR money) N3 (transfer* OR measure* OR incentive* OR allowance* OR exclu* OR reform* OR gain* OR credit OR credits OR benefit OR benefits))) OR AB ((social N1 (assistance OR polic* OR welfare OR insurance* OR protection)) OR "public assistance" OR "family policy" OR ((financial OR cash OR pay* OR monetary OR money) N3 (transfer* OR measure* OR incentive* OR allowance* OR exclu* OR reform* OR gain* OR credit OR credits OR benefit OR benefits)))
Study terms
MH ("clinical trials+" OR "Random Assignment" OR "Placebos" OR "Control Group" OR "Comparative Studies" OR "Prospective Studies+" OR "Evaluation Research+" OR "Program Evaluation") OR TI (random* OR placebo* OR ((single OR double OR triple OR treble) N1 blind*) OR (time N1 series) OR "quasi‐experiment*" OR "pre test" OR pretest OR "pre‐intervention" OR "post test" OR posttest OR "post‐intervention" OR "controlled before" OR "independent panel" OR "panel stud* OR "intervention* stud*" OR "before and after" OR "repeat* measure* OR "evaluat* stud*" OR "compari* stud*" OR trial OR "follow‐up assessment*" OR groups OR ((intervention OR interventional OR process OR program) N8 (evaluat* OR effect* OR outcome*)) OR program OR programme OR "secondary analys*" OR ((evaluat* OR intervention* OR treatment*) and (control* OR study OR program* OR comparison OR comparative))) OR AB (random* OR placebo* OR ((single OR double OR triple OR treble) N1 blind*) OR (time N1 series) OR "quasi‐experiment*" OR "pre test" OR pretest OR "pre‐intervention" OR "post test" OR posttest OR "post‐intervention" OR "controlled before" OR "independent panel" OR "panel stud* OR "intervention* stud*" OR "before and after" OR "repeat* measure* OR "evaluat* stud*" OR "compari* stud*" OR trial OR "follow‐up assessment*" OR groups OR ((intervention OR interventional OR process OR program) N8 (evaluat* OR effect* OR outcome*)) OR program OR programme OR "secondary analys*" OR ((evaluat* OR intervention* OR treatment*) and (control* OR study OR program* OR comparison OR comparative)))
Countries terms
MH ("Developing Countries" OR "Medically Underserved Area" OR "Africa+" OR "Asia+" OR "South America+" OR "Central America+" OR "Latin America") OR TI (Africa OR Asia OR "South America" OR "Latin America" OR "Central America" OR ((developing OR "less* developed" OR "third world" OR "under developed" OR "middle income" OR "low income" OR underserved OR "under served" OR deprived OR poor*) N1 (count* OR nation OR nations OR state OR states OR population OR populations)) OR lmic OR lmics) OR AB (Africa OR Asia OR "South America" OR "Latin America" OR "Central America" OR ((developing OR "less* developed" OR "third world" OR "under developed" OR "middle income" OR "low income" OR underserved OR "under served" OR deprived OR poor*) N1 (count* OR nation OR nations OR state OR states OR population OR populations)) OR lmic OR lmics)
OR
TI(Samoa* OR Argentin* OR Beliz* OR Botswana* OR Brazil* OR Bulgaria* OR Chile* OR Comoro* OR "Costa Rica*" OR Croatia* OR Dominica* OR Guinea* OR Gabon* OR Grenada* OR Hungar* OR Kazakh* OR Latvia* OR Leban* OR Libya* OR Lithuania* OR Malaysia* OR Mauriti* OR Mexic* OR Micronesia* OR Montenegr* OR Oman* OR Palau* OR Panama* OR Poland OR Polish OR Romania* OR Russia* OR Seychelles* OR Slovak* OR "Saint Kitts" OR Nevis OR "Saint Lucia*" OR "Saint Vincent" OR Grenadines OR Turk* OR Urugua* OR Venezuel* OR Yugoslavia* OR Libia* OR Mayotte OR "Mariana Island*" OR Serbia* OR "St Kitts" OR "St Lucia*" OR "St Vincent" OR Albania* OR Algeria* OR Angol* OR Armenia* OR Azerbaijan* OR Belarus* OR Bhutan* OR Bolivia* OR Bosnia* OR Herzegovin* OR Cameroon* OR China OR Chinese OR Colombia* OR Congo* OR Cuba* OR Djibouti* OR Ecuador* OR Egypt* OR "El Salvador*" OR Fiji* OR Georgia* OR Guam* OR Guatemal* OR Guyana* OR Hondur* OR "Indian Ocean Island*" OR Indonesia* OR Iran* OR Iraq* OR Jamaica* OR Jordan* OR Lesotho OR Macedonia* OR "Marshall Island*" OR Micronesia* OR "Middle East*" OR Moldova* OR Morocc* OR Namibia* OR Nicaragua* OR Paraguay* OR Peru* OR Philippin* OR "Sri Lanka*" OR Suriname* OR Swaziland* OR Syria* OR Thai* OR Tonga* OR Tunisia* OR Turkmen* OR Ukrain* OR Vanuatu* OR "Cape Verd*" OR Gaza OR Kiribati* OR Maldives OR Palestin* OR "West Bank" OR Afghan* OR Bangladesh* OR Benin* OR "Burkina Faso*" OR Burundi* OR Cambodia* OR "Central African Republic*" OR Chad* OR Comoros OR Congo* OR "Cote d Ivoire" OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea* OR "Guinea‐Bissau" OR Haiti* OR India* OR Kenya* OR Korea* OR Kyrgyz* OR Laos OR Laot* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Melanesia* OR Mongolia* OR Mozambi* OR Myanmar OR Nepal* OR Niger* OR Nigeria* OR Pakistan* OR "Papua New Guinea*" OR Rwanda* OR Senegal* OR "Sierra Leone*" OR Somalia* OR Sudan* OR Tajikistan* OR Tanzania* OR "East Timor*" OR Togo* OR Uganda* OR Uzbek* OR Vietnam* OR Yemen* OR Zambia* OR Zimbabw* OR Burm* OR Lao.tw. OR "North Korea*" OR "Solomon Island*" OR "Sao Tome" OR Timor* OR "Viet Nam*" OR "ivory coast")
OR
AB(Samoa* OR Argentin* OR Beliz* OR Botswana* OR Brazil* OR Bulgaria* OR Chile* OR Comoro* OR "Costa Rica*" OR Croatia* OR Dominica* OR Guinea* OR Gabon* OR Grenada* OR Hungar* OR Kazakh* OR Latvia* OR Leban* OR Libya* OR Lithuania* OR Malaysia* OR Mauriti* OR Mexic* OR Micronesia* OR Montenegr* OR Oman* OR Palau* OR Panama* OR Poland OR Polish OR Romania* OR Russia* OR Seychelles* OR Slovak* OR "Saint Kitts" OR Nevis OR "Saint Lucia*" OR "Saint Vincent" OR Grenadines OR Turk* OR Urugua* OR Venezuel* OR Yugoslavia* OR Libia* OR Mayotte OR "Mariana Island*" OR Serbia* OR "St Kitts" OR "St Lucia*" OR "St Vincent" OR Albania* OR Algeria* OR Angol* OR Armenia* OR Azerbaijan* OR Belarus* OR Bhutan* OR Bolivia* OR Bosnia* OR Herzegovin* OR Cameroon* OR China OR Chinese OR Colombia* OR Congo* OR Cuba* OR Djibouti* OR Ecuador* OR Egypt* OR "El Salvador*" OR Fiji* OR Georgia* OR Guam* OR Guatemal* OR Guyana* OR Hondur* OR "Indian Ocean Island*" OR Indonesia* OR Iran* OR Iraq* OR Jamaica* OR Jordan* OR Lesotho OR Macedonia* OR "Marshall Island*" OR Micronesia* OR "Middle East*" OR Moldova* OR Morocc* OR Namibia* OR Nicaragua* OR Paraguay* OR Peru* OR Philippin* OR "Sri Lanka*" OR Suriname* OR Swaziland* OR Syria* OR Thai* OR Tonga* OR Tunisia* OR Turkmen* OR Ukrain* OR Vanuatu* OR "Cape Verd*" OR Gaza OR Kiribati* OR Maldives OR Palestin* OR "West Bank" OR Afghan* OR Bangladesh* OR Benin* OR "Burkina Faso*" OR Burundi* OR Cambodia* OR "Central African Republic*" OR Chad* OR Comoros OR Congo* OR "Cote d Ivoire" OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea* OR "Guinea‐Bissau" OR Haiti* OR India* OR Kenya* OR Korea* OR Kyrgyz* OR Laos OR Laot* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Melanesia* OR Mongolia* OR Mozambi* OR Myanmar OR Nepal* OR Niger* OR Nigeria* OR Pakistan* OR "Papua New Guinea*" OR Rwanda* OR Senegal* OR "Sierra Leone*" OR Somalia* OR Sudan* OR Tajikistan* OR Tanzania* OR "East Timor*" OR Togo* OR Uganda* OR Uzbek* OR Vietnam* OR Yemen* OR Zambia* OR Zimbabw* OR Burm* OR Lao.tw. OR "North Korea*" OR "Solomon Island*" OR "Sao Tome" OR Timor* OR "Viet Nam*" OR "ivory coast")
OR
MW(Samoa* OR Argentin* OR Beliz* OR Botswana* OR Brazil* OR Bulgaria* OR Chile* OR Comoro* OR "Costa Rica*" OR Croatia* OR Dominica* OR Guinea* OR Gabon* OR Grenada* OR Hungar* OR Kazakh* OR Latvia* OR Leban* OR Libya* OR Lithuania* OR Malaysia* OR Mauriti* OR Mexic* OR Micronesia* OR Montenegr* OR Oman* OR Palau* OR Panama* OR Poland OR Polish OR Romania* OR Russia* OR Seychelles* OR Slovak* OR "Saint Kitts" OR Nevis OR "Saint Lucia*" OR "Saint Vincent" OR Grenadines OR Turk* OR Urugua* OR Venezuel* OR Yugoslavia* OR Libia* OR Mayotte OR "Mariana Island*" OR Serbia* OR "St Kitts" OR "St Lucia*" OR "St Vincent" OR Albania* OR Algeria* OR Angol* OR Armenia* OR Azerbaijan* OR Belarus* OR Bhutan* OR Bolivia* OR Bosnia* OR Herzegovin* OR Cameroon* OR China OR Chinese OR Colombia* OR Congo* OR Cuba* OR Djibouti* OR Ecuador* OR Egypt* OR "El Salvador*" OR Fiji* OR Georgia* OR Guam* OR Guatemal* OR Guyana* OR Hondur* OR "Indian Ocean Island*" OR Indonesia* OR Iran* OR Iraq* OR Jamaica* OR Jordan* OR Lesotho OR Macedonia* OR "Marshall Island*" OR Micronesia* OR "Middle East*" OR Moldova* OR Morocc* OR Namibia* OR Nicaragua* OR Paraguay* OR Peru* OR Philippin* OR "Sri Lanka*" OR Suriname* OR Swaziland* OR Syria* OR Thai* OR Tonga* OR Tunisia* OR Turkmen* OR Ukrain* OR Vanuatu* OR "Cape Verd*" OR Gaza OR Kiribati* OR Maldives OR Palestin* OR "West Bank" OR Afghan* OR Bangladesh* OR Benin* OR "Burkina Faso*" OR Burundi* OR Cambodia* OR "Central African Republic*" OR Chad* OR Comoros OR Congo* OR "Cote d Ivoire" OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea* OR "Guinea‐Bissau" OR Haiti* OR India* OR Kenya* OR Korea* OR Kyrgyz* OR Laos OR Laot* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Melanesia* OR Mongolia* OR Mozambi* OR Myanmar OR Nepal* OR Niger* OR Nigeria* OR Pakistan* OR "Papua New Guinea*" OR Rwanda* OR Senegal* OR "Sierra Leone*" OR Somalia* OR Sudan* OR Tajikistan* OR Tanzania* OR "East Timor*" OR Togo* OR Uganda* OR Uzbek* OR Vietnam* OR Yemen* OR Zambia* OR Zimbabw* OR Burm* OR Lao.tw. OR "North Korea*" OR "Solomon Island*" OR "Sao Tome" OR Timor* OR "Viet Nam*" OR "ivory coast")
EconLit
14 May 2014
1329 records
Intervention terms
ti((social NEAR/1 (assistance OR polic* OR welfare OR insurance* OR protection)) OR "public assistance" OR "family policy" OR ((financial OR cash OR pay* OR monetary OR money) NEAR/3 (transfer* OR measure* OR incentive* OR allowance* OR exclu* OR reform* OR gain* OR credit OR credits OR benefit OR benefits))) OR ab((social NEAR/1 (assistance OR polic* OR welfare OR insurance* OR protection)) OR "public assistance" OR "family policy" OR ((financial OR cash OR pay* OR monetary OR money) NEAR/3 (transfer* OR measure* OR incentive* OR allowance* OR exclu* OR reform* OR gain* OR credit OR credits OR benefit OR benefits)))
Study terms
