Abstract
Background
Mayotte is a French overseas territory with significant socio-economic and health challenges. This study updates the prevalence of hypertension in Mayotte to estimate the awareness, treatment and control of this disease and identify any associated factors.
Methods
Data were taken from the cross-sectional Unono Wa Maore survey conducted in Mayotte in 2019. Analyses were based on the adult population aged 18–69 years who underwent a clinical examination with at least two blood pressure measurements (n = 2620).
Results
In 2019, the prevalence of hypertension was estimated at 38.4% (36.1–40.7%) in the Mayotte population aged 18–69 years. The prevalence was similar in men (38.5%) and women (38.3%; P = 0.95). The prevalence of certain risk factors was high, with 75% of hypertensives being overweight or obese, 13% reporting diabetes and 69% being occupationally inactive. Among the hypertensives, 48% was aware of their diagnosis, with women more likely to be aware than men (P < 0.0001). Of those who were aware, 45% were treated pharmacologically and 49% reported engaging in physical activity to lower their blood pressure. The control rate was 30.2% among pharmacologically treated hypertensives. Overall, 80% of hypertensive patients had too high blood pressure during the survey’s clinical examination.
Conclusion
The prevalence of hypertension remains high in Mayotte, where certain risk factors like obesity are particularly common in the population. Awareness, treatment and control remain insufficient. Primary prevention measures, access to a healthy food, and screening and treatment of hypertension should be encouraged by targeting the most affected populations.
Introduction
Hypertension is a chronic condition affecting 1.3 billion people worldwide and is a major risk factor for stroke and cardiovascular disease.1–3 Major disparities in the risk, awareness and management of hypertension have been observed according to the socio-economic level of the country as well as the socio-demographic and medical characteristics of the population.4–6
In metropolitan France, which is a high-income country, the prevalence of hypertension was estimated at 30.6% in 2015, with one in two people being aware of their disease.7 In the French overseas territories, the situation tends to be poorer than in metropolitan France and other high-income countries. Only a few recent estimates of the prevalence, awareness and management of hypertension are available for the overseas territories, which are marked by socio-demographic and health care differences compared with metropolitan France.8,9
Mayotte is a French overseas territory located in the Comoros archipelago in the Indian Ocean. The population was estimated at 256 500 in 2017, with half of the inhabitant aged under 18 years.10 The island is subject to many migratory flows as more than half of the population was not born in Mayotte, coming mostly from the island of Anjouan and the other islands of the Comoros.11 Poverty and precarity are major issues in Mayotte, where the majority of the population is unemployed and lives below the national poverty line.12 Access to health care is difficult and the supply of primary care is extremely limited compared with the rest of France.13 Consequently, specific studies on the health status of this territory are needed. This is the purpose of the general population survey ‘Unono Wa Maore’ which aims to assess the health status of the inhabitants of the island of Mayotte.14
In Mayotte, the prevalence of hypertension was estimated at 44% among people aged 30–69 years in 2008, with 75% of hypertensive people being unaware of their diagnosis.15,16
The study therefore aimed to update the prevalence of hypertension in Mayotte, estimate the awareness, treatment and control of this disease, and identify associated factors, based on data from the Unono Wa Maore survey.
Methods
The Unono Wa Maore survey
The Unono Wa Maore survey is a cross-sectional study carried out on a random sample of the general population of Mayotte to describe their health status.14 The inclusion criteria were age under 70 years and residing in Mayotte for at least 3 months. Participants were included between November 2018 and May 2019, using a two-stage survey design (household, household individual). The selected persons were invited to complete a face-to-face questionnaire administered at home by trained investigators. Information was collected on socio-demographic and medical variables. Four questionnaires were used: one for children under 3 years old, one for children between 3 and 14 years old and two (short and long versions) for people aged from 15 to 69. The first person aged 15 years and over who was selected in the household answered the long questionnaire, while the other household members used the short questionnaire. Questions about hypertension were included in both questionnaires for people over 15 years. In total 6946 individuals answered one of the questionnaires, including 4643 aged 15 years and over.
After the interviews, a nurse carried out a clinical examination at home. This clinical examination included standardized anthropometric measurements, blood pressure (BP) measurements, biological blood samples and urine and vaginal self-samples. BP was measured with a validated automatic device (CARAT BOSO pro range BP monitor) with three cuffs available depending on the circumference of the arm. Three measurements were taken in a sitting position, after 5 minutes of rest and with one minute of rest between each BP measurement.. In total, 2993 people aged 15 and over underwent a clinical examination as the investigation was stopped in May 2019 (difficulty in performing fasting venous sampling during Ramadan). For the purpose of this article on hypertension, we only included individuals aged 18–69 years who had at least two BP measurements taken during the clinical examination (n = 2620) (65% had three BP measurements) (Supplementary figure S1).
Ethics
This study received a favourable decision from the Comité de Protection des Personnes Ile-de-France VIII on 23 November 2018. The investigation complies with the reference methodology MR001 (agreement of the Commission Nationale Informatique et Libertés of 25 September 2018). Each randomly selected person was invited to participate in the study after presenting its objectives and participation criteria. The participation rate was 91% for people aged 15–69 and over 98% for children.
