Abstract
Background
Zika virus infection is commonly described as a mild and self-limiting illness. However, cardiac complications were associated with acute Zika virus infection.
Case presentation
A 46-year-old woman without previous comorbidities with a 1-day history of symptoms tested positive for ZIKV by real time reverse transcriptase polymerase chain reaction (rRT-PCR). She was admitted two days after with clinical worsening, cardiac enzymes elevated, and cardiac imaging findings, and the diagnosis of myopericarditis was made. The patient was treated and presented significant clinical improvement after one year.
Conclusions
Cardiac complication following ZIKV infection appears to be infrequent. Here, we report a rare case of viral myopericarditis caused by ZIKV infection.
Keywords: Zika, Myopericarditis, Myopericarditis virus-induced, Heart, Cardiac
Background
Zika virus (ZIKV) is an arthropod-borne virus transmitted by Aedes sp. mosquitoes and has been reportedly detected in humans since 1954 [1]. However, following rapid spread around the globe and reports of neurological complications, in February 2016 the World Health Organization declared it a public health emergency of international concern [2]. Zika virus is regarded as causing a benign and self-limiting infection with symptoms lasting from few days to a week [3]. Occasionally, ZIKV infection has been associated with significant neurological complications, especially microcephaly and other congenital abnormalities, Guillain-Barré syndrome, encephalitis, myelitis, and meningoencephalitis, and other possible threats of the virus may have been overlooked [4]. Although the heart is amongst the organs reported to be affected by this infection, there are few studies describing the cardiac alterations associated to ZIKV infection [5–11]. Here, we describe cardiovascular complications occurred during the acute phase of ZIKV infection.
Case presentation
A 46-year-old healthy woman presented at the outpatient clinic of Tropical Medicine Foundation Doctor Heitor Vieira Dourado (FMT-HVD) with a one-day history of itchy maculopapular rash, fever, conjunctival hyperemia and periarticular edema preceded by myalgia and diarrhea. She lived in Manaus, Amazonas, Brazil and had no history of travelling within the previous month. Initial examination revealed a body temperature of 39.2 °C, bilateral conjunctivitis and maculopapular skin rash in trunk and limbs. Blood pressure (114/80 mm Hg) was normal and heart rate was 122 bpm. Blood and urine samples tested positive for ZIKV by real time reverse transcriptase polymerase chain reaction (rRT-PCR). Blood cell count was normal. After two days of the diagnosis, she returned with worsening of clinical presentation, fatigue, vomiting, diarrhea, dyspnea and lower limbs edema. Physical examination revealed hypotension (103/81 mm Hg) and persistence of the tachycardia (120 bpm). She was admitted to the ward and laboratory results showed an increase in the creatine kinase (CK) 4.027 U/L (normal < 170 U/L), creatine kinase-muscle/brain (CK-MB) 99U/L (normal < 25 U/L) and creatine kinase-muscle mass (CKMB) 29.4 U/L (normal < 4.3 U/L). The troponin T [0.27 ng/mL (normal < 0.04 ng/mL)], and myoglobin [> 500 ng/mL (normal < 107 ng/mL)] were elevated. The chest x-ray revealed hypotransparency on bases and enlarged cardiac silhouette. Her electrocardiogram (ECG) showed normal sinus rhythm. The 24-h ECG monitoring was normal. The echocardiogram (echo) revealed a left ventricular ejection fraction of 64% and a moderate pericardial effusion, without signs of cardiac tamponade. The cardiac magnetic resonance imaging (cMRI) revealed a thickening of the pericardium, moderate pericardial effusion (Fig. 1A) and an intramyocardial area with gadolinium enhancement involving the basal medial segment of the anterior septal wall (Fig. 1B) compatible with inflammatory changes observed in viral myocarditis based on Lake-Louis consensus criteria. The biventricular systolic function was preserved, and the myocardial perfusion was within the normal range. Based on her symptoms, biomarkers and imaging findings, a clinical diagnosis of myopericarditis was made. Treatment with colchicine, bisoprolol, furosemide and spironolactone were introduced. We observed a fast normalization of CK and troponin T levels and clinical improvement. The RT-PCR tests performed yielded negative results for dengue, chikungunya, cytomegalovirus, Epstein Barr virus, herpesvirus, varicella zoster virus, parvovirus B19 and enteroviruses. Serologies were negative for human immunodeficiency virus (HIV), hepatitis B (HBV) and C (HCV) virus. Five months later, the left ventricular ejection fraction was 74% and revealed a minimum pericardial effusion, without signs of cardiac tamponade. After one year, the cMRI showed absence of pericardial effusion (Fig. 1C) and a small area of intramyocardial hyperintensity involving the basal medial segment of the anterior septal wall. This was compatible with a fibrosis with characteristic pattern non-ischemic cardiomyopathies (Fig. 1D). The patient presented significant clinical improvement.
