Abstract
The increasing rates of antimicrobial resistance have demanded the development of new drugs as conventional antibiotics have become significantly less effective. Evidence has identified a variety of phytocompounds with the potential to be used in the combat of infections caused by multidrug-resistant (MDR) bacteria. Considering the verification that terpenes are promising antibacterial compounds, the present research aimed to evaluate the antibacterial and antibiotic-modulating activity of (+)-α-pinene and (-)-borneol against MDR bacterial strains. The broth microdilution method was used to determine the minimum inhibitory concentration (MIC) of the compounds and antibiotics and further evaluate the intrinsic and associated antibiotic activity. These analyses revealed that (+)-α-pinene showed significant antibacterial activity only against E. coli (MIC = 512 μg.mL−1), while no significant inhibition of S. aureus and P. aeruginosa growth was observed (MIC ≥ 1024 μg mL−1). However, when combined with antibiotics, this compound induced a significant improvement in the activity of conventional antibiotics, as observed for ciprofloxacin, amikacin, and gentamicin against Staphylococcus aureus, as well as for amikacin and gentamicin against Escherichia coli, and amikacin against Pseudomonas aeruginosa. On the other hand, (-)-borneol was found to inhibit the growth of E. coli and enhance the antibiotic activity of ciprofloxacin and gentamicin against S. aureus. The present findings indicate that (+)-α-pinene and (-)-borneol are phytocompounds with the potential to be used in the combat of antibacterial resistance.
1. Introduction
In the last decades, the treatment of infections has been threatened by the emergence and spread of an increasing variety of pathogens developing resistance mechanisms against antimicrobial drugs. Antimicrobial resistance occurs when microorganisms such as bacteria, viruses, fungi, and parasites present modifications to evade the action of antimicrobial drugs, resulting in increased rates of transmission, morbidity, and mortality [1].
Consistent evidence has indicated that the antibiotic resistance process has been accelerated in recent years due to the inadequate and uncontrolled use of these drugs, which represents an issue of significant concern for future generations [2].
In order to reduce the irrational use of antimicrobials, the Brazilian Health Regulatory Agency (ANVISA) has published a resolution [3] to regulate and control the use of antimicrobials drugs so that, either alone or in association, they should be sold exclusively under prescription.
In response to the bacterial resistance threat, researchers have made significant efforts to isolate and identify new compounds with antibacterial properties [4], as conventional antibiotics have become significantly less effective [5]. In this context, the development of studies using plant-derived natural products has been pointed as a promising strategy to accelerate and cheapen the production of novel antibacterial compounds [6].
In fact, the use of medicinal plants for therapeutic purposes is an ancient practice. Currently, it is well-established that the therapeutic properties of medicinal species are due to the presence of secondary metabolites [7] which, besides playing critical physiological roles, can interfere with pharmacological targets in human beings and many other species. Therefore, medicinal plants are relevant sources of new molecules with the potential to be used in drug development [8, 9].
However, the development of new antibiotics is limited by the high cost of the process and the restrictions on profits compared to other drugs. In addition, the clinical benefits of antibiotics can decrease over time, so their use needs to be restricted to prevent antibacterial resistance [10].
Terpenes are a class of lipophilic hydrocarbon compounds composed of isoprene units. Such physicochemical characteristic favors their interaction with the lipid bilayer of cell membranes. Consequently, terpenoids can induce significant changes in the structure of membrane components in different microorganisms [11–13].
Pinene (C10H16) is a bicyclic, double-bonded terpenoid hydrocarbon compound [14]. The compound α-pinene is found in nature in essential oils (EO) approximately 40 different essential oils. It is among the best-known representatives of an extensive family of monoterpenes. This compound has two enantiomers (+) and (-), which are commercially available and have proven pharmacological activities, among which their antimicrobial properties stand out [15, 16]. Additionally, these isomers present a number of applications, especially in the composition of flavors and fragrances [17] and in the composition of medicines for the treatment of renal and hepatic diseases [18]. Importantly, it has been postulated that the antibacterial properties of α- and β-pinene are due to their toxic effects on the cell membrane [19].
Borneol is a monoterpene identified in the essential oils of several medicinal plants. It is classified as a bicyclic monoterpenoid alcohol that exists as the D and L enantiomers. This compound has been used in the treatment of gastrointestinal diseases in traditional medicine in China and India [9]. A large number of borneol derivatives have been both designed and synthesized, demonstrating significant activity against Streptococcus sanguinis, Staphylococcus aureus, Escherichia coli, Pseudomonas aeruginosa, and Candida albicans. Among them, the bornyl 3′,4′-dimethoxybenzoate derivative stood out for its strong activity against several pathogens [20].
Recent research identified a number of pharmacological activities for borneol including neuroprotective [21], analgesic [22, 23], muscle relaxing [24], anti-inflammatory [25], antitumor [26], antiasthmatic [27], and anxiolytic [28]. In addition, due to its antiadhesive antimicrobial properties, borneol has potential applications in multifunctional textiles and healthcare [29].
Consistent evidence has indicated that the effectiveness of combined drugs against microorganisms can be greater than that of isolated antibiotics, which has long been observed from studies analyzing the synergism between natural products and conventional antibiotics [30].
Therefore, considering the verification that terpenes are promising antibacterial compounds, the present research aimed to evaluate the antibacterial and antibiotic-modulating activity of (+)-α-pinene and (-)-borneol against MDR bacterial strains.
2. Materials and Methods
2.1. Bacterial Cultures
The standard bacteria used in the tests were obtained from the American Type Culture Collection, clinical isolates were obtained from the University Hospital of the Federal University of Paraíba, and both were stored under refrigeration (8°C) in slanted test tubes containing heart infusion agar (Heart Infusion Agar-HIA, Difco, USA). The standard bacterial strains Escherichia coli ATCC 2592, Staphylococcus aureus ATCC 25923, Pseudomonas aeruginosa ATCC 9027, and multiresistant isolates of E. coli 06, S. aureus 10, and P. aeruginosa 24 were used in the antibacterial tests. All experimental protocols were carried out at the Laboratory of Microbiology and Molecular Biology (LMMB) of the Regional University of Cariri (URCA). Antibiotic susceptibility testing (Table 1) was performed by Kirby-Bauer's disk diffusion method on Muller-Hinton agar (Hi Media, Mumbai, India) in accordance with the standards of the Clinical Laboratory Standards Institute (CLSI) [31].
Table 1.
