Abstract
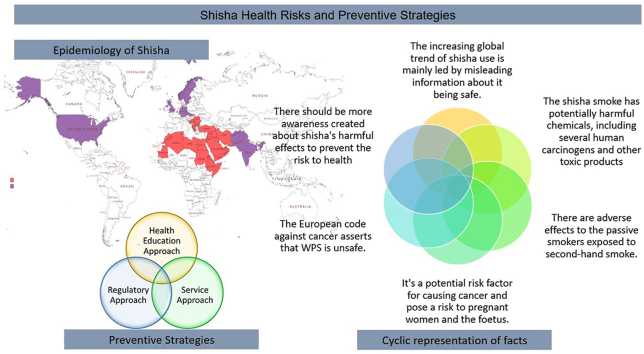
Smoking tobacco through a water pipe, also referred to as Shisha, is prevalent in Middle Eastern countries but has gained popularity worldwide, especially among youth. The increasing global trend of shisha use is mainly led by misleading information about it being safe. The shisha smoke has potentially harmful chemicals, including several human carcinogens and other toxic products. There are recognised adverse effects on passive smokers exposed to second-hand smoke. It is a potential risk factor for several cancers and risks pregnant women and the foetus. A session of shisha smoking for 40 minutes is equivalent to smoking 100 or more cigarettes. There should be awareness about Shisha's harmful effects to reduce the risk to health through a coordinated global effort.
Keywords: Cancer risk, Health effects, Shisha, Waterpipe smoking
Graphical abstract
1. Introduction to shisha
What is Shisha: It is also known as Hukka, Narghile, Arguileh, Goza, Hubble-Bubble, and is commonly referred to as waterpipe smoking in the western world, is a traditional way to smoke tobacco among some population groups, mainly in Arab countries.1,2
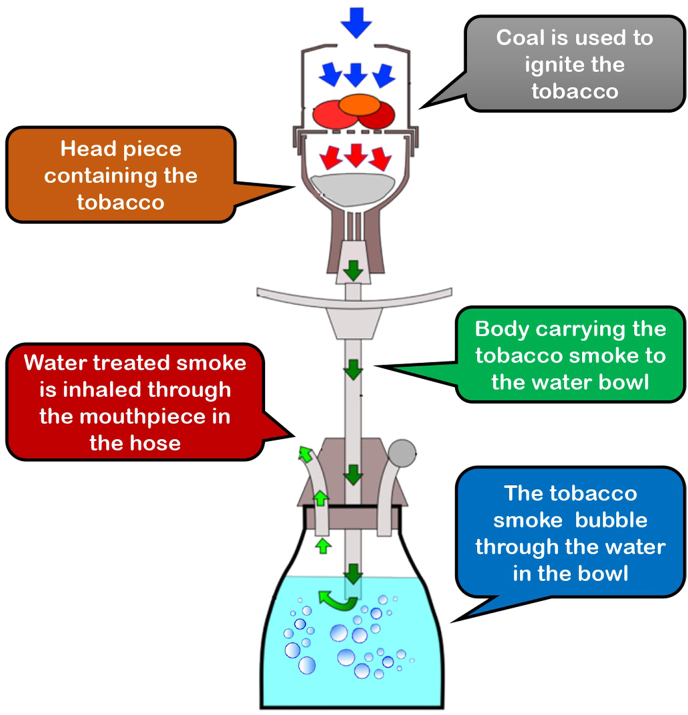
Shisha, referred to as Hukka in the Indian sub-continent, was invented by an Indian physician during Mogul emperor Akbar's rule as a less harmful means of smoking tobacco.3 The shisha smoking apparatus (Fig. 1) has a head in which tobacco and hot coal are kept; this is connected through a hard tube called the body to the bowl where water is placed; the bowl also has a hose connection mouthpiece at the end. The smoke generated from the head moves down to the water bowl, and filtered smoke escapes to the mouthpiece through the hose (Fig. 1). Mixtures of tobacco and non-tobacco products, which are flavoured (mint and fruit flavours), are added to the head to enhance the experience of smoking.2 Non-tobacco brands of shisha are also available. The misleading commercialization of the shisha brands claiming low nicotine (0.5%) and 0% tar has led to the popularity of this smoking habit being a safe alternative to cigarette smoking.4,5 The present review focuses on the risk posed by smoking shisha with and without tobacco on health, the composition of shisha smoke, risk of cancer, and strategies for prevention of shisha habit.
