Abstract
Introduction
We estimated the number of primary total hip and knee replacements (THR and TKR) that will need to be performed up to the year 2060.
Methods
We used data from The National Joint Registry for England, Wales, Northern Ireland and the Isle of Man on the volume of primary THRs (n=94,936) and TKRs (n=100,547) performed in 2018. We projected future numbers of THR and TKR using a static estimated rate from 2018 applied to population growth forecast data from the UK Office for National Statistics up to 2060.
Results
By 2060, THR and TKR volume would increase from 2018 levels by an estimated 37.7% (n=130,766) and 36.6% (n=137,341), respectively. For both males and females demand for surgery was also higher for patients aged 70 and over, with older patients having the biggest relative increase in volume over time: 70–79 years (44.6% males, 41.2% females); 80–89 years (112.4% males, 85.6% females); 90 years and older (348.0% males, 198.2% females).
Conclusion
By 2060 demand for hip and knee joint replacement is estimated to increase by almost 40%. Demand will be greatest in older patients (70+ years), which will have significant implications for the health service requiring forward planning given that morbidity and resource use is higher in this population. These issues, coupled with two waves of COVID-19, will impact the ability of health services to deliver timely joint replacement to many patients for a number of years, requiring urgent planning.
Keywords: Total hip replacement, Total knee replacement, Future numbers, Demand
Introduction
Primary total hip and knee replacement (THR and TKR) are both common clinically, and are cost-effective interventions for treating arthritis.1–3 These operations cost the National Health Service (NHS) approximately £2 billion annually, which represents 1.5% of the entire NHS budget.4
Given the high procedural volume and associated costs, it is important to estimate future demand for THR and TKR so that policymakers and relevant stakeholders can plan in advance regarding what resources are needed to safely deliver care. This planning is complex and multifactorial because in addition to appropriate finances, considerations must be made for delivering primary and secondary care, implant costs and workforce planning, including training surgeons. Although previous attempts have been made to forecast future UK demand for joint replacement,5 these have limitations. These limitations include using data from over a decade ago, which does not reflect current practice, and changes in funding and health policy, especially given changes promoting enhanced recovery after surgery. In addition, these predictions are no longer likely to reflect future demand, given current data suggest the forecasts for 2035 will soon be surpassed.5
In the UK, substantial issues already exist for delivering timely joint replacement surgery, with orthopaedic surgery having the largest waiting list of any individual specialty.6 Over half of the clinical commissioning groups now ration access to joint replacement to reduce local expenditure,7 leading to more patients seeking surgery in the private sector.8 Lengthy waiting times, sometimes over 1 year, exist for many patients needing THR or TKR.9 Furthermore, planned operations are commonly cancelled, with 60% of cancellations on the day of surgery, usually due to lack of beds, staff and/or operating capacity, which can be compounded during the winter months.10 These substantial delays for patients needing joint replacement can result in more severe pain and mobility problems, which can lead to more complex surgery being required that has less-predictive outcomes.9
In the winter of 2017 hospitals had to cancel elective surgery due to seasonal flu and winter bed pressures, with orthopaedics experiencing an 8.4% fall in surgery compared with the previous winter.11 More recently, the advent of the COVID-19 worldwide pandemic has had drastic and unprecedented implications for healthcare services. In the UK, all elective orthopaedic surgery was cancelled during March 2020 for at least 3 months.12 Elective surgery has subsequently been restarted, but at much lower volumes, with elective theatres unlikely to reach full capacity for a number of months.13 This has been impacted further by a second wave of COVID-19 with associated national lockdowns.14 All these factors are likely to impact on the ability to deliver timely joint replacement to many patients. Estimating the future need for joint replacement at this juncture would be useful for planning healthcare delivery.
We estimated the number of primary THRs and TKRs that will need to be performed up to the year 2060. Estimates were made based on the current volume of primary THR and TKR as recorded in The National Joint Registry (NJR) for England, Wales, Northern Ireland and the Isle of Man, and assuming that the population would grow in line with current national projections.
