Abstract
Introduction
We describe a new service model, the Orthopaedic Assessment Unit (OAU), designed to provide care for trauma patients during the COVID-19 pandemic. Patients without COVID-19 symptoms and isolated musculoskeletal injuries were redirected to the OAU.
Methods
We prospectively reviewed patients throughput during the peak of the global pandemic (7 May 2020 to 7 June 2020) and compared with our historic service provision (7 May 2019 to 7 June 2019). The Mann–Whitney and Fisher Exact tests were used to test the statistical significance of data.
Results
A total of 1,147 patients were seen, with peak attendances between 11am and 2pm; 96% of all referrals were seen within 4h. The majority of patients were seen by orthopaedic registrars (52%) and nurse practitioners (44%). The majority of patients suffered from sprains and strains (39%), followed by fractures (22%) and wounds (20%); 73% of patients were discharged on the same day, 15% given follow up, 8% underwent surgery and 3% were admitted but did not undergo surgery. Our volume of trauma admissions and theatre cases decreased by 22% and 17%, respectively (p=0.058; 0.139). There was a significant reduction of virtual fracture clinic referrals after reconfiguration of services (p<0.001).
Conclusions
Rapid implementation of a specialist OAU during a pandemic can provide early definitive trauma care while exceeding national waiting time standards. The fall in trauma attendances was lower than anticipated. The retention of orthopaedic staff in the department to staff the unit and maintain a high standard of care is imperative.
Keywords: COVID-19, Orthopaedic trauma, Service reconfiguration, Specialist assessment unit, Redeployment
Introduction
The COVID-19 pandemic presents significant challenges to healthcare systems globally,1,2 with more than 12 million cases in 215 countries being reported; contributing to more than 556,000 deaths to date.3 In the UK, the NHS reshaped its workforce and clinical services to meet the new demands and to provide best possible care for all patients.4 The reconfiguration of services was left to the discretion of individual healthcare trusts in the UK. The British Orthopaedic Association (BOA) released emergency guidance to aid pragmatic decision-making during these unprecedented times.5 These recommendations included restructuring orthopaedic outpatient and theatre services, with emphasis on conservative treatment and minimising hospital visits.5 Routine elective orthopaedic work was halted and orthopaedic junior staff were redeployed to aid the response to the COVID pandemic, as it was also expected that the burden of trauma would fall during the lockdown period.
We describe our experiences setting up a new service model in the form of an Orthopaedic Assessment Unit (OAU). The primary aim of this reconfigured service was to liberate personnel and resources in our emergency department (ED), allowing timely management of ill patients assumed to be affected by COVID-19. The secondary aim was to deliver initial assessment and early definitive care for all non-COVID acute trauma patients.
Methods
Service reconfiguration and patient triage
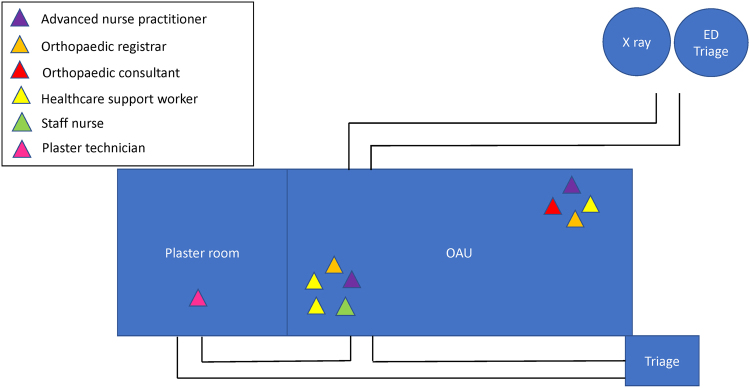
As one of the Major Trauma Centres (MTC) in Scotland, our hospital adapted quickly to challenges posed by COVID-19. The entire ED was transformed into a ‘red zone’ (assumed contagious area), where any patients with COVID-19 symptoms were assessed. Acute musculoskeletal services, including orthopaedic trauma and minor injuries unit, were physically re-sited to a ground-floor minor theatre suite and assigned as the ‘green zone’ for non-COVID patients. The layout of the OAU is illustrated in Figure 1. The OAU was staffed 24h a day and had a capacity of seven beds and three sitting cubicles. During the COVID-19 pandemic, the responsibility for ‘minor’ nonorthopaedic injuries was also absorbed by the Orthopaedic Department, with assistance from advanced nurse practitioners with a mixed background of emergency medicine and orthopaedic surgery.
