Abstract
Background:
Evaluation of acute appendicitis (AA) in pregnancy is supported with diagnostic imaging. Typically, ultrasound (US) is performed first, and then often followed by magnetic resonance imaging (MRI) due to continued diagnostic uncertainty. The purpose of our study was to evaluate the sensitivity, specificity, and accuracy of US as compared to MRI and to evaluate the inter-radiologist agreement amongst body Radiologists with varying levels of expertise.
Methods:
We performed a retrospective study of 364 consecutive pregnant patients with clinical suspicion of AA at a single center over a 6-year period. Sensitivity, Specificity, accuracy, positive and negative predictive values were calculated for US and MRI. Inter Radiologist agreement was determined using Cohen’s Kappa analysis between original interpreting Radiologist and retrospective review by expert Radiologist.
Results:
31 of 364 patients (8.5%) underwent appendectomy based on preoperative diagnosis, with confirmation of acute appendicitis (AA) by pathology in 19. US was able to visualize the appendix in only 6 (1.65%), 5 of whom had appendicitis. 141 patients underwent MRI, and correctly diagnosed appendicitis in 9. No patient with a negative MRI diagnosis had AA.
The sensitivity, and negative predictive value for diagnosing AA with MRI was 100%. The MRI inter-reader agreement for appendix visualization and overall accuracy were 87.9 and 98% with Cohen Kappa of 0.7 and 0.56 respectively.
Conclusion:
Our data suggests that MRI should be considered the first line imaging modality in pregnant patients suspected of having AA. Body Radiologists with varied levels of experience in MRI readouts had substantial agreement.
Keywords: Appendicitis, Pregnancy, Ultrasound, MRI, Diagnosis, Inter-radiologist agreement
Background:
Acute Appendicitis (AA) is the most common non-obstetric cause of abdominal pain requiring surgical treatment in pregnant women 1. Unfortunately, in the pregnant patient, the diagnosis of AA is often clinically difficult owing to normal diagnostic laboratory studies and physiological alterations, as well as the broad range of symptomatology seen during normal pregnancy 2–7 Clinical evaluation of the pregnant patient is challenging due to altered maternal body habitus and organ displacement by the gravid uterus 8. Clinical signs such as guarding and rebound tenderness may be absent while symptoms such as nausea and vomiting, elevation in white blood cell count and C-reactive protein are expected findings in pregnancy 9–11.
Prompt diagnosis of AA decreases the morbidity and mortality in both the pregnant patient and fetus 8,12 The risk of fetal loss increases to 35-55% for perforated appendicitis compared with 1.5% for an intact appendix 11–13. This has led to a lower threshold for surgical intervention in pregnant patients. However, unnecessary surgical interventions may be associated with complications such as preterm labor contractions and fetal loss 13–19.
While ultrasound is still the first recommended investigation, MRI has gained traction per the latest appropriateness criteria published by the American College of Radiology 20. US is widely available, relatively inexpensive and lacks ionizing radiation 21,22. However, the reported diagnostic yield varies widely and there is continued debate regarding its utility2,24–29. Magnetic resonance imaging (MRI) is being increasingly used in the diagnosis of AA during pregnancy, usually following an inconclusive US examination 20,23,29.
Prior studies have demonstrated the superiority of MRI to both identify the appendix and accurately diagnose AA as compared to US 30–35. A meta-analysis performed by Long et al. reported sensitivities, specificities, positive and negative-predictive values of MRI for the diagnosis of AA during pregnancy of 91, 98, 86 and 99%, respectively 36.
Several studies have shown that MRI has a high diagnostic performance for detecting AA in pregnancy. However, these studies are generally performed in highly specialized centers with expert radiologists experienced in interpreting MRI in pregnant patients 37–44.
The purpose of our study was to evaluate the sensitivity, specificity, and accuracy of US and MRI in pregnant patients with suspected AA and to evaluate the inter-Radiologist agreement between general body Radiologists with wide variability in experience who performed the original MRI read with an expert subspecialty radiologist who is experienced in interpreting MRI in pregnant patients.
Methods:
This study was Institutional Review Board approved and compliant with the Health Insurance Portability and Accountability Act. Individual patient consent was waived due to the retrospective nature of this study.
We conducted a retrospective review of the radiology database of the largest women’s hospital in the region to identify all pregnant patients who were at least 15 years old with abdominal pain and suspected AA between January 1st, 2012 and November 31st, 2017 who underwent US and/or MRI imaging which were reviewed by the then in-house Radiologist. If the US was positive, patients proceeded with surgical intervention or MRI for confirmation. If the US was inconclusive, patients underwent MRI for confirmation. One patient underwent a CT scan after an inconclusive US which was negative for AA.
All the patients with preoperative diagnosis of AA underwent surgical intervention. This was decided by the general surgeon if there was high suspicion of appendicitis determined by history, clinical examination, laboratory work and imaging results. The group of patients who were treated non operatively were considered negative for AA. The average follow-up period was 5 months. These pregnant patients had a regular prenatal and postnatal follow up with Gynecology/Obstetrics service. Any suspicion would have generated a general surgery consultation.
Clinical medical records were reviewed for patients age, gestational age, white blood cell count and temperature at presentation to the ER (Emergency Room). If the patient underwent surgical intervention, operative notes and pathology results were reviewed to determine if the appendix was inflamed at resection. Pathologic confirmation of appendix inflammation served as the gold standard for appendicitis in the comparison between the US and MRI diagnostic modalities. Patients with MRI findings that were equivocal for AA were at baseline considered positive. Additional clinical judgement by the general surgeon dictated operative versus non operative management. The medical records were reviewed for patients who were not managed surgically to confirm that the diagnosis of AA was not subsequently made.
All US and MRI examination studies were re-reviewed by a research subspecialty abdominal radiologist (fellowship trained in abdominal imaging and body MRI) for the visualization of the appendix and imaging findings for AA (appendiceal dilation, appendiceal wall thickening, appendicolith, free fluid, fat-stranding and peri-appendiceal collections). The research Radiologist was completely blinded to clinical information during the retrospective re-review of the images. The original reports of US and MRI were tabulated against the expert read during final statistical analysis. The review and read of original general body Radiologist and research Radiologist were interpreted for accuracy and level of agreement. Findings were tabulated for visualization or non-visualization of the appendix for both US and MRI. Results were categorized as positive, negative for AA, non-visualization of appendix with absent secondary signs and equivocal for acute appendicitis. Non visualization with absent secondary signs was considered negative and equivocal was considered positive for statistical analysis.
Ultrasound
Ultrasound examinations were performed using a 5-12MHz linear transducer when possible or a 1-5MHz curved array transducer if necessary, for larger patients. The graded compression technique described by Puylaert was employed. Images were recorded in real time by the sonographers and presented for radiologist interpretation on Picture Archiving and Communication System (PACS). The study interpretations were reviewed retrospectively and tabulated. There was no heterogeneity of the US protocol within the study group.
Visualization of a noncompressible appendix measuring ≥7 mm in diameter with surrounding inflamed fat (usually hyperechoic) was diagnostic for AA (Figure 1), while detection of a compressible appendix <7 mm in diameter was considered negative. Non visualization of appendix with or without secondary signs were reported as such.
