Summary
Background
Prior research provides suggestive evidence on an association between stress-related disorders and mortality. No previous study has however addressed the role of familial confounding on such association.
Methods
We conducted a nationwide cohort study of 189,757 individuals with a first-onset stress-related disorder between January 1, 1981 and December 31, 2016 in Sweden (i.e., exposed patients), 1,896,352 matched unexposed individuals, and 207,479 unaffected full siblings of the exposed patients. Cox proportional hazards models were used to estimate the hazard ratios (HRs) and 95% confidence intervals (CIs) of all-cause and cause-specific mortality.
Findings
During a mean follow-up of 9.42 years, an elevated risk of all-cause mortality was observed during the entire follow-up among patients with stress-related disorders, compared with either unexposed individuals or their unaffected full siblings. Such excess risk was most pronounced within the first year after diagnosis of stress-related disorders (HR, 3.19 [95% CI, 2.87-3.54] in population-based comparison; HR, 3.21 [95% CI, 2.56-4.02] in sibling-based comparison). The excess risk decreased but remained statistically significant thereafter (HR, 1.64 [95% CI, 1.60-1.67] in population-based comparison; HR, 1.61 [95% CI, 1.54-1.68] in sibling-based comparison). An increased risk was observed for almost all cause-specific mortality, with greater risk increase for deaths from unnatural causes, especially suicide, and potentially avoidable causes.
Interpretation
Stress-related disorders were associated with an increased risk of all-cause mortality and multiple cause-specific mortality, and the risk elevation was independent of familial confounding. The excess mortality attributable to unnatural causes and potentially avoidable causes highlights the importance of clinical surveillance of major health hazards among patients with stress-related disorders.
Funding
EU Horizon 2020 Research and Innovation Action Grant, 1.3.5 Project for Disciplines of Excellence at West China Hospital of Sichuan University, National Natural Science Foundation of China, Icelandic Research Fund (Grant of Excellence), ERC Consolidator Grant, and Swedish Research Council.
Keywords: Stress-related disorders, Post-traumatic stress disorder, Reaction to severe stress, All-cause mortality, Cause-specific mortality, Avoidable mortality
Research in context.
Evidence before this study
We searched PubMed up to Nov 30, 2021, with no language restrictions, using the search terms: (“mortality” and (“stress” or “stress-related disorders” or “stress disorders” or “stress reaction” or “post-traumatic stress disorder” or “PTSD” or “acute stress reaction” or “adjustment disorder”) and (“cohort” or “longitudinal”)). This search yielded 29 eligible studies, after title and abstract screening. In addition, we also searched Google Scholar, as a supplement source, using same search items and found 8 additional relevant studies. Most of these 37 identified studies, focusing on US veterans, disaster survivors, inpatients, female nurses, and general population, suggested a possible deleterious role of stress-related disorders on mortality. Specifically, individuals with PTSD or other stress-related disorders were at an elevated risk of all-cause mortality, suicide, and cardiovascular mortality. However, little knowledge has been obtained about the association between all stress-related disorders (including adjustment disorder) and all-cause mortality as well as multiple cause-specific mortality, and no study has assessed the role of familial confounding, due to shared genetic or non-genetic factors (e.g., early environmental exposures and lifestyle) within a family, on such associations.
Added value of this study
To the best of our knowledge, this is the first large-scale study to comprehensively assess the risk of all-cause and cause-specific mortality after diagnosis of stress-related disorders using both population- and sibling-based comparisons. We found that patients with stress-related disorders were at increased risk of all-cause and multiple cause-specific mortality, especially during the first year following the diagnosis, compared with matched unexposed individuals or their unaffected full siblings. The risk elevation was most pronounced for mortality due to unnatural causes (especially suicide) and potentially avoidable (treatable or preventable) causes, both immediately after diagnosis and in the long run. The limited differences in results between the population and sibling-based comparisons add novel evidence to suggest that the excess mortality in relation to stress-related disorders is unlikely attributable to familial confounding.
Implications of all evidence available
These findings underscore the importance of clinical surveillance and, when needed, intervention programs among individuals with stress-related disorders, with the ultimate goal of preventing premature death.
Alt-text: Unlabelled box
Introduction
Stress-related disorders refer to a group of psychiatric disorders, including post-traumatic stress disorder (PTSD), acute stress reaction, and adjustment disorder and other stress reactions, subsequent to traumatic or stressful life events.1,2 Specifically, PTSD and acute stress reaction result from a life-threatening trauma (e.g., combat, natural disaster, and life-threatening diseases). While PTSD stands for a long-lasting and serious psychiatric reaction characterized by re-experiencing, avoidance, negative cognitions and mood, and hyperarousal, acute stress reaction demonstrates similar symptoms but in a transient form.3 Adjustment disorder is usually triggered by other stressful life events (i.e., an identifiable and stressful life change, such as divorce and job loss),1 demonstrating overlapping symptoms and physiological dysfunction with PTSD and acute stress reaction.4,5 Growing evidence suggests that individuals with stress-related disorders have elevated risks of psychiatric comorbidities,2 less healthy lifestyles (e.g., smoking,6 poor diet,7 and lack of physical activity),6,8 and multiple somatic diseases (e.g., cardiovascular disease,9 life-threatening infection,10 autoimmune disease,11 and neurodegenerative disease).12 Although all these adverse health conditions have been shown to be associated with premature death,13, 14, 15 whether there is excess mortality associated with stress-related disorders remains less explored.
Prior studies, focusing on PTSD16, 17, 18, 19, 20 and US military veterans,17, 18, 19, 20 have indicated a possible deleterious role of stress-related disorders on mortality. More recently, a Danish register-based study reported a higher risk of all-cause mortality and suicide after diagnosis of severe stress or adjustment disorders.21 Besides studying stress-related disorders directly, psychiatric comorbidities of stress-related disorders (e.g., depression22 and substance use disorder23) have also been suggested to be associated with even greater risk of mortality. As genome-wide association studies (GWAS) have identified genetic variants for the susceptibility to both stress-related disorders24 and mortality,25 it is possible that a shared genetic predisposition to both traits may contribute to the observed associations. Further, an association between stress-related disorders and mortality might also be attributed to non-genetic factors that cluster within a family, such as early environmental exposures,26 parenting style,27 and lifestyle.28 Regardless, no study has to our knowledge addressed the role of familial confounding due to shared genetic or non-genetic factors on the association of stress-related disorders with all-cause as well as cause-specific mortality.
To this end, leveraging the nationwide population and health registers in Sweden, we conducted a population-based and sibling-controlled cohort study to assess the association of stress-related disorders with all-cause and cause-specific mortality. We hypothesized that patients with stress-related disorders were at increased risk of all-cause and multiple cause-specific mortality, compared with individuals of the same age and sex who had no stress-related disorders as well as their unaffected full siblings, and that the risk elevation was independent of familial confounding. Given the growing burden of stress-related disorders in the context of the current coronavirus disease 2019 (COVID-19) pandemic29 and great public health importance of mortality, such analysis may provide essential information for interventions targeted to reduce the risk of premature mortality among traumatized individuals.