Hypertension definitions
Patients were considered hypertensive if they declared being hypertensive and/or if the average of the last two systolic BP measurements during the clinical examination was ≥140 mm Hg and/or diastolic BP ≥90 mm Hg. As defined by the European Society of Cardiology and the European Society of Hypertension, BP values were classified into six levels: optimal BP, normal BP, high normal BP, hypertension grade 1, hypertension grade 2 and hypertension grade 3 as defined by the European Society of Cardiology and the European Society of Hypertension.17
Participants were considered aware of their hypertension if they responded affirmatively to the question ‘Have you ever been told by a doctor or other health care professional that your BP was too high?’. Among hypertensive participants who were aware of their disease, a person was considered treated for hypertension if they declared taking medication to lower their BP. Among those who reported taking antihypertensive treatment, hypertension was considered controlled when systolic BP was <140 mm Hg and diastolic BP was <90 mm Hg.
To simplify international comparisons, an estimate of the prevalence of treated or measured hypertension was calculated (vs. reported or measured in the main analysis).
Covariates
Body mass index (BMI) was estimated using the anthropometric measurements from the clinical examination. Other variables (diabetes, tobacco and alcohol consumption, level of education, employment, etc.) were collected in the questionnaires. Missing covariate data were attributed to no exposure. Some information such as origin, level of physical activity, financial situation and health insurance is only available for people who answered the long questionnaire.
Statistical analysis
All estimations were weighted to take into account the sampling design and non-responses at the household and individual levels. Comparisons between groups were evaluated using chi-square and Student t-tests. Each prevalence was given with a 95% confidence interval (CI). Weighted logistic regressions were used to identify the factors associated with hypertension in the Mayotte population as well as the awareness, treatment and control of the disease. Logistic regressions were adjusted on hypertension risk factors and on socio-demographic characteristics of the population available in the whole study population (long questionnaire variables) in order to retain sufficient statistical power [sex, age, diabetes, obesity (or overweight), tobacco, alcohol, professional inactivity, couple status]. An analysis of the sub-population aged 30–69 years was carried out to correspond to the age group studied in 2008.16 All the statistical analyses were performed using SAS software (version 7.1; SAS Institute, Cary, NC, USA).
Results
Of the Unono Wa Maore participants, 2620 were included in the hypertension analysis (951 men and 1669 women). After weighting, the mean age was 36.6 years and 54.5% were women. The proportion of overweight or obese people was 61.6%, being higher in women than in men (71.8% vs. 49.4%, P < 0.0001). The proportion of smokers and daily drinkers was 12.1% and 1.4%, respectively, affecting significantly more men than women (23.2% vs. 2.9%, P < 0.0001; 3.1% vs. 0.1%, P < 0.0001). The proportion of people with a low level of physical activity was 34.8%, being significantly lower for women. Of the 1417 respondents to the long questionnaire, 62.8% had health insurance. More than half (53.9%) were from the Comoros, and only a third (37.2%) were born in Mayotte (table 1).
Table 1.
Characteristics of the study population, Mayotte, Unono Wa Maore, 2019
| Total |
95% CI | Men |
Women |
P-value (M/W) | ||
|---|---|---|---|---|---|---|
|
N = 2620 |
N = 951 |
N = 1669 |
||||
| n | %weighted | %weighted | %weighted | |||
| Cardiovascular risk factors | ||||||
| Age, years | ||||||
| 18–29 | 764 | 34.1 | (31.8–36.4) | 31.7 | 36.2 | 0.01 |
| 30–39 | 719 | 28.2 | (26.1–30.3) | 26.4 | 29.7 | |
| 40–49 | 583 | 21.0 | (19.1–22.9) | 22.7 | 19.5 | |
| 50–59 | 343 | 11.0 | (9.6–12.3) | 12.5 | 9.7 | |
| 60–69 | 211 | 5.8 | (4.9–6.7) | 6.8 | 5.0 | |
| Diabetes (reported) | ||||||
| No | 2409 | 92.9 | (91.7–94.1) | 94 | 92.0 | 0.10 |
| Yes | 211 | 7.1 | (5.9–8.3) | 6 | 8.0 | |
| BMI | ||||||
| Under weight (BMI < 18.5) | 72 | 3.2 | (2.3–4.1) | 3.1 | 3.2 | <0.0001 |
| Normal (18.5 ≤ BMI < 25) | 831 | 35.2 | (32.9–37.5) | 47.5 | 25.0 | |