Fig. 1.
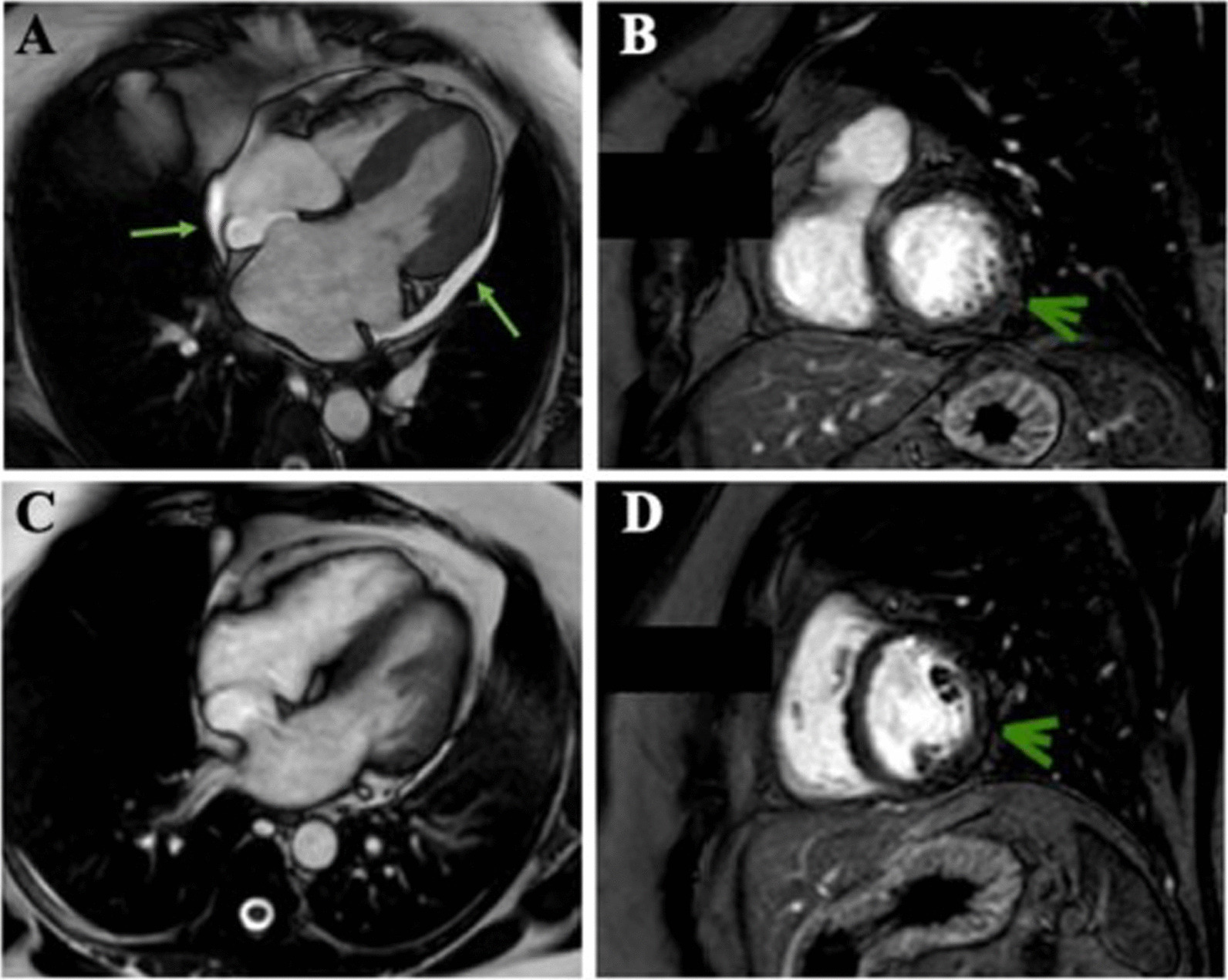
A cMRI of the heart in the FIESTA sequence in the four-chamber plane demonstrating pericardial effusion (green arrows). B cMRI of the heart in the FIESTA sequence in the short-axis demonstrating slight change in myocardial signal intensity (green arrow). C cMRI of the heart in the FIESTA sequence in the four-chamber plane, 1-year evolutionary control, demonstrating significant improvements in pericardial effusion. D cMRI of the heart in the FIESTA sequence in the short-axis, 1-year evolutionary control, demonstrating slight change in myocardial signal intensity (green arrow)
ZIKV, dengue and chikungunya detection was performed by rRT-PCR employing the commercially available kit ZDC from Instituto de Tecnologia em Imunobiológicos Biomanguinhos.. Serum sample was screened for five herpesviruses: herpes simplex virus type 1and 2 (HSV-1 and HSV-2), Cytomegalovirus (CMV), varicella zoster virus (VZV), Epstein-Barr virus (EBV) by multiplex PCR [12]. Seminested PCR was used for the identification of Parvovirus B19 [13] and of all enteroviruses [14]. Serology for HIV, HBV and HCV were assessed by immunochromatographic rapid tests.