Methods
Study design
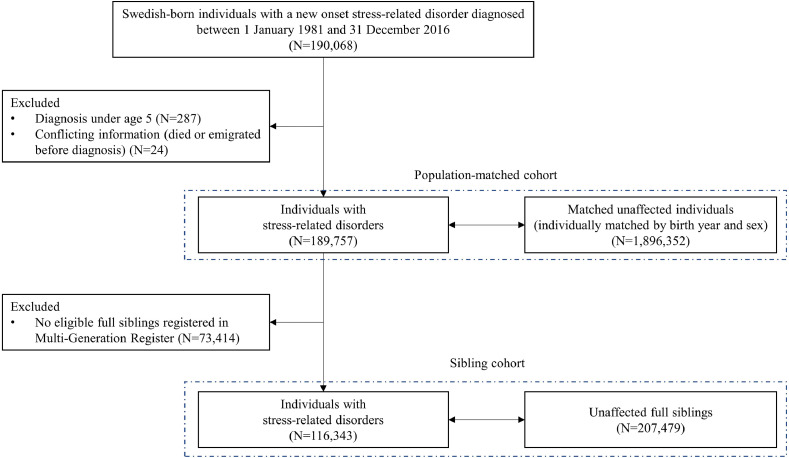
We first identified 8,753,501 individuals who were born during 1932–2011 in Sweden, according to the Swedish Total Population Register. Using the unique personal identification numbers assigned to all Swedish residents, these individuals were cross-linked to the Swedish National Patient Register, Cause of Death Register, Migration Register, and Multi-Generation Register, to retrieve health and family information. The National Patient Register was established in 1964 and has a nationwide coverage on inpatient care since 1987 (86% of all psychiatric inpatient care since 1981) and included more than 80% of specialist-based outpatient care since 2001.30 Through this register, we identified 190,068 patients who received their first diagnosis of stress-related disorders between January 1st 1981 and December 31st 2016 (i.e., exposed group) (Figure 1). We excluded patients with a diagnosis of stress-related disorders under age five31 (N=287) or conflicting information (died or emigrated before diagnosis) (N=24), leaving 189,757 exposed patients for further analyses. Up to 10 unexposed individuals who were free of stress-related disorders at the diagnosis date of the exposed patient (i.e., the index date for both exposed and matched unexposed individuals) were then randomly selected from the study base for each exposed patient, using the method of incidence density sampling.32 The unexposed individuals were individually matched to the exposed patient by birth year and sex. In this population-based matched cohort, we included a total of 1,896,352 unexposed individuals.
Figure 1.
Study design.
To control for familial confounding, we also constructed a sibling cohort. We identified all clusters of full siblings (i.e., with the same biological father and mother) who were discordant for stress-related disorders through the Multi-Generation Register. The unaffected siblings were defined as siblings who were free of stress-related disorders at the diagnosis date of their affected sibling (i.e., the index date for both affected and unaffected full siblings). This sibling cohort included 116,343 exposed patients and their 207,479 unaffected full siblings (Figure 1).
This study was approved by the Regional Ethical Review Board in Stockholm, Sweden. The requirement for informed consent was waived by this approval.
Follow-up of the cohorts
All individuals of the population-based matched cohort and the sibling cohort were followed from the index date until death, emigration, or the end of follow-up (December 31, 2016), whichever occurred first. The follow-up of the matched unexposed individuals and unaffected full siblings were additionally censored at the time of their diagnosis of stress-related disorders, if any, during the follow-up.
Ascertainment of stress-related disorders
We ascertained the occurrence of a first inpatient or outpatient hospital visit with a stress-related disorder as the primary diagnosis in the National Patient Register, according to the 8th, 9th, or 10th Swedish revisions of the International Classification of Diseases (ICD) codes 307 (ICD-8), 308 or 309 (ICD-9), and F43 (ICD-10) (Supplementary Table 1). Stress-related disorders were then classified as PTSD (ICD-9: 309B; ICD-10: F43.1), acute stress reaction (ICD-9: 308, 309A; ICD-10: F43.0), and adjustment disorder and other stress reactions (ICD-9: 309X, 309B; ICD-10: F43.2, F43.8, F43.9). Because other stress-related disorders, especially acute stress reaction, might be a precursor of subsequent PTSD,33 all patients who received a PTSD diagnosis within one year after their first stress-related disorder diagnosis were counted as PTSD patients.
All-cause mortality and cause-specific mortality
All-cause mortality and cause-specific mortality were defined as any death and death from a specific underlying cause of death in the Cause of Death Register, respectively. The Cause of Death Register provides information on the underlying as well as contributory causes of all deaths in Sweden, as well as deaths of Swedish residents that died aboard, since 1952. Specifically, we categorized cause-specific mortality as mortality due to natural or unnatural causes (Supplementary Table 1). Mortality due to natural causes was further classified as deaths due to infection, cancer, endocrine, nutritional and metabolic diseases, mental and behavioral disorders, diseases of nervous system, diseases of circulatory system, diseases of respiratory system, and diseases of digestive system. Mortality due to unnatural causes was classified as suicide (intentional self-harm and events of undetermined intent) and deaths due to other external causes (e.g., accidents, fall, and assaults). We also defined potentially avoidable deaths which are considered to be treatable (i.e., through good-quality health care) or preventable (i.e., through public health intervention), based on the definition of the Office for National Statistics, UK34 (Supplementary Table 1).
Covariates
We extracted information on the highest educational level, yearly family income level, and marital status from the Swedish Longitudinal Integration Database for Health Insurance and Labour Market study database. Based on diagnoses in the National Patient Register, we calculated a Charlson Comorbidity Index35 (CCI) score, as a measure of disease burden due to pre-existing somatic diseases. We used the most updated information before the index date for these covariates. As stress-related disorders commonly co-occur with other psychiatric disorders,2 we also obtained information on diagnoses of other psychiatric disorders from the National Patient Register. We defined such diagnoses received more than three months before the index date as history of other psychiatric disorders (for exposed patients, matched unexposed individuals, and unaffected full siblings), while those received from three months before to one year after the index date as psychiatric comorbidity (for exposed patients only). The ICD codes used are listed in Supplementary Table 1.
Table 1.
Baseline characteristics and follow-up data of study participants.
