Abstract
Introduction
Hashimoto’s thyroiditis (HT) is one of the most common immune-mediated diseases. It makes thyroid surgery more complicated and difficult because there may be adhesions between the thyroid gland and surrounding structures. However, it is still controversial whether HT patients carry a high risk for postoperative complications of thyroid surgery. The purpose of this study was to investigate the significance of HT for the postoperative complications of thyroid surgery.
Methods
A search for studies assessing the postoperative complication risks of HT patients compared with that of patients with benign nodules (BNs) was performed in PubMed, EMBASE and Web of Science. Nine studies (20,118 cases, 1,582 cases of HT and 18,536 cases of BN) were identified, and the data from the relevant outcomes were extracted and analysed.
Results
There were no significant differences between the HT group and BN group in recurrent laryngeal nerve palsy (RLNP) and permanent hypoparathyroidism (PHP). The rate of transient hypocalcaemia (THC) was significantly higher in the HT group (16.85%) than in the BN group (13.20%).
Conclusions
The meta-analysis showed that HT only increased the risk of the postoperative complication THC compared to BN. Understanding the significance of HT in postoperative hypoparathyroidism after thyroid surgery would help clinicians perform sufficient preoperative (and postoperative) assessments and to optimise surgical planning.
Keywords: Benign nodule, Hashimoto’s thyroiditis, Meta-analysis, Postoperative complication, Risk, Thyroid
Introduction
In 1912, Hashimoto first reported that thyroid goitres were characterised by chronic lymphocytic thyroiditis.1 Hashimoto’s thyroiditis (HT) is usually asymptomatic, but the occurrence of hypothyroidism requires medical treatment in the form of thyroid hormone supplementation, and surgery is required when HT patients are complicated by nodular goitre or malignant nodules.2–4 Moreover, in HT patients who have developed large diffuse goitres, an increase in pressure symptoms and unsightly appearance in the anterior neck can occur and should be treated with surgery.4
HT is a common autoimmune disease in which the human immune system mistakenly attacks the thyroid gland.5 Fibrosis, lymphocyte infiltration and atrophied follicular cells are the histological characteristics of HT.6–8 The thyroid gland is repeatedly damaged by HT disease. Intraoperatively, the thyroid gland is firm and often adherent to adjacent structures, and various regional lymphadenopathies are common.9 Therefore, the dense, adherent connective tissue may compress and obscure critical central neck compartment structures and make capsular dissection challenging and identification of the parathyroid glands difficult.10
Recurrent laryngeal nerve palsy (RLNP) and hypocalcaemia/hypoparathyroidism remain the primary complications after thyroid surgery despite the standardisation and updating of surgical equipment for thyroidectomy.11–13 The incidence of hypoparathyroidism ranges from 0.5% to 65% according to previous studies.14,15 Jeannon et al12 reported a 9.8% rate of transient RLNP (T-RLNP) after thyroidectomy, and the incidence rate declined to 2.3% during the first-year follow-up in all patients due to the recovery of RLN function. In general, HT patients might suffer more surgical complications, such as RLNP or hypoparathyroidism, due to adhesions between the thyroid gland and adjacent structures, including the parathyroid gland and RLN, which make dissection of the thyroid gland more difficult.16–19 However, Shih et al9 revealed that HT patients who underwent thyroidectomy had a low risk of permanent surgical complications.
It is still controversial whether the existence of HT increases the risk of postoperative complications of thyroid surgery. This meta-analysis was performed to further explore whether HT increases the risk of postoperative complications of thyroidectomy.
Methods
Guidelines
The study design follows the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) and AMSTAR (Assessing the methodological quality of systematic reviews) guidelines.
Systematic review registration
This systematic review was registered with the international prospective register of systematic reviews (PROSPERO) on 9 October 2018 (registration: PROSPERO 2018 CRD42018109215).
Search strategy and study selection
Individual search criteria were customised, and PubMed, EMBASE and Web of Science were searched for relevant articles published before 1 August 2018.
The following keywords were used in the search: “Hashimoto disease OR Hashimoto thyroiditis OR Hashimoto's syndrome OR chronic lymphocytic thyroiditis” AND “thyroid OR thyroid gland” AND “postoperative complications”. The “related articles” function was applied to expand the scope of the search.