Figure 1 .
Layout of OAU. ED = emergency department; OAU = orthopaedic assessment unit.
All nonambulatory patients were triaged at ED reception by experienced nurses. Clinically stable patients with no COVID-19 symptoms and isolated musculoskeletal injuries were redirected immediately to the OAU. All ambulatory patients were triaged at the OAU front door, which had a separate entrance from the ED. This new unit was staffed by an orthopaedic consultant; three orthopaedic registrars; two advanced nurse practitioners; one plaster technician; one staff nurse and three healthcare support workers.
Common orthopaedic injuries, such as dorsally displaced distal radius fractures, were manipulated and put into moulded plaster casts in the OAU by orthopaedic registrars on the patient’s first contact. Before the COVID-19 pandemic, these injuries were usually put into simple back slabs by our ED during out of hours and referred to the virtual fracture clinic (VFC) for further management. Furthermore, penetrating injuries and lacerations to limbs that were not contaminated and without neurological or vascular deficit were routinely washed and sutured in the OAU by orthopaedic registrars. Previously, these patients may have required hospital admission for wound debridement in the main theatre suite.
In our MTC, the orthopaedic team shares spinal and hand emergency service provision with the neurosurgery and plastic surgery teams, respectively. These rotas are described in the Results section. Our elective Orthopaedic Unit, which is located 2 miles away from the MTC, was used for musculoskeletal tumour and urgent elective cases along with a daily ambulatory trauma list. Routine elective operations were cancelled, in line with clinical practice nationally. A daily trauma theatre operated from Monday to Saturday at the MTC, with an additional second designated trauma theatre on Mondays, Wednesdays and Fridays. Daily access to the CEPOD equivalent emergency theatre was also utilised when necessary.
Data collection and analysis
This study was registered with the local Quality Improvement and Assurance Committee. We collected data prospectively during the COVID-19 pandemic, from 7 May to 7 June 2020 (total of 32 days). We also collected data from 7 May to 7 June 2019 for admission rate and trauma operation cases. Electronic patient databases including Trakcare, Bluespier, the hip fracture audit database and admission records were used to collect the information required. Information such as patient demographics, injuries, time of arrival, time of departure and clinical outcomes were collected.
Data on fracture clinics and VFCs were collected from the electronic clinic record. Paediatric cases were not included in this study as our hospital has a separate paediatric hospital. The number of patient attendances and percentage of patients being seen within 4h in the main ED, from 3 May to 6 June 2020 and from 5 May to 8 June 2019 (total of 35 days, respectively), were collected from electronic NHS Perform records, which present information on a weekly basis.6
Statistical analysis was performed using Statistical Package for the Social Sciences software (SPSS for Microsoft, Version 25). The mean, standard deviation and percentage were used for descriptive statistics. Data were tested for normal distribution using the Kolmogorov–Smirnov test. The Mann–Whitney test was used to test the statistical significance of data relating to trauma admissions and operations. The Fisher Exact test was used to test the statistical significance of data relating to clinic attendances. A p-value <0.05 was used as the criterion for statistical significance.
