Abstract
Background:
Much remains unknown about the course of grief in the early months following bereavement, including the prevalence and timing of a recovery trajectory, whether specific symptoms mark a failure to recover, and the co-occurrence of chronic prolonged grief (PG), posttraumatic stress (PTS) and depression symptoms.
Methods:
Two hundred fifty-nine participants completed PG, PTS and depression questionnaires up to eleven times every six weeks during the two years post-bereavement. We used Latent Class Growth Mixture Modelling (LCGMM) to identify subgroups of bereaved individuals sharing similar trajectories for each disorder. We used repeated measures ANOVA to evaluate differences in individual symptoms between trajectories. Finally, we investigated to what extent chronic trajectories of these three disorders co-occurred.
Results:
Three trajectories of PG symptoms emerged: resilient (66.4%), chronic (25.1%) and acute recovery (8.4%). The overall severity and symptom profile of the acute recovery group were indistinguishable from that of the chronic group through 6 months post-bereavement, followed by reduction in PG from 6 to 18 months post-bereavement. Chronic PTS in the first-year post-bereavement tended to co-occur with chronic PG and/or chronic depression.
Conclusions:
Twenty five percent of those with initial elevations in grief recovered in the period of 6 to 12 months post-bereavement. These findings highlight the clinical importance of severe grief in the initial months following loss, but also suggests caution in diagnosing a grief disorder within the first-year post-bereavement.
Keywords: Prolonged grief, posttraumatic stress, depression, Latent Class Growth Mixture Modelling, loss, bereavement
Introduction
The course of grief is a subject of long-standing interest to bereaved adults, caretakers, and researchers. In studies examining the course of psychiatric symptoms following the death of loved one, researchers have consistently found that (a) most bereaved adults are resilient, exhibiting persistently low symptom severity over the timeframe assessed and (b) a subset of bereaved adults experience chronic elevation in symptoms that may persist for years following the death (Galatzer-Levy, Huang, & Bonanno, 2018)
Findings regarding other possible trajectories of grief (e.g., recovery or delayed onset) have been less consistent. Among the six grief trajectory studies of which we are aware at the writing of this study, four have found evidence for a recovery trajectory, typically characterized by moderate to high grief observed at a single time point during the first-year post-bereavement followed by a modest decrease in grief severity at subsequent time points in the years that follow (Bonanno & Malgaroli, 2019; Djelantik, Smid, Kleber, & Boelen, 2017a; Nielsen, Carlsen, Neergaard, Bidstrup, & Guldin, 2019; Sveen, Johannesson, Cernvall, & Arnberg, 2018). Only one study has found an acute recovery trajectory in which initially elevated symptoms remit during the first-year post-bereavement (Lundorff, Bonanno, Johannsen, & O’Connor, 2020). In other words, recovery in these studies is typically slow and some elevation in symptom severity typically remains for years following the loss. This is noteworthy given ongoing debates regarding the “time since loss” criterion for prolonged grief disorder (PGD; also known as persistent complex bereavement disorder or complicated grief); a syndrome characterized by elevated grief symptoms that do not remit naturally with time. Criteria for prolonged grief disorder in the DSM-5-TR (American Psychiatric Association, 2020, 2022) indicate that the diagnosis can be made only after 12 months post-loss, thereby implicitly adopting the position that it may take up to one year for natural recovery to occur. In contrast, the International Classification of Diseases 11th Revision (ICD-11; World Health Organization, 2018) and the PGD criteria of Prigerson et al. (2009) permit the diagnosis after six months. Unfortunately, there is little empirical data to clarify what this duration criterion should be. It is, thus, of great clinical importance to determine whether there is a subset of bereaved adults who will naturally recover from elevated grief symptoms during the first-year post-bereavement and, if so, to clarify the timing of symptom reduction in this group.
At least three limitations to the extant literature constrain our ability to draw conclusions about the course of grief following bereavement (Bonanno & Malgaroli, 2019; Djelantik et al., 2017a; Lenferink, Nickerson, de Keijser, Smid, & Boelen, 2018; Lundorff et al., 2020; Nam, 2015; Nielsen et al., 2019; Sveen et al., 2018). First, studies have data at only a small number of timepoints during the first year following bereavement. Indeed, many include only one assessment during the first year of bereavement, thereby precluding any assessment of change in grief within that year. Moreover, most studies examining grief in the first year, lacked an assessment in the first six months of bereavement. Thus, although these studies provide valuable information about the long-term course of grief, they tell us little about grief trajectories during the first year following bereavement.
Second, most studies have focused exclusively on sum scores of post-bereavement psychopathology. However, there is growing evidence that a symptom-level focus may afford richer understanding of psychiatric disorders than focusing on sum scores alone (Fried, 2017; Fried et al., 2015). In the domain of grief, loss characteristics and characteristics of the person exhibit distinct patterns of association with specific grief symptoms (Djelantik, Robinaugh, Kleber, Smid, & Boelen, 2019a; Robinaugh, LeBlanc, Vuletich, & McNally, 2014). For example, violent loss is especially associated with difficulty accepting the death whereas the loss of a spouse or child is especially associated with difficult moving on with life. Moreover, some symptoms may be better indicators of change in the broader syndrome than others. For example, preliminary evidence suggests that a change in ‘feelings of emptiness or loss of meaning’ may be especially strongly associated with changes in other grief symptoms (Robinaugh et al., 2014). In other words, just as looking only at group-level means may mask individual differences in the course of symptoms over time, looking only at sum-scores may mask differences in how distinct symptoms evolve over time.
Third, most studies examining trajectories of psychiatric symptoms have focused on a single disorder, typically either on prolonged grief (PG), posttraumatic stress (PTS), or major depression (MD) (Aneshensel, Botticello, & Yamamoto-Mitani, 2004; Galatzer-Levy & Bonanno, 2012; Maccallum, Galatzer-Levy, & Bonanno, 2015; Zhang, Mitchell, Bambauer, Jones, & Prigerson, 2008). Therefore, it is largely unclear whether those exhibiting chronic trajectories for one disorder would also exhibit a chronic trajectory for another disorder. Only Lenferink et al. (2018) assessed PG, PTS, and depression symptoms in the same sample, showing that most individuals with chronic PG also exhibited chronic depression. In contrast, only half of those with PG also exhibited chronic PTS. However, Lenferink et al. (2018) included only three assessments over the four years post-bereavement with the first assessment not occurring until 11 months post-bereavement and, thus, cannot inform our understanding of how these distinct syndrome trajectories may relate to one another in the first year following bereavement.
