Abstract
Objective
This scoping review aimed to synthesize the published literature on family‐based childhood obesity prevention interventions from 2015 to 2021 that focused on children 2–5 years of age from racial and/or ethnic minority households.
Methods
A PICOS (population, intervention, comparison, outcome, and setting) framework was used to guide the development of the research question, search strategy, and inclusion/exclusion criteria. To be included, the study must have been a randomized controlled trial or quasi‐experimental trial that enrolled participants 2–5 years of age and their caregivers who identified as being from a racial and/or ethnic minority group in the United States. The study must have also examined a family‐based intervention that incorporated components to prevent childhood obesity (i.e., fruits and vegetable intake, parental responsive feeding, physical activity), be conducted in a remote (i.e., online, text, mail), home, community, primary care setting, or early childhood education institution setting, and report on body mass index (BMI, kg/m2), BMI z‐score, anthropometric measures (weight, waist circumference, fat mass, etc.), changes in health behaviors, or increase in nutritional knowledge.
Results
Fourteen individual studies were identified. Most interventions used multiple components for promoting nutritional knowledge and behavioral changes among families. Eight interventions included culturally tailored components targeting four aspects: (1) language barriers, (2) food choices, (3) relationships between family members, and (4) rapport building.
Conclusions
There is limited research in this field focusing on children from racial and/or ethnic minority groups. Future efforts should invest in developing culturally appropriate interventions for these groups.
Keywords: childhood obesity, family‐based intervention, obesity prevention, racial/ethnic minority
1. INTRODUCTION
The prevalence of childhood obesity in the United States remains unacceptably high. According to recent data from the 2017–2018 National Health and Nutrition Examination Survey, the prevalence of obesity among preschool‐age children, 2–5 years, is 13.7%. 1 Since the 1970's, the trend of childhood overweight and obesity has maintained an average annual rate of increase of approximately 0.5% for children 2 years old and older. 2 At the start of the millennium, the prevalence of overweight and obesity among US preschoolers rose from 7.2% to 10.3%. 2 Although a decline was seen during the first half of the 2010s, an increase has been seen since 2015. Currently, the prevalence of childhood overweight and obesity in the United States is higher than ever. 3
A closer look at the data reveals important disparities in the pediatric obesity epidemic by race and/or ethnicity. Children who identify as Mexican American or non‐Hispanic Black have a higher prevalence of obesity than their non‐Hispanic White counterparts. 2 Since 2005, children who identify as Alaska Native or American Indian have seen the largest increase in the prevalence of obesity. 4 According to the US Census Bureau, the racial and ethnic composition of the US population is projected to be more pluralistic in the coming decades. By 2060, approximately 32% of the population is predicted to be a race other than White. The change in the racial and/or ethnic representation will be more most pronounced among children. 5 As the racial and/or ethnic diversity of children in the United States increases, health disparities associated with obesity will affect a larger proportion of the US population. 6 This trend of increasing racial and/or ethnic diversity of children in the US highlights the need for pediatric obesity research to include non‐White populations.
Disparities in pediatric obesity might be explained by genetic factors, differences in dietary patterns, physical activity, child feeding practices, cultural norms, attitudes toward weight and aesthetics, availability of healthy foods, and access to social resources. 4 Evidence suggests that obesity risk factors (i.e., fruit and vegetable intake, physical activity, and screen use, rapid infant weight gain) are shaped by cultural practices and make important contributions to the observed racial and/or ethnic disparities of obesity among children. 7
Addressing childhood obesity is important given the detrimental impact obesity has on the physical and mental health of children. Children affected by obesity are more likely to have (1) high blood pressure and plasma cholesterol levels, leading to increased risk of developing cardiovascular disease, (2) respiratory problems, such as sleep apnea and asthma, (3) musculoskeletal discomfort and joint problems, and (4) gallstones, fatty liver disease, and gastroesophageal reflux. 8 , 9 , 10 , 11 , 12 , 13 , 14 Children who suffer from obesity are also at increased risk for depression, anxiety, low self‐esteem, and bullying. 15 , 16 , 17 A child's obesity status appears to be an important predictor for the risk of future obesity starting at age three. 18 In a prior study examining the association between BMI in childhood and later risk of overweight and obesity, Geserick et al found that 90% of the participants with obesity at 3 years continued to be affected by obesity as they became older, with the most significant weight gain occurring between 2 and 6 years old. 19 Additionally, the study showed that having a normal weight during childhood predicted a continued normal weight later in life, indicating that early childhood might be a relatively narrow but critical period for implementing programs preventing excessive weight gain and reducing the risk of obesity. 19
Family‐based interventions are recognized as an effective strategy to prevent and treat childhood obesity. 20 Family‐based interventions engage the family to encourage the adoption of healthy behaviors among all family members. Frequently, the interventions include components focusing on behavior change by teaching caregivers to set goals, solve problems, monitor their child's behaviors, and become a positive model for their child. 21 Sessions are typically held with caregivers and children, but individual sessions for children or caregivers have also been used. 22 Many studies have demonstrated that family‐based behavioral programs can successfully prevent or manage childhood obesity. 23 , 24 , 25 , 26 , 27 , 28 However, according to a systematic review conducted by Ash et al on family‐based childhood obesity prevention interventions prior to 2016, there were few studies focusing on the effectiveness of family‐based interventions among racial and/or ethnic minority communities, and few interventions (16%) targeted obesity risk related behavioral domains other than diet and exercise (i.e., sleep and screen time). 29 These results were similar to the findings of a study conducted by Carr et al that also found a lack of obesity prevention interventions addressing health‐promoting behaviors other than diet and exercise. 30
A current gap in the literature is a summary of the recent evidence for specific component and cultural adaptations of family‐based interventions in the prevention of obesity among children 2–5 years of age who belong to racial and/or ethnic minority groups. Therefore, the aim of our scoping review was to build upon the review by Ash et al and summarize the recently published literature on family‐based childhood obesity prevention interventions with a focus on US preschoolers 2–5 years old who were identified by their caregivers as being from a racial and/or ethnic minority group.
2. METHOD
2.1. Inclusion and exclusion criteria
A PICOS (population, intervention, comparison, outcome, and setting) framework was used to guide the development of the research question, search strategy, and inclusion/exclusion criteria. The inclusion criteria addressed four aspects: participant characteristics, intervention characteristics, setting, and study design. To be included, the study must have been a randomized controlled trial or quasi‐experimental trial that enrolled participants 2–5 years of age and their caregivers who identified as being from a racial and/or ethnic minority groups in the United States. 31 For the purposes of our study families who identified as: Blacks/African‐Americans, Hispanic/Latinx, Asians and Pacific Islanders, and American Indians and Alaska Natives were included in the study. 31 At least half of the children enrolled needed to be at normal weight at baseline for the study to be included in our review. The study must have also examined a family‐based intervention that incorporated components to prevent childhood obesity (i.e., fruits and vegetable intake, parental responsive feeding, physical activity), be conducted in a remote (i.e., online, text, mail), home, community, primary care setting, or early childhood education institution setting, and report on body mass index (BMI, Kg/m2), BMI z‐score, anthropometric measures (weight, waist circumference, fat mass, etc.), changes in health behaviors, or increase in nutritional knowledge. At least 50% of the participants enrolled needed to identify as belonging to a racial and/or ethnic minority group for the study to be included in this review. The current scoping review was limited to studies published since 2015 and sought to serve as an update on the systematic review published by Ash et al on prior family‐based childhood obesity prevention interventions. 29
2.2. Search strategy
The search was limited to studies written in English, published from 1/1/2015 to 3/21/2021, and found in one of the following databases: PubMed, Scopus, PsycINFO, and CINAHL. The development of search strings was based on the five major concepts examined by the scoping review: (1) family, (2) nutrition, (3) preschool‐age children, (4) overweight/obesity and weight status, and (5) racial and/or ethnic minority. With the support from a librarian, tailored search strategies were created for each database.
2.3. Source of evidence screening and selection
After completing the literature search in all four databases, results were exported to a citation manager (Mendeley) and de‐duplicated. The de‐duplicated citations were then exported from Mendeley to Covidence for screening and review.
Two reviewers (XW and CO) independently reviewed the titles, abstracts, and full text of the articles in Covidence and decided whether an article met the inclusion criteria described above. Conflicts were resolved by discussion between the two reviewers.
