Abstract
Purpose:
Unexplained clinical conditions share common features such as pain, fatigue, disability out of proportion to physical examination findings, inconsistent laboratory abnormalities, and an association with stress and psychosocial factors. We examined the extent of the overlap among urological and nonurological unexplained clinical conditions characterized by pain. We describe the limitations of previous research and suggest several possible explanatory models.
Materials and Methods:
Using hallmark symptoms and syndromes as search terms a search of 12 databases identified a total of 1,037 full-length published articles in 8 languages from 1966 to April 2008. The search focused on the overlap of chronic pelvic pain, interstitial cystitis, painful bladder syndrome, chronic prostatitis/chronic pelvic pain syndrome or vulvodynia with fibromyalgia, chronic fatigue syndrome, temporomandibular joint and muscle disorders or irritable bowel syndrome. We abstracted information on authorship, type of case and control groups, eligibility criteria, case definitions, study methods and major findings.
Results:
The literature suggests considerable comorbidity between urological and nonurological unexplained clinical conditions. The most robust evidence for overlap was for irritable bowel syndrome and urological unexplained syndromes with some estimates of up to 79% comorbidity between chronic pelvic pain and symptoms of irritable bowel syndrome. However, most studies were limited by methodological problems, such as varying case definitions and selection of controls.
Conclusions:
The overlap between urological and selected nonurological unexplained clinical conditions is substantial. Future research should focus on using standardized definitions, and rigorously designed, well controlled studies to further assess comorbidity, clarify the magnitude of the association and examine common pathophysiological mechanisms.
Keywords: urogenital system, fatigue syndrome, chronic, fibromyalgia, irritable bowel syndrome, temporomandibular joint disorders
Functional somatic syndromes, medically unexplained symptoms, somato-form disorders and unexplained clinical conditions are common names given to conditions characterized by a lack of clear physical or biological etiology, or an inconsistent demonstration of laboratory abnormalities.1 These conditions are further characterized by symptoms such as pain, fatigue, sleep disturbances and disability. The literature suggests that many of these conditions also share demographic characteristics, clinical courses and psychosocial profiles.1 The diagnosis given to a patient with 1 of these conditions often depends on the hallmark symptom and the expertise of the treating clinician rather than on the illness.1 The frequency of co-diagnosis and the common features shared by unexplained clinical conditions have become topics of growing interest in the last few years.
Physicians are challenged to diagnose and appropriately treat patients with unexplained clinical conditions such as FM, CFS, TMD, IBS, CPP, IC, PBS, CP/CPPS and vulvodynia. A recent review found that patients with IC often have other unexplained conditions and symptoms.2 Although a substantial body of literature describes the comorbidity of nonurological, unexplained clinical conditions such as FM, CFS and IBS,3 the extent of the overlap between urological and nonurological unexplained clinical conditions, and the potential mechanisms of their co-occurrence remain largely unknown.
The recent emphasis by NIDDK on a multidisciplinary approach to the study of urological CPPSs further underscores the need to examine and understand the overlap between urological and nonurological unexplained clinical conditions (http://www2.niddk.nih.gov/Research/ScientificAreas/Urology/MAPP). Thus, we reviewed the literature on comorbidity between the most common urological pelvic pain syndromes, ie CPP, IC, PBS, CP/CPPS and vulvodynia, and the nonurological conditions of FM, CFS, TMD and IBS. We focused on overlap with these nonurological conditions for several reasons. 1) Our goal was to examine overlap among conditions with a significant pain component, which ruled out overlap with psychiatric conditions such as panic disorder that also have been shown to co-occur with urological pelvic pain syndromes. 2) Frequently comorbid pain conditions with a known physical or biological etiology were not included since they would not satisfy the definition of an unexplained clinical condition. 3) These 4 nonurological conditions were the focus of most data based articles in the existing literature and of particular interest to NIDDK. 4) These nonurological conditions differed in the pain site, which could influence the extent of overlap between urological and nonurological unexplained clinical conditions.
MATERIALS AND METHODS
Search Strategy
Articles were identified by a database search, including PubMed® (1966 to April 2008), CINAHL® (1981 to April 2008), The Cochrane Collaboration (Cochrane Reviews) (1993 to April 2008), Current Contents Connect® (2000 to April 2008), EBSCO Academic Search Premier (1975 to April 2008), EMBASE® (1974 to April 2008), ISI Web of Science® (1980 to April 2008), PsycINFO® (1967 to April 2008), Science Citation Indexes (1996 to April 2008), and Scirus®, Scopus® and Google™ Scholar (April 2008).
Our initial search included certain search terms for the 5 urological unexplained clinical conditions, including chronic pelvic pain, interstitial cystitis, painful bladder syndrome, chronic prostatitis and vulvodynia, combined with 4 nonurological unexplained clinical conditions, that is chronic fatigue syndrome, fibromyalgia, temporomandibular disorder and irritable bowel syndrome. MeSH® terms were combined with truncated key words describing the symptoms of the various conditions. All possible combinations of the 2 search term sets were examined.
We then looked for all search terms individually and combined with the words overlapping, overlap, comorbidity and comorbid. Also, we combined the terms for the hallmark symptoms associated with each nonurological condition with the hallmark symptoms associated with each urological condition, eg chronic fatigue and painful bladder. The bibliography of relevant articles was examined to identify reports that may have been missed. Finally, members of the NIDDK Working Group on Urological CPP, a group of experts in urology, rheumatology, epidemiology and internal medicine, were contacted to review the list of relevant articles and locate other pertinent peer reviewed publications. Together these search strategies yielded 1,037 unique publications.
Study Inclusion Criteria
Articles included in this review examined the comorbidity or overlap of at least 1 urological condition or hallmark symptom with at least 1 nonurological condition or hallmark symptom. We focused on articles in English, Hebrew, German, French, Spanish, Korean, Japanese and Russian because we or working group members could review them. No limits were placed on participant age but all relevant articles pertained to adults, of whom most were women.