In the current study, we aimed to gain a more detailed understanding of the course of psychopathology in the initial months following bereavement. We did so in a sample of bereaved adults who completed a minimum of two and a maximum of 11 assessments during their first-year post-bereavement, with assessments occurring every six weeks, providing more time-points than has been available in prior grief trajectory studies. Because participants could start at any time-point in the first year, we gathered data as late as 27 months post-loss. We had three aims. First, we aimed to examine whether there are subgroups of bereaved individuals who share similar trajectories of PG during the first and second year after bereavement. Second, we compared individual PG symptom scores in those exhibiting distinct trajectories of grief over time, allowing us to explore whether trajectories can be distinguished from one another by specific symptoms in the initial months post-bereavement. Third, we examined to what extent individuals were likely to be a member of chronic trajectories of PG, PTS and depression symptoms simultaneously in the first two years post-bereavement.
Methodology
Participants and Procedures
Participants were recruited through announcements on Dutch websites providing information about grief from November 2016 till February 2019. Only participants older than 17 years were included. The questionnaires were filled in online in a secure software environment accessed by a personalized log-in code. Participants were invited to fill in a variety of questionnaires, including questionnaires assessing socio-demographics, loss-related characteristics, and symptoms of PG, PTS, and depression. Participants who were bereaved less than one year ago were invited to complete follow-up questionnaires every six weeks up to ten times, yielding up to eleven assessments over the course of 15 months. The research program was approved by the local ethical review board and informed consent was obtained from all participants. Of all participants who had lost their loved one less than one year ago (N = 372), 259 participants filled in the questionnaires at least one additional time. These participants constitute the current sample. Because initial assessments were conducted at different points in time during the first 12 months post-loss, the available data encompassed a time range varying from one month to 27 months post-bereavement.
Measurements
Prolonged Grief – 11 scale (PGD scale).
The PGD scale is based on the 19-item Inventory of Complicated Grief (Prigerson et al., 2009). It contains 11 items representing criteria for PGD. Participants rate how often symptoms occurred in the preceding month on 5-point scales (1 = never; 5 = always). The Dutch version has adequate psychometric properties (Boelen, 2017) and includes two additional items “recurrent thoughts” and “emotional pain”. Given our interest in better understanding individual symptoms in this study, we included all 13 items in the analyses. The range of possible scores on this scale is 13 – 73. Cronbach’s alpha for the 13 items at Time 1 (T1) was .91.
PTSD Symptom Scale–Self-Report version (PSS-SR).
The PSS-SR is a 17-item measure of PTSD symptoms, as defined in DSM-IV (American Psychiatric Association, 2000). Respondents are instructed to rate PTSD symptoms, on 4-point scales (1 = not at all; 4 = five or more times per week/almost always). The index event was defined as “the death of your loved one” (e.g., “How often did you have unpleasant dreams or nightmares about the death of your loved one?”). The English and Dutch versions have good psychometric properties (Engelhard, Arntz, & van den Hout, 2007). In the present sample for T1, the Cronbach’s alpha was .89.
Hospital Anxiety and Depression Scale-Depression Scale (HADS-D).
The HADS-D is a 7-item scale measuring depressive symptoms. Respondents are instructed to rate their depression symptoms on a 4-point scale, ranging from 0 to 3, with different anchors. The scale is widely used and has good psychometric properties (Spinhoven et al., 1997). Cronbach’s alpha in this sample at T1 was .92.
Statistical Analysis
Preliminary analyses.
If a questionnaire had less than 20% missing item-level data, missing items were handled by mean imputation. If a questionnaire had more than 20% missing item-level data, the summed score was set as missing. We compared the socio-demographic characteristics of the participants who participated in at least two waves of the study to the participants who dropped out after Wave 1 using Chi Square and T-tests. All preliminary analyses were conducted using R (R Core Team, 2013; Yoshida, Bohn, & Yoshida, 2019).
Aim 1: Trajectory analysis of PG.
Using the summed scores of the PGD scale items, we estimated the trajectories using Mplus 8.2 (Muthén & Muthén, 1998–2017). We choose Latent Growth Mixture Modelling (LGMM) instead of Latent Class Growth Analysis (LCGA) because this technique allows for taking into account the variation of the individual responses among the classes (van de Schoot, 2015). Missing sum scores were handled by Full Information Maximum Likelihood (FIML). Because the time since loss of each participant differed at the first assessment point (T1), we first calculated the time varying scores (T-score) for each time wave. The T-scores contain the number of months since loss for each participant. We began with a 1-class linear model (including slope and intercept parameters) and increased the number of classes until the Bayesian information criterion (BIC) fit index started to increase and/or the sample size within a given class became too small for clear interpretation. After this, we repeated this process for models including slope, intercept and quadratic parameters.
The best-fitting model was selected using Akaike Information Criterion (AIC), Bayesian information criterion (BIC), sample-size adjusted BIC (SS‐BIC), entropy, and sample size of the classes. The Lo–Mendel–Rubin likelihood ratio test, and bootstrap likelihood ratio test were not possible because our model included time-varying t-scores (Muthén & Muthén, 1998–2017). Lower BIC and AIC values and higher entropy values indicate better fit. Furthermore, the parsimony and interpretability of the models were considered (van de Schoot, Sijbrandij, Winter, Depaoli, & Vermunt, 2017). To assess whether we could improve the model convergence, we reran the final models with fixed linear slope variances. Following the selection of the final model, participants were assigned to the most likely class.
Aim 2: Symptom-level analysis of the bereaved individuals in the classes.
To evaluate symptom-level differences between trajectories over time, we first averaged symptom scores within each trajectory. Because of the low sample size for some trajectories at some time points, we aimed for more stable estimates by averaging over multiple assessments (i.e., six periods of three months). We did not assess beyond 18 months because it was beyond the timeframe of most interest and low sample sizes prevented stable assessment of means in some trajectories.
We then conducted a one-way ANOVA to examine differences among the found classes identified in Aim 1. Finally, we conducted t-tests and estimated the effect sizes for symptom level comparisons between the different classes. These analyses were conducted using R.
Aim 3: Co-occurrence of trajectories of PG, PTS and depression symptoms.
We repeated the trajectories analyses for PTS and depression following the same procedure used to examine PG trajectories (see Aim 1). We then examined the co-occurrence of PG, PTS, and depression trajectories.
