Abstract
Testicular torsion is the most common urosurgical emergency in infants, children, and young adolescents, resulting in irreversible ischemic injury within hours; hence demanding urgent surgical attention. It has a bimodal distribution with the highest incidence occurring after puberty, followed by the neonatal period peak. Though the imaging modalities are helpful in the diagnosis, nothing can supersede the clinical findings and judgment.
Keywords: Testicular torsion, Ischemia, Sonology, Scintigraphy, Exploration
Introduction
The testis is vulnerable to torsion because of the nature of its anatomical suspension within the sac or layers of peritoneum within the scrotum, hence it's sudden twisting within the sac (tunica vaginalis) occludes its arterial supply, rendering it ischemic, tender, and painful. Unless surgically corrected within 8-12 hours, the impairment of the blood supply sets in and results in loss of the testis.
The extent of the twist and the duration of the episode are the most important factors; a 720° twist causes more rapid ischemia than twists of 360° or less, If untwisted or detorted within 6 hours there is nearly a 100% chance of testicular salvage compared with a 20% salvage rate if the surgery is delayed by 24 hours.
Case report
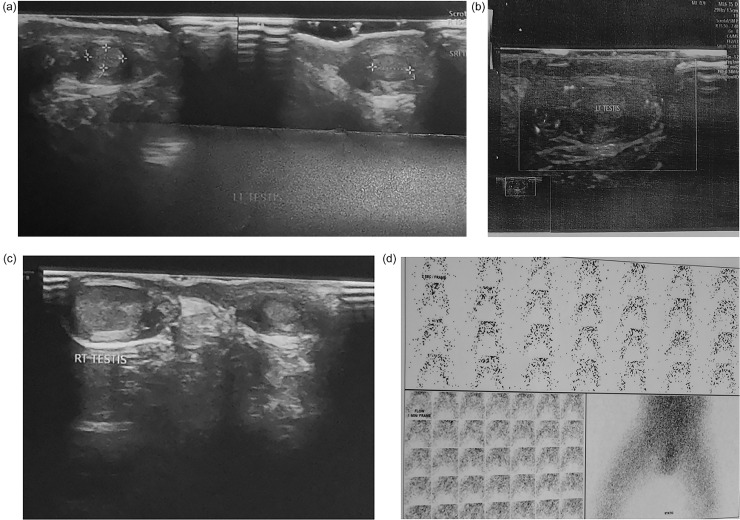
A 5 months old male baby born by full-term vaginal delivery with 2.5 kg birth weight was noted to have left scrotal painful swelling for 15 days along with irritability, fever, and sonology showing left testicular torsion. The baby was observed without any medications for 15 days, baby was referred to us after 15 days for further management due to persistent symptoms. On examination left testis was tender on admission; sonology done again showed the same findings consistent with left testicular torsion (Fig. 1A-C), but however, radionuclide scan, Technetium 99 pertechnate; revealed bilaterally normal testis and cord structures without any ischemic changes (Fig. 1D). Since clinical findings didn't correlate with sonological findings, the author decided to conserve with intravenous medications. Baby improved clinically in 5 days and was discharged once asymptomatic. But however sonology done on follow-up even after 15 days persisted to show left testicular torsion without any blood flow (Fig. 1A-C); hence this time scrotal exploration was done, which revealed bilaterally normal testis and cord structures without any kind of inflammation or loss of vascularity. Baby is doing well and is on follow-up with us.
Fig. 1.
(A and B) Gray scale sonographic image showing left testis having heteroechoic echotexture, (C) Gray scale sonographic image of right testis showing normal echo pattern, (D) Radionuclide scan showing normal uptake of both testis and epididymis bilaterally.
Discussion
The high investment of the tunica vaginalis (intravaginal) over the cord causing the testis to hang within the tunica like a clapper in a bell, is the most common cause especially in adolescents as well as in neonates. Whereas, the torsion of the entire cord occurring before fixation of the tunica vaginalis and the dartos within the scrotum (extra vaginal), commonly occurs in perinatal infants [1], [2].