The patient was enrolled in a prospective cohort study designed to assess the persistence of ZIKV in different body fluids. The study protocol was approved by institutional ethics committee as described by Calvet et al., 2018 [15]. Written informed consent was obtained from the patient.
Discussion and conclusions
We describe a ZIKV infection case presenting with rarely described myopericarditis. Viral infections are among the most common reported causes of myopericarditis in high-income countries especially the genus enteroviruses, herpesviruses, adenoviruses, influenza A and B, parvovirus B19, HBV, HCV, HIV, and Varicella [16]. Potential infectious causes of myopericarditis were ruled out in this case. Immunopathic causes of myopericarditis are vasculitis in connective tissue diseases, inflammatory bowel diseases, radiation-induced and drug-induced myopericarditis [16]. Congenital ZIKAV syndrome has been associated with neurological disorders. Involvement of other organs such as the heart has also been reported, but without clinical and complementary exam evidence of myocarditis or pericarditis. A previous study reported that 13.5% of the echocardiograms performed in children with congenital ZIKV infection presented findings compatible with congenital heart disease [5]. The most common echocardiographic findings were ostium secundum atrial septal defect and ventricular septal defect [5]. Chan et al. observed the presence of viral RNA in the cardiac muscle of mice infected by ZIKV [6]. Acute inflammatory disease of the myocardium or pericardium has been rarely described in ZIKV infection. Aletti et al. documented transitory myocarditis associated with the ZIKV. The diagnosis of cardiac involvement was made by the increase of CPK, troponin T and ST-segment elevation in anteroseptal region, associated with serological confirmation of ZIKV infection. The cMRI performed 10 days later showed a slight left ventricular dilatation [7]. The evaluation of critical patients, with unfavorable outcome, by Zonneveld et al., revealed only elevation of CK and its CK-MB fraction, without electrocardiographic changes suggesting acute myocardial infarction [8]. Carta et al. detected the presence of arrhythmias in patients with cardiac symptoms from ZIKV endemic area. The main manifestations at the ECG were acute atrial fibrillation, ventricular arrhythmias, and non-sustained atrial tachycardia. Five of the six heart failure patients had a low ejection fraction [9]. This study focused on the potential threat that ZIKV may pose to the heart like others arboviral diseases [10]. Villamil-Goméz et al. suggested that ZIKV can frequently affect the heart, as shown by electrocardiographic changes and pericardial effusion by echocardiogram, but without clinical manifestations of cardiac involvement. It is possible that the described changes could be part of a systemic inflammatory response rather than a direct viral aggression [11]. The cMRI showed fibrosis in the acute phase. Two other cases reported fibrosis in the acute phase of myopericarditis associated with ECHO virus and with primary HIV infection in young people [17, 18]. Although cRMI is mandatory to have a non-invasive confirmation of the clinical diagnosis in high-income countries, it is not highly accessible in low-income countries because of its high cost [19]. Our patient was managed with beta-blocker, diuretics and colchicine. Colchicine has been shown to be useful in myopericarditis due to its mechanisms of down, such as down regulation of multiple inflammatory pathways and modulation of inate immunity [20]. A previous study has shown that colchicine was associated with complete resolution of myocarditis in 63% of cases [21]. A recent report confirmed the benefit of colchicine in 86 patients with myopericarditis, with 64% of complete resolution on cardiac resonance at one year of follow-up. We did not use in this case non-steroidal anti-inflammatory because of the high risk of acute kidney injury in a patient with shock and rhabdomyolysis [22].