Results
Preliminary Analyses
Table 1 shows characteristics of participants who were (n = 259) vs. were not (n = 113) included in the final analysis and differences between groups. Participants included were older M(SD) = 55.9 (13.9) than the excluded participants (M (SD) = 50.76 (15.01), p = .00). Furthermore, the included participants were more likely to have lost a partner or a child, n = 151 (58.3%), compared to the excluded participants, n = 44 (39.9%, p = .00). There were no differences in terms of the time since loss, gender, education, having experienced a violent cause and the sum-score of PG, PTS and depression. In the final sample, the mean time since loss at T1 was 4.6 months (SD = 4.8). Most participants were women, n = 198 (76.4%) and had received a higher education (n = 143, 55.2%); 29 participants had lost their loved one due to a violent cause (11.2%) (Table 1).
Table 1.
Socio-demographic differences between excluded and included patients
| Excluded patients (N = 113) | Included patients (N = 259) | ||
|---|---|---|---|
| Age, M (SD) | 50.76 (15.01) | 55.85 (13.90) | .002** |
| Time since loss, M (SD) | 4.92 (3.44) | 4.61 (2.77) | .37 |
| Gender, N (%) | |||
| Males | 20 (17.7) | 61 (23.6) | |
| Females | 93 (82.3) | 198 (76.4) | .26 |
| Education, N (%) | |||
| Lower education | 46 (40.7) | 116 (44.8) | |
| Higher education | 67 (59.3) | 143 (55.2) | .58 |
| Cause of death, N (%) | |||
| Violent | 9 (8.0) | 29 (11.2) | .45 |
| Natural | 102 (82) | 151 (88.8) | |
| Kinship, N (%) | |||
| Partner/child | 44 (38.9) | 151 (58.3) | |
| Other | 69 (61.1) | 108 (41.7) | .001*** |
| PG sum score T1, M (SD) | 34.43 (12.28) | 35.35 (11.09) | .48 |
| PTSD sum score T1, M (SD) | 31.57 (11.00) | 32.60 (9.42) | .36 |
| MDD sum score T1, M (SD) | 12.89 (5.58) | 13.88 (5.19) | .10 |
Note. M = mean, N = number of patients. SD = Standard Deviation. MD = major depression. PG = Prolonged grief. PTS = posttraumatic stress
p < .05.
p < .01.
p < .001.
Excluded patients are bereaved patients who completed questionnaires at only one timepoint. Included patients are bereaved patients who completed questionnaires at least at two time points.
Aim 1: Trajectory Analysis of PG
Fit-indices for all model solutions appear in Table 2. In the 5-class solution of the linear models and the 2-class solution of the quadratic models, a very low sample size was found for one class (n = 1). Accordingly, we did not examine additional class solutions beyond these models. The 3-class solution exhibit the best fit and was the most interpretable, and, thus, was chosen as the final model. Fixed slope variances did not improve the model fit. The 3-class linear model solution consisted of (a) a chronic trajectory characterized by persistent high and slightly increasing PG (25.1% [n = 65], intercept = 40.88, slope = 0.054), (b) what we will refer to as an acute recovery trajectory of individuals with decreasing PG (8.4% [n = 22], intercept = 42.65, slope = −1.68) and, (c) a resilient trajectory characterized by low and slightly decreasing PG (66.4% [n = 172], intercept = 30.29, slope = −0.50) (Figure 1).
Table 2.
Goodness-of-fit statistics for prolonged grief model solutions
| Classes | Log likelihood | AIC | BIC | SS-BIC | Entropy | Smallest sample size (n) |
|---|---|---|---|---|---|---|
| Lineair model | ||||||
| 1 class | −6131.558 | 12295.116 | 12352.025 | 12301.299 | ||
| 2 class | −6120.552 | 12279.103 | 12346.683 | 12286.446 | 0.662 | 67 |
| 3 class | −6111.708 | 12267.416 | 12345.666 | 12275.918 | 0.696 | 22 |
| 4 class | −6104.785 | 12259.570 | 12348.490 | 12269.231 | 0.685 | 22 |
| 5 class | −6102.970 | 12261.940 | 12361.531 | 12272.761 | 0.731 | 1 |
| Quadratic model | ||||||
| 1 class | −6118.680 | 12277.360 | 12348.497 | 12285.089 | ||
| 2 class | −6104.508 | 12257.016 | 12342.380 | 12266.291 | 1 | 1 |
Note. BIC = Bayesian Information Criterion, SS-BIC = Sample-Size Adjusted BIC, AIC = Akaike Information Criterion.
Figure 1. Trajectories of prolonged grief in the first 27 months following bereavement.
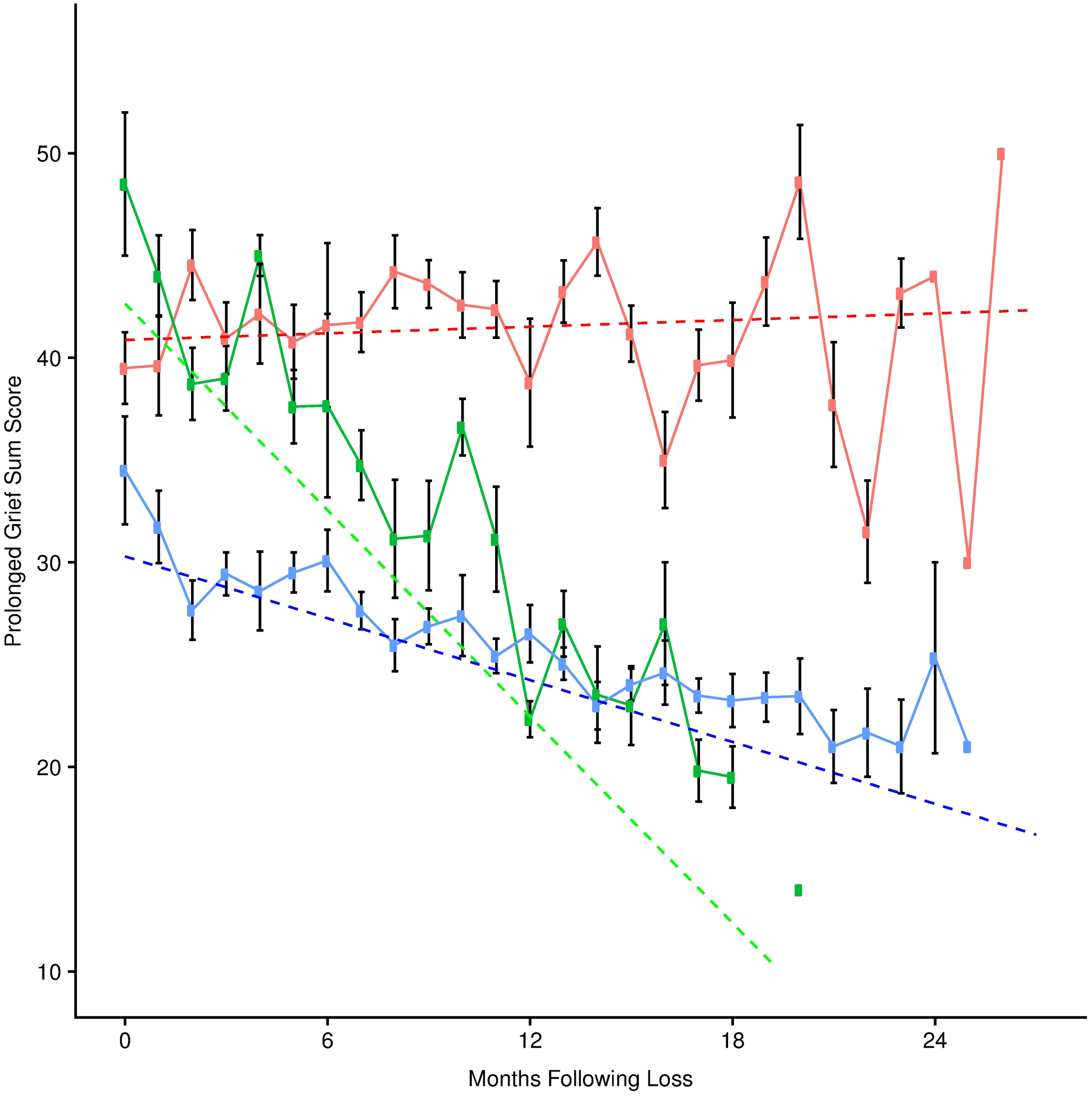
The red, green, and black lines denote the chronic, recover, and resilient trajectories respectively. The continuous lines are the observed scores for each trajectory and the dotted lines denote the estimated trajectories. From 18 months following loss, the observed scores are less stable due to low sample size.