Figure 1:
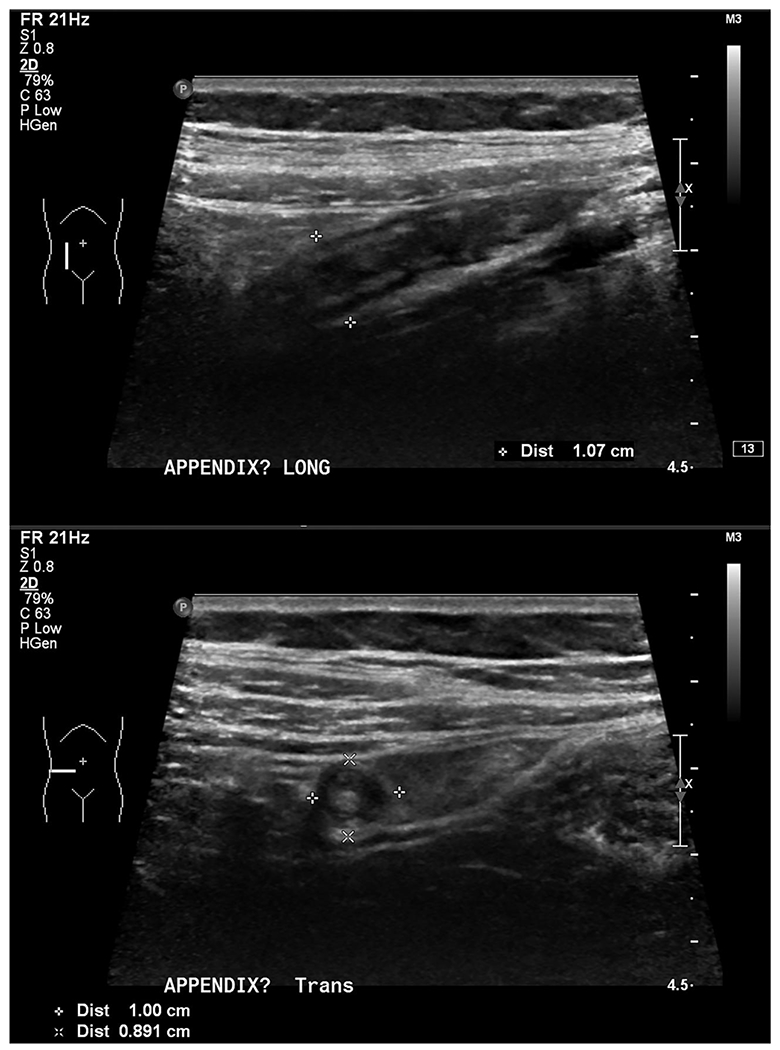
Acute Appendicitis on US Examination: Longitudinal (A) and transverse (B) gray scale sonographic images demonstrate dilated, thick walled, blind ending appendix with peri-appendiceal inflamed fat
MRI
MRI of the abdomen and pelvis was performed on 1.5T GE Excite HDx with a dedicated body Phase Array coil. No intravenous or oral contrast was administered. The MR sequences and image acquisition parameters are tabulated (Table 1). We performed optional sequences when there was confusion in localizing the appendix. One such sequences was the time of flight (TOF) sequence which is sensitive to flowing blood. This sequence was useful to differentiate a dilated appendix from a gonadal vessel. An additional sequence was axial in and out of phase imaging to assess for susceptibility artifacts from gas in the appendix. There was no heterogeneity of the MRI protocol within the study group.
Table 1:
Magee-Women’s Hospital pregnancy appendicitis MRI Protocol
| Coronal T2SSFSE & Fat Sat | Axial T2SSFSE & Fat Sat | Sagittal T2SSFSE | Axial FRFSET2 | Axial FIESTA & Fat Sat | Coronal FIESTA & Fat Sat | Axial DWI | Axial LAVA | |
|---|---|---|---|---|---|---|---|---|
| Pulse Sequence | Spin Echo | Spin Echo | Spin Echo | Spin Echo | Grad Echo | Grad Echo | Spin Echo | Lava-XV |
| Slice Thickness-mm | 5 | 4 | 5 | 5 | 5 | 5 | 5 | 5 |
| Matrix size | 320x288 | 320x288 | 320x288 | 256x192 | 232x256 | 232x256 | 96x96 | 320x256 |
| TR-Repetition Time-ms | 1000 | 1000 | 1000 | 2450 | 4.6 | 4.9 | 4500 | 4.4 |
| TE Echo Time-ms | 90 | 90 | 90 | 87 | 1.8 | 1.8 | 64.7 | 2.1 |
The normal appendix is a tubular blind ending structure from the cecum. It is usually collapsed with intermediate to hypointense T2 signal with diameter of ≤ 6mm in size. The single wall layer thickness is under 2 mm. Air filled appendix can be greater than 6mm in diameter.
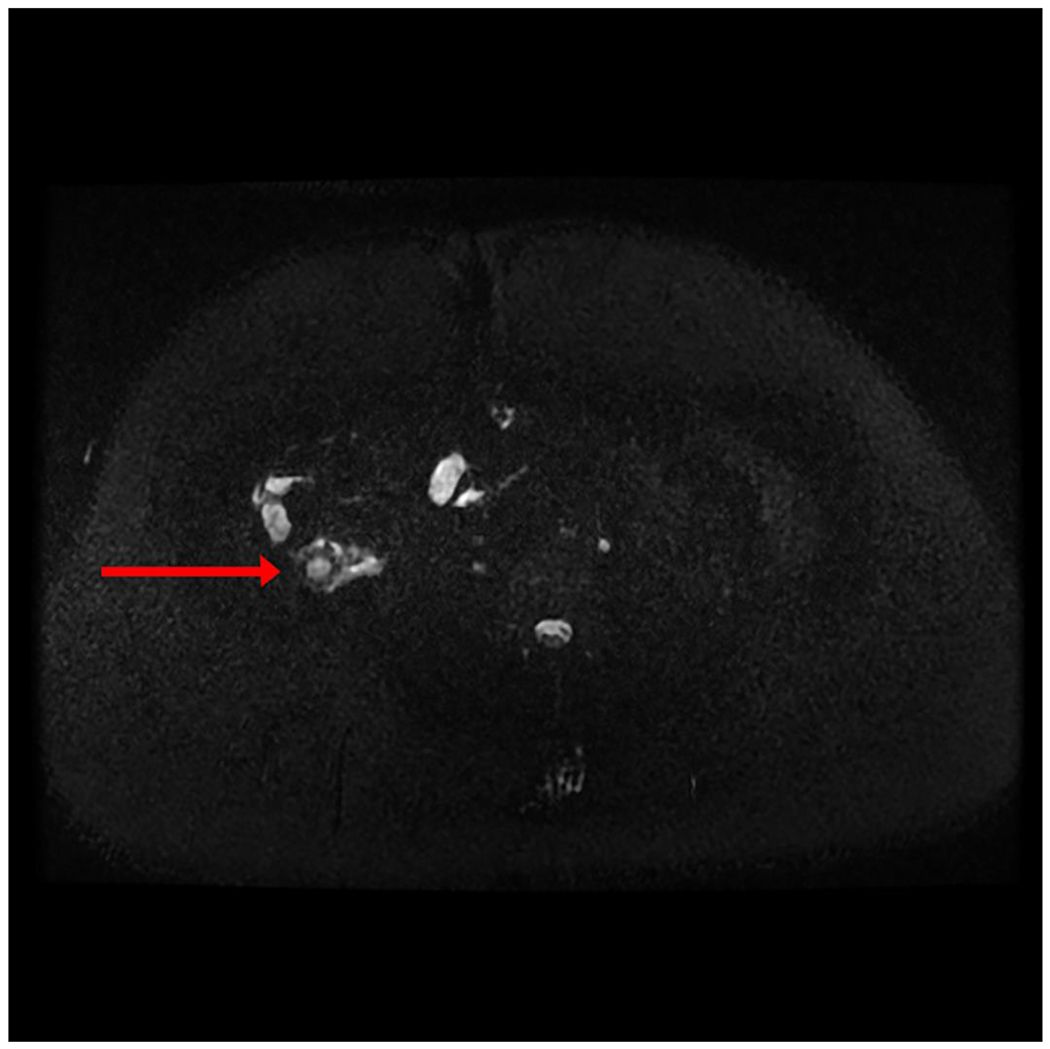
The positive findings at MRI included: fluid filled and dilated appendix with a diameter of ≥ 7mm, appendiceal wall thickening ≥ 2 mm, peri-appendiceal fat stranding/edema, and peri appendiceal/RLQ (right lower quadrant) fluid. The peri-appendiceal edema was best visualized on the T2 fat saturation sequences (Figure 2). Figure 3 demonstrates a negative US but a positive MRI pictures of the same patient (Figure 3).