We report a rare case of viral myopericarditis likely caused by ZIKV infection. The case described was unusual because the virus-induced myopericarditis resolved quickly and without sequelae. However, the cRMI performed after one year revealed myocardial fibrosis. Knowing the possible cardiac impact of ZIKV, careful monitoring of its function and rhythm should be done in ZIKV infected patients who present with any cardiac symptoms.
Acknowledgements
We are grateful to the patient who consent to report the case, the ZIKABRA study staff in Manaus (Aline Alencar, Luiz Henrique Maciel, Francielen Furtado, Nágila Rocha, Pâmela Cunha Teixeira, Thaís Sodré, and Mirlene Alencar) for the administrative and clinical support and to the ZIKABRA Study Team (in alphabetical order): Abreu, André Luiz de; Bermudez, Ximena Pamela Diaz; Bôtto-Menezes, Camila Helena Aguiar; Brasil, Patrícia; Brito, Carlos Alexandre Antunes; Broutet, Nathalie Jeanne Nicole; Calvet, Guilherme Amaral; Castilho, Marcia da Costa; Fernandes, Tatiana Jorge; Filippis, Ana Maria Bispo de; Franca, Rafael Freitas Oliveira; Giozza, Silvana Pereira; Habib, Ndema; Kara, Edna Oliveira; Lacerda, Marcus Vinicius Guimarães; Landoulsi, Sihem; Lima, Morganna Costa; Lima, Noemia; Mello, Maeve Brito de; Menezes, Ana Izabel Costa de; Meurant, Robyn; Modjarrad, Kayvon; Neto, Armando Menezes; Pereira, Gerson Fernando, Pimenta, Cristina; Storme, Casey; Ströher, Ute; Thorson, Anna; Trautman, Lydie.
Abbreviations
- ZIKV
Zika virus
- FMT-HVD
Tropical Medicine Foundation Doctor Heitor Vieira Dourado
- rRT-PCR
Real time reverse transcriptase polymerase chain reaction
- CK
Creatine kinase
- CK-MB
Creatine kinase-muscle/brain
- CKMB
Creatine kinase-muscle mass
- ECG
Electrocardiogram
- echo
Echocardiogram
- cMRI
Cardiac magnetic resonance imaging
- HIV
Human immunodeficiency virus
- HBV
Hepatitis B virus
- HCV
Hepatitis C virus
- HSV-1
Herpes simplex virus type 1
- HSV-2
Herpes simplex virus type 2
- CMV
Cytomegalovirus
- VZV
Varicella zoster virus
- EBV
Epstein–Barr virus
Author contributions
Conceptualization, CB-M, GAC and EOK; investigation, IPS, CB-M, KNC, MVGdL, CAAdB, MdCC and MBB; data curation, CB-M; writing—original draft preparation, IPS and CB-M; writing—review and editing, IPS, CB-M, MVGdL, RFOF, GAC, AMBdF, EOK, and LAH, visualization, IPS, CB-M, KNC, ACdCF, MVGdL, AMN, RFOF, CAAdB, GAC, PB, AMBdF, EOK, NJNB, MdCC, MBB, KM and LAH; supervision, MVGdL; project administration, CB-M. All authors read and approved the final manuscript.
Funding
This case report was conducted in the context of the ZIKABRA cohort study which received support from: Wellcome Trust (Grant Number 206522/Z/17/Z), World Health Organization (Reference TSA1-2017/720873-0 and TSA2-2017/731359-0), Brazilian Ministry of Health (Convênio 837059/2016, Processo 25000162039201616), National Institute Of Allergy And Infectious Diseases of the National Institutes of Health (Award Number R21AI139777) and the Henry M. Jackson Foundation for the Advancement of Military Medicine (Prime Award No W81XWH-18-2-0040). The publication fee was supported by Fapeam (Resolução N. 002/2008, 007/2018 and 005/2019-Pró-Estado). All the funders had no role in study design, data collection, analysis, decision to publish, or preparation of the manuscript.