Resistant profile of the strains.
| Bacteria | Origin | Resistance profile |
|---|---|---|
| Staphylococcus aureus 10 | Rectal swab | Amc, Amox, Amp, Asb, Azi, Ca, Cef, Cf, Cip, Cla, Clin, Eri, Lev, Mox, Oxa, Pen |
| Pseudomonas aeruginosa 24 | Nasal discharge | Ami, Cip, Cpm, Ctz, Imi, Lev, Mer, Ptz |
| Escherichia coli 06 | Urine culture | Asb, Ca, Cef, Cfo, Cmp, Cro |
Subtitle: Amc: amoxicillin + clavulanic acid (20/10 μg); Ami: amikacin (30 μg); Amox: amoxicillin (20 μg); Amp: ampicillin (10 μg); Asb: ampicillin + sulbactam (10/10 μg); Azi: azithromycin (15 μg); Ca: cefadroxil (30 μg); Cef: cephalexin (30 μg); Cfo: cefoxitin (30 μg); Cip: ciprofloxacin (5 μg); Cla: clarithromycin (15 μg); Clin: clindamycin (2 μg); Cmp: cefepime (30 μg); Cro: ceftriaxone (30 μg); Ctz: ceftazidime (30 μg); Eri: erythromycin (15 μg); Imi: imipenem (10 μg); Lev: levofloxacin (5 μg); Mer: meropenem (10 μg); Mox: moxifloxacin (5 μg); Oxa: oxacillin (1 μg); Pen: penicillin (30 μg); Ptz: piperacillin (100 μg) [40].
2.2. Drugs and Reagents
The compounds (+)-α-pinene and (-)-borneol were weighed and 10 mg of each substance was diluted in 1 mL of dimethyl sulfoxide (DMSO, purity = 99.9%) and sterile distilled water until reaching a concentration of 1,024 μg/mL. Resazurin, sodium salt (Sigma-Aldrich, St. Louis, MO, USA) was used as a colorimetric indicator of bacterial growth through the oxidation-reduction method [32, 33].
The test substances were prepared as previously described in the literature [34, 35]. The antibiotics, trimethoprim/sulfamethoxazole, metronidazole, ciprofloxacin, clindamycin, amikacin, and gentamicin, were dissolved and diluted in sterile water to 1,024 μg/mL.
2.3. Strains
Bacterial culture samples were seeded in Petri dishes containing solid heart infusion agar (HIA) medium and stored at 37°C for growth for 24 h. Then, an aliquot of the microbial culture was removed with an inoculation loop and transferred to test tubes containing sterile saline solution (0.9%). The turbidity of the inoculum was compared to the McFarland scale corresponding to 1 × 108 CFU. This test was carried out in triplicate.
2.4. Determination of Minimum Inhibitory Concentration (MIC)
The minimum inhibitory concentration (MIC) was defined as the lowest concentration capable of preventing bacterial growth in the microdilution plate wells as detected macroscopically [31]. The MIC was determined using standard nonresistant bacterial strains. To this end, each strain was cultured in three Petri dishes containing HIA. After 24 h, an aliquot of each plate was collected to obtain an inoculum with a final concentration of 105 CFU. Test tubes were filled with 1350 μL of 10% brain heart infusion (BHI) + 150 μL of inoculum. Then, 100 μL of this solution was distributed in each well of 96-well plates. Then, 100 μL of each monoterpene was added to the first well, and a serial dilution was performed in each column of the plate to achieve concentrations ranging from 512 μg/ml to 0.5 μg/ml. The plates were then placed in an incubator for 24 h at 37°C, followed by the addition of 20 μl of resazurin to each well. After 1 h, the reading was carried out by ocular observation of the solution color, so that a change from blue to red or purple was used as an indication of bacterial growth. Of note, according to Houghton et al. [36], a natural product with an effective concentration higher than 1 mg/mL cannot be considered clinically relevant due to the impossibility of achieving adequate plasma concentrations.
2.5. Modulation Antibiotic Activity by Direct Contact
The method proposed by Coutinho et al. [37] was used in the analysis of antibiotic activity modulation against MDR isolates. Briefly, the bacterial inoculum was prepared in BHI as described above, and the compounds were added at a subinhibitory concentration (equivalent to its MIC÷8). The wells in a 96-well plate were filled with 100 μL of this solution, followed by the addition of 100 μL of each antibiotic at concentrations ranging from 512 to 0.5 μg/mL. The MIC of each drug in the presence or absence of the natural product was determined, and the occurrence of synergism was interpreted as increased antibiotic activity. Experimental controls and readings were performed as previously described.
2.6. Statistical Analysis
The data were analyzed through the statistical program GraphPad Prism version 7.0. The analysis was performed by two-way ANOVA, using the geometric average of the triplicates as the central data and the standard deviation of the average. A Bonferroni post hoc test was then performed, and a p < 0.05 was considered significant.
3. Results
As shown in Table 2, both (+)-α-pinene and (-)-borneol presented a MIC of 512 μg/mL against the ATCC strain of E. coli, while MICs ≥ 1024 μg/mL were obtained against S. aureus and P. aeruginosa. Therefore, both compounds were found to present significant antibacterial effects only against E. coli.
Table 2.
Minimum inhibitory concentration of (+)-α-pinene and (-)-borneol.
| Microorganisms | MIC | |
|---|---|---|
| (+)-α-Pinene | (-)-Borneol | |
| E. coli | 512 μg/mL | 512 μg/mL |
| S. aureus | ≥1024 μg/mL | ≥1024 μg/mL |
| P. aeruginosa | ≥1024 μg/mL | ≥1024 μg/mL |
To evaluate the potentiation of antibiotic activity, we investigated the ability of the natural products to reduce the antibiotic MIC. Figure 1 shows that the MIC of ciprofloxacin against S. aureus was reduced from 101.5 μg/mL to 80.6 μg/mL when associated with (+)-α-pinene. The results were even more expressive with the drugs amikacin and gentamicin whose MIC was reduced by 90% and 92%, respectively, against the same strain. On the other hand, the association of (+)-α-pinene with the trimethoprim/sulfamethoxazole, metronidazole, and clindamycin had no significant impact on their MIC, indicating an absence of antibiotic activity modulation.
Figure 1.
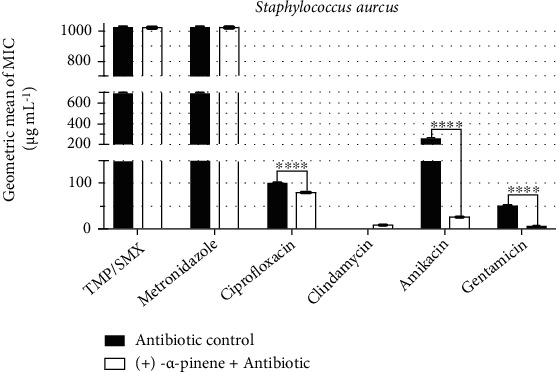
Antibiotic-modulating activity of (+)-α-pinene associated with antibiotics against S. aureus. TMP/SMX: trimethoprim/sulfamethoxazole. p < 0.0001 = ∗∗∗∗.