All reviews, retrieved studies and conference abstracts were searched. Only the most recent or complete study was included if multiple published studies that demonstrated the same population existed. The adopted literature needed to match the following criteria: (1) original articles which demonstrated that the benign cysts/nodules or non-toxic nodular goitres were assessed only as thyroid specimens by histopathologic examination. Classic HT was assessed by the histopathologic examination of thyroid specimens; (2) articles published before August 2018; (3) articles that defined T-RLNP as patients with postoperative voice changes, hoarseness or difficulty swallowing within six months and diagnosed by preoperative and postoperative laryngoscopy examination. RLNP that continued after six months was considered permanent RLNP (P-RLNP). Transient hypocalcaemia (THC) was defined by signs and symptoms of hypocalcaemia or a serum calcium <8–8.5mg/dl for less than six months. Permanent hypoparathyroidism (PHP) was defined by calcium and/or vitamin D requirements for longer than six months. The HT group was defined by a single HT thyroid goitre. The BN group included benign cysts/nodules and non-toxic nodular goitres; (4) articles that reported the type of surgery and extent of resection; (5) articles such as reviews, meta-analysis, editorials, case reports, meeting abstracts and letters were excluded, as well as studies published in other languages except for English; and (6) articles that did not mention particular applications, including laparoscopic thyroid surgery or tracers.
Data extraction
Data such as the first author’s last name, publication year, study design, country, sample size, type of surgery, and number of RLNP cases and hypocalcaemia/hypoparathyroidism were extracted and summarised independently by two investigators. Disagreements between the investigators were resolved by consensus or by a third party.
Study quality assessment
The quality of observational literature was assessed based on the Newcastle–Ottawa Scale (NOS), which included participant selection, study group comparability and outcome assessment. A score of 0–9 stars was used to assess each study by two investigators independently. Studies with NOS scores of six or more stars were considered high-quality studies.
Statistical analysis
The chi-squared test evaluated the statistical heterogeneity among studies. I2 ≥70% was regarded as high heterogeneity. Then, a random-effects model was applied if the literature had high heterogeneity. If not, the fixed-effect model would be applied. Review Manager 5.3 (Cochrane Collaboration, Oxford, UK) was used to perform the meta-analysis. The odds ratio (OR) was used to compare dichotomous variables; 95% confidence intervals (CIs) were used to estimate all results. The publication bias was evaluated by Egger’s test and Begg’s funnel plot. A p-value <0.05 was considered statistically significant.
Results
Study characteristics
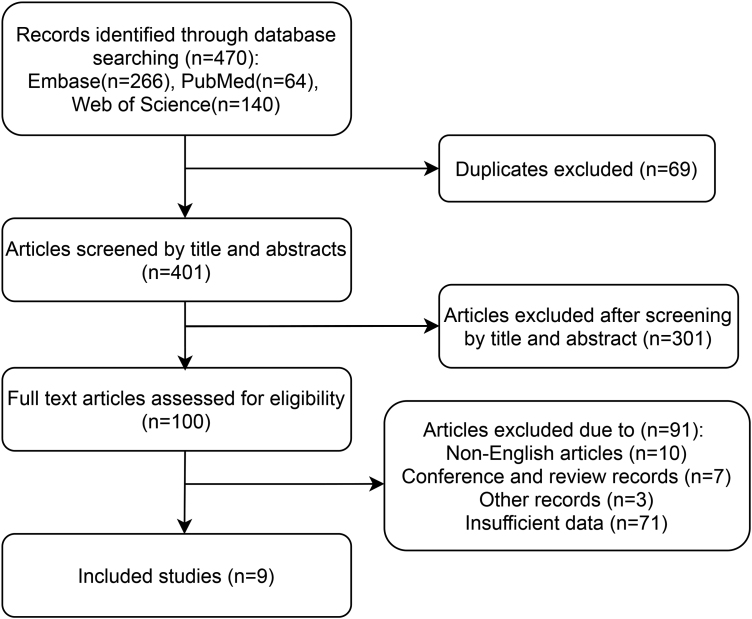
Nine studies including 20,118 cases, with 1,582 cases of HT and 18,536 cases of BN, fulfilled the included criteria and consisted of five case-control,16,20–23, two cohort9,24 and two prospective25,26 studies (Figure 1, Table 1). Based on the NOS, three studies were awarded 5 stars,16,22,23 three received 6 stars,20,24,25 two received 7 stars,9,21 and one received 8 stars26 (Table 1).
Figure 1 .
Flowchart of the study selection process
Table 1 .