Methods
Data sources
Current procedural volumes for primary THR and TKR were obtained from publicly available data recorded in the NJR for England, Wales, Northern Ireland and the Isle of Man.15 The registry started collecting data in 2003 and is the world’s largest mandatory joint replacement registry, with excellent levels of data completion and accuracy.16,17 Currently, 94% of patients consent for their personal data to be included in the NJR.15 The NJR collects data on procedures performed in both the NHS and the independent/private sector.
Participants
Counts of the number of patients receiving primary THR and TKR operations, by age and gender in 2018, were obtained from publicly available NJR data.
Population counts
Every 2 years, the UK Office for National Statistics (ONS) calculates national population projections by age and sex for the UK and publishes them on its website. The projections are created by taking the latest mid-year population estimates and combining them with assumptions about likely levels of migration, mortality and fertility in future years. These projections are widely used by government centrally in the UK and also within the devolved nations to make future estimates about education, pensions, taxation and other important policy areas.
We obtained age- and gender-specific population projections for England, Wales and Northern Ireland from the ONS covering the period 2018 to 2060,18 upon which to project the estimated THR and TKR rates.
Analysis
Age was grouped as follows: 18–29, 30–39, 40–49, 50–59, 60–69, 70–79, 80–89 and 90 years and above. Rates for hips and knees were estimated separately. The projection method used counts of primary THR and TKR held at 2018 levels from the NJR, applied to the population forecast data sets which contain population growth estimates by age and gender over time, as forecast by the ONS.
Results
Primary THR
In 2018, the NJR recorded 94,936 primary THRs. The projected overall numbers of primary THRs were 98,114 in 2020, 111,724 in 2030, 121,855 in 2040, 127,383 in 2050 and 130,766 in 2060 (Table 1). By 2060, there would be an estimated 37.7% increase in the number of primary THRs compared with 2018. In males, the increase in the number of primary THRs was 39.3% compared with 36.7% in females.
Table 1 .
Projections for primary total hip replacement (THR) up until 2060
| Recorded number of THR | Projected number of THR | Percentage change 2060 vs 2018 | |||||
|---|---|---|---|---|---|---|---|
| 2018 | 2020 | 2030 | 2040 | 2050 | 2060 | ||