We reviewed comparison and single condition studies. The first type compared 2 or more groups diagnosed with different unexplained clinical conditions, eg patients with IC vs patients with FM, to each other or compared 1 group diagnosed with a urological unexplained clinical condition to a healthy control group, eg patients with CP vs healthy volunteers. In single condition studies participants with a specific unexplained clinical condition or symptom were examined for the co-occurrence of other conditions, eg the frequency of vulvar pain in IBS cases or of IBS in vulvodynia cases. Comparison studies can more precisely estimate the extent of comorbidity or overlap than single condition studies and highlight potential similarities in pathophysiology across conditions.
Studies that were initially excluded because they did not meet the overlap criterion were reviewed again for possible incidental findings on the overlap of urological and nonurological conditions that may have been reported as part of the data analysis or in the context of other study findings.
Study Exclusion Criteria
Of identified articles 90% were excluded from analysis because they did not examine the overlap between urological and nonurological conditions. Other articles were excluded because the main patient group did not have an unexplained clinical condition (eg migraine or panic), the article focused on an unexplained clinical condition or symptom not considered in our review or presented data on broad symptom categories, including conditions other than those considered (eg functional digestive disorders), despite mentioning overlap the article lacked relevant data or the main topic was not pertinent to our review (eg abuse or pharmacological treatment approaches). Articles that did not present primary data, such as reviews, were not included in our analysis or tables even when they supported our findings and conclusions.
Data Extraction and Synthesis
Based on study inclusion and exclusion criteria 41 relevant publications were identified and reported (tables 1 and 2).1 For each study we extracted information on study characteristics (eg name of first author and publication year), participant group type (eg patients or community participants), group sample size, diagnostic criteria, methods and major findings. Initial review findings were examined by a second reviewer who independently extracted information from the relevant publications. Working group members reviewed drafts of the findings for completeness of the literature review and contributed to the synthesis and interpretation of the findings.
Table 1.
Symptoms and syndrome overlap among urological and nonurological unexplained clinical conditions in studies comparing at least 2 groups
| References | Groups (No. pts) | Diagnostic Criteria | Study Methods | Major Findings |
|---|---|---|---|---|
| Waylonis and Heck4 | FM (554), controls (169) | Physician diagnosis | Medical history questionnaire | Pelvic pain in 68.4% of males with FM vs 0% of male controls + in 65.8% of females with FM vs 33.3% of female controls |
| Koziol21 | IC (565), healthy controls (171), pts without IC | Physician diagnosis | Medical history questionnaire | IBS in 22.5% of pts with IC vs 6.7% of controls (p <0.0001) |
| Walker et al25 | IBS (60), IBD (26) | Physician diagnosis, symptom based | Structured psychiatric interview, structured interview, medical + psychiatric history questionnaire | CPP in 35% of pts with IBS vs 13.8% of those with IBD (p <0.05) |
| Clauw et al5 | FM (60), IC (30), controls (30) | American College of Rheumatology, National Institutes of Health IC criteria | Questionnaire on current + lifetime history of symptoms + syndromes, tender point examination | Of pts 12% with IC met FM criteria, 23% with FM vs 2% of controls had bladder fullness symptoms, 23% with FM vs 4% of controls had urinary urgency symptoms + 27% with FM vs 2% of controls had pelvic pain |
| Ostensen + Schei6 | Musculoskeletal disorders (1,988), controls (2,046) | Symptom based | Health problem questionnaire, self-reported history of health problems + behaviors, health screening | Of women consulting for FM symptoms 4% had gynecological symptoms including CPP |
| Aaron et al20 | Twins with chronic fatigue or CFS (127), control twins (127) | Symptom based | Questionnaires on demographics, habits, lifestyle, physical conditions + checklist of medical disorders, fatigue classified according to 3 levels of stringency | Twins with fatigue at the 3 levels were 2–20 times more likely to have IC + 3.5–6 times more likely to have CPP than co-twins without fatigue |
| Erickson et al7 | IC (35), controls (35) | Physician diagnosis, NIDDK criteria | University of Wisconsin questionnaire | Pts with IC had higher scores than controls for other pelvic discomfort, backache, dizziness, chest pain, aches in joints, abdominal cramps + headache (p <0.01) |
| Zimmerman26 | IBS (53), IBD (55), controls (56) | Clinical criteria, Rome I IBS criteria | Standardized questionnaire | Pts with IBS had higher urinary symptom scores than those with IBD (p <0.02) + controls (p <0.001) |
| Novi et al23 | IC (46), controls (46) | ICD-9 | Standardized IC symptom questionnaire, Rome II standardized IBS questionnaire | Women with IC 11 times more likely to be diagnosed with IBS than controls (95% CI 2.7–52, p <0.001) |
| Arnold et al8 | Vulvodynia (208), controls (77) | Physician diagnosis | Questionnaire on health history, use of health system, quality of life + vulvodynia | Pts with vulvodynia 3.84 times more likely to report FM (95% CI 1.54–9.55) and 3.11 times more likely to report IBS (95% CI 1.60–6.05) than controls |
| Clemens et al22 | CP/CPPS (174), IC (111, men excluded) | ICD-9 | Questionnaires on medical history, lifestyle + reproductive history in females | IBS in 22.4% of pts with CP/CPPS + 40% of those with IC |
| Grace + Zondervan24 | CPPS (286), dysmenorrhoea (286), dyspareunia (110), healthy controls (397) | Symptom based, Rome II criteria | Postal questionnaire on women’s health and functioning | Of women with CPP symptoms 37.3% met IBS criteria |
| Kato et al9 | Twins with CWP (1,776), control twins (41,562) | Symptom based, ACR criteria for CWP | Symptom questionnaire, standardized questionnaires, structured psychiatric interview | Urinary tract problems in 23.4% of twins with CWP vs 10.7% of control twins |
| Kennedy et al10 | PBS symptoms (190) bladder pain (55), gynecology pts without bladder symptoms (400) | Symptom based, Rome II criteria | Standardized questionnaires, medical history questionnaires | Of pts with vs without bladder pain 48% vs 14% had IBS (p <0.01) + 27% vs 7% had generalized pain (p <0.01) |