ti(random* OR placebo* OR ((single OR double OR triple OR treble) NEAR/1 blind*) OR (time NEAR/1 series) OR "quasi‐experiment*" OR "pre test" OR pretest OR "pre‐intervention" OR "post test" OR posttest OR "post‐intervention" OR "controlled before" OR "independent panel" OR "panel stud* OR "intervention* stud*" OR "before and after" OR "repeat* measure* OR "evaluat* stud*" OR "compari* stud*" OR trial OR "follow‐up assessment*" OR groups OR ((intervention OR interventional OR process OR program) NEAR/8 (evaluat* OR effect* OR outcome*)) OR program OR programme OR "secondary analys*" OR ((evaluat* OR intervention* OR treatment*) AND (control* OR study OR program* OR comparison OR comparative))) OR ab(random* OR placebo* OR ((single OR double OR triple OR treble) NEAR/1 blind*) OR (time NEAR/1 series) OR "quasi‐experiment*" OR "pre test" OR pretest OR "pre‐intervention" OR "post test" OR posttest OR "post‐intervention" OR "controlled before" OR "independent panel" OR "panel stud* OR "intervention* stud*" OR "before and after" OR "repeat* measure* OR "evaluat* stud*" OR "compari* stud*" OR trial OR "follow‐up assessment*" OR groups OR ((intervention OR interventional OR process OR program) NEAR/8 (evaluat* OR effect* OR outcome*)) OR program OR programme OR "secondary analys*" OR ((evaluat* OR intervention* OR treatment*) AND (control* OR study OR program* OR comparison OR comparative)))
Countries terms
SU.EXACT("Developing Countries") OR ti(Africa OR Asia OR "South America" OR "Latin America" OR "Central America" OR ((developing OR "less* developed" OR "third world" OR "under developed" OR "middle income" OR "low income" OR underserved OR "under served" OR deprived OR poor*) NEAR/1 (count* OR nation OR nations OR state OR states OR population OR populations)) OR lmic OR lmics) OR ab(Africa OR Asia OR "South America" OR "Latin America" OR "Central America" OR ((developing OR "less* developed" OR "third world" OR "under developed" OR "middle income" OR "low income" OR underserved OR "under served" OR deprived OR poor*) NEAR/1 (count* OR nation OR nations OR state OR states OR population OR populations)) OR lmic OR lmics) OR su(Africa OR Asia OR "South America" OR "Latin America" OR "Central America")
OR
(Samoa* OR Argentin* OR Beliz* OR Botswana* OR Brazil* OR Bulgaria* OR Chile* OR Comoro* OR "Costa Rica*" OR Croatia* OR Dominica* OR Guinea* OR Gabon* OR Grenada* OR Hungar* OR Kazakh* OR Latvia* OR Leban* OR Libya* OR Lithuania* OR Malaysia* OR Mauriti* OR Mexic* OR Micronesia* OR Montenegr* OR Oman* OR Palau* OR Panama* OR Poland OR Polish OR Romania* OR Russia* OR Seychelles* OR Slovak* OR "Saint Kitts" OR Nevis OR "Saint Lucia*" OR "Saint Vincent" OR Grenadines OR Turk* OR Urugua* OR Venezuel* OR Yugoslavia* OR Libia* OR Mayotte OR "Mariana Island*" OR Serbia* OR "St Kitts" OR "St Lucia*" OR "St Vincent" OR Albania* OR Algeria* OR Angol* OR Armenia* OR Azerbaijan* OR Belarus* OR Bhutan* OR Bolivia* OR Bosnia* OR Herzegovin* OR Cameroon* OR China OR Chinese OR Colombia* OR Congo* OR Cuba* OR Djibouti* OR Ecuador* OR Egypt* OR "El Salvador*" OR Fiji* OR Georgia* OR Guam* OR Guatemal* OR Guyana* OR Hondur* OR "Indian Ocean Island*" OR Indonesia* OR Iran* OR Iraq* OR Jamaica* OR Jordan* OR Lesotho OR Macedonia* OR "Marshall Island*" OR Micronesia* OR "Middle East*" OR Moldova* OR Morocc* OR Namibia* OR Nicaragua* OR Paraguay* OR Peru* OR Philippin* OR "Sri Lanka*" OR Suriname* OR Swaziland* OR Syria* OR Thai* OR Tonga* OR Tunisia* OR Turkmen* OR Ukrain* OR Vanuatu* OR "Cape Verd*" OR Gaza OR Kiribati* OR Maldives OR Palestin* OR "West Bank" OR Afghan* OR Bangladesh* OR Benin* OR "Burkina Faso*" OR Burundi* OR Cambodia* OR "Central African Republic*" OR Chad* OR Comoros OR Congo* OR "Cote d Ivoire" OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea* OR "Guinea‐Bissau" OR Haiti* OR India* OR Kenya* OR Korea* OR Kyrgyz* OR Laos OR Laot* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Melanesia* OR Mongolia* OR Mozambi* OR Myanmar OR Nepal* OR Niger* OR Nigeria* OR Pakistan* OR "Papua New Guinea*" OR Rwanda* OR Senegal* OR "Sierra Leone*" OR Somalia* OR Sudan* OR Tajikistan* OR Tanzania* OR "East Timor*" OR Togo* OR Uganda* OR Uzbek* OR Vietnam* OR Yemen* OR Zambia* OR Zimbabw* OR Burm* OR Lao OR "North Korea*" OR "Solomon Island*" OR "Sao Tome" OR Timor* OR "Viet Nam*" OR "ivory coast")
3IE database
9 June 2014 5 records
cash transfer OR financial credit OR financial benefit or financial incentive
PsycINFO
7 May 2014
962 records
Interventions terms
DE ("Welfare Services (Government)" OR "Social Security" OR "Monetary Incentives" OR "Government Programs") OR TI ((social N1 (assistance OR polic* OR welfare OR insurance* OR protection)) OR "public assistance" OR "family policy" OR ((financial OR cash OR pay* OR monetary OR money) N3 (transfer* OR measure* OR incentive* OR allowance* OR exclu* OR reform* OR gain* OR credit OR credits OR benefit OR benefits))) OR AB ((social N1 (assistance OR polic* OR welfare OR insurance* OR protection)) OR "public assistance" OR "family policy" OR ((financial OR cash OR pay* OR monetary OR money) N3 (transfer* OR measure* OR incentive* OR allowance* OR exclu* OR reform* OR gain* OR credit OR credits OR benefit OR benefits)))
Study terms
DE ("Between Groups Design" OR "Clinical Trials" OR "Cohort Analysis" OR "Followup Studies" OR "Longitudinal Studies" OR "Repeated Measures" OR "Between Groups Design" OR "Cohort Analysis" OR "Prospective Studies" OR "Retrospective Studies" OR "Placebo" OR "Experiment Controls" OR "Program Evaluation") OR TI (random* OR placebo* OR ((single OR double OR triple OR treble) N1 blind*) OR (time N1 series) OR "quasi‐experiment*" OR "pre test" OR pretest OR "pre‐intervention" OR "post test" OR posttest OR "post‐intervention" OR "controlled before" OR "independent panel" OR "panel stud* OR "intervention* stud*" OR "before and after" OR "repeat* measure* OR "evaluat* stud*" OR "compari* stud*" OR trial OR "follow‐up assessment*" OR groups OR ((intervention OR interventional OR process OR program) N8 (evaluat* OR effect* OR outcome*)) OR program OR programme OR "secondary analys*" OR ((evaluat* OR intervention* OR treatment*) and (control* OR study OR program* OR comparison OR comparative))) OR AB (random* OR placebo* OR ((single OR double OR triple OR treble) N1 blind*) OR (time N1 series) OR "quasi‐experiment*" OR "pre test" OR pretest OR "pre‐intervention" OR "post test" OR posttest OR "post‐intervention" OR "controlled before" OR "independent panel" OR "panel stud* OR "intervention* stud*" OR "before and after" OR "repeat* measure* OR "evaluat* stud*" OR "compari* stud*" OR trial OR "follow‐up assessment*" OR groups OR ((intervention OR interventional OR process OR program) N8 (evaluat* OR effect* OR outcome*)) OR program OR programme OR "secondary analys*" OR ((evaluat* OR intervention* OR treatment*) and (control* OR study OR program* OR comparison OR comparative)))
Countries terms
DE ("Developing Countries") OR TI (Africa OR Asia OR "South America" OR "Latin America" OR "Central America" OR ((developing OR "less* developed" OR "third world" OR "under developed" OR "middle income" OR "low income" OR underserved OR "under served" OR deprived OR poor*) N1 (count* OR nation OR nations OR state OR states OR population OR populations)) OR lmic OR lmics) OR AB (Africa OR Asia OR "South America" OR "Latin America" OR "Central America" OR ((developing OR "less* developed" OR "third world" OR "under developed" OR "middle income" OR "low income" OR underserved OR "under served" OR deprived OR poor*) N1 (count* OR nation OR nations OR state OR states OR population OR populations)) OR lmic OR lmics) OR KW (Africa OR Asia OR "South America" OR "Latin America" OR "Central America" OR ((developing OR "less* developed" OR "third world" OR "under developed" OR "middle income" OR "low income" OR underserved OR "under served" OR deprived OR poor*) N1 (count* OR nation OR nations OR state OR states OR population OR populations)) OR lmic OR lmics)
OR
TI( Samoa* OR Argentin* OR Beliz* OR Botswana* OR Brazil* OR Bulgaria* OR Chile* OR Comoro* OR "Costa Rica*" OR Croatia* OR Dominica* OR Guinea* OR Gabon* OR Grenada* OR Hungar* OR Kazakh* OR Latvia* OR Leban* OR Libya* OR Lithuania* OR Malaysia* OR Mauriti* OR Mexic* OR Micronesia* OR Montenegr* OR Oman* OR Palau* OR Panama* OR Poland OR Polish OR Romania* OR Russia* OR Seychelles* OR Slovak* OR "Saint Kitts" OR Nevis OR "Saint Lucia*" OR "Saint Vincent" OR Grenadines OR Turk* OR Urugua* OR Venezuel* OR Yugoslavia* OR Libia* OR Mayotte OR "Mariana Island*" OR Serbia* OR "St Kitts" OR "St Lucia*" OR "St Vincent" OR Albania* OR Algeria* OR Angol* OR Armenia* OR Azerbaijan* OR Belarus* OR Bhutan* OR Bolivia* OR Bosnia* OR Herzegovin* OR Cameroon* OR China OR Chinese OR Colombia* OR Congo* OR Cuba* OR Djibouti* OR Ecuador* OR Egypt* OR "El Salvador*" OR Fiji* OR Georgia* OR Guam* OR Guatemal* OR Guyana* OR Hondur* OR "Indian Ocean Island*" OR Indonesia* OR Iran* OR Iraq* OR Jamaica* OR Jordan* OR Lesotho OR Macedonia* OR "Marshall Island*" OR Micronesia* OR "Middle East*" OR Moldova* OR Morocc* OR Namibia* OR Nicaragua* OR Paraguay* OR Peru* OR Philippin* OR "Sri Lanka*" OR Suriname* OR Swaziland* OR Syria* OR Thai* OR Tonga* OR Tunisia* OR Turkmen* OR Ukrain* OR Vanuatu* OR "Cape Verd*" OR Gaza OR Kiribati* OR Maldives OR Palestin* OR "West Bank" OR Afghan* OR Bangladesh* OR Benin* OR "Burkina Faso*" OR Burundi* OR Cambodia* OR "Central African Republic*" OR Chad* OR Comoros OR Congo* OR "Cote d Ivoire" OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea* OR "Guinea‐Bissau" OR Haiti* OR India* OR Kenya* OR Korea* OR Kyrgyz* OR Laos OR Laot* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Melanesia* OR Mongolia* OR Mozambi* OR Myanmar OR Nepal* OR Niger* OR Nigeria* OR Pakistan* OR "Papua New Guinea*" OR Rwanda* OR Senegal* OR "Sierra Leone*" OR Somalia* OR Sudan* OR Tajikistan* OR Tanzania* OR "East Timor*" OR Togo* OR Uganda* OR Uzbek* OR Vietnam* OR Yemen* OR Zambia* OR Zimbabw* OR Burm* OR Lao.tw. OR "North Korea*" OR "Solomon Island*" OR "Sao Tome" OR Timor* OR "Viet Nam*" OR "ivory coast")
OR
AB(Samoa* OR Argentin* OR Beliz* OR Botswana* OR Brazil* OR Bulgaria* OR Chile* OR Comoro* OR "Costa Rica*" OR Croatia* OR Dominica* OR Guinea* OR Gabon* OR Grenada* OR Hungar* OR Kazakh* OR Latvia* OR Leban* OR Libya* OR Lithuania* OR Malaysia* OR Mauriti* OR Mexic* OR Micronesia* OR Montenegr* OR Oman* OR Palau* OR Panama* OR Poland OR Polish OR Romania* OR Russia* OR Seychelles* OR Slovak* OR "Saint Kitts" OR Nevis OR "Saint Lucia*" OR "Saint Vincent" OR Grenadines OR Turk* OR Urugua* OR Venezuel* OR Yugoslavia* OR Libia* OR Mayotte OR "Mariana Island*" OR Serbia* OR "St Kitts" OR "St Lucia*" OR "St Vincent" OR Albania* OR Algeria* OR Angol* OR Armenia* OR Azerbaijan* OR Belarus* OR Bhutan* OR Bolivia* OR Bosnia* OR Herzegovin* OR Cameroon* OR China OR Chinese OR Colombia* OR Congo* OR Cuba* OR Djibouti* OR Ecuador* OR Egypt* OR "El Salvador*" OR Fiji* OR Georgia* OR Guam* OR Guatemal* OR Guyana* OR Hondur* OR "Indian Ocean Island*" OR Indonesia* OR Iran* OR Iraq* OR Jamaica* OR Jordan* OR Lesotho OR Macedonia* OR "Marshall Island*" OR Micronesia* OR "Middle East*" OR Moldova* OR Morocc* OR Namibia* OR Nicaragua* OR Paraguay* OR Peru* OR Philippin* OR "Sri Lanka*" OR Suriname* OR Swaziland* OR Syria* OR Thai* OR Tonga* OR Tunisia* OR Turkmen* OR Ukrain* OR Vanuatu* OR "Cape Verd*" OR Gaza OR Kiribati* OR Maldives OR Palestin* OR "West Bank" OR Afghan* OR Bangladesh* OR Benin* OR "Burkina Faso*" OR Burundi* OR Cambodia* OR "Central African Republic*" OR Chad* OR Comoros OR Congo* OR "Cote d Ivoire" OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea* OR "Guinea‐Bissau" OR Haiti* OR India* OR Kenya* OR Korea* OR Kyrgyz* OR Laos OR Laot* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Melanesia* OR Mongolia* OR Mozambi* OR Myanmar OR Nepal* OR Niger* OR Nigeria* OR Pakistan* OR "Papua New Guinea*" OR Rwanda* OR Senegal* OR "Sierra Leone*" OR Somalia* OR Sudan* OR Tajikistan* OR Tanzania* OR "East Timor*" OR Togo* OR Uganda* OR Uzbek* OR Vietnam* OR Yemen* OR Zambia* OR Zimbabw* OR Burm* OR Lao.tw. OR "North Korea*" OR "Solomon Island*" OR "Sao Tome" OR Timor* OR "Viet Nam*" OR "ivory coast")
