Abstract
Introduction
With the emergence of the COVID-19 pandemic, all elective surgery was temporarily suspended in the UK, allowing for diversion of resource to manage the anticipated surge of critically unwell patients. Continuing to deliver time-critical surgical care is important to avoid excess morbidity and mortality from pathologies unrelated to COVID-19. We describe the implementation and short-term surgical outcomes from a system to deliver time-critical elective surgical care to patients during the COVID-19 pandemic.
Materials and methods
A protocol for the prioritisation and safe delivery of time-critical surgery at a COVID-19 ‘clean’ site was implemented at the Nuffield Health Exeter Hospital, an independent sector hospital in the southwest of England. Outcomes to 30 days postoperatively were recorded, including unplanned admissions after daycase surgery, readmissions and complications, as well as the incidence of perioperative COVID-19 infection in patients and staff.
Results
A total of 128 surgical procedures were performed during a 31-day period by a range of specialties including breast, plastics, urology, gynaecology, vascular and cardiology. There was one unplanned admission and and two readmissions. Six complications were identified, and all were Clavien-Dindo grade 1 or 2. All 128 patients had preoperative COVID-19 swabs, one of which was positive and the patient had their surgery delayed. Ten patients were tested for COVID-19 postoperatively, with none testing positive.
Conclusion
This study has demonstrated the implementation of a safe system for delivery of time-critical elective surgical care at a COVID-19 clean site. Other healthcare providers may benefit from implementation of similar methodology as hospitals plan to restart elective surgery.
Keywords: COVID-19, Surgery, Elective, Cancer, Patient safety
Introduction
The novel severe acute respiratory syndrome SARS-CoV-2 (COVID-19) was declared a pandemic on 11 March 2020 by the World Health Organization,1 and hospitals in countries affected have become rapidly overwhelmed with patients affected by the virus.2 Escalation plans were developed around the world to manage the surge in critically unwell patients and to reduce spread of the highly transmissible COVID-19.3 In substantial numbers of patients with COVID-19, their illness becomes so severe that multi-organ support is needed and this has quickly overburdened intensive care units and critical care systems around the world.4
On 15 April 2020, NHS England published guidance advising that all elective operations should be suspended for three months,5 which would reduce both unnecessary patient traffic in hospitals and the risk of further virus transmission. The intention was to release resources including hospital beds, personal protective equipment and staff that would allow recovery rooms and operating rooms to be repurposed as ventilator-level care zones, thus increasing intensive and critical care capacity.6 Despite the cancellation of elective operations, NHS England stated that emergency admissions, certain cancer treatments and other clinically urgent care should continue where possible.5
Guidance on prioritisation of emergency cases was published by the Federation of Specialty Surgical Associations and guidance for the management of cancer patients was released by NHS England.7,8 Local hospital protocols were to be based on clinical need and balance both the risks to patients from their surgical condition and their personal risk from COVID-19 infection and overall service delivery. Any plans or protocols should be dynamic and should have clear guidance for the detection and care of patients who tested positive for COVID-19.9,10 To increase the existing capacity for delivery of care, NHS England secured significant resources from independent sector healthcare providers to allow time-critical NHS elective care services to continue while demand from COVID-19-related admissions remained high or potentially volatile.11
Delays in time-critical elective surgery, such as cancer care, are well recognised to cause patients harm and reduce survival.12–14 The suspension of elective surgery was important in preparing for the primary surge in COVID-19 seen around the world, but as hospitals learnt to manage the patients affected by the virus and admissions fell it became increasingly important that healthcare systems generated capacity for time-critical elective surgery.15,16 Protocols were developed to facilitate clinical prioritisation of operating room time and permit safe delivery of this time-critical elective surgery during the COVID-19 pandemic. These protocols could be usefully shared to allow healthcare providers to consider how adaptations might be made in their own healthcare setting.
From the beginning of April 2020, a partnership between a private healthcare provider and the local NHS foundation trust in the southwest of England delivered time-critical elective surgical provision. This partnership aimed to deliver healthcare at a COVID-19 ‘clean’ site, where multiple steps were taken to minimise the risk of operating on patients who are COVID-19 positive and transmission of COVID-19 between patients and staff. The aim of this narrative report is to describe the development and implementation of this pathway and to review the short-term surgical outcomes.
