Abstract
A 61-year-old woman was diagnosed with an incidental liver lesion with a satellite lesion that had features of a secondary liver metastasis. Investigations for primary sites did not reveal a primary tumour. The lesion was not amenable to biopsy due to location. Intraoperatively, the two lesions were adjacent, but the first was on the diaphragm and the lesion was in segment 7 of the liver. The liver lesion underwent non-anatomical resection and the diaphragmatic lesion was resected separately. The histopathology diagnosed peritoneal mesothelioma in the lesion removed from diaphragm and the liver lesion to be local metastatic spread to an area of liver that was in close contact (a ‘kissing’ lesion). This report portrays a rare occurrence of liver metastases from peritoneal mesothelioma and discusses the current evidence for diagnosis and treatment.
Keywords: Peritoneal, Mesotheliomas, Liver, Metastases
Introduction
Peritoneal mesothelioma is an exceedingly rare disease. Liver metastasis from mesothelioma being an even rarer occurrence. The incidence in industrialised countries ranges between 0.5 and 3 cases per million in men and between 0.2 and 2 cases per million in women. Despite this, mesothelioma is an important differential when presented with abdominal lesions. We report a case of an incidentally diagnosed case of peritoneal mesothelioma with an adjacent metastatic liver lesion.
Case history
A 61-year-old woman presented to the accident and emergency department feeling generally unwell and haemodynamically unstable. She was diagnosed to have Addisonian crisis and treated with steroid replacement and resuscitation. She is known to have asthma and high cholesterol.
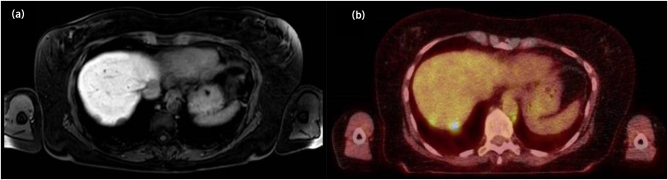
A computed tomography (CT) scan of the abdomen was performed to look for pathology in her adrenal glands. The CT scan showed atrophic adrenal glands and found two lesions in the liver suggestive of liver metastases. Magnetic resonance imaging (MRI) of the liver (Figure 1a) showed 19mm and 14mm lesions in segment 7. This was confirmed on positive emission tomography–computed tomography scan which showed intensely avid focus in segment 7 with a further discrete satellite lesion in the vicinity (Figure 1b); there was no other evidence of disease elsewhere. Percutaneous biopsy was not considered as a preferred option to make a histological diagnosis because it would require a transpleural route. The patient underwent extensive evaluation to look for a primary cancer site including oesophagogastroduodenoscopy (OGD) and colonoscopy. OGD diagnosed a Schatzki ring of the oesophagus but there were no other lesions in the rest of the gastrointestinal tract. There were no primary lesions identified even after thorough evaluation. The tumour markers such as carcinoembryonic antigen (CEA), cancer antigen (CA)125, CA19-9 and alpha-fetoprotein were within normal limits. With a diagnosis of localised metastatic lesions in segment 7 of the liver with unknown primary, surgical resection of the liver lesion with satellite nodule (segment 7 resection) was planned.
Figure 1 .
(a) Magnetic resonance imaging of the liver showing segment 7 lesions. (b) Positive emission tomography–computed tomography scan showing segment 7 lesions.
Surgical resection and follow-up
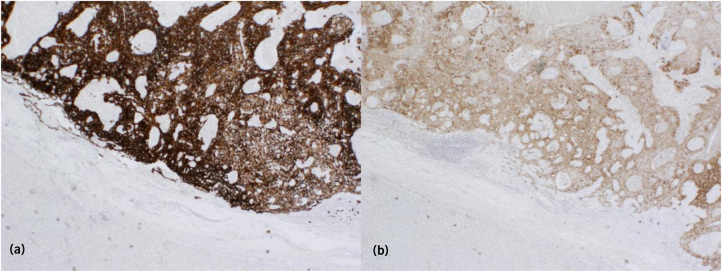
Intraoperative findings revealed a 14mm diaphragmatic nodule that was adjacent to the liver lesion (2cm) in segment 7. The diaphragmatic lesion was excised with a full thickness segment of diaphragm and the liver lesion had a non-anatomical resection. The histopathology of the specimens was identical and diagnosed mesothelioma. Both lesions were completely excised with negative margins. They showed solid architecture composed of epitheloid cells with focal cytoplasmic clearing. There were intranuclear inclusions with infrequent mitoses and focal necrosis. Vascular invasion was present. Immunohistochemistry was positive only for cell markers AE1/3, CK7, nuclear WT1, nuclear/cytoplasmic CK5 (Figure 2a) and Calciretinin (Figure 2b). Ki67 index was 11%. The liver lesions showed no invasion of the liver tissue and were confined to the liver capsule only. These findings suggest a direct spread by local implantation of malignant cells on the liver from the adjacent diaphragmatic mesothelioma (‘kissing lesions’). The patient made an excellent recovery without any postoperative complications.