Figure 2:

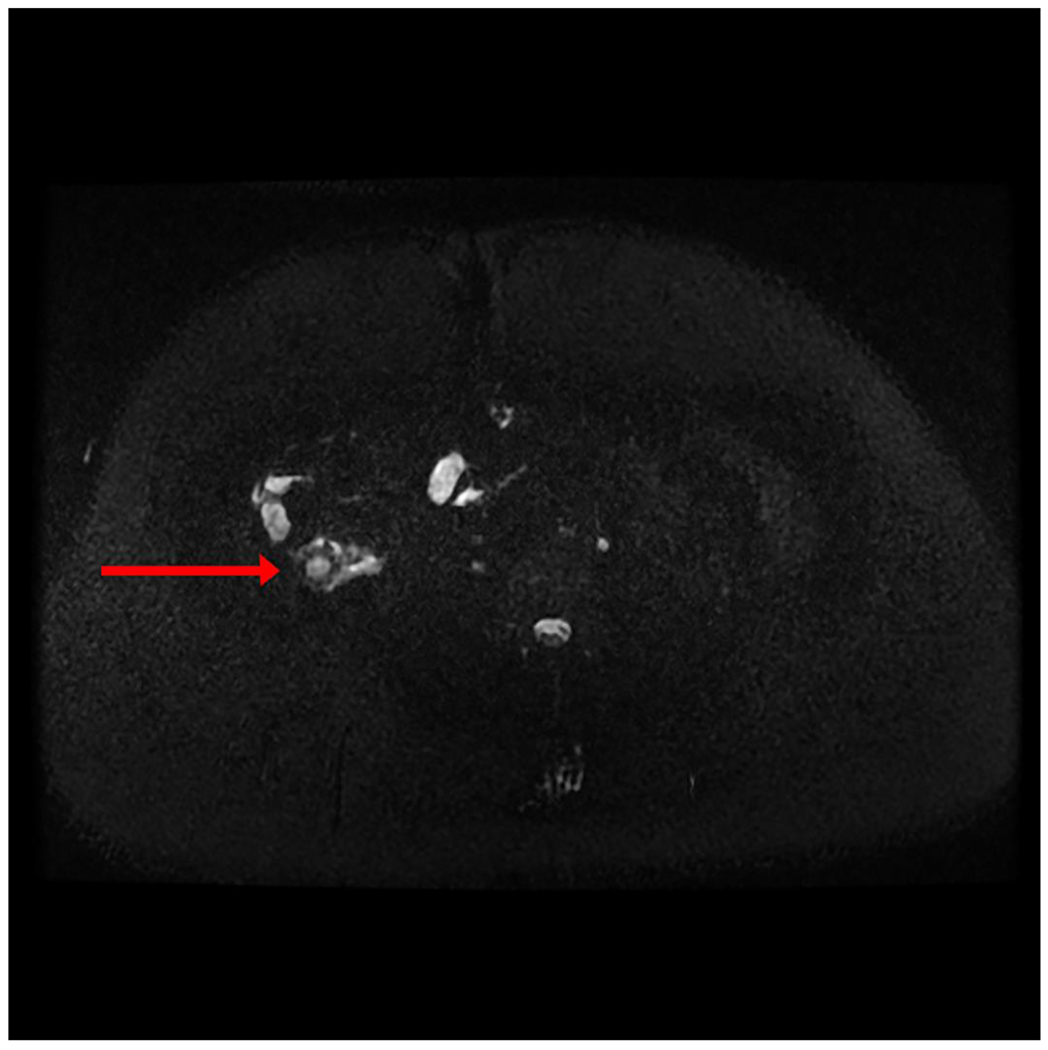
Acute Appendicitis on MRI Examination. A: Coronal T2SSFSE imaging through the abdomen shows a fluid filled dilated appendix (Red arrow) containing multiple appendicoliths with wall thickening and peri appendiceal fluid, B: Axial T2SSFSE fat saturated (fluid sensitive sequence) image clearly demonstrates the fluid filled dilated appendix (Red arrow) with surrounding fluid
Figure 3:


Non visualization of appendix on US with definite AA on MRI. A: US Longitudinal Image fails to show the appendix in the RLQ of the abdomen. B: MRI: Coronal T2SSFSE image shows the retrocecal, thick walled, fluid filled appendix (Red arrow) with surrounding fluid. C: MRI Axial T2SSFSE image shows the retrocecal, thick walled, fluid filled appendix (Red arrow) with surrounding fluid
Data analysis
The performance of US and MRI in diagnosing AA was assessed relative to pathology findings. Inter-reader agreement for the visualization of appendix and accuracy of diagnosis between the original and re-review radiologist were calculated through Percent agreement, Cohen’s Kappa, sensitivity, specificity, positive predictive value, and negative predictive values. The Kappa statistic for inter-reader agreement was interpreted as < or = 0 as indicating no agreement and 0.01 – 0.20 as none to slight, 0.21 – 0.40 as fair, 0.41 – 0.60 as moderate, 0.61 – 0.80 as substantial, and 0.81 – 1.00 as almost perfect agreement [45].
We reported Cohen’s kappa to reflect the level of agreement removing the chance agreement 45. The propensity for the two groups of Radiologists to select the same categories was tested using McNemar’s test.
To predict visualization of appendix and appendicitis through MRI we used logistic regression model adjusted for gestational age, WBC, maternal age, and body temperature. All statistical analyses were conducted through SAS 9.4 (SAS Inc., Cary, N.C).
Results:
A total of 364 pregnant patients (15-45 years old; mean age: 26 years) presenting to the ER with abdominal pain and suspected AA were included in this study. The gestational age ranged from 3 weeks and 4 days to 38 weeks and 1 day. Appendectomy was performed on 31 patients. 363 patients underwent US as first diagnostic testing modality (Table 2), 1 patient underwent MRI as first imaging modality. The US appendix visualization rate was 1.65% (6/363) and correspondingly the non-visualization rate was 98.3% (357/363). Amongst the appendices visualized, US was positive for AA in 5 patients and was negative for AA in 1 patient. The results for the rereview expert Radiologist with US were similar. Thus, while Ultrasound was quite specific for the diagnosis of AA, the sensitivity was only 26.3%.
Table 2:
Comparison of US and Pathology findings
| Gold standard (Pathology*) | Total | |||
|---|---|---|---|---|
| Positive | Negative | |||
| US diagnosis | Positive | 5 | 1 | 6 |
| Negative | 14 | 343 | 357 | |
| Total | 19 | 344 | 363 | |
Follow up was the gold standard for all non-surgical US negative patients.
33 patients of the 364 (9.1%) underwent laparoscopy, 31 (8.5 %) of which had appendectomy. Of the 33, 19 (57.6%) were found to have pathology proven AA. Of these 19 patients, 5 (26.3%) were reported as positive for AA on ultrasound and only 1 out of these 5 patients underwent MRI confirmation. 9 of these 19 patients underwent an MRI. All these patients were categorized as positive on MRI. There were no false negative MRI results.