| Total | 94,936 | 98,114 | 111,724 | 121,855 | 127,383 | 130,766 | 37.7 |
| Sex | |||||||
| Males | 38,095 | 39,393 | 44,862 | 48,692 | 51,173 | 53,053 | 39.3 |
| Females | 56,841 | 58,721 | 66,862 | 73,164 | 76,210 | 77,713 | 36.7 |
| Males by age (years) | |||||||
| <30 | 168 | 166 | 169 | 176 | 166 | 172 | 2.7 |
| 30–39 | 502 | 509 | 515 | 506 | 542 | 507 | 1.0 |
| 40–49 | 2,205 | 2,186 | 2,321 | 2,344 | 2,310 | 2,474 | 12.2 |
| 50–59 | 6,416 | 6,535 | 6,023 | 6,401 | 6,482 | 6,408 | −0.1 |
| 60–69 | 11,258 | 11,502 | 13,884 | 12,895 | 13,799 | 14,046 | 24.8 |
| 70–79 | 12,379 | 13,059 | 14,210 | 17,422 | 16,451 | 17,894 | 44.6 |
| 80–89 | 4,922 | 5,170 | 7,358 | 8,331 | 10,643 | 10,454 | 112.4 |
| ≥90 | 245 | 266 | 382 | 614 | 780 | 1,098 | 348.0 |
| Females by age (years) | |||||||
| <30 | 203 | 199 | 202 | 210 | 198 | 206 | 1.4 |
| 30–39 | 527 | 532 | 514 | 501 | 536 | 502 | −4.8 |
| 40–49 | 2,064 | 2,043 | 2,173 | 2,100 | 2,050 | 2,192 | 6.2 |
| 50–59 | 7,212 | 7,364 | 6,763 | 7,194 | 6,966 | 6,817 | −5.5 |
| 60–69 | 15,206 | 15,532 | 18,890 | 17,439 | 18,627 | 18,109 | 19.1 |
| 70–79 | 21,488 | 22,633 | 24,521 | 30,097 | 28,101 | 30,348 | 41.2 |
| 80–89 | 9,504 | 9,759 | 13,034 | 14,493 | 18,349 | 17,639 | 85.6 |
| ≥90 | 637 | 657 | 766 | 1,129 | 1,382 | 1,899 | 198.2 |
In both males and females, the number of primary THRs in 2060 remains fairly constant in patients under 60 years of age. For patients aged between 60 and 69 there was a modest increase in the number of primary THRs by 2060 compared with 2018 (Table 1). For both males and females demand for surgery was higher for patients aged 70 and over, with older patients having the biggest relative increase in volume over time (Figures 1 and 2): 48,242 THRs by 2060 in 70–79 year olds (44.6% males, 41.2% females); 28,093 THRs in 80–89 year olds (112.4% males, 85.6% females); and 2,997 THRs in patients 90 years and older (348.0% males, 198.2% females).
Figure 1 .
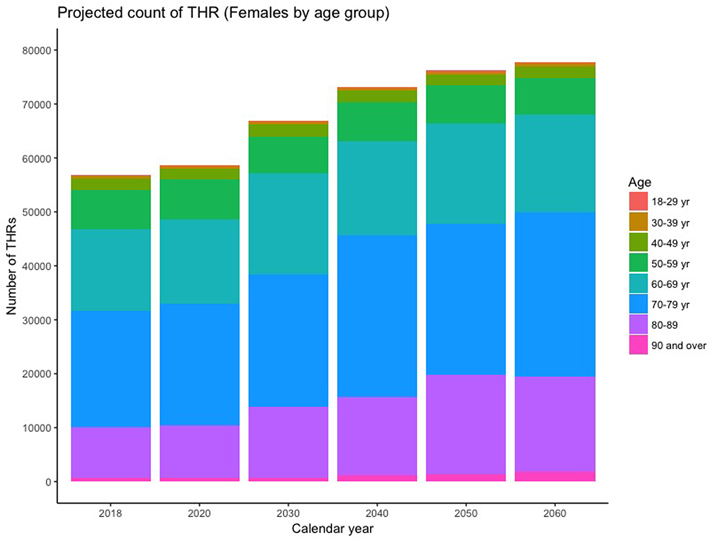
Projections for primary total hip replacement (THR) in females to 2060
Figure 2 .
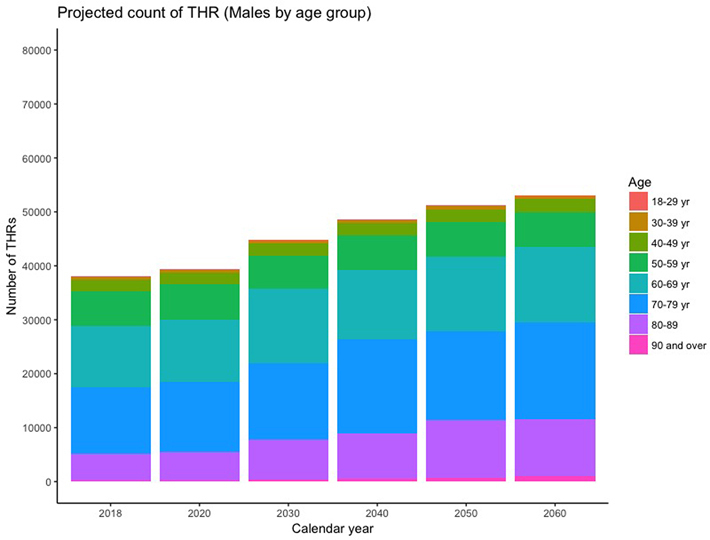
Projections for primary total hip replacement (THR) in males to 2060
Primary TKR
In 2018, the NJR recorded 100,547 primary TKRs. The projected overall numbers of primary TKRs were 104,059 in 2020, 118,503 in 2030, 128,849 in 2040, 133,789 in 2050 and 137,341 in 2060 (Table 2). By 2060, there would be an estimated 36.6% increase in the number of primary TKRs compared with 2018. In males, the increase in the number of primary TKRs was 40.4% compared with 33.6% in females.