Results
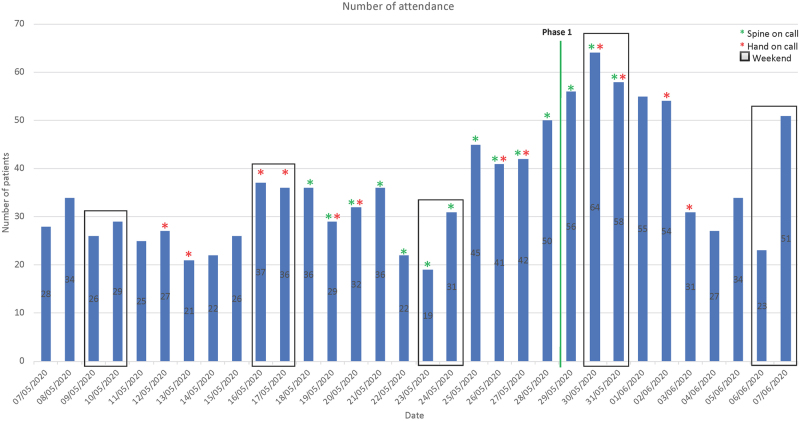
In the period of interest, there were 3500 ED attendances in 2020 and 5926 ED attendances in 2019—a 41% reduction in ED attendances.6 In the 32 days following service reconfiguration in 2020, 1,147 patients were directed to the OAU, with an average of 36 patients attending the unit each day during national lockdown. There was an upward trend of patient attendances towards the first phase of lifting lockdown (29 May 2020).7 The details of the patient attendances are outlined in Figure 2.
Figure 2 .
Breakdown of the number of patient attendances over a 32-day period
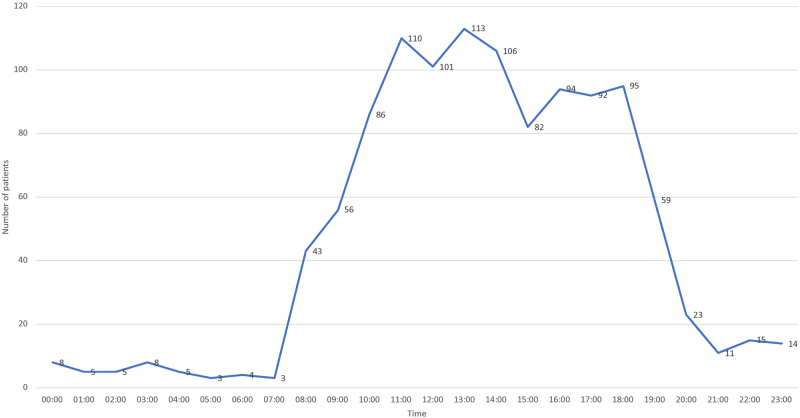
The mean patient age was 47 years, with a standard deviation of 20 years. We had a similar proportion of female and male patients (female:male, 598:549). Complete electronic discharge data was available for 1,140/1,147 (99%) patients and complete clinical information was available for 1,123/1,147 (98%) patients; 96% of the patients were seen within 4hr; the average time to review and discharge was 1hr 27min with a standard deviation of 1hr 11min. Peak attendance was observed between 11am and 2pm (Figure 3). During the same period, 88% and 95% of patients were seen within the waiting time target of 4h in ED in 2019 and 2020, respectively.6
Figure 3 .