Aim 2: PG Symptom-level Analysis in those with Distinct Grief Trajectories.
Symptom profiles for each of the three grief trajectories every three months from Month 1–3 to Month 16–18 are depicted in Figure 2. The ANOVAs and the effect sizes comparing the severity of each symptom between trajectories at each of these time points appear in Supplementary Materials A. Several findings from this analysis are worth highlighting. First, trajectories were better distinguished by some symptoms than others. For example, a feeling that ‘life is empty/ meaningless’, ‘difficulties moving on in life’, and ‘subjective impairment’ each exhibited consistently strong effect sizes in the comparison between resilient and chronic trajectories, whereas ‘avoidance’ and ‘difficulty trusting others’ consistently differentiated worse between the trajectories. In fact, ‘avoidance’ did not differ between the resilient and chronic trajectories until 7–9 months post-bereavement. Second, the distinction between the chronic and resilient trajectories became increasingly stark over time, with the effect sizes for every symptom-level comparison rising over time. Third, we found little evidence that participants in the recovery group exhibited a distinct symptom profile from participants in the chronic group in the early months following bereavement. During the first nine months post-bereavement, only one symptom (i.e., ‘subjective impairment’) at one time point (Month 4–6) was significantly lower in the recovery group than the chronic group. However, no such difference was observed at either Month 1–3 or 7–9, suggesting this may have been a spurious finding. It was not until 10–12 months post-bereavement that any symptom began to consistently distinguish the recovered and resilient trajectories. At that point, several symptoms distinguished these groups, including ‘recurrent thoughts’, ‘emotional pain’, ‘yearning’, ‘difficulty accepting the loss’, ‘emptiness’, ‘shock’, and ‘subjective impairment’).
Figure 2. The development of the mean severity of grief symptoms for each class.
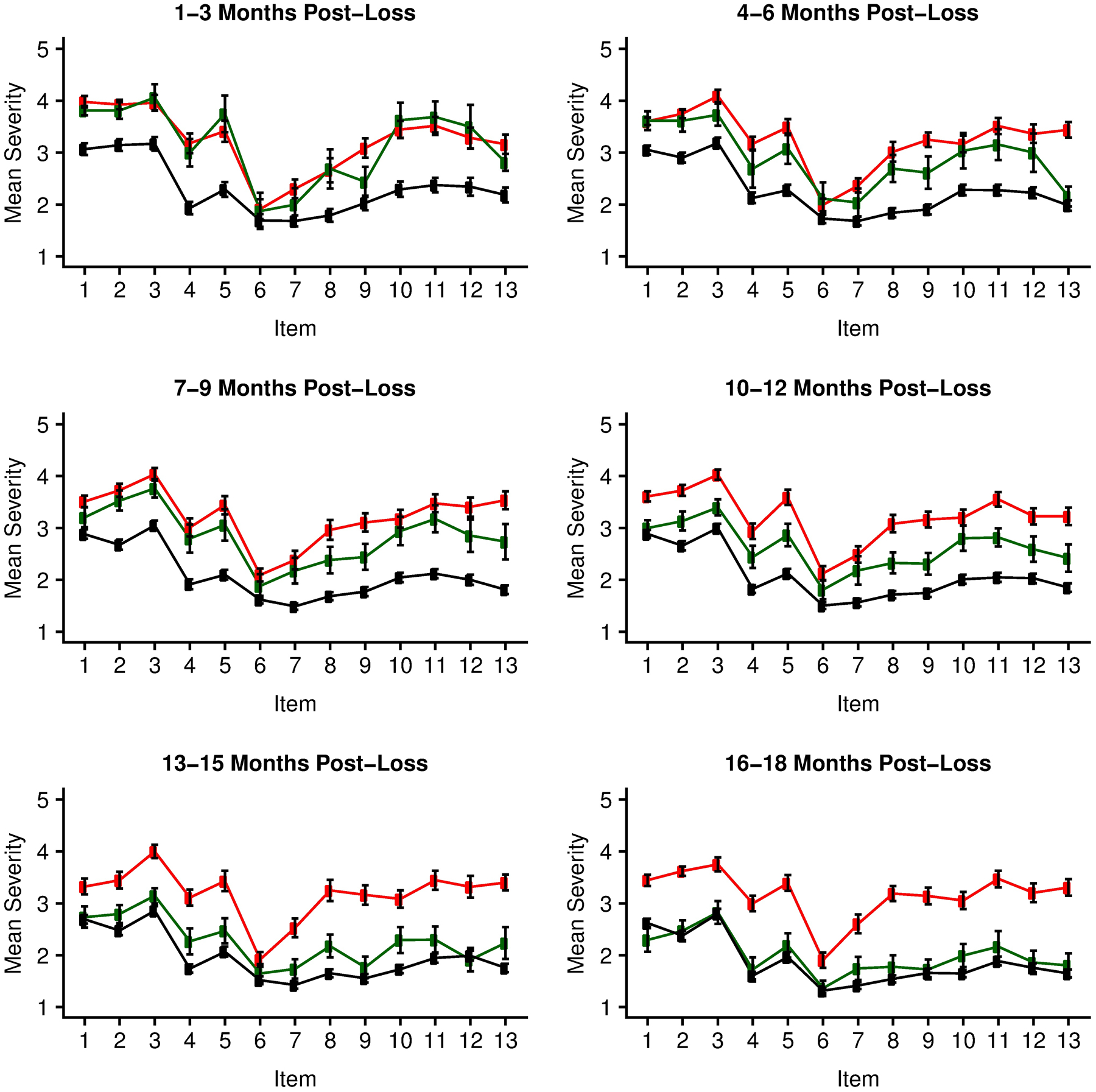
The red, green, and black lines denote the chronic, recover, and resilient trajectories respectively. Items reflect the following symptoms: (1) recurrent thoughts, (2) emotional pain, (3) yearning, (4) confusion about one’s role in life (5) difficulties accepting the loss (6) avoidance of reminders (7) difficulties trusting others, item (8) bitterness/ anger (9) difficulty moving on with life, item (10) feeling numb (11) life is empty/ meaningless (12) feeling stunned, shocked (13) subjective impairment.