Table 2 .
Projections for primary total knee replacement (TKR) to 2060
| Recorded number of TKR | Projected number of TKR | Percentage change 2060 vs 2018 | |||||
|---|---|---|---|---|---|---|---|
| 2018 | 2020 | 2030 | 2040 | 2050 | 2060 | ||
| Total | 100,547 | 104,059 | 118,503 | 128,849 | 133,789 | 137,341 | 36.6 |
| Sex | |||||||
| Males | 44,195 | 45,819 | 52,491 | 57,118 | 59,744 | 62,051 | 40.4 |
| Females | 56,352 | 58,240 | 66,012 | 71,730 | 74,045 | 75,290 | 33.6 |
| Males by age (years) | |||||||
| <30 | 7 | 7 | 7 | 7 | 7 | 7 | 2.7 |
| 30–39 | 74 | 75 | 76 | 75 | 80 | 75 | 1.0 |
| 40–49 | 909 | 901 | 957 | 966 | 952 | 1,020 | 12.2 |
| 50–59 | 6,447 | 6,567 | 6,052 | 6,432 | 6,513 | 6,439 | −0.1 |
| 60–69 | 14,743 | 15,063 | 18,182 | 16,887 | 18,071 | 18,394 | 24.8 |
| 70–79 | 16,445 | 17,348 | 18,877 | 23,145 | 21,854 | 23,772 | 44.6 |
| 80–89 | 5,352 | 5,621 | 8,001 | 9,059 | 11,573 | 11,368 | 112.4 |
| ≥90 | 218 | 236 | 340 | 547 | 694 | 977 | 348.0 |
| Females by age (years) | |||||||
| <30 | 13 | 13 | 13 | 13 | 13 | 13 | 1.4 |
| 30–39 | 102 | 103 | 100 | 97 | 104 | 97 | −4.8 |
| 40–49 | 1,352 | 1,339 | 1,423 | 1,375 | 1,343 | 1,436 | 6.2 |
| 50–59 | 8,284 | 8,459 | 7,768 | 8,264 | 8,001 | 7,831 | −5.5 |
| 60–69 | 17,191 | 17,560 | 21,356 | 19,716 | 21,059 | 20,473 | 19.1 |
| 70–79 | 21,400 | 22,541 | 24,420 | 29,973 | 27,986 | 30,224 | 41.2 |
| 80–89 | 7,699 | 7,905 | 10,558 | 11,740 | 14,864 | 14,289 | 85.6 |
| ≥90 | 311 | 321 | 374 | 551 | 675 | 927 | 198.2 |
In both males and females, the number of primary TKRs in 2060 remains fairly constant in patients under 60 years of age. For patients aged between 60 and 69 there was a modest increase in the number of primary TKRs by 2060 compared with 2018 (Table 2). For both males and females, demand for surgery was higher for patients aged 70 and over, with older patients having the biggest relative increase in volume over time (Figures 3 and 4): 53,996 TKRs by 2060 in 70–79 year olds (44.6% males, 41.2% females); 25,657 TKRs in 80–89 year olds (112.4% males, 85.6% females); and 1,904 TKRs in patients 90 years and older (348.0% males, 198.2% females).
Figure 3 .