2.4. Eligible articles
Using the search strategy described above, one reviewer (XW) identified 4800 studies from the four databases. After removing duplicates, 3669 studies were screened based on title and abstract. At this stage, studies were excluded mainly because (1) study was not conducted in the United States, (2) study did not describe an intervention, and (3) study included an intervention that was out of the scope of the review (i.e., a training program targeting educators instead of children and their caregivers). Forty‐four studies were included for full‐text screening. Among these studies, 11, 13, and 5 studies were excluded because of irrelevant or unavailable population, outcome, and intervention data/information, respectively. On manual review a duplicated article we identified and removed, leaving 14 studies meeting all the inclusion criteria for the final synthesis. Figure 1 depicts the study screening process using the PRISMA flowchart.
FIGURE 1.
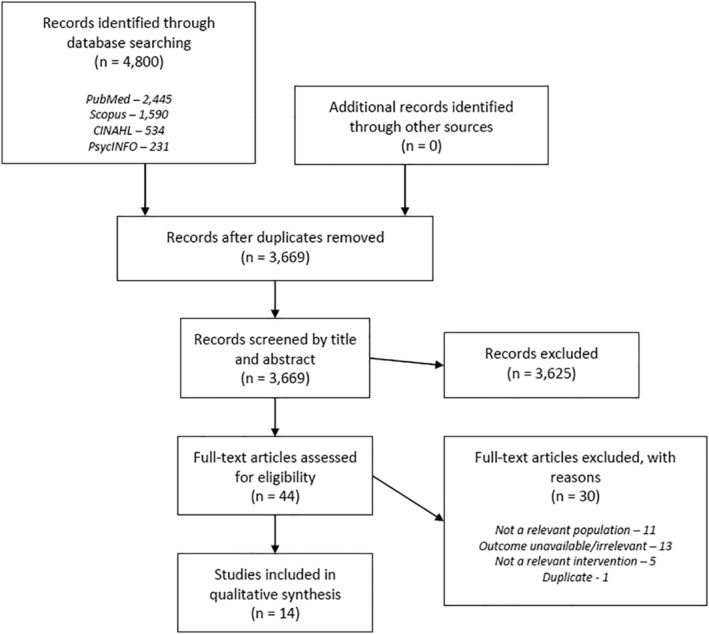
PRISMA flow diagram
2.5. Data extraction
A data extraction spreadsheet including study information (title, year, author, study design, location), participant characteristics (child age, sample size, race and/or ethnicity, socioeconomic status), intervention characteristics (name, theory, behavioral domain component, target population, setting, delivery mode, component, length, frequency), and intervention outcomes (outcome measure, result) were developed. One reviewer (XW) was responsible for data extraction and information categorization, while the completed spreadsheet was examined by the other reviewer (CO). Given our study is a scoping review, we did not evaluate the methodological quality of the studies. 32 , 33
3. RESULT
3.1. Study design, outcome measures, & sample
A total of 14 studies were included in the final analysis (Table 1). Eleven of the studies employed a randomized controlled trial design, 34 , 36 , 43 , 46 , 47 and three used a quasi‐experimental design. 35 , 44 , 45 Three studies were pilot evaluations. 41 , 42 , 45 Half of the studies used child body mass index (BMI), BMI z‐score, or BMI trajectory as the primary outcome. Others focused on child health‐related behaviors, dietary patterns, parent‐feeding practices, or other anthropometric measures. There was heterogeneity in the study sample size and demographics. The sample sizes ranged from 17 to 610. A majority of the studies recruited participants who identified as Hispanic/Latinx, followed by Black/African American and American Indian. A majority of the participants were from low‐income families. The studies were conducted in geographically diverse locations.
TABLE 1.
Study and participants characteristics
| Author, year | Study design | Total participants | Geographic region | Race/ethnicity |
|---|---|---|---|---|
| Barkin et al, 2018 34 | RCT | 610 parent/child dyads | Nashville, Tennessee | Hispanic (91.4%), non‐Hispanic Black (5.9%), non‐Hispanic White/Other (2.6%) |
| Brown et al, 2019 35 | Quasi‐experimental | 17 parents | An American Indian reservation | American Indian (47%) a |
| Fisher et al, 2019 36 | RCT | 119 mothers | Philadelphia, Pennsylvania | Black/African American (90.8%), Other (9.2%) |
| French et al, 2018 37 | RCT | 534 parent–child dyads | Minneapolis, Minnesota | Hispanic (58.4%), non‐Hispanic Black (18.4%), non‐Hispanic White (12.6%), multiracial (8.4%), other (2.3%) |
| Haines et al, 2016 38 | RCT | 112 families | Boston, Massachusetts | Hispanic (59%), Black/African American (22%), White/Other (18.7%) |
| Heerman et al, 2018 39 | RCT | 117 parent–child dyads | Nashville, Tennessee | Hispanic (100%) |
| Hughes et al, 2020 40 | RCT | 255 families | Houston, Texas; Pasco, Washington | Hispanic (100%) |
| Jastreboff et al, 2018 41 | Pilot, RCT | 42 parent/child dyads | New Haven, Connecticut | 62% non‐White a |
| Linville et al, 2020 42 | Pilot, RCT | 27 families | Oregon | Hispanic (89%) |
| Nix et al, 2021 43 | RCT | 73 parent–child dyads | Pennsylvania | Non‐Hispanic white (48%), Black/African American (29%), Hispanic (23%) |
| Sosa et al, 2016 44 | Quasi‐experimental | 423 children | San Antonio, Texas | Hispanic (90%) a |
| Taverno Ross et al, 2018 45 | Pilot, quasi‐experimental | 49 parent–child dyads | Allegheny, Pennsylvania | Hispanic (100%) |
| Tomayko et al, 2016 46 | RCT | 150 parent–child dyads | Wisconsin | American Indian (91%), White (7%), unknown (1%) |
| Tomayko et al, 2019 47 | RCT | 450 parent–child dyads | Wisconsin; Minnesota; Montana; New Mexico; New York | American Indian (78.7%), White (18.7%), other (2.6%) |
Further break‐downs unavailable.
3.2. Intervention characteristics
Most of the interventions built on previously studied behavioral change theories and models. The most frequently referenced theories were (1) social cognitive theory, 48 and (2) self‐determination theory. 49
Among the 14 interventions, four interventions included components only for parents, while others included components for parents and children. 35 , 36 , 40 , 41 Interventions targeting parents addressed authoritative parenting skills, parental mindfulness and behavioral strategies, parental strategies to improve child portion control and family environment, and information on child nutrition and health‐related behaviors. 35 , 36 , 40 , 41
Five and three interventions, respectively, enrolled primarily Hispanic/Latinx and American Indian families, and included culturally tailored curriculum or materials. 35 , 39 , 40 , 42 , 44 , 45 , 46 , 47 The remaining studies targeted diverse racial and/or ethnic minority communities. None of the studies enrolling Black/African American participants created culturally tailored components for this community. Components tailored for Hispanic/Latinx participants included recruiting local educators who shared the same cultural background with and were trusted by participants, 45 providing educational materials written in Spanish and delivered by bilingual/Spanish‐speaking educators, 39 , 40 , 42 , 44 selecting intervention locations that participants were familiar with, 42 using food examples that were culturally congruent, 40 , 42 building rapport between educators and participants, 42 tailoring content to participants' needs in navigating individual, family, and community level barriers. 39 Components tailored for American Indian participants included recruiting educators from the area (tribe), promoting culturally appropriate food and activities, adopting a traditional model of younger generations inheriting life‐skills from the elders, and incorporating the functions of family structure and interactions into the interventions. 35 , 46 , 47
Seven interventions were delivered in‐person in group settings, two were delivered by home mentors, one used phone‐based using text messages, one used mail‐based, and the rest incorporated multifaceted components delivered via home‐based, group‐based, and/or phone/mail‐based sessions.
Behavioral, cognitive, and psychomotor domains targeted by interventions varied. Five interventions featured a combination of education on healthy lifestyles (i.e., information on child nutrition, physical activity, sleep, screen use) and behavior change components (i.e., goal setting and skill building). 34 , 36 , 39 , 45 , 46 Two promoted parenting and feeding skills and self‐efficacy building. 36 , 38 Two provided education/information on healthy lifestyles without further supplemental components. 35 , 47 Others covered parent mindfulness‐based stress reduction, child eating self‐regulation, and healthy meals preparation skills. 40 , 41 , 43 Of note, the studies conducted by Haines et al and Tomayko et al in 2019 targeted all four aspects of the behavioral domain (diet, physical activity, sleep, and screen use). 38 , 47
There were also differences among the length and frequency of the interventions. The length of the interventions ranged from 5 weeks to 36 months, with a majority (n = 8) of interventions engaging participants for 12 weeks or less. For interventions delivered in‐person, the majority of studies consisted of weekly sessions lasting 1–2 h, with the exception of two interventions that delivered biweekly 5–10 min sessions, 44 and weekly 45‐min sessions. 43 We were unable to quantify frequency of contact for studies using remote deliveries (text, phone call, etc). A full description of intervention characteristics can be found in Table 2.