| Overweight (25≤BMI < 30) | 802 | 30.6 | (28.4–32.7) | 33.1 | 28.5 | |
| Obese (BMI ≥ 30) | 915 | 31.0 | (28.9–33.1) | 16.3 | 43.3 | |
| Physical activitya | ||||||
| Less than once a week | 516 | 34.8 | (31.6–38.0) | 25.3 | 42.6 | <0.0001 |
| At least once a week | 901 | 65.2 | (62.0–68.4) | 74.7 | 57.4 | |
| Smoking | ||||||
| Never | 2120 | 78.6 | (76.7–80.6) | 59.5 | 94.7 | <0.0001 |
| Former smoker | 220 | 9.2 | (7.8–10.6) | 17.3 | 2.4 | |
| Current smoker | 280 | 12.1 | (10.5–13.7) | 23.2 | 2.9 | |
| Alcohol | ||||||
| Never | 76 | 92.6 | (91.3–93.8) | 85.9 | 98.1 | <0.0001 |
| Less than once a week | 74 | 3.0 | (2.3–3.8) | 5.2 | 1.2 | |
| 2–6 times a week | 2443 | 3.0 | (2.2–3.8) | 5.8 | 0.6 | |
| Daily consumption | 27 | 1.4 | (0.8–2.1) | 3.1 | 0.1 | |
| Socio-demographic characteristics | ||||||
| Reported chronic disease | ||||||
| No | 1798 | 70.8 | (68.7–72.9) | 72.4 | 69.6 | 0.21 |
| Yes | 822 | 29.2 | (27.1–31.3) | 27.6 | 30.4 | |
| Education level | ||||||
| No diploma | 1780 | 64.9 | (62.6–67.2) | 61.3 | 67.9 | 0.01 |
| Less than baccalaureate | 550 | 21.7 | (19.8–23.6) | 22.8 | 20.8 | |
| Baccalaureate or higher | 290 | 13.4 | (11.6–15.1) | 15.8 | 11.3 | |
| Professional activity | ||||||
| Inactive | 1773 | 65.4 | (63.2–67.7) | 55.1 | 74 | <0.0001 |
| Active | 847 | 34.6 | (32.3–36.8) | 44.9 | 26 | |
| Couple | ||||||
| No | 939 | 34.9 | (32.7–37.1) | 30.9 | 38.2 | 0.002 |
| Yes | 1681 | 65.1 | (62.9–67.3) | 69.1 | 61.8 | |
| Place of birtha | ||||||
| Mayotte | 495 | 37.2 | (33.9–40.5) | 37.0 | 37.3 | 0.15 |
| Comoros | 783 | 53.9 | (50.5–57.3) | 53.0 | 54.6 | |
| Another Indian Ocean island | 86 | 4.7 | (3.3–6.1) | 4.1 | 5.2 | |
| Metropolitan France | 25 | 1.6 | (0.9–2.4) | 1.8 | 1.5 | |
| Other area | 28 | 2.6 | (1.4–3.7) | 4.0 | 1.4 | |
| Perception of financial situationa | ||||||
| Struggling | 685 | 44.8 | (41.5–48.2) | 46.8 | 43.2 | 0.30 |
| Average to good | 732 | 55.2 | (51.8–58.5) | 53.2 | 56.8 | |
| Health insurancea | ||||||
| No | 543 | 37.2 | (34.0–40.5) | 36.8 | 37.5 | 0.84 |
| Yes | 874 | 62.8 | (59.5–66.0) | 63.2 | 62.5 | |
Only available for respondents to the long questionnaire (n = 1417).
In the adult population of Mayotte, mean systolic BP and diastolic BP were 126.8 and 81.8 mmHg, respectively. In the Unono Wa Maore survey, 18.4% (16.7–20.1%) of participants reported that a doctor or other health care professional had told them that their BP was too high, more often women than men (21.5% vs. 14.7%, P < 0.0001). At the clinical examination, 30.2% (28.1–40.7%) of adults had very high BP and 23.1% (21.1–25.1%) had high normal BP (table 2).
Table 2.
BP measurement and prevalence, awareness, treatment and control of hypertension, Mayotte, Unono Wa Maore, 2019
| Total |
||||||||
|---|---|---|---|---|---|---|---|---|
| 18–69 years | 18–29 | 30–39 | 40–49 | 50–59 | 60–69 | Men | Women | |
| BP | ||||||||
| SBP, mean (mm Hg) | 126.8 | 118.9 | 123.3 | 132.0 | 139.1 | 149.1 | 130.6 | 123.7 |
| DBP, mean (mm Hg) | 81.8 | 76.5 | 81.4 | 86.5 | 87.6 | 88.1 | 82.0 | 81.8 |
| Arterial pulse pressure (mm Hg) (SBP−DBP) | 45.0 | 42.4 | 42.0 | 45.5 | 51.5 | 61.0 | 48.7 | 41.9 |
| Isolated systolic hypertension (%) (SBP ≥ 140 and DBP < 90) | 6.5 | 3.3 | 4.7 | 3.8 | 13.0 | 32.0 | 8.9 | 4.6 |
| Classification of BP and grade of hypertension, % | ||||||||
| Optimal (≤120/80) | 30.8 | 47.9 | 33.8 | 17.7 | 8.7 | 4.5 | 22.5 | 37.7 |
| Normal (120–129/80–84) | 23.1 | 24.7 | 25.7 | 22.1 | 18.5 | 13.5 | 26.7 | 20.1 |
| High normal (130–139/85–89) | 15.9 | 15.0 | 16.1 | 16.5 | 18.8 | 12.1 | 17.8 | 14.3 |
| Grade 1 hypertension (140–159/90–99) | 21.1 | 10.6 | 18.3 | 29.1 | 35.1 | 40.1 | 23.8 | 18.8 |
| Grade 2 hypertension (160–179/100–109) | 6.6 | 1.7 | 4.4 | 11.3 | 12.6 | 17.5 | 5.9 | 7.1 |
| Grade 3 hypertension (≥180/≥110) | 2.6 | 0.1 | 1.8 | 3.3 | 6.2 | 12.3 | 3.3 | 2..0 |
| BP measurements (SBP ≥ 140 or DBP ≥ 90), % | 30.2 | 12.4 | 24.5 | 43.7 | 54.0 | 70.0 | 33.0 | 27.9 |
| Prevalence, awareness, treatment and control of hypertension, % | ||||||||
| Prevalence of hypertension | 38.4 | 19.2 | 32.3 | 51.6 | 65.1 | 83.2 | 38.5 | 38.3 |
| Proportion of participants aware of their hypertensiona | 47.9 | 45.1 | 42.9 | 42.9 | 58.7 | 56.9 | 38.1 | 56.2 |
| Proportion of hypertensives who practise physical activityb | 48.5 | 25.6 | 34.5 | 55.6 | 71.3 | 46.2 | 60.5 | 41.7 |