| Pontari11 | CP/CPPS (463), control (121) | Symptom based | Medical history + sexual practice epidemiological questionnaires | IBS history in 12.8% of pts with CP/CPPS symptoms vs 2.5% of controls, musculoskeletal, rheumatological or connective tissue disease history in 21.2% vs 10.8% + CFS history in 2.2% vs 0.8% |
| Shaver et al12 | FM (442), control (205) | Physician diagnosis | Medical diagnosis + lifestyle behavior telephone survey, standardized questionnaires | Bladder infection in 68.4% of pts with FM vs 47.2% of controls |
| Wu et al13 | IC (992), control (9, 920) | Physician diagnosis | Database analysis | IC diagnosis probability in women vs men within 3 yrs after initial FM diagnosis 0.59% vs 0.08% if 1 IC episode + 0.77% vs 0.09% if multiple episodes, + within 3 yrs after initial IBS diagnosis 0.83% vs 0.08% if 1 IC episode + 1.14% vs 0.09% if multiple episodes |
| Wu et al14 | IC (749), control (1,498) | Physician diagnosis | Database analysis | IBS in 7.21% of pts with IC vs 1.47% of controls + FM in 8.68% vs 3.34% |
| Arnold et al15 | Vulvodynia (100), control (325) | Symptom based | Medical + pain history, + health care use telephone survey | Women with vulvodynia symptoms vs controls were 2.78 times more likely to report CFS (95% CI 1.33–6.19), 2.15 times more likely to report FM (95% CI 1.06–4.36) + 1.86 times more likely to have IBS (95% CI 1.07–3.23) |
| Berger et al16 | CP/CPPS (62), control (98) | Physician diagnosis | Standardized questionnaires, manual tender point examination | Of pts with CP/CPPS 16.7% vs 11.8% of controls had high manual tender point examination scores (OR 2.64, 95% CI 0.93–7.51, p = 0.069) |
| Kennedy et al28 | Primary vulvar disease (324), gynecology control (321) | Physician diagnosis, 1999 Rome II IBS criteria | Standardized questionnaires | Pts with dysplasia, vestibulitis, lichen sclerosus, lichen planus + lichen simplex were 3–26.7 times more likely to have IBS than controls |
| Whitehead et al27 | IBS (3,153), IBD (571), control (3,153) | Physician diagnosis | ICD-9 code computer search | Pts with IBS vs controls were more likely to be diagnosed with cystitis (OR 3.6, 95% CI 1.94–6.69), pelvic pain (OR 2.76, 95% CI 2.13–3.58) + prostatitis (OR 2.65, 95% CI 1.70–4.10) |
| Araújo et al17 | Lower urinary tract symptoms with (51) + without (50) FM | Physician diagnosis, symptom based | Urinary symptom + health function questionnaire, gynecologic examination, urodynamics, filling cystometry | Urge urinary incontinence in 64% vs 90.2% of pts with vs without FM (p = 0.004), increased urinary frequency in 8% vs 31.4% (p = 0.007) + detrusor overactivity in 28% vs 60.8% (p = 0.002) |
| Clemens et al18 | IC/PBS (239), control (717) | Physician diagnosis | ICD-9 code computer search | Gastritis or duodenitis in 1.7% of pts with IC/PBS vs 0.7% of controls (OR 12.2, p = 0.004) + myalgia or myositis in 16.3% vs 6.1% (OR 3.0, p <0.00001) |
| Dimitrakov et al19 | CP/CPPS (27), control (29) | NIDDK criteria | Standardized questionnaire, blood + urine tests | Av 2.4 comorbid disorders in pts with CP/CPPS (CFS, FM or arthritis in 7 + IBS in 6) |
Table 2.
Symptom and syndrome overlap among urological and nonurological unexplained clinical conditions in studies of 1 group
| References | Groups (No.) | Diagnostic Criteria | Study Methods | Major Findings |
|---|---|---|---|---|
| Maxton et al36 | • IBS (100) | Physician diagnosis, symptom based | Interview assessing symptoms, standardized questionnaire | Urinary problems in 56% of pts |
| Walker et al38 | • CPP (137) | Symptom based | Physician diagnosis, standardized questionnaires | IBS symptoms in 79% of pts |
| Alagiri et al30 | IC (2,682) | Symptom based, patient registry | Symptoms + syndrome medical history questionnaire | IBS diagnosis in 30.2% of pts, IBS symptoms in 37.7%, FM diagnosis in 17.2%, FM symptoms in 28.6%, CFS diagnosis in 8.7% + CFS symptoms in 13.8% |
| Korszun et al33 | • CFS +/or FM (92, TMD in 42%) | 1990 American College of Rheumatology FM criteria, 1988 Centers for Disease Control + Prevention CFS criteria | Prior psychosomatic illness, facial pain + TMD questionnaire | IC history in 19% of pts with CFS +/or FM + 13% with TMD |
| Giamberardino34 | • IC (2,405) | NIDDK, 1999 Rome II IBS criteria | Standardized questionnaires | IBS criteria met in 75% of pts |
| Nimnuan et al29 | Gastroenterology, gynecology, neurology, rheumatology, respiratory medicine, cardiology + dentistry clinics (550) | Symptom based | Various syndrome questionnaire, severity, sleep + psychological complaint measures | Of pts with CPP symptoms, 19% had IBS symptoms, 19% had FM symptoms + 8% had CFS symptoms |
| Zondervan KT: Am J Obstet Gynecol 2001; 184: 114 | Oxfordshire Health Authority Register randomly selected women (3,916) | Symptom based | Women health issue questionnaire | IBS and CPP in 114 women |
| Gordon et al31 | Internet savvy women on vulvar pain discussion lists (428) | Symptom based | Web based survey | IBS in 34.6%, FM in 20.6%, TMD in 18.5% + chronic fatigue in 11.2% of women |
| Blanchard et al37 | IBS (196) | 1999 Rome II IBS criteria, physician diagnosis | Standardized questionnaires | Urinary track disorders in 26% of 50 pts with IBS |
| Bernatsky S: Swiss med wkly 2005; 135: 76 | FM (180) | 1990 American College of Rheumatology FM criteria, physician diagnosis | Clinical + psychosocial variable, health care use + standardized questionnaires | IBS in 36.1%, CFS in 2.2% + irritable bladder in 1% of pts |
| Williams et al39 | CPP (987) | 1988 Rome I IBS criteria | Standardized questionnaires | IBS criteria met in 35% of pts |
| Yamada et al32 | IC (30) | NIDDK, 1990 American College of Rheumatology FM criteria, physician diagnosis | Standardized questionnaires | FM diagnostic criteria met in 11% of pts |
| FitzGerald et al35 | Pain associated with urinary symptoms (589) | Symptom based | Questionnaires | IBS in 30%, CFS in 18% + FM in 9% of pts |
| Hughes L: Orthopaed Nurs 2006; 25: 112 | FM (107) | 1990 American College of Rheumatology FM criteria | Standardized questionnaires, physical measures | Fatigue, pelvic pain + physical trauma explained 23% of sensory pain score variance, + activity level, depression + pelvic pain explained 23% of affective pain score variance |
| Temml C: Eur Urol 2007; 51: 803 | IC symptoms (981) | Symptom based | Standardized questionnaires | Women with bowel disorders at 4.5-fold increased risk for moderate or severe IC symptoms (95% CI 1.3–15.1, p = 0.016) |
| Fenton et al40 | CPP (175) | Physician diagnosis, 1999 Rome II IBS criteria | Questionnaires, physician examination | IC in 35%, IBS in 24% + myalgia in 45% of pts |
RESULTS
Symptom and Syndrome Overlap in Comparison Studies