TABLE 2.
Intervention characteristics
| Name | Setting | Theory | Participant | Component & dose | Cultural adaptation | Weight‐unrelated outcome assessment tool | Significant outcome a |
|---|---|---|---|---|---|---|---|
| Parenting Mindfully for Health 41 | Research center | Mindfulness‐Based Stress Reduction 50 | Parent | 2 h per week (mindfulness‐based parent stress group session + nutrition & physical activity counseling) × 8 weeks | N/A | Mindfulness skills—Mindfulness Attention Awareness Scale 51 ; nutrition data—Nutrition Questionnaire, 52 Dutch Eating Behavior Questionnaire 53 ; parenting behaviors—Toy Wait Task 54 , 55 ; physical activity—pedometer, accelerometer | Parental involvement, parental emotional eating rate, increase in BMI |
| Parents and Tots Together 38 | Community health center | Social contextual framework 56 | Parent & child | 2 h per week (parenting & weight‐related behaviors discussion session + children's healthy weight session + homework assignments) × 9 weeks | N/A | Changes in child weight‐related behaviors—Children's Harvard Service Food Frequency Questionnaire, 57 National Longitudinal Survey of Children and Youth, 58 Child Feeding Questionnaire 59 ; parenting strategies—Parenting Questionnaire, 60 Toddler Care Questionnaire 61 | Restrictive feeding practices |
| GROW Healthier 34 | Community center | Social cognitive theory 48 ; socioecological model 62 | Parent & child | Once per week (parent & child skills‐building session) × 12 weeks + once per month (coaching telephone call) × 9 months + 24‐month sustainability phase | N/A | Physical activity—accelerometer; dietary intake—24 h diet recall; food insecurity—US Household Food Security Survey Module 63 ; Parent‐reported community center use—parental survey | Child mean caloric intake, use of community centers |
| Food, Fun, and Families 36 | University clinic | Authoritative food parenting 64 , 65 | Parent | 1 h per week (behavioral change group session) × 12 weeks | N/A | Child daily energy from SoFAS—24 h dietary recall; authorative food parenting practices—meal observation in a lab setting | Child daily energy intake from SoFAS, authoritative parenting practices |
| ANDALE Pittsburgh 45 | Home | Social cognitive theory 48 ; socioecological framework 66 | Parent & child | Culturally tailored for Hispanic; 1.5 h per week (home‐based nutrition education + behavioral change session) × 10 weeks | Recruiting local educators (promotoras) who shared the same cultural background with and were trusted by participants | Physical activity—accelerometer, self‐report survey 67 ; dietary intake—Block Food Screener for Kids 2007 68 ; home environment—a survey adapted from several sources 69 , 70 , 71 , 72 , 73 , 74 | BMI percentile of child with obesity, child saturated fat and added‐sugar intake, parent moderate‐to‐vigorous physical activity and self‐efficacy, child and parent screen time, child and parent daily fruit and vegetable intake |
| SEEDS 40 | Early learning institution | Self‐determination theory 49 | Parent | Culturally tailored for Hispanic; once per week (video viewing + experimental learning activities) × 7 weeks | Providing education materials written in Spanish and delivered by bilingual/Spanish‐speaking educators; using food examples that were culturally congruent | Parental feeding practices, styles, and knowledge—Food Parenting Inventory & Children's Eating Behavior Questionnaire, 75 Child Feeding Questionnaire, 59 Family Rituals Questionnaire, 76 Caregiver's Feeding Styles Questionnaire, 77 Feeding Knowledge Questionnaire; child self‐regulation, willingness to try new foods, and fruit and vegetable preferences—observed trial and eating self‐regulation score (COMPX), 78 food tasting protocol, 79 food preference questionnaire, 80 Eating in Absence of Hunger Task 81 | Feeding practices, styles, and knowledge, child different vegetables tried |
| Healthy Balance 42 | Family resource center | Cognitive dissonance theory 82 ; family systems theory 83 | Parent & child | Culturally tailored for Hispanic; 2 h per session (parents' behavioral change session + children's healthy eating education) × six sessions | Providing education materials written in Spanish and delivered by bilingual/Spanish‐speaking educators; selecting intervention location that participants were familiar with (family resource center); using food examples that were culturally congruent; building rapport between educators and participants by adding socializing time | Healthy habits and attitudes—self‐report survey, EDDS, 84 Block Food Frequency Questionnaire, 85 Active Where Study Survey 86 | Parents' BMI, neck circumference, and diastolic blood pressure |
| Healthy Children, Strong Families 46 | Home, mail | AI model of elders teaching life‐skills to the next generation | Parent & child | Culturally tailored for American Indian; mentor group: 1 h per month (home‐based toolkit lessons on healthy lifestyle) × 12 months + once per month (newsletter + behavioral change group session) × 12 months; non‐mentor group: Once per month (mailed toolkit lessons on healthy lifestyle) × 12 months + once per month (newsletter) × 12 months | Recruiting educators from the area (tribe) and promoting culturally appropriate food and activities; a traditional model of young generations inheriting life‐skills from the elders and the value toward family interaction | Nutrition and activity behaviors—24 h dietary recall, interview; physical activity—accelerometer; psychosocial factors—SF12 87 | In both groups: BMI percentile of child with obesity, child fruit/vegetable consumption, child and adult mean television watching, adult self‐efficacy, adult quality of life |
| Healthy Children, Strong Families 2 47 | AI model of elders teaching life‐skills to the next generation | Parent & child | Culturally tailored for American Indian; once per month (mailed toolkit lessons on healthy lifestyle) × 12 months + social media engagement | Recruiting educators from the area (tribe) and promoting culturally appropriate food and activities; a traditional model of young generations inheriting life‐skills from the elders and the value toward family interaction | Health behaviors—self‐report surveys 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 | Child and adult healthy diet patterns, adult F/V intake, moderate‐to‐vigorous physical activity, and self‐efficacy, home nutrition environment | |
| Short Messaging System (SmS) Parent Action Intervention 35 | Rural American Indian reservation/Text message | N/A | Parent | Culturally tailored for American Indian; 3 times per week (text message on child healthy lifestyle) × 5 weeks | Recruiting educators from the area (tribe) and promoting culturally appropriate food and activities | Parent knowledge and child behaviors—a 10‐item survey adapted from the 2013 Maine Integrated Youth Health Survey 97 | Child overall health behaviors, behaviors related to PA and sleep |
| ¡Míranos! (Look at Us, We Are Healthy!) 44 | Early learning institution, home | Social cognitive theory 48 | Parent & child | Culturally tailored for Hispanic; 5–10 min per week (parent obesity education + take‐home activities) × six sessions | Providing education materials written in Spanish and delivered by bilingual/Spanish‐speaking educators | Parent message recall—interview; parent knowledge, family supportive behaviors, and child health behaviors—a questionnaire generating/including/asking for a knowledge score, 5‐point Likert‐type item, a family supportbehaviors score, and frequency of child specific behaviors | Adult knowledge scores and family supportive behaviors |
| Competency‐Based Approaches to Community Health 39 | Community center | Self‐determination theory 49 ; social cognitive theory 48 | Parent & child | Culturally tailored for Hispanic; 1.5 h per week (education on healthy lifestyle + skill building session + individualized coaching) × 15 weeks + twice per month (coaching call on behavioral change) × 3 months | Providing education materials written in Spanish and delivered by bilingual/Spanish‐speaking educators; tailoring content to participants' needs in navigating individual, family, and community level barriers | Acculturation—Brief Acculturation Scale for Hispanics 98 ; diet—survey 99 ; child physical activity—parent self‐report; Parent physical activity—Behavioral Risk Factor Surveillance System 100 ; eating behaviors—survey 101 ; parent self‐efficacy—a 16‐item scale 102 ; parenting practices—Preschooler Physical Activity Parenting Practices 103 | Child BMI growth |
| Now Everybody Together for Amazing and Healthful Kids (NET‐Works) 37 | Home, community center | Social ecological model 104 | Parent & child | 1 h per month (home‐based behavioral change session) × 36 months + monthly check‐in calls + once per week (community‐based parenting class) × 12 weeks | N/A | Dietary intake—24‐h dietary recall, Healthy Eating Index 2010; physical activity—accelerometer; screen time—parent self‐report | Child energy intake and television viewing, BMI of Hispanic children and children affected by overweight/obesity |
| Recipe 4 Success 43 | Home | Recipe 4 Success conceptual model | Parent & child | 45 min per week (home‐based nutrition education + coaching on food preparation skills) × 10 weeks | N/A | Toddlers' healthy eating habits—24 h dietary recall, percentage of healthy meals; toddlers' self‐regulation—snack delay task, 105 task orientation and/or regulation subscale of the Infant Behavior Record, 106 Infant‐Toddler Social and Emotional Assessment 107 ; parents' responsive feeding practices—video recordings and scoring of how parents introduced toddlers to 3 novel healthy foods; parents' sensitive scaffolding—scoring of parents' tendencies to structure interaction tasks in an developmentally appropriate manner | Child healthy meals and snacks and self‐regulation, adult responsive feeding practices and sensitive scaffolding |
The outcomes listed were statistically significant at a p‐value of at least <0.05.
