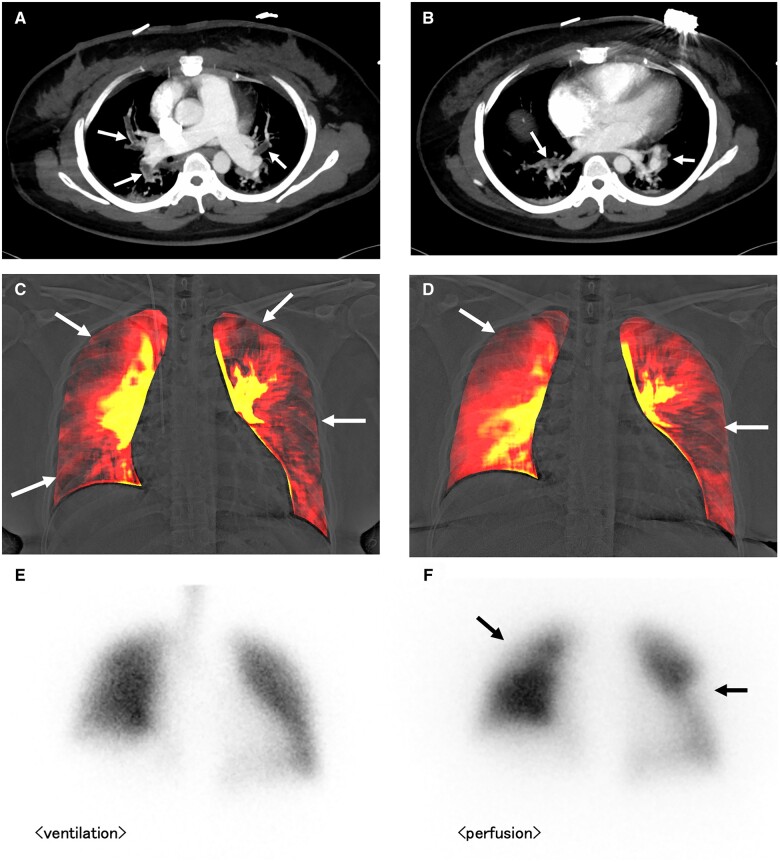
A 32-year-old woman on oral antipsychotics suddenly presented with cardiopulmonary arrest following acute dyspnoea and syncope. She recovered her spontaneous circulation after cardiopulmonary resuscitation in-ambulance during transit to a hospital. The patient was diagnosed with acute massive pulmonary thromboembolism (PTE) based on clinical presentation, elevated D-dimer level (9.5 μg/mL), and contrast-enhanced computed tomography findings (thrombi mainly located in the centres of the pulmonary arteries; PanelsA and B, arrows) in another hospital, and was referred to our hospital due to residual haemodynamic instability. Thrombolytic, catecholamine, and oxygen therapies were initiated immediately. Transthoracic echocardiography demonstrated right ventricular dilatation and left-sided deviation of the interventricular septum (parasternal short-axis view, Supplementary data online, Video S1). Dynamic chest radiography (DCR) was performed on Day 3 of hospitalization, revealing multiple triangular perfusion defects in bilateral lung fields (PanelC, Supplementary data online, Video S2). After gradual improvement, the patient was discharged on oral anticoagulants. The patient’s D-dimer level had normalized as of the time of discharge. However, she suffered from mild-effort dyspnoea even after 6 months; progression to chronic thromboembolic pulmonary hypertension (CTEPH) was suspected. Transthoracic echocardiography showed mild dilatation of right ventricle (parasternal short-axis view, Supplementary data online, Video S3). Repeat DCR demonstrated persistent large perfusion defects in bilateral lung fields (PanelD, Supplementary data online, Video S4), and it was very similar to the findings of the subsequently performed ventilation/perfusion (V/Q) scintigraphy (V/Q mismatch; PanelsE and F, arrows). Following re-admission, pulmonary hypertension was proven by invasive right heart catheterization (mean pulmonary arterial pressure 26 mmHg, pulmonary arterial wedge pressure 13 mmHg, Cardiac output 4.3 L/min, pulmonary vascular resistance 3.0 wu), and the diagnosis of CTEPH was confirmed.
CTEPH is a relatively rare but serious complication after acute PTE. Although V/Q scintigraphy is recommended to detect residual perfusion abnormalities, it is not frequently used. DCR is a novel cineradiography technique using a flat-panel detector and a pulsed X-ray generator that shows pulmonary perfusion from temporal change in X-ray attenuation without any contrast media or radionuclide. The radiation exposure is much lower than that for V/Q and computed tomography scans. Moreover, it can be performed efficiently in outpatient settings. Conversely, the patient’s inability to keep still or to hold his or her breath for 7–10 s could lower the accuracy of the study. This is the first report that shows DCR-based detection of progression of acute PTE to CTEPH.
Supplementary data are available at European Heart Journal - Cardiovascular Imaging online.
Supplementary Material
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing and Takenori Fukumoto (KONICAMNOLTA, Japan) for technical support in image creation.
Funding
This work was supported by the research grant from KONICAMINOLTA, the Japan Society for the Promotion of Science (JSPS) KAKENHI (20K16728), and Konica Minolta Imaging Science Encouragement Award from Konica Minolta Science and Technology Foundation.
Conflict of interest: Y.Y., K.A., and K.I. received a research grant from Konica Minolta, Inc.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.