| Characteristics | Population-based matched cohort |
Sibling cohort |
||
|---|---|---|---|---|
| Exposed patients | Matched unexposed individuals | Exposed patients | Unaffected full siblings | |
| No. of participants | 189,757 | 1,896,352 | 116,343 | 207,479 |
| Age at entry, mean (SD), years | 37.33 (14.56) | 37.33 (14.56) | 37.55 (14.13) | 38.67 (15.28) |
| Sex, No. (%) | ||||
| Male | 71,750 (37.81) | 717,136 (37.82) | 44,115 (37.92) | 106,138 (51.16) |
| Female | 118,007 (62.19) | 1,179,216 (62.18) | 72,228 (62.08) | 101,341 (48.84) |
| Educational level, No. (%), years | ||||
| <9 | 7,061 (3.72) | 65,455 (3.45) | 4,099 (3.52) | 12,138 (5.85) |
| 9-12 | 126,965 (66.91) | 1,141,889 (60.22) | 77,402 (66.53) | 133,356 (64.27) |
| >12 | 47,691 (25.13) | 625,442 (32.98) | 30,800 (26.47) | 52,488 (26.26) |
| Unknown | 8,040 (4.24) | 63,566 (3.35) | 4,042 (3.48) | 7,497 (3.62) |
| Marital status, No. (%) | ||||
| Single | 101,139 (53.30) | 998,289 (52.64) | 61,609 (52.95) | 99,255 (47.84) |
| Married or cohabiting | 46,510 (24.51) | 667,338 (35.19) | 29,796 (25.61) | 75,113 (36.20) |
| Divorced or widowed | 35,122 (18.51) | 170,749 (9.00) | 21,337 (18.34) | 23,249 (11.21) |
| Unknown | 6,986 (3.68) | 59,976 (3.17) | 3,601 (3.10) | 9,862 (4.75) |
| Yearly family income level, No. (%) | ||||
| Lowest 20% | 62,057 (32.70) | 343,459 (18.11) | 29,424 (25.29) | 33,554 (16.17) |
| Middle | 98,373 (51.84) | 1,118,046 (58.96) | 64,105 (55.10) | 124,633 (60.07) |
| Top 20% | 22,991 (12.12) | 382,371 (20.16) | 19,566 (16.82) | 43,337 (20.89) |
| Unknown | 6,336 (3.34) | 52,476 (2.77) | 3,248 (2.79) | 5,955 (2.87) |
| Charlson Comorbidity Index, No. (%) | ||||
| 0 | 145,486 (76.67) | 1,604,120 (84.59) | 90,313 (77.63) | 169,965 (81.92) |
| 1 | 29,170 (15.37) | 204,475 (10.78) | 17,115 (14.71) | 26,018 (12.54) |
| ≥2 | 15,101 (7.96) | 87,757 (4.63) | 8,915 (7.66) | 11,496 (5.54) |
| Type of stress-related disorders, No. (%) | ||||
| PTSD | 14,521 (7.65) | - | 8,376 (7.20) | - |
| Acute stress reaction | 81,948 (43.19) | - | 50,127 (43.09) | - |
| Adjustment disorder and other stress reactions | 93,288 (49.16) | - | 57,840 (49.72) | - |
| History of other psychiatric disordersa, No. (%) | ||||
| Yes | 73,602 (38.79) | 177,663 (9.37) | 43,330 (37.24) | 28,767 (13.87) |
| No | 116,155 (61.21) | 1,718,689 (90.63) | 73,013 (62.76) | 178,712 (86.13) |
| Psychiatric comorbidityb, No. (%) | ||||
| Yes | 40,001 (21.08) | - | 24,935 (21.43) | - |
| No | 149,756 (78.92) | - | 91,408 (78.57) | - |
| Follow-up time, mean (SD), years | 9.15 (7.75) | 9.45 (7.97) | 9.30 (7.79) | 10.04 (8.25) |
| Number of deaths (mortalityc) | 13,812 (7.95) | 55,761 (3.11) | 7,825 (7.23) | 8,898 (4.27) |
History of other psychiatric disorders was defined as the first diagnosis of any psychiatric disorders, other than stress-related disorders, >3 months before the index date.
Psychiatric comorbidity was defined as the first diagnosis of any psychiatric disorders, other than stress-related disorders, from 3 months before to 1 year after diagnosis of stress-related disorders.
Per 1,000 person-years, unadjusted.
Statistical analysis
As the elevation of mortality following a diagnosis of stress-related disorders may be time-dependent,17 we first visualized the association of stress-related disorders with all-cause mortality by time since diagnosis using flexible parametric models. Because of the pronounced risk elevation during the first year after diagnosis (Supplementary Fig. 1), we assessed the relative risk of all-cause and cause-specific mortality within the first year (i.e., as one period, as well as during first month, 2-3 months, 4-6 months, and 7-11 months) and beyond the first year after a diagnosis of stress-related disorders separately, using hazard ratios (HRs) derived from Cox model. The proportional hazard assumptions for Cox models were tested graphically and by Schoenfeld residuals, and no obvious violation of this assumption was observed.
In the population-based matched cohort, we stratified all analyses by the matching identifiers (birth year and sex), with partial (models 1-3) or full (model 4) adjustment for the highest educational level (<9 years, 9-12 years, >12 years, or unknown), yearly family income level (top 20%, middle, lowest 20%, or unknown), marital status (single, married/cohabiting, divorced/widowed, or unknown), CCI score, and history of other psychiatric disorders (yes or no). The missing data of covariates (e.g., educational level) were marked as unknown. These variables were then included in the Cox models as nominal variables. The analyses were first performed for any stress-related disorder and then for PTSD, acute stress reaction, and adjustment disorder and other stress reactions separately. In addition to all-cause mortality, we estimated HRs for cause-specific mortality and potentially avoidable mortality separately.
In the sibling cohort, we repeated the main analyses using Cox models stratified by family identifiers after adjustment for birth year, sex, and all covariates.
In stratification analyses, HRs were calculated separately by sex, age at cohort entry (by tertile distribution: ≤28 years, 29-42 years, or ≥43 years), calendar year at cohort entry (1981-1996, 1997-2006, or 2007-2016), the highest educational level (<9 years, 9-12 years, or >12 years), CCI score (0, 1, or ≥2), and history of other psychiatric disorders (yes or no). The difference between HRs was assessed by introducing an interaction term to the Cox models. We further analyzed the exposed patients with or without psychiatric comorbidity (any other psychiatric disorder, depression, anxiety, and substance use disorders), as well as by the type (inpatient or outpatient) and intensity (<2 times or ≥2 times) of psychiatric care received within one year after diagnosis. Wald test was used to examine the difference of HRs between groups.
To account for the impact of competing risk in the analysis of cause-specific mortality (i.e., deaths from other causes removed individuals from being at risk of death due to the specific cause of interest), we estimated the relative risk of cause-specific mortality and potentially avoidable mortality by sub-hazard ratios (SHRs) based on the modified Cox model developed by Fine and Gray.36 Finally, we assessed residual confounding not accounted for by multivariable analysis and sibling comparison, using the E values based on the method of Vanderweele,37 to assess the minimum strength of unmeasured confounding required to explain the observed effect estimates.
All analyses were conducted in SAS statistical software version 9.4 (SAS Institute, Cary, NC) and Stata 15.1 (STATA, College Station, TX). A 2-sided P<0.05 was considered statistically significant.
Role of the funding source
The funders had no role in the study design, data collection, data analysis, data interpretation, or writing of the manuscript. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
With a total of 19,653,565 accumulated person-years in the population-based matched cohort, the mean follow-up time was 9.15 (standard deviation [SD], 7.75) and 9.45 (SD, 7.97) years for exposed and unexposed individuals, respectively (Table 1). The mean age at diagnosis of stress-related disorders was 37.33 (SD, 14.56) years and 37.81% of the exposed patients were male. Compared with matched unexposed individuals, individuals with stress-related disorders were more likely to be divorced or widowed (18.51% vs 9.00%) and had lower family income level (lowest 20%, 32.70% vs 18.11%) but higher burden of somatic diseases (CCI score ≥1, 23.33% vs 15.41%) and history of other psychiatric disorders (38.79% vs 9.37%). In the sibling cohort, the mean follow-up time was 9.30 (SD, 7.79) and 10.04 (SD, 8.25) years for exposed patients and their unaffected full siblings, respectively. We observed similar discrepancies regarding these characteristics between exposed patients and their unaffected full siblings, although the differences were smaller than those of the population-based comparison (Table 1).
All-cause mortality
During follow-up of the population-based matched cohort, 13,812 and 55,761 deaths were identified among the exposed and unexposed individuals (crude mortality rate, 7.95 and 3.11 per 1,000 person-years, respectively). According to the flexible parametric model, the most pronounced risk elevation of all-cause mortality was observed immediately after diagnosis of a stress-related disorder, followed by a rapid decline within the first year of follow-up (Supplementary Fig. 1). The magnitude of association was stabilized after the first year and remained statistically significant over the entire follow-up. This was consistent with the risk pattern revealed by the fully adjusted Cox models (Table 2 and Supplementary Table 2). Compared with unexposed individuals, patients with stress-related disorders were at 3-fold risk of all-cause mortality within the first year of follow-up (HR, 3.19 [95% CI, 2.87-3.54]) which decreased rapidly with time (HR, 6.04 [95% CI, 2.50-14.59] for the first month, 4.04 [95% CI, 2.76-5.92] for 2-3 months, 3.87 [95% CI, 3.03-4.94] for 4-6 months, and 2.85 [95% CI, 2.51-3.24] for 7-11 months), and 1.6-fold risk thereafter (HR, 1.64 [95% CI, 1.60-1.67]). In the sibling cohort, 7,825 and 8,898 deaths were identified among the exposed patients and their unaffected full siblings, respectively, corresponding to a crude mortality rate of 7.23 and 4.27 per 1,000 person-years. A similar temporal pattern of the association was illustrated by flexible parametric model as well as Cox models stratified by follow-up period (Supplementary Fig. 1). The HRs derived from fully adjusted Cox models were 3.21 (95% CI, 2.56-4.02) for the first year of follow-up and 1.61 (95% CI, 1.54-1.68) thereafter (Table 2).