Materials and methods
Setting
The Nuffield Health Exeter Hospital is an independent hospital located in the southwest of England. From 6 April 2020, during the initial COVID-19 pandemic response, three operating theatres were appropriated by the NHS to provide surgical capacity for time-critical elective surgical procedures. The service was set up for patients without COVID-19 in the population whose care was ordinarily delivered by the local acute University teaching hospital, the Royal Devon and Exeter Foundation Trust (RDEFT).
Staffing
Surgical and anaesthetic staff worked across both the clean site and the RDEFT, without individual staff being allocated exclusively to either site. All staff and patients answered screening questions and had their temperatures checked on entering the clean site (Nuffield Health Exeter Hospital). Staff allocation to service commitment was organised by the respective specialty team. Staff at greater personal risk, should they acquire COVID-19, were prioritised to work at the clean site and were taken off on-call rotas at RDEFT, when this was mutually agreed. There was a junior doctor present in the hospital 24 hours a day. Further out of hours cover from surgical, anaesthesia or medical teams was available via the RDEFT on-call rotas.
Protocol
The consideration of how to best allocate resources was made by a cross-specialty medical clinical reference group, which provided assessments of anticipated clinical needs. This information was supplied to a surgical prioritisation team chaired by an independent senior clinician and staffed by surgeons, anaesthetists, surgical division managers and senior nurses. There was a nominated operational lead, operational capacity leads, clinical leads and performance and data lead. This was modelled on a process developed and shared by the Royal Marsden Partners, London.17 An administration team was established to facilitate the organisation of resources and to schedule operating theatre allocation dependent upon need, as determined by the surgical prioritisation team.
Assessment of clinical need
NHS England priority level principles were applied to cases in order to define clinical urgency.8 NHS England established this guidance for cancer patients requiring surgery, but the concept was broadened to include time-critical but non-cancer surgical cases. Priority level 1a (emergency surgery required within 24 hours) and 1b (urgent surgery required within 72 hours) were planned to be delivered at the RDEFT. All other cases for which a delay to treatment would result in harm or excess mortality were identified. According to the NHS England model, this included both priority level 2 and 3 cases; namely those requiring treatment within 4 and 12 weeks, respectively. Complex surgical cases likely to require intensive or high-dependency postoperative care were allocated to be performed at RDEFT where higher-care facilities are available.
Historical trust data were used to determine anticipated resource requirements, as well as modelling data made available through the Royal Marsden Partners Cancer Capacity Hub in London.17 Template operating theatre schedules were developed in which each specialty was allocated the necessary time and resources (including medical, nursing and support staffing) to deliver care for these priority level 2 and 3 cases.
Surgical prioritisation
Strategies for delivering time-critical surgical services within other hospital trusts were reviewed to develop a model of care delivery suitable to the location, facilities and service demands. Information sources included the Royal Marsden Partners Cancer Capacity Hub methodology and approaches adopted by the Northern Care Alliance and Nottingham University Hospitals.17–19
For all priority level 2 and 3 patients, specialties were recommended to consider the following factors when prioritising patients for surgery:
-
•
scheduling priority according to likelihood of surgery being curative: this assigns one of six levels for the proposed treatment, with levels 1–4 being curative intent and priority level 1 having greater than 50% chance of success8
-
•
alternative treatments: the presence or absence of equivalent and available non-surgical treatment options
-
•
frailty score: characterised using the Rockwood Frailty Scale20
-
•
COVID-19 vulnerability level: this is a scale from 1 to 3 comparing expected excess mortality in the event of contracting COVID-19 to that of a fit 70-year-old person18
-
•
anticipated length of hospital stay, intensive care admission and other special requirements.
Recommendations were made for prioritisation of patients with a high likelihood of cure, high subsequent life expectancy and low vulnerability level.
Risk oversight
A database of patients awaiting time-critical surgery was maintained by the surgical prioritisation team to permit reprioritisation of cases at short notice and act as a risk register. This oversight ensured appropriate resource allocation and coordinated testing for COVID-19 in advance of patient admission.