Fig. 1.
Functioning of shisha.
2. What does the smoke of shisha consist of?
Waterpipe smoking usually lasts from 20 to 80 minutes with 50–200 puffs per session, and the smoke inhaled is 530 ml of mean value per puff, considerably more volume of smoke than in cigarette smoking. It is stated that per session of waterpipe smoking is equal to smoking more than 100 cigarettes.6 Most of the smoke from tobacco and coal products is made up of nicotine, carbon monoxide, tobacco-specific nitrosamines, polyaromatic hydrocarbons, volatile aldehydes, and traces of heavy metals like arsenic and chromium lead.7 Tobacco smoke generated from Shisha has over 4800 different chemicals, 69 of which are human carcinogens and tumour promoters.7
Shisha smoking is an emerging health risk behaviour, especially amongst the youth and the use of shisha is habit-forming.6 The use of Shisha with tobacco products leads to particulate matter, nicotine, carbon monoxide, and nitrogen oxide. The presence of nicotine in smoke is the primary cause of dependence on tobacco-related products. The nicotine enters the bloodstream to reach the receptors in the brain to release dopamine, which makes the individual feel good and is the main reason for tobacco addiction.4,7,8
The instant coal most popularly used in Shisha to burn tobacco is produced from the coconut husk. It is known to produce carbon monoxide, tar, and other harmful gases like polycyclic aromatic hydrocarbons (PHA) and volatile aldehydes (V.A.) irrespective of the presence of tobacco in it. The smoke produced poses a high risk to the health of the smoker and non-smokers in and around the zone of shisha use, as a second-hand smoker.1,6,7
3. Global epidemiology of shisha use
The Shisha is known the world over by different names in East Mediterranean countries it is known as “narghile” and even in Turkey and Syria, “shisha” and “Goza” in some North African countries and Egypt, and in India, it is called as “hookah".9 Shisha is mainly popular in Middle Eastern states and European countries but now has gained equal popularity worldwide, especially amongst the youth. Several surveys confirm that shisha smoking has replaced cigarette smoking as the widely used form of tobacco in the middle east.2,10, 11, 12, 13 Shisha smoking in the Arabian countries (United Arab Emirates, Kuwait, Bahrain, Oman, Qatar, and Yemen) showed a prevalence of 9%–15% among 13–15-year-old schoolchildren in several countries in the Arabian Peninsula.10 Studies indicate an increasing trend in the use of shisha in the rest of the world.13 A survey conducted amongst 100,000 students at 152 colleges in the U.S. revealed a prevalence of 8.4%.12 The Global Adult Tobacco Survey (GATS 2008–2012) conducted amongst 15 years and older individuals shows an increasing trend of shisha smoking worldwide.13 The countries showing high prevalence were Lithuania, Cyprus, Denmark, Czech Republic, and Austria, while Uruguay shows the least prevalence. In the U.S., the Tobacco Products and Risk Perceptions Surveys of 2014 and 2015 found a prevalence of 15.8% of ever waterpipe smoking among adults.14
The main reasons attributed to the increasing prevalence of shisha smoking are the use of flavoured tobacco (Maasel), the emerging café culture with an increase in the use of internet cafés, social media hype, and the lack of proper regulatory approaches from the policymakers of various countries.2