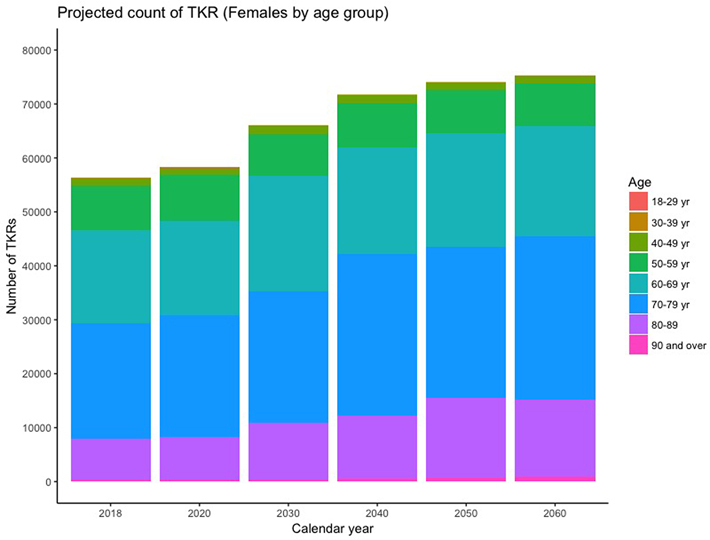
Projections for primary total knee replacement (TKR) in females to 2060
Figure 4 .
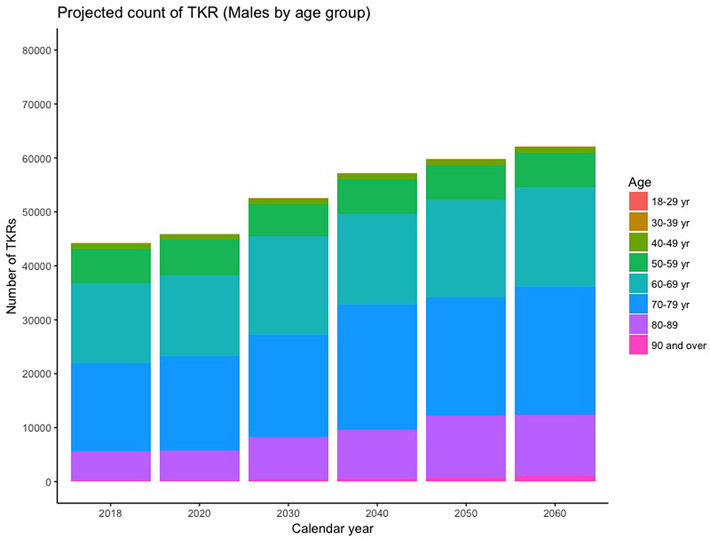
Projections for primary total knee replacement (TKR) in males to 2060
Discussion
We estimate that by 2060 the UK demand for hip and knee joint replacement will increase by almost 40%. Previous studies also show joint replacement demand continues to grow worldwide.5,19 The important new study finding is the increased demand in older male patients, particularly the very elderly, with numbers doubling by 2060 in patients aged 80–89 years and increasing almost fourfold in those aged 90 years and above. The risk of medical and surgical complications after joint replacement, including mortality, is significantly higher in older patients, with patients 40% more likely to have any complication for each subsequent 10 years of age.20–23 This increased patient risk should be accounted for when planning future healthcare.
The NHS already struggles to meet joint replacement demand.9 Substantial delays for surgery can exacerbate pain and mobility problems for patients, who may need stronger analgesia, which can raise issues such as opiate dependence, side-effects and worse outcomes postoperatively.24,25 The impact of surgical delay can be substantial on a patient’s physical and mental health,9 with recent evidence observing that over one-third of patients waiting for surgery have a health state worse than death.26 Ultimately, these delays may lead to patients needing more complex surgery with less-predictive outcomes.