Table 2.
Hazard ratios (HRs) with 95% confidence intervals (CIs) for all-cause mortality among patients with stress-related disorders, compared to their matched unexposed individuals or unaffected full siblings, during or beyond the first year of follow-up.
| Model information | Population-based matched cohort |
Sibling cohort |
||
|---|---|---|---|---|
| No. of deaths (mortalitya) in exposed/unexposed individuals | HR (95% CI) | No. of deaths (mortalitya) in exposed/unexposed individuals | HR (95% CI) | |
| ≤1 year of follow-up | ||||
| Model 1: adjusted for birth year, sex | 2,023 (10.74)/3,305 (1.75) |
6.22 (5.88-6.57) | 1,123 (9.72)/492 (2.38) |
4.83 (4.28-5.44) |
| Model 2: Model 1 + educational level, yearly family income level, marital status | 4.61 (4.21-5.05) | 3.84 (3.17-4.65) | ||
| Model 3: Model 2 + Charlson comorbidity index | 4.15 (3.75-4.58) | 3.81 (3.07-4.72) | ||
| Model 4: Model 3 + history of other psychiatric disorders | 3.19 (2.87-3.54) | 3.21 (2.56-4.02) | ||
| Subtypes of stress-related disordersb | ||||
| PTSD | 83 (5.74)/196 (1.36) | 2.78 (1.68-4.61) | 46 (5.51)/24 (1.64) | 5.21 (0.34-80.36) |
| Acute stress reaction | 1,040 (12.81)/1,539 (1.89) | 3.53 (3.06-4.10) | 589 (11.85)/225 (2.52) | 3.52 (2.57-4.83) |
| Adjustment disorder and other stress reactions | 900 (9.71)/1,570 (1.69) | 2.90 (2.48-3.40) | 488 (8.49)/243 (2.37) | 2.93 (2.09-4.13) |
| >1 year of follow-up | ||||
| Model 1: adjusted for birth year, sex | 11,789 (7.58)/50,835 (3.20) |
2.54 (2.49-2.59) | 6,672 (6.90)/8,229 (4.42) |
2.07 (1.99-2.15) |
| Model 2: Model 1 + educational level, yearly family income level, marital status | 2.20 (2.16-2.25) | 1.90 (1.83-1.98) | ||
| Model 3: Model 2 + Charlson comorbidity index | 2.05 (2.00-2.09) | 1.82 (1.75-1.90) | ||
| Model 4: Model 3 + history of other psychiatric disorders | 1.64 (1.60-1.67) | 1.61 (1.54-1.68) | ||
| Subtypes of stress-related disordersb | ||||
| PTSD | 633 (6.69)/2,567 (2.68) | 1.63 (1.48-1.81) | 353 (6.12)/463 (4.27) | 1.45 (1.21-1.75) |
| Acute stress reaction | 5,119 (7.84)/20,952 (3.15) | 1.67 (1.62-1.74) | 2,947 (7.28)/3,506 (4.49) | 1.64 (1.54-1.75) |
| Adjustment disorder and other stress reactions | 6,037 (7.47)/27,316 (3.31) | 1.61 (1.56-1.66) | 3,372 (6.68)/4,260 (4.38) | 1.61 (1.52-1.70) |
Per 1,000 person-years, unadjusted.
HRs were derived from fully adjusted models (i.e., Model 4).
In both cohorts, we found similar results for all diagnoses of stress-related disorders (Table 2), while the association was somehow stronger for acute stress reaction, compared with PTSD and adjustment disorder and other stress reactions, within the first year of follow-up. The stratification analyses indicated that the association between stress-related disorders and all-cause mortality was greater among males (compared with females), younger individuals (compared with older individuals), and individuals with higher educational level (compared with individuals with lower educational level) (all P for interaction <0.05; Table 3 and Supplementary Table 3). We also observed a stronger association among individuals with lower CCI score (compared with individuals with higher CCI score), and individuals without a history of other psychiatric disorders (compared with individuals with such a history) (both P for interaction <0.05).
Table 3.
Hazard ratios (HRs)a and 95% confidence intervals (CIs) for all-cause mortality among patients with stress-related disorders, compared to their matched unexposed individuals, during the entire follow-up and by different characteristics.
| Characteristics | Any stress-related disorder |
PTSD |
Acute stress reaction |
Adjustment disorder and other stress reactions |
||||
|---|---|---|---|---|---|---|---|---|
| No. of deaths (mortalityb) in exposed/unexposed individuals | HR (95% CI) | No. of deaths (mortalityb) in exposed/unexposed individuals | HR (95% CI) | No. of deaths (mortalityb) in exposed/unexposed individuals | HR (95% CI) | No. of deaths (mortalityb) in exposed/unexposed individuals | HR (95% CI) | |
| Overall | 13,812 (7.95)/ 55,761 (3.11) |
1.70 (1.67-1.74) |
716 (6.61)/ 2,834 (2.57) |
1.68 (1.52-1.85) |
6,159 (8.42)/ 23,221 (3.08) |
1.76 (1.70-1.82) |
6,937 (7.74)/ 29,706 (3.21) |
1.66 (1.61-1.71) |
| Sex | ||||||||
| Male | 7,241 (10.87)/ 28,299 (4.02) |
1.76 (1.71-1.81) |
312 (9.72)/ 1,298 (3.90) |
1.65 (1.43-1.91) |
3,383 (11.15)/ 12,257 (3.83) |
1.82 (1.74-1.91) |
3,546 (10.73)/ 14,744 (4.21) |
1.71 (1.64-1.79) |
| Female | 6,571 (6.14)/ 27,462 (2.52) |
1.65 (1.60-1.71) |
404 (5.30)/ 1,536 (1.99) |
1.71 (1.49-1.95) |
2,776 (6.48)/ 10,964 (2.52) |
1.71 (1.62-1.79) |
3,391 (5.99)/ 14,962 (2.60) |
1.61 (1.54-1.68) |
| Pinteractionc | <0.001 | |||||||
| Age at cohort entry, years | ||||||||
| ≤28 | 1,818 (2.95)/ 3,386 (0.55) |
3.47 (3.24-3.72) |
123 (2.70)/ 183 (0.40) |
4.01 (2.99-5.39) |
762 (2.98)/ 1,247 (0.49) |
3.66 (3.28-4.08) |