We found 25 publications on comparison studies that provided data on the comorbidity of urological and nonurological unexplained clinical conditions or symptoms (table 1). Although some studies were published in the early 1990s, 68% were published since 2005. Of these 25 studies 19 described patient populations and 6 described nonclinical samples derived from population surveys. The studies used diverse diagnostic approaches, including physician diagnosis, symptom based definitions and more rigorous, well established criteria, such as NIDDK criteria for IC diagnosis or American College of Rheumatology criteria for fibromyalgia. Study methods included self-report questionnaires on medical history, standardized surveys and interviews, physician and tender point examinations, and computerized reviews of ICD-9 codes.
A total of 16 groups reported data on the overlap between urological unexplained clinical conditions and musculoskeletal conditions, or symptoms such as FM or chronic widespread pain, joint pain, generalized pain or myalgia.4–19 However, only 4 studies were specifically designed to examine the comorbidity of FM or chronic widespread pain with 1 of the urological conditions.5,8,14,15 About 9% to 12% of patients with IC also experienced FM,5,14 and 23% to 27% of patients with FM had symptoms consistent with IC.5 An early study showed that 68% of men and 66% of women with FM also reported pelvic pain symptoms.4 In a twin study that controlled for genetic and environmental confounding approximately 23% of twins with chronic widespread pain and 11% of their pain-free co-twins reported urinary tract problems.9 Although to our knowledge the overlap between CP/CPPS and FM has not been directly examined, 1 group noted that 21% of individuals with CP/CPPS symptoms reported a history of musculoskeletal, rheumatological or connective tissue diseases11 and another observed a trend toward higher manual tender point examination scores in patients with CP/CPPS vs controls.16 Vulvodynia was also described as co-occurring with FM.8,15
Only 3 studies, all in nonclinical populations, examined the overlap between urological unexplained clinical conditions and CFS. A study of twin pairs discordant for various definitions of chronic fatigue or CFS showed that fatigued twins were up to 20 times more likely to have IC and up to 6 times more likely to have CPP than their nonfatigued co-twins.20 Conversely CFS was reported more than twice as often by individuals with CP/CPPS symptoms than by asymptomatic age matched controls.11 Also, individuals with vulvodynia more often reported CFS than asymptomatic controls.15 We did not find comparative studies of overlap between TMD and any urological unexplained clinical condition.
Finally, 15 of 25 comparison studies examined the overlap between urological unexplained clinical conditions and IBS. Using different methods several groups reported that 7% to 48% of patients with IC or symptoms of PBS also had IBS.10,14,21,22 Others found that patients with IC were 11 times more likely to be diagnosed with IBS than controls.23 Furthermore, 22% of men with CP/CPPS or its symptoms had IBS11,19,22 and 37% of women with CPP met IBS criteria.24 Conversely 1 group found that 35% of patients with IBS but only 14% with inflammatory bowel disease reported CPP symptoms.25 In other studies IBS was associated with an increased probability of an IC diagnosis and increased urinary symptom scores.13,26,27 Vulvodynia was also documented as comorbid with IBS.8,15,28
Symptom and Syndrome Overlap in Single Condition Studies
We found 16 publications that assessed individuals with a single unexplained clinical condition for at least 1 additional syndrome or hallmark symptom (table 2). Despite methodological differences the results of these investigations are generally consistent with those listed in table 1. A study of patients with CPP symptoms showed that 19% also had FM symptoms and 8% had CFS symptoms.29 These rates are similar to those in other publications of self-reported FM (17%) and CFS (9%) in individuals with IC30 and vulvar pain.31 Conversely a recent study using American College of Rheumatology criteria for FM showed that 11% of patients with IC met FM diagnostic criteria.32 Also, 2 studies provided data on the overlap between TMD and at least 1 urological unexplained clinical condition. One group found that 13% of patients with TMD had a history of IC33 and the other reported that almost 20% of women with vulvar pain reported TMD.31
Most single condition studies examined the comorbidity of urological unexplained clinical conditions and symptoms with IBS. They indicated that 30% to 75% of individuals with IC or IC symptoms had IBS or IBS symptoms,30,34,35 and 26% to 56% of patients with IBS reported urinary problems.36,37 Likewise 19% to 79% of patients with CPP had IBS or IBS symptoms.29,38–40 Of women with vulvar pain 35% reported IBS.31
DISCUSSION
Evidence of Overlap
Our extensive review of the literature on urological and nonurological unexplained clinical conditions identified a small but growing body of published reports on the comorbidity of these conditions. The most robust evidence for overlap exists for IBS and unexplained urological conditions in terms of the number of publications and the relative consistency of results across studies. This overlap may reflect publication bias or the anatomical fact that urological CPP conditions and IBS develop in a similar region of the body and involve visceral pain sensations. In contrast, the few studies of FM, CFS and TMD suggest more modest comorbidity with urological unexplained clinical conditions. Nonetheless, our findings generally support previous assertions of overlap among some or all of the urological and nonurological unexplained clinical conditions.2,3,41
The common sociodemographic and clinical features shared by these conditions, the symptom overlap in many case definitions and the tendency to respond to the same therapies have led several investigators to suggest that all unexplained clinical conditions are different manifestations of the same underlying pathophysiological process.1,3 Also, some experts argue that the comorbidity of FM, CFS, TMD and IBS could result from similarities in their case definitions.1 Although this explanation may apply to the overlap between urological pelvic pain conditions and IBS,41 urinary and pelvic pain symptoms are not part of the symptom criteria for FM, CFS or TMD. Thus, commonalities in symptom criteria cannot completely account for the overlap that we summarize. Nonetheless, the heterogeneity of these conditions, especially subgroups of patients with uncharacteristic symptoms, can in part account for the substantial overlap between these conditions.