Characteristics of the included studies
| First author | Country | Year | Type | Patients, n (HT/BN) | Extent of surgery | Surgery of TT (HT/BN) | Transient RLN palsy (HT/BN) | Permanent RLN palsy (HT/BN) | THC (HT/BN) | PHP (HT/BN) | Definition | Quality score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wagner16 | Switzerland | 1994 | CC | 21/73 | I | NA | 0/1 | 1/0 | NA | NA | a | 5 |
| Shih9 | US | 2008 | C | 25/316 | II | 17/162 | 1/0 | 0/0 | 8/77 | 0/0 | a.b | 7 |
| Ebrahimi32 | Australia | 2009 | C | 93/312 | II | 93/312 | NA | NA | 3/18 | 0/3 | b | 6 |
| Pradeep23 | India | 2011 | CC | 33/236 | II | 24/117 | 0/0 | 0/0 | 3/10 | 0/0 | a | 5 |
| Enomoto22 | Japan | 2014 | CC | 20/375 | II | NA | 1/23 | 0/0 | NA | NA | a | 5 |
| Nawrot20 | Poland | 2014 | CC | 10/243 | I | NA | NA | NA | NA | 0/18 | d | 6 |
| Gupta25 | India | 2015 | P | 4/62 | II | 4/62 | NA | NA | 2/14 | NA | b | 6 |
| Thomusch26 | Germany Poland Czech Austria | 2018 | P | 1268/16467 | II | 844/8890 | 44/642 | 11/132 | 194/2124 | 14/148 | a.b | 8 |
| Ravikumar21 | India | 2018 | CC | 108/452 | II | 108/452 | 12/34 | 5/8 | 48/112 | 4/10 | a.c | 7 |
BN = benign nodule; C = cohort; CC = case-control; HT = Hashimoto’s thyroiditis; NA = data not available; P = prospective; RLN = recurrent laryngeal nerve
I = including subtotal, total thyroidectomy together with lobectomy or completion thyroidectomy; II = all total thyroidectomy
a = preoperative and postoperative laryngoscopy; b = THC is defined by a serum calcium <8–8.5mg/dl for less than 6 months, and permanent hypoparathyroidism (PHP) is defined by calcium and/or vitamin D requirements for longer than 6 months; c = THC is defined by a parathyroid hormone (PTH) level <10pg/ml within 24 h of the operation that eventually increases to >10pg/ml within 6 months or permanent hypocalcaemia longer than 6 months; d = PHP is defined by calcium and/or vitamin D requirements for longer than 12 months
Transient recurrent laryngeal nerve palsy
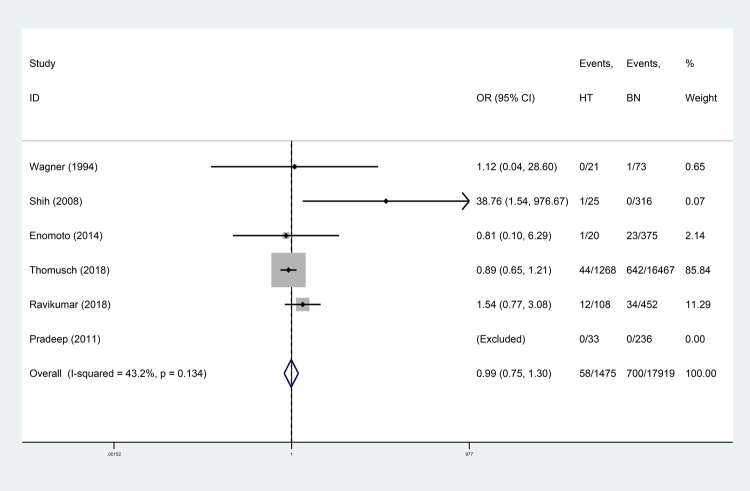
Six studies9,16,21–23,26 were used for this meta-analysis, and results showed that the risk for T-RLNP was similar between the HT group and BN group (OR 0.99, 95% CI: 0.75–1.30, p=0.842; Figure 2). Low heterogeneity was found among these studies (I2 43.2%, p=0.134; Table 2), and no publication bias was detected by Egger’s test (p=0.259; Table 2).
Figure 2 .
Forest plot and meta-analysis of transient RLN; BN = benign nodule; HT = Hashimoto’s thyroiditis; RLN = recurrent laryngeal nerve
Table 2 .