933 (2.97)/ 1,956 (0.62) |
3.31 (3.02-3.63) |
| 29-42 | 3,718 (6.20)/ 11,602 (1.87) |
1.96 (1.87-2.05) |
183 (5.46)/ 533 (1.56) |
1.96 (1.58-2.42) |
1,555 (6.09)/ 4,236 (1.61) |
2.07 (1.93-2.23) |
1,980 (6.36)/ 6,833 (2.12) |
1.88 (1.77-2.00) |
| ≥43 | 8,276 (15.88)/ 40,773 (7.35) |
1.42 (1.39-1.47) |
410 (13.98)/ 2,118 (6.86) |
1.35 (1.20-1.53) |
3,842 (17.42)/ 17,738 (7.52) |
1.49 (1.43-1.55) |
4,024 (14.83)/ 20,917 (7.27) |
1.38 (1.32-1.43) |
| Pinteractionc | <0.001 | |||||||
| Calendar year at cohort entry | ||||||||
| 1981-1996 | 5,903 (9.76)/ 25,017 (3.88) |
1.78 (1.72-1.84) |
339 (10.42)/ 1,512 (4.38) |
1.70 (1.48-1.95) |
2,250 (9.69)/ 9,453 (3.84) |
1.74 (1.64-1.83) |
3,314 (9.75)/ 14,052 (3.86) |
1.83 (1.75-1.91) |
| 1997-2006 | 4,368 (7.12)/ 18,275 (2.92) |
1.62 (1.56-1.69) |
186 (5.95)/ 638 (2.02) |
1.88 (1.53-2.29) |
2,055 (7.52)/ 8,105 (2.89) |
1.67 (1.58-1.77) |
2,127 (6.89)/ 9,532 (3.04) |
1.56 (1.47-1.64) |
| 2007-2016 | 3,541 (6.83)/ 12,469 (2.39) |
1.71 (1.64-1.80) |
191 (4.29)/ 684 (1.54) |
1.48 (1.21-1.82) |
1,854 (8.20)/ 5,663 (2.48) |
1.98 (1.85-2.11) |
1,496 (6.03)/ 6,122 (2.46) |
1.49 (1.39-1.60) |
| Pinteractionc | 0.10 | |||||||
| Educational level, years | ||||||||
| <9 | 1,953 (21.55)/ 11,845 (13.26) |
1.25 (1.17-1.34) |
116 (19.40)/ 674 (12.45) |
1.42 (1.07-1.87) |
966 (22.54)/ 5,492 (13.53) |
1.31 (1.18-1.45) |
871 (20.85)/ 5,679 (13.10) |
1.18 (1.06-1.30) |
| 9-12 | 7,390 (6.40)/ 27,937 (2.64) |
1.78 (1.72-1.84) |
435 (5.50)/ 1,538 (2.20) |
1.81 (1.57-2.08) |
3,607 (6.73)/ 12,811 (2.65) |
1.85 (1.76-1.94) |
3,348 (6.20)/ 13,588 (2.69) |
1.71 (1.63-1.79) |
| >12 | 1,864 (5.31)/ 8,379 (1.67) |
1.94 (1.80-2.10) |
97 (4.65)/ 454 (1.36) |
1.78 (1.25-2.53) |
832 (5.76)/ 3,726 (1.66) |
2.09 (1.86-2.35) |
935 (5.04)/ 4,199 (1.73) |
1.83 (1.65-2.04) |
| Pinteractionc | <0.001 | |||||||
| Charlson Comorbidity Index | ||||||||
| 0 | 8,300 (6.02)/ 37,417 (2.40) |
1.84 (1.79-1.89) |
448 (5.28)/ 1,929 (2.00) |
1.86 (1.64-2.11) |
3,627 (6.27)/ 15,094 (2.31) |
1.89 (1.81-1.98) |
4,225 (5.91)/ 20,394 (2.52) |
1.80 (1.73-1.87) |
| 1 | 2,324 (9.35)/ 7,711 (4.56) |
1.52 (1.38-1.67) |
129 (7.81)/ 404 (3.81) |
1.45 (0.94-2.23) |
1,067 (9.97)/ 3,385 (4.57) |
1.76 (1.53-2.03) |
1,128 (9.01)/ 3,922 (4.65) |
1.34 (1.17-1.53) |
| ≥2 | 3,188 (29.08)/ 10,633 (16.59) |
1.36 (1.25-1.47) |
139 (20.12)/ 501 (14.36) |
1.53 (1.05-2.24) |
1,465 (31.61)/ 4,742 (17.14) |
1.36 (1.21-1.54) |
1,584 (28.09)/ 5,390 (16.37) |
1.34 (1.19-1.50) |
| Pinteractionc | <0.001 | |||||||
| History of other psychiatric disordersd | ||||||||
| Yes | 6,526 (12.08)/ 9,765 (8.96) |
1.23 (1.16-1.30) |
361 (7.99)/ 483 (6.27) |
1.33 (1.05-1.68) |
3,023 (13.39)/ 4,342 (9.10) |
1.31 (1.20-1.42) |
3,142 (11.66)/ 4,940 (9.22) |
1.13 (1.04-1.24) |
| No | 7,286 (6.09)/ 45,996 (2.73) |
1.99 (1.94-2.05) |
355 (5.63)/ 2,351 (2.29) |
1.91 (1.68-2.17) |
3,136 (6.20)/ 18,879 (2.67) |
2.06 (1.97-2.15) |
3,795 (6.05)/ 24,766 (2.84) |
1.95 (1.88-2.03) |
| Pinteractionc | <0.001 | |||||||
Derived from Cox models, stratified by matching identifiers (birth year and sex) and adjusted for educational level, yearly family income level, marital status, Charlson comorbidity index, and history of other psychiatric disorders.
Per 1,000 person-years, unadjusted.
The difference between HRs was assessed by introducing an interaction term to the Cox models.
The first diagnosis of any psychiatric disorder (other than stress-related disorders) >3 months before index date.
Cause-specific mortality
In the population-based matched cohort, the most common causes of death among the exposed individuals were cancer (3,306 deaths [23.94%]), circulatory disease (2,775 deaths [20.09%]), and suicide (2,657 deaths [19.24%]) (Supplementary Table 4). The percentage of deaths attributed to potentially avoidable causes was higher among exposed individuals, compared with their matched unexposed individuals (68.46% vs 67.87% for ≤1 year and 72.23% vs 65.70% for >1 year of follow-up). The leading cause of potentially avoidable mortality was suicide among the exposed individuals (Supplementary Table 5).
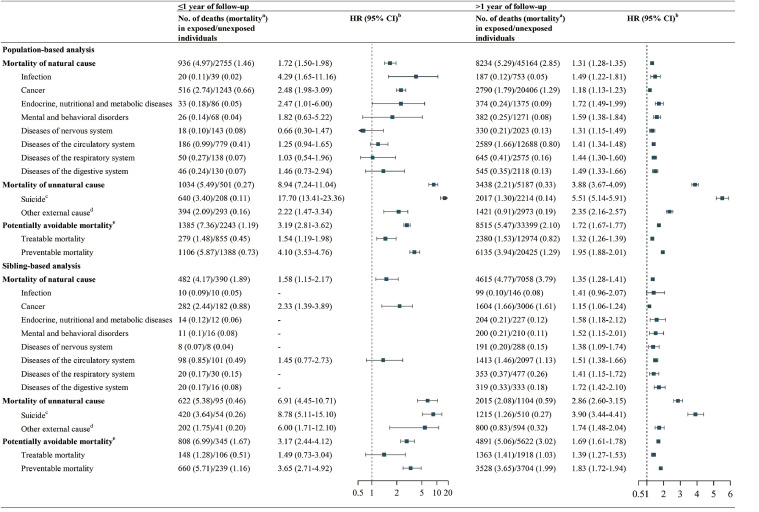
During the first year of follow-up, the HR was 8.94 (95% CI, 7.24-11.04) for deaths due to unnatural causes, especially suicide (HR, 17.70 [95% CI, 13.41-23.36]) (Figure 2). A higher mortality due to natural causes was also observed during the first year of follow-up (HR, 1.72 [95% CI, 1.50-1.98]), especially infection (HR, 4.29 [95% CI, 1.65-11.16]) and cancer (HR, 2.48 [95% CI, 1.98-3.09]). During the first year of follow-up, an excess risk was also noted for potentially avoidable mortality (HR, 3.19 [95% CI, 2.81-3.62]), especially preventable mortality (HR, 4.10 [95% CI, 3.53-4.76]). Beyond one year of follow-up, the HRs attenuated for almost all studied cause-specific mortality, ranging from 1.18 (95% CI, 1.13-1.23) for cancer to 5.51 (95% CI, 5.14-5.91) for suicide.