Proposed Explanations
Despite decades of research on unexplained clinical conditions their etiology and pathophysiology remain elusive. We identified 3 dominant perspectives on the mechanisms of these conditions, including 1) physiological processes, particularly neuroendocrine, immunological and neurotransmitter dysfunction in the central nervous system, 2) victimization, abuse and trauma, and 3) psychological distress, psychiatric disorders, stress tolerance and recovery from stress.3 Although abnormalities have been demonstrated across several domains that are consistent with all of these perspectives, most groups have examined only single hypotheses. Also, many affected patients do not have neuroendocrine abnormalities, or depression or other psychiatric conditions and were not abused or victimized. Organ based approaches, ie examining the bladder, prostate or skeletal system, have similarly failed to provide useful insights into the etiology of or effective treatments for these conditions. Generally research on urological CPP conditions and similar disorders has not distinguished epiphenomena from underlying pathophysiology.
A multidimensional conceptual model seems better suited to guide research and understanding of these conditions and their co-occurrence.1 A multidimensional model can encompass the range of predisposing (eg genetic and environmental influences, and physiological perturbations), precipitating (eg trauma and infection) and perpetuating (eg central sensitization and perceptual amplification) factors as well as predictors of chronicity (eg psychological and sleep disturbances) that are necessary but not individually sufficient for 1 or more unexplained clinical conditions to develop (see figure). A strength of this conceptualization is that it incorporates the 2 most prominent overarching theories of pain to facilitate the understanding and treatment of unexplained clinical conditions. The diathesis-stress model considers predisposing biological and genetic factors as well as the environmental and life events that interact to trigger behaviors and disorders.42 Alternately the gate control theory of pain and its more recent expansion emphasize the role of the brain and its interaction with cognitive and emotional factors in pain transmission and modulation.43 The multidimensional model presented combines these overarching theories to offer multiple hypotheses that test similarities in vulnerability factors and stressors as well as the central affective, sensory, cognitive, motor, inhibitory and autonomic responses involved in pain processing. Elements of this model have spurred a small but growing body of literature, especially in pain sensitivity, and its enhanced perception and central sensitization of pain in FM and CFS cases,44,45 and support basic similarities across these conditions. A more broadly based conceptual model can facilitate interdisciplinary linkages among basic, clinical and population sciences to investigate etiology, clinical manifestations, comorbidity and prognosis.
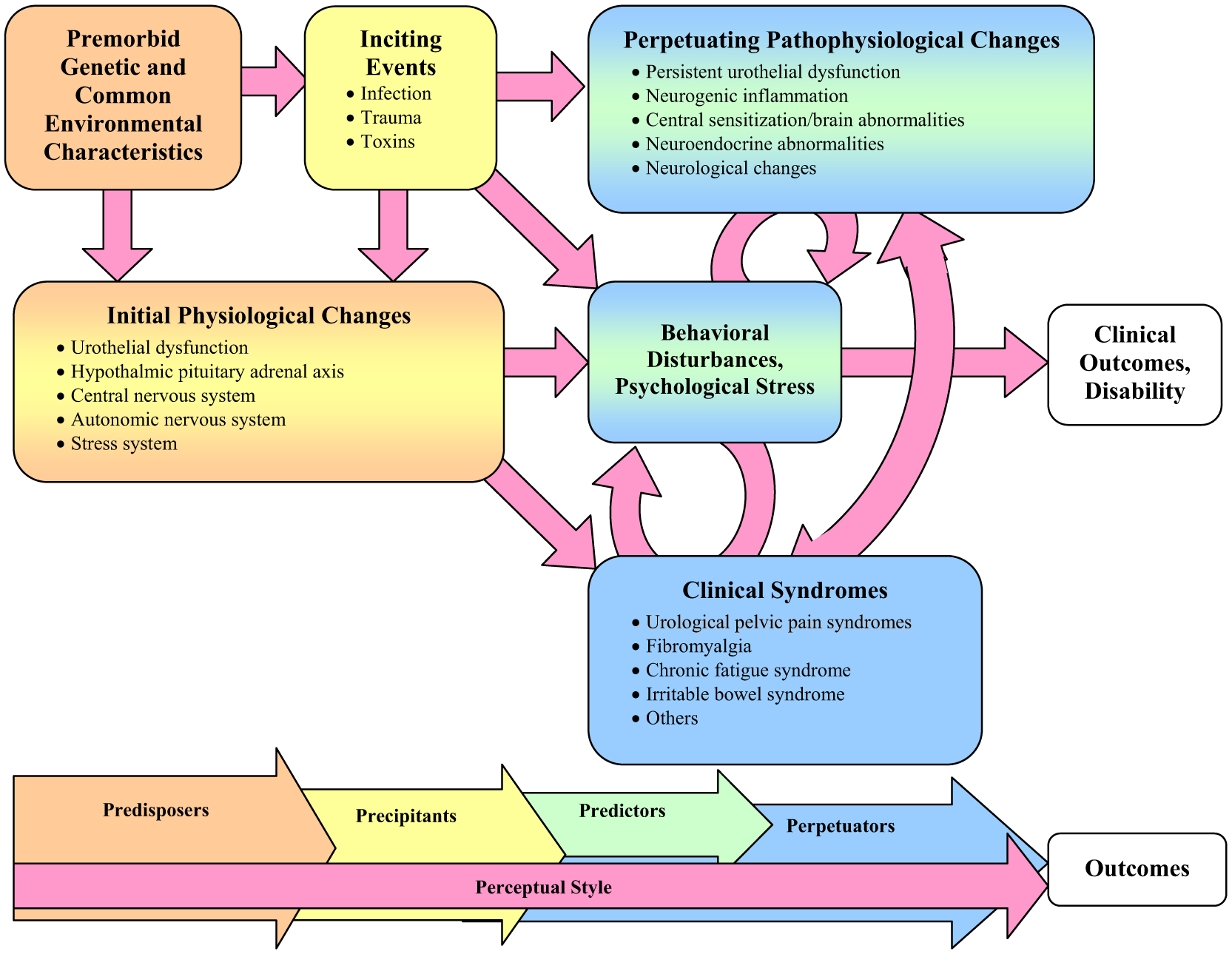
Multidimensional conceptual model of unexplained clinical conditions
Conceptually driven investigations of the mechanisms that may predispose, precipitate, perpetuate and predict these conditions can improve our understanding of urological unexplained clinical conditions and their comorbidities. Given the prominence of pain across the syndromes of interest, examination of the central sensitization hypothesis is crucial to understanding their substantial comorbidity. Furthermore, twin and family studies can clarify the role of shared genetic and environmental factors in syndrome genesis and perpetuation.