Results of the meta-analysis comparing HT to BNs
| Studies, n | HT | Benign | Total | Study heterogeneity | Publication bias | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patients, n | Patients, n | Patients, n | OR [95% CI] | p-value | Chi2 | I2 (%) | p-value | Begg | Egger | ||
| T-RLN palsy | 6 | 1475 | 17,919 | 19,394 | 0.99 (0.75–1.30) | 0.842 | 7.04 | 43.20 | 0.134 | 0.462 | 0.259 |
| P-RLN palsy | 6 | 1475 | 17,919 | 19,394 | 1.39 (0.84–2.33) | 0.234 | 3.46 | 42.20 | 0.177 | 1 | 0.223 |
| THC | 6 | 1531 | 17,845 | 19,376 | 1.32 (1.14–1.52) | <0.001 | 11.91 | 58.00 | 0.036 | 0.452 | 0.780 |
| PHP | 6 | 1537 | 18,026 | 19,563 | 1.21 (0.75–1.97) | 0.431 | 0.96 | 0.00 | 0.812 | 0.308 | 0.421 |
| All TT | |||||||||||
| THC | 3 | 205 | 826 | 1031 | 2.00 (1.35–2.95) | 0.001 | 5.23 | 61.80 | 0.073 | 1 | 0.689 |
| PHP | 2 | 201 | 764 | 965 | 1.33 (0.45–3.90) | 0.605 | 0.63 | 0.00 | 0.427 | 1 | NA |
BN = benign nodule; CI = confidence interval; HT = Hashimoto’s thyroiditis; OR = odds ratio; PHP = permanent hypoparathyroidism; P-RLN palsy = permanent recurrent laryngeal nerve palsy; THC = transient hypocalcaemia; T-RLN palsy = transient recurrent laryngeal nerve palsy; TT = total thyroidectomy
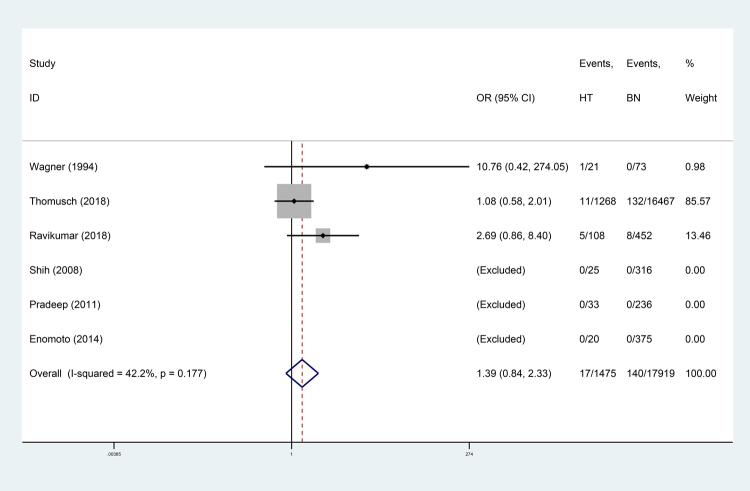
Permanent recurrent laryngeal nerve palsy
Six studies9,16,21–23,26 fulfilled this meta-analysis, but the data of three studies9,22,23 could not be estimated in the analysis. The results demonstrated no significant difference between the HT group and BN group in the risk for P-RLNP (OR 1.39, 95% CI: 0.84–2.33, p=0.234; Figure 3). Low between-studies heterogeneity was found (I2 42.20%, p=0.117; Table 2). No significant publication bias was found by Egger’s test (p=0.082; Table 2).
Figure 3 .
Forest plot and meta-analysis of permanent RLN; BN = benign nodule; HT = Hashimoto’s thyroiditis; RLN = recurrent laryngeal nerve
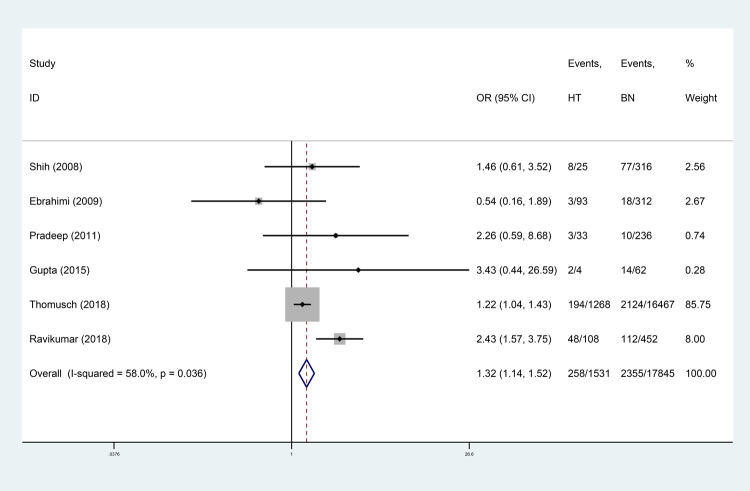
Transient hypocalcaemia
Six studies (19,376 cases) matched this meta-analysis of THC risk in the HT group versus that in the BN group.9,21,23–26 The rate of THC was significantly higher in the HT group (16.9%) than in the BN group (13.2%) (OR 1.32, 95% CI: 1.14–1.52, p<0.001; Figure 4). There was low heterogeneity among the studies (I2 58.00%, p=0.036; Table 2). There was no evidence of publication bias (Egger’s test p=0.780; Table 2).