Total number of patient attendances in 32 days over a 24h period
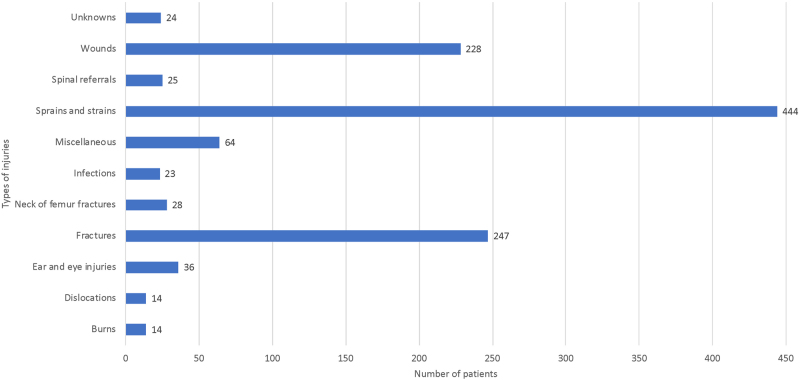
The majority of the patients were seen by orthopaedic registrars (52%) or nurse practitioners (44%). The remaining patients were seen by consultants or a junior doctor (less than ST2 grade). Most patients suffered from sprains and strains (39%); fractures (22%) and wounds (20%) (Figure 4); 73% of patients were discharged on the same day, 15% of patients were given fracture clinic follow-up appointments, 8% of patients underwent surgery and 3% of patients were admitted but did not undergo surgery. A total of 34% of surgical cases were classified as ambulatory trauma suitable for operative treatment at our elective hospital.
Figure 4 .
Types of injuries presented to the unit
There was a total of 203 patients referred to VFC and 924 attendances to fracture clinics between 7 May and 7 June 2019, in comparison to only 1 patient being referred to VFC and 461 attendances to fracture clinics between 7 May and 7 June 2020 (p<0.001). A total of 189 patients were admitted to our trauma unit between 7 May and 7 June 2019, with an average of 6 patients each day; in comparison with 147 patients between 7 May and 7 June 2020, with an average of 5 patients each day (p=0.058).
There were a total of 183 theatre cases between 7 May to 7 June 2019, with an average of 6 cases each day, in comparison with 151 patients between 7 May and 7 June 2020, with an average of 5 patients each day (p=0.139). Our total volume of trauma admissions and theatre cases decreased by 22% and 17%, respectively, but this did not reach statistical significance. There were 48 hip fracture patients between 7 May and 7 June 2019, whereas there were 45 hip fracture patients between 7 May and 7 June 2020—again, not a significant decrease.
Discussion
The COVID-19 pandemic has brought unprecedented challenges to healthcare systems globally. Our predicted reduction of total volume of trauma admissions and theatre cases during the lockdown period was less than current published studies.8–11 Our volume of hip fracture admissions remained stable during the COVID-19 pandemic and this finding is consistent with both UK and Spanish studies.10–12 During the lockdown period the majority of elective orthopaedic centres cancelled routine elective work.
Due to the combination of decreased elective workload and initial expectation of decreased trauma workload, junior orthopaedic trainees were redeployed. Published reports on experiences with redeployment have generally been positive.13–15 However, the expected significant reduction of trauma cases was not observed in our unit, which is consistent with other Scottish studies.9,11 Trauma, tumours and infection still necessitated urgent care. This study demonstrates that there is an important need to retain orthopaedic staff to deliver urgent trauma care and surgical intervention in a timely fashion when indicated.
The OAU in our MTC has assessed more patients than all other surgical specialties combined during the same study period. The Surgical Assessment Unit (SAU) was established to assess and treats patients who were referred primarily, but not restricted to, the general surgical service.16 The SAU accepted subspecialty referrals for general surgery; urology; neurosurgery; gynaecology; plastic; maxillofacial; vascular; cardiothoracic and ear, nose and throat surgery. Data from the SAU in our MTC demonstrated they assessed a total of 797 patients in May 2020,17 compared with the 1,147 seen by the OAU in the same time period. Again this highlights the significant workload that the trauma service routinely deals with.
Our service model supports the use of specialist assessment units, particularly in the surgical division during pandemics. Based on present published data, it is unlikely that the trauma workload would decrease in the event of a potential second wave.9
In our unit, it was apparent that the trauma caseload was dealt with proficiently in the hands of the Trauma and Orthopaedic Department, with at least 96% of patients being seen within 4hr, exceeding the national waiting time target where 95% of patients are to wait no longer than 4hr from arrival to admission, discharge or transfer for ED treatment.18 This potentially had the desirable effect of allowing ED to focus on the medical management of their patients and allow them to achieve 95% of their patients meeting the target within the same time period. In response to COVID-19, we feel that the ED would have been more appropriately supplemented by medical doctors, allowing orthopaedic staff to be retained and provide a fast and high level of care to those who required it.