The onset of the COVID-19 pandemic has massively disrupted the delivery of elective surgical care worldwide. In the UK, two waves of COVID-19 with national lockdowns have led to prolonged periods of no, followed by reduced, elective surgery, which is still far from reaching pre-pandemic volumes. It is estimated that 75,000 joint replacement cases were lost in 2020 (37.5% of annual volume).27 Therefore, in 2021, the volume of joint replacement will need to increase by 37.5% to treat all patients needing surgery. This is a substantial increase in surgical volume and healthcare costs over a short timeframe, especially given that our projections for primary THR and TKR volume would not increase to these levels for 40 years in 2060.
Previous population studies have described how future rates of THR and TKR may change. Dixon et al28 used data from English Hospital Episode Statistics, and assumed a continual linear trend, looking at the past linear increase in THR and TKR numbers to predict future numbers increasing at the same linear rate. Kurtz et al19 used Poisson regression combined with US census data making assumptions about observed prior trends in the prevalence of surgery observed from 1990 to 2003 to determine whether this would continue to increase or remain constant. In our previous work, as a secondary analysis, we also incorporated an exponential extrapolation directly from a log-linear model based on previous estimated rates for THR and TKR.5 The main limitation of all these data-driven estimates based on historical increases in THR and TKR numbers is that they do not incorporate or consider constraints in relation to capacity and planning (availability of hospital theatres, beds, surgeons, etc).
It is important to understand the policy context when making such projections. Between 2002–2003 and 2007–2008 the NHS saw a large and sustained increase in investment and funding (average annual increase in real terms of 7.4%). This increased capacity to deliver elective surgery, which included using the independent sector to improve productivity. However, the current climate involves increasingly strained NHS funding, with growth now slower than historical trends.29 There are fewer hospital beds available for joint replacement today than previously, and wards have been closed. Therefore, with a current lack of investment, ever-increasing waiting times, cancellations of elective surgery, further delays from two waves of COVID-19 and limited ability for further efficiency savings than has already been achieved in the past with enhanced recovery protocols, it is unrealistic to base our modelled projections on historical increases in the numbers of THRs and TKRs performed. Furthermore, NJR annual reports show the numbers being stable over recent years.15 Therefore, the projections we produce here are simply based on the current numbers of operations being performed and expected future changes in the age–gender population demographics due to an ageing population.
It is highly unlikely that COVID-19 will be eradicated in the medium term and thus strategies need to be developed to deliver routine care effectively in the presence of COVID-19. Patients undergoing joint replacement commonly suffer from obesity (40% for THR and 56% for TKR)15 and have comorbidities. Taking this together with our projections, we can conclude that the NHS will need to make provision to undertake a large number of joint replacements on old, obese comorbid patients within the context and risks of COVID-19. Our estimates represent an urgent call for engagement of the health service, government, policymakers and relevant stakeholders (such as The British Orthopaedic Association, The Royal College of Surgeons of England and The National Institute for Health and Care Excellence) to now plan what resources are needed to safely deliver primary THR and TKR to patients. This will be complex and must involve consideration of hospital capacity, healthcare resources, staffing, workforce planning and implant procurement. Although some investment has been made with regards to workforce planning (increases in medical and nursing student places and an increase in non-UK trained healthcare professionals working in the NHS),30–32 this alone is unlikely to be enough to deliver the future demand for joint replacement in the UK. Therefore, the only solution we can see is to greatly upscale capacity without delay. The costs of this will be considerable and although THR and TKR are cost-effective treatments,1,33 society needs to decide if it is willing to pay. Failure to act will result in a backlog that is so severe that many patients may die before treatment.
Conclusions
We estimate that by 2060 the UK demand for hip and knee joint replacement will increase by almost 40% from current levels. Demand will be greatest in older male patients (70 years and above) and will have significant implications for the health service that requires forward planning given that morbidity and resource use is higher in this population. The existing backlog of patients awaiting elective joint replacement has been substantially impacted further by two waves of COVID-19. The health service, government, policymakers and relevant stakeholders must therefore use this information to urgently plan what resources are needed to safely deliver primary THR and TKR.