Figure 2 .
Histopathology staining positive for (a) CK5 and (b) calretinin.
Retrospective exploration of risk factors showed no previous asbestos exposure. As both lesions were completely resected with negative margins, the oncology team decided to continue surveillance without the need for adjuvant treatment. Ten months after the surgery the patient remains well and recurrence free.
Discussion
Exposure to asbestos is the main known cause of peritoneal mesothelioma. However, it is estimated that 20–40% of cases occur spontaneously, especially in female patients. Other risk factors include Mediterranean familial fever, mutations in BRCA genes, chronic peritonitis and simian viruses. There are several epidemiological differences between pleural and peritoneal mesothelioma. Peritoneal mesothelioma has a lower median age of diagnosis (63 vs 71 years), incidence of cases not related to asbestos exposure is higher and there is a shorter latent period between exposure and development (20 vs 35 years). Peritoneal mesothelioma is also more prevalent in women.1
The most common symptoms are abdominal pain and distension which occur in 30–50% of patients. Aggressive mesotheliomas present with abdominal distension and intestinal obstruction due to omental disease and ascites. Often mesothelioma will be found incidentally on cross-sectional imaging or intraoperatively.
Because there is no characteristic feature on radiology, diagnosis is often made by histopathology. Microscopically, mesothelioma can be epithelioid, sarcomatoid or mixed, which reflects the ability of mesothelial cells to develop into epithelium or mesenchymal stromal cells. It is difficult to differentiate from adenocarcinoma but features favouring mesothelioma include positive staining for acid mucopolysaccharide, lack of staining for CEA, staining for keratin proteins (particularly peripheral staining) and lastly, positive staining for calretinin, WT1, CK5/6 and D2-40. Serum CA125 and CA15-3 tumour markers are more useful in identifying recurrence than for diagnosis, with sensitivity being 53% and 48.5%, respectively.2
Conventional treatment for pleural mesothelioma is a debulking procedure combined with systemic chemotherapy. For peritoneal mesothelioma with disseminated disease, cytoreductive surgery (CRS) with hyperthermic intraperitoneal chemotherapy (HIPEC) has shown improved survival. There is an increased risk of major complications such as haemorrhage, enterocutaneous fistula, perforation, dehiscence and abscess formation. CRS and HIPEC are also useful as an effective palliative procedure for symptom control.3,4
Conclusion
Peritoneal mesothelioma is a rare diagnosis. In this case, a single diaphragmatic lesion with adjacent liver metastatic lesion could be considered as a locoregional spread rather than systemic metastasis. Surgical resection offered the best possible treatment. Preoperative diagnosis is difficult unless lesions can be biopsied because there are no characteristic radiological features.
References
- 1.Boffetta P. Epidemiology of peritoneal mesothelioma: a review. Ann Oncol 2007; 18: 985–990. [DOI] [PubMed] [Google Scholar]
- 2.Kumar V, Abbas A, Fausto N, Aster J. Robbins and Cotran Pathologic Basis of Disease. 8th edn. Philadelphia: Saunders Elsevier; 2010. [Google Scholar]
- 3.García-Fadrique A, Mehta A, Mohamed F, et al. Clinical presentation, diagnosis, classification and management of peritoneal mesothelioma: a review. J Gastrointest Oncol 2017; 8: 915–924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Su SS, Zheng GQ, Liu YG, et al. Malignant peritoneum mesothelioma with hepatic involvement: A single institution experience in 5 patients and review of the literature. Gastroenterol Res Pract 2016; 2016: 6242149. [DOI] [PMC free article] [PubMed] [Google Scholar]