OR
KW (Argentin* OR Beliz* OR Botswana* OR Brazil* OR Bulgaria* OR Chile* OR Comoro* OR "Costa Rica*" OR Croatia* OR Dominica* OR Guinea* OR Gabon* OR Grenada* OR Hungar* OR Kazakh* OR Latvia* OR Leban* OR Libya* OR Lithuania* OR Malaysia* OR Mauriti* OR Mexic* OR Micronesia* OR Montenegr* OR Oman* OR Palau* OR Panama* OR Poland OR Polish OR Romania* OR Russia* OR Seychelles* OR Slovak* OR "Saint Kitts" OR Nevis OR "Saint Lucia*" OR "Saint Vincent" OR Grenadines OR Turk* OR Urugua* OR Venezuel* OR Yugoslavia* OR Libia* OR Mayotte OR "Mariana Island*" OR Serbia* OR "St Kitts" OR "St Lucia*" OR "St Vincent" OR Albania* OR Algeria* OR Angol* OR Armenia* OR Azerbaijan* OR Belarus* OR Bhutan* OR Bolivia* OR Bosnia* OR Herzegovin* OR Cameroon* OR China OR Chinese OR Colombia* OR Congo* OR Cuba* OR Djibouti* OR Ecuador* OR Egypt* OR "El Salvador*" OR Fiji* OR Georgia* OR Guam* OR Guatemal* OR Guyana* OR Hondur* OR "Indian Ocean Island*" OR Indonesia* OR Iran* OR Iraq* OR Jamaica* OR Jordan* OR Lesotho OR Macedonia* OR "Marshall Island*" OR Micronesia* OR "Middle East*" OR Moldova* OR Morocc* OR Namibia* OR Nicaragua* OR Paraguay* OR Peru* OR Philippin* OR "Sri Lanka*" OR Suriname* OR Swaziland* OR Syria* OR Thai* OR Tonga* OR Tunisia* OR Turkmen* OR Ukrain* OR Vanuatu* OR "Cape Verd*" OR Gaza OR Kiribati* OR Maldives OR Palestin* OR "West Bank" OR Afghan* OR Bangladesh* OR Benin* OR "Burkina Faso*" OR Burundi* OR Cambodia* OR "Central African Republic*" OR Chad* OR Comoros OR Congo* OR "Cote d Ivoire" OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea* OR "Guinea‐Bissau" OR Haiti* OR India* OR Kenya* OR Korea* OR Kyrgyz* OR Laos OR Laot* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Melanesia* OR Mongolia* OR Mozambi* OR Myanmar OR Nepal* OR Niger* OR Nigeria* OR Pakistan* OR "Papua New Guinea*" OR Rwanda* OR Senegal* OR "Sierra Leone*" OR Somalia* OR Sudan* OR Tajikistan* OR Tanzania* OR "East Timor*" OR Togo* OR Uganda* OR Uzbek* OR Vietnam* OR Yemen* OR Zambia* OR Zimbabw* OR Burm* OR Lao.tw. OR "North Korea*" OR "Solomon Island*" OR "Sao Tome" OR Timor* OR "Viet Nam*" OR "ivory coast")
PubMed
24 June 2014
4,626 records
Intervention terms
social assistance[tiab] OR social polic*[tiab] OR social welfare[tiab] OR social insurance*[tiab] OR social protection*[tiab] OR public assistance[tiab] OR family policy[tiab] OR ((financial[tiab] OR cash[tiab] OR pay*[tiab] OR monetary[tiab] OR money[tiab]) AND (transfer*[tiab] OR measure*[tiab] OR incentive*[tiab] OR allowance*[tiab] OR exclu*[tiab] OR reform*[tiab] OR gain*[tiab] OR credit*[tiab] OR benefit*[tiab]))
Study terms
random*[tiab] OR placebo*[tiab] OR single blind*[tiab] OR double blind*[tiab] OR triple blind*[tiab] OR treble blind*[tiab] OR time series[tiab] OR quasi‐experiment*[tiab] OR pre test[tiab] OR pretest[tiab] OR pre‐intervention[tiab] OR post test[tiab] OR posttest[tiab] OR post‐intervention[tiab] OR controlled before[tiab] OR independent panel[tiab] OR panel stud*[tiab] OR intervention stud*[tiab] OR interventional stud*[tiab] OR "before and after"[tiab] OR repeat measure*[tiab] OR repeated measure*[tiab] OR evaluation stud*[tiab] OR evaluative stud*[tiab] OR comparison stud*[tiab] OR comparative stud*[tiab] OR trial[tiab] OR follow‐up assessment*[tiab] OR groups[tiab] OR ((intervention[tiab] OR interventional[tiab] OR process[tiab] OR program[tiab]) AND (evaluat*[tiab] OR effect*[tiab] OR outcome*[tiab])) OR program[tiab] OR programme[tiab] OR secondary analys*[tiab] OR ((evaluat*[tiab] OR intervention*[tiab] OR treatment*[tiab]) AND (control*[tiab] OR study[tiab] OR program*[tiab] OR comparison[tiab] OR comparative[tiab]))
Country terms
Africa[tw] OR Asia[tw] OR South America[tw] OR Latin America[tw] OR Central America[tw] OR developing countr*[tw] OR less developed countr*[tw] OR third world countr*[tw] OR under developed countr*[tw] OR middle income countr*[tw] OR low income countr*[tw] OR underserved countr*[tw] OR under served countr*[tw] OR deprived countr*[tw] OR poor countr*[tw] OR third world nation*[tw] OR under developed nation*[tw] OR middle income nation*[tw] OR low income nation*[tw] OR underserved nation*[tw] OR under served nation*[tw] OR deprived nation*[tw] OR poor nation*[tw] OR third world state*[tw] OR under developed state*[tw] OR middle income state*[tw] OR low income state*[tw] OR underserved state*[tw] OR under served state*[tw] OR deprived state*[tw] OR poor state*[tw] OR third world population*[tw] OR under developed population*[tw] OR middle income population*[tw] OR low income population*[tw] OR underserved population*[tw] OR under served population*[tw] OR deprived population*[tw] OR poor population*[tw] OR limic[tw] OR Samoa*[tw] OR Argentin*[tw] OR Beliz*[tw] OR Botswana*[tw] OR Brazil*[tw] OR Bulgaria*[tw] OR Chile*[tw] OR Comoro*[tw] OR Costa Rica*[tw] OR Croatia*[tw] OR Dominica*[tw] OR Equatorial Guinea*[tw] OR Gabon*[tw] OR Grenada*[tw] OR Hungar*[tw] OR Kazakh*[tw] OR Latvia*[tw] OR Leban*[tw] OR Libya*[tw] OR Lithuania*[tw] OR Malaysia*[tw] OR Mauriti*[tw] OR Mexic*[tw] OR Micronesia*[tw] OR Montenegr*[tw] OR Oman*[tw] OR Palau*[tw] OR Panama*[tw] OR Poland[tw] OR Polish[tw] OR Romania*[tw] OR Russia*[tw] OR Seychelles*[tw] OR Slovakia*[tw] OR South Africa*[tw] OR "Saint Kitts and Nevis"[tw] OR Saint Lucia*[tw] OR Saint Vincent*[tw] OR Grenadines[tw] OR Turk*[tw] OR Urugua*[tw] OR Venezuel*[tw] OR Yugoslavia*[tw] OR Guinea*[tw] OR Libia*[tw] OR Mayotte*[tw] OR Northern Mariana Island*[tw] OR Russian Federation[tw] OR Serbia*[tw] OR Slovak*[tw] OR Albania*[tw] OR Algeria*[tw] OR Angol*[tw] OR Armenia*[tw] OR Azerbaijan*[tw] OR Belarus*[tw] OR Bhutan*[tw] OR Bolivia*[tw] OR Bosnia*[tw] OR Herzegovina[tw] OR Cameroon*[tw] OR China[tw] OR Chinese[tw] OR Colombia*[tw] OR Congo*[tw] OR Cuba*[tw] OR Djibouti*[tw] OR Dominican Republic*[tw] OR Ecuador*[tw] OR Egypt*[tw] OR El Salvador*[tw] OR Fiji*[tw] OR "Georgia (Republic)"[tw] OR Georgian*[tw] OR Guam*[tw] OR Guatemal*[tw] OR Guyana*[tw] OR Hondur*[tw] OR Indian Ocean[tw] OR Indonesia*[tw] OR Iran*[tw] OR Iraq*[tw] OR Jamaica*[tw] OR Jordan*[tw] OR Lesotho[tw] OR Macedonia*[tw] OR Marshall Island*[tw] OR Micronesia*[tw] OR Middle East*[tw] OR Moldova*[tw] OR Morocc*[tw] OR Namibia*[tw] OR Nicaragua*[tw] OR Paraguay*[tw] OR Peru*[tw] OR Philippin*[tw] OR Sri Lanka*[tw] OR Suriname*[tw] OR Swaziland*[tw] OR Syria*[tw] OR Thai*[tw] OR Tonga*[tw] OR Tunisia*[tw] OR Turkmen*[tw] OR Ukrain*[tw] OR Vanuatu*[tw] OR Cape Verd*[tw] OR Gaza[tw] OR Kiribati*[tw] OR Maldives[tw] OR Marshall Island*[tw] OR Palestin*[tw] OR Syrian*[tw] OR West Bank[tw] OR Afghan*[tw] OR Bangladesh*[tw] OR Benin*[tw] OR Burkina*[tw] OR Faso*[tw] OR Burundi*[tw] OR Cambodia*[tw] OR Central African Republic*[tw]
Scopus
3 July 2014
692 records
(TITLE(conditional* OR unconditional*) OR TITLE({subject to})) AND (TITLE‐ABS‐KEY(cash OR benefit* OR money* OR monetary OR credit*) OR TITLE‐ABS‐KEY(grant* OR transfer* OR assistance OR support OR welfare) OR TITLE‐ABS‐KEY("unconditional CT*") OR TITLE‐ABS‐KEY(uct*) OR TITLE‐ABS‐KEY("safety net") OR TITLE‐ABS‐KEY("public policy" OR "public policies") OR TITLE‐ABS‐KEY("social policy" OR "social policies") OR TITLE‐ABS‐KEY("family policy" OR "family policies") OR TITLE‐ABS‐KEY("social security") OR TITLE‐ABS‐KEY("social insurance") OR TITLE‐ABS‐KEY("social protection")) AND (TITLE‐ABS‐KEY("systematic review" OR metaanalys* OR "meta‐analys*") OR TITLE‐ABS‐KEY(randomi*) OR TITLE‐ABS‐KEY(random* W/0 allocat*) OR TITLE‐ABS‐KEY(placebo*) OR TITLE‐ABS‐KEY("single‐blind" OR "double‐blind") OR TITLE‐ABS‐KEY((single PRE/0 blind*) OR (double PRE/0 blind*) OR (triple PRE/0 blind*) OR (treble PRE/0 blind*)) OR TITLE‐ABS‐KEY("control group*") OR TITLE‐ABS‐KEY((clinical PRE/0 trial*) OR (clinical PRE/0 stud*)) OR TITLE‐ABS‐KEY((comparative PRE/0 stud*) OR (comparison PRE/0 stud*)) OR TITLE‐ABS‐KEY(intervention* W/2 stud*) OR TITLE‐ABS‐KEY(cohort PRE/0 stud*) OR TITLE‐ABS‐KEY(evaluat* W/2 stud*) OR TITLE‐ABS‐KEY(program* W/3 evaluat*) OR TITLE‐ABS‐KEY(time PRE/0 series) OR TITLE‐ABS‐KEY("quasi‐experiment*") OR TITLE‐ABS‐KEY("pre test" OR pretest OR "pre‐intervention" OR "post test" OR posttest OR "post‐intervention") OR TITLE‐ABS‐KEY("controlled before") OR TITLE‐ABS‐KEY("independent panel") OR TITLE‐ABS‐KEY(panel PRE/0 stud*) OR TITLE‐ABS‐KEY({before and after}) OR TITLE‐ABS‐KEY(repeat* W/3 measure*) OR TITLE‐ABS‐KEY((follow‐up PRE/0 assessment*) OR ("follow up" PRE/0 assessment*)) OR TITLE‐ABS‐KEY((follow‐up PRE/0 trial*) OR ("follow up" PRE/0 trial*)) OR TITLE‐ABS‐KEY((follow‐up PRE/0 group*) OR ("follow up" PRE/0 group*)) OR TITLE‐ABS‐KEY((intervention* W/8 evaluat*) OR (process* W/8 evaluat*) OR (program* W/8 evaluat*)) OR TITLE‐ABS‐KEY((intervention* W/8 effect*) OR (process* W/8 effect*) OR (program* W/8 effect*)) OR TITLE‐ABS‐KEY((intervention* W/8 outcome*) OR (process* W/8 outcome*) OR (program* W/8 outcome*)) OR TITLE‐ABS‐KEY(secondary PRE/2 analys*) OR TITLE‐ABS‐KEY((evaluat* OR assess* OR compar* OR outcome* OR analys*) AND (intervention* OR program* OR strateg* OR initiative* OR policy OR policies)) OR TITLE‐ABS‐KEY(economic* OR socioeconomic*) OR TITLE‐ABS‐KEY(cost* W/3 analys*) OR TITLE‐ABS‐KEY(cost* W/3 health*) OR TITLE‐ABS‐KEY(cost* W/3 high) OR TITLE‐ABS‐KEY(cost* W/3 low) OR TITLE‐ABS‐KEY(cost* W/3 effective*) OR TITLE‐ABS‐KEY(cost* W/3 benefit*) OR TITLE‐ABS‐KEY(cost* W/3 minim*) OR TITLE‐ABS‐KEY(fiscal* OR funding OR financ*) OR TITLE‐ABS‐KEY(expenditure*) OR TITLE‐ABS‐KEY(value) OR TITLE‐ABS‐KEY(budget*)) AND (EXCLUDE(SUBJAREA, "ENGI") OR EXCLUDE(SUBJAREA, "COMP") OR EXCLUDE(SUBJAREA, "MATH") OR EXCLUDE(SUBJAREA, "AGRI") OR EXCLUDE(SUBJAREA, "ENGI") OR EXCLUDE(SUBJAREA, "COMP") OR EXCLUDE(SUBJAREA, "MATH") OR EXCLUDE(SUBJAREA, "AGRI") OR EXCLUDE(SUBJAREA, "ENVI") OR EXCLUDE(SUBJAREA, "EART") OR EXCLUDE(SUBJAREA, "PHYS") OR EXCLUDE(SUBJAREA, "CENG") OR EXCLUDE(SUBJAREA, "ENER") OR EXCLUDE(SUBJAREA, "MATE") OR EXCLUDE(SUBJAREA, "CHEM") OR EXCLUDE(SUBJAREA, "ENGI") OR EXCLUDE(SUBJAREA, "COMP") OR EXCLUDE(SUBJAREA, "MATH") OR EXCLUDE(SUBJAREA, "AGRI") OR EXCLUDE(SUBJAREA, "ENVI") OR EXCLUDE(SUBJAREA, "EART") OR EXCLUDE(SUBJAREA, "PHYS") OR EXCLUDE(SUBJAREA, "CENG") OR EXCLUDE(SUBJAREA, "ENER") OR EXCLUDE(SUBJAREA, "MATE") OR EXCLUDE(SUBJAREA, "CHEM"))