Out of 33 patients who underwent laparoscopy, 12 patients had an appendectomy but with a negative pathology result and 2 patients did not undergo appendectomy (normal looking appendix per the operating surgeon). US did not visualize the appendix in all these 14 patients. 10 of these 14 patients underwent MRI due to clinical suspicion prior to laparoscopy. Of these 10 patients, the original radiologist reported 4 positives while the re-review subspecialty radiologist identified 1 positive for AA. These were hence considered false positive MRI results for AA.
A total of 144 patients (39.5% of the 364) underwent MRI, of which 3 studies were nondiagnostic (patient did not complete the study). 141 patients had diagnostic quality MRI, the original radiologist correctly diagnosed 136 patients, and incorrectly diagnosed 5 patients (Table 3A). Upon rereview by the subspecialty radiologist, 139 of the 141 patients were correctly diagnosed by MRI, and 2 were incorrectly diagnosed (Table 3B).
Table 3:
Comparison of MRI findings read by: A. General Hospital (original) Radiologist and Pathology results, B. Subspecialty (Rereview) Radiologist and Pathology results
| A. | ||||
|---|---|---|---|---|
| Gold standard (Pathology*) | Total | |||
| Positive | Negative | |||
| MRI Diagnosis by original radiologist | Positive | 9 | 5 | 14 |
| Negative | 0 | 127 | 127 | |
| Total | 9 | 132 | 141 | |
| B. | ||||
| Gold standard (Pathology**) | Total | |||
| Positive | Negative | |||
| MRI Diagnosis by re-review radiologist | Positive | 9 | 2 | 11 |
| Negative | 0 | 130 | 130 | |
| Total | 9 | 132 | 141 | |
Follow up was the gold standard for all non-surgical MRI negative patients.
Follow up was the gold standard for all non-surgical MRI negative patients.
Both radiologists had 100% (9/9) sensitivity to diagnose AA with MRI, but the original radiologist had a 96% (127/132) specificity, while the re-review radiologist had a 98% (130/132) specificity. The original radiologist had a positive predictive value of 64% (9/14), and the re-review radiologist had a positive predictive value of 82% (9/11). Both radiologists had a negative predictive value of 100% for AA.
The original hospital radiologist visualized the appendix in 96/141 patients (68%) and reported AA in 13 including 2 patients with equivocal diagnoses. There were 45 patients (31.9%) in which the appendix could not be visualized. Re-review subspecialty radiologist visualized the appendix in 109/141 patients (77.3%) and reported AA in 11 including 2 patients with equivocal diagnoses. The subspecialty radiologist did not identify the appendix in 32 (22.6%) patients. The MRI findings in equivocal patients were fluid filled but non-dilated appendix with no wall thickening or nonspecific fluid around the non-dilated appendix. Equivocal category was deemed positive for AA and included in the positive group for statistical purposes.
Cohen’s Kappa analysis towards inter reader agreement was performed for MRI appendix visualization and overall accuracy for AA.
The raw percent inter-reader agreement for MRI visualization of the appendix was 87.9% (Table 4). This translates to a Cohen’s Kappa inter-reader agreement of 0.70 (95% confidence interval 0.5697-0.8293). Cohen Kappa between 0.61-0.80 is considered substantial.
Table 4:
Comparison of visualization of appendix between original and re-review radiologists
| Original radiologist | ||||
|---|---|---|---|---|
| Yes (n, %) | No (n, %) | Total | ||
| Re-review radiologist | Yes | 94 (66.7%) | 15 (10.6%) | 109 (77.3%) |
| No | 2 (1.4%) | 30 (21.3%) | 32 (22.7%) | |
| Total | 96 (68.1%) | 45 (31.9) | 141 | |