COVID-19 testing
Patients undergoing elective surgery were required to have no symptoms suggestive of COVID-19 infection, to self-isolate for up to 14 days preoperatively if required and to have a negative COVID-19 nasopharyngeal swab within 72 hours of surgery.21 Nasopharyngeal viral polymerase chain reaction swab tests were performed by appropriately trained personnel at the patient’s primary residence or a ‘drive-through’ facility to prevent unnecessary attendance to the acute hospital site (RDEFT). In the event of a patient testing positive for COVID-19 their surgery was deferred.
Donning and doffing
National guidance on donning and doffing from Public Health England was followed.22 This guidance was displayed on the trust website and within operation rooms. The guidance involved the use of appropriate ‘fit tested’ respirators for aerosol-generating procedures and surgical masks for non-aerosol-generating procedures.
Laparoscopic procedures
Inline filters were used for insufflation and desufflation. Suction was also used around port sites when changing instruments. Meticulous attention to port removal at the end of the procedure, specifically the abdomen was desuffulated fully via the inline particle filter and ports were only removed when the abdominal pressure was zero.
Data collection
Pseudonymised data were provided from the private hospital to the accompanying NHS trust and adhered to the trust’s audit and quality improvement project procedures. Data were extracted from the prospectively collected theatre management system for weeks commencing 6 April 2020 to 7 May 2020. The primary procedure code (OPCS) was extracted with the associated operative data, length of stay, patient’s age and sex. Age-adjusted Charlson Comorbidity Index was calculated for each patient.23
Any readmissions, intensive care support and step-down surgical care was planned to be delivered, if needed, at the acute hospital. Data on unplanned admissions from daycase surgery, readmissions and complications were collected and cross-referenced with the RDEFT’s database. A search of postoperative patient deaths within the study period was undertaken on the same database.
Preoperative COVID-19 swabs results were cross-checked and confirmed as negative. The testing date and results of any patient who underwent a further swab in the postoperative period was recorded. The impact on service delivery due to staff absence as a result of self-isolation because of COVID-19 symptoms, and records of any staff testing positive for COVID-19 was collected in conjunction with the surgical human resources management team.
The daily numbers of inpatients who were COVID-19 positive within the RDEFT was collated to serve as an indication of the prevalence of COVID-19 in the local population and to inform future service provision.
Analysis
All data are presented using descriptive statistics and graphical summaries without inferential analysis. Data management was undertaken in a Microsoft Excel spreadsheet.
Results
Episode data
In total, there were 128 surgical procedures performed during a 31-day period from 6 April 2020 to 7 May 2020. The median patient age was 67 years (range 18–99 years) and 58% were female. Median age-adjusted Charlson Comorbidity Index was 4 (range 0–10). Table 1 shows patient demographics and an overview of COVID-19 swab testing pre- and postoperatively.
Table 1 .
Patient demographics for 128 patients and COVID-19 swab testing
| Demographic | Patients |
|
|---|---|---|
| (n) | (%) | |
| Median age (years) | 67 (range 18–99) | – |
| Male | 54 | 42 |
| Female | 74 | 58 |
| Median (age-adjusted) Charlson Comorbidity Index | 4 (0–10) | – |
| Preoperative COVID-19 swab (within 72 hours) | 128 | 100 |
| Postoperative COVID-19 swab (within 14 days) | 10 | 8 |
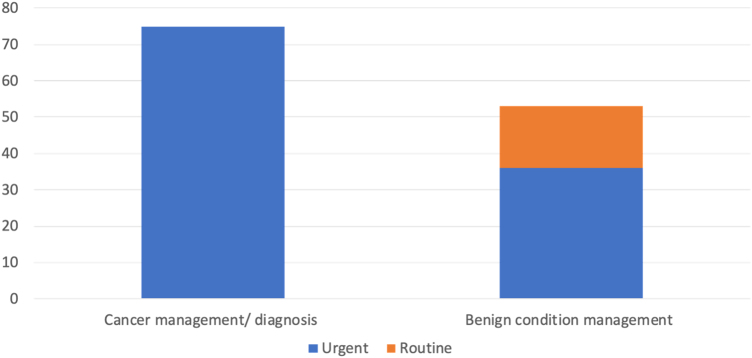
Of the 128 surgical procedures, 59% (75/128) were for the diagnosis or management of cancer and 41% (53/128) were for the management of benign conditions. Of those performed for the management of benign conditions, 36 were classified as urgent and 17 as routine (Figure 1). Some 80% (102/128) of patients had daycase procedures, 19% (24/128) stayed one night and 1.6% (2/128) stayed two nights following surgery. Data on anaesthesia were available for 109 patients, of whom 56% (61/109) had general anaesthesia, 36% (39/109) had a local anaesthetic procedure and 8.3% (9/109) were sedated.