Social Sciences Citation Index
16 May 2014
2,569 records
Intervention terms
TS=((social NEAR/1 (assistance OR polic* OR welfare OR insurance* OR protection)) OR "public assistance" OR "family policy" OR ((financial OR cash OR pay* OR monetary OR money) NEAR/3 (transfer* OR measure* OR incentive* OR allowance* OR exclu* OR reform* OR gain* OR credit OR credits OR benefit OR benefits)))
Study terms
TS=(random* OR "random allocation" OR placebo* OR ((single OR double OR triple OR treble) NEAR/1 blind*) OR (time NEAR/1 series) OR "quasi experiment*" OR "pre test" OR pretest OR "pre‐intervention" OR "post test" OR posttest OR "post‐intervention" OR "controlled before" OR "independent panel" OR ((panel OR intervention* OR evaluat* OR compari*) NEAR/1 stud*) OR "before and after" OR "repeat* measure*" OR trial OR "follow up assessment*" OR groups OR ((intervention OR interventional OR process OR program) NEAR/8 (evaluat* OR effect* OR outcome*)) OR program OR programme OR "secondary analys*" OR ((evaluat* OR intervention* OR treatment*) AND (control* OR study OR program* OR comparison OR comparative)))
Countries terms
TS=(Africa OR Asia OR "South America" OR "Latin America" OR "Central America" OR ((developing OR "less* developed" OR "third world" OR "under developed" OR "middle income" OR "low income" OR underserved OR "under served" OR deprived OR poor*) NEAR/1 (count* OR nation OR nations OR state OR states OR population OR populations)) OR lmic OR lmics)
TS=(Samoa* OR Argentin* OR Beliz* OR Botswana* OR Brazil* OR Bulgaria* OR Chile* OR Comoro* OR "Costa Rica*" OR Croatia* OR Dominica* OR Guinea* OR Gabon* OR Grenada* OR Hungar* OR Kazakh* OR Latvia* OR Leban* OR Libya* OR Lithuania* OR Malaysia* OR Mauriti* OR Mexic* OR Micronesia* OR Montenegr* OR Oman* OR Palau* OR Panama* OR Poland OR Polish OR Romania* OR Russia* OR Seychelles* OR Slovak* OR "Saint Kitts" OR Nevis OR "Saint Lucia*" OR "Saint Vincent" OR Grenadines OR Turk* OR Urugua* OR Venezuel* OR Yugoslavia* OR Libia* OR Mayotte OR "Mariana Island*" OR Serbia* OR "St Kitts" OR "St Lucia*" OR "St Vincent" OR Albania* OR Algeria* OR Angol* OR Armenia* OR Azerbaijan* OR Belarus* OR Bhutan* OR Bolivia* OR Bosnia* OR Herzegovin* OR Cameroon* OR China OR Chinese OR Colombia* OR Congo* OR Cuba* OR Djibouti* OR Ecuador* OR Egypt* OR "El Salvador*" OR Fiji* OR Georgia* OR Guam* OR Guatemal* OR Guyana* OR Hondur* OR "Indian Ocean Island*" OR Indonesia* OR Iran* OR Iraq* OR Jamaica* OR Jordan* OR Lesotho OR Macedonia* OR "Marshall Island*" OR Micronesia* OR "Middle East*" OR Moldova* OR Morocc* OR Namibia* OR Nicaragua* OR Paraguay* OR Peru* OR Philippin* OR "Sri Lanka*" OR Suriname* OR Swaziland* OR Syria* OR Thai* OR Tonga* OR Tunisia* OR Turkmen* OR Ukrain* OR Vanuatu* OR "Cape Verd*" OR Gaza OR Kiribati* OR Maldives OR Palestin* OR "West Bank" OR Afghan* OR Bangladesh* OR Benin* OR "Burkina Faso*" OR Burundi* OR Cambodia* OR "Central African Republic*" OR Chad* OR Comoros OR Congo* OR "Cote d Ivoire" OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea* OR "Guinea‐Bissau" OR Haiti* OR India* OR Kenya* OR Korea* OR Kyrgyz* OR Laos OR Laot* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Melanesia* OR Mongolia* OR Mozambi* OR Myanmar OR Nepal* OR Niger* OR Nigeria* OR Pakistan* OR "Papua New Guinea*" OR Rwanda* OR Senegal* OR "Sierra Leone*" OR Somalia* OR Sudan* OR Tajikistan* OR Tanzania* OR "East Timor*" OR Togo* OR Uganda* OR Uzbek* OR Vietnam* OR Yemen* OR Zambia* OR Zimbabw* OR Burm* OR Lao OR "North Korea*" OR "Solomon Island*" OR "Sao Tome" OR Timor* OR "Viet Nam*" OR "ivory coast")
Sociological Abstracts
14 May 2014
1857 records
Intervention terms
ti((social NEAR/1 (assistance OR polic* OR welfare OR insurance* OR protection)) OR "public assistance" OR "family policy" OR ((financial OR cash OR pay* OR monetary OR money) NEAR/3 (transfer* OR measure* OR incentive* OR allowance* OR exclu* OR reform* OR gain* OR credit OR credits OR benefit OR benefits))) OR ab((social NEAR/1 (assistance OR polic* OR welfare OR insurance* OR protection)) OR "public assistance" OR "family policy" OR ((financial OR cash OR pay* OR monetary OR money) NEAR/3 (transfer* OR measure* OR incentive* OR allowance* OR exclu* OR reform* OR gain* OR credit OR credits OR benefit OR benefits)))
Study terms
SU.EXACT("Evaluation Research" OR "Program Evaluation" OR "Cohort Analysis") OR ti(random* OR placebo* OR ((single OR double OR triple OR treble) NEAR/1 blind*) OR (time NEAR/1 series) OR "quasi‐experiment*" OR "pre test" OR pretest OR "pre‐intervention" OR "post test" OR posttest OR "post‐intervention" OR "controlled before" OR "independent panel" OR "panel stud* OR "intervention* stud*" OR "before and after" OR "repeat* measure* OR "evaluat* stud*" OR "compari* stud*" OR trial OR "follow‐up assessment*" OR groups OR ((intervention OR interventional OR process OR program) NEAR/8 (evaluat* OR effect* OR outcome*)) OR program OR programme OR "secondary analys*" OR ((evaluat* OR intervention* OR treatment*) AND (control* OR study OR program* OR comparison OR comparative))) OR ab(random* OR placebo* OR ((single OR double OR triple OR treble) NEAR/1 blind*) OR (time NEAR/1 series) OR "quasi‐experiment*" OR "pre test" OR pretest OR "pre‐intervention" OR "post test" OR posttest OR "post‐intervention" OR "controlled before" OR "independent panel" OR "panel stud* OR "intervention* stud*" OR "before and after" OR "repeat* measure* OR "evaluat* stud*" OR "compari* stud*" OR trial OR "follow‐up assessment*" OR groups OR ((intervention OR interventional OR process OR program) NEAR/8 (evaluat* OR effect* OR outcome*)) OR program OR programme OR "secondary analys*" OR ((evaluat* OR intervention* OR treatment*) AND (control* OR study OR program* OR comparison OR comparative)))
Countries terms
SU.EXACT("Developing Countries") OR ti(Africa OR Asia OR "South America" OR "Latin America" OR "Central America" OR ((developing OR "less* developed" OR "third world" OR "under developed" OR "middle income" OR "low income" OR underserved OR "under served" OR deprived OR poor*) NEAR/1 (count* OR nation OR nations OR state OR states OR population OR populations)) OR lmic OR lmics) OR ab(Africa OR Asia OR "South America" OR "Latin America" OR "Central America" OR ((developing OR "less* developed" OR "third world" OR "under developed" OR "middle income" OR "low income" OR underserved OR "under served" OR deprived OR poor*) NEAR/1 (count* OR nation OR nations OR state OR states OR population OR populations)) OR lmic OR lmics) OR su(Africa OR Asia OR "South America" OR "Latin America" OR "Central America")
OR
(Samoa* OR Argentin* OR Beliz* OR Botswana* OR Brazil* OR Bulgaria* OR Chile* OR Comoro* OR "Costa Rica*" OR Croatia* OR Dominica* OR Guinea* OR Gabon* OR Grenada* OR Hungar* OR Kazakh* OR Latvia* OR Leban* OR Libya* OR Lithuania* OR Malaysia* OR Mauriti* OR Mexic* OR Micronesia* OR Montenegr* OR Oman* OR Palau* OR Panama* OR Poland OR Polish OR Romania* OR Russia* OR Seychelles* OR Slovak* OR "Saint Kitts" OR Nevis OR "Saint Lucia*" OR "Saint Vincent" OR Grenadines OR Turk* OR Urugua* OR Venezuel* OR Yugoslavia* OR Libia* OR Mayotte OR "Mariana Island*" OR Serbia* OR "St Kitts" OR "St Lucia*" OR "St Vincent" OR Albania* OR Algeria* OR Angol* OR Armenia* OR Azerbaijan* OR Belarus* OR Bhutan* OR Bolivia* OR Bosnia* OR Herzegovin* OR Cameroon* OR China OR Chinese OR Colombia* OR Congo* OR Cuba* OR Djibouti* OR Ecuador* OR Egypt* OR "El Salvador*" OR Fiji* OR Georgia* OR Guam* OR Guatemal* OR Guyana* OR Hondur* OR "Indian Ocean Island*" OR Indonesia* OR Iran* OR Iraq* OR Jamaica* OR Jordan* OR Lesotho OR Macedonia* OR "Marshall Island*" OR Micronesia* OR "Middle East*" OR Moldova* OR Morocc* OR Namibia* OR Nicaragua* OR Paraguay* OR Peru* OR Philippin* OR "Sri Lanka*" OR Suriname* OR Swaziland* OR Syria* OR Thai* OR Tonga* OR Tunisia* OR Turkmen* OR Ukrain* OR Vanuatu* OR "Cape Verd*" OR Gaza OR Kiribati* OR Maldives OR Palestin* OR "West Bank" OR Afghan* OR Bangladesh* OR Benin* OR "Burkina Faso*" OR Burundi* OR Cambodia* OR "Central African Republic*" OR Chad* OR Comoros OR Congo* OR "Cote d Ivoire" OR Eritrea* OR Ethiopia* OR Gambia* OR Ghana* OR Guinea* OR "Guinea‐Bissau" OR Haiti* OR India* OR Kenya* OR Korea* OR Kyrgyz* OR Laos OR Laot* OR Liberia* OR Madagascar OR Malagasy OR Malawi* OR Mali* OR Mauritania* OR Melanesia* OR Mongolia* OR Mozambi* OR Myanmar OR Nepal* OR Niger* OR Nigeria* OR Pakistan* OR "Papua New Guinea*" OR Rwanda* OR Senegal* OR "Sierra Leone*" OR Somalia* OR Sudan* OR Tajikistan* OR Tanzania* OR "East Timor*" OR Togo* OR Uganda* OR Uzbek* OR Vietnam* OR Yemen* OR Zambia* OR Zimbabw* OR Burm* OR Lao OR "North Korea*" OR "Solomon Island*" OR "Sao Tome" OR Timor* OR "Viet Nam*" OR "ivory coast")
The Campbell Library: The Campbell Collaboration
11 June 2014
318 records
No search term (Social welfare)
Records: 96
Cash transfer (all text)
Records: 105
Financial credit (all text)
Records: 117
TRoPHI
9 June 2014
20 records
cash transfer OR financial credit OR financial benefit OR financial incentive
WHOLIS
9 June 2014 6 records cash transfer OR financial credit OR financial benefit or financial incentive
Data and analyses
Comparison 1. Unconditional cash transfer compared with no unconditional cash transfer (or co‐intervention only).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Use of health service outcomes | Other data | No numeric data | ||
| 2 Died, previous three months | 1 | 2885 | Hazard Ratio (Random, 95% CI) | 0.26 [0.10, 0.66] |
| 3 Anthropometric measures, disease prevalence, and level of depression | Other data | No numeric data | ||
| 4 Level of child development, current | Other data | No numeric data | ||
| 5 Became severely acutely malnourished, previous three months | 1 | 2885 | Hazard Ratio (Random, 95% CI) | 0.44 [0.24, 0.80] |
| 6 Social determinants of health | Other data | No numeric data |
1.2. Analysis.
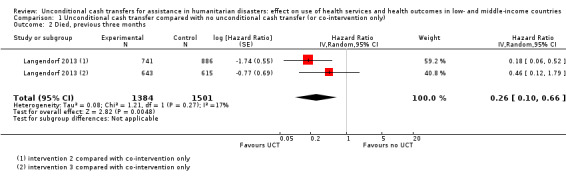
Comparison 1 Unconditional cash transfer compared with no unconditional cash transfer (or co‐intervention only), Outcome 2 Died, previous three months.