The raw percent inter-reader agreement for overall accuracy of AA was 98% (Table 5). This translates to a Cohen’s Kappa inter-reader agreement of 0.56 (95% confidence interval 0.1222-1). Cohen Kappa between 0.41 – 0.60 is considered moderate. McNemar’s test was not statistically significant (p=0.083) which reflects a propensity for the two groups of Radiologists to select the same categories. Figures 4 & 5 show 2 patients with discrepant MRI interpretation between the 2 groups of Radiologists.
Table 5:
Comparison of overall accuracy of acute appendicitis diagnosis between original and re-review radiologists
| Re-review radiologist | Original radiologist | ||
|---|---|---|---|
| Incorrectly diagnosed. (n, %) (TP*+TN?) | Incorrectly diagnosed (n, %) (FP#+FN**) | Total | |
| Correctly diagnosed (TP*+TN?) | 136 (96.5%) | 3 (2.1%) | 139 (98.6%) |
| Incorrectly diagnosed (FP#+FN**) | 0 (0%) | 2 (1.4%) | 2(1.4%) |
| Total | 136 (96.5%) | 5 (3.5%) | 141 |
TP = True Positive;
= True Negative;
= False Positive;
= False Negative
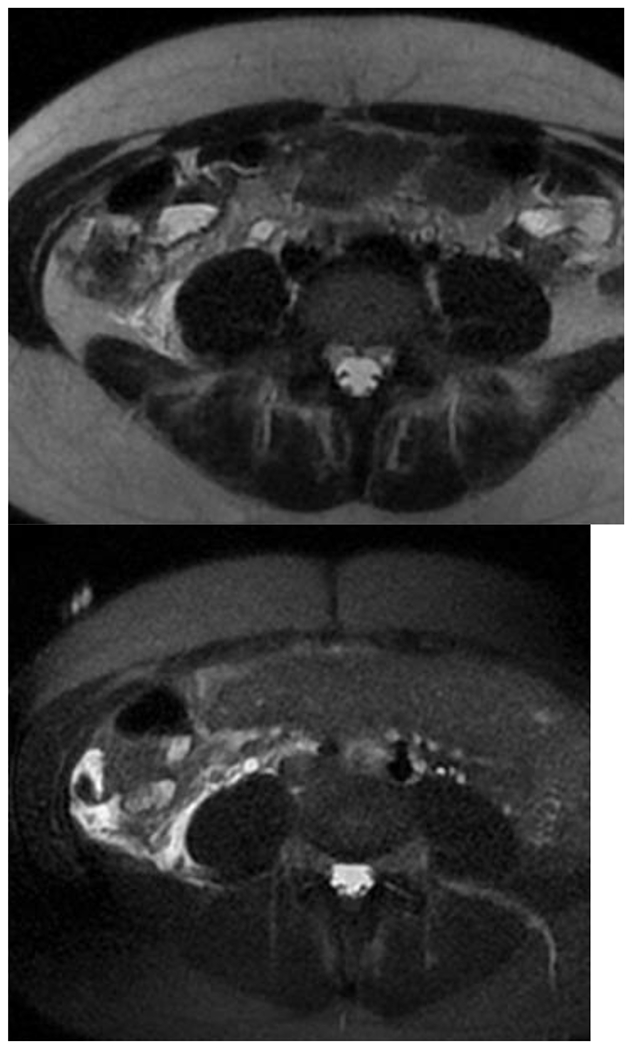
Figure 4:
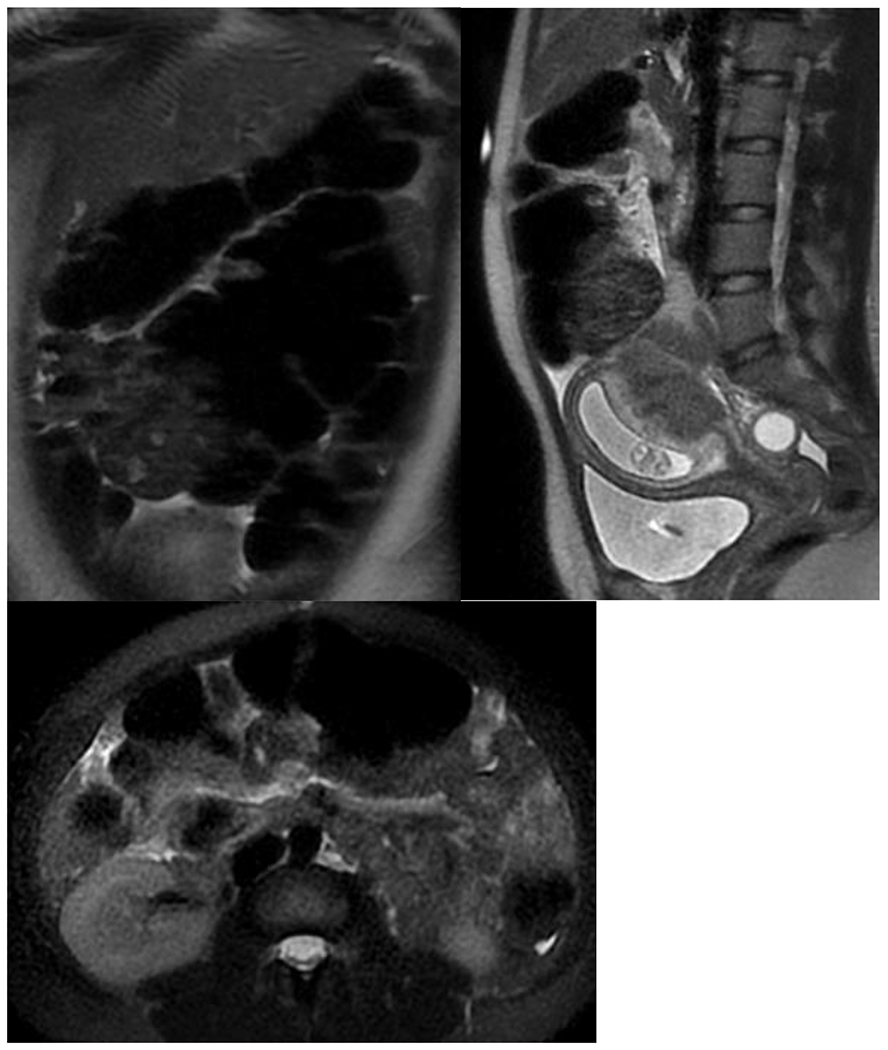
Discrepant interpretation between original and rereview radiologist: A: Coronal T2SSFSE image shows cecum in the LUQ of the abdomen. B: Sagittal T2SSFSE image denotes (red arrow) presumed inflamed appendix per the original interpreting Radiologist. C: Axial T2SSFSEFS image denotes (red arrow) presumed inflamed appendix per the original interpreting Radiologist. The finding was concluded to be segment of small bowel/terminal ileum by rereview Radiologist. The appendix was not visualized and study was deemed negative due to absence of secondary signs. Patient underwent Laparoscopic Appendectomy with no significant abnormality at final pathology.
Figure 5:
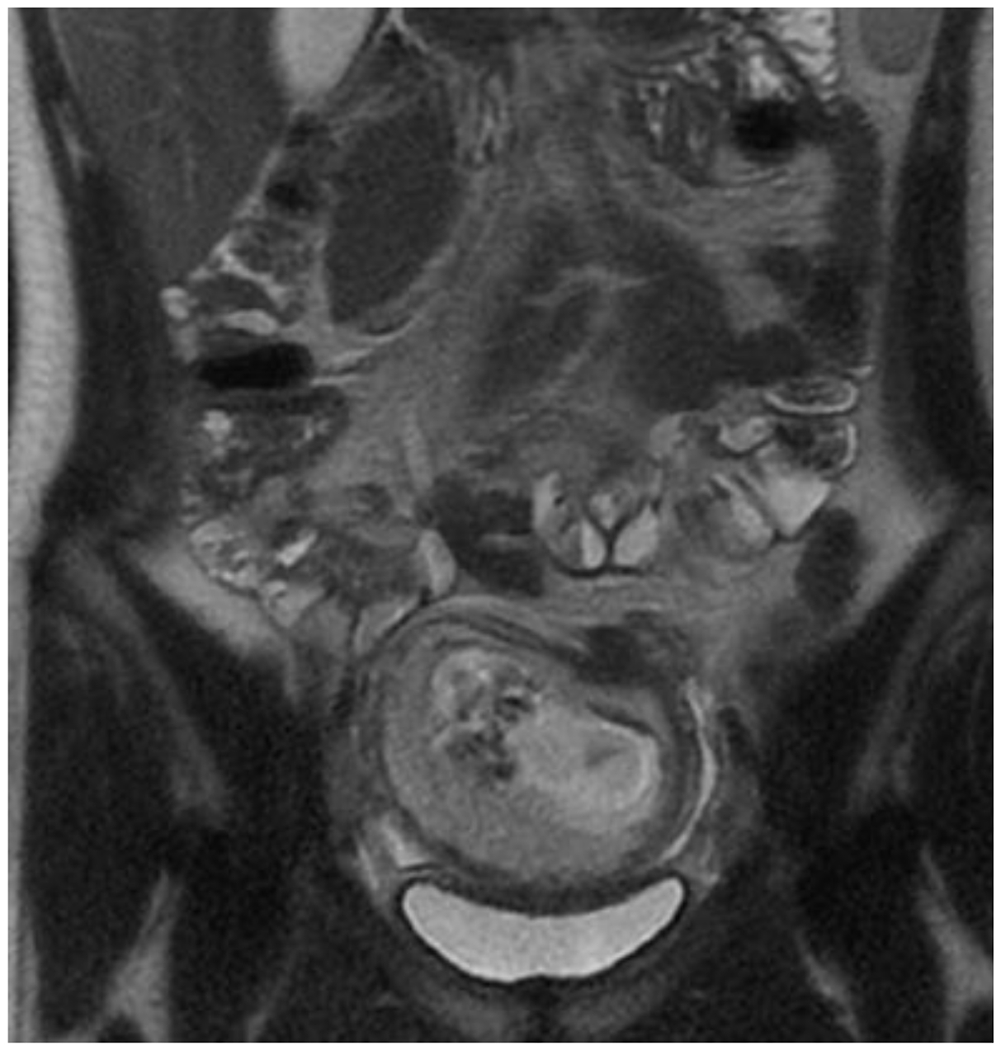
A&B: Axial T2SSFSE and T2SSFSEFS images demonstrate free fluid (green arrow) in the expected region of the appendix and around the cecum and right colon. These findings were interpreted as secondary signs of acute appendicitis by the original Radiologist. C: The normal appendix was visualized on Coronal T2SSFSE images (red arrow) by the rereview Radiologist and study was deemed negative. The patient underwent Laparoscopic Appendectomy, and the appendix was normal at pathology.
An additional analysis of our data found WBC count to be statistically significant for predicting AA. Of the 364 patients, 6 did not have complete laboratory data. In examining the 358 patients with recorded WBC count, leukocytosis was associated with a higher risk of having AA (p = 0.0089). The odds of having AA were increased by 1.112 times (95% CI 1.027 – 1.205) with 1 unit increase in WBC. However, there was no significant association of AA based on gestational age (p = 0.29), maternal age (p = 0.74), and body temperature (p = 0.36). We also found no significant association between gestational age and visualization of the appendix (p = 0.45).
The average clinical follow up time for the whole cohort of 364 patients was 5 months. This was part of their perinatal follow up evaluation. All surgical patients were also followed by general surgeons. There were no recurrent appendicitis symptoms in the non-surgical group during the follow up period.
Discussion:
Reports in the literature note that US has a high rate of non-visualization of the appendix up to 97%, especially as patients gestational age increases into the 2nd and 3rd trimesters 27. We also found a high rate of non-visualization in our data of 98.3%, resulting in low sensitivity 26.3% for diagnosis of AA. When US does visualize the appendix, our evidence shows radiologist interpretation is accurate (100% positive predictive value, and 100% specificity). It is a fast study with no significant attributable risks to the fetus, which argues for its continued use.