Limitations of Studies
We discovered several methodological shortcomings in the literature that undermine the strength of our conclusions and limit comparability across studies.
Study participants were drawn primarily from tertiary care clinics, hampering the generalizability of findings to primary care patients and to the general population. Clinical ascertainment and other biases associated with the study of treatment seeking populations are well-known46 and can be an important source of spurious comorbidity. Anxiety, poor coping, stressful events and other psychological factors also may have a role in health care seeking in IBS and FM cases.47 Thus, the comorbidity of urological and nonurological unexplained clinical conditions may be an artifact of health care use.
We found inconsistencies in assessment. Although research on unexplained clinical conditions may be hampered by a lack of diagnostic markers, these conditions have established case definitions designed to facilitate symptom based diagnosis and comparability across research studies. Nonetheless, many methods were used to assess the conditions of interest, ranging from established case definitions to self-reported physician diagnoses and review of computerized ICD-9 codes. Several investigations relied on medical history questionnaires or self-reported diagnoses without independent confirmation by medical record reviews or clinical examinations. This reliance questions the accuracy of all rates of conditions based on self-report but especially those requiring physical examination findings (eg FM) or the exclusion of specific medical disorders (eg CFS). Also, studies based on physician diagnoses in medical records may underestimate comorbidity if a patient attends 1 clinic for primary symptoms but is discouraged from seeking specialty care for other symptoms, which may occur in health maintenance organizations. Studies also differed in inclusion and exclusion criteria. All of these factors affect the degree of overlap among urological and nonurological unexplained clinical conditions, and make comparisons across studies problematic.
Except CP/CPPS in men, most participants with unexplained clinical conditions were women. It has been debated whether certain urological unexplained clinical conditions, particularly IC/PBS and CP/CPPS in men, represent somewhat different manifestations of the same disorder and whether IC/PBS risk factors and manifestations differ in men and women.48 Sex differences clearly exist in the epidemiology, symptomatology, physiology and psychological features of FM, CFS and IBS,49 raising the possibility that the overlap between urological and nonurological unexplained clinical conditions is sex specific. Clearly there are too few studies in men to fully examine any sex differences in overlap that may exist. Studies in large samples of men are needed to examine the role of sex in the co-occurrence of these conditions. Likewise, more data are needed to examine the association of these conditions across different cultural, racial and ethnic groups.
In studies comparing 2 or more groups controls consisted variously of healthy individuals, those with another chronic illness or controls with unreported health status. Only 2 studies were controlled for genetic and common environmental effects using co-twin control methods.9,20 Most groups did not use multivariate analytical techniques to adjust for demographic or other differences that could decrease the strength of the association between comorbid conditions.
CONCLUSIONS
Our extensive review of the published literature on the overlap between urological and nonurological unexplained clinical conditions suggests that comorbidity is common. However, these studies have several methodological shortcomings that undermine the strength of our conclusions and limit comparability across studies. Future studies of the overlap should adhere to the established research diagnostic criteria for each condition. Large-scale, rigorously designed and well controlled studies in clinical and community populations can yield more definitive answers to questions of overlapping symptoms and syndromes. Also, longitudinal cohort designs are needed to examine risk factors, temporal onset and prognosis. A recent study published since this review was done showed significant associations between antecedent nonurological unexplained clinical conditions and incident cases of IC/PBS,50 further underscoring the need for longitudinal studies. Other studies of urological unexplained clinical conditions should focus on health and behavior related characteristics, for example quality of life, disability or health care use, that can estimate the added burden of co-occurring syndromes on meaningful outcomes such as functional status, employment and health care costs. Examining possible mediators for comorbidity, for example abuse, victimization or psychological distress, can elucidate the relationship between overlapping conditions and identify subgroups at risk for urological CPP syndromes and related conditions. Well controlled studies to assess comorbidity and pathophysiological mechanisms can advance our understanding and improve treatment for these conditions.
ACKNOWLEDGMENTS
Dayron Rodriguez, Michael D. Smith, Jaeseop Lee and Michael O’Leary, Harvard Medical School; Almudena López, University Rey Juan Carlos, Madrid, Spain; and Debra Sprague, University of Washington assisted with the literature review and reviewed the manuscript. Drs. John Kusek, Leroy Nyberg and Christopher Mullins of the primary funding agency reviewed the manuscript.
Supported by NIDDK Grant U01 DK082325 (DSB, NA), and National Institute of Arthritis and Musculoskeletal and Skin Diseases Grants R21 AR053963 (DSB) and R01AR51524 (NA).