| Proportion of hypertensives who are treated pharmacologicallyc | 45.4 | 9.6 | 21.0 | 48.7 | 67.6 | 79.1 | 49.7 | 42.9 |
| Proportion of hypertensives who are controlledd | 30.2 | 42.1 | 52.7 | 29.3 | 25.8 | 27.0 | 29.3 | 30.8 |
DBP = diastolic blood pressure, SBP = systolic blood pressure.
Proportion of people reporting high BP, among all hypertensives.
Proportion of people reporting doing sports to reduce their BP, among aware hypertensives.
Proportion of people reporting taking treatment to reduce their BP, among aware hypertensives.
Proportion of people with BP < 140/90 mmHg at the clinical examination of the survey, among all those reporting treatment to lower their BP.
In 2019, the prevalence of hypertension (reported or measured) was 38.4% (36.1–40.7%) in 18- to 69-year olds. The prevalence of hypertension increased with age, rising from 19.2% in 18- to 29-year old to 83.2% in 60- to 69-year olds (P < 0.0001). The prevalence of hypertension did not differ by sex (38.5% men, 38.3% women, P = 0.95). Grade 3 hypertension affected 2.6% (1.9–3.3%) of the adult population aged 18–69 years but 16.2% of 30- to 39-year olds and 12.4% of 60- to 69-year olds (table 2). In the subgroup of patients aged 30–69 years, the prevalence of hypertension was 48.4% (45.6–51.2%), with no significant between-gender difference (46.9% in men vs. 49.7% in women, P = 0.32).
Taking the definition of hypertension as treated or measured, a third [32.8% (30.6–34.9%)] of the Mayotte population was hypertensive. Among them, the mean age was 44.4 years.
Among hypertensive individuals (reported or measured), 47.9% were aware of their diagnosis of hypertension. This proportion was 56.2% among hypertensive women and 38.1% among hypertensive men. Among the individuals aware of their hypertension, 48.5% reported engaging in physical activity to lower their BP, while 45.4% reported taking antihypertensive pharmacological treatment (28.4% did both) and 34.5% did not do follow either approach. Non-management (pharmacological or physical activity) was more common in women than in men (41.3% vs. 22.6%, P = 0.0003). The control rate (BP < 140/90 mm Hg at the clinical examination of the survey) was 30.2% among pharmacologically treated hypertensives. Overall, only 21.3% of hypertensives had controlled BP. This was more common in young people (35.5%) and women (27.2%) than in older people (15.9%) and men (14.2%) (P < 0.0001) (table 2).
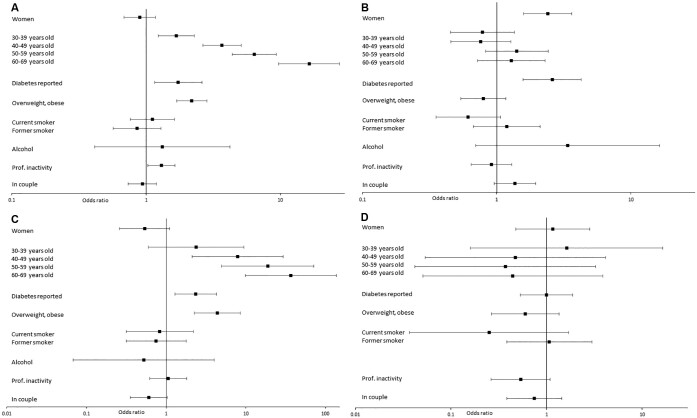
The characteristics of hypertensive individuals are presented in Supplementary table S2. Among hypertensives, 54.4% were women and 40.4% were aged under 40 years, compared with 54.5% women and 75.8% under 40 years in the non-hypertensive population. There were significantly more overweight (31.0% vs. 30.3% P < 0.0001) or obese (43.8% vs. 23.1%, P < 0.0001) individuals among the hypertensives. In the hypertensive population aged under 30 years, 69.0% were overweight or obese compared with 39.0% in the non-hypertensive population of the same age (P < 0.0001) (Supplementary table S1). In the older age group (40–69 years), this difference was less marked, as 75.9% of the non-hypertensive population in this age group was overweight or obese compared with 67.8% of the non-hypertensive population (data not shown). There was no significant difference in alcohol or tobacco consumption between hypertensives and non-hypertensives in this study. Regarding geographical origin, there were significantly fewer people born in metropolitan France among hypertensives compared with non-hypertensives (0.5% vs. 2.4%, P = 0.01). Other geographical origins did not vary with hypertensive status. In terms of socio-economic status, hypertensive patients were more likely to report financial difficulties (49.2% vs. 42.0%, P = 0.04), were less likely to be employed (30.7% vs. 37.0%, P = 0.004) and were less educated (10.3% vs. 15.3%, P = 0.004). Age, self-reported diabetes, overweight and obesity, education level, single status, professional inactivity and financial difficulties were associated with more hypertension. However, after adjustments, hypertension was positively associated only with age [odds ratio (OR)adj 69-60/20-29 =16.4 (9.7–27.7), P < 0.0001], overweight and obesity [ORadj = 2.2 (1.7–2.8), P < 0.0001], self-reported diabetes [ORadj = 1.7 (1.2–2.6), P = 0.008] and professional inactivity [ORadj = 1.3 (1.0–1.6), P = 0.03] (figure 1a).