4. What are the health effects of shisha smoking?
Shisha smoking has become a common practice in social gatherings. Generally shared in a group of 4–5 individuals, there are similar smoking trends amongst males and females.10,15 The harmful health effects of shisha smoking are mainly due to the presence of carbon monoxide, polycyclic aromatic hydrocarbons, volatile aldehydes (formaldehyde, acetaldehyde, acrolein, propionaldehyde, and methacrolein), nitric oxide (NO), nicotine, phenolic compounds, tar, ammonia, heavy metal and particulate matter in the smoke generated.7 The carbon monoxide in the smoke competes with oxygen in the blood to form carboxyhemoglobin, leading to cell hypoxia and impaired cell respiration. The nicotine in smoke has been shown to have acute and chronic cardiovascular effects and increased heart rate.4 The PHAs, VA, heavy metals, and tar are known to cause carcinogenesis by mutation of the p53 tumour suppressor gene. Carbon monoxide, tar, NO, and other particulate material cause lung pathologies by decreasing forced vital capacity and impairing other lung functions. Shisha smokers have shown increased oxidative stress leading to cardiovascular changes and carcinogenesis.4,7 Sharing of the shisha's mouthpiece poses a high risk of transmission of communicable diseases, including hepatitis A and tuberculosis.10,15
Human Cancer: The amount of aldehyde compounds, carbon monoxide, and tar found in one shisha smoking session is 4–30 times more than in a single session of cigarette smoking and are potentially known human carcinogens along with other toxic substances. Shisha smoking is known to cause oxidative stress, have a genotoxic effect, cause carbon monoxide poisoning, and the presence of heavy metals in smoke, causes carcinogenesis. There is evidence of shisha smoking being a risk factor for lung, oral, oesophageal, stomach, bladder, colorectal, and nasopharyngeal cancer.16, 17, 18 Table 1 lists the reported associations of shisha smoking with various cancer sites.17,19, 20, 21, 22, 23, 24
Table 1.
Summary data from case-control studies showing the association of shisha smoking with different types of cancer.
| Study & year | Study Location & Duration |
Cancer Site | Number of cases studied | OR (95% CI) | Adjusted Co-variables | Outcome |
|---|---|---|---|---|---|---|
| Nasrollahzadeh et al. (2008)19 | Iran December 2003 to June 2007 | Oesophageal | Out of 300, 20 Shisha smokers with Epithelial Squamous Cell Carcinoma cases and out of 571 controls, 23 matched controls | OR, CI: 1.85 (0.95–3.58) |
Education and ethnicity | Shisha smoking shows association and higher risk of oesophageal cancer |
| Feng et al. (2009)20 | North Africa 2002 January to 2005 March |
Nasopharyngeal | 636 cases and 615 controls | OR, CI:0.49, (0.20–1.23) | Associated dietary factors, age, and SES | There was no association of shisha smoking with nasopharyngeal cancer |
| Malik et al. (2010)21 | India, Kashmir May 2006 to August 2008 |
Oesophageal | Cases with E.C. (135) and healthy controls (195) | OR, CI:21.4 (11.6–39.5) | Age and gender | There was significantly higer risk of oesophageal cancer with shisha smoking. |
| Dar et al. (2012)22 | India, Kashmir 2008 September to 2012 January |
Oesophageal | Cases 420 and matched controls 699 | OR, CI:1.85 (1.41–2.44) | Age, education, religion, ethnicity, residence, cumulative use of cigarette, hookah and nass, and ever use of bidi, gutka, cannabis and alcohol, daily consumption of fruit and fresh vegetable | There was higher risk of oesohageal cancer with increased frequency, duration and cumulative use of shisha smoking |
| Khlifi et al. (2013)23 | North Africa, January 2007 and December 2009 |
Head and neck (laryngeal, nasopharyngeal, pharyngeal, oral) |
Cases 169 (laryngeal, nasopharyngeal, pharyngeal, oral) cancer and controls 351 |
OR, CI: 2.73 (1.65–4.41) | Adjusted for smoking, alcohol and tap water drinking, neffa and nearby environment | Increased amount of carcinogens like blood chromium and nickel was associated with shisha smoking |
| Quadri et al. (2015)24 | Saudi Arabia, year 2014 |
Oral cancer | Cases 48 of oral cancer and Controls 96 | OR, CI:4.20 (1.32–13.3) | Adjusted for Khat, Shamma, Cigarette | Shisha smoking was associated with a statistically significant risk for oral cancer |
*WPS - Waterpipe smoking; OR - odds ratio; CI - confidence interval.