1.5. Analysis.
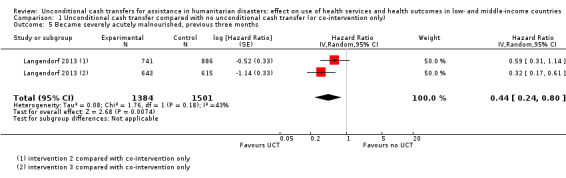
Comparison 1 Unconditional cash transfer compared with no unconditional cash transfer (or co‐intervention only), Outcome 5 Became severely acutely malnourished, previous three months.
Comparison 2. Unconditional cash transfer compared with in‐kind transfer.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health outcomes | Other data | No numeric data |
Comparison 3. Unconditional cash transfer compared with same unconditional cash transfer paid through different mechanism.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Health outcomes | Other data | No numeric data | ||
| 2 Social determinants of health | Other data | No numeric data | ||
| 3 Health service expenditure | Other data | No numeric data | ||
| 4 Local markets and infrastructure | Other data | No numeric data |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Aker 2011.
| Methods | Controlled before‐and‐after study; difference‐in‐differences method; 8 months (2010). | |
| Participants | 1200 households interviewed twice (April 2010 and December 2010); all households with children aged 0 to 4 years; 116 food deficit villages (i.e., villages officially classified as producing less than 50% of their consumption needs in the 2009 harvest; clusters), 6 communes, Tahoua region, Niger. | |
| Interventions | 3 intervention groups and no control group:
Intervention duration: 5 months. Follow‐up: 3 months after 5 months of the intervention. Intervention design: aimed to reduce malnutrition and prevent asset depletion in households during and after droughts; targeted to poor households with at least one child aged 0 to 4; provided a total amount of USD 225 (USD 45 per month for 5 months) to women. |
|
| Outcomes |
Alternative outcome measures not reported in this review:
|
|
| Notes | Intervention context: experiment by a non‐governmental organisation (Concern Worldwide); humanitarian disaster context was drought; implemented by non‐governmental organisation (Concern Worldwide); intervention costs and uptake unclear. Funders of the study: Concern Worldwide, European Commission, Hitachi Center, Irish Aid, and Tufts University. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Random sequence generation ensured for some interventions, but not for others. Clusters allocated randomly to two groups, but non‐randomly to one. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Baseline outcome measurements similar | Low risk | No baseline differences (P < 0.05) reported between the intervention and comparator groups in outcome measurements |
| Baseline characteristics similar | Unclear risk | Baseline differences (P < 0.05) reported between the intervention and comparator group in one characteristic. The proportion of participants with some education in the intervention group was lower than that in the comparator group (0.07 compared with 0.15, P < 0.05). However, this baseline difference was comprehensively adjusted using regression analysis. Investigators thought evaluating baseline differences for factors such as presence and magnitude of local natural disasters, man‐made disasters, epidemics, and economic shocks was possible, but these differences could not be assessed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants not possible and blinding of personnel unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Contamination | High risk | Allocation was by village, but additional income from UCTs provided to participants in the intervention group may have been transferred to participants in the comparator group (e.g., between family members). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Initial survey non‐response rates were unclear. Attrition rate was low (3% to 5%) and non‐differential by intervention and comparator group. For each intervention group, numbers of missing clusters and participants were unclear. For each intervention group, percentage of missing participants was:
Numbers of missing participants per outcome were unclear. We considered the missing data unlikely to have impacted effect estimates, because only a small percentage of participants missed data (3% to 5%). |
| Selective reporting (reporting bias) | Unclear risk | No study protocol identified |
| Other bias | Low risk | None identified |
Langendorf 2013.
| Methods | Controlled before‐and‐after study; marginal Cox proportional hazards modelling with propensity scores methods; four months (2011) | |
| Participants | 5395 participants interviewed 5 times (August to December 2011); all children aged 6 to 23 months and measuring > 60.0 cm and ≤ 80.0 cm in length; 48 villages or hamlets (clusters) within 15 km of a health care centre, Madarounfa district, Maradi, Niger. | |
| Interventions | 7 intervention groups and no control group:
Intervention duration: 4 months. Follow‐up: 4 months. Intervention design: aimed to prevent acute malnutrition after droughts; targeted at children aged 6 to 23 months and measuring > 60.0 cm and ≤ 80.0 cm in length; UCT interventions 2 and 3 provided a total amount of USD 208 (USD 52 per month for 4 months) and UCT intervention 4 USD 236 (USD 59 per month for 4 months); was paid to women (mothers); food transfer 1 provided nutritional supplements of 500 kcal/day (92 g/day of Supplementary Plumpy), food transfer 2 provided 820 kcal/day (200 g/day of Super Cereal Plus), food transfer 3 provided 820 kcal/day (200 g/day of Super Cereal Plus) plus a monthly family food ration (50 kg cereals, 7.5 kg pulses, and 2.5 kg oil), and food transfer 4 provided 250 kcal/day (46 g/day of Plumpy’Doz); and provided as co‐intervention to all intervention and comparator groups educational material that aimed to ensure nutritional value and dietary diversity of food purchased by parents for their children. Participants did not receive the same number of transfers across intervention and comparator groups, partially because enrolment was continuous throughout the study period. While on average 69% of participants received 4 or 5 of the 5 total transfers, this percentage ranged from 62% to 74% across intervention and comparator groups. |
|
| Outcomes | Primary outcomes: health outcomes (mortality: died; and nutrition: became severely acutely malnourished) Alternative outcome measures not reported in this review: Primary outcomes: health outcomes (nutrition: became moderately acutely malnourished) |
|
| Notes | Intervention context: experiment by research organisation (Epicentre); humanitarian disaster context was drought; implemented by research organisation (Epicentre); intervention costs unclear; and intervention uptake high (on average about 95% of participants present at all their payment meetings), but ranged across intervention groups (93% to 99%) Funders of the study: Médecins Sans Frontiéres and World Food Programme Potential conflict of interest: Funders of the study contributed to study design and the preparation of study records. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Random sequence generation ensured for some interventions, but not for others. Clusters allocated randomly to four intervention and comparator groups, but non‐randomly to three intervention and comparator groups. |
| Allocation concealment (selection bias) | High risk | Allocation concealment not ensured among participants and personnel |
| Baseline outcome measurements similar | Low risk | Baseline differences (P < 0.05) reported between the intervention and comparator groups in two outcome measurements. The proportion of children with severe acute malnutrition ranged between 0.03 and 0.07 (P = 0.01). However, these baseline differences were comprehensively adjusted for using regression analysis. |
| Baseline characteristics similar | High risk | Baseline differences (P < 0.05) reported between the intervention and comparator groups in two characteristics. The proportion of children who were stunted ranged between 0.58 and 0.67 (P = 0.04), and the proportion of girls ranged between 0.46 and 0.56 (P = 0.00). However, these baseline differences were comprehensively adjusted for using regression analytic methods. There were likely baseline differences due to factors such as presence and magnitude of local natural disasters, man‐made disasters, epidemics, and economic shocks, considering that, for example, the death rates observed across intervention groups were highly differential, ranging between 0.2% and 2.3%. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants not possible, and blinding of personnel unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessors not blinded for outcome assessment, but all outcomes measured objectively |
| Contamination | High risk | Allocation was by village, but additional income from UCTs provided to participants in the intervention groups may have been transferred to participants in the comparator groups (e.g., between family members). |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Initial survey non‐response rate was unclear. Of 60 eligible villages, 12 villages (20%) were excluded from study before intervention allocation commenced because they were attached to ineligible or relatively inaccessible health posts. Attrition rate was moderate (7%) and differential by intervention and comparator group (3% to 18%). No intervention group missed any clusters. For each intervention group, the number of missing participants was unclear, but the percentage of missing participants was:
The exact number of missing participants per outcome was unclear. However, analyses of severe acute malnutrition excluded 230 participants (5.5% of all participants) with this condition at baseline. We considered the reasons for missing data to be acceptable, as children were missing for similar reasons across intervention groups (i.e., they were removed after reaching 80.1 cm, dying, withdrawing, or failing to meet inclusion criteria). We considered the missing data to potentially have impacted effect estimates, because a moderate percentage of participants missed data (7%) and the chance of the events occurring was low (died: 0.33 per 100 child‐months, became severely acutely malnourished: 1.56 per 100 child‐months). |
| Selective reporting (reporting bias) | Unclear risk | No study protocol identified. |
| Other bias | Low risk | None identified. |
Macours 2008.
| Methods | Cluster‐randomised controlled trial (four stages: first, all communities in 6 municipalities were enumerated; second, 56 intervention communities and 50 control communities were randomly selected; third, intervention communities were randomly allocated to 3 arms; and fourth, participants residing in intervention‐allocated communities and eligible for the intervention received the intervention); regression methods; 49 months (2005 to 2009). | |
| Participants | 8490 participants interviewed 3 times (baseline: April to May 2005; follow‐up 1: July to August 2006; and follow‐up 2: August 2008 to May 2009); 4245 children and 4245 adults (the children's mothers) in poor households; 106 communities (clusters), 6 rural municipalities, Nicaragua. | |
| Interventions | 3 intervention groups and 1 control group:
Intervention duration: 12 months. Follow‐up: at 8 to 9 months of the intervention and 8 to 29 months after 12 months of the intervention. Intervention design: aimed to reduce the impact of shocks on human and physical capital investments after a drought (World Bank 2011b); targeted to children in poor households in rural areas; intervention 1 provided a total amount of USD 145 for families without children or with children aged 0 to 6 years (about USD 24 every 2 months for 12 months) and of USD 235 plus USD 25 per child for families with children aged 7 to 15 years (about USD 42 every second month for 12 months for a family with 1 eligible child); paid in‐hand to women (mothers); had a fuzzy design, with conditions (i.e., regular preventive health check‐ups) for households with children aged 0 to 6 years not monitored, and non‐compliance not penalised, but with conditions (i.e., children's school enrolment and regular school attendance) for households with children aged 7 to 15 years monitored and non‐compliance penalised; minor messaging to all recipients that transfers intended to improve the diversity and nutrient content of children’s diets and to buy school material. |
|
| Outcomes |
Alternative outcome measures not reported in this review
|
|
| Notes | Intervention context: pilot programme of the Government of Nicaragua called Atención a Crisis; humanitarian disaster context was drought; implemented by the Government of Nicaragua through the Ministry of the Family; intervention costs unclear; and intervention uptake very high (> 95%). Funders of the study: World Bank, BASIS Assets and Market Access Collaborative Research Support Program. Potential conflict of interest: Funders of the study contributed to study design and the preparation of study records. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random sequence generation ensured. |
| Allocation concealment (selection bias) | High risk | Allocation concealment not possible among participants (with intervention determined by public lottery) and unclear among study personnel. |
| Baseline outcome measurements similar | Low risk | Baseline differences (P < 0.05) reported between the intervention and control groups in one outcome. More specifically, the proportion of children in the intervention groups who had received deworming drugs in the last six months was lower than in the control group (0.59 compared with 0.51, P = 0.04). However, these baseline differences were comprehensively adjusted for using regression analytic methods. |
| Baseline characteristics similar | Unclear risk | No baseline differences (P < 0.05) reported between the intervention and control groups in characteristics. There were possible baseline differences due to factors such as presence and magnitude of local natural disasters, man‐made disasters, epidemics, and economic shocks, but these could not be assessed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants not possible, and blinding of personnel unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome assessment not ensured. However, statistical analysis controlled for identity of outcome assessor and month of outcome assessment, and there were no differences between intervention and control groups for self‐reported outcomes that could be validated with administrative records. |
| Contamination | High risk | Allocation was by community, but additional income from unconditional cash transfers provided to participants in the intervention groups may have been transferred to participants in the comparator group (e.g., between family members). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Initial survey non‐response rate was unclear. Attrition rate was low (2%) and non‐differential between intervention and comparator groups. For each intervention and control group, numbers of missing clusters and participants were unclear. Number of missing participants per outcome was also unclear. We considered the missing data unlikely to have impacted effect estimates, because only a small percentage of participants missed data (2%). |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or study protocol identified |
| Other bias | Low risk | None identified |
UCT: unconditional cash transfer
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ahmed 2009 | No eligible UCT studied |
| Bailey 2013 | No eligible outcomes studied |
| Baird 2010 | No eligible UCT studied |
| Bazzi 2012 | No eligible UCT studied |
| Cluver 2013 | Ineligible study type used |
| Cunha 2014 | No eligible UCT studied |
| Currie 1993 | No eligible UCT studied |
| Devereux 2006 | Ineligible comparator used |
| Devereux 2008a | Ineligible comparator used |
| Dutta 2010 | No eligible outcome studied |
| Fenn 2013 | Ineligible study type used |
| Harvey 2006 | Ineligible study type used |
| Haushofer 2013 | No eligible UCT studied |
| Kardan 2010 | Ineligible study type used |
| Kebede 2006 | No eligible outcome studied |
| Leroy 2010 | No eligible UCT studied |
| Levy 2007 | No eligible UCT studied |
| MacAuslan 2011 | Ineligible study type used |
| Mattinen 2006 | No eligible UCT studied |
| Miller 2008 | No eligible UCT studied |
| Ntata 2010 | Ineligible study type used |
| Oxford Policy Management 2012 | No eligible UCT studied |
| Pellerano 2014 | No eligible UCT studied |
| Poulsene 2011 | Ineligible study type used |
| Robertson 2012 | No eligible UCT studied |
| Santos 2011 | No eligible outcomes studied |
| Save the Children 2009 | No eligible UCT studied |
| Schwab 2013 | Ineligible study type used |
| Tadesse 2014 | Ineligible study type used |
| Woolard 2014 | No eligible outcome studied |
Characteristics of studies awaiting assessment [ordered by study ID]
Devereux 2008b.