3.3. Outcomes
Outcomes included child weight, diet, and behavioral outcomes, and parental feeding practices and styles, diet, and behavioral outcomes (Table 2). Most of the studies compared baseline data to post intervention data, while studies conducted by Haines et al, Hughes et al, and Heerman et al incorporated follow‐up periods of 9, 12, and 5 months post intervention. 38 , 39 , 40
3.3.1. Child outcomes
Weight‐related outcomes
Among the seven studies including weight‐related measurements as primary outcomes, three found statistically significant results. 37 , 39 , 41 Jastreboff et al found that the BMI percentile of participants in the intervention group remained unchanged, while the BMI percentile in the control group increased significantly. 41 Heerman et al found a marginally statistically significant effect of the intervention on participants' BMI, with an annual decrease of 0.41 kg/m2 (95% CI −0.82 to 0.01; p = 0.05). 39 The study conducted by French et al showed a decreased BMI at study time points of 24 and 36 months among Hispanic/Latinx children who participated in the intervention. 37
Diet‐related outcomes
Eight studies described child diet‐related outcomes. 34 , 36 , 37 , 40 , 43 , 45 , 46 , 47 Two studies found that children in the intervention groups had statistically significant lower mean energy intake at 36 months, compared with children in the control groups. 34 , 37 Three studies described a statistically significant improvement in children's fruits and vegetable intake. 40 , 45 , 46 The study conducted by Nix et al demonstrated healthier meals and snacks consumption which included fruit and/or vegetables and protein without sweets or junk food. 43 The study conducted by Fisher et al focused on children's daily energy intake from solid fats and added sugar in foods (SoFAS) and found a significantly reduced energy intake from SoFAS of children in the intervention group, compared with their counterparts in the control group. 36 Tomayko et al found an improved dietary pattern at 12 months, measured with a scale adopted from Trude et al, among both adults and children in the intervention group. 47 , 108
Other behavioral outcomes
Eight, five, three, and two studies measured physical activity, sedentary behaviors (i.e., screen time), sleep, and self‐regulation, respectively. Five studies found improvements in child health‐related behaviors. Among them, studies conducted by French et al, Tomayko et al in 2016, and Taverno et al found significantly reduced screen time for children at study timepoints 24 and 36 months, 24 months, and 10 weeks, respectively. 37 , 45 , 46 Nix et al found increased self‐regulation of children as measured by “delay of gratification, task orientation, and emotional and/or behavioral control”. 43 Brown et al identified improved overall child health behaviors related to sleep, physical activity, and TV viewing. 35
3.3.2. Parental outcomes
Feeding practices and styles
Four studies described parental feeding practices or styles‐related outcomes. The study conducted by Hughes et al found improved parental feeding practices, styles, and knowledge. 40 Haines et al found significantly reduced restrictive feeding practices among parents in the intervention group compared to control, Fisher et al saw increased authoritative parenting practices, and Nix et al found more responsive feeding practices. 36 , 38 , 43 These three outcomes have been identified by previous studies as being associated with better child weight status and feeding behaviors. 109 , 110 , 111
Diet‐related outcomes
Three studies included measurements of parental intake, 45 , 46 , 47 and two studies reported statistically significant improvements in parental dietary consumption, as measured by amount of fruits and vegetable intake of parents. 45 , 47
Behavioral outcomes
Six studies described the effects of interventions on parental behavioral changes related to their own health. 36 , 38 , 40 , 41 , 43 , 44 A variety of parental health‐related behaviors were studied. The most frequent statistically significant behavioral outcomes were increased physical activity and self‐efficacy to conquer impediments to physical activity.
4. DISCUSSION
Our study summarizes the recently published literature of a gap identified by the systematic review conducted by Ash et al., namely a paucity of studies evaluating family‐based obesity prevention interventions among preschool‐aged children from racial and/or ethnic minority groups. 29 Our review differs from the systematic review by Ash et al by focusing on preschool‐age children living in the United States as opposed to the global community. 29 Social, environmental, and cultural backgrounds vary between countries and play critical roles in the development of childhood obesity. Given this, and the changing racial and ethnic demographics of children in the United States, it is important to review the evidence of family‐based interventions in the prevention of overweight/obesity in racial and ethnic communities in the United States.
Overall, there was limited research in the field from 2015 to 2021. We identified 14 individual studies, with a majority of the studies published after 2017 (n = 11), suggesting an increased interest in studying health‐promoting interventions for children 2–5 years old who identify as Hispanic/Latinx, American Indian, or Black/African American. The most frequently addressed obesity risk related behaviors were diet (n = 8) and physical activity (n = 8), followed by screen use (n = 5), and sleep (n = 3). Five (35.7%) studies reported statistically significant improvements of behavioral outcomes including screen use (n = 4), sleep (n = 1), and physical activity (n = 1). The lack of interventions targeting all four behavioral domains (n = 2) and a disproportionately focus on diet and physical activity was consistent with the findings of prior work. 29 Half of the 14 studies used child weight‐related measurements as the primary outcome. Only 5 studies (35.7%) found statistically significant change in BMI or BMI percentile results. These results might be due to, relatively brief, non‐intense interventions, or lack of interventions incorporating comprehensive behavioral change strategies. These findings regarding the effectiveness of interventions on behavioral and weight‐related changes were consistent with two recent reviews looking at similar interventions among Hispanic/Latinx children and families. 112 , 113
Looking at culturally tailored components of the reviewed interventions, we found that the most frequently addressed aspects were (1) language barriers, (2) food choices, (3) relationships among family members, and (4) rapport building. None of the 14 interventions included all four components. As obesity prevention efforts are increasingly conducted in diverse populations and communities, it is important to consider how adaptations could be made to increase the cultural relevance and effectiveness of interventions.
Language and food preferences are important factors to consider when developing obesity preventing strategies. Language can be a barrier for non‐English speaking communities and food recommendations need to be consistent with cultural preferences and norms. 114 , 115 Studies included in this review tailored interventions for Spanish‐speaking populations by using frequently suggested strategies, such as developing education materials in Spanish, inviting bilingual facilitators or health coaches to lead group sessions and interviews, investigating dietary cultural practices of target population, and suggesting food choices that are more familiar and culturally congruent with family preference. 116 , 117 It will be important for future curricula/programs to consider the use of different dialects and cultures to accommodate Spanish‐speakers from various regions (i.e., Mainlanders and Caribbeans) and generations (i.e., those who were born and raised in the United States and those who recently arrived). 118
Family structure is another element to be considered when designing interventions targeting minority populations. The concept of “family” and roles of family members can be particularly important among racial and/or ethnic minority groups. For example, in American Indians families, elders are viewed as leaders of the family unit and family decisions are made with needs of the family/clan taking priority. 119 , 120 Among the 14 studies, Tomayko et al incorporated the American Indian model of inheriting life‐skills from the elders into the delivery of their toolkit designed to be used in participant's homes. 46 The combination of the traditional model with a focus on the home environment achieved significant improvements in both child and adult weight‐related behaviors. Included studies also employed various methods to build rapport among participants, such as recruiting “promotoras” (individuals who were trusted from the community of target population), creating educational videos featuring families from diverse cultural background, and adding time for open communication between educators and participants prior to every education session. 42 Leveraging the existing interactions among family members and building rapport could be specifically beneficial for racial and/or ethnic minority participants.