Figure 4 .
Forest plot and meta-analysis of THC; BN = benign nodule; HT = Hashimoto’s thyroiditis; THC = transient hypocalcaemia
In all total thyroidectomy (TT) subgroup analyses, pooled analysis showed that the HT group had a higher risk for THC than the BN group (OR 2.00, 95% CI: 1.35–2.95, p=0.001; supplemental figure 1), with moderate heterogeneity (I2 61.80%, p=0.073, Table 2).
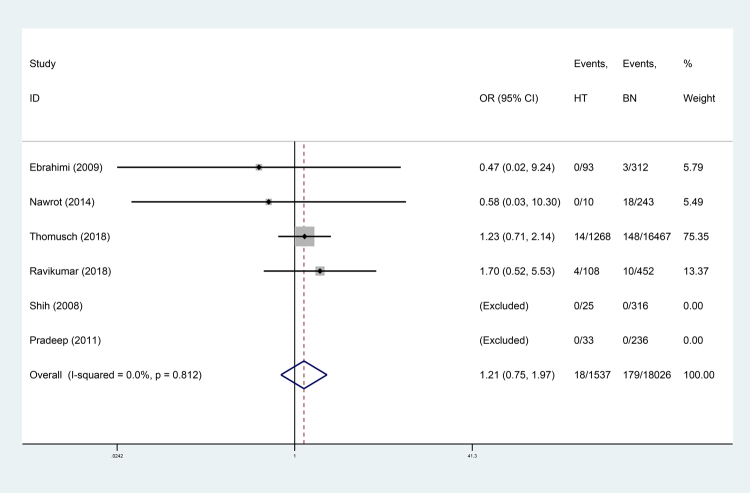
Permanent hypoparathyroidism
Six studies9,20,21,23,24,26 were used to conduct the analysis on the risk for PHP between the HT group and BN group. This analysis showed that there was no significant difference in the risk for PHP between the HT group and BN group (OR 1.21, 95% CI: 0.75–1.97, p=0.431; Figure 5), and no evidence of heterogeneity among the studies was found (I2 0.00%, p=0.812; Table 2). No publication bias was illustrated by Egger’s test (p=0.421; Table 2).
Figure 5 .
Forest plot and meta-analysis of PNP; BN = benign nodule; HT = Hashimoto’s thyroiditis; PNP = permanent hypoparathyroidism
In the analysis of all TT subgroups, there was no significant difference between the HT group and BN group (OR 1.33, 95% CI: 0.45–3.90, p=0.605; Supplemental figure 2), and there was no between-studies heterogeneity identified (I2 61.80%, p=0.073, Table 2).
Discussion
It is the common opinion of most surgeons that HT may increase the risk for postoperative complications.27 The adherence of thyroid tissue to the surrounding structures can be serious due to the fibrosis from HT inflammation in the thyroid region, which makes the RLN difficult to isolate.27 Moreover, most researchers believe that the main reasons HT inflammation results in parathyroid function injuries are based on the following viewpoints: first, HT inflammation-induced adhesions make operative procedures difficult and increase the likelihood of an insufficient blood supply. In general, the coexistence of HT and an associated fibrovascular connective tissue reaction involving the thyroid capsule and pericapsular soft tissues obviously enlarges the thyroid gland.19,28 It is difficult to dissect the parathyroid glands, which are located in the adhesive fibre coating between the natural capsule and surgical capsule.29 Second, the difficulty in identifying the thyroid glands will increase the chance of mistakenly making an incision. Concomitant regional lymphadenopathy is a common comorbidity in the thyroid gland surrounding HT. Furthermore, dense capsular tissue due to inflammatory changes may obscure the identification of glands located either within or close to the capsule, which makes the identification of the parathyroid glands even more challenging.30
However, it is still controversial whether the existence of HT would increase the risk for postoperative complications of thyroid surgery. This is thought to be the first meta-analysis to provide comprehensive insights into the risk for postoperative complications in HT patients. Results showed that there were no significant differences between the HT group and BN group in postoperative complications, including T-RLNP (3.93% and 3.91%, p=0.842; Figure 2) and P-RLNP (1.15% and 0.78%, p=0.234; Figure 3). Similarly, Thomusch et al26 demonstrated that autoimmune thyroid disease did not appear to influence T-RLNP and P-RLNP.