| Methods | Study type unclear; methods unclear; study period unclear |
| Participants | Participants unclear; Dowa district, Malawi |
| Interventions | One intervention group and one control group
Intervention duration: 4 months. Follow‐up: unclear. Intervention design: aimed to prevent food insecurity after a drought; targeted to individuals residing in drought‐affected areas; provided an unclear total amount; and provided via smart card per month to women (mothers) |
| Outcomes | Primary outcomes: use of health services, health outcomes (nutrition and disease prevalence) Secondary outcomes: social determinants of health (employment and social cohesion) |
| Notes | Intervention context: pilot programme of a non‐governmental organisation (Concern Worldwide) called the Dowa Emergency Cash Transfer Project; implemented by the non‐governmental organisation (Concern Worldwide); and intervention costs and uptake unclear. We requested the record for this study from the principal study author and the issuing organisation by email, but did not receive it. |
Characteristics of ongoing studies [ordered by study ID]
REFANI‐N.
| Trial name or title | Research on Food Assistance for Nutritional Impact ‐ Niger (REFANI‐N) |
| Methods | Cluster‐randomised controlled trial; longitudinal data analytic methods; 2014 to 2015. |
| Participants | About 7500 participants from about 2000 households interviewed twice (baseline: March to April 2015; follow‐up: September to October 2015); about 3500 children aged 6 to 59 months and about 4000 children or adults aged 15 to 49 years (the children's mothers); Affala and Takanamatt communes, Tahoua district, Niger. |
| Interventions | Two intervention groups and no control group:
Although the trial will not include a control group, the wider study will also randomly sample non‐recipient households, who may be used as a comparison group. Intervention duration: 4 months and 6 months, respectively. Follow‐up: 5 to 7 months. Intervention design: will be targeted to very poor households; will provide an unclear total amount (expected to be about 75% of a household's total energy needs); will be paid per month to women (mothers); will provide as co‐interventions nutritional supplements to all children aged 6 to 23 months and all pregnant and lactating women in both intervention groups, as well as health, hygiene, and nutrition education messages to both intervention groups. |
| Outcomes | Primary outcomes: use of health services (used health service); health outcomes (anthropometric measures: weight, length, height; nutrition: became acutely malnourished, level of dietary diversity) Secondary outcomes: social determinants of health (asset ownership: outcome measurements unclear) |
| Starting date | March 2014 |
| Contact information | Dr Andrew Seale (a.seal@ucl.ac.uk) |
| Notes | Trial registration: ISRCTN25360839 Funding organisation: United Kingdom Department for International Development. |
REFANI‐P.
| Trial name or title | Research on Food Assistance for Nutritional Impact ‐ Pakistan (REFANI‐P) |
| Methods | Cluster‐randomised controlled trial; longitudinal generalised mixed models methods; 2015. |
| Participants | 11,360 participants from 2580 poor or very poor households interviewed 3 times (baseline: April 2015; follow‐up 1: September 2015; follow‐up 2: April 2016); 5680 children aged 6 to 48 months at baseline and 5680 adults aged over 17 years (the children's mothers); 78 villages, Sindh province, Pakistan. |
| Interventions | Three intervention groups and one control group:
Intervention duration: 6 months. Follow‐up: 6 months and 12 months. Intervention design: will be targeted to poor and very poor households; will provide total amount of about USD 87 for the smaller UCT (about USD 14.50 per month for 6 months) and about USD 174 for the larger UCT (about USD 29.00 per month for 6 months); and will provide as co‐intervention the ACF Women and Children/Infant Improved Nutrition in Sindh (EU‐WINS) programme to all intervention groups and the control group. |
| Outcomes | Primary outcomes: health outcomes (anthropometric measures: wasting, stunting, body mass index; disease prevalence: has anaemia, has diarrhoea, has malaria, has respiratory illness; and nutrition: level of dietary diversity). |
| Starting date | April 2015 |
| Contact information | Ms Bridget Fenn (bridget@ennonline.net) |
| Notes | Trial registration: ISRCTN10761532 Funding organisation: United Kingdom Department for International Development. |
UCT: unconditional cast transfer
Differences between protocol and review
There are the following differences between the protocol and the review.
Background: updated to reflect the most recent state of evidence.
Objectives: with agreement from the editors, expanded the review objectives to also include the additional aim to assess the relative effectiveness of UCTs compared with the same UCTs paid through a different mechanism.
Types of studies: refined the inclusion and exclusion criteria for comparators. For UCT interventions provided alongside or in combination with co‐interventions, we added the co‐interventions only as comparators for assessing the effectiveness of UCTs in improving health services use and health outcomes. For the newly introduced review objective, we added the relevant comparator, that is a UCT paid through a different mechanism. We refined exclusion criteria for in‐kind and CCT as comparators, adding explicit acknowledgement that such comparators provided in combination with or alongside other interventions were ineligible for inclusion in the review.
Types of interventions: expanded the definition of interventions from within three months to any period of months, up to one year, as considered periods of this length comparable.
Types of interventions: refined the definition of UCTs by excluding vouchers. Unlike transfers of cash, transfers via vouchers restrict their recipients' ability to spend the additional income from the transfers, for example, by requiring recipients to only purchase certain goods and services from certain suppliers. Therefore, voucher transfers may impact health differently from genuine cash transfers, and may potentially act through different pathways.
Types of interventions: refined the definition of UCTs by including payments via mobile phone.
Types of interventions: changed the inclusion/exclusion of fuzzy UCTs. In the protocol, we included fuzzy UCTs if their intention was to be unconditional, and excluded (but noted) UCTs with any de facto conditions. In the review, we included fuzzy UCTs that were in practice unconditional, regardless of intention, and excluded fuzzy UCTs with de facto conditions (e.g., major administrative linking of the cash transfer or major messaging around the cash transfer). We now believe that what matters for effects on use of health services and health outcomes is likely more so the actual, experienced conditionality of the cash transfer, rather than the cash transfer's design as such.
Types of outcomes: added criteria around selection of time points to be reported.
Search: added searches of web pages of two additional key non‐governmental organisations, namely Cash Transfer Projects in Humanitarian Aid and Save the Children, as search sources.
Search: added handsearches of previous reviews in the field as a search source.
Search: did not search the Global Health, Web of Science database as planned.
Assessment of heterogeneity: introduced a cut‐off for the I2 statistic of 75% for meta‐analysis.
Assessment of risk of bias in included studies: If the review had included interrupted time series studies, to assess risk of bias in interrupted time series studies, we would have used the Cochrane Effective Practice and Organisation of Care’s risk of bias criteria (EPOC 2012) plus an item assessing the risk of bias from confounding. Had the review included cohort studies, in the absence of credible standard tools for assessing risk of bias, we would have at a minimum assessed the risk of bias from sampling; low response rates; attrition; exposure measurement; outcome measurement; confounding; and reverse causation (as per our previous and forthcoming reviews: Pega 2013; Pega 2014a).
Data synthesis: did not undertake harvest plots for narrative synthesis.
Data synthesis: did not include secondary outcomes in 'Summary of findings' tables.
Data synthesis: did not present 'Summary of findings' table for comparison of UCT with the same UCT paid through a different mechanism, because we judged the outcome measured and the applicability of the comparison insufficient to make an additional table helpful.
Data synthesis: used Review Mananger 5.3, rather than Review Manager 5.2.
Subgroup analyses: If subgroup analyses had been feasible, we would have conducted such analyses by: age (children (0 to 17 years), adults (≥ 18years)); disaster type (natural, man‐made); gender; level of income (e.g. total personal or household annual income after tax); and WHO region (Africa, Americas, Eastern Mediterranean, Europe, South‐East Asia and Western Pacific).
Contributions of authors
Pega conceived and led the review, and all authors contributed to protocol development. Bain and Pega searched the electronic and grey literature databases. Liu, Pabayo, Pega, and Walter searched key organisational websites. Walter led and all authors contributed to screening of records identified in the searches. Pega led and Lhachimi and Liu contributed to the data extraction. Pega led and all authors contributed to the quality assessment of included studies. Pega led and Lhachimi and Liu contributed to the interpretation and analysis of included studies and to the writing of the review.
Sources of support
Internal sources
-
Leibniz Institute for Prevention Research and Epidemiology & University of Bremen, Germany.
The Leibniz Institute for Preventive Research and Epidemiology and the University of Bremen provided funding through the Cooperative Research Group for Evidence Based Public Health to Lhachimi.
-
University of Otago, New Zealand.
The University of Otago provided salary funding through a Health Sciences Career Development Programme Postdoctoral Fellowship to Pega.
External sources
-
Harvard Medical School, USA.
The Harvard Medical School provided salary funding to Bain.
Declarations of interest
Frank Pega ‐ None known
Sze Yan Liu ‐ None known
Stefan Walter ‐ None known
Stefan K Lhachimi ‐ None known
New
References
References to studies included in this review
Aker 2011 {published data only}
- Aker JC, Boumnijel R, McClelland A, Tierney N. Zap it to me: the short‐term impacts of a mobile cash transfer program. Washington, DC: Center for Global Development; 2011 Sept. CGD Working Paper 268 2011.
Langendorf 2013 {published data only (unpublished sought but not used)}
- Langendorf C, Roederer T, Pee S, Brown D, Doyon S, Mamaty A, et al. Comparison of effect of cash transfer with or without special nutritious food on preventing childhood acute malnutrition in Niger [Abstract]. Annals of Nutrition and Metabolism 2013;63(Suppl 1):253. [Google Scholar]
- Langendorf C, Roederer T, Pee S, Brown D, Doyon S, Mamaty A, et al. Preventing acute malnutrition among children aged 6 to 23 months in Niger: effect of supplementation and cash transfer [Abstract]. Annals of Nutrition and Metabolism 2013;63(Suppl 1):625‐6. [Google Scholar]
- Langendorf C, Roederer T, Pee S, Brown D, Doyon S, Mamaty AA, et al. Preventing acute malnutrition among young children in crises: a prospective intervention study in Niger. PLoS Medicine 2014;11(9):e1001714. [DOI: 10.1371/journal.pmed.1001714] [DOI] [PMC free article] [PubMed] [Google Scholar]
Macours 2008 {published and unpublished data}
- Macours K, Schady N, Vakis R. Cash transfers, behavioral changes, and cognitive development in early childhood: evidence from a randomized experiment. American Economic Journal: Applied Economics 2012;4(2):247‐73. [DOI: 10.1257/app.4.2.247] [DOI] [Google Scholar]
- Macours K, Schady N, Vakis R. Cash transfers, behavioral changes, and cognitive development in early childhood: evidence from a randomized experiment. Washington, DC: The World Bank; 2008 Oct. Policy Research Working Paper 4759.
- Macours K. (Paris School of Economics, Paris, France). [personal communication]. Conversation with: F Pega (Public Health, University of Otago, Wellington, New Zealand) 4 May 2015.
References to studies excluded from this review
Ahmed 2009 {published data only}
- Ahmed SM. Capability development among the ultra‐poor in Bangladesh: a case study. Journal of Health, Population and Nutrition 2009;4:528‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bailey 2013 {published data only}
- Bailey S. Evaluation of Concern Worldwide’s emergency response in Masisi, North Kivu, DRC (2012‐2013). https://www.concern.net/sites/default/files/media/resource/evaluation_of_concern_worldwides_emergency_response_in_masisi_north_kivu_drc.pdf (accessed 25 July 2015).
Baird 2010 {published data only}
- Baird S, McIntosh C, Özler B. Cash or condition? Evidence from a cash transfer experiment. Quarterly Journal of Economics 2011;126(4):1709‐53. [DOI: 10.1093/qje/qjr032] [DOI] [Google Scholar]
- Baird S, McIntosh C, Özler B. Cash or condition? Evidence from a cash transfer experiment. Washington, DC: World Bank; 2010. Policy Research Working Paper 5259.
- Baird S, Hoop J, Özler B. Income shocks and adolescent mental health. Journal of Human Resources 2013;48(2):370‐403. [DOI: 10.1353/jhr.2013.0014] [DOI] [Google Scholar]
- Baird S, Hoop J, Özler B. Income shocks and adolescent mental health. Washington, DC: World Bank; 2011. Policy Research Working Paper 5644.
- Baird SJ, Chirwa E, Hoop J, Özler B. Girl power: cash transfers and adolescent welfare: evidence from a cluster‐randomized experiment in Malawi. Cambridge (MA): National Bureau of Economic Research; 2013. NBER Working Paper No. 19479.
- Baird SJ, Garfein RS, McIntosh CT, Ozler B. Effect of a cash transfer programme for schooling on prevalence of HIV and herpes simplex type 2 in Malawi: a cluster randomised trial. The Lancet 2012;379(9823):1320‐9. [DOI: 10.1016/S0140-6736(11)61709-1] [DOI] [PubMed] [Google Scholar]
Bazzi 2012 {published data only}
- Bazzi S, Sumarto S, Suryahadi A. Evaluating Indonesia’s unconditional cash transfer program, 2005‐6. Washington, DC: International Initiative for Impact Evaluation; 2012. Final report.
Cluver 2013 {published data only}
- Cluver L, Boyes M, Orkin M, Pantelic M, Molwena T, Sherr L. Child‐focused state cash transfers and adolescent risk of HIV infection in South Africa: a propensity‐score‐matched case‐control study. The Lancet Global Health 2013;1(6):e362‐70. [DOI: 10.1016/S2214-109X(13)70115-3] [DOI] [PubMed] [Google Scholar]
Cunha 2014 {published data only}
- Cunha JM. Testing paternalism: cash versus in‐kind transfers. American Economic Journal: Applied Economics 2014;6(2):195‐230. [DOI: 10.1257/app.6.2.195] [DOI] [Google Scholar]
Currie 1993 {published data only}
- Currie J. Welfare and the well‐being of children: the relative effectiveness of cash and in‐kind transfers. Cambridge (MA): National Bureau of Economic Research; 1993. NBER Working Paper No. 4539.