When the appendix is not visualized on ultrasound in a patient with clinical suspicion, MRI is generally agreed upon to be the next step in the diagnostic algorithm 2,18,32 Additionally, MRI can avoid a negative surgical exploration rate which can be up to 25-50% of patients with clinically suspected AA 17,31,33,42,46–48 in our cohort, the surgical exploration could have been avoided in 6 out of 10 patients for the original interpreting radiologist and in 9 out of 10 patients for the re-review radiologist.
Use of MRI in the evaluation of AA has been published as a reliable and accurate tool. In recent systematic review, MRI is reported to have a sensitivity of 91.8% and specificity of 97.9% when analyzing data in 2400 patients in 5 different countries 32. Pooling the results by country found 91.5% sensitivity and 98.1% specificity for studies in the USA. Other meta-analyses with data solely from the USA had sensitivity 95% and specificity 99.9% 2, which is similar to our Radiologists’ sensitivity of 100% and specificities of 96% and 98%. 32 Like others, we suggest that MRI can be used as first line imaging tool in pregnant patients with suspected AA 33,41,42. As with others, there were no patients in our cohort with AA and negative MRI examination 43. There is a paucity of evidence in literature analyzing inter-radiologist interpretation of MRI findings of AA in pregnancy. Another study evaluated the overall impression of AA and found a high degree of sub-specialty trained inter-radiologist agreement Kappa k = 0.81 – 1 regarding MRI findings of peri appendiceal soft-tissue stranding, and final overall impression of AA, however they reported K= 0.21 for visualization of the appendix 44. Our Radiologist group interpreting these studies were Board certified Radiologists working during day and night shifts. They were Body Imaging and Women’s Imaging trained Radiologists. The experience of the readers varied and ranged from 2-28 years. In addition, we did not base our inter-reader agreement on individual signs of AA. Rather our approach was based on individual radiologist experience in the visualization and diagnosis of AA. This we feel is more clinically relevant as diagnosis of AA is made by a collection of radiological findings.
Raw inter-reader agreement for visualization and overall accuracy respectively were 87.9 and 98%. Cohen’s Kappa analysis between general body and a sub-specialty trained research abdominal radiologist demonstrated substantial agreement for visualization of the appendix (k = 0.61 – 0.8), and moderate agreement for overall accuracy (k = 0.41 – 0.6). We attribute the less robust Kappa to the low population prevalence of disease, incorrect diagnosis, and the high levels of raw agreement. The original radiologist incorrectly diagnosed 5 patients with AA, and the re-review radiologist incorrectly diagnosed 2 patients with AA. Given this low prevalence of negatively identified patients, the moderate Kappa may not necessarily reflect low rates of overall agreement. We found McNemar’s test to not be statistically significant (p=0.083) which reflects a propensity for the two groups of Radiologists to select the same categories.
In contradiction with others, we found an association between leukocytosis and risk of having AA in our cohort of patients 49. However, there wasn’t any association between the gestational age and visualization of the appendix.
There are of course limitations to our study, the first being the retrospective observational analysis that introduces inherent bias. The original Radiologist reports were provided during day and night in a real-life clinical scenario. The duration of time available may not be similar to expert Radiologist read done in research like scenario. Despite this the raw agreement on visualization and overall accuracy was very high.
Most of the pregnant patients seen and discharged from our ER typically come back to our institution for their regular perinatal follow up. It is known that recurrent AA typically presents early after the first presentation. Most of these radiologically negative appendicitis patients would likely return to our hospital for follow up. As our tertiary referral hospital covers a wide geographic area, there is a very small chance of a patient returning to a different hospital and us having missed somebody with recurrent AA 50. Nonetheless a diligent review of electronic medical records did not reveal such a scenario.
To our knowledge this study is the largest single-center study to date, examining 364 patients with suspected AA during pregnancy. We had a lower incidence of AA at 5% (19/364) than other studies reported in the literature, 6% 44 and 9% 31. This lower incidence may have contributed to falsely elevated negative predictive value from our radiologists.
Additionally, the 100% sensitivity of our MRI results translates to a negative predictive value of 100% as well. There are potentially 127-130 patients with negative MRI studies, however no subsequent AA was recorded upon follow up. Further analysis with a larger cohort of patients is necessary to obtain a power high enough to validate our inter-radiologist kappa statistic.
Conclusion
MRI should be used as the first line imaging modality to diagnose AA in pregnant patients given its high accuracy. Negative MRI or non-visualization of appendix with no reported secondary signs virtually excludes acute AA. Our data suggests substantial agreement amongst Interpreting Body Radiologists with varied levels of experience. These results should allow for a lower threshold for such studies to be performed at community centers and reviewed by community Radiologists. MRI combined with appropriate surgical intervention will decrease the number of negative explorations and adverse outcomes for mother and fetus in this medical emergency.
Highlights:
Our data demonstrated that MRI has a higher sensitivity and specificity for identifying acute appendicitis in pregnant women than ultrasound.
It also showed there was a high level of inter-reader agreement between general body radiologist of varying levels of experience in MRI reading and an abdominal specialty expert research radiologist.
This suggests that MRI should be considered the first line imaging modality in pregnant patients suspected of having acute appendicitis.
Acknowledgements of Conflict of Interest:
No disclosures, conflict or competing of interest for Drs: Bestoun Ahmed, Jon Williams, William Gourash, Jun Zhang, Runjia Li, and Balasubramanya Rangaswamy. Dr. G.K. Balasubramani reports no conflicts of interest with the current study or manuscript and discloses that he serves as an advisor or consultant at New World Medical Inc., Ocular Therapeutix, Inc., and Sight Sciences, Inc.; and received grant funding from Merck &Co. Inc.