There were two gaps identified by this review. First, none of the interventions developed culturally tailored curriculum/program for Black/African American populations who, like Hispanic/Latinx and American Indians, experience weight‐related health disparities. A previous systematic review examining the effect of culturally adapted interventions for Black/African American women found that 17 of 28 studies saw significant improvements in diet‐ and weight‐related outcomes in treatment over control groups, demonstrating the benefit of incorporating culturally appropriate components into interventions targeting Black/African Americans. 121 More tailored interventions for this population may be important in reducing obesity disparities among children. Second, only 3 of 14 studies included a follow‐up period after the completion of the intervention to evaluate long‐term impact of the intervention on weight status. As a result, it is difficult to evaluate the effectiveness of interventions in preventing obesity at later time points in childhood and adulthood. This gap was also identified by a systematic review examining the impact of childhood obesity prevention interventions targeting children 0–5 years old from socioeconomically disadvantaged backgrounds. 122 Future studies should incorporate longer follow‐up periods (i.e., >12 months) to allow sufficient time to observe the changes of anthropometric outcomes and maintenance of healthy weight behaviors.
A majority of the interventions lasted 12 weeks or less. Only 4 out of the 14 interventions (28.6%) were equal to or more than 12 months. This finding is consistent with prior reviews targeting the same age group. 123 , 124 Some short, but intense, interventions have demonstrated a positive impact on weight/health behaviors. 125 The interventions examined by this review only arranged weekly sessions which could not be categorized as intense, which may contribute to the lack of statistically significant findings. Although longer follow‐up periods translate into greater costs and have higher rates of missing data, it would be constructive in addressing the question of do childhood obesity preventing interventions impact weight status in adolescence and adulthood.
Several limitations of this study are worth noting. First, this review was not intended to be a systematic evidence review to summarize findings across similar but separate studies, limiting the interpretation of the findings; instead, the review focused primarily on a scoping review of study/intervention design and search results to identify intervention gaps, providing guidance and reference for future interventions and research. Secondly, the review targeted only interventions published in 2015 and beyond which was a rather short period of time, weakening the comprehensiveness of this review and disenabling the analysis of time trends. However, this review was conducted with an intention to build on previous work looking at family‐based childhood obesity prevention interventions including a review done in 2015, 29 , 123 and focused on racial and/or ethnic minority groups which had not been independently addressed by prior reviews.
5. CONCLUSION
There is a limited but increasing number of studies examining family‐based interventions studies to prevent obesity among minority preschool children (2–5 years of age) in the United States. Unfortunately, there is a lack of culturally tailored components for each racial and/or ethnic group, especially those targeting Black/African American families. Interventions also focused on addressing nutrition and physical activity as obesity prevention activities and did not address other drivers of obesity such as sleep. Future interventions covering these gaps should be studied to further the evidence for culturally appropriate and efficient means to prevent obesity among high risk minority children.
CONFLICTS OF INTEREST
Authors have no conflicts of interest.
Supporting information
Supporting Information 1
ACKNOWLEDGMENT
I would like to express my special thanks to librarian Emily Paige Jones who instructed on the scoping review procedures and contributed to the revision of search strategies.
Wang X, Ammerman A, Orr CJ. Family‐based interventions for preventing overweight or obesity among preschoolers from racial/ethnic minority groups: a scoping review. Obes Sci Pract. 2022;8(3):371‐386. 10.1002/osp4.578
REFERENCES
- 1. Ogden CL, Fryar CD, Martin CB, et al. Trends in obesity prevalence by race and Hispanic origin—1999‐2000 to 2017‐2018. J Am Med Assoc. 2020;324(12):1208‐1210. 10.1001/jama.2020.14590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta‐regression analysis. Epidemiol Rev. 2007;29(1):6‐28. 10.1093/epirev/mxm007 [DOI] [PubMed] [Google Scholar]
- 3. Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007‐2008 to 2015‐2016. Jama. 2018;319(16):1723‐1725. 10.1001/jama.2018.3060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pan L, McGuire LC, Blanck HM, May‐Murriel AL, Grummer‐Strawn LM. Racial/ethnic differences in obesity trends among young low‐income children. Am J Prev Med. 2015;48(5):570‐574. 10.1016/j.amepre.2014.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Vespa J, Medina L, Armstrong DM. Demographic Turning Points for the United States: Population Projections for 2020 to 2060 Population Estimates and Projections Current Population Reports. US Department of Commerce, Economics and Statistics Administration, US Census Bureau; 2018. Accessed May 30, 2021. www.census.gov/programs-surveys/popproj [Google Scholar]
- 6. Jackson CS, Gracia JN. Addressing health and health‐care disparities: the role of a diverse workforce and the social determinants of health. Public Health Rep. 2014;129(Suppl 2):57‐61. 10.1177/00333549141291S211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Isong IA, Rao SR, Bind M‐A, Avendaño M, Kawachi I, Richmond TK. Racial and ethnic disparities in early childhood obesity. Pediatrics. 2018;141(1):e20170865. 10.1542/peds.2017-0865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Africa JA, Newton KP, Schwimmer JB. Lifestyle interventions including nutrition, exercise, and supplements for nonalcoholic fatty liver disease in children. Dig Dis Sci. 2016;61(5):1375‐1386. 10.1007/s10620-016-4126-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bacha F, Gidding SS. Cardiac abnormalities in youth with obesity and type 2 diabetes. Curr Diabetes Rep. 2016;16(7):1‐9. 10.1007/s11892-016-0750-6 [DOI] [PubMed] [Google Scholar]
- 10. Cote AT, Harris KC, Panagiotopoulos C, Sandor GGS, Devlin AM. Childhood obesity and cardiovascular dysfunction. J Am Coll Cardiol. 2013;62(15):1309‐1319. 10.1016/j.jacc.2013.07.042 [DOI] [PubMed] [Google Scholar]
- 11. Lloyd LJ, Langley‐Evans SC, McMullen S. Childhood obesity and risk of the adult metabolic syndrome: a systematic review. Int J Obes. 2012;36(1):1‐11. 10.1038/ijo.2011.186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mohanan S, Tapp H, McWilliams A, Dulin M. Obesity and asthma: pathophysiology and implications for diagnosis and management in primary care. Exp Biol Med. 2014;239(11):1531‐1540. 10.1177/1535370214525302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Narang I, Mathew JL. Childhood obesity and obstructive sleep apnea. J Nutr Metab. 2012;2012:134202. 10.1155/2012/134202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pollock NK. Childhood obesity, bone development, and cardiometabolic risk factors. Mol Cell Endocrinol. 2015;410:52‐63. 10.1016/j.mce.2015.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Halfon N, Larson K, Slusser W. Associations between obesity and comorbid mental health, developmental, and physical health conditions in a nationally representative sample of us children aged 10 to 17. Acad Pediatr. 2013;13(1):6‐13. 10.1016/j.acap.2012.10.007 [DOI] [PubMed] [Google Scholar]
- 16. Morrison KM, Shin S, Tarnopolsky M, Taylor VH. Association of depression & health related quality of life with body composition in children and youth with obesity. J Affect Disord. 2015;172:18‐23. 10.1016/j.jad.2014.09.014 [DOI] [PubMed] [Google Scholar]
- 17. Sagar R, Gupta T. Psychological aspects of obesity in children and adolescents. Indian J Pediatr. 2018;85(7):554‐559. 10.1007/s12098-017-2539-2 [DOI] [PubMed] [Google Scholar]
- 18. Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. 2009;10(6):204. 10.1056/NEJM199709253371301 [DOI] [PubMed] [Google Scholar]