Because the surgical operation for HT is more difficult than that for non-HT (including single BN) due to intraoperative adhesions,31 difficult surgical procedures may increase the probability of developing postoperative complications. However, assessing the risk for RLN injury according to just surgical difficulty itself may be insufficient because the RLNP risk factors, including the technique of RLN identification, use of magnifying glasses, nerve monitoring and the extent of resection, need to be considered.26 Therefore, it is believed that the adhesions of HT were not a significant factor for RLN injury.
Moreover, these results demonstrated that HT increased the risk of THC compared with BN (16.85% and 13.20%, p<0.001, Table 2). However, there was no significant difference in the risk for PHP (1.17% and 0.99%, p=0.431) between the two groups. It has been reported that PHP is caused by removing all four parathyroid glands or by causing permanent damage as well as performing an inadequate parathyroid autotransplantation (PAT). THC is caused by reversible ischaemia to the parathyroid glands, hypothermia and the release of endothelin I.25,32 It is thought that HT patients suffer from a higher risk of reversible ischaemia to the parathyroid gland than single BN patients because Hashimoto’s inflammation increases vascularity as well as increasing fibrotic changes. Therefore, HT patients showed a higher risk of THC than BN patients. However, successful PAT could avoid the occurrence of PHP in thyroid surgery.32 Furthermore, HT did not appear to influence the vitality of PAT. Therefore, there was no significant difference in the risk for PHP between the HT and BN groups. To rule out the influence of the different extents of resection on the incidence rate of complications, further TT subgroup analysis was performed; the HT group showed higher risks for THC than the BN group (25.85% and 17.43%, p=0.001), but there was no significant difference in the risk of PHP between the two groups (p=0.605). Moreover, all TT groups were found to show a higher incidence rate of THC than the non-all TT group.
Nevertheless, this work does not provide evidence that the adhesions of HT inflammation make operative procedures more difficult, which would increase the risk for RLNP and PHP in patients with HT. We believe that HT patients have a higher prevalence of postoperative complications than BN patients, especially a higher risk for THC. THC is a frequent postoperative complication of thyroid surgery and the main reason for prolonged hospitalisation of these patients.33 Therefore, HT patients should receive preoperative and postoperative monitoring of their serum calcium (and parathyroid hormone) levels and calcium (and vitamin D) supplementation to prevent the occurrence of THC when undergoing surgery for HT. Moreover, the obviously increased risk for postoperative THC means that special attention should be paid to preserving the parathyroid glands. HT is commonly assessed by histopathologic examinations of thyroid specimens.34 If HT is diagnosed preoperatively, it may help clinicians evaluate the postoperative complication risks and facilitate making the optimal decision regarding the surgical approach and the extent of surgery. Several studies demonstrated that the preoperative anti-thyroglobulin antibody levels (positive anti-thyroglobulin antibodies, thyroglobulin >150ng/ml) could be used to predict a potentially more difficult operation in HT patients, and these levels may be associated with longer operative times and increased postoperative risk.19,27,31 Further investigations are necessary to clarify the link between anti-thyroglobulin antibody levels and degrees of adhesion and the incidence rate of complications in thyroidectomy.
Study limitations
This meta-analysis has several significant limitations. First, the study is based on the theory that HT causes adhesions, which make operative procedures difficult and increases the risk for postoperative complications. However, HT is the most common inflammatory thyroid disease. The degree of adhesion and the operative difficulty for each case in these studies is unclear. Second, only nine studies were included, and this small number especially impacts all of the TT subgroup analyses on the postoperative risk between the HT and BN groups (only three studies). Third, different study eras resulted in significantly different study weights. Fourth, thyroid surgeons with different levels of experience may have different effects on postoperative complications, but the subgroup analysis was unable to be carried out in this study. Finally, the definitions of THC and PHP among the various medical centres were inconsistent.
Conclusions
The meta-analysis showed that HT only increased the risk for the postoperative complication THC compared to BN. However, HT patients commonly have a higher prevalence rate of postoperative complications than those with a single BN. Understanding the significance of HT in postoperative hypoparathyroidism after thyroid surgery would help clinicians perform sufficient preoperative (and postoperative) assessments and to optimise surgical planning.
Acknowledgements
Thanks to Professor Xu for this design, Dr Lu and Dr Feng for manuscript revision and Dr Tan providing language help.
Disclosure
The authors reported no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Formatting of funding sources
This research was supported by Guangzhou medicine and healthcare technology projects (20141A011011, 20151A011007 and 20161A011008).