The analysis of antibiotic-enhancing activity of (-)-borneol in S. aureus cultures (Figure 2) demonstrated that its association with ciprofloxacin caused a reduction of 37% in the antibiotic MIC. In addition, the association with gentamicin, reduced the antibiotic MIC by 75%, changing from 32 μg/mL to 8 μg/mL, indicating potentiated antibiotic activity.
Figure 2.
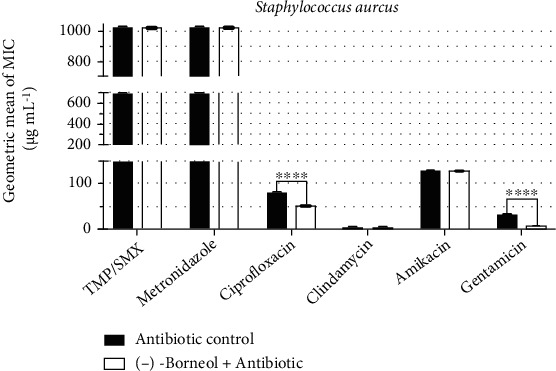
Antibiotic-modulating activity of (-)-borneol associated with antibiotics against S. aureus. TMP/SMX: trimethoprim/sulfamethoxazole. p < 0.0001 = ∗∗∗∗.
The analysis of antibiotic resistance modulation by (+)-α-pinene against E. coli is shown in Figure 3. Among the antibiotics, only amikacin and gentamicin had their MIC changed by the compound. While the MIC of amikacin was reduced from 50.8 μg/mL to 40.3 μg/mL, the MIC of gentamicin was reduced from 20.1 μg/mL to 16 μg/mL.
Figure 3.
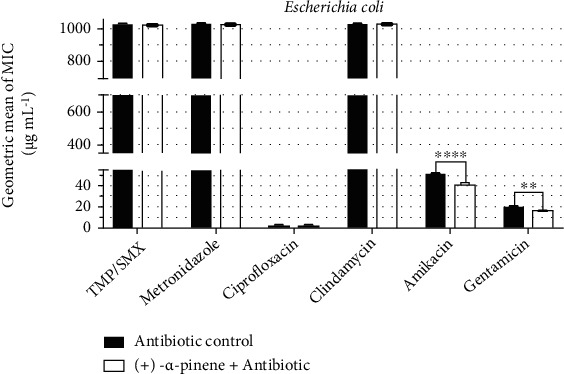
Antibiotic-modulating activity of (+)-α-pinene associated with antibiotics against E. coli. TMP/SMX: trimethoprim/sulfamethoxazole. p < 0.0001 = ∗∗∗∗.
On the other hand, under the same conditions described above, an antagonistic activity was observed from the combination of (-)-borneol with trimethoprim/sulfamethoxazole against E. coli, since the antibiotic MIC increased from 512 μg/mL to ≥1024 μg/mL (Figure 4). However, no significant modulation of antibiotic activity was observed from the association of (-)-borneol with the other drugs.
Figure 4.
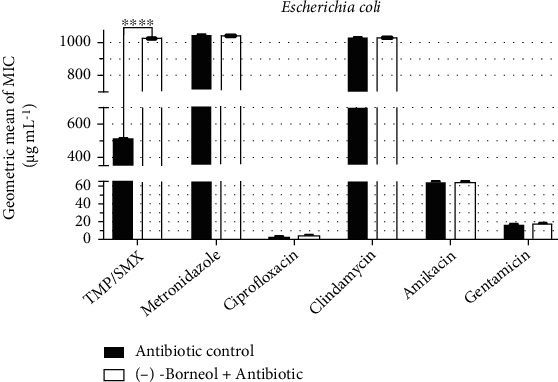
Antibiotic-modulating activity of (-)-borneol associated with antibiotics against E. coli. TMP/SMX: trimethoprim/sulfamethoxazole. p < 0.0001 = ∗∗∗∗.
P. aeruginosa was found to present significant resistance to antibiotics, whose MIC was poorly affected by the association with (+)-α-pinene. Nevertheless, it is worth mentioning that this monoterpene caused a reduction of 37% in the MIC of amikacin in comparison with the control (Figure 5).
Figure 5.
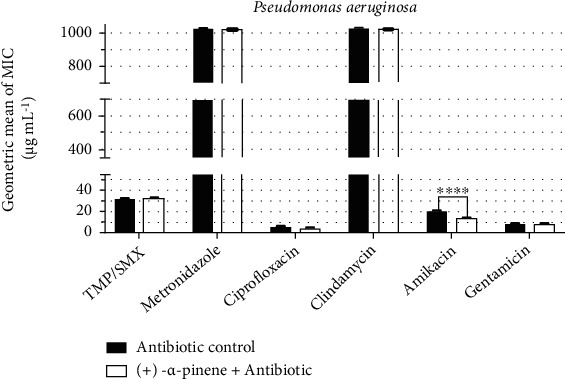
Antibiotic-modulating activity of (+)-α-pinene associated with antibiotics against P. aeruginosa. TMP/SMX: trimethoprim/sulfamethoxazole. p < 0.0001 = ∗∗∗∗.
Under the same conditions described above, (-)-borneol failed to modulate the activity of all antibiotics against P. aeruginosa, as no significant MIC change was observed (Figure 6).
Figure 6.
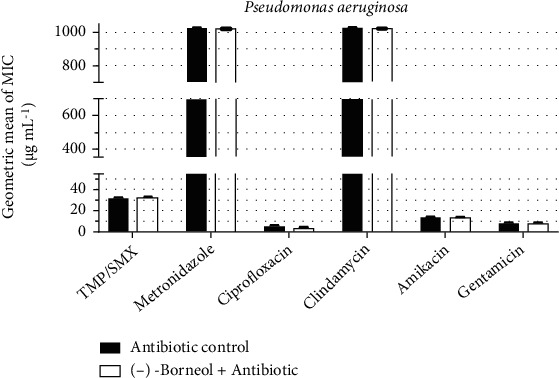
Antibiotic-modulating activity of (-)-borneol associated with antibiotics against P. aeruginosa. TMP/SMX: trimethoprim/sulfamethoxazole. p < 0.0001 = ∗∗∗∗.
Discussion
The use of these natural compounds in the treatment of infections is considered a traditional alternative to the use of synthetic drugs [33]. Studies have demonstrated that monoterpenes can improve the activity of antimicrobial drugs, increasing their effectiveness against resistant pathogens, which can accelerate the healing, as well as hinder the microbial adaptability. Resistance to aminoglycosides and other antibacterial drugs has been a major threat to public health. Aminoglycosides inhibit protein synthesis by altering the conformation of the bacterial ribosome [34, 38] presenting enzymatic inactivation and efflux pump expression as major resistance mechanisms [37].