- 19. Geserick M, Vogel M, Gausche R, et al. Acceleration of BMI in early childhood and risk of sustained obesity. N Engl J Med. 2018;379(14):1303‐1312. 10.1056/nejmoa1803527 [DOI] [PubMed] [Google Scholar]
- 20. Berge JM, Everts JC. Family‐based interventions targeting childhood obesity: a meta‐analysis. Child Obes. 2011;7(2):110‐121. 10.1089/chi.2011.07.02.1004.berge [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jeor STS, Perumean‐Chaney S, Sigman‐Grant M, Williams C, Foreyt J. Family‐based interventions for the treatment of childhood obesity. J Am Diet Assoc. 2002;102(5):640‐644. 10.1016/S0002-8223(02)90146-X [DOI] [PubMed] [Google Scholar]
- 22. Weir K. Family‐based behavioral treatment is key to addressing childhood obesity. Monit Psychol. 2019;50:430. https://www.apa.org/monitor/2019/04/ce-corner-childhood-obesity [Google Scholar]
- 23. Croker H, Viner RM, Nicholls D, et al. Family‐based behavioural treatment of childhood obesity in a UK national health service setting: randomized controlled trial. Int J Obes. 2012;36(1):16‐26. 10.1038/ijo.2011.182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Golley RK, Magarey AM, Baur LA, Steinbeck KS, Daniels LA. Twelve‐month effectiveness of a parent‐led, family‐focused weight‐management program for prepubertal children: a randomized, controlled trial. Pediatrics. 2007;119(3):517‐525. 10.1542/peds.2006-1746 [DOI] [PubMed] [Google Scholar]
- 25. Kalarchian MA, Levine MD, Arslanian SA, et al. Family‐based treatment of severe pediatric obesity: randomized, controlled trial. Pediatrics. 2009;124(4):1060‐1068. 10.1542/peds.2008-3727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sacher PM, Kolotourou M, Chadwick PM, et al. Randomized controlled trial of the MEND program: a family‐based community intervention for childhood obesity. Obesity. 2010;18((Suppl 1)). 10.1038/oby.2009.433 [DOI] [PubMed] [Google Scholar]
- 27. Savoye M, Shaw M, Dziura J, et al. Effects of a weight management program on body composition and metabolic parameters in overweight children: a randomized controlled trial. J Am Med Assoc. 2007;297(24):2697‐2704. 10.1001/jama.297.24.2697 [DOI] [PubMed] [Google Scholar]
- 28. Wasser HM, Thompson AL, Suchindran CM, et al. Family‐based obesity prevention for infants: design of the “Mothers & Others” randomized trial. Contemp Clin Trials. 2017;60:24‐33. 10.1016/j.cct.2017.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ash T, Agaronov A, Young T, Aftosmes‐Tobio A, Davison KK. Family‐based childhood obesity prevention interventions: a systematic review and quantitative content analysis. Int J Behav Nutr Phys Act. 2017;14(1):113. 10.1186/s12966-017-0571-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Carr K, Epstein L. Choice is relative: reinforcing value of food and activity in obesity treatment. Am Psychol. 2020;75(2):139‐151. 10.1037/AMP0000521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Agency for Healthcare Research and Quality . Topic: Racial/Ethnic Minorities. Accessed November 1, 2021. https://www.ahrq.gov/topics/racial-ethnic-minorities.html [Google Scholar]
- 32. Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):1‐7. 10.1186/S12874-018-0611-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sucharew H, Macaluso M. Methods for research evidence synthesis: the scoping review approach. J Hosp Med. 2019;14(7):416‐418. 10.12788/JHM.3248 [DOI] [PubMed] [Google Scholar]
- 34. Barkin SL, Heerman WJ, Sommer EC, et al. Effect of a behavioral intervention for underserved preschool‐age children on change in body mass index: a randomized clinical trial. J Am Med Assoc. 2018;320(5):450‐460. 10.1001/jama.2018.9128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Brown B, Harris K, Dybdal L, Malich J, Bodnar B, Hall E. Feasibility of text messaging to promote child health in a rural community on an American Indian reservation. Health Educ J. 2019;78(5):557‐569. 10.1177/0017896918824624 [DOI] [Google Scholar]
- 36. Fisher JO, Serrano EL, Foster GD, et al. Title: efficacy of a food parenting intervention for mothers with low income to reduce preschooler’s solid fat and added sugar intakes: a randomized controlled trial. Int J Behav Nutr Phys Act. 2019;16(1):6. 10.1186/s12966-018-0764-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. French SA, Sherwood NE, Veblen‐Mortenson S, et al. Multicomponent obesity prevention intervention in low‐income preschoolers: primary and subgroup analyses of the NET‐works randomized clinical trial, 2012‐2017. Am J Public Health. 2018;108(12):1695‐1706. 10.2105/AJPH.2018.304696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Haines J, Rifas‐Shiman SL, Gross D, McDonald J, Kleinman K, Gillman MW. Randomized trial of a prevention intervention that embeds weight‐related messages within a general parenting program. Obes (Silver Spring). 2016;24(1):191‐199. 10.1002/oby.21314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Heerman WJ, Burgess LE, Escarfuller J, et al. Competency Based Approach to Community Health (COACH): the methods of a family‐centered, community‐based, individually adaptive obesity randomized trial for pre‐school child‐parent pairs. Contemp Clin Trials. 2018;73:1‐7. 10.1016/j.cct.2018.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hughes SO, Power TG, Beck A, et al. Short‐term effects of an obesity prevention program among low‐income hispanic families with preschoolers. J Nutr Educ Behav. 2020;52(3):224‐239. 10.1016/j.jneb.2019.12.001 [DOI] [PubMed] [Google Scholar]
- 41. Jastreboff AM, Chaplin TM, Finnie S, et al. Preventing childhood obesity through a mindfulness‐based parent stress intervention: a randomized pilot study. J Pediatr. 2018;202:136‐142. 10.1016/j.jpeds.2018.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Linville D, Mintz B, Martinez C, Gau JM, Shune S, Stice E. Preliminary effects of tailoring an obesity prevention intervention program for latino immigrant families. Fam Community Health. 2020;43(2):118‐130. 10.1097/FCH.0000000000000252 [DOI] [PubMed] [Google Scholar]
- 43. Nix RL, Francis LA, Feinberg ME, et al. Improving toddlers’ healthy eating habits and self‐regulation: a randomized controlled trial. Pediatrics. 2021;147(1):e20193326. 10.1542/peds.2019-3326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Sosa ET, Parra‐Medina D, He M, Trummer V, Yin Z. ¡Miranos! (Look at Us! We are Healthy!): home‐based and parent peer‐led childhood obesity prevention. Health Promot Pract. 2016;17(5):675‐681. 10.1177/1524839915623762 [DOI] [PubMed] [Google Scholar]
- 45. Taverno Ross SE, Barone Gibbs B, Documet PI, Pate RR. ANDALE Pittsburgh: results of a promotora‐led, home‐based intervention to promote a healthy weight in Latino preschool children. BMC Public Health. 2018;18(1):360. 10.1186/s12889-018-5266-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Tomayko EJ, Prince RJ, Cronin KA, Adams AK. The Healthy Children, Strong Families intervention promotes improvements in nutrition, activity and body weight in American Indian families with young children. Public Health Nutr. 2016;19(15):2850‐2859. 10.1017/S1368980016001014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Tomayko EJ, Prince RJ, Cronin KA, Kim K, Parker T, Adams AK. The Healthy Children, Strong Families 2 (HCSF2) randomized controlled trial improved healthy behaviors in American Indian families with young children. Curr Dev Nutr. 2019;3(Suppl 2):53‐62. 10.1093/cdn/nzy087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Prentice‐Hall, Inc.; 1986. Accessed May 11, 2021. https://psycnet.apa.org/record/1985-98423-000 [Google Scholar]
- 49. Ryan RM, Deci EL. Self‐determination theory and the facilitation of intrinsic motivation, social development, and well‐being. Am Psychol. 2000;55(1):68‐78. 10.1037//0003-066x.55.1.68 [DOI] [PubMed] [Google Scholar]
- 50. Kabat‐Zinn J. Mindfulness‐Based Stress Reduction Curriculum. Center for Mindfulness in Medicine, Health Care, and Society; 2009. [Google Scholar]
- 51. Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well‐being. J Pers Soc Psychol. 2003;84(4):822‐848. 10.1037/0022-3514.84.4.822 [DOI] [PubMed] [Google Scholar]
- 52. Haines PS, Siega‐Riz AM, Popkin BM. The Diet Quality Index Revised: a measurement instrument for populations. J Am Diet Assoc. 1999;99(6):697‐704. 10.1016/S0002-8223(99)00168-6 [DOI] [PubMed] [Google Scholar]