Devereux 2006 {published data only}
- Devereux S, Mvula P, Solomon C. After the FACT: an evaluation of Concern Worldwide’s Food And Cash Transfers Project in three districts of Malawi, 2006. Sussex, UK: University of Sussex, 2006. [Google Scholar]
Devereux 2008a {published data only}
- Devereux S, Jere P. "Choice, Dignity and Empowerment": Cash and Food Transfers in Swaziland: an Evaluation of Save the Children’s Emergency Drought Response, 2007/08. London: Institute of Development Studies & Save the Children, 2008. [Google Scholar]
Dutta 2010 {published data only}
- Dutta P, Howes S, Rinku M. Small but effective: India's unconditional cash transfers. Canberra: Australian National University; 2010. ASARC Working Paper.
- Dutta P, Howes S, Rinku M. Small but effective: India's unconditional cash transfers. Economic and Political Weekly 2010;45(52):63‐70. [Google Scholar]
Fenn 2013 {published data only}
- Fenn B, Noura G, Sibson V, Dolan C, Shoham J. The role of unconditional cash transfers during a nutritional emergency in Maradi region, Niger: a pre‐post intervention observational study. Public Health Nutrition 2014 Mar 28:1‐9. [Epub ahead of print]. [DOI: 10.1017/S1368980014000378] [DOI] [PMC free article] [PubMed]
- Fenn B, Trepel D, Dolan C, Shoham J, Sibson V. Seasonal unconditional cash transfers and wasting in Niger [Abstract]. Annals of Nutrition & Metabolism 2013;63(Suppl 1):1002. [Google Scholar]
Harvey 2006 {published data only}
- Harvey P, Marongwe N. Independent Evaluation of Oxfam GB Zambia’s Emergency Cash‐Transfer Programme. London: Humanitarian Policy Group, Overseas Development Institute, 2006. [Google Scholar]
Haushofer 2013 {published data only}
- Haushofer J, Shapiro J. Household Response to Income Changes: Evidence from an Unconditional Cash Transfer Program in Kenya. Princeton: Princeton University, 2013. [Google Scholar]
Kardan 2010 {published data only}
- Kardan A, MacAuslan I, Marimo N. Evaluation of Zimbabwe’s Emergency Cash Transfer Programme: Final Report. Oxford: Oxford Policy Management, Concern Worldwide & World Food Programme, 2010. [Google Scholar]
Kebede 2006 {published data only}
- Kebede E. Moving from emergency food aid to predictable cash transfers: recent experience in Ethiopia. Development Policy Review 2006;24(5):579‐99. [DOI: 10.1111/j.1467-7679.2006.00349.x] [DOI] [Google Scholar]
Leroy 2010 {published data only}
- Leroy JL, Gadsden P, Cossio TG, Gertler P. Cash and in‐kind transfers lead to excess weight gain in a population of women with a high prevalence of overweight in rural Mexico. Journal of Nutrition 2013;143(3):378‐83. [DOI: 10.3945/jn.112.167627] [DOI] [PubMed] [Google Scholar]
- Leroy JL, Gadsden P, Rodriguez‐Ramirez S, Cossio TG. Cash and in‐kind transfers in poor rural communities in Mexico increase household fruit, vegetable, and micronutrient consumption but also lead to excess energy consumption. Journal of Nutrition 2010;140(3):612‐7. [DOI: 10.3945/jn.109.116285] [DOI] [PubMed] [Google Scholar]
Levy 2007 {published data only}
- Levy D, Ohls J. Evaluation of Jamaica’s PATH Program: final report. Washington, DC: Mathematica Policy Research; 2007.
MacAuslan 2011 {published data only}
- MacAuslan I, Schofield L. Evaluation of Concern Kenya's Korogocho Emergency and Food Security Cash Transfer Initiative. Oxford, United Kingdom: Concern Worldwide & Oxford Policy Management, 2011. [Google Scholar]
Mattinen 2006 {published data only}
- Mattinen H, Ogden K. Cash‐based interventions: lessons from southern Somalia. Disasters 2006;30(3):297‐315. [DOI: 10.1111/j.0361-3666.2005.00322.x] [DOI] [PubMed] [Google Scholar]
Miller 2008 {published data only}
- Miller C, Tsoka M, Reichert K. The impacts of the cash transfer on children in Malawi. In: Handa S, Devereux S, Webb D editor(s). Social Protection for Africa’s Children. New York, NY: Routledge, 2010:96‐116. [Google Scholar]
- Miller CM, Tsoka M, Reichert K. Impact Evaluation Report: External Evaluation of the Mchinji Social Cash Transfer Pilot. Boston: Boston University & University of Malawi, 2008. [Google Scholar]
- Miller CM, Tsoka M, Reichert K. The impact of the Social Cash Transfer Scheme on food security in Malawi. Food Policy 2011;36(2):230‐8. [DOI: 10.1016/j.foodpol.2010.11.020] [DOI] [Google Scholar]
Ntata 2010 {published data only}
- Ntata PRT. Bridging the hunger gap with cash transfers: experiences from Malawi. Development in Practice 2010;20(3):422‐7. [DOI: 10.1080/09614521003709924] [DOI] [Google Scholar]
Oxford Policy Management 2012 {published data only}
- Merttens F, Hurrell A, Marzi M, Attah R, Farhat M, Kardan A, et al. Kenya Hunger Safety Net Programme Monitoring and Evaluation Component: Impact Evaluation Final Report: 2009 to 2012. Oxford: Oxford Policy Management, 2013. [Google Scholar]
- Oxford Policy Management, Institute of Development Studies. Kenya Hunger Safety Net Programme: Monitoring and Evaluation Component: Quantitative Impact Evaluation Report: 2009/10 to 2010/11. Oxford: Oxford Policy Management, 2012. [Google Scholar]
Pellerano 2014 {published data only}
- Pellerano L, Moratti M, Jakobsen M, Bajgar M, Barca V. The Lesotho Child Grants Programme Impact Evaluation: Follow‐up Report. Maseru: UNICEF‐Lesotho, Oxford Policy Management, 2014. [Google Scholar]
Poulsene 2011 {published data only}
- Poulsene L, Fabre D. UNICEF Emergency Project Niger: cash transfer for protection of blanket feeding: Maradi and Tahoua regions. 2011. www.unicef.org/evaluation/files/HQ_2010‐007_UNICEF_Cash_Transfer_‐_Final_Evaluation.pdf. République du Niger and UNICEF, (accessed 25 July 2015).
Robertson 2012 {published data only}
- Robertson L, Mushati P, Eaton JW, Dumba L, Mavise G, Makoni J, et al. Effects of unconditional and conditional cash transfers on child health and development in Zimbabwe: a cluster‐randomised trial. The Lancet 2013;381(9874):1283‐92. [DOI: 10.1016/S0140-6736(12)62168-0] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson L, Mushati P, Eaton JW, Dumba L, Mavise G, Makoni JC, et al. Conditional cash transfers improve birth registration and school attendance amongst orphans and vulnerable children in Manicaland, Zimbabwe [Abstract]. Journal of the International AIDS Society 2012;15(Suppl 3):158‐9. [Google Scholar]
Santos 2011 {published data only}
- Santos LM, Pasquim EM, Santos SM. Cash transfer programs in Brazil: a multidimensional study of the implementation of Bolsa Escola, Bolsa Alimentação and Cartão Alimentacão program implementation [Programas de transferência de renda no Brasil: um estudo multidimensional da implementação do Bolsa Escola, Bolsa Alimentão e Cartão Alimentação]. Ciência & Saúde Coletiva 2011;16(3):1821‐34. [DOI: 10.1590/S1413-81232011000300018] [DOI] [PubMed] [Google Scholar]
Save the Children 2009 {published data only}
- Save the Children. How Cash Transfers Can Improve the Nutrition of the Poorest Children: Evaluation of a Pilot Safety Net Programme in Southern Niger. London: Save the Children, 2009. [Google Scholar]
Schwab 2013 {published data only}
- Schwab B, Margolies A, Hoddinott J. Impact Evaluation of Cash and Food Transfers for the Seasonal Emergency Safety Net in Hajjah and Ibb Governorates, Yemen: Endline Report. Washington, DC: International Food Policy Research Institute, 2013. [Google Scholar]
Tadesse 2014 {published data only}
- Tadesse S. Cash transfers for Somali refugees: experiences from a pilot programme in Ethiopia. Nutrition Exchange 2014;4:25‐6. [Google Scholar]
Woolard 2014 {published data only}
- Woolard I, Leibbrandt M. The evolution and impact of unconditional cash transfers in South Africa. Rondebosch, South Africa: Southern Africa Labour and Development Research Unit; 2010. Working paper.
References to studies awaiting assessment
Devereux 2008b {published data only}
- Devereux S, Mthinda C, Power F, Sakala P, Suka A. Smart Cards for Smart Women: an Evaluation of Concern Worldwide’s Dowa Emergency Cash Transfer Project in Malawi, 2006/07. Lilongwe: Concern Worldwide, 2008. [Google Scholar]
References to ongoing studies
REFANI‐N {published data only}
- ISRCTN25360839. Effectiveness and cost effectiveness of early initiation and longer duration of emergency/seasonal unconditional cash transfers on children’s nutritional status in Tahoua, Niger. http://www.controlled‐trials.com/ISRCTN25360839 (accessed 25 July 2015). [DOI: 10.1186/ISRCTN25360839] [DOI]
REFANI‐P {published data only}
- ISRCTN10761532. REFANI Pakistan study ‐ effect of differing modalities of cash transfers on reducing the risk of wasting in children in Pakistan. http://www.controlled‐trials.com/ISRCTN10761532 (accessed 25 July 2015). [DOI: 10.1186/ISRCTN10761532] [DOI]
Additional references
Adato 2009
- Adato M, Bassett L. Social protection to support vulnerable children and families: the potential of cash transfers to protect education, health and nutrition. AIDS Care 2009;21(Suppl 1):60‐75. [DOI: 10.1080/09540120903112351] [DOI] [PMC free article] [PubMed] [Google Scholar]
Arnold 2011
- Arnold C, Conway T, Greenslade M. Cash Transfers Literature Review. London: Department for International Development, 2011. [Google Scholar]
Bailey 2007
- Bailey S, Walsh S. The use of cash in emergency and post‐emergency non‐food item programs: a case study from the Democratic Republic of Congo. http://sites.tufts.edu/jha/archives/49 (accessed 27 July 2014).
Baird 2011
- Baird S, McIntosh C, Özler B. Cash or condition? Evidence from a cash transfer experiment. Quarterly Journal of Economics 2011;126(4):1709‐53. [DOI: 10.1093/qje/qjr032] [DOI] [Google Scholar]
Baird 2013
- Baird S, Ferreira FHG, Özler B, Woolcock M. Relative effectiveness of conditional and unconditional cash transfers for schooling outcomes in developing countries: a systematic review. Campbell Systematic Reviews 2013;8. [DOI: 10.4073/csr.2013.8] [DOI] [Google Scholar]
Balshem 2011
- Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. Journal of Clinical Epidemiology 2011;64(4):401‐6. [DOI: 10.1016/j.jclinepi.2010.07.015] [DOI] [PubMed] [Google Scholar]
Barrientos 2006
- Barrientos A, DeJong J. Reducing child poverty with cash transfers: a sure thing?. Development Policy Review 2006;24(5):537‐52. [DOI: 10.1111/j.1467-7679.2006.00346.x] [DOI] [Google Scholar]
Barrientos 2008
- Barrientos A, Hulme D. Social protection for the poor and poorest in developing countries: reflections on a quiet revolution. http://papers.ssrn.com/sol3/papers.cfm?abstract_id=1265576 (accessed 23 July 2014).
Bassani 2013
- Bassani DG, Arora P, Wazny K, Gaffey MF, Lenters L, Bhutta ZA. Financial incentives and coverage of child health interventions: a systematic review and meta‐analysis. BMC Public Health 2013;13(Suppl 3):S30. [DOI: 10.1186/1471-2458-13-S3-S30] [DOI] [PMC free article] [PubMed] [Google Scholar]
Benach 2010a
- Benach J, Solar O, Santana V, Castedo A, Chung H, Muntaner C, et al. A micro‐level model of employment relations and health inequalities. International Journal of Health Services 2010;40(2):223‐7. [DOI: 10.2190/HS.40.2.d] [DOI] [PubMed] [Google Scholar]
Benach 2010b
- Benach J, Solar O, Vergara M, Vanroelen C, Santana V, Castedo A, et al. Six employment conditions and health inequalities: a descriptive overview. International Journal of Health Services 2010;40(2):269‐80. [DOI: 10.2190/HS.40.2.g] [DOI] [PubMed] [Google Scholar]
Boccia 2011
- Boccia D, Hargreaves J, Lönnroth K, Jaramillo E, Weiss J, Uplekar M, et al. Cash transfer and microfinance interventions for tuberculosis control: review of the impact evidence and policy implications. International Journal of Tuberculosis and Lung Disease 2011;15(Suppl 2):S37‐49. [DOI: 10.5588/ijtld.10.0438] [DOI] [PMC free article] [PubMed] [Google Scholar]
Borjas 2013
- Borjas GJ. Labor economics. 6th Edition. New York: McGraw‐Hill Irwin, 2013. [Google Scholar]
Bornemesiza 2010
- Bornemisza O, Ranson MK, Poletti TM, Sondorp E. Promoting health equity in conflict‐affected fragile states. Social Science and Medicine 2010;70(1):80‐8. [DOI: 10.1016/j.socscimed.2009.09.032] [DOI] [PubMed] [Google Scholar]
Carpenter 2012
- Carpenter S, Slater R, Mallett R. Social protection and basic services in fragile and conflict‐affected situations: a global review of the evidence. London: Secure Livelihoods Research Consortium, Overseas Development Institute; 2012. Working paper no. 8.
CCEMG 2011
- Campbell and Cochrane Equity Methods Group. Equity checklist for systematic review authors. www.equity.cochrane.org/sites/equity.cochrane.org/files/uploads/EquityChecklist2012.pdf (accessed 23 July 2014).
Clarke 2014
- Clarke M, Allen C, Archer F, Wong D, Eriksson A, Puri J. What evidence is available and what is required, in humanitarian assistance?. New Delhi: International Initiative for Impact Evaluation; 2014. Scoping paper 1.