Funding:
The statistical analysis for this study was supported by the National Institutes of Health through Grant Number UL1 TR001857, Clinical and Translational Science Center of the University of Pittsburgh. There was no industry, or other financial or in-kind funding support utilized to carry out this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Andersson RE, Lambe M. Incidence of appendicitis during pregnancy. Int J Epidemiol 2001. Dec;30(6):1281–5. doi: 10.1093/ije/30.6.1281. [DOI] [PubMed] [Google Scholar]
- 2.Blumenfeld YJ, Wong AE, Jafari A, Barth RA, El-Sayed YY. MR imaging in cases of antenatal suspected appendicitis--a meta-analysis. J Matern Fetal Neonatal Med 2011. Mar;24(3):485–8. doi: 10.3109/14767058.2010.506227. Epub 2010 Aug 9. [DOI] [PubMed] [Google Scholar]
- 3.Wilasrusmee C, Sukrat B, McEvoy M, Attia J, Thakkinstian A. Systematic review and meta-analysis of safety of laparoscopic versus open appendicectomy for suspected appendicitis in pregnancy. Br J Surg 2012. Nov;99(11):1470–8. doi: 10.1002/bjs.8889. Epub 2012 Sep 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buser KB. Laparoscopic surgery in the pregnant patient: results and recommendations. JSLS 2009. Jan-Mar;13(1):32–5. [PMC free article] [PubMed] [Google Scholar]
- 5.Firstenberg MS, Malangoni MA. Gastrointestinal surgery during pregnancy. Gastroenterol Clin North Am 1998. Mar;27(1):73–88. doi: 10.1016/s0889-8553(05)70348-4. [DOI] [PubMed] [Google Scholar]
- 6.Zingone F, Sultan AA, Humes DJ, West J. Risk of acute appendicitis in and around pregnancy: a population-based cohort study from England. Ann Surg 2015. Feb;261(2):332–7. doi: 10.1097/SLA.0000000000000780. [DOI] [PubMed] [Google Scholar]
- 7.Freeland M, King E, Safcsak K, Durham R. Diagnosis of appendicitis in pregnancy. Am J Surg 2009. Dec;198(6):753–8. doi: 10.1016/j.amjsurg.2009.05.023. [DOI] [PubMed] [Google Scholar]
- 8.Mukherjee R, Samanta S. Surgical emergencies in pregnancy in the era of modern diagnostics and treatment. Taiwan J Obstet Gynecol 2019. Mar;58(2):177–182. doi: 10.1016/j.tjog.2019.01.001. [DOI] [PubMed] [Google Scholar]
- 9.Pitkin RM, Witte DL. Platelet and leukocyte counts in pregnancy. JAMA 1979. Dec 14;242(24):2696–8. [PubMed] [Google Scholar]
- 10.Spalluto LB, Woodfield CA, DeBenedectis CM, Lazarus E. MR imaging evaluation of abdominal pain during pregnancy: appendicitis and other nonobstetric causes. Radiographics 2012. Mar-Apr;32(2):317–34. doi: 10.1148/rg.322115057. [DOI] [PubMed] [Google Scholar]
- 11.Abbasi N, Patenaude V, Abenhaim HA. Evaluation of obstetrical and fetal outcomes in pregnancies complicated by acute appendicitis. Arch Gynecol Obstet 2014. Oct;290(4):661–7. doi: 10.1007/s00404-014-3276-7. Epub 2014 May 20. [DOI] [PubMed] [Google Scholar]
- 12.Silvestri MT, Pettker CM, Brousseau EC, Dick MA, Ciarleglio MM, Erekson EA. Morbidity of appendectomy and cholecystectomy in pregnant and nonpregnant women. Obstet Gynecol 2011. Dec;118(6):1261–1270. doi: 10.1097/AOG.0b013e318234d7bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dewhurst C, Beddy P, Pedrosa I. MRI evaluation of acute appendicitis in pregnancy. J Magn Reson Imaging 2013. Mar;37(3):566–75. doi: 10.1002/jmri.23765. [DOI] [PubMed] [Google Scholar]
- 14.McGory ML, Zingmond DS, Tillou A, Hiatt JR, Ko CY, Cryer HM. Negative appendectomy in pregnant women is associated with a substantial risk of fetal loss. J Am Coll Surg 2007. Oct;205(4):534–40. doi: 10.1016/j.jamcollsurg.2007.05.025. Epub 2007 Aug 23. [DOI] [PubMed] [Google Scholar]
- 15.Fonseca AL, Schuster KM, Kaplan LJ, Maung AA, Lui FY, Davis KA. The use of magnetic resonance imaging in the diagnosis of suspected appendicitis in pregnancy: shortened length of stay without increase in hospital charges. JAMA Surg 2014. Jul;149(7):687–93. doi: 10.1001/jamasurg.2013.4658. [DOI] [PubMed] [Google Scholar]; Erratum in: JAMA Surg. 2014. Jul;149(7):749. [Google Scholar]
- 16.Rapp EJ, Naim F, Kadivar K, Davarpanah A, Cornfeld D. Integrating MR imaging into the clinical workup of pregnant patients suspected of having appendicitis is associated with a lower negative laparotomy rate: single institution study. Radiology 2013;267:137–44. [DOI] [PubMed] [Google Scholar]
- 17.Pedrosa I, Lafornara M, Pandharipande PV, Goldsmith JD, Rofsky NM. Pregnant patients suspected of having acute appendicitis: effect of MR imaging on negative laparotomy rate and appendiceal perforation rate. Radiology 2009;250:749–57. [DOI] [PubMed] [Google Scholar]
- 18.Aggenbach L, Zeeman GG, Cantineau AE, Gordijn SJ, Hofker HS. Impact of appendicitis during pregnancy: no delay in accurate diagnosis and treatment. Int J Surg 2015. Mar;15:84–9. doi: 10.1016/j.ijsu.2015.01.025. Epub 2015 Jan 29. [DOI] [PubMed] [Google Scholar]
- 19.Hée P, Viktrup L. The diagnosis of appendicitis during pregnancy and maternal and fetal outcome after appendectomy. Int J Gynaecol Obstet 1999. May;65(2):129–35. doi: 10.1016/s0020-7292(99)00013-2. [DOI] [PubMed] [Google Scholar]
- 20.Expert Panel on Gastrointestinal Imaging, Garcia EM, Camacho MA, Karolyi DR, Kim DH, Cash BD, Chang KJ, Feig BW, Fowler KJ, Kambadakone AR, Lambert DL, Levy AD, Marin D, Moreno C, Peterson CM, Scheirey CD, Siegel A, Smith MP, Weinstein S, Carucci LR. ACR Appropriateness Criteria® Right Lower Quadrant Pain-Suspected Appendicitis. J Am Coll Radiol 2018. Nov;15(11S):S373–S387. doi: 10.1016/j.jacr.2018.09.033. [DOI] [PubMed] [Google Scholar]
- 21.Houston LE, Odibo AO, Macones GA. The safety of obstetrical ultrasound: a review. Prenat Diagn 2009. Dec;29(13):1204–12. doi: 10.1002/pd.2392. [DOI] [PubMed] [Google Scholar]
- 22.Torloni MR, Vedmedovska N, Merialdi M, Betrán AP, Allen T, González R, Platt LD; ISUOG-WHO Fetal Growth Study Group. Safety of ultrasonography in pregnancy: WHO systematic review of the literature and meta-analysis. Ultrasound Obstet Gynecol 2009. May;33(5):599–608. doi: 10.1002/uog.6328. [DOI] [PubMed] [Google Scholar]
- 23.Vu L, Ambrose D, Vos P, Tiwari P, Rosengarten M, Wiseman S. Evaluation of MRI for the diagnosis of appendicitis during pregnancy when ultrasound is inconclusive. J Surg Res 2009. Sep;156(1):145–9. doi: 10.1016/j.jss.2009.03.044. Epub 2009 May 3. [DOI] [PubMed] [Google Scholar]
- 24.Pedrosa I, Levine D, Eyvazzadeh AD, Siewert B, Ngo L, Rofsky NM. MR imaging evaluation of acute appendicitis in pregnancy. Radiology 2006. Mar;238(3):891–9. doi: 10.1148/radiol.2383050146. [DOI] [PubMed] [Google Scholar]
- 25.Hiersch L, Yogev Y, Ashwal E, From A, Ben-Haroush A, Peled Y. The impact of pregnancy on the accuracy and delay in diagnosis of acute appendicitis. J Matern Fetal Neonatal Med 2014. Sep;27(13):1357–60. doi: 10.3109/14767058.2013.858321. Epub 2013 Nov 15. [DOI] [PubMed] [Google Scholar]