- 53. Francis LA, Birch LL. Maternal influences on daughters’ restrained eating behavior. Heal Psychol. 2005;24(6):548‐554. 10.1037/0278-6133.24.6.548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Coatsworth J, Duncan L, Greenberg M, Nix R. Changing parent’s mindfulness, child management skills and relationship quality with their youth: results from a randomized pilot intervention trial. J Child Fam Stud. 2010;19(2):203‐217. 10.1007/S10826-009-9304-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Chaplin TM, Fahy T, Sinha R, Mayes LC. Emotional arousal in cocaine exposed toddlers: prediction of behavior problems. Neurotoxicol Teratol. 2009;31(5):275‐282. 10.1016/j.ntt.2009.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Sorensen G, Emmons K, Hunt MK, et al. Model for incorporating social context in health behavior interventions: applications for cancer prevention for working‐class, multiethnic populations. Prev Med (Baltim). 2003;37(3):188‐197. 10.1016/S0091-7435(03)00111-7 [DOI] [PubMed] [Google Scholar]
- 57. Blum RE, Wei EK, Rockett HR, et al. Validation of a food frequency questionnaire in Native American and Caucasian children 1 to 5 years of age. Matern Child Health J. 1999;3(3):167‐172. 10.1023/A:1022350023163 [DOI] [PubMed] [Google Scholar]
- 58. Baker PC, Keck CK, Mott FLQS. NLYS Child Handbook, Revised Edition: A Guide to the 1986–90 National Longitudinal Survey of Children and Youth Child Data. 1993. https://eric.ed.gov/?id=ED373860 [Google Scholar]
- 59. Birch LL, Fisher JO, Grimm‐Thomas K, Markey CN, Sawyer R, Johnson SL. Confirmatory factor analysis of the Child Feeding Questionnaire: a measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite. 2001;36(3):201‐210. 10.1006/appe.2001.0398 [DOI] [PubMed] [Google Scholar]
- 60. McCabe KM, Clark R, Barnett D. Family protective factors among urban African American youth. J Clin Child Adolesc Psychol. 1999;28(2):137‐150. 10.1207/s15374424jccp2802_2 [DOI] [PubMed] [Google Scholar]
- 61. Gross D, Rocissano L. Maternal confidence in toddlerhood: its measurement for clinical practice and research. Nurse Pract. 1988;13(3):19‐31. 10.1097/00006205-198803000-00004 [DOI] [PubMed] [Google Scholar]
- 62. Bronfenbrenner U. Ecology of the family as a context for human development: research perspectives. Dev Psychol. 1986;22(6):723‐742. 10.1037/0012-1649.22.6.723 [DOI] [Google Scholar]
- 63. Gulliford MC, Mahabir D, Rocke B. Reliability and validity of a short form household food security scale in a Caribbean community. BMC Public Health. 2004;4:1‐9. 10.1186/1471-2458-4-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Shloim N, Edelson LR, Martin N, Hetherington MM. Parenting styles, feeding styles, feeding practices, and weight status in 4‐12 year‐old children: a systematic review of the literature. Front Psychol. 2015;6:1849. 10.3389/fpsyg.2015.01849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Vaughn AE, Ward DS, Fisher JO, et al. Fundamental constructs in food parenting practices: a content map to guide future research. Nutr Rev. 2016;74(2):98‐117. 10.1093/nutrit/nuv061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Harvard University Press; 1979. Accessed June 6, 2021. https://www.hup.harvard.edu/catalog.php?isbn=9780674224575&content=reviews [Google Scholar]
- 67. Neumark‐Sztainer D, MacLehose R, Loth K, Fulkerson JA, Eisenberg ME, Berge J. What’s for dinner? Types of food served at family dinner differ across parent and family characteristics. Public Health Nutr. 2014;17(1):145‐155. 10.1017/S1368980012004594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Hunsberger M, O’Malley J, Block T, Norris JC. Relative validation of Block Kids Food Screener for dietary assessment in children and adolescents. Matern Child Nutr. 2015;11(2):260‐270. 10.1111/j.1740-8709.2012.00446.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Dennison BA, Erb TA, Jenkins PL. Television viewing and television in bedroom associated with overweight risk among low‐income preschool children. Pediatrics. 2002;109(6):1028‐1035. 10.1542/peds.109.6.1028 [DOI] [PubMed] [Google Scholar]
- 70. Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med (Baltim). 1987;16(6):825‐836. 10.1016/0091-7435(87)90022-3 [DOI] [PubMed] [Google Scholar]
- 71. Stephens JW, Thacker SB, Shaw FE, et al. Morbidity and Mortality Weekly Report Editorial and Production Staff; 2009. Accessed June 6, 2021. www.cdc.gov/mmwr [Google Scholar]
- 72. Larios SE, Ayala GX, Arredondo EM, Baquero B, Elder JP. Development and validation of a scale to measure Latino parenting strategies related to children’s obesogenic behaviors. The parenting strategies for eating and activity scale (PEAS). Appetite. 2009;52(1):166‐172. 10.1016/j.appet.2008.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Song MK, Carroll DD, Lee SM, Fulton JE. Physical activities of U.S. High school students‐‐2010 National Youth Physical activity and Nutrition Survey. J Phys Act Health. 2015;12:S11‐S17. 10.1123/jpah.2014-0117 [DOI] [PubMed] [Google Scholar]
- 74. Sallis JF, Taylor WC, Dowda M, Freedson PS, Pate RR. Correlates of vigorous physical activity for children in grades 1 through 12: comparing parent‐reported and objectively measured physical activity. Pediatr Exerc Sci. 2002;14(1):30‐44. 10.1123/PES.14.1.30 [DOI] [Google Scholar]
- 75. Power TG, Johnson SL, Beck AD, Martinez AMD, Hughes SO. The Food Parenting Inventory: factor structure, reliability, and validity in a low‐income, Latina sample. Appetite. 2019;134:111‐119. 10.1016/j.appet.2018.11.033 [DOI] [PubMed] [Google Scholar]
- 76. Fiese BH, Kline CA. Development of the Family Ritual Questionnaire: initial reliability and validation studies. J Fam Psychol. 1993;6(3):290‐299. 10.1037/0893-3200.6.3.290 [DOI] [Google Scholar]
- 77. Hughes SO, Anderson CB, Power TG, Micheli N, Jaramillo S, Nicklas TA. Measuring feeding in low‐income African‐American and Hispanic parents. Appetite. 2006;46(2):215‐223. 10.1016/j.appet.2006.01.002 [DOI] [PubMed] [Google Scholar]
- 78. Johnson SL, Birch LL. Parents’ and children’s adiposity and eating style. Pediatrics. 1994;94(5):653‐661. [PubMed] [Google Scholar]
- 79. Sullivan SA, Birch LL. Pass the sugar, pass the salt: experience dictates preference. Dev Psychol. 1990;26(4):546‐551. 10.1037/0012-1649.26.4.546 [DOI] [Google Scholar]
- 80. Skinner JD, Carruth BR, Bounds W, Ziegler PJ. Children’s food preferences: a longitudinal analysis. J Am Diet Assoc. 2002;102(11):1638‐1647. 10.1016/S0002-8223(02)90349-4 [DOI] [PubMed] [Google Scholar]
- 81. Fisher JO, Birch LL. Restricting access to foods and children’s eating. Appetite. 1999;32(3):405‐419. 10.1006/appe.1999.0231 [DOI] [PubMed] [Google Scholar]
- 82. Festinger L. A Theory of Cognitive Dissonance. Stanford University Press; 1957. Accessed June 6, 2021. https://psycnet.apa.org/record/1993-97948-000 [Google Scholar]
- 83. Becvar RJ, Becvar DS. Systems Theory and Family Therapy: A Primer. University Press of America; 1982. [Google Scholar]
- 84. Bacon L, Aphramor L. Weight science: evaluating the evidence for a paradigm shift. Nutr J. 2011;10(1):1‐13. 10.1186/1475-2891-10-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Block G, Hartman AM, Naughton D. A reduced dietary questionnaire: development and validation. Epidemiology. 1990;1(1):58‐64. 10.1097/00001648-199001000-00013 [DOI] [PubMed] [Google Scholar]
- 86. Sallis JF, Haskell WL, Wood PD, et al. Physical activity assessment methodology in the five‐city project. Am J Epidemiol. 1985;121(1):91‐106. 10.1093/oxfordjournals.aje.a113987 [DOI] [PubMed] [Google Scholar]
- 87. Ware JE, Kosinski M, Keller SD. A 12‐item short‐form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220‐233. 10.1097/00005650-199603000-00003 [DOI] [PubMed] [Google Scholar]
- 88. Katula JA, Vitolins MZ, Morgan TM, et al. The healthy living partnerships to prevent diabetes study: 2‐year outcomes of a randomized controlled trial. Am J Prev Med. 2013;44(4 Suppl):S324‐S332. 10.1016/j.amepre.2012.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Eaton DK, Olsen EOM, Brener ND, et al. A comparison of fruit and vegetable intake estimates from three survey question sets to estimates from 24‐hour dietary recall interviews. J Acad Nutr Diet. 2013;113(9):1165‐1174. 10.1016/j.jand.2013.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Amireault S, Godin G. The Godin‐shepherd leisure‐time physical activity questionnaire: validity evidence supporting its use for classifying healthy adults into active and insufficiently active categories. Percept Mot Skills. 2015;120(2):604‐622. 10.2466/03.27.PMS.120v19x7 [DOI] [PubMed] [Google Scholar]
- 91. Janz KF, Broffitt B, Levy SM. Validation evidence for the Netherlands physical activity questionnaire for young children: the Iowa bone development study. Res Q Exerc Sport. 2005;76(3):363‐369. 10.1080/02701367.2005.10599308 [DOI] [PubMed] [Google Scholar]