Availability of data and materials
Data sharing is not applicable to this case report as no datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
The study protocol was approved by Research Ethics Review Committee (WHO ERC), Protocol ID: ERC.0002786; Brazilian National Research Ethics Commission (CONEP) (CAAE: 62.518.016.6.1001.0008); Institutional Ethics and Research Committee of the Evandro Chagas National Institute of Infectious Diseases, Fiocruz, Rio de Janeiro (CAAE: 62.518.016.6.2002.5262), Ethics and Research Committee of the Rio de Janeiro’s Municipal Secretary of Health (CAAE: 2.518.016.6.3001.5279); Institutional Ethics and Research Committee of the Aggeu Magalhães Research Center, Fiocruz, Recife (CAAE: 62.518.016.6.2001.5190) and Institutional Ethics and Research Committee of the Tropical Medicine Foundation, Manaus, Amazonas (CAAE: 62.518.016.6.2003.0005). Written informed consent was obtained from the patient.
Consent for publication
Written informed consent for the publication was obtained from the patient.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Camila Helena Aguiar Bôtto-Menezes, Email: camila.chabm@gmail.com.
Izabella Picinin Safe, Email: izabellasafe@gmail.com.
Ana Cláudia da Cunha Ferreira, Email: anaclaudiadacunha@hotmail.com.
Katia do Nascimento Couceiro, Email: kcouceiro@uea.edu.br.
Armando Menezes Neto, Email: armandomenezes@gmail.com.
Rafael Freitas Oliveira Franca, Email: rafael.franca@cpqam.fiocruz.br.
Guilherme Amaral Calvet, Email: guilherme.calvet@ini.fiocruz.br.
Ana Maria Bispo de Filippis, Email: ana.bispo@ioc.fiocruz.br.
Edna Oliveira Kara, Email: karae@who.int.
Marcia da Costa Castilho, Email: mcastilho@fmt.am.gov.br.
Michele Souza Bastos, Email: michelebastos99@gmail.com.
Carlos Alexandre Antunes de Brito, Email: cbritoc@gmail.com.
Kayvon Modjarrad, Email: kmodjarrad@hivresearch.org.
Nathalie Jeanne Nicole Broutet, Email: broutetn@who.int.
Patrícia Brasil, Email: patricia.brasil@ini.fiocruz.br.
Ludhmila Abrahão Hajjar, Email: ludhmila@terra.com.br.
Marcus Vinícius Guimarães de Lacerda, Email: marcuslacerda.br@gmail.com.
References
- 1.Macnamara FN. Zika virus: a report on three cases of human infection during an epidemic of jaundice in Nigeria. Trans R Soc Trop Med Hyg. 1954;48:139–145. doi: 10.1016/0035-9203(54)90006-1. [DOI] [PubMed] [Google Scholar]
- 2.Gulland A. Zika virus is a global public health emergency, declares WHO. BMJ. 2016;352:i657. doi: 10.1136/bmj.i657. [DOI] [PubMed] [Google Scholar]
- 3.CDC. Zika virus disease. Available online: https://www.cdc.gov/zika/about/overview.html. (accessed on 5 August 2019).
- 4.PAHO. Epidemiological alert: neurological syndrome, congenital malformations, and Zika virus infection—implications for public health in the Americas. Washington, DC: Pan American Health Organization, December 1, 2015. Available online: https://www.paho.org/hq/dmdocuments/2015/2015-dec-1-cha-epi-alert-zika-neuro-syndrome.pdf. (accessed on 5 August 2019).
- 5.Di Cavalcanti D, Alves LV, Furtado GJ, Santos CC, Feitosa FG, Ribeiro MC, et al. Echocardiographic findings in infants with presumed congenital Zika syndrome: retrospective case series study. PloS ONE. 2017; 12 (4). [DOI] [PMC free article] [PubMed]
- 6.Chan JFW, Yip CCY, Tsang JOL, Tee KM, Cai JP, Chik KKH, et al. Differential cell line susceptibility to the emerging Zika virus: implications for disease pathogenesis, non-vector-borne human transmission and animal reservoirs. Emerg Microbes Infect. 2016;5(8):e93. doi: 10.1038/emi.2016.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aletti M, Lecoules S, Kanczuga V, Soler C, Maquart M, Simon F, et al. Transient myocarditis associated with acute Zika virus infection. Clin Infect Dis. 2017;64(5):678–679. doi: 10.1093/cid/ciw802. [DOI] [PubMed] [Google Scholar]