The VFC model was initially introduced at Glasgow Royal Infirmary in 2011, where patients with fractures that did not require immediate admission were referred to the VFC by ED.19 The VFC is now a regular service provided by most units, where the clinical notes and radiographs are reviewed by orthopaedic consultants. One of the aims of VFC is to ensure that the patient's first clinic attendance takes place at the most appropriate time following injury, with the most appropriate person, rather than the first available appointment.20
As a direct result of having an experienced workforce in the OAU, our unit was capable of delivering early definitive care and this was reflected in the very significant reduction of patients referred to the VFC. The overall fracture clinic attendances were impacted positively by the OAU, with there being 461 fracture clinic attendances during the period 2020, compared to 924 attendances in the corresponding period in 2019, a 50% reduction in clinic attendances.
A new clinic feature was developed in our existing electronic system at short notice to facilitate the OAU service in rapid reaction to the developing COVID-19 pandemic. Initial inexperience in its use resulted in a delay in electronic discharge of patients on the system in a minority of cases, although these patients had physically left the unit. This may have falsely increased recorded times in the department for a small number of cases during this study period, meaning the number of patients seen within the 4h period is in all probability higher than 96%. The majority of the cases did have clear and accurate electronic information on arrival times as it was recorded by the receptionist upon presentation. Overall, our unit exceeded national waiting time standards for ED. We feel this is particularly impressive given the large number of attendances through the OAU during this time period and the implications of reviewing patients utilising appropriate personal protective equipment.
Conclusion
Rapid implementation of a specialist OAU during a pandemic can provide early definitive trauma care while exceeding national waiting time standards. The fall in trauma attendances at our MTC was lower than projected and anticipated, with the OAU assessing more patients than all other surgical specialties combined. Our study demonstrates that retention of orthopaedic staff in the orthopaedic department to run the OAU and maintain a high standard of care is imperative.
Acknowledgements
The authors would like to thank the trauma unit research nurses in Aberdeen Royal Infirmary for information on hip fractures admission and Miss Zalkina Rycko for the information on fracture clinic attendances. We thank Miss Fiona Griffin and Miss Lok Ka Cheung for providing the data on the SAU.
Conflict of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1.Willan J, King AJ, Jeffery Ket al. Challenges for NHS hospitals during covid-19 epidemic. BMJ 2020; 368: m1117. 10.1136/bmj.m1117 [DOI] [PubMed] [Google Scholar]
- 2.Armocida B, Formenti B, Ussai Set al. The Italian health system and the COVID-19 challenge. Lancet Public Health 2020; 5: e253. 10.1016/S2468-2667(20)30074-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Worldometer. COVID-19 coronavirus pandemic .. https://www.worldometers.info/coronavirus/#countries (cited July 2020).
- 4.NHS Employers. Workforce supply and deployment. https://www.nhsemployers.org/covid19/increasing-workforce-supply (cited June 2020).
- 5.British Orthopaedic Association. Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic. https://www.boa.ac.uk/uploads/assets/ee39d8a8-9457-4533-9774e973c835246d/4e3170c2-d85f-4162-a32500f54b1e3b1f/COVID-19-BOASTs-Combined-FINAL.pdf (cited June 2020).
- 6.NHS Performs. Aberdeen royal infirmary. https://www.nhsperforms.scot/hospital-data?hospitalid=3 (cited June 2020).
- 7.Scottish Government. Lockdown begins to ease in Phase 1 https://www.gov.scot/news/lockdown-begins-to-ease-in-phase-1/ (cited June 2020).