References
- 1.Hashimoto H. Zur Kenntniss der Lymphomatosen Veranderung der Schilddruse (Struma lymphomatosa). Arch Klin Chir 1912; 97: 219–248. [Google Scholar]
- 2.Thomas CG, Jr, Rutledge RG. Surgical intervention in chronic (Hashimoto's) thyroiditis. Ann Surg 1981; 193: 769–776. 10.1097/00000658-198106000-00013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gyory F, Lukacs G, Juhasz Fet al. Surgically treated Hashimoto's thyroiditis. Acta Chir Hung 1999; 38: 243–247. [PubMed] [Google Scholar]
- 4.Shimizu K, Nakajima Y, Kitagawa Wet al. Surgical therapy in Hashimoto's thyroiditis. J Nippon Med Sch 2003; 70: 34–39. 10.1272/jnms.70.34 [DOI] [PubMed] [Google Scholar]
- 5.Dayan CM, Daniels GH. Chronic autoimmune thyroiditis. N Engl J Med 1996; 335: 99–107. 10.1056/NEJM199607113350206 [DOI] [PubMed] [Google Scholar]
- 6.Zaletel K. Determinants of thyroid autoantibody production in Hashimoto's thyroiditis. Expert Rev Clin Immunol 2014; 3: 217. 10.1586/1744666x.3.2.217 [DOI] [PubMed] [Google Scholar]
- 7.Gasbarri A, Sciacchitano S, Marasco Aet al. Detection and molecular characterisation of thyroid cancer precursor lesions in a specific subset of Hashimoto's thyroiditis. Br J Cancer 2004; 91: 1096–1104. 10.1038/sj.bjc.6602097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.LiVolsi VA. The pathology of autoimmune thyroid disease: a review. Thyroid 1994; 4: 333–339. 10.1089/thy.1994.4.333 [DOI] [PubMed] [Google Scholar]
- 9.Shih ML, Lee JA, Hsieh CBet al. Thyroidectomy for Hashimoto's thyroiditis: complications and associated cancers. Thyroid 2008; 18: 729–734. 10.1089/thy.2007.0384 [DOI] [PubMed] [Google Scholar]
- 10.Goldenberg D, Swegal W, Dunklebarger M, Pellitteri PK. Surgery for fibro-adherent inflammatory thyroid disease. Oper Tech Otolaryngol Head Neck Surg 2018; 29: 2–9. 10.1016/j.otot.2017.12.002 [DOI] [Google Scholar]
- 11.Sarı S, Erbil Y, Sümer Aet al. Evaluation of recurrent laryngeal nerve monitoring in thyroid surgery. Int J Surg 2010; 8: 474–478. 10.1016/j.ijsu.2010.06.009 [DOI] [PubMed] [Google Scholar]
- 12.Jeannon JP, Orabi AA, Bruch GAet al. Diagnosis of recurrent laryngeal nerve palsy after thyroidectomy: a systematic review. Int J Clin Pract 2010; 63: 624–629. 10.1111/j.1742-1241.2008.01875.x [DOI] [PubMed] [Google Scholar]
- 13.Haugen BR. 2015. American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: What is new and what has changed? Arch Intern Med 2016; 156: 2165. 10.1002/cncr.30360 [DOI] [PubMed] [Google Scholar]
- 14.Harris SC. Thyroid and parathyroid surgical complications. Am J Surg 1992; 163: 476–478. 10.1016/0002-9610(92)90391-4 [DOI] [PubMed] [Google Scholar]
- 15.Proye C, Carnaille B, Maynou Cet al. The parathyroid risk in thyroid surgery. Argument against the early postoperative prescription of vitamin D. Experience with 729 thyroidectomies in 1988. Chirurgie; memoires de l'Academie de chirurgie 1990; 116: 493–500. [PubMed] [Google Scholar]
- 16.Wagner HE, Seiler C. Recurrent laryngeal nerve palsy after thyroid gland surgery. Br J Surg 2010; 81: 226–228. 10.1002/bjs.1800810222 [DOI] [PubMed] [Google Scholar]
- 17.Wilhelm SM, Mchenry CR. Total Thyroidectomy Is Superior to Subtotal Thyroidectomy for Management of Graves’ Disease in the United States. World J Surg 2010; 34: 1261–1264. 10.1007/s00268-009-0337-3 [DOI] [PubMed] [Google Scholar]
- 18.Wormer BA, Mchenry CR. Hashimoto's thyroiditis: Outcome of surgical resection for patients with thyromegaly and compressive symptoms. Am J Surg 2011; 201: 416–419. 10.1016/j.amjsurg.2010.08.021 [DOI] [PubMed] [Google Scholar]