Figure 1.
Factors associated with hypertension, its awareness, treatment and control, Mayotte, Unono Wa Maore, 2019. (A) Factors associated with hypertension. (B) Factors associated with hypertension awareness (in hypertensives). (C) Factors associated with hypertension treatment (in aware hypertensives). (D) Factors associated with hypertension control (in treated hypertensives)
The distributions of the characteristics of the hypertensive population according to their awareness, treatment and control of the disease are presented in Supplementary tables S2 and S3.
Factors independently associated with being aware of the diagnosis of hypertension were female sex [ORadj = 2.4 (1.6–3.6), P < 0.0001] and self-reported diabetes [ORadj = 2.6 (1.6–4.3), P = 0.0002] (figure 1b). Factors independently associated with the treatment of hypertension were age, self-reported diabetes [ORadj = 2.3 (1.3–4.3), P = 0.006] and BMI [ORadj = 4.4 (2.2–8.6), P < 0.0001) (figure 1c).
The proportion of people covered by health insurance was higher in treated hypertensives (74.5%) than in untreated hypertensives (63.3%), although the difference was not significant (P = 0.10). None of the listed characteristics was associated with hypertension control in our study (figure 1d). Education was associated with BP control before adjusting for other factors (Supplementary table S3).
Discussion
This is the first study since 2008 to investigate the prevalence of hypertension in a representative sample of the population living in Mayotte, with the results showing that the prevalence of hypertension remains high in 2019, including among young people. Some risk factors like obesity were particularly prevalent in the hypertensive population. In addition, the rates of awareness of the diagnosis of hypertension as well as its treatment and control were insufficient, as one in two hypertensive patients did not know about their diagnosis, one in four were not treated and more than one in five were not controlled.
The BP status of the population of Mayotte has not improved in 11 years. In 2008, the MAYDIA study estimated the prevalence of hypertension in the 30- to 69-year-old population at 44%, with a third of 30- to 39-year olds being hypertensive.15 In 2019, the prevalence of hypertension in the sub-population aged 30–69 years was 48%. The evolution of the prevalence of hypertension is particularly worrying among women, as it increased by 12% between 2008 and 2019.
In 2015, the Esteban study estimated the prevalence of hypertension in people aged 18–74 years in metropolitan France at 30.6% based on health insurance reimbursements for antihypertensive drugs and a clinical examination.7 From the data reported in the Esteban survey, we were able to make a new estimate of the prevalence of hypertension in metropolitan France using a similar methodology to our own (hypertension declared in the questionnaire or measured during the clinical examination of the survey), with the estimated prevalence being 33.7% in 18- to 69-year olds. Thus, the difference between Mayotte and metropolitan France was around 5%. Nevertheless, the comparison of these two studies should be taken with caution, as the age structure of the populations included in both studies was very different. The people included in Esteban were 9 years older than in Unono Wa Maore on average, which accentuates the gap between metropolitan France and Mayotte. Among 30- to 39-year olds, a sub-population with a similar average age in the two studies (34.9 years in Esteban vs. 34.4 years in Unono) showed that the prevalence of hypertension was twice as high in Mayotte (32.3%) compared with metropolitan France (16.0%).
Comparisons between territories are difficult because of the different survey methodologies and the small samples on which surveys to estimate the prevalence of hypertension are conducted. Nevertheless, the prevalence of hypertension is very high overall in the Indian Ocean territories: 49% on Reunion Island, another French overseas territory,9 39% on the island of Anjouan,18 and 29% in Madagascar.17 In the other French overseas territories, the prevalence of treated or measured hypertension in people aged 15 years and over ranged from 18% in French Guiana to 29% in Guadeloupe.19 Awareness and treatment rates were similar to those observed in Mayotte. In Mayotte, less than half of hypertensives were aware of their condition and less than half of aware hypertensives were treated. In low-income countries, such as those around in Africa, one-third of the prevalent hypertensive population is aware of their condition.20 Similarly, for treatment, in Madagascar, for example, the rate of treated hypertensives was only 5%.17 However, although it is better than the developing countries, and these indicators were lower than those observed in Reunion, another French island in the Indian Ocean (52% and 46%, respectively),9 and in metropolitan France (55% and 47%)21 or other European or North American countries where they are over 80% aware of the diagnosis and 75% treated.22–24 These rates are still insufficient.