Figure 1 .
Breakdown of cancer compared with benign work
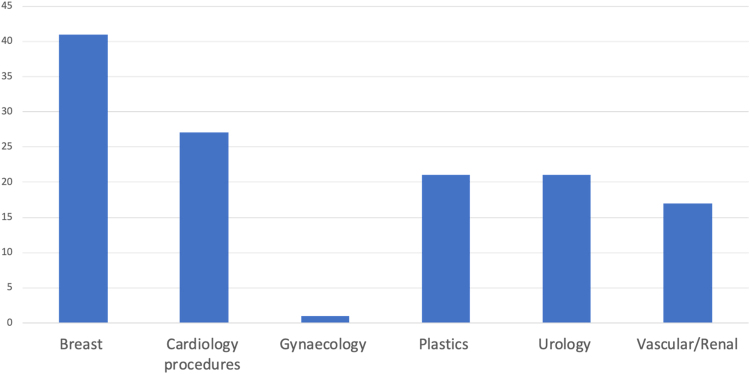
During the study period, 32% (41/128) of operations were breast surgery, 16% (21/128) plastic surgery, 16% (21/128) urology, and one patient (1.6%) underwent total laparoscopic hysterectomy under the gynaecological surgeons. Arteriovenous fistula formation for renal dialysis accounted for 13% (17/128) of cases and the cardiology team undertook 21% (27/128) of procedures, including pacemaker implantations, cardiac ablations and coronary catheterisations (Figure 2, Table 2).
Figure 2 .
Cases performed by surgical specialty
Table 2 .
Procedures list
| Specialty | Procedure | Patients (n) |
|---|---|---|
| Breast | Mastectomy | 14 |
| + axillary node clearance | 3 | |
| + sentinel node biopsy | 9 | |
| Wide local excision | 23 | |
| + axillary node clearance | 2 | |
| + sentinel node biopsy | 18 | |
| Re-excision for positive surgical margins | 3 | |
| Axillary lymph node dissection | 1 | |
| Cardiology | Coronary catheterisation | 9 |
| Cardiac ablation | 7 | |
| Pacemaker insertion | 8 | |
| Pacemaker box change | 3 | |
| Gynaecology | Total laparoscopic hysterectomy and bilateral salpingo-oophorectomy | 1 |
| Plastic surgery | Biopsy/excision of skin lesion | 6 |
| Wide local excision of skin lesion | 11 | |
| Melanoma | 9 | |
| Merkel cell carcinoma | 1 | |
| Cutaneous sarcoma | 1 | |
| Excision of soft tissue lesion | 2 | |
| Dissection of inguinal lymph nodes | 2 | |
| Urology | Ureteroscopic laser fragmentation of calculus | 4 |
| Trans-perineal prostate biopsy | 9 | |
| Trans-urethral resection of a bladder tumour | 4 | |
| Diagnostic flexible cystoscopy | 1 | |
| Cystoscopy and retrograde pyelography | 1 | |
| Ureteric stent change/ removal | 2 | |
| Vascular/renal | Arteriovenous fistula formation | 17 |
COVID-19 screening results
All patients had a COVID-19 swab within 72 hours prior to admission; one patient tested positive to COVID-19 and surgery was deferred. Ten patients were tested within 14 days postoperatively, either through self-presentation or on a reattendance. All results were negative.
Staff absence through self-isolation or shielding occurred in line with government guidelines but did not impinge on the staffing of the operating theatres. No staff member was screened with COVID-19 swabs prior to the escalation of testing on 29 April 2020. Subsequently, symptomatic staff members have been tested but none has been diagnosed with COVID-19. During the study period and up to 17 May 2020, no staff members were admitted to hospital for investigation or treatment of suspected COVID-19.
Post-procedural complications
Complications occurred in 4.7% (6/128) of patients in the 30-day postoperative period. There were no severe complications (Clavien–Dindo ≥ 3).24 Specific complications and their management are recorded in Table 3.