Abbreviations and Acronyms
- CFS
chronic fatigue syndrome
- CP
chronic prostatitis
- CPP
chronic pelvic pain
- CPPS
CPP syndrome
- CWP
chronic widespread pain
- FM
fibromyalgia
- IBD
inflammatory bowel disease
- IBS
irritable bowel syndrome
- IC
interstitial cystitis
- NIDDK
National Institute of Diabetes and Digestive and Kidney Diseases
- PBS
painful bladder syndrome
- TMD
temporomandibular joint and muscle disorders
APPENDIX
NIDDK Working Group on Urological CPP: Drs. Niloofar Afari, Dedra S. Buchwald, Daniel Clauw, Jordan Dimitrakov, John Kusek, Christopher Mullins, Leroy Nyberg, Christopher Payne, Cecilia Peñacoba, Michael Pezzone, Michel Pontari, Jeannette Potts, María Ángeles Bullones Rodríguez, and John Warren.
Footnotes
Final review findings are endorsed by and represent the views of the authors, and the National Institute of Diabetes and Digestive and Kidney Diseases Working Group on Urological CPP.
REFERENCES
- 1.Wessely S, Nimnuan C and Sharpe M: Functional somatic syndromes: one or many? Lancet 1999; 354: 936. [DOI] [PubMed] [Google Scholar]
- 2.Buffington CA: Comorbidity of interstitial cystitis with other unexplained clinical conditions. J Urol 2004; 172: 1242. [DOI] [PubMed] [Google Scholar]
- 3.Aaron LA and Buchwald D: A review of the evidence for overlap among unexplained clinical conditions. Ann Intern Med 2001; 134: 868. [DOI] [PubMed] [Google Scholar]
- 4.Waylonis GW and Heck W: Fibromyalgia syndrome. New associations. Am J Phys Med Rehabil 1992; 71: 343. [DOI] [PubMed] [Google Scholar]
- 5.Clauw DJ, Schmidt M, Radulovic D et al. : The relationship between fibromyalgia and interstitial cystitis. J Psychiatr Res 1997; 31: 125. [DOI] [PubMed] [Google Scholar]
- 6.Ostensen M and Schei B: Sociodemographic characteristics and gynecological disease in 40–42 year old women reporting musculoskeletal disease. Scand J Rheumatol 1997; 26: 426. [DOI] [PubMed] [Google Scholar]
- 7.Erickson DR, Morgan KC, Ordille S et al. : Non-bladder related symptoms in patients with interstitial cystitis. J Urol 2001; 166: 557. [PubMed] [Google Scholar]
- 8.Arnold LD, Bachmann GA, Rosen R et al. : Vulvodynia: characteristics and associations with comorbidities and quality of life. Obstet Gynecol 2006; 107: 617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kato K, Sullivan PF, Evengard B et al. : Chronic widespread pain and its comorbidities: a population-based study. Arch Intern Med 2006; 166: 1649. [DOI] [PubMed] [Google Scholar]
- 10.Kennedy CM, Bradley CS, Galask RP et al. : Risk factors for painful bladder syndrome in women seeking gynecologic care. Int Urogynecol J Pelvic Floor Dysfunct 2006; 17: 73. [DOI] [PubMed] [Google Scholar]
- 11.Pontari MA: Chronic prostatitis/chronic pelvic pain syndrome and interstitial cystitis: are they related? Curr Urol Rep 2006; 7: 329. [DOI] [PubMed] [Google Scholar]
- 12.Shaver JL, Wilbur J, Robinson FP et al. : Women’s health issues with fibromyalgia syndrome. J Womens Health (Larchmt) 2006; 15: 1035. [DOI] [PubMed] [Google Scholar]
- 13.Wu EQ, Birnbaum H, Kang YJ et al. : A retrospective claims database analysis to assess patterns of interstitial cystitis diagnosis. Curr Med Res Opin 2006; 22: 495. [DOI] [PubMed] [Google Scholar]
- 14.Wu EQ, Birnbaum H, Mareva M et al. : Interstitial cystitis: cost, treatment and co-morbidities in an employed population. Pharmacoeconomics 2006; 24: 55. [DOI] [PubMed] [Google Scholar]
- 15.Arnold LD, Bachmann GA, Rosen R et al. : Assessment of vulvodynia symptoms in a sample of US women: a prevalence survey with a nested case control study. Am J Obstet Gynecol 2007; 196: 128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berger RE, Ciol MA, Rothman I et al. : Pelvic tenderness is not limited to the prostate in chronic prostatitis/chronic pelvic pain syndrome (CPPS) type IIIA and IIIB: comparison of men with and without CP/CPPS. BMC Urol 2007; 7: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Araujo MP, Faria AC, Takano CC et al. : Urodynamic study and quality of life in patients with fibromyalgia and lower urinary tract symptoms. Int Urogynecol J Pelvic Floor Dysfunct 2008; 19: 1103. [DOI] [PubMed] [Google Scholar]
- 18.Clemens JQ, Meenan RT, O’Keeffe Rosetti MC et al. : Case-control study of medical comorbidities in women with interstitial cystitis. J Urol 2008; 179: 2222. [DOI] [PubMed] [Google Scholar]
- 19.Dimitrakov J, Joffe HV, Soldin SJ et al. : Adrenocortical hormone abnormalities in men with chronic prostatitis/chronic pelvic pain syndrome. Urology 2008; 71: 261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aaron LA, Herrell R, Ashton S et al. : Comorbid clinical conditions in chronic fatigue: a co-twin control study. J Gen Intern Med 2001; 16: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koziol JA: Epidemiology of interstitial cystitis. Urol Clin North Am 1994; 21: 7. [PubMed] [Google Scholar]
- 22.Clemens JQ, Brown SO, Kozloff L et al. : Predictors of symptom severity in patients with chronic prostatitis and interstitial cystitis. J Urol 2006; 175: 963. [DOI] [PubMed] [Google Scholar]
- 23.Novi JM, Jeronis S, Srinivas S et al. : Risk of irritable bowel syndrome and depression in women with interstitial cystitis: a case-control study. J Urol 2005; 174: 937. [DOI] [PubMed] [Google Scholar]