Cochrane PHG 2011
- Cochrane Public Health Group. Guide for developing a Cochrane protocol. http://ph.cochrane.org/sites/ph.cochrane.org/files/uploads/Guide%20for%20PH%20protocol_Nov%202011_final%20for%20website.pdf (accessed 23 July 2014).
CSDH 2008
- Commission on Social Determinants of Health. Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health. Geneva: World Health Organization, 2008. [DOI] [PubMed] [Google Scholar]
Devereux 2005
- Devereux S, Marshall J, MacAskill J, Pelham L. Making Cash Count: Lessons from Cash Transfer Schemes in East and Southern Africa for Supporting the Most Vulnerable Children and Households. London: Save the Children UK, HelpAge International, and Institute of Development Studies, 2005. [Google Scholar]
Doocy 2014
- Doocy S, Tappis H. The effectiveness and efficiency of cash‐based approaches in protracted and sudden onset emergencies: a systematic review [Title registration]. Campbell Collaboration. Oslo, 2014 April 6.
Eaton 2004
- Eaton WW, Muntaner C, Smith C, Tien A, Ybarra M. Center for Epidemiologic Studies Depression Scale: Review and Revision (CESD and CESD‐R). In: Maruish ME editor(s). The Use of Psychological Testing for Treatment Planning and Outcomes Assessment. 3rd Edition. Mahwah, NJ: Lawrence Erlbaum, 2004:363‐77. [Google Scholar]
EPOC 2012
- Cochrane Effective Practice and Organisation of Care Group. EPOC Resources for review authors. Suggested risk of bias criteria for EPOC reviews. Oslo: Norwegian Knowledge Centre for the Health Services; 2012. Available at: http://epoc.cochrane.org/epoc‐specific‐resources‐review‐authors.
Filmer 2011
- Filmer D, Schady N. Does more cash in conditional cash transfer programs always lead to larger impacts on school attendance?. Journal of Development Economics 2011;96(1):150‐7. [DOI: 10.1016/j.jdeveco.2010.05.006] [DOI] [Google Scholar]
Fiszbein 2009
- Fiszbein A, Schady N. Conditional Cash Transfers: Reducing Present and Future Poverty. Washington, DC: World Bank, 2009. [Google Scholar]
Forde 2012
- Forde I, Rasanathan K, Krech R. Cash transfer schemes and the health sector: making the case for greater involvement. Bulletin of the World Health Organization 2012;90(7):551‐3. [DOI: 10.2471/BLT.11.097733] [DOI] [PMC free article] [PubMed] [Google Scholar]
Frankenberg 1996
- Frankenberg WK, Dodds JB. The Denver Developmental Screening Test. Denver: University of Colorado, 1996. [Google Scholar]
Gaarder 2010
- Gaarder MM, Glassman A, Todd J. Conditional cash transfers and health: unpacking the causal chain. Journal of Development Effectiveness 2010;2(1):6‐50. [DOI: 10.1080/19439341003646188] [DOI] [Google Scholar]
Gaarder 2011
- Gaarder M, Snilstveit B, Waddington H. Conditional and unconditional cash transfers for health and nutritional outcomes in poor families in low‐ and middle‐income countries: a systematic review [Title registration]. Campbell Collaboration. Oslo, Norway, 2011 November 18.
Garcia 2012
- Garcia M, Moore CMT. The Cash Dividend: the Rise of Cash Transfer Programs in Sub‐Saharan Africa. Washington, DC: World Bank, 2012. [Google Scholar]
GHA 2014
- Global Humanitarian Assistance. Defining humanitarian assistance. http://www.globalhumanitarianassistance.org/data‐guides/defining‐humanitarian‐aid (accessed 23 July 2014).
Guha‐Sapir 2010
- Guha‐Sapir D, D'aoust O. Demographic and health consequences of civil conflict. Washington, DC: World Bank; 2011. World Development Report 2011: Background paper.
Guha‐Sapir 2013
- Guha‐Sapir D, Hoyois P, Below R. Annual Disaster Statistical Review 2012: The Numbers and Trends. Brussels: Centre for Research on the Epidemiology of Disasters, 2013. [Google Scholar]
Harvey 2011
- Harvey P, Bailey S. Cash Transfer Programming in Emergencies: Good Practice Review 11. London: Humanitarian Practice Network, Overseas Development Institute, 2011. [Google Scholar]
Heise 2013
- Heise L, Lutz B, Ranganathan M, Watts C. Cash transfers for HIV prevention: considering their potential. Journal of the International AIDS Society 2013;16(1):18615. [DOI: 10.7448/IAS.16.1.18615] [DOI] [PMC free article] [PubMed] [Google Scholar]
Heltberg 2007
- Heltberg R. Helping South Asia cope better with natural disasters: the role of social protection. Development Policy Review 2007;25(6):681‐98. [DOI: 10.1111/j.1467-7679.2007.00392.x] [DOI] [Google Scholar]
Higgins 2011a
- Higgins JPT, Green S, editors. Chapter 8: Assessing risk of bias in included studies. In: Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from http://handbook.cochrane.org/. The Cochrane Collaboration.
Higgins 2011b
- Higgins JPT, Green S, editors. Chapter 9: Analysing data and undertaking meta‐analyses. In: Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from http://handbook.cochrane.org/. The Cochrane Collaboration.
Higgins 2011c
- Higgins JPT, Green S, editors. Chapter 10: Addressing reporting biases. In: Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from http://handbook.cochrane.org/.
Higgins 2011d
- Higgins JPT, Green S, editors. Chapter 11: Presenting results and ‘Summary of findings’ tables. In: Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from http://handbook.cochrane.org/. The Cochrane Collaboration.
Higgins 2011e
- Higgins JPT, Green S, editors. Chapter 16: Special topics in statistics. In: Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from http://handbook.cochrane.org/. The Cochrane Collaboration.
Lagarde 2009
- Lagarde M, Haines A, Palmer N. The impact of conditional cash transfers on health outcomes and use of health services in low and middle income countries. Cochrane Database of Systematic Reviews 2009, Issue 4. [DOI: 10.1002/14651858.CD008137] [DOI] [PMC free article] [PubMed] [Google Scholar]
Leaning 2013
- Leaning J, Guha‐Sapir D. Natural disasters, armed conflict, and public health. New England Journal of Medicine 2013;369:1836‐42. [DOI: 10.1056/NEJMc1315507] [DOI] [PubMed] [Google Scholar]
Lundberg 2010
- Lundberg O, Fritzell J, Aberg Yngwe M, Kölgard ML. The potential power of social policy programmes: income redistribution, economic resources and health. International Journal of Social Welfare 2010;19:S2–S13. [DOI: 10.1111/j.1468-2397.2010.00727.x] [DOI] [Google Scholar]
Manley 2013
- Manley J, Gitter S, Slavchevska V. How effective are cash transfers at improving nutritional status?. World Development 2013;48:133‐55. [DOI: 10.1016/j.worlddev.2013.03.010] [DOI] [Google Scholar]
Marmot 2012
- Marmot M, Allen J, Bell R, Bloomer E, Goldblatt P, Consortium for the European Review of Social Determinants of Health and the Health Divide. WHO European review of social determinants of health and the health divide. The Lancet 2012;380(9846):1011‐29. [DOI: 10.1016/S0140-6736(12)61228-8] [DOI] [PubMed] [Google Scholar]
Mayo‐Wilson 2011
- Mayo‐Wilson E, Imdad A, Herzer K, Yakoob MY, Bhutta ZA. Vitamin A supplements for preventing mortality, illness, and blindness in children aged under 5: systematic review and meta‐analysis. BMJ 2011;343:d5094. [DOI: 10.1136/bmj.d5094] [DOI] [PMC free article] [PubMed] [Google Scholar]
McCarthy 1972
- McCarthy D. The McCarthy Scales of Children’s Abilities. New York: The Psychological Corporation, 1972. [Google Scholar]
McMichael 2006
- McMichael AJ, Woodruff RE, Hales S. Climate change and human health: present and future risks. The Lancet 2006;367(9513):859‐69. [DOI: 10.1016/S0140-6736(06)68079-3] [DOI] [PubMed] [Google Scholar]
Pega 2012
- Pega F, Blakely T, Carter K, Sjöberg O. The explanation of a paradox? A commentary on Mackenbach with perspectives from research on financial credits and risk factor trends. Social Science and Medicine 2012;75(4):770‐3. [DOI: 10.1016/j.socscimed.2012.03.052] [DOI] [PubMed] [Google Scholar]
Pega 2013
- Pega F, Carter K, Blakely T, Lucas P. In‐work tax credits for families and their impact on health status in adults. Cochrane Database of Systematic Reviews 2013, Issue 8. [DOI: 10.1002/14651858.CD009963.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pega 2014a
- Pega F, Walter S, Liu SY, Pabayo R, Lhachimi SK, Saith R. Unconditional cash transfers for reducing poverty and vulnerabilities: effect on use of health services and health outcomes in low‐ and middle‐income countries. Cochrane Database of Systematic Reviews 2014, Issue 6. [DOI: 10.1002/14651858.CD011135] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pega 2014b
- Pega F, Walter S, Liu SY, Lhachimi SK. Unconditional cash transfers for assistance in humanitarian disasters: effect on use of health services and health outcomes in low‐ and middle‐income countries. Cochrane Database of Systematic Reviews 2014, Issue 8. [DOI: 10.1002/14651858.CD011247] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pega 2015
- Pega F, Shaw C, Rasanathan K, Yablonski J, Kawachi I, Hales S. Climate change, cash transfers and population health. Bulletin of the World Health Organization in press. [DOI] [PMC free article] [PubMed]
Pettifor 2012
- Pettifor A, MacPhail C, Nguyen N, Rosenberg M. Can money prevent the spread of HIV? A review of cash payments for HIV prevention. AIDS and Behavior 2012;16(7):1729‐38. [DOI: 10.1007/s10461-012-0240-z] [DOI] [PMC free article] [PubMed] [Google Scholar]
Popay 2008
- Popay J. Should disadvantaged people be paid to take care of their health? No. BMJ 2008;337:a594. [DOI: 10.1136/bmj.a594] [DOI] [PMC free article] [PubMed] [Google Scholar]
Puri 2014
- Puri J, Aladysheva A, Iversen V, Ghorpade Y, Brück T. What methods may be used in impact evaluations of humanitarian assistance?. New Delhi: International Initiative for Impact Evaluation; 2014. Working Paper 22.
RevMan [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Schubert 2006
- Schubert B, Slater R. Social cash transfers in low‐income African countries: conditional or unconditional?. Development Policy Review 2006;24(5):571‐8. [DOI: 10.1111/j.1467-7679.2006.00348.x] [DOI] [Google Scholar]
Schünemann 2009
- Schünemann H, Brożek J, Oxman A. Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach. http://www.who.int/hiv/topics/mtct/grade_handbook.pdf (accessed 1 September 2015).
Sjöberg 2010
- Sjöberg O. Social insurance as a collective resource: unemployment benefits, job insecurity and subjective well‐being in a comparative perspective. Social Forces 2010;88(3):1281–304. [DOI: 10.1353/sof.0.0293] [DOI] [Google Scholar]
Spiegel 2010
- Spiegel PB, Checchi F, Colombo S, Paik E. Health‐care needs of people affected by conflict: future trends and changing frameworks. The Lancet 2010;375(9711):341‐5. [DOI: 10.1016/S0140-6736(09)61873-0] [DOI] [PubMed] [Google Scholar]
Sridhar 2006
- Sridhar D, Duffield A. A Review of the Impact of Cash Transfer Programmes on Child Nutritional Status and Some Implications for Save the Children UK Programmes. London: Save the Children, 2006. [Google Scholar]
Stocker 2013
- Stocker TF, Qin D, Plattner GK, Tignor M, Allen SK, Boschung J, et al. Climate change 2013: the physical science basis. Cambridge; Cambridge University Press; 2013. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change.
Tierney 2007
- Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time‐to‐event data into meta‐analysis. Trials 2007;8:16. [DOI: 10.1186/1745-6215-8-16] [DOI] [PMC free article] [PubMed] [Google Scholar]
UNCEB 2009
- United Nations Chief Executives Board. Social Protection Floor Initiative. www.socialprotectionfloor‐gateway.org/index.html (accessed 23 July 2014).
UNRISD 2010
- United Nations Research Institute for Social Development. Combating Poverty and Inequality: Structural Change, Social Policy and Politics. Geneva: United Nations Research Institute for Social Development, 2010. [Google Scholar]
WHO 2008
- World Health Organization. Social Determinants of Health in Countries in Conflict: a Perspective from the Eastern Mediterranean Region. Cairo: Regional Office for the Eastern Mediterranean, World Health Organization, 2008 (WHO Regional Publications, Eastern Mediterranean Series 32). [Google Scholar]
WHO 2011
- World Health Organization. Closing the Gap: Policy into Practice on Social Determinants of Health. Geneva: World Health Organization, 2011. [Google Scholar]
World Bank 2011a
- World Bank. Safety nets and transfers: glossary. http://web.worldbank.org/WBSITE/EXTERNAL/TOPICS/EXTSOCIALPROTECTION/EXTSAFETYNETSANDTRANSFERS/0,,contentMDK:22200792˜pagePK:210058˜piPK:210062˜theSitePK:282761,00.html (accessed 23 July 2014).
World Bank 2011b
- World Bank. Learning from the “Atención a Crisis” Pilot Program in Nicaragua’s drought region. http://web.worldbank.org/WBSITE/EXTERNAL/COUNTRIES/LACEXT/EXTLACREGTOPPOVANA/0,,contentMDK:21762443˜pagePK:34004173˜piPK:34003707˜theSitePK:841175,00.html (accessed 22 October 22 2014).
World Bank 2014a
- World Bank. Social protection and labour. www.worldbank.org/en/topic/socialprotectionlabor (accessed 23 July 2014).
World Bank 2014b
- World Bank. Country and lending groups. www.data.worldbank.org/about/country‐classifications/country‐and‐lending‐groups#Low_income (accessed 23 July 2014).