Testicular torsion is a clinical diagnosis, typically presenting with severe acute unilateral scrotal pain, nausea, and vomiting. Physical examination may reveal a high-riding transversely oriented tender testicle, an anterior epididymis with an absent cremasteric reflex. In contrast, torsion of the appendix testis or appendix epididymis often presents with localized tenderness at the superior pole of the testis or caput epididymis with reactive hydrocele [1], [2].
Testicular ultrasonography (US) is an initial ideal imaging tool to diagnose. The reduced or absent testicular blood flow has high diagnostic accuracy with a sensitivity of 86%-100% and a specificity of 97.9%-100%. The "whirlpool sign" of the twisted spermatic cord, is considered to be a more direct and specific sign of testicular torsion and is valuable for the diagnosis of complete, intermittent, and incomplete torsion of the testis. Despite its high sensitivity and specificity, both false-negative and false-positive findings occur. However, Testis with color Doppler flow signals might be an obstacle for surgical exploration with resultant testicular loss in the false-negative cases [2], [3].
Heterogeneity of the testis with swelling and edema suggests no viability, whereas a homogenous echotexture suggests testicular viability on gray scale sonography [2], [3].
Scrotal scintigraphy using Technicium 99 pertechnate injected intravenously on an emergency basis is a valid and reliable test to diagnose testicular torsion whenever clinical and sonological findings are inconclusive [3,4].
The surgical exploration of the scrotum is the most definitive and reliable management option, consisting of detorsion of the affected testis and waiting for its “pinking” up or improved perfusion or orchiectomy for necrosed and gangrenous testis followed by contralateral orchidopexy [1], [5].
The golden time for torsion reduction is 6-8 hours. The salvage rate is almost 100% if treated within 6 hours after onset but decreases quickly with time, declining subsequently to 70% within 6-12 hours and 20% within 12-24 hours [1], [5].
If history and physical examination suggests torsion, immediate surgical exploration is indicated which should not be postponed to perform imaging studies. Delay in treatment may be associated with decreased fertility, or may necessitate orchiectomy [1], [5].
The author had 5 months male baby with sudden onset of left testicular pain since 15 days and immediate as well as follow up sonology persisted to show testicular torsion with loss of vascularity, but however clinical findings and radionuclide scan did not suggest so, revealing normal bilateral testis and epididymis on scrotal exploration.
Conclusion
Clinical findings and clinical judgment from the attending surgeon are sufficient to take a decision for scrotal exploration for salvaging the testis.
Ethical approval taken
Written and verbal consent taken from parents.
Patient consent
Both verbal and written informed consent has been obtained from parents for the publication of this manuscript.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment: Author would like to thank all staffs of IGICH, Bengaluru, Karnataka, India.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.radcr.2022.05.010.
Appendix. Supplementary materials
References
- 1.Bandarkar AN, Blask AR. Testicular torsion with preserved flow: key sonographic features and value-added approach to diagnosis. Pediatr Radiol. 2018;48:735–744. doi: 10.1007/s00247-018-4093-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Osemlak P., Jędrzejewski G., Woźniak M., Nachulewicz P. Ultrasound evaluation of long-term outcome in boys operated on due to testicular torsion. Medicine (Baltimore) 2021;100(21):e26057. doi: 10.1097/MD.0000000000026057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aihole JS, Narendrababu M, Deepak J, Jadhavv V, Ramesh S. Acute scrotum: a rare presentation. IntJ Case Rep Images. 2015;6:267–271. [Google Scholar]
- 4.Burud IAS, Alsagoff SMI, Ganesin R, Selvam ST, Zakaria NAB, Tata MD. Correlation of ultrasonography and surgical outcome in patients with testicular torsion. Pan Afr Med J. 2020;36:45. doi: 10.11604/pamj.2020.36.45.21824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DaJusta DG, Granberg CF, Villanueva C, Baker LA. Contemporary review of testicular torsion: new concepts, emerging technologies and potential therapeutics. J Pediatr Urol. 2013;9(6 Pt A):723–730. doi: 10.1016/j.jpurol.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.