A significant body of research has demonstrated that antibiotic resistance can be reversed using natural products such as extracts, fractions, essential oils, and isolated phytocompounds, as well as their synthetic and semisynthetic derivatives [33, 34, 37, 38]. While the molecular mechanism underlying this phenomenon remains mostly unknown, it has been suggested that it involves interactions between the natural product structure and constituents of the bacterial cell membrane, such as transmembrane proteins [37, 38].
Yousefzadi et al. [39] isolated α-pinene from the essential oil of Salvia chloroleuca and evaluated its antibacterial activity, demonstrating moderate and strong inhibitory activities against S. aureus and E. coli, respectively. However, no activity was found against P. aeruginosa, which can be explained due to differences in the structure of the cell membrane of Gram-positive and Gram-negative bacteria, in particular, the lipid bilayer [38, 40].
Da Silva et al. [17] evaluated the antimicrobial activity of pinenes, demonstrating that (-)-α-pinene and (-)-β-pinene had no significant antimicrobial activity at concentrations below 20 mg/mL, while the positive enantiomers showed inhibitory activities against methicillin-resistant S. aureus strains with MIC values ranging from 117 μg/mL to 6,250 μg/mL. Accordingly, the studies of Da Silva et al. [17] and Dhar et al. [41] found that (+)-α-pinene presented antibacterial activity against S. aureus strains. Moreover, De Sousa Eduardo et al. [42] and Freitas et al. [43] showed that α-pinene has promising effects against S. aureus, demonstrating a potential to be used in the combat of antibacterial resistance.
The results of the present work corroborate those presented by Da Silva et al. [17] who evaluated the combination of (+)-α-pinene and (+)-β-pinene with ciprofloxacin, showing synergistic activity against methicillin-resistant S. aureus (MRSA).
An antibiotic-potentiating effect was also obtained by Do Amaral et al. [44] who showed that the association of α-pinene with ceftazidime, amoxicillin, cefepime, cefoxitin, and amikacin resulted in enhanced antibiotic activity against E. coli.
This enhanced antibiotic effect may result from different mechanisms such as alteration in membrane permeability; inhibition of efflux pumps activity, or alteration in the expression of genes that codify proteins that mediate these mechanisms [45].
S. aureus can become resistant to antibiotics through genetic mutations that alter the target DNA gyrase or reduce outer membrane proteins, thus reducing drug accumulation [46, 47]. Martin et al. [48] reported a marked increase in resistance to trimethoprim-sulfamethoxazole in clinical isolates of Staphylococcus aureus and 7 genera of Enterobacteriaceae, including E. coli, from 1988-1995 at a hospital in California.
E. coli is naturally susceptible to almost all clinically relevant antimicrobial agents, in addition to being capable of accumulating resistance genes, mainly through horizontal gene transfer [49].
Studies performed by Breidenstein et al. [50] showed that Pseudomonas aeruginosa presents a high level of intrinsic resistance to most antibiotics, which can be explained by the restricted permeability of its outer membrane, in addition to the expression of efflux systems and antibiotic-inactivating enzymes such as β-lactamases.
Corroborating the results of this study, Ali et al. [51] evaluated P. aeruginosa isolates and found significant resistance to amikacin, while resistance to trimethoprim-sulfamethoxazole was described by Bayraktar et al. [52].
Barbosa [53] evaluated the essential oil of Chamaemelum nobile, which has α-pinene and β-pinene as major components. The oil strongly modulated the activity of amikacin activity against P. aeruginosa PA01, causing a 128-fold reduction in the MIC of this antibiotic, corroborating the results of this study.
Nitroimidazole prodrugs such as metronidazole are activated by the reduction of the nitro group, which occurs at low oxygen rates, since oxygen can inhibit metronidazole uptake. Thus, the effective use of nitroimidazoles is limited to anaerobic bacteria, protozoa, and microaerophiles [54–57], corroborating the resistance profile observed in this study.
It is known lipophilic substances like beta-caryophyllene can induce significant changes in the membrane structure, resulting in morpho-physiological damage, such as reduced membrane potential, cytochrome C/protein and radical loss, proton pump collapse, and ATP depletion, among other toxic effects [30, 58–63]. Accordingly, studies by Andrews et al. [63], Harrewijn et al. [64], and Singh et al. [65] state that the mechanism of action by α-pinene is associated with cell membrane damage.
Kovač et al. [66] evaluated the antibacterial activity of the negative enantiomer α-pinene at the concentration of 125 mg/L, showing that this compound increased the membrane permeability, in addition to inducing an intracellular accumulation of antibiotics due to the inhibition of antimicrobial efflux systems, providing further inhibition of antimicrobial resistance. A number of studies [63–66] have also demonstrated that pinene compounds have caused damage to the membrane, which may also explain its effects on antibiotic activity potentiation, as demonstrated in this research.
Badawy et al. [67] described the antimicrobial effects of various monoterpenes, among which thymol and α-terpineol had the most potent activity against E. coli and S. aureus. De Souza et al. [68] evidenced the efficacy of the association between carvone and penicillin against MRSA, as well as demonstrated the potentiating effects of eugenol and thymol associated with penicillin against beta-lactam-resistant E. coli. In corroboration, the work of De Souza et al. [68] found that d-limonene had a synergistic effect when associated with gentamicin against S. aureus and E. coli while the monoterpene geraniol enhanced the activity of kanamycin against the bacterial strain 358 of S. aureus [69].
Sill with regard to effects of monoterpenes against resistant S. aureus strains, Freitas et al. [43] also stated that α-pinene potentiated the effect of tetracycline against the S. aureus IS-58 strain, while studies with E. coli conducted by Pereira et al. [70] showed that the complex (+)-β-citronellol (βCT)/β-cyclodextrin (β-CD) in combination with gentamicin showed a synergistic effect against E. coli.
Research by Gachkar et al. [71] has attributed the antimicrobial activity of some essential oils to the presence borneol, which has been identified as a major constituent of the essential oils obtained from the flowers, leaves, and stem of Rhynchanthus beesianus [72], which presented significant antibacterial activity against Bacillus subtilis, Enterococcus faecalis, S. aureus, Proteus vulgaris, P. aeruginosa, and E. coli.
