Abstract
Bronchopulmonary arterial fistula consists of an abnormal connection between the bronchus and the vascular tree and is a rare but serious complication associated with a variety of lung interventions. We present a case of a 61-year-old female with a history of metastatic breast cancer treated with lumpectomy and radiation 20 years prior, who was found to have a fistula between the right pulmonary artery and the right mainstem bronchus. Our patient was treated endovascularly with coil embolization in the setting of massive hemoptysis flooding the trachea, which was successful in controlling the acute bleed, although care was withdrawn in the following days following a discussion with the family given the presence of advanced metastatic disease. This case illustrates the use of endovascular techniques to treat an actively bleeding bronchopulmonary arterial fistulae, including a review of the existing literature regarding the optimal endovascular management strategy. Although our patient did not achieve the best outcome, endovascular intervention with stent-placement or embolization can serve to temporarily halt blood flow through the fistula, stabilizing the patient and allowing for more radical therapy after improvement.
Keywords: Bronchopulmonary arterial fistula, Bronchovascular fistula, Coil embolization, Endobronchial stent
Abbreviations: BPAF, bronchopulmonary arterial fistula; SEMS, self-expanding metallic stent; RPA, right pulmonary artery; RMB, right mainstem bronchus; RUL, right upper lobe; RPA-TA, right pulmonary artery-truncus anterior; DSA, digital subtraction angiogram; IP, interventional pulmonologist
Introduction
Bronchopulmonary arterial fistula (BPAF) consists of an abnormal connection between the bronchus and the vascular tree and is associated with a variety of lung interventions including lung transplantation, endobronchial stent placement with erosion, radiation therapy, and anastomotic complications following pulmonary sleeve resection [1]. It is a rare but serious complication that often presents with large-volume hemoptysis and has a high risk of respiratory arrest and death. Fistulae may connect the bronchus with the pulmonary artery, pulmonary vein, azygos vein, aorta, or left atrium [2,3].
We present a case of a 61-year-old female with a history of metastatic breast cancer treated with lumpectomy and radiation 20 years prior, who was found to have a fistula between the right pulmonary artery (RPA) and the right mainstem bronchus (RMB) after a silicone Y-stent placement three weeks prior to presentation. Our patient was treated endovascularly with metallic coils embolization.
Case report
A 61-year-old female with a history of left breast invasive ductal carcinoma (status post lumpectomy, hormonal therapy, and adjuvant radiation 20 years prior) presented with progressive dyspnea and worsening cough over the last 6 months, with recent onset of blurry vision and headaches. One-month prior, CT of the head and chest were performed showing at least 4 small brain lesions, a RUL perihilar mass, and multiple other lung nodules, all likely metastatic. She then underwent bronchoscopy which revealed 30% and 70% luminal narrowing of the trachea and right main stem bronchus, respectively. The RUL bronchus was 100% obstructed and cannulation was not attempted. Endobronchial biopsy of the mass followed by balloon dilation and Y-stent placement were performed successfully. She was discharged on high dose steroids and planned for outpatient radiation treatment to the brain and lungs. One month later, she presented to the emergency department with hemoptysis and a syncopal episode. Repeat CT head revealed known enhancing lesions. Seizure was ruled out after a detailed workup. A CT angiogram of the chest showed interval development of central cavitation within the RUL paratracheal lung mass. The right pulmonary artery truncus anterior (RPA-TA) was in close proximity to the mass, with evidence of subtle wall irregularity suggesting a possible pseudoaneurysm or fistula to the cavitary mass and RMB (Fig. 1).
Fig. 1.
(a-b). Coronal oblique multiplanar reconstructed (a), and axial images of the patient CT pulmonary angiogram showing the right upper lobe para-hilar cavitary mass (star) with close proximity to the right pulmonary artery truncus anterior (arrow). On the thin-slice image (not shown), there was subtle wall irregularity of this vessel suggesting the possibility of a pseudoaneurysm or a fistula.
External chest radiation therapy was initiated on hospital day 2 which was well tolerated. On hospital day 4, she started developing worsening shortness of breath with massive hemoptysis that necessitated emergent endotracheal intubation. Interventional radiology (IR) was consulted for possible RPA embolization, while the patient was taken for emergent bronchoscopy at the same time. There was scant blood within the left lung, and significant clot burden within the right main stem bronchus. The latter was suctioned with restoration of 50% luminal patency. She was then brought from endoscopy to the IR suite for diagnostic arteriogram and possible intervention.
