With the disappointment brought by modest results of trials testing single-agent immune checkpoint inhibitors in recurrent ovarian cancer,1,2 renewed optimism arose around the possibility that combination treatments would deliver the positive results the community was waiting for. Surely, there would be a way to enhance the activity of immunotherapy in recurrent ovarian cancer, a setting in which progress had remained elusive. In other tumour types, chemotherapy had been shown to induce antigen presentation, priming tumour cells to become receptive to the immune attack triggered by PD-L1 inhibitors and yielding improved clinical outcomes.3,4 Those data revitalising the field of immunotherapy in solid tumours provided the rationale for also testing immune checkpoint inhibitors with chemotherapy in ovarian cancer.
In The Lancet Oncology, Eric Pujade-Lauraine and colleagues5 describe the results of the JAVELIN-200 trial, an open-label, randomised, phase 3 study of avelumab monotherapy, avelumab plus pegylated liposomal doxorubicin (PLD), and PLD monotherapy in women with platinum-resistant or platinum-refractory ovarian cancer. The primary endpoints were progression-free survival by blinded independent central review and overall survival. Prespecified biomarker analyses included assessment of PD-L1 expression and presence of CD8-positive cells. Overall, the trial did not show improvement in progression-free survival or overall survival with avelumab alone or avelumab plus PLD compared with PLD alone, either in the main analysis or in the predefined PD-L1-positive or CD8-positive subsets. However, in the cohort of patients whose tumours expressed PD-L1 and had CD8-positive cells, a group not prespecified a priori and representing approximately one third of the study population, the unstratified hazard ratios for both progression-free survival and overall survival were significant in favour of the combination.
The results of the study bring closure to a key question in the field and open the door for speculation, new hypotheses, and hope. JAVELIN-200 was a well designed and conducted trial, addressed a legitimate question, and, yet, yielded solidly negative results. The trial did not show a benefit for either single-agent immunotherapy or for chemoimmunotherapy in hard-to-treat, platinum-resistant ovarian cancer.5 The study population was a group with high, unmet need—approximately half of the participants had primary resistance to platinum, and a quarter of the participants had platinum-refractory cancer. The results confirm, and perhaps predict, outcomes of ongoing trials addressing a similar question. The randomised phase 3 IMagyn500 study, which examined carboplatin–paclitaxel–bevacizumab–atezolizumab versus carboplatin–paclitaxel–bevacizumab–placebo in patients with newly diagnosed ovarian cancer, reported no difference in progression-free survival or overall survival for the atezolizumab group.6 The ongoing NRG-GY009 trial, the results of which have not yet been reported, compares PLD plus bevacizumab, PLD plus atezolizumab, and PLD plus bevacizumab and atezolizumab. Whether the addition of VEGF blockade to the chemoimmunotherapy regimen will be sufficient to show a benefit remains to be answered; however, the results from JAVELIN-200 and IMagyn500 dampen optimism. Future directions for improving the activity of immune checkpoint blockade focus on combinations with novel immunomodulatory drugs (such as anti-CTLA-4, neoepitope vaccines, and chimeric antigen receptor T cells) or with drugs targeting the homologous recombination pathway, as attempted in TOPACIO and the ongoing DUO-O study.7,8
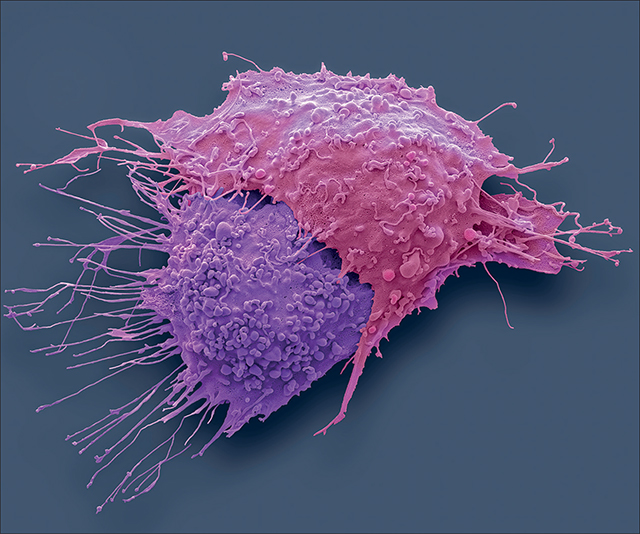
An alternative possibility is that immunotherapy might not be active for all patients with ovarian cancer, which means that it will be important to find biomarkers predictive of response for patient selection. Pujade-Lauraine and colleagues5 began to address this point by testing for PD-L1 and CD8 expression in archival or in de-novo collected tissue. A clinical benefit for the combination regimen was not found for either subgroup; however, improved hazard ratios for progression-free survival and overall survival versus chemotherapy alone were described for patients whose tumours were positive for both PD-L1 and CD8. Whether dual expression of CD8 and PD-L1 truly identifies an immune responsive subgroup of patients remains to be validated but represents a new starting point. Rapidly advancing technologies, including single cell sequencing and cytometry by time of flight, enable capturing immune cell populations within tumours at the single cell and single molecule level.9,10 Although the divide between the understanding of regulatory mechanisms fine-tuning antitumour immune responses and clinical investigation remains wide, we envision application of high-dimensional analyses to specimens from trials to occur in the immediate future. The ability to dive deeply into the tumour microenvironment will provide clues to optimal combinations for preselected groups of patients, extending the scope of personalised medicine beyond precision genomics and transcriptomics to include individualised approaches based on neighbouring cells and their effects within tumours.