Studies on the antibacterial mechanism of action of terpenes [73–75] have indicated that the antimicrobial activities of thymol and carvacrol are associated with their ability to cause changes in membrane permeability. According to Breidenstein et al. [50], the restricted permeability of the outer membrane, as well as the presence of efflux systems, and the production of antibiotic-inactivating enzymes, such as β-lactamases, collaborate to the high level of antibiotic resistance observed in Pseudomonas aeruginosa, which could justify the lack of significant modulation of the antibiotic activity by the compounds evaluated in the present research. Finally, the present findings corroborate those obtained by Siddique et al. [76] who showed that borneol did not exhibit antibacterial activity against MDR clinical isolates of S. aureus and MRSA.
While specific mechanisms involved in the antimicrobial action of monoterpenes remain poorly characterized, studies by Sikkema et al. [61] and Sikkema et al. [11] have suggested that due to their lipophilic character, monoterpenes will preferentially divide from an aqueous phase into membrane structures, thus causing structural and functional damage, which has been used to explain the antimicrobial action of oils and their monoterpenoid components in most works. According to Trombetta et al. [77], the action of these compounds on the bacterial membrane leads to expansion, increased fluidity and permeability, disturbance of protein function, and inhibition of ion transport. Thus, the existence of certain epistatic interactions that result in variable responses in studies addressing different species and antibiotics cannot be ruled out.
Besides the antibacterial activity, research has demonstrated that borneol has analgesic, anti-inflammatory, antioxidant, healing, and antifungal activities [78, 79].
Yang et al. [79] reported that (+)-borneol (BNL1) and (-)-borneol (BNL2) can induce drug accumulation in cells due to its interference with P-glycoprotein (Pgp), an efflux protein that contributes to multidrug resistance to antibiotics and anticancer drugs, which could potentially explain the synergistic effects observed from the association between monoterpenes and antibiotics, as demonstrated in this work.
Of note, to date, no study evaluating the antibiotic-enhancing activity of (-)-borneol has been found in the literature, highlighting the pioneering aspect of the present research.
4. Conclusions
The results presented in this work suggest that (+)-α-pinene and (-)-borneol are promising compounds in the inhibition of antibiotic resistance, although further research is required to investigate both the safety and effectiveness of this combined treatment in the management of infections caused by S. aureus, E. coli, and P. aeruginosa.
The results of this work can contribute to the development of new antibacterial therapies using lower doses of monoterpenes and antibiotics, increasing the effectiveness and reducing the side effects resulting from antibiotic therapy.
Acknowledgments
We express our deep gratitude to the ESTÁCIO|FMJ faculty of medicine for technical support for this research and project CICECO-Aveiro Institute of Materials, UIDB/50011/2020 and UIDP/50011/2020, national funds by FCT/MCTES. This research was also supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF2020R1I1A2066868) and the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (no. 2020R1A5A2019413).
Contributor Information
Abolghasem Siyadatpanah, Email: asiyadatpanah@yahoo.com.
Bonglee Kim, Email: bongleekim@khu.ac.kr.
Henrique D. M. Coutinho, Email: hdmcoutinho@gmail.com.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.World Health Organization–Who. Antimicrobial resistance. 2020.
- 2.Yagui M. Antimicrobial resistance: a new approach and opportunity. Revista peruana de medicina experimental y salud publica . 2018;35(1):7–8. doi: 10.17843/rpmesp.2018.351.3594. [DOI] [PubMed] [Google Scholar]
- 3.Dispõe sobre o controle de medicamentos à base de substâncias classificadas como antimicrobianos, de uso sob prescrição, isoladas ou em associação. 2011. p. p. 2011. Anvisa. Resolução-rdc n° 20, de 5 de maio de.
- 4.Taylor P. W., Stapleton P. D., Paul L. J. New ways to treat bacterial infections. Drug Discovery Today . 2002;7(21):1086–1091. doi: 10.1016/S1359-6446(02)02498-4. [DOI] [PubMed] [Google Scholar]
- 5.da Silva Marangoni C. G. P., Machado T. N., Thaler J., et al. Detecção E Caracterização De Antimicrobianos Usando Espectroscopia Raman Amplificada Por Superfície. Brazilian Journal of Infectious Diseases . 2022;26, article 101999 doi: 10.1016/j.bjid.2021.101999. [DOI] [Google Scholar]
- 6.Guimaraes D. O., Momesso L. S., Pupo M. T. Antibiotics: therapeutic importance and prospects for the discovery and development of new agents. Quím. Nova . 2010;33(3):667–679. [Google Scholar]
- 7.de Oliveira C. F., Morey A. T., Biasi-Garbin R. P., Perugini M. R. E., Yamauchi L. M., Yamada-Ogatta S. F. Emergência de Staphylococcus aureus resistentes aos antimicrobianos: um desafio contínuo. Rev. Ciênc. Méd. Biol. . 2015;13:242–247. [Google Scholar]
- 8.Almeida Neto J. R., de Barros R. F. M., Silva P. R. R. Uso de plantas medicinais em comunidades rurais da Serra do Passa-Tempo, estado do Piauí. Nordeste do Brasil. Rev. Bras. Biocienc. . 2015;13:165–175. [Google Scholar]
- 9.Zielińska-Błajet M., Feder-Kubis J. Monoterpenes and their derivatives—recent development in biological and medical applications. International Journal of Molecular Sciences . 2020;21(19):p. 7078. doi: 10.3390/ijms21197078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wright G. D. The antibiotic resistome: the nexus of chemical and genetic diversity. Nature Reviews. Microbiology . 2007;5(3):175–186. doi: 10.1038/nrmicro1614. [DOI] [PubMed] [Google Scholar]