A right common femoral venous access was obtained. The right pulmonary artery was catheterized using the combination of 0.035" stiff angled glide guidewire, J tipped wire, an angled pigtail catheter, and a 90 cm Flexor Check-Flo guiding sheath (Cook Medical LLC. Blommington, IN). An RPA digital subtraction angiogram (DSA) revealed a slightly irregular RUL-PA with possible small pseudoaneurysm without clear evidence of active arterial bleed. The initial plan was to catheterize across the abnormality, then evaluate for embolization with coils vs. deploying a covered stent. We had Viabahn (W. L. Gore & Associates, Inc. Flagstaff, AZ) covered stents 5 mm and 6 mm, each in the length of 2.5 cm and 5 cm, made available in the room based on the prior CTA of the chest. A 5F Berenstein catheter preloaded with a Progreat microcatheter and a Fathom microwire were inserted to catheterize the RPA-TA. However, a few minutes after the initial angiogram, the patient began having increased hemoptysis from the endotracheal tube during the procedure. Hand contrast injection through the catheter within the RPA showed possible active bleed into the right mainstem bronchus. A repeat DSA through the sidearm of the sheath revealed a widely open fistula between the proximal segment of the RPA-TA and the RMB with blood flooding the tracheobronchial tree (Fig. 2).
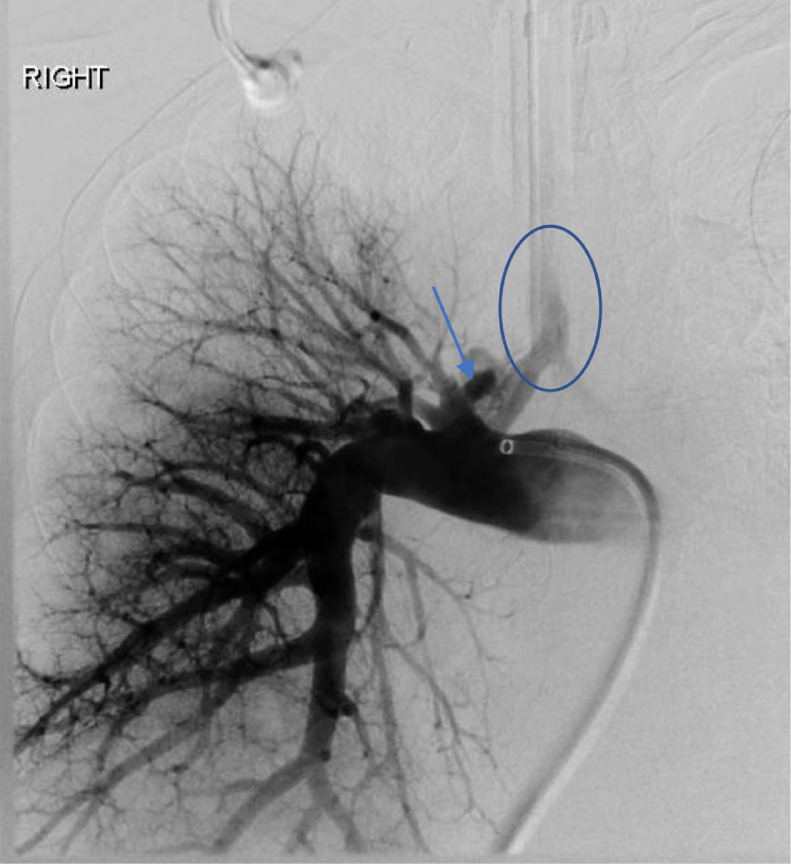
Fig. 2.
Right pulmonary digital subtraction angiogram showing a fistula (arrow) between the right pulmonary artery truncus anterior, the cavitary lesion and the right main stem bronchus with blood flooding the trachea (circle).
While the rapid response code and anesthesia team were called to resuscitate the patient and actively suction the ET tube, the Berenstein catheter was advanced quickly into the RPA-TA with contrast injection opacifying the fistula. It was evident that our catheter was within the fistula and not across. Due to the emergent need to control the bleeding and protect the airway, multiple detachable coils were deployed through the microcatheter in this location. Some of the coils protruded partially into the RMB. Post embolization angiogram showed occlusion of the fistula and near complete occlusion of the RPA-TA (Fig. 3).
Fig. 3.
Repeat pulmonary digital subtraction angiography post coil (circle) embolization showed complete occlusion of the truncus anterior artery and the fistula.
Following the procedure, the patient was transferred to the ICU for continued management. Diagnostic bronchoscopy one day following the procedure revealed the metallic coils protruding into the RMB which were mobile on expiratory phase, with no bleeding identified. Chest radiograph later the same day showed the coil starting to unravel into the right bronchial tree. A multidisciplinary discussion among the family and providers was taken. The different options were discussed including surgical intervention versus rendezvous procedure of bronchoscopy and angiography, where the coils will be removed carefully through a bronchoscope while catheterization across the fistula is attempted, to be followed by a planned coiling or covered stent placement. Although the pulmonary bleeding was temporarily controlled, due to presence of brain metastases and poor prognostic survival, a family agreement was made to deny further intervention and opted for withdrawal of care. Unfortunately, the patient was terminally extubated later on post-op day 2.