Mechanistic Data: In shisha smokers, p53 overexpression was described in oral squamous cell carcinoma and pre-malignant lesions of the oral cavity.25,26 Recent in-vitro experimental work describes genomic alterations, proteomic alterations, and differentially altered gene expression patterns in oral keratinocytes when chronically exposed to shisha extract (Table .2).27, 28, 29 Specific types of proteins secreted by the oral cells during oral carcinogenesis may serve as diagnostic biomarkers for early diagnosis of oral cancer amongst subjects chronically exposed to shisha smoking.30,31
Table 2.
Changes in the oral karitinocytes exposed to shisha extract (In-vitro studies).
| Author (year) | In vitro testing | Findings |
|---|---|---|
| S.Patil et al. 201927 | Oral keratinocytes chronically exposed to shisha and their multiomic analysis | In cells treated with shisha extract, two hundred forty-seven genes expressed differently. Changes in the activate MAPK 1 pathway and the interferon signaling pathway were demonstrated. RNA-Seq dataset noted allele-specific expression of mutant LIMA1. |
| S.Patil et al. 201928 | Examination of phosphoproteome of oral keratinocytes with chronic shisha exposure |
|
| S.Patil et al. 201929 | Proteomic changes tested in Oral keratinocytes chronically exposed to Shisha |
|
| S.Patil et al. 201930 | Oral keratinocytes chronically exposed to shisha and their secretome analysis |
|
Respiratory effects: Shisha smoking for prolonged hours in a closed environment has led to acute carbon monoxide (C·O.) poisoning.32 The authors recommend that carboxyhemoglobin (COHb) levels of the blood should be analysed at acute admissions with a shisha smoking history, presenting with nausea, vomiting, headache, and muscle lethargy. Studies indicated an association of shisha smoking with chronic obstructive pulmonary disorder (COPD), bronchitis, and nasal congestion and were linked to a higher amount of blood chromium and nickel.18,23,32
Cardiovascular disease and metabolic syndrome: Shisha smoking has been shown to increase the heart rate by 6–13 beats per minute, systolic blood pressure by 3–16 mm Hg, and diastolic blood pressure by 2–14 mm Hg in young and healthy individuals post smoking session and reported more coronary artery disease than among non-smokers (odds ratio for association of waterpipe smoking and heart disease was 1.67). Shisha smokers are known to have an association with hypertriglyceridemia, hyperglycaemia, hypertension, and abnormal obesity, indicating an association with metabolic syndrome.33,34
Periodontal disease: A study conducted by Javed et al. amongst various smokers (waterpipe, cigarette, and non-smokers) on periodontal health by assessing the plaque index, clinical attachment loss, probing depth ≥4 mm, marginal bone loss, and number of missing teeth showed statistically significant differences in all parameters between waterpipe smokers and non-smokers. There were no differences in the periodontal indices amongst the waterpipe and cigarette smokers. The authors concluded that waterpipe smoking poses a similar risk to periodontal health as cigarette smoking.35, 36, 37
Effect on pregnancy and infertility: Smoking shisha during pregnancy is associated with low-birth-weight babies and increased pulmonary problems for the new-born. There are reported harmful impacts of second-hand smoke on the mother and the foetus. Pregnant women should refrain from smoking shisha and exposure to second-hand smoke or passive smoke. Semen analysis studies confirm male infertility associated with shisha smoking (OR 2.5 compared with never smokers).38
Prevention of shisha use: The global trend of shisha smoking is increasing rapidly, especially among youth. The misleading information that shisha smoke is less harmful to humans because it passes through the water to get purified has led to increased acceptance. The Shisha smoking addiction is mainly due to the nicotine content in the tobacco, thus making the deaddiction or cessation process similar to smoking. The systematic review concluded that behavioural therapy and behavioural therapy with buproprion proved to be effective than the usual care in the control group, however authors concluded that there is a lack of enough evidence and studies in waterpipe smoking cessation.39
The systematic review emphasises effective measures for the prevention and control of waterpipe smoking (WPS). It is broadly divided into three main domains: prevention of WPS; control of WPS; and international and national level enactment and implementation of legislative policies, which include school and college-based programmes to raise awareness about the harmful effects of WPS, decrease social acceptability; raise community awareness; and empower adolescents. Enforcement of new laws to control access, marketing, taxation, and utilisation of WPS. Involving health care professionals in the WPS control programme through training, encouraging researchers to develop WPS-control interventions, and generating evidence for policymakers.40
The prevention of the Shisha smoking habit can be dealt with multiple approaches:
Health Education Approach: There has to be sufficient awareness created through social marketing about shisha smoking's harmful effects, as the shisha smoke despite filtering, bears carcinogens and other toxic products. The sensitization of youth has to be undertaken at every educational institution/university campus about the harmful effects of shisha smoking.