Aim 3: Co-occurrence of the Chronic Trajectories of PG, PTS, depression.
The optimal model solution for PTS was a 2-class linear model, which included a chronic trajectory class with persistent high symptoms (5% (n = 13), intercept = 44.463 p < .01, slope 0.232, p = .60) and a resilient class with moderate and decreasing symptoms (95% (n = 246), intercept 31.053, slope - 0.323, ps < .01; see Supplementary Materials B and C). The optimal model solution for depression was a 2-class linear model, which included a chronic trajectory class with high and slightly decreasing symptoms (32% (n = 82), intercept 10.800, slope −0.095, ps < .01) and a resilient trajectory class with low and slightly decreasing symptoms (68% (n = 177), intercept 4.948, slope 0.023, ps < .01; see Supplementary Materials D and E). Fixed slope variances did not increase model fit.
As seen in Figure 3, Chronic trajectories of PG, PTS and depression commonly co-occurred. Among those with chronic PG symptoms, 68% exhibited chronic depression symptoms and 15% exhibited both chronic depression and PTS. Yet, this overlap was far from complete. Among those with chronic PG, 31% exhibited neither chronic PTS or depression. Similarly, 45% of those with chronic depression exhibited depression symptoms alone. In contrast, the majority of those in the chronic PTS group exhibited both chronic PG and depression (77%) and only 8% exhibited PTS alone.
Figure 3. Venn diagram depicting the co-occurrence of chronic trajectories.
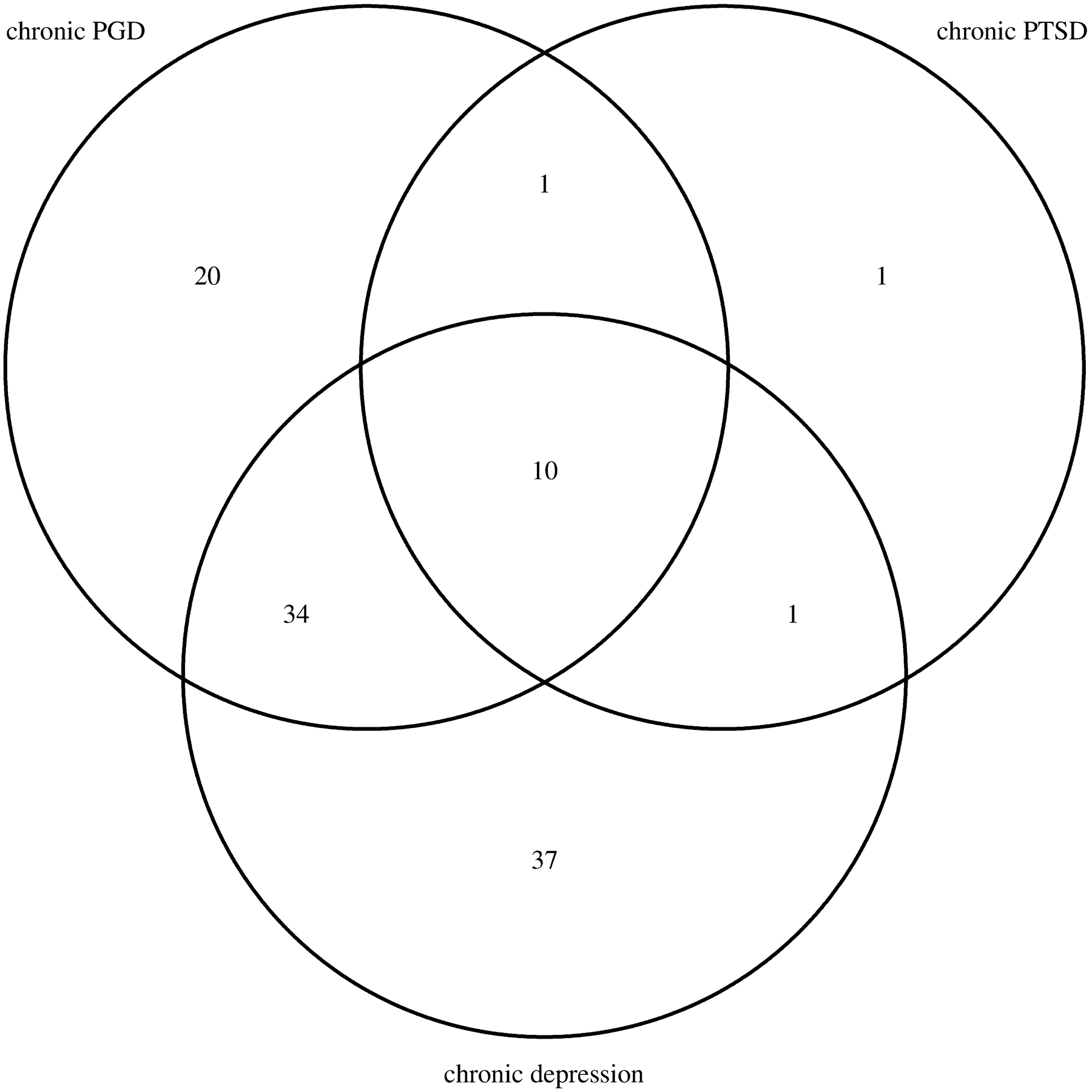
Chronic PGD: individuals who are member of the chronic prolonged grief class. Chronic PTSD: individuals who are member of the chronic posttraumatic stress class. Chronic depression: individuals who are member of the chronic major depression class. Total N = 259.