- 24.Grace V and Zondervan K: Chronic pelvic pain in women in New Zealand: comparative well-being, comorbidity, and impact on work and other activities. Health Care Women Int 2006; 27: 585. [DOI] [PubMed] [Google Scholar]
- 25.Walker EA, Gelfand AN, Gelfand MD et al. : Chronic pelvic pain and gynecological symptoms in women with irritable bowel syndrome. J Psychosom Obstet Gynaecol 1996; 17: 39. [DOI] [PubMed] [Google Scholar]
- 26.Zimmerman J: Extraintestinal symptoms in irritable bowel syndrome and inflammatory bowel diseases: nature, severity, and relationship to gastrointestinal symptoms. Dig Dis Sci 2003; 48: 743. [DOI] [PubMed] [Google Scholar]
- 27.Whitehead WE, Palsson OS, Levy RR et al. : Comorbidity in irritable bowel syndrome. Am J Gastroenterol 2007; 102: 2767. [DOI] [PubMed] [Google Scholar]
- 28.Kennedy CM, Nygaard IE, Bradley CS et al. : Bladder and bowel symptoms among women with vulvar disease: are they universal? J Reprod Med 2007; 52: 1073. [PubMed] [Google Scholar]
- 29.Nimnuan C, Rabe-Hesketh S, Wessely S et al. : How many functional somatic syndromes? J Psychosom Res 2001; 51: 549. [DOI] [PubMed] [Google Scholar]
- 30.Alagiri M, Chottiner S, Ratner V et al. : Interstitial cystitis: unexplained associations with other chronic disease and pain syndromes. Urology 1997; 49: 52. [DOI] [PubMed] [Google Scholar]
- 31.Gordon AS, Panahian-Jand M, McComb F et al. : Characteristics of women with vulvar pain disorders: responses to a Web-based survey. J Sex Marital Ther, suppl., 2003; 29: 45. [DOI] [PubMed] [Google Scholar]
- 32.Yamada T, Funahashi M and Murayama T: Clinical evaluation of 30 patients with interstitial cystitis complicated by fibromyalgia. Nippon Hinyokika Gakkai Zasshi 2005; 96: 554. [DOI] [PubMed] [Google Scholar]
- 33.Korszun A, Papadopoulos E, Demitrack M et al. : The relationship between temporomandibular disorders and stress-associated syndromes. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998; 86: 416. [DOI] [PubMed] [Google Scholar]
- 34.Giamberardino M: Sex-related and hormonal modulation of visceral pain. In: Sex, Gender and Pain. Edited by Fillingim R. Seattle: IASP Press; 2000; vol 17, pp 135–162. [Google Scholar]
- 35.FitzGerald MP, Brensinger C, Brubaker L et al. : What is the pain of interstitial cystitis like? Int Urogynecol J Pelvic Floor Dysfunct 2006; 17: 69. [DOI] [PubMed] [Google Scholar]
- 36.Maxton DG, Morris JA and Whorwell PJ: Ranking of symptoms by patients with the irritable bowel syndrome. BMJ 1989; 299: 1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Blanchard EB, Keefer L, Lackner JM et al. : The role of childhood abuse in Axis I and Axis II psychiatric disorders and medical disorders of unknown origin among irritable bowel syndrome patients. J Psychosom Res 2004; 56: 431. [DOI] [PubMed] [Google Scholar]
- 38.Walker EA, Katon WJ, Jemelka R et al. : The prevalence of chronic pelvic pain and irritable bowel syndrome in 2 university clinics. J Psychosom Obstet Gynaecol, suppl., 1991; 12: 65. [Google Scholar]
- 39.Williams RE, Hartmann KE, Sandler RS et al. : Recognition and treatment of irritable bowel syndrome among women with chronic pelvic pain. Am J Obstet Gynecol 2005; 192: 761. [DOI] [PubMed] [Google Scholar]
- 40.Fenton BW, Durner C and Fanning J: Frequency and distribution of multiple diagnoses in chronic pelvic pain related to previous abuse or drug-seeking behavior. Gynecol Obstet Invest 2008; 65: 247. [DOI] [PubMed] [Google Scholar]
- 41.Riedl A, Schmidtmann M, Stengel A et al. : Somatic comorbidities of irritable bowel syndrome: a systematic analysis. J Psychosom Res 2008; 64: 573. [DOI] [PubMed] [Google Scholar]
- 42.Turk DC: A diathesis-stress model of chronic pain and disability following traumatic injury. Pain Res Manag 2002; 7: 9. [DOI] [PubMed] [Google Scholar]
- 43.Melzack R: From the gate to the neuromatrix. Pain, suppl., 1999; 6: S121. [DOI] [PubMed] [Google Scholar]
- 44.Gracely RH, Petzke F, Wolf JM et al. : Functional magnetic resonance imaging evidence of augmented pain processing in fibromyalgia. Arthritis Rheum 2002; 46: 1333. [DOI] [PubMed] [Google Scholar]
- 45.Ullrich PM, Afari N, Jacobsen C et al. : Cold pressor pain sensitivity in monozygotic twins discordant for chronic fatigue syndrome. Pain Med 2007; 8: 216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bogenschutz MP and Nurnberg HG: Theoretical and methodological issues in psychiatric comorbidity. Harv Rev Psychiatry 2000; 8: 18. [PubMed] [Google Scholar]
- 47.Ringstrom G, Abrahamsson H, Strid H et al. : Why do subjects with irritable bowel syndrome seek health care for their symptoms? Scand J Gastroenterol 2007; 42: 1194. [DOI] [PubMed] [Google Scholar]
- 48.Moldwin RM: Similarities between interstitial cystitis and male chronic pelvic pain syndrome. Curr Urol Rep 2002; 3: 313. [DOI] [PubMed] [Google Scholar]
- 49.Munce SE and Stewart DE: Gender differences in depression and chronic pain conditions in a national epidemiologic survey. Psychosomatics 2007; 48: 394. [DOI] [PubMed] [Google Scholar]
- 50.Warren JW, Howard FM, Cross RK et al. : Antecedent nonbladder syndromes in case-control study of interstitial cystitis/painful bladder syndrome. Urology 2009; 73: 52. [DOI] [PubMed] [Google Scholar]