- 11.Sikkema J., Bont J. A. M., Poolman B. Mechanisms of membrane toxicity of hydrocarbons. Microbiological Reviews . 1995;59(2):201–222. doi: 10.1128/mr.59.2.201-222.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burt S. Essential oils: their antibacterial properties and potential applications in foods--a review. International Journal of Food Microbiology . 2004;94(3):223–253. doi: 10.1016/j.ijfoodmicro.2004.03.022. [DOI] [PubMed] [Google Scholar]
- 13.Morales-Yuste M., Morillas-Márquez F., Martín-Sánchez J., Valero-López A., Navarro-Moll M. Activity of (-)α-bisabolol against _Leishmania infantum_ promastigotes. Phytomedicine . 2010;17(3-4):279–281. doi: 10.1016/j.phymed.2009.05.019. [DOI] [PubMed] [Google Scholar]
- 14.Winnacker M. Pinenes: abundant and renewable building blocks for a variety of sustainable polymers. Angewandte Chemie International Edition . 2018;57(44):14362–14371. doi: 10.1002/anie.201804009. [DOI] [PubMed] [Google Scholar]
- 15.Vespermann K. A., Paulino B. N., Barcelos M. C., Pessôa M. G., Pastore G. M., Molina G. Biotransformation of α-and β-pinene into flavor compounds. Applied Microbiology and Biotechnology . 2017;101(5):1805–1817. doi: 10.1007/s00253-016-8066-7. [DOI] [PubMed] [Google Scholar]
- 16.Berger R. G. Flavours and fragrances: chemistry, bioprocessing and sustainability. Springer Science & Business Media: Berlin . 2007;1:1–648. doi: 10.1007/978-3-540-49339-6. [DOI] [Google Scholar]
- 17.da Silva A. C., Lopes P. M., de Azevedo M. M., Costa D. C., Alviano C. S., Alviano D. S. Biological activities of a-pinene and β-pinene enantiomers. Molecules . 2012;17(6):6305–6316. doi: 10.3390/molecules17066305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sybilska D., Kowalczyk J., Asztemborska M., Ochocka R. J., Lamparczyk H. Chromatographic studies of the enantiomeric composition of some therapeutic compositions applied in the treatment of liver and kidney diseases. Journal of Chromatography. A . 1994;665(1):67–73. doi: 10.1016/0021-9673(94)87033-0. [DOI] [PubMed] [Google Scholar]
- 19.Alma M. H., Nitz S., Kollmannsberger H., Digrak M., Efe F. T., Yilmaz N. Chemical composition and antimicrobial activity of the essential oils from the gum of Turkish pistachio (Pistacia veraL.) Journal of Agricultural and Food Chemistry . 2004;52(12):3911–3914. doi: 10.1021/jf040014e. [DOI] [PubMed] [Google Scholar]
- 20.Silva E., Macie A. T., Pereira V. V., Takahashi J. A., Silva R. R., Duarte L. P. Microwave-assisted synthesis of borneol esters and their antimicrobial activity. Natural Product Research . 2018;32(14):1714–1720. doi: 10.1080/14786419.2017.1399380. [DOI] [PubMed] [Google Scholar]
- 21.Chen Z. X., Xu Q. Q., Shan C. S., et al. Borneol for regulating the permeability of the blood-brain barrier in experimental ischemic stroke: preclinical evidence and possible mechanism. Oxidative Medicine and Cellular Longevity . 2019;2019:16. doi: 10.1155/2019/2936737. [DOI] [Google Scholar]
- 22.Zhou H. H., Zhang L., Zhou Q. G., Fang Y., Ge W. H. (+)-Borneol attenuates oxaliplatin-induced neuropathic hyperalgesia in mice. Neuroreport . 2016;27(3):160–165. doi: 10.1097/WNR.0000000000000516. [DOI] [PubMed] [Google Scholar]
- 23.Wang S., Zhang D., Hu J., et al. A clinical and mechanistic study of topical borneol-induced analgesia. EMBO Molecular Medicine . 2017;9(6):802–815. doi: 10.15252/emmm.201607300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Santos S. E., Ribeiro F. P. R. A., Menezes P. M. N., et al. New insights on relaxant effects of (—)-borneol monoterpene in rat aortic rings. Fundamental & Clinical Pharmacology . 2019;33(2):148–158. doi: 10.1111/fcp.12417. [DOI] [PubMed] [Google Scholar]
- 25.Bansod S., Chilvery S., Saifi M. A., Das T. J., Tag H., Godugu C. Borneol protects against cerulein-induced oxidative stress and inflammation in acute pancreatitis mice model. Environmental Toxicology . 2021;36(4):530–539. doi: 10.1002/tox.23058. [DOI] [PubMed] [Google Scholar]
- 26.Wang Z., Li Q., Xia L., et al. Borneol promotes apoptosis of human glioma cells through regulating HIF-1a expression via mTORC1/eIF4E pathway. Journal of Cancer . 2020;11(16):4810–4822. doi: 10.7150/jca.45304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang J. Y., Dong X., Yu Z., et al. Borneol inhibits CD4 + T cells proliferation by down-regulating miR-26a and miR-142-3p to attenuate asthma. International Immunopharmacology . 2021;90, article 107223 doi: 10.1016/j.intimp.2020.107223. [DOI] [PubMed] [Google Scholar]
- 28.Cao B., Ni H. Y., Li J., et al. (+)-Borneol suppresses conditioned fear recall and anxiety-like behaviors in mice. Biochemical and Biophysical Research Communications . 2018;495(2):1588–1593. doi: 10.1016/j.bbrc.2017.12.025. [DOI] [PubMed] [Google Scholar]
- 29.Xin Y., Zhao H., Xu J., et al. Borneol-modified chitosan: antimicrobial adhesion properties and application in skin flora protection. Carbohydrate Polymers . 2020;228, article 115378 doi: 10.1016/j.carbpol.2019.115378. [DOI] [PubMed] [Google Scholar]
- 30.Hector R. F., Braun P. C. Synergistic action of nikkomycins X and Z with papulacandin B on whole cells and regenerating protoplasts of Candida albicans. Antimicrobial Agents and Chemotherapy . 1986;29(3):389–394. doi: 10.1128/AAC.29.3.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.C L S I. CLSI document M07-A9 . Wayne, PA: Clinical and Laboratory Standards Institute; 2012. Methods for dilution antimicrobial susceptibility tests f or bacteria that grow aerobically; approved standard—ninth edition. [Google Scholar]
- 32.Sales G. W. P., Batista A. H. M., Rocha L. Q., Nogueira M. A. P. Efeito antimicrobiano e modulador do óleo essencial extraído da casca de frutos da Hymenaea courbaril L. Rev. Ciênc Farm. Apl. . 2014;35:709–715. [Google Scholar]
- 33.Salvat A., Antonnacci L., Fortunato R. H., Suarez E. Y., Godoy H. M. Screening of some plants from Northern Argentina for their antimicrobial activity. Letters in Applied Microbiology . 2001;32(5):293–297. doi: 10.1046/j.1472-765X.2001.00923.x. [DOI] [PubMed] [Google Scholar]