Although trials testing immune checkpoint inhibitors in ovarian cancer have not delivered positive results, improved understanding of immune interactions in the tumour milieu, made possible by using high-dimensional technologies, stimulates continued efforts to overcome resistance to immune attack in this disease. We hope that the focus on rational combinations and the use of sophisticated real-time biomarkers will lead to long-awaited success.
Footnotes
We declare no competing interests.
Contributor Information
Emma Barber, Department of Obstetrics and Gynecology, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA; Robert H Lurie Comprehensive Cancer Center, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA.
Daniela Matei, Department of Obstetrics and Gynecology, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA; Robert H Lurie Comprehensive Cancer Center, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA; Jesse Brown VA Medical Center, Chicago, IL, USA.
References
- 1.Disis ML, Taylor MH, Kelly K, et al. Efficacy and safety of avelumab for patients with recurrent or refractory ovarian cancer: phase 1b results from the JAVELIN solid tumor trial. JAMA Oncol 2019; 5: 393–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Varga A, Piha-Paul S, Ott PA, et al. Pembrolizumab in patients with programmed death ligand 1-positive advanced ovarian cancer: analysis of KEYNOTE-028. Gynecol Oncol 2019; 152: 243–50. [DOI] [PubMed] [Google Scholar]
- 3.Shu CA, Gainor JF, Awad MM, et al. Neoadjuvant atezolizumab and chemotherapy in patients with resectable non-small-cell lung cancer: an open-label, multicentre, single-arm, phase 2 trial. Lancet Oncol 2020; 21: 786–95. [DOI] [PubMed] [Google Scholar]
- 4.Gandhi L, Rodríguez-Abreu D, Gadgeel S, et al. Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med 2018; 378: 2078–92. [DOI] [PubMed] [Google Scholar]
- 5.Pujade-Lauraine E, Fujiwara K, Ledermann JA, et al. Avelumab alone or in combination with chemotherapy versus chemotherapy alone in platinum-resistant or platinum-refractory ovarian cancer (JAVELIN Ovarian 200): an open-label, parallel-group, three-arm, randomised, phase 3 study. Lancet Oncol 2021; published online June 15. 10.1016/S1470-2045(21)00216-3 [DOI] [PubMed] [Google Scholar]
- 6.Moore KN, Bookman M, Sehouli J, et al. Atezolizumab, bevacizumab, and chemotherapy for newly diagnosed stage III or IV ovarian cancer: placebo-controlled randomized phase III trial (IMagyn050/GOG 3015/ENGOT-OV39). J Clin Oncol 2021; published online April 23. 10.1200/JCO.21.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Konstantinopoulos PA, Waggoner S, Vidal GA, et al. Single-arm phases 1 and 2 trial of niraparib in combination with pembrolizumab in patients with recurrent platinum-resistant ovarian carcinoma. JAMA Oncol 2019; 5: 1141–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harter P, Bidziński M, Colombo N, et al. DUO-O: a randomized phase III trial of durvalumab (durva) in combination with chemotherapy and bevacizumab (bev), followed by maintenance durva, bev and olaparib (olap), in newly diagnosed advanced ovarian cancer patients. Proc Am Soc Clin Oncol 2019; 37: TPS5598. [Google Scholar]
- 9.Krieg C, Nowicka M, Guglietta S, et al. High-dimensional single-cell analysis predicts response to anti-PD-1 immunotherapy. Nat Med 2018; 24: 144–53. [DOI] [PubMed] [Google Scholar]
- 10.Yofe I, Dahan R, Amit I. Single-cell genomic approaches for developing the next generation of immunotherapies. Nat Med 2020; 26: 171–77. [DOI] [PubMed] [Google Scholar]