Competing interests
GSM has received personal fees for undertaking medicolegal work for Leigh Day. AWB received a grant funded by Stryker investigating the outcome of a total knee replacement manufactured by Stryker. AJ has received consultancy fees from Freshfields Bruckhaus Deringer and has held advisory board positions (which involved receipt of fees) from Anthera Pharmaceuticals, INC. DJC has no conflicts of interest.
Funding
AWB and AJ are in receipt of a grant from Health Data Research UK and are also supported by the NIHR Biomedical Research Centre at the University Hospitals Bristol NHS Foundation Trust and the University of Bristol. The views expressed in this publication are those of the authors and do not necessarily reflect those of the NHS, the National Institute for Health Research or the Department of Health and Social Care. The funders of this study had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication. AJ had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Author contributions
GSM, DJC and AJ conceived the study and all authors were involved in its design. DJC performed the data analysis. All authors interpreted data and wrote, edited and approved the final report. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. AJ is the guarantor for this study and had final responsibility for manuscript submission.
References
- 1.Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet 2007; 370: 1508–1519. [DOI] [PubMed] [Google Scholar]
- 2.Evans JT, Walker RW, Evans JPet al. . How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet 2019; 393: 655–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Evans JT, Evans JP, Walker RWet al. . How long does a hip replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet 2019; 393: 647–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Institute for Health and Care Excellence. Joint replacement (primary): hip, knee and shoulder. https://www.nice.org.uk/guidance/ng157. [PubMed]
- 5.Culliford D, Maskell J, Judge Aet al. . Future projections of total hip and knee arthroplasty in the UK: results from the UK Clinical Practice Research Datalink. Osteoarthritis Cartilage 2015; 23: 594–600. [DOI] [PubMed] [Google Scholar]
- 6.British Orthopaedic Association. A message for people waiting for joint replacement and other orthopaedic surgery. https://www.boa.ac.uk/resources/a-message-for-people-waiting-for-joint-replacement-and-other-orthopaedic-surgery.html.
- 7.Daily Telegraph. NHS faces £1bn decit and widespread shortages of staff. https://www.telegraph.co.uk/news/2018/2002/2021/nhs-faces-2011bn-deficit-widespread-shortages-staff/.
- 8.Iacobucci G. Nearly 1700 requests for knee and hip surgery were rejected in England last year. BMJ 2018; 362: k3002. [DOI] [PubMed] [Google Scholar]
- 9.British Orthopaedic Association. BOA statement regarding hip and knee waiting times FOI data. https://www.boa.ac.uk/resources/boa-statement-regarding-hip-and-knee-waiting-times-foi-data.html.
- 10.Royal College of Surgeons of England. New Royal College of Surgeons of England survey reveals a lack of beds halted operations in November 2019. https://www.rcseng.ac.uk/news-and-events/media-centre/press-releases/rcs-survey-lack-of-nhs-beds-halted-operations/.
- 11.The Royal College of Surgeons of England. Over 62,000 fewer operations performed this winter, following necessary cancellations. https://www.rcseng.ac.uk/news-and-events/media-centre/press-releases/more-patients-wait-longer-for-elective-surgery/.
- 12.Haddad FS. COVID-19 and orthopaedic and trauma surgery. Bone Joint J 2020; 102-B: 545–546. [DOI] [PubMed] [Google Scholar]
- 13.Oussedik S, Zagra L, Shin GYet al. . Reinstating elective orthopaedic surgery in the age of COVID-19. Bone Joint J 2020; 102-B: 807–810. [DOI] [PubMed] [Google Scholar]
- 14.Xu S, Li Y. Beware of the second wave of COVID-19. Lancet 2020; 395: 1321–1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Joint Registry (NJR). National Joint Registry (NJR) for England, Wales, Northern Ireland and the Isle of Man 16th Annual Report. https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR 16th 20Annual 20Report 2019.pdf.