In metropolitan France, as in most high-income countries, the prevalence of hypertension is higher in men than in women, whereas its prevalence is just as high in women and men in low-income countries.6,7 In our study, we found a similar prevalence of hypertension between men and women, whereas in 2008, it was higher in men (50%) than in women (37%). Part of this increase may be attributed to obesity in women.19 This increase in hypertension prevalence could thus be directly linked to the greater corpulence of the Mayotte population. Since 2008, the proportion of obese people increased by 7.7 points in women and 3.3 points in men.18 Obesity is a well-known risk factor for hypertension and is largely described in the literature.17,19 It is therefore urgent to implement measures to make healthy food products available to the whole population and to promote health, healthy diet and physical activity. The problem of obesity appears to be most prevalent among women and young people, so measures should target these populations as a priority. In the coming years, obesity among young people may result in a further increase in the prevalence of hypertension, in addition to the ageing population. This could lead to an increase in the incidence of stroke, heart failure, kidney failure and other cardiovascular complications linked to hypertension in Mayotte.
The proportion of treated people has not increased, remaining at half of those aware of their hypertension. In Mayotte, as in the majority of territories, women are more often aware of their hypertension diagnosis than men.6 This may be linked to the health check-ups carried out during pregnancies, with an average of 5.0 children per woman in Mayotte.25 Nevertheless, with equal awareness of the disease, women are less often treated than men.7 Screening and treatments should be developed for the entire population, in particular screening for men and treatment for women. In metropolitan France, the general practitioner plays a central role in the screening, therapeutic education and initial management of hypertension.26,27 In Mayotte, the medical density is particularly low compared with metropolitan France.28 In addition, poor access to health care can be an obstacle to screening and treatment of hypertension in this island, where almost a third of the population is not covered by health insurance, where access laws are different from those in metropolitan France and where there are many people in an irregular situation. In a 2020 study, 12% of the Mayotte population reported that they refused health care, especially those without health insurance.29 Although our study did not show a significant association between awareness or treatment of the disease on the one hand and social security coverage on the other, the proportion of insured people was higher among aware and treated hypertensives than among those who were not aware or treated. Nevertheless, this information was only available for those who completed the long questionnaire, and the lack of association may be explained by the lack of statistical power.
This low awareness of hypertension and its poor treatment, combined with the silent nature of hypertension, the lack of knowledge of its risk factors may explain why 80% of the hypertensive population was not controlled. Among treated people, the control rate was only 30%. Although some patients may have difficulty in managing their BP, the control rates remain suboptimal. Further, the high rate of grade 3 hypertension, which is a high-risk factor for cardiovascular complications and death, is worrying.30,31 BP control reduces the risk of complications and should be improved to reduce the burden of hypertension. The application of hygienic and dietary rules, effective drug treatment and regular monitoring of patients should also be further encouraged.
Strengths and limitations
The high participation rate in the Unono Wa Maore survey as well as the adjustment and weighting of the data provided reliable indicators that could be extrapolated to the entire population of Mayotte. The high participation rate could be explained by the fact that participants viewed the study as an opportunity to have access to a free health examination at home and with reporting of results, which is usually difficult to obtain in Mayotte. The methodology of the survey using a questionnaire and standardized BP measurements taken by a nurse allowed the prevalence of hypertension to be estimated with the inclusion of a large proportion of undiagnosed or unreported cases of hypertension.
However, there are some limitations: Ramadan, which began in May 2019, did not allow the clinical examination to be completed. A total of 1650 people only had the questionnaire, so this particularity had to be taken into account in the calculation of the weights. This premature stopping of clinical examinations and refusals to participate (in particular for men) may have led to selection bias. However, to take into account this possible source of bias, appropriate weights for each participant were calculated to take into account survey design and non-response at the different stages of the survey (including no clinical examination) and ensure the representativity of the selected sample.
Furthermore, according to the recommendations of the European Society of Hypertension,31 in clinical practice, hypertension should be diagnosed based on elevated BP measurements obtained at three different visits. This survey included only one clinical examination, and therefore the identification of hypertension was based on BP measurements taken during a single examination (involving three BP measurements), as done in the majority of studies. The prevalence of hypertension may therefore be slightly biased by BP variability. Similarly, we cannot exclude stress during the clinical examination (‘white-coat’ effect), especially as the use of primary health care is rare in Mayotte, thus leading to a possible overestimation of the prevalence of hypertension. Similarly, one-third of the individuals had only two BP measurements, which could have slightly increased the average BP. In our data, there was no difference between the average of the last two BP measurements and the first two. Conversely, the single examination may have masked the hypertension of some individuals.32
The wording of the question regarding the declaration of existing hypertension may have overestimated the prevalence if people had experienced an elevated BP measurement at an isolated medical consultation, without confirming the diagnosis based on several measurements or consultations. This formulation is the same as in 2008, which allowed us to observe any changes between the two study years. In addition, sensitivity analysis was performed to estimate the prevalence of treated or measured hypertension, with the results showing the same socio-demographic characteristics in the hypertensive population, except for a lower proportion of young women.