Discussion
In this study, we examined the course of PG, PTS and depression in the first two years following the loss of a loved one while addressing three gaps in prior research on trajectories of grief: (a) the lack of multiple assessment points during the first year post-bereavement, (b) the exclusive focus on sum-scores rather than individual symptoms, and (c) the tendency for studies to focus on trajectories of only one disorder, thereby limiting our understanding of the overlap in these trajectories of response.
For our first aim, we examined trajectories of PG. Consistent with prior research, we found that a majority of bereaved individuals exhibited a resilient trajectory (66.4%) and a significant minority (25.1%) exhibited a chronic trajectory of elevated grief. However, we also found that 8.4% exhibited a recovery trajectory characterized by significant reductions in grief symptoms during the eighteen months post-bereavement. Although some previous studies have identified a recovery trajectory (Bonanno & Malgaroli, 2019; Lundorff et al., 2020; Nielsen et al., 2019; Sveen et al., 2018), our findings differ from prior results in at least three ways. First, in most previous studies recovery occurred over a longer time course than was observed in this study, with symptoms declining over years rather than months. In the current study, the gains made by those in the recovery trajectory occurred largely between 6- and 18-months post-bereavement.
Second, in previous studies, those in the recovery trajectory exhibited initial symptom severity that was lower than that of the chronic trajectory. In contrast, the recovery trajectory and chronic trajectories in our study were highly similar during the initial months post-bereavement, both in overall grief severity and in symptom profile.
Third, in previous studies, those in the recovery trajectory continue to exhibit symptom severity that is higher than the resilient trajectory through the final assessment point. In contrast, the recovered trajectory identified here exhibited roughly the same severity of grief as the resilient group by 12 months post-bereavement. In conjunction with prior research and the findings from this study, we believe there may be at least two types of recovery trajectories for bereaved adults: one subgroup with elevated grief in the first months after the loss that recover during the first year (i.e., an “acute recovery” trajectory) and another group with persistent moderate-to-high grief that gradually reduces over multiple years (i.e., a “gradual recovery” trajectory).
This study has important, but nuanced implications for the duration criterion for PGD. Our findings seem to argue in favor of the 12-month duration criterion. We found that a subgroup of participants exhibited substantial reduction in symptoms during the first-year post-bereavement. This trajectory was nearly indistinguishable from those with chronic grief through the first 6 months post-bereavement, both in regards to overall grief severity and in regards to symptom profiles. Yet, by 12 months post-bereavement, the recovery group exhibited significantly lower overall severity and by 15–18 months, those in this recovery trajectory exhibited roughly the same symptom profile as those in the resilient trajectory. Although these findings seem to support the value of withholding a diagnosis until 12 months post-bereavement, there are two important qualifications. First, treatment engagement for participants is unknown and, thus, we cannot conclude with certainty that this acute recovery trajectory occurs in the absence of treatment. Second, it is important to note that this acute recovery trajectory was relatively small, comprising only 8% of the overall sample and only 25% of those with initially elevated symptoms. In other words, 75% of those with elevated symptoms at six months post-bereavement continued to experience persistent elevations in grief through at least 18 months post-loss. Clinically, these findings suggest that, at a minimum, some level of clinical monitoring may be warranted for those whose grief is persistently elevated at six months post-bereavement.
Notably, the intercept of our resilient trajectory is 30.29. This is consistent with a mean agreement of 2 or 3 on each item, indicating existing grief symptoms that are relatively low in frequency and severity. Given that grief is a natural response to the death of a loved one, we would expect most bereaved individuals to experience some grief symptoms in the initial weeks following a loss and these findings appear to reflect that, with even the “resilient” trajectory exhibiting some elevation in symptoms in the initial weeks post-loss.
For our second aim, we found that symptoms varied in the extent to which they differed between groups. For example, a feeling that ‘life is empty or meaningless’, ‘difficulties moving on in life’, and ‘a subjective feeling of being impaired by grief’ best differentiated the chronic and resilient trajectories, especially at 6 – 12 months post-bereavement. Conversely, ‘difficulty trusting others’ and ‘grief-related avoidance’ were consistently the most similar across groups. The findings regarding avoidance are especially noteworthy, as bereavement theories have posited that avoidance plays an important role in the persistence of grief over time (Boelen, Van Den Hout, & Van Den Bout, 2006; Maccallum & Bryant, 2018). Given these theories, we might expect that the chronic group would be strongly characterized by excessive avoidance. However, among all symptoms examined, the chronic and resilient trajectories were least distinguished by avoidance. Indeed, during the early months post-bereavement, there was not a statistically significant difference in avoidance between these groups. This finding accords with other recent studies that have used network analysis to examine the conditional dependence relationships among PG symptoms (Djelantik, Robinaugh, Kleber, Smid, & Boelen, 2019b; Maccallum, Malgaroli, & Bonanno, 2017; Malgaroli, Maccallum, & Bonanno, 2018; Robinaugh, Millner, & McNally, 2016). These studies consistently find avoidance to be among the symptoms with the lowest concurrent associations with other aspects of grief and, in one of these studies, changes in avoidance were not significantly associated with changes in the remainder of the syndrome over time. In future empirical research and theory development, it will be important to grapple with these findings and consider why a behavior posited to play a critical role in prolonging grief would not differ substantially between those with a chronic vs resilient trajectory. For instance, it could be that individuals experiencing avoidance may not be aware of it and, hence, will not answer on self-reported questionnaires that they are avoiding. It is also possible that the item used in our study overemphasizes avoidance of stimuli connected with the deceased (which is less characteristic of prolonged grief) and underemphasizes avoidance of stimuli associated with the irreversibility of the loss (which is strongly characteristic of disturbed grief).
The symptom profiles of the chronic and recovery groups were highly similar through six months post-bereavement, suggesting that these groups cannot be readily distinguished by their early symptom profile. The symptoms ‘difficulty moving on in life’ and ‘subjective impairment’ consistently exhibited the largest effect sizes in symptom-level comparisons between these trajectories during the initial months post-bereavement, providing some modest evidence that they may be worth investigating further as potential early indicators of a more chronic course of grief. However, in the current study, differences between trajectories in these symptoms were not consistently statistically significant. Moreover, effect size estimates were somewhat unstable over time, likely due to the small number of individuals exhibiting the recovery trajectory. Clinically, this precludes firm conclusions about the value of specific symptoms as early indicators that distinguish chronic and resilient trajectories.