Table 3 .
Complications
| Specific complications and Clavien–Dindo score | Patients |
Days postoperatively | Management | |
|---|---|---|---|---|
| (n) | (%) | |||
| Total grade 1 | 5 | 3.9 | ||
| Haematoma following pacemaker box change | 1 | 0.78 | 0 | Overnight admission, no intervention |
| Pneumothorax following pacemaker | 1 | 0.78 | 0 | No intervention |
| Haematuria following TURBT | 1 | 0.78 | 2 | Overnight admission, bladder washout |
| Seroma following mastectomy | 2 | 1.6 | 16, 27 | Diagnosed and aspirated in routine follow-up clinic |
| Total grade 2 | 1 | 0.78 | ||
| Surgical site infection following brachiocephalic fistula | 1 | 0.78 | 20 | Treated with intravenous antibiotics |
TURBT, Trans-urethral resection of a bladder tumour.
There was one unplanned admission for a patient who developed a haematoma formation following a pacemaker change. This patient was admitted for observation and discharged home the following day. The readmission rate was 1.56% (2/128). Both patients were readmitted to RDEFT, one with haematuria managed with catheter insertion and bladder washout, and one with superficial infection of their brachiocephalic fistula managed with intravenous antibiotics (Table 3). The latter patient died on day 11 of their admission. The cause of death was thought to relate to the underlying chronic disease process and not the postoperative infection.
There was a single acute transfer of care in a patient who developed atrial fibrillation detected on admission to the clean site prior to their surgical procedure but after their preadmission checks. There were no acute postoperative transfers to the acute hospital or intensive care transfers. There were no deaths recorded in the 14 days post-procedure for any of the 128 patients.
Local COVID-19 hospital prevalence
During the study period the number of inpatients with COVID-19 at the RDEFT ranged from 19 to 58 (mean 38.3).
Discussion
We have described the development of a process for delivery of and early outcomes for the safe provision of time-critical elective surgery during the current global COVID-19 pandemic. During a 31-day period, 128 time-critical surgical procedures were performed in patients confirmed as symptom-free and also COVID-19 negative on diagnostic testing. Of those tested in the 14-day period following surgery, none tested positive for COVID-19.
The overall readmission rate was 1.6%, which is in keeping with readmission rates seen in larger studies of ambulatory surgery,25 but higher than the less than 0.5% proposed UK national standard for best practice.26 These standards are proposed for daycase surgery and as 20% of patients in this study required admission for at least one night following their procedure, a higher readmission rate might be expected. The unplanned admission rate was 0.78%, in keeping with the less than 2% proposed national standard.26
Complications were rare and none was severe (Clavien–Dindo ≥ 3). The one patient death in our study population was recorded as being a result of underlying chronic disease process rather than due to complications from their surgical procedure. The low readmission, unplanned admission and complication rates in our results demonstrate that it is possible to perform a high volume of time-critical surgical work safely during the current COVID-19 pandemic.
We aimed to create a clean site for surgery to reduce patient and staff transmission of COVID-19. Reducing transmission of and infection with the virus within the healthcare system is a crucial aspect to continuing safe elective surgery. The effects of surgery and anaesthetic stress on predisposition to or exacerbation of COVID-19 are currently under investigation.27 The most recent data from COVIDSurg, an international cohort study aiming to assess outcomes of surgery in patients diagnosed with COVID-19, suggests that mortality in some groups could be as high as 44%.28 Clean-site surgery is equally important for the safety of surgical personnel due to the risk of COVID-19 transmission from patients by aerosolisation and droplet generating procedures such as endotracheal intubation.29
To ensure maintenance of a clean site, guidance from the Royal College of Surgeons of England was implemented as detailed in the methods section.21 All patients undergoing surgery had a negative swab result within 72 hours prior to admission and there were no diagnosed cases of COVID-19 in any of our patient cohort postoperatively. There were no confirmed cases of COVID-19 within staff working at the hospital and symptomatic staff isolated in accordance with UK government guidelines. This demonstrates the ability to safely perform a wide range of surgical procedures across different specialties at a clean site during the COVID-19 pandemic if carefully planned and delivered through a clinically managed process.