Self-reported alcohol and tobacco use may lead to a classification bias and an underestimation of the prevalence of these factors in the population. However, the use of these substances is lower in this overseas territory compared with mainland France due to cultural factors.
Conclusions
The Unono Wa Maore study has allowed a new estimate of the prevalence of hypertension in Mayotte. In 2019, more than a third of the population of Mayotte was hypertensive (38.4%). The population of Mayotte cumulates several major cardiovascular risk factors with a high prevalence of hypertension, diabetes and obesity even though the age of the population is young. The burden of cardio-neurovascular pathologies is therefore likely to increase in the years to come and should be closely monitored.
The high prevalence of hypertension and the low proportion of awareness, treatment and control of this disease in Mayotte are alarming and underline the need to continue and to develop primary prevention actions and access to healthy food but also to provide hypertension screening and treatment that is adapted to the demographic, social and medical characteristics of this territory.
Supplementary data
Supplementary data are available at EURPUB online.
Supplementary Material
Acknowledgements
We thank the Unono Wa Maore team (Marc Ruello, Marion Fleury, Youssouf Hassani, Jean-Baptiste Richard, Jean-Louis Solet, Laurent Filleul, Delphine Jezewski-Serra, Julie Chesneau) and we thank Victoria Grace for her English editing of the manuscript.
Funding
This study was supported by the French Public Health Agency and French Ministry of Health (no grant number).
Patient and public involvement
This study received a favourable opinion from the ‘Comité de Protection des Personnes Ile-de-France VIII’ on 23 November 2018 and complies with the reference methodology MR001 (agreement of the ‘Commission Nationale Informatique et Libertés’ of 25 September 2018). Each randomly selected person was invited to participate in the study and to give their consent after the presentation of the objectives and participation criteria.
Conflicts of interest: None declared.
Key points.
In 2019, the prevalence of hypertension was 38.4% in the Mayotte adult population.
The prevalence of hypertension is increasing in Mayotte, particularly among women.
Obesity concerns a large part of the adult population of Mayotte.
Awareness, treatment and control remain insufficient.
Contributor Information
Lucinda Calas, Santé Publique France, French Public Health Agency, Saint-Maurice, France.
Marion Subiros, Santé Publique France, French Public Health Agency, Saint-Maurice, France.
Marc Ruello, Santé Publique France, French Public Health Agency, Saint-Maurice, France.
Youssouf Hassani, Santé Publique France, French Public Health Agency, Saint-Maurice, France.
Amélie Gabet, Santé Publique France, French Public Health Agency, Saint-Maurice, France.
Marion Angue, Department of Cardiology, Centre Hospitalier de Mayotte, Mamoudzou, France.
Odile Pointeau, Department of Cardiology, Centre Hospitalier de Mayotte, Mamoudzou, France.
Valérie Olié, Santé Publique France, French Public Health Agency, Saint-Maurice, France.
Clémence Grave, Santé Publique France, French Public Health Agency, Saint-Maurice, France.
References
- 1. Zhou B, Carrillo-Larco RM, DanaeiG, Riley LM, Paciorek CJ, Stevens GA, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. The Lancet 2021;398:957–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yusuf S, Joseph P, Rangarajan S, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet 2020;395:795–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. OD M, Hankey GJ, Rangarajan S, et al. Variations in knowledge, awareness and treatment of hypertension and stroke risk by country income level. Heart 2020. 10.1136/heartjnl-2019-316515. [DOI] [PubMed] [Google Scholar]
- 4. Schutte AE, Srinivasapura Venkateshmurthy N, Mohan S, Prabhakaran D. Hypertension in low- and middle-income countries. Circ Res 2021;128:808–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.NCD Risk Factor Collaboration (NCD-RisC). Long-term and recent trends in hypertension awareness, treatment, and control in 12 high-income countries: an analysis of 123 nationally representative surveys. Lancet 2019;394:639–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation 2016;134:441–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Perrine A-L, et al. L'hypertension artérielle en France: prévalence, traitement et contrôle en 2015 et évolutions depuis 2006. Bull Epidémiol Hebd 2018;2018:170–9. [Google Scholar]
- 8. Inamo J, Daigre JL, Boissin JL, et al. High blood pressure and obesity: disparities among four French Overseas Territories. J Hypertens 2011;29:1494–501. [DOI] [PubMed] [Google Scholar]
- 9. Cournot M, Lenclume V, Moullec NL, et al. Prevalence, treatment and control of hypertension in La Réunion: the RÉDIA population-based cohort study. Blood Press 2017;26:39–47. [DOI] [PubMed] [Google Scholar]
- 10. Genay V, Merceron S. Institut national de la statistique et des études économiques(INSEE). 256 500 habitants à Mayotte en 2017 - Insee Analyses Mayotte - 15, 2017. Available from: https://www.insee.fr/fr/statistiques/3284395.