- 34.Hollis L., Jones R. S. US Environmental Protection Agency O_ce of pesticide programs. Biopestic. Pollut. Prev. Div. Farnesol. Nerolidol. . 2009;1:p. 24. [Google Scholar]
- 35.Canton M., Onofre S. B. Interferência de extratos da Baccharis dracunculifolia DC., Asteraceae, sobre a atividade de antibióticos usados na clínica. Revista Brasileira de Farmacognosia . 2010;20(3):348–354. doi: 10.1590/S0102-695X2010000300010. [DOI] [Google Scholar]
- 36.Houghton P. J., Howes M. J., Lee C. C., Steventon G. Uses and abuses of in vitro tests in ethnopharmacology: visualizing an elephant. Journal of Ethnopharmacology . 2007;110(3):391–400. doi: 10.1016/j.jep.2007.01.032. [DOI] [PubMed] [Google Scholar]
- 37.Coutinho H. D. M., Costa J. G. M., Lima E. O., Falcão-Silva V. S., Siqueira-Júnior J. P. Enhancement of the antibiotic activity against a multiresistant Escherichia coli by Mentha arvensis L. and chlorpromazine. Chemotherapy . 2008;54(4):328–330. doi: 10.1159/000151267. [DOI] [PubMed] [Google Scholar]
- 38.Jana S., Deb J. K. Molecular understanding of aminoglycoside action and resistance. Applied Microbiology and Biotechnology . 2006;70(2):140–150. doi: 10.1007/s00253-005-0279-0. [DOI] [PubMed] [Google Scholar]
- 39.Yousefzadi M., Sonboli A., Ebrahimi S. N., Hashemi S. H. Antimicrobial activity of essential oil and major constituents of Salvia chloroleuca. Zeitschrift für Naturforschung C . 2008;63(5-6):337–340. doi: 10.1515/znc-2008-5-605. [DOI] [PubMed] [Google Scholar]
- 40.Coutinho H. D. M., Costa J. G. M., Falcão-Silva V. S., Siqueira-Júnior J. P., Lima E. O. Fruits to potentiate the antibiotic activity: the efect of Eugenia uniflora and Eugenia jambolanum L. against MRSA. Acta Alimentaria . 2011;41:67–72. [Google Scholar]
- 41.Dhar P., Chan P., Cohen D. T., et al. Synthesis, antimicrobial evaluation, and structure–activity relationship of α-pinene derivatives. Journal of Agricultural and Food Chemistry . 2014;62(16):3548–3552. doi: 10.1021/jf403586t. [DOI] [PubMed] [Google Scholar]
- 42.De Sousa Eduardo L., Farias T. C., Ferreira S. B., Ferreira P. B., Lima Z. N., Ferreira S. B. Antibacterial activity and time-kill kinetics of positive enantiomer of α-pinene against strains of Staphylococcus aureus and Escherichia coli. Current Topics in Medicinal Chemistry . 2018;18(11):917–924. doi: 10.2174/1568026618666180712093914. [DOI] [PubMed] [Google Scholar]
- 43.Freitas P. R., De Araújo A. C. J., Barbosa C. R., et al. Inhibition of efflux pumps by monoterpene (α-pinene) and impact on Staphylococcus aureus resistance to tetracycline and erythromycin. Current Drug Metabolism . 2021;22(2):123–126. doi: 10.2174/1389200221999200730212721. [DOI] [PubMed] [Google Scholar]
- 44.do Amaral, Felipe Lemos E., Farias T. C., et al. Effect of the association and evaluation of the induction to adaptation of the (+)-α-pinene with commercial antimicrobials against strains of Escherichia coli. Current Topics in Medicinal Chemistry . 2020;20(25):2300–2307. doi: 10.2174/1568026620666200820150425. [DOI] [PubMed] [Google Scholar]
- 45.Blair J. M. A., Webber M. A., Baylay A. J., Ogbolu D. O., Piddock L. J. Molecular mechanisms of antibiotic resistance. Nature Reviews Microbiology . 2015;13(1):42–51. doi: 10.1038/nrmicro3380. [DOI] [PubMed] [Google Scholar]
- 46.Kime L., Randall C. P., Banda F. I., et al. Transient silencing of antibiotic resistance by mutation represents a significant potential source of unanticipated therapeutic failure. MBio . 2019;10(5, article e01755):p. 19. doi: 10.1128/mBio.01755-19. [DOI] [Google Scholar]
- 47.Yang J. J., Cheng A., Tai H. M., Chang L. W., Hsu M. C., Sheng W. H. Selected mutations by nemonoxacin and fluoroquinolone exposure among relevant gram-positive bacterial strains in Taiwan. Microbial Drug Resistance . 2020;26(2):110–117. doi: 10.1089/mdr.2019.0048. [DOI] [PubMed] [Google Scholar]
- 48.Martin J. N., Rose D. A., Hadley W. K., Perdreau-Remington F., Lam P. K., Gerberding J. L. Emergence of trimethoprim-sulfamethoxazole resistance in the AIDS era. Journal of Infectious Diseases . 1999;180(6):1809–1818. doi: 10.1086/315132. [DOI] [PubMed] [Google Scholar]
- 49.Poirel L., Madec J. Y., Lupo A., et al. Antimicrobial resistance in Escherichia coli. Microbiology Spectrum . 2018;6:1–27. [Google Scholar]
- 50.Breidenstein E. B. M., De La Fuente-Núñez C., Hancock R. E. W. _Pseudomonas aeruginosa_ : all roads lead to resistance. Trends in Microbiology . 2011;19(8):419–426. doi: 10.1016/j.tim.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 51.Ali N. M., Chatta S., Liaqat I., Mazhar S. A., Mazhar B., Zahid S. Pseudomonas aeruginosa associated pulmonary infections and in vitro amplification virulent rhamnolipid (rhlR) gene. Brazilian Journal of Biology . 2021;82:1–9. [Google Scholar]
- 52.Bayraktar M., Kaya E., Ozturk A., İbahim B. M. S. Antimicrobial susceptibility of bacterial pathogens isolated from healthcare workers' cellphones. Infectious Diseases Now . 2021:1–7. doi: 10.1016/j.idnow.2021.05.007. [DOI] [Google Scholar]
- 53.Barbosa M. P. Atividade antimicrobiana do óleo essencial de camomila romana (Chamaemelum nobile) Dissertação de Mestrado . Santa Maria, RS, Brasil: Universidade Federal de Santa Maria; 2019. [Google Scholar]
- 54.Dingsdag S. A., Hunter N. Metronidazole: an update on metabolism, structure–cytotoxicity and resistance mechanisms. Journal of Antimicrobial Chemotherapy . 2018;73(2):265–279. doi: 10.1093/jac/dkx351. [DOI] [PubMed] [Google Scholar]
- 55.Baughn A. D., Malamy M. H. The strict anaerobe _Bacteroides fragilis_ grows in and benefits from nanomolar concentrations of oxygen. Nature . 2004;427(6973):441–444. doi: 10.1038/nature02285. [DOI] [PubMed] [Google Scholar]
- 56.Moore R. A., Beckthold B., Bryan L. E. Metronidazole uptake in Helicobacter pylori. Canadian Journal of Microbiology . 1995;41(8):746–749. doi: 10.1139/m95-102. [DOI] [PubMed] [Google Scholar]
- 57.Church D. L., Laishley E. J. Reduction of metronidazole by hydrogenase from clostridia. Anaerobe . 1995;1(2):81–92. doi: 10.1006/anae.1995.1002. [DOI] [PubMed] [Google Scholar]