Figure 2.
Risk of cause-specific mortality and potentially avoidable mortality among patients with stress-related disorders, compared to their matched unexposed individuals or unaffected full siblings.
aPer 1,000 person-years, unadjusted.
bIn the population-based matched cohort, HRs were derived from Cox models, stratified by matching identifiers (birth year and sex) and adjusted for educational level, yearly family income level, marital status, Charlson comorbidity index, and history of other psychiatric disorders. In the sibling cohort, HRs were derived from Cox models, stratified by family identifiers and adjusted for birth year, sex, educational level, yearly family income level, marital status, Charlson comorbidity index, and history of other psychiatric disorders.
cSuicide includes deaths from intentional self-harm, and events of undetermined intent.
dOther external causes include accidents, fall, assaults, and other external causes.
ePotentially avoidable mortality refers to deaths that are considered treatable or preventable. Treatable mortality refers to deaths that are treatable through timely and effective healthcare interventions. Preventable mortality refers to deaths that can be reduced through effective public health and primary prevention interventions.
In the sibling cohort, we found largely similar results, indicating higher HRs for mortality due to unnatural causes (HR, 6.91 [95% CI, 4.45-10.71] for ≤1 year and HR, 2.86 [95% CI, 2.60-3.15] for >1 year of follow-up) than mortality due to natural causes (HR, 1.58 [95% CI, 1.15-2.17] for ≤1 year and HR, 1.35 [95% CI, 1.28-1.41] for >1 year of follow-up), among individuals with stress-related disorders (Figure 2). An excess risk of potentially avoidable mortality was also observed (HR, 3.17 [95% CI, 2.44-4.12] for ≤1 year and HR, 1.69 [95% CI, 1.61-1.78] for >1 year of follow-up).
Secondary analyses
In both the population-based matched cohort and sibling cohort, we observed greater risk increase of all-cause mortality among the exposed individuals with the severe form of stress-related disorders, indicated by the presence of psychiatric comorbidities (i.e., HR, 2.83 [95% CI, 2.70-2.97] vs HR, 1.48 [95% CI, 1.45-1.52] for stress-related disorders with or without psychiatric comorbidities in the population-based comparison; HR, 2.66 [95% CI, 2.42-2.92] vs HR, 1.44 [95% CI, 1.37-1.51] for stress-related disorders with or without psychiatric comorbidities in the sibling comparison), admission to inpatient care (HR, 1.86 [95% CI, 1.81-1.91] vs HR, 1.44 [95% CI, 1.38-1.50] for stress-related disorders with or without inpatient care in the population-based comparison; HR, 1.79 [95% CI, 1.70-1.88] vs HR, 1.41 [95% CI, 1.31-1.52] for stress-related disorders with or without inpatient care in the sibling comparison), or more frequent inpatient visits within one year after diagnosis (HR, 2.18 [95% CI, 2.03-2.34] vs HR, 1.82 [95% CI, 1.76-1.87] for stress-related disorders with ≥2 times or <2 times inpatient visits in the population-based comparison; HR, 2.14 [95% CI, 1.88-2.43] vs HR, 1.73 [95% CI, 1.64-1.83] for stress-related disorders with ≥2 times or <2 times inpatient visits in the sibling comparison; Supplementary Table 6). The relative risk assessed by SHRs were similar, although slightly weaker, compared with the HRs of the main analyses (Supplementary Fig. 2). Finally, the calculation of E values revealed that a minimal magnitude of 2 to 17-fold increased risk of mortality was required to be associated with any unmeasured confounder to entirely explain the observed associations (Supplementary Table 7).
Discussion
In this Swedish population-based and sibling-controlled cohort study, we found that individuals with stress-related disorders were at increased risk of all-cause as well as multiple cause-specific mortality, especially during the first year following the diagnosis of stress-related disorders. The risk elevation was more evident for deaths due to unnatural causes (e.g., suicide), compared with deaths due to natural causes, after taking into account familial confounding, history of other psychiatric disorders, and multiple somatic comorbidities. Further, the excess mortality in relation to stress-related disorders was largely attributable to potentially avoidable causes.
To the best of our knowledge, the present study is the first large-scale endeavor to comprehensively examine the associations of all stress-related disorders with all-cause and cause-specific mortality using both population- and sibling-based comparisons. In line with the present findings, results of previous prospective cohort studies16,19,21 have demonstrated an association of PTSD or other stress-related disorders with a higher risk of all-cause mortality, suicide, and death due to cardiovascular disease (CVD). Our study expands the existing knowledge by showing that the excess mortality was especially pronounced for unnatural death and death with potentially avoidable cause, both immediately after the diagnosis of stress-related disorders and in the long run. Importantly, we found that about 70% of the deaths were potentially avoidable (i.e., attributable to treatable or preventable causes), with suicide as the leading cause. Further, although a few previous studies on the association between stress-related disorders and CVD mortality have considered family history of CVD among veterans,38,39 the influence of other familial confounding has rarely been addressed. In contrast to the previous studies,16,19,21,38,39 we therefore used a sibling comparison to account for potential confounding due to genetic and non-genetic factors shared between full siblings. Importantly, our finding of similar results between population-based comparison and sibling comparison indicates that the excess mortality associated with stress-related disorders is likely largely independent of familial confounding. Moreover, the greater magnitude of the associations noted among individuals with no history of other psychiatric disorders, males, and younger individuals suggests that the relative importance of stress-related disorders on mortality varies by patient characteristics.
Our finding of the time-dependent relative risk of all-cause mortality indicates that the first year after diagnosis of stress-related disorders entails the highest excess risk period among individuals diagnosed with stress-related disorders. This is consistent with previous studies reporting the most pronounced risk elevation of suicide immediately after receiving a positive result on PTSD among US veterans.17 Our results extend previous literature by showing similar decreasing trend of excess mortality across siblings discordant on all subtypes of stress-related disorders. Notably, acute stress reaction was associated with comparable or even greater risk of all-cause mortality, compared with PTSD and adjustment disorder, within the first year of follow-up, supporting the notion that acute and severe psychological symptoms after exposure to a traumatic event might lead to an immediately increased risk of death such as suicide.23
Furthermore, as the risk elevation of natural and unnatural causes of death was sustained beyond one year, the impact of stress-related disorders on mortality seems to be long-lasting. There are likely multiple explanations. First, the increased susceptibilities of individuals with stress-related disorders to other psychiatric disorders,21 including depression, anxiety, and substance use disorders, are known risk factors for unnatural death and suicide.40 This is supported by our findings as well as previous research,22 indicating that co-occurring stress-related disorders with other psychiatric disorders might reflect more severe psychological stress than stress-related disorder alone, potentially inducing a greater risk of mortality. Second, chronic psychological distress of individuals with stress-related disorders may lead to dysregulation of immune responses5 and chronic inflammation,41 which, in return, may cause elevated risks of several chronic and fatal diseases, such as CVD,9 life-threatening infection,10 and autoimmune disease.11 Third, negative behavioral changes as a result of maladaptation to trauma or stressful events, such as misuse of alcohol or illicit drugs,42 may compromise executive function and capacity of decision making, putting the patients in dangerous situations or leading to impaired capacity to identify and react appropriately to potential threats, which may consequently increase the risk of mortality due to unnatural causes. Likewise, other unfavorable behaviors (e.g., smoking,6 poor diet,7 and lack of physical activity6,8) may contribute to increased incidence of natural death through elevating the risks of multiple major chronic diseases. Last, it is possible that suboptimal access to health care,31 health-seeking behavior,43 and poor compliance to treatment8 among exposed patients could contribute to the long-term excess risk of mortality, especially the mortality due to avoidable causes.