- 8.Zonneveld R, Roosblad J, van Staveren JW, Wilschut JC, Vreden SGS, Codringtin J. Three atypical lethal cases associated with acute Zika virus infection in Suriname. ID Cases. 2016;5:49–53. doi: 10.1016/j.idcr.2016.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carta KAG, Mendonza I, Morr I, Misticchio F, Meza Y, Finizola V, et al. Myocarditis, heart failure and arrhythmias in patients with Zika. JACC. 2017;69(11):906. doi: 10.1016/S0735-1097(17)34295-X. [DOI] [Google Scholar]
- 10.Minhas AM, Nayab A, Iyer S, Narmeen M, Fatima K, Khan MS, Constantin J. Association of zika virus with myocarditis, heart failure, and arrhythmias: a literature review. Cureus. 2017;9(6):e1399. doi: 10.7759/cureus.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Villamil-Goméz WE, Ramirez-Vallejo E, Rodriguez-Morales AJ. Cardiac compromise in Zika virus infection. Mayo Clin Proc. 2018;93(3):393–394. doi: 10.1016/j.mayocp.2017.12.006. [DOI] [PubMed] [Google Scholar]
- 12.Markoulatos P, Georgopoulou A, Siafakas N, Plakokefalos E, Tzanakaki G, Kourea-Kremastinou J. Laboratory diagnosis of common herpesvirus infections of the central nervous system by a multiplex PCR assay. J Clin Microbiol. 2001;39:4426–4432. doi: 10.1128/JCM.39.12.4426-4432.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mendonça MC, Ferreira AM, Santos MG, Oviedo EC, Bello MS, Siqueira MM, et al. Genotyping of human parvovirus B19 in clinical samples from Brazil and Paraguay using heteroduplex mobility assay, single-stranded conformation polymorphism and nucleotide sequencing. Mem Inst Oswaldo Cruz. 2011;106(4):502–504. doi: 10.1590/S0074-02762011000400019. [DOI] [PubMed] [Google Scholar]
- 14.Nix WA, Oberste MS, Pallansch MA. Sensitive, seminested PCR amplification of VP1 sequences for direct identification of all enterovirus serotypes from original clinical specimens. J Clin Microbiol. 2006;44(8):2698–2704. doi: 10.1128/JCM.00542-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Calvet GA, Kara EO, Giozza SP, Bôtto-Menezes CHA, Gaillard P, de Oliveira Franca RF, et al. Study on the persistence of Zika virus (ZIKV) in body fluids of patients with ZIKV infection in Brazil. BMC Infect Dis. 2018;18(1):49. doi: 10.1186/s12879-018-2965-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Imazio M, Trinchero R. Myopericarditis: etiology, management, and prognosis. Int J Cardiol. 2008;127:17. doi: 10.1016/j.ijcard.2007.10.053. [DOI] [PubMed] [Google Scholar]
- 17.Fukuhara T, Kinoshita M, Bito K, Sawamura M, Motomura M, Kawakita S, Kawanishi K. Myopericarditis associated with ECHO virus type 3 infection–a case report. Jpn Circ J. 1983;47(11):1274–1280. doi: 10.1253/jcj.47.1274. [DOI] [PubMed] [Google Scholar]
- 18.Vandi G, Calza L, Girometti N, Manfredi R, Musumeci G, Bon I, Re MC. Acute onset myopericarditis as unusual presentation of primary HIV infection. Int J STD AIDS. 2017;28(2):199–201. doi: 10.1177/0956462416654852. [DOI] [PubMed] [Google Scholar]
- 19.Friedrich MG, Sechtem U, Schulz-Menger J, et al. Cardiovascular magnetic resonance in myocarditis: a JACC white paper. J Am Coll Cardiol. 2009;53:1475. doi: 10.1016/j.jacc.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leung YY, Yao Hui LL, Kraus VB. Colchicine-Update on mechanisms of action and therapeutic uses. Semin Arthritis Rheum. 2015;45(3):341–350. doi: 10.1016/j.semarthrit.2015.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morgenstern D, Lisko J, Boniface NC, et al. Myocarditis and colchicine: a new perspective from cardiac MRI. J Cardiovasc Magn Reson. 2016;18:O100. doi: 10.1186/1532-429X-18-S1-O100. [DOI] [Google Scholar]
- 22.Opstal TSJ, Fiolet ATL, van Broekhoven A, Mosterd A, Eikelboom JW, Nidorf SM, Thompson PL, Duyvendak M, van Eck JWM, van Beek EA, den Hartog F, Budgeon CA, Bax WA, Tijssen JGP, El Messaoudi S, Cornel JH, LoDoCo2 Trial Investigators Colchicine in patients with chronic coronary disease in relation to prior acute coronary syndrome. J Am Coll Cardiol. 2021;78(9):859–866. doi: 10.1016/j.jacc.2021.06.037. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this case report as no datasets were generated or analysed during the current study.