Service Approach: Trained nurses and other health care professionals assess and counsel each individual who has developed a dependence on Shisha, providing information about its harmful effects on general health and as a risk factor for cancer.
Regulatory Approach: There has to be intense advocacy by public health associations to ban shisha smoking through regulatory approaches. The policymakers should be alerted about the increasing trend of shisha smoking and its health effects. There should be a ban on smoking shisha in public places as harmful effects on passive smokers are considerable. There should be more research promoted on poly tobacco use and the personal effects of Shisha. The shisha products should come with a strong health warning on them.
World health organizations' MPOWER measures for the tobacco-free initiative have led Middle Eastern countries to raise tobacco taxation on all tobacco products, including tobacco used for waterpipe smoking. This has a positive benefit on individuals' health with less purchase capacity and monetary gains for the government with high taxation.41
5. Conclusion
The increasing global trend of shisha use is mainly driven by misleading information about it being safe. Shisha smoke has potentially harmful chemicals, including several human carcinogens and other toxic products that affect the oral and upper aero-digestive tract. There are adverse effects on passive smokers exposed to second-hand smoke. It is a potential carcinogen and endangers pregnant women and their unborn children. The European code against cancer asserts that WPS is unsafe.42 There should be more awareness created about Shisha's harmful effects to prevent the risk to health.
Contributor Information
Shankargouda Patil, Email: dr.ravipatil@gmail.com.
Amit Vasant Mahuli, Email: amitmahuli@gmail.com.
Saman Warnakulasuriya, Email: Saman.warne@kcl.ac.uk.
References
- 1.Maziak W., Ward K.D., Afifi Soweid R.A., Eissenberg T. Tobacco smoking using a waterpipe: a re-emerging strain in a global epidemic. Tobac Control. 2004 Dec;13(4):327–333. doi: 10.1136/tc.2004.008169. PMID: 15564614; PMCID: PMC1747964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maziak W., Taleb Z.B., Bahelah R., et al. The global epidemiology of waterpipe smoking. Tobac Control. 2015 Mar;24(Suppl 1):i3–i12. doi: 10.1136/tobaccocontrol-2014-051903. (Suppl 1) Epub 2014 Oct 8. PMID: 25298368; PMCID: PMC4345835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chattopadhyay A. Emperor Akbar as a healer and his eminent physicians. Bull Indian Inst Hist Med Hyderabad. 2000 Jul-Dec;30(2):151–157. PMID: 12577995. [PubMed] [Google Scholar]
- 4.Shihadeh A., Eissenberg T., Rammah M., Salman R., Jaroudi E., El-Sabban M. Comparison of tobacco-containing and tobacco-free waterpipe products: effects on human alveolar cells. Nicotine Tob Res. 2014 Apr;16(4):496–499. doi: 10.1093/ntr/ntt193. Epub 2013 Dec 3. PMID: 24302635; PMCID: PMC4007115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Knishkowy B., Amitai Y. Water-pipe (narghile) smoking: an emerging health risk behavior. Pediatrics. 2005 Jul;116(1):e113–e119. doi: 10.1542/peds.2004-2173.PMID:15995011. [DOI] [PubMed] [Google Scholar]
- 6.Shihadeh A., Azar S., Antonios C., Haddad A. Towards a topographical model of narghile waterpipe café smoking: a pilot study in a high socioeconomic status neighborhood of Beirut, Lebanon. Pharmacol Biochem Behav. 2004 Sep;79(1):75–82. doi: 10.1016/j.pbb.2004.06.005. PMID: 15388286. [DOI] [PubMed] [Google Scholar]