- 58.Almirall M., Montana J., Escribano E., Obach R., Berrozpe J. D. Effect of d-limonene, alpha-pinene and cineole on in vitro transdermal human skin penetration of chlorpromazine and haloperidol. Arzneimittel Forschung . 1996;46(7):676–680. [PubMed] [Google Scholar]
- 59.Werf M. J., de Bont J. A., Leak D. J. Opportunities in microbial biotransformation of monoterpenes. In: Berger R. G., Babel W., Blanch H. W., et al., editors. In Biotechnology of Aroma Compounds . Springer: Berlin/Heidelberg, Germany; 1997. pp. 147–177. [Google Scholar]
- 60.Hirayama K. B., Speridiao P. G., Fagundes-Neto U. Ácidos graxos poli-insaturados de cadeia longa. The Electronic Journal of Pediatric Gastroenterology, Nutrition and Liver Diseases . 2006;10:1–10. [Google Scholar]
- 61.Sikkema J., De Bont J. A. M., Poolman B. Interactions of cyclic hydrocarbons with biological membranes. The Journal of Biological Chemistry . 1994;269(11):8022–8028. doi: 10.1016/S0021-9258(17)37154-5. [DOI] [PubMed] [Google Scholar]
- 62.Turina A. D. V., Nolan M. V., Zygadlo J. A., Perillo M. A. Natural terpenes: self-assembly and membrane partitioning. Biophysical Chemistry . 2006;122(2):101–113. doi: 10.1016/j.bpc.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 63.Andrews R. E., Parks L. W., Spence K. D. Some effects of Douglas fir terpenes on certain microorganisms. Applied and Environmental Microbiology. . 1980;40(2):301–304. doi: 10.1128/aem.40.2.301-304.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Harrewijn P., van Oosten A. M., Piron P. G. Natural terpenoids as messengers: a multidisciplinary study of their production, biological functions, and practical applications . Springer Science & Business Media; 2001. [Google Scholar]
- 65.Singh H. P., Batish D. R., Kaur S., Arora K., Kohli R. K. α-Pinene inhibits growth and induces oxidative stress in roots. Annals of Botany . 2006;98(6):1261–1269. doi: 10.1093/aob/mcl213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kovač J., Šimunović K., Wu Z., et al. Antibiotic resistance modulation and modes of action of (-)-α-pinene in Campylobacter jejuni. PloS one . 2015;10(4):p. e0122871. doi: 10.1371/journal.pone.0122871. [DOI] [Google Scholar]
- 67.Badawy M. E., Marei G. I. K., Rabea E. I., Taktak N. E. Antimicrobial and antioxidant activities of hydrocarbon and oxygenated monoterpenes against some foodborne pathogens through _in vitro_ and _in silico_ studies. Pesticide Biochemistry and Physiology . 2019;158:185–200. doi: 10.1016/j.pestbp.2019.05.008. [DOI] [PubMed] [Google Scholar]
- 68.De Souza I. S., Duarte Filho C. E., do Socorro Costa M., Pereira R. T., de Lima M. A. Anais do III Congresso Brasileiro de Ciências da Saúde . Campina Grande: Editora Realize; 2018. Atividade antibacteriana do D-limoneno simples e complexado com a βciclodextrina e em avaliação do potencial modulador associado com diferentes classes de antibióticos. [Google Scholar]
- 69.Coutinho H. D. M., de Freitas M. A., Gondim C. N. F. L., de Albuquerque R. S., de Alencar Ferreira J. V., Andrade J. C. Actividad antimicrobiana de Geraniol e Cariofileno contra Staphylococcus aureus. Revista Cubana de Plantas Medicinales . 2015;20(1):98–105. [Google Scholar]
- 70.Pereira R. L. S., Campina F. F., do Socorro Costa M., et al. Antibacterial and modulatory activities of β-cyclodextrin complexed with (+)-β-citronellol against multidrug-resistant strains. Microbial Pathogenesis . 2021;156:p. 104928. doi: 10.1016/j.micpath.2021.104928. [DOI] [PubMed] [Google Scholar]
- 71.Gachkar L., Yadegari D., Rezaei M. B., Taghizadeh M., Astaneh S. A., Rasooli I. Chemical and biological characteristics of _Cuminum cyminum_ and _Rosmarinus officinalis_ essential oils. Food Chemistry . 2007;102(3):898–904. doi: 10.1016/j.foodchem.2006.06.035. [DOI] [Google Scholar]
- 72.Chen Q., Zhao X., Lu T., et al. Chemical composition, antibacterial, and anti-inflammatory activities of essential oils from flower, leaf, and stem of Rhynchanthus beesianus. BioMed Research International . 2021;2021:11. doi: 10.1155/2021/5562461. [DOI] [Google Scholar]
- 73.Helander I. M., Alakomi H. L., Latva-Kala K., et al. Characterization of the action of selected essential oil components on gram-negative bacteria. Journal of Agricultural and Food Chemistry . 1998;46(9):3590–3595. doi: 10.1021/jf980154m. [DOI] [Google Scholar]
- 74.Cristani M., D'Arrigo M., Mandalari G., et al. Interaction of four monoterpenes contained in essential oils with model membranes: implications for their antibacterial activity. Journal of Agricultural and Food Chemistry . 2007;55(15):6300–6308. doi: 10.1021/jf070094x. [DOI] [PubMed] [Google Scholar]
- 75.García-García R., López-Malo A., Palou E. Bactericidal action of binary and ternary mixtures of carvacrol, thymol, and eugenol against Listeria innocua. Journal of Food Science . 2011;76:95–100. [Google Scholar]
- 76.Siddique H., Pendry B., Rahman M. M. Terpenes from Zingiber montanum and their screening against multi-drug resistant and methicillin resistant Staphylococcus aureus. Molecules (Basel, Switzerland) . 2019;24(3):p. 385. doi: 10.3390/molecules24030385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Trombetta D., Castelli F., Sarpietro M. G., et al. Mechanisms of antibacterial action of three monoterpenes. Antimicrobial Agents and Chemotherapy . 2005;49(6):2474–2478. doi: 10.1128/AAC.49.6.2474-2478.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Al-Farhan K., Warad I., Al-Resayes S., Fouda M., Ghazzali M. Synthesis, structural chemistry and antimicrobial activity of−(−) borneol derivative. Open Chemistry . 2010;8(5):1127–1133. doi: 10.2478/s11532-010-1093-0. [DOI] [Google Scholar]
- 79.Yang R., Chen Z., Xie F., et al. (+/−)-Borneol reverses mitoxantrone resistance against P-glycoprotein. Journal of Chemical Information and Modeling . 2021;61(1):252–262. doi: 10.1021/acs.jcim.0c00892. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.