With regard to our third aim, we found that, among the members of the PG chronic trajectory, 30.8% were not included in the PTS and/or depression chronic classes. This accords with previous work done by Simon et al. 2012 in a sample of individuals receiving treatment for PGD, where 32 % of individuals with a PGD diagnosis did not have co-morbidity with PTSD or depression, further suggesting that PGD overlaps with, but is distinguishable from, PTSD and MD. In contrast, almost all members of the chronic PTS class were also members of the chronic PG or MD classes, suggesting that PTS symptoms are more likely to be experienced alongside PG symptoms in bereaved adults, rather than as a stand-alone condition. This is in accordance with a prior cross-sectional study in which a resilient group, a PG group and a combined PG/PTS group were identified among Dutch bereaved individuals (Djelantik, Smid, Kleber, & Boelen, 2017b). Clinically, this provides further evidence that clinicians should be aware of PG symptoms in bereaved individuals with PTSD.
Our findings regarding the overlap in trajectories differ from those of Lenferink et al. (2018), who found a much larger percentage of bereaved individuals in the chronic depression class who were member of the chronic PG class (i.e., 85.7% vs. 42.3% in the current study) and a much smaller percentage of bereaved individuals in the chronic PTS class who were member of the chronic PG class (i.e., 64.7% vs. 91.7% in the current study). The studies differed in the nature of the death (i.e., participants in the Lenferink et al. 2018 study lost loved ones in an airplane crash, whereas in our study most people suffered natural losses) and the timeframe (i.e., 1–4 years instead of 0–24 months) which may account for differences between these studies. More longitudinal studies including PG, PTS, and depression in the same sample are necessary to clarify the co-occurrence of PG, PTS, and depression symptoms further.
Limitations
There are several limitations to our study. First, our sample was a convenience sample including a large number of older women. This means that the sample is not representative for all bereaved individuals and that generalization of our findings needs to be done with caution. For example, we found that avoidance was among the symptoms that least distinguished the distinct trajectories following grief. Convenience sampling may have contributed to this finding by leading to the selection of individuals comparatively low on avoidance, regardless of their other symptoms. Second, we had a relatively low number of participants in the recovery group, which may have impaired our ability to detect differences in symptom scores between the recovery and chronic trajectories. Lastly, participants were able to enter the study at different time points post loss. This means that we had most information in the time frame between 6- and 18-months post-loss. The findings found outside this time frame (e.g., before 6-months and after 18-months) are likely to be less robust than the findings from within this timeframe. In addition, it should be noted that we used the Prigerson et al. criteria for PG symptoms (Prigerson et al., 1999), which diverge slightly from the recent DSM-5-TR and ICD-11 PGD criteria. Future studies, examining DSM-5-TR and ICD-11 PGD criteria are needed to examine if the current findings generalize to these symptom criteria.
Conclusions
In this study, we explored trajectories of PG symptoms, evolving symptom profiles for each PG trajectory, and the co-occurrence of chronic PG, PTS, and depression trajectories in individuals in the first two years post-bereavement. Our results provide further evidence that while the majority of the bereaved individuals experience persistent low grief, a significant minority experiences chronic elevation in grief reactions. We add to those robust findings evidence for an acute recovery trajectory, characterized by recovery during the first year following bereavement. In terms of both symptom profile and overall severity, the recovery group strongly resembled the chronic group through six months post-bereavement and, by 12–15 months post-bereavement, closely resembled the resilient trajectory. These findings suggest that a time-criterion of 6 months for a grief disorder might be too soon and it is better to wait to 12 months to diagnose and treat PGD. However, some level of clinical monitoring may be warranted for those whose grief is elevated at six months post-bereavement, because they are at a higher risk for persistent problems. We found little evidence that certain specific symptoms were characteristic of the recovered trajectory during the first six months post-bereavement. This may mean that early grief screeners should rather focus on the severity of grief in general instead of focusing on specific grief symptoms. PTS chronic trajectories in the first-year post-bereavement tend to co-occur with chronic PG and/or depression trajectories, but not the other way around. This means that clinicians should be extra aware of PG symptoms in bereaved individuals with PTSD in the first year.
Supplementary Material
FINANCIAL SUPPORT
This research did not receive any direct specific grant from funding agencies in the public, commercial, or not-for-profit sectors. DJR’s work on this study was supported by a National Institute of Mental Health Career Development Award (1K23MH113805).
Footnotes
CONFLICT OF INTEREST
None.
References
- American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders (4th ed., rev text. ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- American Psychiatric Association. (2020). Board approves new prolonged grief disorder for DSM. Retrieved from 10.1176/appi.pn.2020.11a12 [DOI]
- American Psychiatric Association. (2022). Diagnostic and Statistical Manual of Mental Disorders (5th ed., rev text. ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Aneshensel CS, Botticello AL, & Yamamoto-Mitani N (2004). When caregiving ends: The course of depressive symptoms after bereavement. Journal of health and social behavior, 45(4), 422–440. [DOI] [PubMed] [Google Scholar]
- Boelen PA (2017). “It feels as if she might return one day”: A sense of unrealness as a predictor of bereavement-related emotional distress/“Tengo la sensación de que ella puede volver algún día”: la sensación de irrealidad como un predictor del sufrimiento emocional relacionado con la pérdida. Estudios de Psicología, 38(3), 734–751. [Google Scholar]
- Boelen PA, Van Den Hout MA, & Van Den Bout J (2006). A cognitive‐behavioral conceptualization of complicated grief. Clinical Psychology: Science and Practice, 13(2), 109–128. doi: 10.1111/j.1468-2850.2006.00013.x [DOI] [Google Scholar]
- Bonanno GA, & Malgaroli M (2019). Trajectories of grief: Comparing symptoms from the DSM‐5 and ICD‐11 diagnoses. Depression and Anxiety. doi: 10.1002/da.22902 [DOI] [PubMed] [Google Scholar]