- 92. Ihmels MA, Welk GJ, Eisenmann JC, Nusser SM. Development and preliminary validation of a Family Nutrition and Physical activity (FNPA) screening tool. Int J Behav Nutr Phys Act. 2009;6(1):1‐10. 10.1186/1479-5868-6-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Latimer L, Walker LO, Kim S, Pasch KE, Sterling BS. Self‐efficacy scale for weight loss among multi‐ethnic women of lower income: a psychometric evaluation. J Nutr Educ Behav. 2011;43(4):279‐283. 10.1016/j.jneb.2010.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385‐396. 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- 95. Goins RT, Spencer SM, McGuire LC, Goldberg J, Wen Y, Henderson JA. Adult caregiving among American Indians: the role of cultural factors. Gerontologist. 2011;51(3):310‐320. 10.1093/geront/gnq101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Hager ER, Quigg AM, Black MM, et al. Development and validity of a 2‐item screen to identify families at risk for food insecurity. Pediatrics. 2010;126(1):e26‐e32. 10.1542/peds.2009-3146 [DOI] [PubMed] [Google Scholar]
- 97. Maine Department of Education and Maine Department of Health and Human Services. Maine Integrated Youth Health Survey; 2014. Accessed July 7, 2021. https://www.maine.gov/miyhs/ [Google Scholar]
- 98. Mills SD, Malcarne VL, Fox RS, Sadler GR. Psychometric evaluation of the brief acculturation scale for hispanics. Hisp J Behav Sci. 2014;36(2):164‐174. 10.1177/0739986314526697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Ziegler P, Briefel R, Clusen N, Devaney B. Feeding Infants and Toddlers Study (FITS): development of the FITS survey in comparison to other dietary survey methods. J Am Diet Assoc. 2006;106(1 Suppl):12.e1‐12.e50. 10.1016/j.jada.2005.09.033 [DOI] [PubMed] [Google Scholar]
- 100. Centers for Disease Control and Prevention . Behavioral Risk Factor Surveillance System. www.cdc.gov/brfss/index.htm [Google Scholar]
- 101. Heerman WJ, Jackson N, Hargreaves M, et al. Clusters of healthy and unhealthy eating behaviors are associated with body mass index among adults. J Nutr Educ Behav. 2017;49(5):415‐421. 10.1016/j.jneb.2017.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Wright JA, Adams WG, Laforge RG, Berry D, Friedman RH. Assessing parental self‐efficacy for obesity prevention related behaviors. Int J Behav Nutr Phys Act. 2014;11(1):1‐9. 10.1186/1479-5868-11-53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. O’Connor TM, Cerin E, Hughes SO, et al. Psychometrics of the preschooler physical activity parenting practices instrument among a Latino sample. Int J Behav Nutr Phys Act. 2014;11(1):1‐14. 10.1186/1479-5868-11-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Stokols D. Establishing and maintaining healthy environments: toward a social ecology of health promotion. Am Psychol. 1992;47(1):6‐22. 10.1037//0003-066x.47.1.6 [DOI] [PubMed] [Google Scholar]
- 105. Kochanska G, Murray KT, Harlan ET. Effortful control in early childhood: continuity and change, antecedents, and implications for social development. Dev Psychol. 2000;36(2):220‐232. [PubMed] [Google Scholar]
- 106. Balasundaram P, Avulakunta ID. Bayley Scales of Infant and Toddler Development. StatPearls Publishing; 2021. Accessed June 6, 2021. http://www.ncbi.nlm.nih.gov/pubmed/33620792 [PubMed] [Google Scholar]
- 107. Carter AS, Briggs‐Gowan MJ, Jones SM, Little TD. The Infant‐Toddler Social and Emotional Assessment (ITSEA): factor structure, reliability, and validity. J Abnorm Child Psychol. 2003;31(5):495‐514. 10.1023/A:1025449031360 [DOI] [PubMed] [Google Scholar]
- 108. Trude ACB, Kharmats A, Jock B, et al. Patterns of food consumption are associated with obesity, self‐reported diabetes and cardiovascular disease in five american Indian communities. Ecol Food Nutr. 2015;54(5):437‐454. 10.1080/03670244.2014.922070 [DOI] [PubMed] [Google Scholar]
- 109. Sokol RL, Qin B, Poti JM. Parenting styles and body mass index: a systematic review of prospective studies among children. Obes Rev. 2017;18(3):281‐292. 10.1111/OBR.12497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Rodgers RF, Paxton SJ, Massey R, et al. Maternal feeding practices predict weight gain and obesogenic eating behaviors in young children: a prospective study. Int J Behav Nutr Phys Act. 2013;10(1):1‐10. 10.1186/1479-5868-10-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Spill M, Callahan E, Shapiro M, et al. Caregiver feeding practices and child weight outcomes: a systematic review. Am J Clin Nutr. 2019;109(Suppl_7):990S‐1002S. 10.1093/AJCN/NQY276 [DOI] [PubMed] [Google Scholar]
- 112. Soltero EG, Peña A, Gonzalez V, et al. Family‐based obesity prevention interventions among hispanic children and families: a scoping review. Nutr. 2021;13(8):2690. 10.3390/NU13082690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Tamayo M, Dobbs P, Pincu Y. Family‐centered interventions for treatment and prevention of childhood obesity in hispanic families: a systematic review. J Community Health. 2021;46(3):635‐643. 10.1007/S10900-020-00897-7 [DOI] [PubMed] [Google Scholar]
- 114. Timmins C. The impact of language barriers on the health care of Latinos in the United States: a review of the literature and guidelines for practice. J Midwifery Womens Health. 2002;47(2):80‐96. 10.1016/S1526-9523(02)00218-0 [DOI] [PubMed] [Google Scholar]
- 115. Lindberg NM, Stevens VJ, Halperin RO. Weight‐loss interventions for Hispanic populations: the role of culture. J Obes. 2013;2013:542736‐6. 10.1155/2013/542736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Branscum P, Sharma M. A systematic analysis of childhood obesity prevention interventions targeting Hispanic children: lessons learned from the previous decade. Obes Rev. 2011;12(5):e151‐e158. 10.1111/J.1467-789X.2010.00809.X [DOI] [PubMed] [Google Scholar]
- 117. Pérez‐Morales M, Bacardí‐Gascón M, Jiménez‐Cruz A. Childhood overweight and obesity prevention interventions among Hispanic children in the United States: systematic review. Nutr Hosp. 2012;27(5):1415‐1421. 10.3305/NH.2012.27.5.5973 [DOI] [PubMed] [Google Scholar]
- 118. Otheguy R, Zentella AC, Livert D. Language and dialect contact in Spanish in New York: toward the formation of a speech community. Lang (Baltim). 2007;83(4):770‐802. 10.1353/LAN.2008.0019 [DOI] [Google Scholar]
- 119. Jumper‐Reeves L, Dustman PA, Harthun ML, Kulis S, Brown EF. American Indian cultures: how CBPR illuminated intertribal cultural elements fundamental to an adaptation effort. Prev Sci. 2014;15(4):547‐556. 10.1007/s11121-012-0361-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Parra‐Medina D, Messias DAKH. Promotion of physical activity among Mexican‐origin women in Texas and South Carolina: an examination of social, cultural, economic, and environmental factors. Quest. 2011;63(1):100‐117. 10.1080/00336297.2011.10483668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Kong A, Tussing‐Humphreys LM, Odoms‐Young AM, Stolley MR, Fitzgibbon ML. Systematic review of behavioural interventions with culturally adapted strategies to improve diet and weight outcomes in African American women. Obes Rev. 2014;15(0 4):62‐92. 10.1111/obr.12203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Laws R, Campbell KJ, van der Pligt P, et al. The impact of interventions to prevent obesity or improve obesity related behaviours in children (0–5 years) from socioeconomically disadvantaged and/or indigenous families: a systematic review. BMC Public Health. 2014;14(1):1‐18. 10.1186/1471-2458-14-779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Landgren K, Quaye AA, Hallström E, Tiberg I. Family‐based prevention of overweight and obesity in children aged 2–6 years: a systematic review and narrative analysis of randomized controlled trials. Child Adolesc Obes. 2020;3(1):57‐104. 10.1080/2574254x.2020.1752596 [DOI] [Google Scholar]
- 124. Yavuz H, van Ijzendoorn M, Mesman J, van der Veek S. Interventions aimed at reducing obesity in early childhood: a meta‐analysis of programs that involve parents. J Child Psychol Psychiatry. 2015;56(6):677‐692. 10.1111/JCPP.12330 [DOI] [PubMed] [Google Scholar]
- 125. Stice E, Shaw H, Marti CN. A meta‐analytic review of obesity prevention programs for children and adolescents: the skinny on interventions that work. Psychol Bull. 2006;132(5):667‐691. 10.1037/0033-2909.132.5.667 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information 1