Limitations of our study include the low prevalence of COVID-19 in Devon during the data collection period,30 which may limit the generalisability of our model to higher prevalence areas. However, there are many locations nationally and internationally that share a similar prevalence and need to maintain a safe approach to delivering time-critical care. A limited range of operations were initially performed at the clean site in order to establish proof of concept for this model of care. As such, our data set does not report on delivery of certain operations which might feasibly be performed at a clean site without higher levels of support, such as colorectal resections. As a retrospective single centre review, results were dependent on local databases and documentation but recognition of any unplanned attendances of patients postoperatively to hospitals out of area was limited. However, the effect of this is likely to be minimal, as only essential travel was permissible within the UK during the study period.
While some cancer surgery and non-malignant time-critical surgery was continued where possible in England, waiting lists continued to grow for non-time-critical surgical problems. NHS England’s referral to treatment statistics show the number of patients waiting over 52 weeks to start planned treatment nearly doubled during March 2020.31 With current projections forecasting that COVID-19 will persist for some time yet,32 healthcare providers need to consider how to safely deliver surgical care to manage the time-critical needs of the non-COVID patient population. This paper shows a safe mechanism and structure for the delivery of time-critical elective care at a clean site in the epoch of COVID-19. We hope that by sharing our learning and experiences, other healthcare providers will be able to implement similar pathways of care to ensure safe surgical management of patients with conditions requiring a range of time-critical procedures.
Acknowledgements
The authors would like to acknowledge Dr Sheena Hubble and Dr Quentin Milner for their input in establishing the surgical prioritisation process; Dr Andrew Ludman and Mr David Oliver, who reviewed the manuscript and provided clinical oversight; and Mr Ian Harvey and Mr Michael Browning, who helped with data aggregation.
References
- 1.World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19: 11 March 2020. https://www.who.int/dg/speeches/detail/ who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march- 2020 (cited September 2020).
- 2.Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet 2020; 395: 1225–1228. 10.1016/S0140-6736(20)30627-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth 2020; 67: 568–576. 10.1007/s12630-020-01591-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang C, Wang Y, Li Xet al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497–506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stevens S, Pritchard A. Important and urgent – next steps on NHS response to COVID-19, 17 March 2020. https://www.england.nhs.uk/coronavirus/publication/next-steps-on-nhs-response-to-covid-19-letter-from-simon-stevens-and-amanda-pritchard (cited September 2020).
- 6.COVIDSurg Collaborative. Global guidance for surgical care during the COVID-19 pandemic. Br J Surg 2020; doi: 10.1002/bjs.11646 (cited September 2020). 10.1002/bjs.11646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Federation of Specialty Surgical Associations. Clinical Guide to Surgical Prioritisation During the Coronavirus Pandemic. London: FSSA; 2020. https://www.rcseng.ac.uk/coronavirus/surgical-prioritisation-guidance (cited September 2020). [Google Scholar]
- 8.NHS England; NHS Improvement. Clinical guide for the management of non-coronavirus patients requiring acute treatment: Cancer. March 2020. https://www.england.nhs.uk/coronavirus/secondary-care/other-resources/specialty- guides/#cancer (cited September 2020).
- 9.Stahel PF. How to risk-stratify elective surgery during the COVID-19 pandemic? Patient Saf Surg 2020; 14: 8. 10.1186/s13037-020-00235-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu Z, Zhang Y, Wang X et al. Recommendation for surgery during the novel coronavirus (COVID-19) epidemic. Indian J Surg 2020; 82: 124–128. 10.1007/s12262-020-02173-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Permain N. COVID-19: Partnership working with the independent sector providers and the independent healthcare providers network. NHS England; NHS Improvement, March 2020. https://www.england.nhs.uk/coronavirus/publication/ partnership-working-with-the-independent-sector-providers-and-the-ihpn (cited September 2020).