Discussion
Bronchovascular fistula formation is a rare but serious complication associated with a high risk of mortality. It has been most well-described following lung transplantation procedures but is also associated with malignancy and endobronchial stent placement. Factors leading to the formation of bronchovascular fistulae include ischemia of the airway, devascularization of the bronchial tree, and altered bronchial anastomotic healing [4]. Fistulae usually result from ischemic or infectious necrosis of the bronchus accompanied by erosion of an adjacent pulmonary vessel [5].
Bronchovascular fistula has most often been associated with placement of self-expanding metallic stent (SEMS) placement [6] in the literature and has been reported anytime post-stenting, from early days to weeks to years after placement, and is fatal in most cases. Our patient underwent stent placement three weeks prior to fistula detection. Radiation by itself has been reported as a risk factor with a case report describing fistula development 19 years post-radiation, even in the absence of cancer recurrence on autopsy [7]. The risk of fistula development increases with the coexistence of multiple factors, such as our patient who had a history of malignancy, radiation therapy, and recent endobronchial stent placement.
The ideal management approach for BPAF is not well known given the rarity of this complication. Immediate surgical management is required to achieve the most optimal outcome with rare case reports in the literature [8], [9], [10]. There are sparse cases of endovascular repairs of BPAF. Stent grafts were used in 2 cases. Both patients were alive and bleeding recurrence free on follow up periods of 2 and 6 months [11,12]. In one case, stent assisted coiling and glue were used initially, however bleeding recurred which required complete embolization of the right interlobar artery using coils and Amplatzer plug. The patient died 82 days after the initial embolization due to sepsis complications [13]. Plugs were used in two cases, in one case the entire right main pulmonary artery was embolized while in the second case the right lower lobe pulmonary artery was embolized. In the first case, the patient remained hemoptysis free during the reported follow up period of 6 months, and in the latter the patient was discharged on day 4 post-op without a reported longer follow up [14,15].
Our case illustrates the role of endovascular intervention and coil embolization in temporarily halting blood flow through the fistula, stabilizing the patient, and allowing for more radical therapy after improvement. A multidisciplinary team that includes a cardiothoracic surgeon, interventional pulmonologist (IP), and an endovascular interventionist, is critical in these cases. More research is needed to determine the most effective treatment strategy for patients who are not surgical candidates. Nonetheless, we can pull some teaching points from the sparse case reports that were managed using an endovascular approach. We suggest a rendezvous with the IP placing an endobronchial balloon to tamponade the fistula while an endovascular interventionist attempts to catheterize across the BFAF. Ideally, the goal is to embolize using a plug or coils, or to place a covered stent across the pulmonary branch culprit of the fistula. However, if this is challenging, placing a covered stent to exclude the entire culprit lobar pulmonary artery, or even embolization using coils or plugs in the lobar artery or the main ipsilateral pulmonary artery are viable options in the correct scenario based on prior case reports (Fig. 4). These interventions have shown to prolong survival in these otherwise fatal cases [11], [12], [13], [14], [15].
Fig. 4.
The angiogram annotation summarizes prior case reports of endovascular treatments of the BPAF. Straight blue line: A covered stent was placed to treat RPA fistula. The stent excluded the right upper and middle lobe pulmonary artery branches. Green line: a covered stent was placed within the right interlobar pulmonary artery, area of the fistula, only some segmental pulmonary artery branches were excluded. Blue cylinders: Amplatzer plugs and coils were used to embolize the right interlobar pulmonary artery and main pulmonary artery in two different cases of BPAF. Orange line: Ideal coil embolization or covered stent placement in our case.
Conclusion
Bronchovascular fistula is a rare complication which can be associated with malignancy, prior radiation therapy, and endobronchial stent placement. This case illustrates the use of endovascular techniques to treat an actively bleeding bronchopulmonary arterial fistulae, including a review of the existing literature regarding the optimal endovascular management strategy. Although our patient did not achieve the best outcome, endovascular intervention with stent-placement or embolization can serve to temporarily halt blood flow through the fistula, stabilizing the patient and allowing for more radical “second-look” therapy after improvement. A multidisciplinary team that includes a cardiothoracic surgeon, interventional pulmonologist (IP), and an endovascular interventionist, is critical in these cases. More research is needed to determine the most optimal endovascular management strategy for patients with BPAF who are not good surgical candidates.
Acknowledgments
Patient consent statement
Written, informed consent was obtained from the patient's family for publication of this manuscript.
Financial Support
This study was not supported by any funding.