Taken together, stress-related disorders are increasingly recognized as a globally important public health problem, which is specifically relevant in the context of the current coronavirus disease 2019 (COVID-19) pandemic. Growing evidence has indeed demonstrated significant mental health burden among patients directly affected by COVID-19, their families, healthcare workers involved in the care of COVID-19, and the general public during the pandemic.44 Specifically, according to a recent systematic review, the pooled prevalence of post-pandemic PTSD was 24.6% across these populations (COVID-19 patients, healthcare workers, and the general public).29 Given the growing burden of stress-related disorders, during the pandemic but also thereafter, our findings highlight the need of clinical surveillance and, when needed, interventions to reduce the risk of premature mortality among individuals with stress-related disorders.
The major strength of our study includes the population-based cohort design with a long and complete follow-up of a large sample of patients with stress-related disorders, and the sibling comparison to address the concern about residual confounding. The large sample size allowed us to perform detailed subgroup analyses, including examining the time-dependent risk of death and specific causes of death. The availability of rich information on sociodemographic characteristics and disease histories enabled the control of a wide range of confounding factors in the analyses.
This study has several limitations. First, misclassification of stress-related disorders cannot be ruled out, even though the diagnosis of PTSD in National Patient Register has been validated with satisfactory accuracy.45 However, such misclassification is likely non-differential with respect to mortality and could have led to an attenuation of the studied association. Second, changes in the diagnostic criteria for stress-related disorders over time might have influenced the results. The stratification analysis by calendar period suggested however a negligible effect of such factor. Third, as data on outpatient specialist care were not included in the National Patient Register until 2001,30 the exposed individuals in our study mainly represent a group with relatively severe stress-related disorders. Mortality for individuals with less severe stress-related disorders needs to be studied further. Fourth, this study only included a Swedish population, and the generalizability of our findings to other countries remains unknown. However, as our results are generally consistent with previous studies using Danish and US samples, it is likely that the risk pattern of mortality among patients with stress-related disorders is similar across populations of most western countries. Finally, we cannot rule out the possibility of residual confounding, particularly lifestyle factors that change over time. However, the calculated E-values suggest that the observed associations could only be explained by unmeasured confounders with very strong association with mortality.
In conclusion, in this Swedish cohort, we found that patients with stress-related disorders were at an increased risk of all-cause and multiple cause-specific mortality, and the risk elevation was independent of familial confounding. As the excess mortality was mainly attributable to deaths due to unnatural causes and potentially avoidable causes, this finding underscores the importance of clinical surveillance and treatment of individuals with stress-related disorders.
Contributors
HS and FF were responsible for the study's concept and design. FT, QS, and YH performed the data cleaning and analysis. FT, QS, YH, WY, UAV, HS, and FF interpreted the data. FT, QS, UAV, HS, and FF drafted the manuscript. All the authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Data availability statement
The data are not publicly available due to Swedish laws.
Declaration of interests
The authors declare no competing interests.
Acknowledgments
This work was supported by EU Horizon 2020 Research and Innovation Action Grant (847776 to Drs Valdimarsdóttir and Fang), 1.3.5 Project for Disciplines of Excellence, West China Hospital, Sichuan University (ZYYC21005 to Dr Song), the National Natural Science Foundation of China (81971262 to Dr Song), Grant of Excellence, Icelandic Research Fund (163362 to Dr Valdimarsdóttir), the ERC Consolidator Grant (StressGene 726413 to Dr Valdimarsdóttir), and Swedish Research Council (2016-02234 to Dr Valdimarsdóttir).
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanepe.2022.100402.
Contributor Information
Huan Song, Email: songhuan@wchscu.cn.
Fang Fang, Email: fang.fang@ki.se.
Appendix. Supplementary materials
References
- 1.World Health Organization . World Health Organization; Geneva, Switzerland: 1992. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. [Google Scholar]
- 2.Gradus J.L. Prevalence and prognosis of stress disorders: a review of the epidemiologic literature. Clin Epidemiol. 2017;9:251–260. doi: 10.2147/CLEP.S106250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ursano R.J., Bell C., Eth S., et al. Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. Am J Psychiatry. 2004;161(11):3–31. Suppl. [PubMed] [Google Scholar]
- 4.Bisson J.I., Sakhuja D. Adjustment disorders. Psychiatry. 2006;5(7):240–242. [Google Scholar]
- 5.Glaser R., Kiecolt-Glaser J.K. Stress-induced immune dysfunction: implications for health. Nat Rev Immunol. 2005;5(3):243–251. doi: 10.1038/nri1571. [DOI] [PubMed] [Google Scholar]
- 6.van den Berk-Clark C., Secrest S., Walls J., et al. Association between posttraumatic stress disorder and lack of exercise, poor diet, obesity, and co-occuring smoking: A systematic review and meta-analysis. Health Psychol. 2018;37(5):407. doi: 10.1037/hea0000593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim Y., Roberts A.L., Rimm E.B., et al. Posttraumatic stress disorder and changes in diet quality over 20 years among US women. Psychol Med. 2021;51(2):310–319. doi: 10.1017/S0033291719003246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zen A.L., Whooley M.A., Zhao S., Cohen B.E. Post-traumatic stress disorder is associated with poor health behaviors: findings from the heart and soul study. Health Psychol. 2012;31(2):194. doi: 10.1037/a0025989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Song H., Fang F., Arnberg F.K., et al. Stress related disorders and risk of cardiovascular disease: population based, sibling controlled cohort study. BMJ (Clin Res Ed) 2019:365. doi: 10.1136/bmj.l1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Song H., Fall K., Fang F., et al. Stress related disorders and subsequent risk of life threatening infections: population based sibling controlled cohort study. BMJ (Clin Res Ed) 2019:367. doi: 10.1136/bmj.l5784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Song H., Fang F., Tomasson G., et al. Association of stress-related disorders with subsequent autoimmune disease. JAMA. 2018;319(23):2388–2400. doi: 10.1001/jama.2018.7028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Song H., Sieurin J., Wirdefeldt K., et al. Association of stress-related disorders with subsequent neurodegenerative diseases. JAMA Neurol. 2020;77(6):700–709. doi: 10.1001/jamaneurol.2020.0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Colpani V., Baena C.P., Jaspers L., et al. Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: a systematic review and meta-analysis. Eur J Epidemiol. 2018;33(9):831–845. doi: 10.1007/s10654-018-0374-z. [DOI] [PubMed] [Google Scholar]