- 7.Elsayed Y., Dalibalta S., Abu-Farha N. Chemical analysis and potential health risks of hookah charcoal. Sci Total Environ. 2016 Nov 1;569–570:262–268. doi: 10.1016/j.scitotenv.2016.06.108. Epub 2016 Jun 22. PMID: 27343945. [DOI] [PubMed] [Google Scholar]
- 8.Herman A.I., DeVito E.E., Jensen K.P., Sofuoglu M. Pharmacogenetics of nicotine addiction: role of dopamine. Pharmacogenomics. 2014 Feb;15(2):221–234. doi: 10.2217/pgs.13.246. PMID: 24444411; PMCID: PMC4154357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shihadeh A., Antonios C., Azar S. A portable, low-resistance puff topography instrument for pulsating, high-flow smoking devices. Behav Res Methods. 2005 Feb;37(1):186–191. doi: 10.3758/bf03206414.PMID:16097360. [DOI] [PubMed] [Google Scholar]
- 10.Jawad M., Charide R., Waziry R., Darzi A., Ballout R.A., Akl E.A. The prevalence and trends of waterpipe tobacco smoking: a systematic review. PLoS One. 2018 Feb 9;13(2) doi: 10.1371/journal.pone.0192191. PMID: 29425207; PMCID: PMC5806869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moh'd Al-Mulla A., Abdou Helmy S., Al-Lawati J., et al. Prevalence of tobacco use among students aged 13-15 years in health ministers' council/gulf cooperation council member states, 2001-2004. J Sch Health. 2008 Jun;78(6):337–343. doi: 10.1111/j.1746-1561.2008.00311.x.PMID:18489467. [DOI] [PubMed] [Google Scholar]
- 12.Primack B.A., Shensa A., Kim K.H., et al. Waterpipe smoking among U.S. university students. Nicotine Tob Res. 2013 Jan;15(1):29–35. doi: 10.1093/ntr/nts076. Epub 2012 May 28. PMID: 22641433; PMCID: PMC3524056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization (WHO) World Health Organization; Geneva, Switzerland: 2015. The GATS Atlas Global Adult Tobacco Survey. [Google Scholar]
- 14.Agaku I.T., Filippidis F.T., Vardavas C.I., et al. Poly-tobacco use among adults in 44 countries during 2008-2012: evidence for an integrative and comprehensive approach in tobacco control. Drug Alcohol Depend. 2014 Jun 1;139:60–70. doi: 10.1016/j.drugalcdep.2014.03.003. Epub 2014 Mar 15. PMID: 24685560. [DOI] [PubMed] [Google Scholar]
- 15.Waziry R., Jawad M., Ballout R.A., Al Akel M., Akl E.A. The effects of waterpipe tobacco smoking on health outcomes: an updated systematic review and meta-analysis. Int J Epidemiol. 2017 Feb 1;46(1):32–43. doi: 10.1093/ije/dyw021.PMID:27075769. [DOI] [PubMed] [Google Scholar]
- 16.Warnakulasuriya S., Dietrich T., Bornstein M.M., et al. Oral health risks of tobacco use and effects of cessation. Int Dent J. 2010 Feb;60(1):7–30. PMID: 20361572. [PubMed] [Google Scholar]
- 17.Patil S., Awan K.H., Arakeri G., et al. The relationship of "shisha" (water pipe) smoking to the risk of head and neck cancer. J Oral Pathol Med. 2019 Apr;48(4):278–283. doi: 10.1111/jop.12823. Epub 2019 Jan 20. PMID: 30604900. [DOI] [PubMed] [Google Scholar]