- 12.Richards M, Westcombe AM, Love SB et al. Influence of delay on survival in patients with breast cancer: a systematic review. Lancet 1999; 353: 1119–1126. 10.1016/S0140-6736(99)02143-1 [DOI] [PubMed] [Google Scholar]
- 13.Bleicher RJ. Timings and delays in breast cancer evaluation and treatment. Ann Surg Oncol 2018; 25: 2829–2838. 10.1245/s10434-018-6615-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sud A, Jones M, Broddio Jet al. Collateral damage: the impact on outcomes from cancer surgery of the COVID-19 pandemic. Ann Oncol 2020; 31: 1065-1074. 10.1016/j.annonc.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Iacobucci G. COVID-19: NHS will restart some paused services this week. BMJ 2020; 369: m1709. [DOI] [PubMed] [Google Scholar]
- 16.Stevens S, Pritchard A.. Important – for action – second phase of NHS response to COVID-19. April 2020. https://www.england.nhs.uk/coronavirus/publication/ second-phase-of-nhs-response-to-covid-19-letter-from-simon-stevens-and-amanda- pritchard (cited September 2020).
- 17.Royal Marsden NHS Foundation Trust. Cancer Hub delivers treatment during coronavirus pandemic. April 2020. Available at: https://www.royalmarsden.nhs.uk/cancer-hub-deliver-treatment-during-coronavirus-pandemic (cited September 2020).
- 18.Carlson G. Prioritising surgical treatment in coronavirus pandemic ‘Salford score’ [blog post]. Cutting Edge 1 April 2020. https://cuttingedgeblog.com/2020/04/01/prioritising-surgical-treatment-in-coronavirus-pandemic-salford-score (cited September 2020).
- 19.Taylor T. An open letter from the Chief Executive: How we have been preparing for and managing the Coronavirus outbreak. 24 March 2020. https://mailchi.mp/c473bd784a4e/covid-19-daily-staff-briefing-24-march-910865 (cited September 2020).
- 20.Rockwood K, Song X, Macknight Cet al. A global clinical measure of fitness and frailty in elderly people. Can Med Assoc J 2005; 173: 489–495. 10.1503/cmaj.050051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guidelines for pre-operative COVID-19 testing for elective cancer surgery. April 2020. Available from: https://www.rcsed.ac.uk/media/681195/guidelines-for-pre-operative-covid-19-testing-for-elective-cancer-surgery-1305202.pdf (cited September 2020).
- 22.Public Health England. Putting on (donning) personal protective equipment (PPE) for aerosol generating procedures (AGPs): airborne precautions. 2020. https://www.gov.uk/government/publications/covid-19-personal-protective-equipment-use-for-aerosol-generating-procedures (cited September 2020).
- 23.Charleston M, Pompei P, Ales Ket al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis 1987; 40: 373–383. 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 24.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004; 240: 205–213. 10.1097/01.sla.0000133083.54934.ae [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fortier J, Chung F, Su J. Unanticipated admission after ambulatory surgery: a prospective study. Can J Anaesth 1998; 45: 612–619. 10.1007/BF03012088 [DOI] [PubMed] [Google Scholar]
- 26.McEwan L, Russon K. Unplanned hospital admission after day surgery. In: Chereshneva M, Johnstone C, Colvin JR, Peden CJ.. Raising the Standards: RCoA Quality Improvement Compendium, 4th ed. London: Royal College of Anaesthetists; 2012. pp. 204–205. [Google Scholar]
- 27.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004; 240: 205–213. 10.1097/01.sla.0000133083.54934.ae [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lei S, Jiang F, Su Wet al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine 2020; 21: 100331. 10.1016/j.eclinm.2020.100331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.COVIDSurg Collaboration. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet 2020; 396: 27–38. 10.1016/S0140-6736(20)31182-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tran K, Cimon K, Severn Met al. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One 2012; 7: e35797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Public Health England. Weekly Coronavirus Disease 2019 (COVID-19): Surveillance Report. London: PHE; 2020. week 21. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/886864/Weekly_ National_COVID19_Surveillance_w21_FINAL.pdf (cited September 2020). [Google Scholar]
- 32.NHS England; NHS Improvement. Referral to treatment waiting times, England. March 2020. https://www.nhs.uk/using-the-nhs/nhs-services/hospitals/guide-to-nhs-waiting-times-in-england (cited September 2020).
- 33.Yi Y, Lagniton PNP, Ye Set al. COVID-19: what has been learned and to be learned about the novel coronavirus disease. Int J Biol Sci 2020; 16: 1753–1766. 10.7150/ijbs.45134 [DOI] [PMC free article] [PubMed] [Google Scholar]