- 8.Hernigou J, Morel X, Callewier Aet al. Staying home during ‘COVID-19’ decreased fractures, but trauma did not quarantine in one hundred and twelve adults and twenty eight children and the ‘tsunami of recommendations could not lockdown twelve elective operations. Int Orthop 2020; 44: 1–8. 10.1007/s00264-020-04619-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jenkins P. The early effect of COVID-19 on trauma and elective orthopaedic surgery. https://www.boa.ac.uk/policy-engagement/journal-of-trauma-orthopaedics/journal-of-trauma-orthopaedics-and-coronavirus/the-early-effect-of-covid-19-on-trauma-and-elect.html (cited July 2020).
- 10.Hampton M, Clark M, Baxter Iet al. The effects of a UK lockdown on orthopaedic trauma admissions and surgical cases. Bone & Joint Open 2020; 1: 137–143. 10.1302/2046-3758.15.BJO-2020-0028.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scott CEH, Holland G, Powell-Bowns MFRet al. Population mobility and adult orthopaedic trauma services during the COVID-19 pandemic: fragility fracture provision remains a priority. Bone & Joint Open 2020; 1: 182–189. 10.1302/2046-3758.16.BJO-2020-0043.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nuñez JH, Sallent A, Lakhani Ket al. Impact of the COVID-19 pandemic on an emergency traumatology service: experience at a tertiary trauma centre in Spain. Injury 2020; 51: 1414–1418. 10.1016/j.injury.2020.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sarpong NO, Forrester LA, Levine WN. What’s important: redeployment of the orthopaedic surgeon during the COVID-19 pandemic: perspectives from the trenches. J Bone Joint Surg Am 2020; 102: 1019–1021. 10.2106/jbjs.20.00574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gonzi G, Gwyn R, Rooney Ket al. Our experience as Orthopaedic Registrars redeployed to the ITU emergency rota during the COVID-19 pandemic. https://www.boa.ac.uk/policy-engagement/journal-of-trauma-orthopaedics/journal-of-trauma-orthopaedics-and-coronavirus/our-experience-as-orthopaedic-registrars.html (cited June 2020). [DOI] [PubMed]
- 15.Lezak BA, Cole PA, Jr., Schroder LKet al. Global experience of orthopaedic trauma surgeons facing COVID-19: a survey highlighting the global orthopaedic response. Int Orthop 2020; 44: 1–11. 10.1007/s00264-020-04644-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reeds MG, Andreani SM, Rohatgi Aet al. Surgical assessment units: the key to more efficient emergency surgical provision and admissions? Qual Manag Health Care 2020; 29: 7–14. 10.1097/qmh.0000000000000236 [DOI] [PubMed] [Google Scholar]
- 17.Griffin F, Cheung LL. Surgical Assessment Unit: Figures for May 2020. NHS Grampian; 2020. [Google Scholar]
- 18.Public Health Scotland. Supporting documentation: national targets & standards. https://www.isdscotland.org/Health-Topics/Waiting-Times/Supporting-Documentation/National-Standards.asp (cited June 2020).
- 19.Jenkins PJ, Stephenson DA, Rymaszewski LA. Legal aspects of virtual fracture clinics. https://www.boa.ac.uk/resources/medicolegal-articles/legal-aspects-of-virtual-fracture-clinics.html#:∼:text=In%20response%20to%20these%20deficiencies,experience%20by%20standardising%20treatment%20pathways.&text=Simple%2C%20patient%2Dremovable%2C%20splintage%20was%20provided%20to%20relieve%20pain%20 (cited July 2020).
- 20.Holgate J, Kirmani S, Anand B. Virtual fracture clinic delivers British Orthopaedic Association compliance. Ann R Coll Surg Engl 2017; 99: 51–54. 10.1308/rcsann.2016.0255 [DOI] [PMC free article] [PubMed] [Google Scholar]