- 19.McManus C, Luo J, Sippel R, Chen H. Is thyroidectomy in patients with Hashimoto thyroiditis more risky? J Surg Res 2012; 178: 529–532. 10.1016/j.jss.2012.09.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nawrot I, Pragacz A, Pragacz Ket al. Total Thyroidectomy is Associated with Increased Prevalence of Permanent Hypoparathyroidism. Med Sci Monit 2014; 20: 1675–1681. 10.12659/MSM.890988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ravikumar K, Muthukumar S, Sadacharan Det al. The Impact of Thyroiditis on Morbidity and Safety in Patients Undergoing Total Thyroidectomy. Indian J Endocrinol Metab 2018; 22: 494–498. 10.4103/ijem.IJEM_209_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Enomoto K, Uchino S, Watanabe Set al. Recurrent laryngeal nerve palsy during surgery for benign thyroid diseases: Risk factors and outcome analysis. Surgery 2014; 155: 522–528. 10.1016/j.surg.2013.11.005 [DOI] [PubMed] [Google Scholar]
- 23.Pradeep PV, Ragavan M, Ramakrishna BAet al. Surgery in Hashimoto's thyroiditis: Indications, complications, and associated cancers. J Postgrad Med 2011; 57: 120. 10.4103/0022-3859.81867 [DOI] [PubMed] [Google Scholar]
- 24.Houman E, Pam E, Ihre L Catharinaet al. Does autoimmune thyroid disease affect parathyroid autotransplantation and survival? ANZ J Surg 2010; 79: 383–385. 10.1111/j.1445-2197.2009.04894.x [DOI] [PubMed] [Google Scholar]
- 25.Gupta S, Chaudhary P, Durga CK, Naskar D. Validation of intra-operative parathyroid hormone and its decline as early predictors of hypoparathyroidism after total thyroidectomy: A prospective cohort study. Int J Surg 2015; 18: 150–153. 10.1016/j.ijsu.2015.04.074 [DOI] [PubMed] [Google Scholar]
- 26.Thomusch O, Sekulla C, Billmann Fet al. Risk profile analysis and complications after surgery for autoimmune thyroid disease. Br J Surg 2018; 105: 677-85. 10.1002/bjs.10770 [DOI] [PubMed] [Google Scholar]
- 27.McManus C, Luo J, Sippel R, Chen H. Should patients with symptomatic Hashimoto's thyroiditis pursue surgery? J Surg Res 2011; 170: 52–55. 10.1016/j.jss.2011.01.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schneider DF, Mazeh H, Oltmann SCet al. Novel thyroidectomy difficulty scale correlates with operative times. World J Surg 2014; 38: 1984–1989. 10.1007/s00268-014-2489-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lin DT, Patel SG, Shaha ARet al. Incidence of inadvertent parathyroid removal during thyroidectomy. The Laryngoscope 2002; 112: 608–611. 10.1097/00005537-200204000-00003 [DOI] [PubMed] [Google Scholar]
- 30.Goldenberg D, Swegal W, Dunklebarger M, Pellitteri PK. Surgery for fibro adherent inflammatory thyroid disease. Oper Tech Otolaryngol Head Neck Surg 2017; 29: 2–9. 10.1016/j.otot.2017.12.002 [DOI] [Google Scholar]
- 31.Mok VM, Oltmann SC, Herbert Cet al. Identifying predictors of a difficult thyroidectomy. J Surg Res 2014; 190: 157–163. 10.1016/j.jss.2014.03.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ebrahimi H, Edhouse P, Lundgren CIet al. Does autoimmune thyroid disease affect parathyroid autotransplantation and survival? ANZ J Surg 2009; 79: 383–385. 10.1111/j.1445-2197.2009.04894.x [DOI] [PubMed] [Google Scholar]
- 33.Saad J Jeffrey, Pieter N J, Dukas AGet al. Prediction of hypocalcemia after using 1- to 6-hour postoperative parathyroid hormone and calcium levels: an analysis of pooled individual patient data from 3 observational studies. Head Neck 2010; 32: 427–434. 10.1002/hed.21199 [DOI] [PubMed] [Google Scholar]
- 34.Kim HG, Kim E-K, Han KHet al. Pathologic spectrum of lymphocytic infiltration and recurrence of papillary thyroid carcinoma. Yonsei Med J 2014; 55: 879–885. 10.3349/ymj.2014.55.4.879 [DOI] [PMC free article] [PubMed] [Google Scholar]