- 14.Stringhini S., Carmeli C., Jokela M., et al. Socioeconomic status and the 25× 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1· 7 million men and women. Lancet N Am Ed. 2017;389(10075):1229–1237. doi: 10.1016/S0140-6736(16)32380-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moraga P., GBD Causes of Death Collaborators Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the global burden of disease study 2016. Lancet N Am Ed. 2017;390(10100):1151–1210. doi: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Giesinger I., Li J., Takemoto E., Cone J.E., Farfel M.R., Brackbill R.M. Association between posttraumatic stress disorder and mortality among responders and civilians following the september 11, 2001, disaster. JAMA Netw Open. 2020;3(2) doi: 10.1001/jamanetworkopen.2019.20476. [DOI] [PubMed] [Google Scholar]
- 17.Cooper S.A., Szymanski B.R., Bohnert K.M., Sripada R.K., McCarthy J.F. Association between positive results on the primary care-posttraumatic stress disorder screen and suicide mortality among US veterans. JAMA Netw Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.15707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fudim M., Cerbin L.P., Devaraj S., Ajam T., Rao S.V., Kamalesh M. Post-traumatic stress disorder and heart failure in men within the veteran affairs health system. Am J Cardiol. 2018;122(2):275–278. doi: 10.1016/j.amjcard.2018.04.007. [DOI] [PubMed] [Google Scholar]
- 19.Boscarino J.A. Posttraumatic stress disorder and mortality among U.S. Army veterans 30 years after military service. Ann Epidemiol. 2006;16(4):248–256. doi: 10.1016/j.annepidem.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 20.Flood A.M., Boyle S.H., Calhoun P.S., et al. Prospective study of externalizing and internalizing subtypes of posttraumatic stress disorder and their relationship to mortality among Vietnam veterans. Compr Psychiatry. 2010;51(3):236–242. doi: 10.1016/j.comppsych.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gradus J.L., Antonsen S., Svensson E., Lash T.L., Resick P.A., Hansen J.G. Trauma, comorbidity, and mortality following diagnoses of severe stress and adjustment disorders: a nationwide cohort study. Am J Epidemiol. 2015;182(5):451–458. doi: 10.1093/aje/kwv066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roberts A.L., Kubzansky L.D., Chibnik L.B., Rimm E.B., Koenen K.C. Association of posttraumatic stress and depressive symptoms with mortality in women. JAMA Netw Open. 2020;3(12) doi: 10.1001/jamanetworkopen.2020.27935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gradus J.L., Qin P., Lincoln A.K., et al. Acute stress reaction and completed suicide. Int J Epidemiol. 2010;39(6):1478–1484. doi: 10.1093/ije/dyq112. [DOI] [PubMed] [Google Scholar]
- 24.Meier S.M., Trontti K., Purves K.L., et al. Genetic variants associated with anxiety and stress-related disorders: a genome-wide association study and mouse-model study. JAMA Psychiatry. 2019;76(9):924–932. doi: 10.1001/jamapsychiatry.2019.1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Christensen K., Johnson T.E., Vaupel J.W. The quest for genetic determinants of human longevity: challenges and insights. Nat Rev Genet. 2006;7(6):436–448. doi: 10.1038/nrg1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Helbich M., De Beurs D., Kwan M.P., O'Connor R.C., Groenewegen P.P. Natural environments and suicide mortality in the Netherlands: a cross-sectional, ecological study. Lancet Planet Health. 2018;2(3):e134. doi: 10.1016/S2542-5196(18)30033-0. e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Demakakos P., Pillas D., Marmot M., Steptoe A. Parenting style in childhood and mortality risk at older ages: a longitudinal cohort study. Br J Psychiatry. 2016;209(2):135–141. doi: 10.1192/bjp.bp.115.163543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Repetti R.L., Taylor S.E., Seeman T.E. Risky families: family social environments and the mental and physical health of offspring. Psychol Bull. 2002;128(2):330. [PubMed] [Google Scholar]
- 29.Yuan K., Gong Y.M., Liu L., et al. Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including COVID-19: a meta-analysis and systematic review. Mol Psychiatry. 2021;26(9):4982–4998. doi: 10.1038/s41380-021-01036-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ludvigsson J.F., Andersson E., Ekbom A., et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11(1):1–16. doi: 10.1186/1471-2458-11-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.National Collaborating Centre for Mental Health . National Collaborating Centre for Mental Health; 2005. Post-Traumatic Stress Disorder: The Management of PTSD in Adults and Children in Primary and Secondary Care. [Google Scholar]
- 32.Knol M.J., Vandenbroucke J.P., Scott P., Egger M. What do case-control studies estimate? Survey of methods and assumptions in published case-control research. Am J Epidemiol. 2008;168(9):1073–1081. doi: 10.1093/aje/kwn217. [DOI] [PubMed] [Google Scholar]
- 33.Classen C., Koopman C., Hales R., Spiegel D. Acute stress disorder as a predictor of posttraumatic stress symptoms. Am J Psychiatry. 1998;155(5):620–624. doi: 10.1176/ajp.155.5.620. [DOI] [PubMed] [Google Scholar]
- 34.Office for National Statistics . Office for National Statistics; 2019. Avoidable Mortality in the UK.https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/causesofdeath/bulletins/avoidablemortalityinenglandandwales/2019 Accessed February 26, 2021. [Google Scholar]
- 35.Quan H., Li B., Couris C.M., et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676–682. doi: 10.1093/aje/kwq433. [DOI] [PubMed] [Google Scholar]
- 36.Fine J.P., Gray R.J. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496–509. [Google Scholar]
- 37.VanderWeele T.J., Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268–274. doi: 10.7326/M16-2607. [DOI] [PubMed] [Google Scholar]
- 38.Boscarino J.A. A prospective study of PTSD and early-age heart disease mortality among Vietnam veterans: implications for surveillance and prevention. Psychosom Med. 2008;70(6):668–676. doi: 10.1097/PSY.0b013e31817bccaf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ahmadi N., Hajsadeghi F., Mirshkarlo H.B., Budoff M., Yehuda R., Ebrahimi R. Post-traumatic stress disorder, coronary atherosclerosis, and mortality. Am J Cardiol. 2011;108(1):29–33. doi: 10.1016/j.amjcard.2011.02.340. [DOI] [PubMed] [Google Scholar]
- 40.Hiroeh U., Appleby L., Mortensen P.B., Dunn G. Death by homicide, suicide, and other unnatural causes in people with mental illness: a population-based study. Lancet N Am Ed. 2001;358(9299):2110–2112. doi: 10.1016/S0140-6736(01)07216-6. [DOI] [PubMed] [Google Scholar]
- 41.Cohen S., Janicki-Deverts D., Miller G.E. Psychological stress and disease. JAMA. 2007;298(14):1685–1687. doi: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- 42.Bray R.M., Fairbank J.A., Marsden M.E. Stress and substance use among military women and men. Am J Drug Alcohol Abuse. 1999;25(2):239–256. doi: 10.1081/ada-100101858. [DOI] [PubMed] [Google Scholar]
- 43.Goldstein R.B., Smith S.M., Chou S.P., et al. The epidemiology of DSM-5 posttraumatic stress disorder in the United States: results from the national epidemiologic survey on alcohol and related conditions-III. Soc Psychiatry Psychiatr Epidemiol. 2016;51(8):1137–1148. doi: 10.1007/s00127-016-1208-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rogers J.P., Chesney E., Oliver D., et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7(7):611–627. doi: 10.1016/S2215-0366(20)30203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hollander A.C., Askegård K., Iddon-Escalante C., Holmes E.A., Wicks S., Dalman C. Validation study of randomly selected cases of PTSD diagnoses identified in a Swedish regional database compared with medical records: is the validity sufficient for epidemiological research? BMJ Open. 2019;9(12) doi: 10.1136/bmjopen-2019-031964. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data are not publicly available due to Swedish laws.