Footnotes
Competing Interests: The authors declare that they have no relevant financial or non-financial interests to disclose.
Acknowledgments: None.
References
- 1.Yee Gabrielle, et al. Massive hemoptysis resulting from a fistula between the bronchus intermedius and pulmonary artery: a novel clinical presentation. J Surg Case Rep. 2020;2020(8):rjaa209. doi: 10.1093/jscr/rjaa209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Santacruz Jose Fernando, Mehta Atul C. Airway complications and management after lung transplantation: ischemia, dehiscence, and stenosis. Proc Am Thoracic Soc. 2009;6(1):79–93. doi: 10.1513/pats.200808-094GO. [DOI] [PubMed] [Google Scholar]
- 3.Hoff Steven J., Johnson Joyce E., Frist William H. Aortobronchial fistula after unilateral lung transplantation. Ann Thoracic Surg. 1993;56(6):1402–1403. doi: 10.1016/0003-4975(93)90695-e. [DOI] [PubMed] [Google Scholar]
- 4.Murthy SC, Blackstone EH, Gildea TR, et al. Impact of anastomotic airway complications after lung transplantation. Ann Thorac Surg. 2007;84(2):401–409. doi: 10.1016/j.athoracsur.2007.05.018. Aug409.e1-4. doi: 10.1016/j.athoracsur.2007.05.018. PMID: 17643606. [DOI] [PubMed] [Google Scholar]
- 5.Guth S, Mayer E, Fischer B, Lill J, Weiler N, Oelert H. Bilobectomy for massive hemoptysis after bilateral lung transplantation. J Thorac Cardiovasc Surg. 2001;121(6):1194–1195. doi: 10.1067/mtc.2001.112460. JunPMID: 11385388. [DOI] [PubMed] [Google Scholar]
- 6.Choudhary Chirag, et al. Broncho-vascular fistulas from self-expanding metallic stents: a retrospective case review. Ann Thoracic Med. 2013;8(2):116. doi: 10.4103/1817-1737.109830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Suzuki Hideto, Fukunaga Tatsushige. Death due to a bronchus-pulmonary artery fistula developed 19 years after radiotherapy: a forensic autopsy case report. Legal Med. 2020;47 doi: 10.1016/j.legalmed.2020.101774. [DOI] [PubMed] [Google Scholar]
- 8.Rea Federico, et al. Salvage right pneumonectomy in a patient with bronchial–pulmonary artery fistula after bilateral sequential lung transplantation. J Heart Lung Transplant. 2006;25(11):1383–1386. doi: 10.1016/j.healun.2006.09.013. [DOI] [PubMed] [Google Scholar]
- 9.Shilyansky Joel, et al. Pulmonary artery–bronchial fistula during lymphoma treatment. J Thoracic Cardiovasc Surg. 1994;108(4):790–791. [PubMed] [Google Scholar]
- 10.Rea F, Marulli G, Loy M, Bortolotti L, Giacometti C, Schiavon M, Calabrese F. Salvage right pneumonectomy in a patient with bronchial-pulmonary artery fistula after bilateral sequential lung transplantation. J Heart Lung Transplant. 2006;25(11):1383–1386. doi: 10.1016/j.healun.2006.09.013. NovPMID: 17097507. [DOI] [PubMed] [Google Scholar]
- 11.Davison Brian D., et al. Endovascular stent-graft repair of a pulmonary artery–bronchial fistula. J Vasc Interventional Radiol. 2003;14(7):929–932. doi: 10.1097/01.rvi.0000082825.75926.82. [DOI] [PubMed] [Google Scholar]
- 12.Raissi Driss, et al. Pulmonary artery stent graft repair of bronchovascular fistula. Ann Thoracic Surg. 2020;110(2):e103–e105. doi: 10.1016/j.athoracsur.2019.12.029. [DOI] [PubMed] [Google Scholar]
- 13.Woodhams R, Fujii K, Takigawa M, Inoue Y. Pulmonary artery-bronchus fistula treated with a combination of bare metal stent, metallic coil, and N-Butyl cyanoacrylate. J Vasc Interv Radiol. 2021;32:152–155. doi: 10.1016/j.jvir.2020.08.010. [DOI] [PubMed] [Google Scholar]
- 14.Chehab Monzer A., et al. Massive hemoptysis due to bronchopulmonary arterial fistula successfuly treated with amplatzer plug occlusion. J Biomed Graph Comput. 2014;4(4):68. [Google Scholar]
- 15.Mhanna Laurent, et al. Endobronchial protrusion of an amplatzer plug after embolization of the pulmonary artery. J Bronchol Interventional Pulmonol. 2017;24(3):33–34. doi: 10.1097/LBR.0000000000000376. [DOI] [PubMed] [Google Scholar]