- Djelantik AAAMJ, Robinaugh DJ, Kleber RJ, Smid GE, & Boelen PA (2019a). Symptomatology following loss and trauma: Latent class and network analyses of prolonged grief disorder, posttraumatic stress disorder, and depression in a treatment-seeking trauma-exposed sample. Depress Anxiety. doi: 10.1002/da.22880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djelantik AAAMJ, Robinaugh DJ, Kleber RJ, Smid GE, & Boelen PA (2019b). Symptomatology following loss and trauma: Latent class and network analyses of prolonged grief disorder, posttraumatic stress disorder, and depression in a treatment‐seeking trauma‐exposed sample. Depression and Anxiety. doi: 10.1002/da.22880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djelantik AAAMJ, Smid GE, Kleber RJ, & Boelen PA (2017a). Early indicators of problematic grief trajectories following bereavement. European Journal of Psychotraumatology, 8(sup6), 1423825. doi: 10.1080/20008198.2018.1423825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djelantik AAAMJ, Smid GE, Kleber RJ, & Boelen PA (2017b). Symptoms of prolonged grief, post-traumatic stress, and depression after loss in a Dutch community sample: A latent class analysis. Psychiatry research, 247, 276–281. doi: 10.1016/j.psychres.2016.11.023 [DOI] [PubMed] [Google Scholar]
- Engelhard IM, Arntz A, & van den Hout MA (2007). Low specificity of symptoms on the post-traumatic stress disorder (PTSD) symptom scale: a comparison of individuals with PTSD, individuals with other anxiety disorders and individuals without psychopathology. British Journal of Clinical Psychology, 46(Pt 4), 449–456. doi: [DOI] [PubMed] [Google Scholar]
- Fried EI (2017). The 52 symptoms of major depression: Lack of content overlap among seven common depression scales. Journal of Affective Disorders, 208, 191–197. doi: 10.1016/j.jad.2016.10.019 [DOI] [PubMed] [Google Scholar]
- Fried EI, Boschloo L, van Borkulo CD, Schoevers RA, Romeijn J, Wichers M, … Borsboom D (2015). Commentary: “Consistent superiority of selective serotonin reuptake inhibitors over placebo in reducing depressed mood in patients with major depression”. Frontiers in Psychiatry, 6, 117. doi: 10.3389/fpsyt.2015.00117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galatzer-Levy IR, & Bonanno GA (2012). Beyond normality in the study of bereavement: heterogeneity in depression outcomes following loss in older adults. Social Science & Medicine, 74(12), 1987–1994. doi: 10.1016/j.socscimed.2012.02.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galatzer-Levy IR, Huang SH, & Bonanno GA (2018). Trajectories of resilience and dysfunction following potential trauma: A review and statistical evaluation. Clinical Psychology Review, 63, 41–55. [DOI] [PubMed] [Google Scholar]
- Lenferink LIM, Nickerson A, de Keijser J, Smid GE, & Boelen PA (2018). Trajectories of grief, depression, and posttraumatic stress in disaster‐bereaved people. Depression and Anxiety. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundorff M, Bonanno GA, Johannsen M, & O’Connor M (2020). Are there gender differences in prolonged grief trajectories? A registry-sampled cohort study. Journal of Psychiatric Research, 129, 168–175. [DOI] [PubMed] [Google Scholar]
- Maccallum F, & Bryant RA (2018). Prolonged grief and attachment security: A latent class analysis. Psychiatry Research, 268, 297–302. [DOI] [PubMed] [Google Scholar]
- Maccallum F, Galatzer-Levy IR, & Bonanno GA (2015). Trajectories of depression following spousal and child bereavement: A comparison of the heterogeneity in outcomes. Journal of Psychiatric Research, 69, 72–79. doi: 10.1016/j.jpsychires.2015.07.017 [DOI] [PubMed] [Google Scholar]
- Maccallum F, Malgaroli M, & Bonanno GA (2017). Networks of loss: Relationships among symptoms of prolonged grief following spousal and parental loss. Journal of Abnormal Psychology, 126(5), 652–662 doi: 10.1037/abn0000287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malgaroli M, Maccallum F, & Bonanno GA (2018). Symptoms of persistent complex bereavement disorder, depression, and PTSD in a conjugally bereaved sample: A network analysis. Psychological medicine, 1–10. doi: 10.1017/S0033291718001769 [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998–2017). Mplus User`s Guide. (6th ed.). Los Angeles, CA: Mutheén & Mutheén. [Google Scholar]
- Nam I (2015). Trajectories of complicated grief. The European Journal of Psychiatry, 29(3), 173–182. [Google Scholar]
- Nielsen MK, Carlsen AH, Neergaard MA, Bidstrup PE, & Guldin M-B (2019). Looking beyond the mean in grief trajectories: A prospective, population-based cohort study. Social Science & Medicine, 232, 460–469. [DOI] [PubMed] [Google Scholar]
- Prigerson HG, Horowitz MJ, Jacobs SC, Parkes CM, Aslan M, Goodkin K, … Maciejewski PK (2009). Prolonged grief disorder: Psychometric validation of criteria proposed for DSM-V and ICD-11. PLOS Medicine, 6(8), e1000121. doi: 10.1371/journal.pmed.1000121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prigerson HG, Shear MK, Jacobs SC, Reynolds CF 3rd, Maciejewski PK, Davidson JR, … Zisook S (1999). Consensus criteria for traumatic grief. A preliminary empirical test. The British Journal of Psychiatry, 174, 67–73. doi: 10.1192/bjp.174.1.67 [DOI] [PubMed] [Google Scholar]
- R Core Team. (2013). R: A language and environment for statistical computing.
- Robinaugh DJ, LeBlanc NJ, Vuletich HA, & McNally RJ (2014). Network analysis of persistent complex bereavement disorder in conjugally bereaved adults. Journal of Abnormal Psychology, 123(3), 510–522. doi: 10.1037/abn0000002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinaugh DJ, Millner AJ, & McNally RJ (2016). Identifying highly influential nodes in the complicated grief network. Journal of Abnormal Psychology, 125(6), 747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinhoven PH, Ormel J, Sloekers PPA, Kempen GIJM, Speckens AEM, & Van Hemert AM (1997). A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychological Medicine, 27(2), 363–370. [DOI] [PubMed] [Google Scholar]
- Sveen J, Johannesson KB, Cernvall M, & Arnberg FK (2018). Trajectories of prolonged grief one to six years after a natural disaster. PloS One, 13(12), e0209757. doi: 10.1371/journal.pone.0209757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Schoot R (2015). Latent trajectory studies: the basics, how to interpret the results, and what to report. European Journal of Psychotraumatology, 6, 27514. doi: 10.3402/ejpt.v6.27514 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Schoot R, Sijbrandij M, Winter SD, Depaoli S, & Vermunt JK (2017). The GRoLTS-checklist: guidelines for reporting on latent trajectory studies. Structural Equation Modeling: A Multidisciplinary Journal, 24(3), 451–467. [Google Scholar]
- Yoshida K, Bohn J, & Yoshida MK (2019). Package ‘tableone’. R Foundation for Statistical Computing, Vienna, Austria (30 November 2016). [Google Scholar]
- Zhang B, Mitchell SL, Bambauer KZ, Jones R, & Prigerson HG (2008). Depressive symptom trajectories and associated risks among bereaved Alzheimer disease caregivers. The American Journal of Geriatric Psychiatry, 16(2), 145–155. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