- 26.Cobben LP, Groot I, Haans L, Blickman JG, Puylaert J. MRI for clinically suspected appendicitis during pregnancy. AJR Am J Roentgenol 2004. Sep;183(3):671–5. doi: 10.2214/ajr.183.3.1830671. [DOI] [PubMed] [Google Scholar]
- 27.Israel GM, Malguria N, McCarthy S, Copel J, Weinreb J. MRI vs. ultrasound for suspected appendicitis during pregnancy. J Magn Reson Imaging 2008. Aug;28(2):428–33. doi: 10.1002/jmri.21456. [DOI] [PubMed] [Google Scholar]
- 28.Lehnert BE, Gross JA, Linnau KF, Moshiri M. Utility of ultrasound for evaluating the appendix during the second and third trimester of pregnancy. Emerg Radiol 2012. Aug;19(4):293–9. doi: 10.1007/s10140-012-1029-0. Epub 2012 Feb 28. [DOI] [PubMed] [Google Scholar]
- 29.Smith MP, Katz DS, Lalani T, Carucci LR, Cash BD, Kim DH, Piorkowski RJ, Small WC, Spottswood SE, Tulchinsky M, Yaghmai V, Yee J, Rosen MP. ACR Appropriateness Criteria® Right Lower Quadrant Pain--Suspected Appendicitis. Ultrasound Q. 2015. Jun;31(2):85–91. doi: 10.1097/RUQ.0000000000000118. [DOI] [PubMed] [Google Scholar]
- 30.Aguilera F, Gilchrist BF, Farkas DT. Accuracy of MRI in Diagnosing Appendicitis during Pregnancy. Am Surg 2018. Aug 1;84(8):1326–1328. [PubMed] [Google Scholar]
- 31.Burke LM, Bashir MR, Miller FH, Siegelman ES, Brown M, Alobaidy M, Jaffe TA, Hussain SM, Palmer SL, Garon BL, Oto A, Reinhold C, Ascher SM, Demulder DK, Thomas S, Best S, Borer J, Zhao K, Pinel-Giroux F, De Oliveira I, Resende D, Semelka RC. Magnetic resonance imaging of acute appendicitis in pregnancy: a 5-year multiinstitutional study. Am J Obstet Gynecol 2015. Nov;213(5):693.e1–6. doi: 10.1016/j.ajog.2015.07.026. Epub 2015 Jul 26. [DOI] [PubMed] [Google Scholar]
- 32.Kave M, Parooie F, Salarzaei M. Pregnancy and appendicitis: a systematic review and meta-analysis on the clinical use of MRI in diagnosis of appendicitis in pregnant women. World J Emerg Surg 2019. Jul 22;14:37. doi: 10.1186/s13017-019-0254-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ramalingam V, LeBedis C, Kelly JR, Uyeda J, Soto JA, Anderson SW. Evaluation of a sequential multi-modality imaging algorithm for the diagnosis of acute appendicitis in the pregnant female. Emerg Radiol 2015. Apr;22(2):125–32. doi: 10.1007/s10140-014-1260-y. Epub 2014 Aug 23. [DOI] [PubMed] [Google Scholar]
- 34.Duke E, Kalb B, Arif-Tiwari H, Daye ZJ, Gilbertson-Dahdal D, Keim SM, Martin DR. A Systematic Review and Meta-Analysis of Diagnostic Performance of MRI for Evaluation of Acute Appendicitis. AJR Am J Roentgenol 2016. Mar;206(3):508–17. doi: 10.2214/AJR.15.14544. [DOI] [PubMed] [Google Scholar]
- 35.Kereshi B, Lee KS, Siewert B, Mortele KJ. Clinical utility of magnetic resonance imaging in the evaluation of pregnant females with suspected acute appendicitis. Abdom Radiol (NY) 2018. Jun;43(6):1446–1455. doi: 10.1007/s00261-017-1300-7. [DOI] [PubMed] [Google Scholar]
- 36.Long SS, Long C, Lai H, Macura KJ. Imaging strategies for right lower quadrant pain in pregnancy. AJR Am J Roentgenol. 2011. Jan;196(1):4–12. doi: 10.2214/ajr.10.4323. [DOI] [PubMed] [Google Scholar]
- 37.Patel D, Fingard J, Winters S, Low G. Clinical use of MRI for the evaluation of acute appendicitis during pregnancy. Abdom Radiol (NY) 2017. Jul;42(7):1857–1863. doi: 10.1007/s00261-017-1078-7. [DOI] [PubMed] [Google Scholar]
- 38.Wi SA, Kim DJ, Cho ES, Kim KA. Diagnostic performance of MRI for pregnant patients with clinically suspected appendicitis. Abdom Radiol (NY) 2018. Dec;43(12):3456–3461. doi: 10.1007/s00261-018-1654-5. [DOI] [PubMed] [Google Scholar]
- 39.Oto A, Ernst RD, Ghulmiyyah LM, Nishino TK, Hughes D, Chaljub G, Saade G. MR imaging in the triage of pregnant patients with acute abdominal and pelvic pain. Abdom Imaging 2009. Mar-Apr;34(2):243–50. doi: 10.1007/s00261-008-9381-y. [DOI] [PubMed] [Google Scholar]
- 40.Masselli G, Brunelli R, Casciani E, Polettini E, Bertini L, Laghi F, Anceschi M, Gualdi G. Acute abdominal and pelvic pain in pregnancy: MR imaging as a valuable adjunct to ultrasound? Abdom Imaging 2011. Oct;36(5):596–603. doi: 10.1007/s00261-010-9654-0. [DOI] [PubMed] [Google Scholar]
- 41.Theilen LH, Mellnick VM, Longman RE, Tuuli MG, Odibo AO, Macones GA, Cahill AG. Utility of magnetic resonance imaging for suspected appendicitis in pregnant women. Am J Obstet Gynecol 2015. Mar;212(3):345.e1–6. doi: 10.1016/j.ajog.2014.10.002. Epub 2014 Oct 5. [DOI] [PubMed] [Google Scholar]
- 42.Jang KM, Kim SH, Choi D, Lee SJ, Rhim H, Park MJ. The value of 3D T1-weighted gradient-echo MR imaging for evaluation of the appendix during pregnancy: preliminary results. Acta Radiol 2011. Oct 1;52(8):825–8. doi: 10.1258/ar.2011.110116. Epub 2011 Aug 11. [DOI] [PubMed] [Google Scholar]
- 43.Konrad J, Grand D, Lourenco A. MRI: first-line imaging modality for pregnant patients with suspected appendicitis. Abdom Imaging 2015. Oct;40(8):3359–64. doi: 10.1007/s00261-015-0540-7. [DOI] [PubMed] [Google Scholar]
- 44.Tsai R, Raptis C, Fowler KJ, Owen JW, Mellnick VM. MRI of suspected appendicitis during pregnancy: interradiologist agreement, indeterminate interpretation, and the meaning of non-visualization of the appendix. Br J Radiol. 2017. Nov;90(1079):20170383. doi: 10.1259/bjr.20170383. Epub 2017 Sep 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb) 2012;22(3):276–82. [PMC free article] [PubMed] [Google Scholar]
- 46.Yilmaz HG, Akgun Y, Bac B, Celik Y. Acute appendicitis in pregnancy--risk factors associated with principal outcomes: a case control study. Int J Surg. 2007. Jun;5(3):192–7. doi: 10.1016/j.ijsu.2006.05.005. Epub 2006 Jun 21. [DOI] [PubMed] [Google Scholar]
- 47.McGory ML, Zingmond DS, Tillou A, Hiatt JR, Ko CY, Cryer HM. Negative appendectomy in pregnant women is associated with a substantial risk of fetal loss. J Am Coll Surg 2007. Oct;205(4):534–40. doi: 10.1016/j.jamcollsurg.2007.05.025. Epub 2007 Aug 23. [DOI] [PubMed] [Google Scholar]
- 48.Thompson MM, Kudla AU, Chisholm CB. Appendicitis during pregnancy with a normal MRI. West J Emerg Med 2014. Sep;15(6):652–4. doi: 10.5811/westjem.2014.7.22988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mourad J, Elliott JP, Erickson L, Lisboa L. Appendicitis in pregnancy: new information that contradicts long-held clinical beliefs. Am J Obstet Gynecol 2000. May; 182(5):1027–9. doi: 10.1067/mob.2000.105396. [DOI] [PubMed] [Google Scholar]
- 50.Al-Katib S, Sokhandon F, Farah M. MRI for appendicitis in pregnancy: is seeing believing? clinical outcomes in cases of appendix nonvisualization. Abdom Radiol (NY) 2016. Dec;41(12):2455–2459. doi: 10.1007/s00261-016-0864-y. [DOI] [PubMed] [Google Scholar]