- 16.Sabah SA, Henckel J, Cook Eet al. . Validation of primary metal-on-metal hip arthroplasties on the National Joint Registry for England, Wales and Northern Ireland using data from the London implant retrieval centre: a study using the NJR dataset. Bone Joint J 2015; 97-B: 10–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sabah SA, Henckel J, Koutsouris Set al. . Are all metal-on-metal hip revision operations contributing to the National Joint Registry implant survival curves?: a study comparing the London implant retrieval centre and National Joint Registry datasets. Bone Joint J 2016; 98-B: 33–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Office for National Statistics . Population projections. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections (cited July 2020).
- 19.Kurtz S, Ong K, Lau Eet al. . Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007; 89: 780–785. [DOI] [PubMed] [Google Scholar]
- 20.Ogino D, Kawaji H, Konttinen Let al. . Total hip replacement in patients eighty years of age and older. J Bone Joint Surg Am 2008; 90: 1884–1890. [DOI] [PubMed] [Google Scholar]
- 21.Hunt LP, Ben-Shlomo Y, Clark EMet al. . 45-day mortality after 467,779 knee replacements for osteoarthritis from the National Joint Registry for England and Wales: an observational study. Lancet 2014; 384: 1429–1436. [DOI] [PubMed] [Google Scholar]
- 22.Hunt LP, Ben-Shlomo Y, Clark EM, Dieppe Pet al. . 90-day mortality after 409,096 total hip replacements for osteoarthritis, from the National Joint Registry for England and Wales: a retrospective analysis. Lancet 2013; 382: 1097–1104. [DOI] [PubMed] [Google Scholar]
- 23.Higuera CA, Elsharkawy K, Klika AKet al. . 2010 Mid-America Orthopaedic Association Physician in Training Award: predictors of early adverse outcomes after knee and hip arthroplasty in geriatric patients. Clin Orthop Relat Res 2011; 469: 1391–1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brat GA, Agniel D, Beam Aet al. . Postsurgical prescriptions for opioid naive patients and association with overdose and misuse: retrospective cohort study. BMJ 2018; 360: j5790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arden N, Altman D, Beard Det al. . Lower limb arthroplasty: can we produce a tool to predict outcome and failure, and is it cost-effective? An epidemiological study. Southampton, UK: Programme Grants for Applied Research, 2017. [PubMed] [Google Scholar]
- 26.Clement ND, Scott CEH, Murray JRDet al. . The number of patients ‘worse than death’ while waiting for a hip or knee arthroplasty has nearly doubled during the COVID-19 pandemic. Bone Joint J 2021; 103-B: 672–680. [DOI] [PubMed] [Google Scholar]
- 27.National Joint Registry. NJR StatsOnline. https://www.njrcentre.org.uk/njrcentre/Healthcare-providers/Accessing-the-data/StatsOnline/NJR-StatsOnline.
- 28.Dixon T, Shaw M, Ebrahim S, Dieppe P. Trends in hip and knee joint replacement: socioeconomic inequalities and projections of need. Ann Rheum Dis 2004; 63: 825–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Luchinskaya D, Simpson P, Stoye G.. UK health and social care spending. https://www.ifs.org.uk/publications/8879.
- 30.Gov.UK. Press release: NHS nurse numbers continue to rise with 13,502 more than last year. https://www.gov.uk/government/news/nhs-nurse-numbers-continue-to-rise-with-13502-more-than-last-year.
- 31.UK Parliament. NHS staff from overseas: statistics. https://commonslibrary.parliament.uk/research-briefings/cbp-7783/.
- 32.Rimmer A. Medical school places: what will be the effect of lifting the cap? BMJ 2020; 370: m3358. [DOI] [PubMed] [Google Scholar]
- 33.Beard DJ, Davies LJ, Cook JAet al. . The clinical and cost-effectiveness of total versus partial knee replacement in patients with medial compartment osteoarthritis (TOPKAT): 5-year outcomes of a randomised controlled trial. Lancet 2019; 394: 746–756. [DOI] [PMC free article] [PubMed] [Google Scholar]