- 18.Aslam H.M., Saleem S., German S., Qureshi W.A. Harmful effects of Shisha: literature review. Int Arch Med. 2014 Apr 4;7:16. doi: 10.1186/1755-7682-7-16. PMID: 24708750; PMCID: PMC4003490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nasrollahzadeh D., Kamangar F., Aghcheli K., et al. Opium, tobacco, and alcohol use in relation to oesophageal squamous cell carcinoma in a high-risk area of Iran. Br J Cancer. 2008 Jun 3;98(11):1857–1863. doi: 10.1038/sj.bjc.6604369. Epub 2008 May 13. PMID: 18475303; PMCID: PMC2410115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Feng B.J., Khyatti M., Ben-Ayoub W., et al. Cannabis, tobacco and domestic fumes intake are associated with nasopharyngeal carcinoma in North Africa. Br J Cancer. 2009 Oct 6;101(7):1207–1212. doi: 10.1038/sj.bjc.6605281. Epub 2009 Sep 1. PMID: 19724280; PMCID: PMC2768108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Malik M.A., Upadhyay R., Mittal R.D., Zargar S.A., Mittal B. Association of xenobiotic metabolizing enzymes genetic polymorphisms with esophageal cancer in Kashmir Valley and influence of environmental factors. Nutr Cancer. 2010;62(6):734–742. doi: 10.1080/01635581003605904.PMID:20661821. [DOI] [PubMed] [Google Scholar]
- 22.Dar N.A., Bhat G.A., Shah I.A., et al. Hookah smoking, nass chewing, and oesophageal squamous cell carcinoma in Kashmir, India. Br J Cancer. 2012 Oct 23;107(9):1618–1623. doi: 10.1038/bjc.2012.449. Epub 2012 Oct 2. Erratum in: Br J Cancer. 2013 Apr 16;108(7):1552. Kakhdoomi, M A [corrected to Makhdoomi, M A]. PMID: 23033008; PMCID: PMC3493783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khlifi R., Olmedo P., Gil F., et al. Blood nickel and chromium levels in association with smoking and occupational exposure among head and neck cancer patients in Tunisia. Environ Sci Pollut Res Int. 2013 Nov;20(11):8282–8294. doi: 10.1007/s11356-013-1466-7. Epub 2013 Apr 28. PMID: 23625117. [DOI] [PubMed] [Google Scholar]
- 24.Quadri M.F., Alharbi F., Bajonaid A.M., Moafa I.H., Sharwani A.A., Alamir A.H. Oral squamous cell carcinoma and associated risk factors in Jazan, Saudi Arabia: a hospital based case control study. Asian Pac J Cancer Prev APJCP. 2015;16(10):4335–4338. doi: 10.7314/apjcp.2015.16.10.4335.PMID:26028095. [DOI] [PubMed] [Google Scholar]
- 25.Zaid K., Azar-Maalouf E., Barakat C., Chantiri M. p53 overexpression in oral mucosa in relation to shisha smoking in Syria and Lebanon. Asian Pac J Cancer Prev APJCP. 2018 Jul 27;19(7):1879–1882. doi: 10.22034/APJCP.2018.19.7.1879. PMID: 30049200; PMCID: PMC6165666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li V.D., Li K.H., Li J.T. TP53 mutations as potential prognostic markers for specific cancers: analysis of data from the Cancer Genome Atlas and the International Agency for Research on Cancer TP53 Database. J Cancer Res Clin Oncol. 2019 Mar;145(3):625–636. doi: 10.1007/s00432-018-2817-z. Epub 2018 Dec 12. PMID: 30542790. [DOI] [PubMed] [Google Scholar]
- 27.Patil S., Patel K., Advani J., et al. Multiomic analysis of oral keratinocytes chronically exposed to Shisha. J Oral Pathol Med. 2019 Apr;48(4):284–289. doi: 10.1111/jop.12828. Epub 2019 Feb 15. PMID: 30659648. [DOI] [PubMed] [Google Scholar]
- 28.Patil S., Rajagopalan P., Patel K., et al. Chronic shisha exposure alters phosphoproteome of oral keratinocytes. J Cell Commun Signal. 2019 Sep;13(3):281–289. doi: 10.1007/s12079-019-00528-4. Epub 2019 Jul 19. PMID: 31321732; PMCID: PMC6732141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Patil S., Subbannayya T., Mohan S.V., et al. Proteomic changes in oral keratinocytes chronically exposed to shisha (water pipe) OMICS. 2019 Feb;23(2):86–97. doi: 10.1089/omi.2018.0173.PMID:30767727. [DOI] [PubMed] [Google Scholar]