- 11. Marie C-V, Breton D, Crouzet M, Fabre E, Merceron S. Migrations, natalités et solidarités familiales—La société de Mayotte en pleine mutation. Insee Analyses Mayotte n°12. 2017. Available from: https://www.insee.fr/fr/statistiques/2656589.
- 12. Paillole P. Enquête Emploi Mayotte 2018—Un taux de chômage de 35%. Insee Flash Mayotte, 2019. Available from : https://www.insee.fr/fr/statistiques/3716585.
- 13.Agence de Santé Océan Indien. Les professions de santé à Mayotte et à la Réunion. Dossier Statistiques, 2012. Available from https://www.mayotte.ars.sante.fr/dossier-statistiques-ndeg6-juillet-2012-les-professions-de-sante-mayotte-et-la-reunion-2.
- 14. Ruello M, Richard J. Enquête de santé à Mayotte 2019—Unono Wa Maore. Méthode. Saint-Maurice: Santé Publique France, 2021. [Google Scholar]
- 15. Solet JL, Baroux N, Pochet M, et al. Prevalence of type 2 diabetes and other cardiovascular risk factors in Mayotte in 2008: the MAYDIA study. Diabetes Metab 2011;37:201–7. [DOI] [PubMed] [Google Scholar]
- 16.Santé Publique France. Etude de la prévalence et des caractéristiques du diabète en population générale à Mayotte. Etude Maydia, 2008. Available from https://www.santepubliquefrance.fr/regions/ocean-indien/documents/rapport-synthese/2009/etude-maydia-2008.-etude-de-la-prevalence-et-des-caracteristiques-du-diabete-en-population-generale-a-mayotte.
- 17. Ratovoson R, Rasetarinera OR, Andrianantenaina I, et al. Hypertension, a neglected disease in rural and urban areas in Moramanga, Madagascar. PLoS One 2015;10:e0137408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ali RAB, Hannoun Z, Harraqui K, et al. Profile of diabetes and cardiovascular risk factors in adults Anjouan Island (Comoros). Pan Afr Med J 2019;33:140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Atallah A, Atallah V, Daigre JL, et al. Hypertension artérielle et obésité: disparités entre quatre régions d’Outre-mer. Annal Cardiol Angéiol 2014;63:155–62. [DOI] [PubMed] [Google Scholar]
- 20. Tibazarwa KB, Damasceno AA. Hypertension in developing countries. Can J Cardiol 2014;30:527–33. [DOI] [PubMed] [Google Scholar]
- 21. Vallée A, Gabet A, Grave C, et al. Patterns of hypertension management in France in 2015: the ESTEBAN survey. J Clin Hypertens 2020;22:663–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Neuhauser HK, Adler C, Rosario AS, et al. Hypertension prevalence, awareness, treatment and control in Germany 1998 and 2008-11. J Hum Hypertens 2015;29:247–53. [DOI] [PubMed] [Google Scholar]
- 23. Polonia J, Martins L, Pinto F, Nazare J. Prevalence, awareness, treatment and control of hypertension and salt intake in Portugal: changes over a decade. The PHYSA study. J Hypertens 2014;32:1211–21. [DOI] [PubMed] [Google Scholar]
- 24. DeGuire J, Clarke J, Rouleau K, et al. Blood pressure and hypertension. Health Rep 2019;30:14–21. [PubMed] [Google Scholar]
- 25. Chaussy C, Merceron S, Genay V. A Mayotte, près d'un habitant sur deux est de nationalité étrangère. Insee Première, 2019;1737. Available from https://www.insee.fr/fr/statistiques/3713016.
- 26. Samson S, Ricordeau P, Pépin S, et al. Hypertension artérielle et facteurs de risque associés: évolutions des traitements entre 2000 et 2006. Points Repères 2007;10:1–8. [Google Scholar]
- 27.Haute Autorité de Santé. Prise en charge de l’hypertension artérielle de l’adulte. Saint-Denis La Plaine: HAS, 2016. [Google Scholar]
- 28. Anguis MBM, Pisarik J, Vergier N, Chaput H. Quelle démographie récente et à venir pour les professions médicales et pharmaceutique? Constats et projections démographiques. DRESS, 2021. [Google Scholar]
- 29.INED AM. IN EXTENSP Migrations Famille Vieillissement No 9, October 2020.
- 30. Brown DW, Giles WH, Greenlund KJ. Blood pressure parameters and risk of fatal stroke, NHANES II mortality study. Am J Hypertens 2007;20:338–41. [DOI] [PubMed] [Google Scholar]
- 31. Williams B, Mancia G, Spiering W, et al. ; ESC Scientific Document Group. 2018 ESC/ESH Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur Heart J 2018;39:3021–104. [DOI] [PubMed] [Google Scholar]
- 32. Pioli MR, Ritter AM, de Faria AP, Modolo R. White coat syndrome and its variations: differences and clinical impact. Integr Blood Press Control 2018;11:73–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.