- 30.Patil S., Babu N., Subbannayya T., et al. Secretome analysis of oral keratinocytes chronically exposed to Shisha. Cancer Biomarkers. 2019;25(1):29–41. doi: 10.3233/CBM-182099. PMID: 31033461. [DOI] [PubMed] [Google Scholar]
- 31.Awan K.H., Siddiqi K., Patil Sh, Hussain Q.A. Assessing the effect of waterpipe smoking on cancer outcome - a systematic review of current evidence. Asian Pac J Cancer Prev APJCP. 2017 Feb 1;18(2):495–502. doi: 10.22034/APJCP.2017.18.2.495. PMID: 28345836; PMCID: PMC5454749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Türkmen S., Eryigit U., Sahin A., Yeniocak S., Turedi S. Carbon monoxide poisoning associated with water pipe smoking. Clin Toxicol. 2011 Aug;49(7):697–698. doi: 10.3109/15563650.2011.598160.Epub.2011.Aug.8. PMID: 21819288. [DOI] [PubMed] [Google Scholar]
- 33.Baalbaki R., Itani L., El Kebbi L., et al. Association between smoking hookahs (shishas) and higher risk of obesity: a systematic review of population-based studies. J Cardiovasc Dev Dis. 2019 Jun 16;6(2):23. doi: 10.3390/jcdd6020023. PMID: 31208138; PMCID: PMC6617155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bhatnagar A., Maziak W., Eissenberg T., et al. Water pipe (hookah) smoking and cardiovascular disease risk: a scientific statement from the American heart association. Circulation. 2019 May 7;139(19):e917–e936. doi: 10.1161/CIR.0000000000000671. PMID: 30845826; PMCID: PMC6600812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Javed F., Al-Kheraif A.A., Rahman I., et al. Comparison of clinical and radiographic periodontal status between habitual water-pipe smokers and cigarette smokers. J Periodontol. 2016 Feb;87(2):142–147. doi: 10.1902/jop.2015.150235. Epub 2015 Oct 2. PMID: 26430928. [DOI] [PubMed] [Google Scholar]
- 36.Natto S., Baljoon M., Bergström J. Tobacco smoking and periodontal bone height in a Saudi Arabian population. J Clin Periodontol. 2005 Sep;32(9):1000–1006. doi: 10.1111/j.1600-051X.2005.00813.x. PMID: 16104965. [DOI] [PubMed] [Google Scholar]
- 37.Baljoon M., Natto S., Abanmy A., Bergström J. Smoking and vertical bone defects in a Saudi Arabian population. Oral Health Prev Dent. 2005;3(3):173–182. PMID: 16355651. [PubMed] [Google Scholar]
- 38.Akl E.A., Gaddam S., Gunukula S.K., Honeine R., Jaoude P.A., Irani J. The effects of waterpipe tobacco smoking on health outcomes: a systematic review. Int J Epidemiol. 2010 Jun;39(3):834–857. doi: 10.1093/ije/dyq002. Epub 2010 Mar 4. PMID: 20207606. [DOI] [PubMed] [Google Scholar]
- 39.Maziak W., Jawad M., Jawad S., Ward K.D., Eissenberg T., Asfar T. Interventions for waterpipe smoking cessation. Cochrane Database Syst Rev. 2015;7 doi: 10.1002/14651858.CD005549.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Babaie J., Ahmadi A., Abdollahi G., Doshmangir L. Preventing and controlling water pipe smoking: a systematic review of management interventions. BMC Publ Health. 2021 Dec;21(1):1–2. doi: 10.1186/s12889-021-10306-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tobacco taxation in the eastern mediterranean region. http://applications.emro.who.int/dsaf/emropub_2010_1247.pdf?ua=1&ua=1 [accessed September 08, 2019]. Available at URL:
- 42.European code against cancer. http://cancer-code-europe.iarc.fr/index.php/en/ecac-12-ways/tobacco/201-water-pipe-smoking-safe [accessed September 08, 2019]. Available at URL: