Abstract
Ethiopia has taken unprecedented preventive measures, such as confinement to home and closure of schools and offices to halt the spread of Corona virus pandemic in the country. Unfortunately, such orders may have been associated with intimate partner violence (IPV) against women but there is no study conducted to assess the magnitude of IPV during the lock-downs in the country. Thus, this study intended to investigate the prevalence and associated factors of IPV against women during the COVID-19 pandemic restrictions. A community-based cross-sectional study was conducted on sample of 617 married or cohabited women. A systematic random sampling technique was employed to identify and enroll women who are married. A logistic regression analysis was used to identify the predictors of IPV among women and all statistical analyses were carried out using STATA 14.2. In this study, amongst the 589 married women who were included in the analysis, 22.4% [95% CI: 19.1%, 25.9%] were experienced at least one form of IPV. Additionally, 11.0%, 20.0%, and 13.8% of women also experienced physical, psychological, and sexual IPVs respectively. After adjusting for covariate; being illiterate [AOR=2.37: 95% CI 1.29, 4.35], having illiterate husband [AOR=2.67: 95% CI 1.36, 5.21], having substance user husband (alcohol, chat or cigarettes) [AOR=2.75: 95% CI 1.42, 5.34], and community tolerant attitude to violence [AOR=2.97: 95% CI 1.17, 7.61] were the independent predictors of IPV amongst married women. In conclusion, the prevalence of IPV among married women was comparable to the national pre-COVID figure of IPV. Therefore, national and regional governments should work toward enhancing gender equality, coupled with addressing risk factors at multiple levels, using community- and institution-based approaches to prevent IPV and to specifically achieve SDG5 of eliminating violence against women by 2030.
Keywords: intimate partner violence, associated factors, COVID-19, married women, Ethiopia
Introduction
The World Health Organization (WHO) declared the coronavirus disease 2019 (COVID-19) as a pandemic due to the ease of spread and severity of the virus (Wu et al., 2020), and it caused an estimated 7 million cases and nearly half a million deaths (WHO, 2020a). As a direct result, countries across the world have taken different preventive measures to help reduce the spread, which include population movement restriction, confinement to home, school closure, and other social services, some of which have been seen to increase the risk of domestic violence against women (Davis et al., 2020; Dong et al., 2020; Hatchimonji et al., 2020; Lee, 2020).
Intimate partner violence (IPV) is defined by the WHO as “a physical, sexual, or psychological coercive act by a current or former partner or spouse to a woman” (WHO, 2012). IPV has increased during the COVID-19 crisis across the globe, remarkably in Africa (Duncan et al., 2020; Jarnecke & Flanagan, 2020; John et al., 2020; Mazza et al., 2020). According to a WHO report, COVID-19 pandemic restrictions have created an opportunity for violence against women (Campbell, 2020; WHO, 2020b). For example, the government’s stay-at-home order and closure of workplaces may have indirectly forced women to spend more time in home and ultimately, exposed these women to increased domestic violence by their partners. This scenario is supported by the CDC report, which states approximately one in four women report experiencing any form of IPV (Boserup et al., 2020).
Moreover, other studies have revealed that majority of economically disadvantaged women and young age women are prone to IPV. In addition, noneducated women, women whose partners control behavior and finance, and women who have alcohol drinking partners are the most common victims of IPV during COVID-19 pandemic restrictions (Mazza et al., 2020; Moreira & Da Costa, 2020; Roesch et al., 2020).
Specifically, Ethiopia has taken similar preventive and control measures to halt the spread of COVID-19. These include school closure, stay-at-home, social distancing, increased hand hygiene stations, creation of isolation centers, and establishment of state emergency at the national level (FMOH, 2020a, 2020b; Jemal et al., 2020). However, the federal government has not addressed any consequences due to these preventive measures such as IPV against women (Moreira & Da Costa, 2020).
Despite the increased reports of IPV cases during the ongoing COVID-19 pandemic (Duncan et al., 2020; Jarnecke & Flanagan, 2020; Taub, 2020; Van Gelder et al., 2020), there is a little research to assess the factors and magnitude of IPV during the pandemic. Therefore, this study aimed to assess the prevalence and associated factors of IPV against women during COVID-19 pandemic restrictions. Furthermore, the results of this study will offer vital information for policymakers, program planners, and other stakeholders who have interests to stop violence against women in developing nations including Ethiopia.
Methods and Materials
Study Setting and Participants
The community-based, cross-sectional study was conducted from June 26, 2020 to July 10, 2020 in Dessie administration city to assess the prevalence of IPV and its determinants among married women living during the COVID-19 pandemic restrictions. Dessie is located 401km away from the capital city of Ethiopia, Addis Ababa. It is also the capital city of South Wollo zone, it has five sub-cities, and 26 kebeles (lower administrative units).
According to the city’s administration plan commission report (CAPCR, 2020), it has a total population of 422,471. Of these, 224,332 (53.14%) are females.
All married/cohabitated women who are living in Dessie since the pandemic was declared were included in this study. However, women who had serious illness and unable to communicate during data collection period were excluded in this study.
Sample Size Determination and Sampling Techniques
The final sample size was determined using a single population proportion formula with assumptions: 5% type I error, 95% confidence intervals (CI), design effect of 2, 24% proportion for physical and emotional violence from Ethiopian Demographic and Health Survey (EDHS)-2016 report (Central Statistical Agency - CSA/Ethiopia & ICF, 2017). The maximum sample size was considered after checking various parameters of measurement from prevalence and associate factors. Then, the researchers added 10% to compensate for the nonresponse of participants and the final sample size became 617.
Where: n = required sample size, Zα/2 = critical value for normal distribution at 95% confidence level (1.96), p = proportion of physical and emotional IPV among married women, d = 0.05 (5 % margin of error), and DEFF= design effect to compensate loss of efficient of sample power.
Out of five sub-cities, two sub-cities (Menafesha and Hotie sub-cities) were selected using lottery method. The calculated sample size was proportionally allocated into four randomly selected kebeles. There were a total of 4,320 married women in the randomly selected kebeles (i.e., Kebele-1 = 990, Kebele-2 = 1,120, Kebele-3 = 1,080, and Kebele-4 = 1130). A systematic random sampling technique was employed to enroll the study participants. Accordingly, every seventh participant was selected using a systematic random sampling technique till the required sample size reached.
Study Variables
Dependent variable. Any IPV against women (yes/no), in which women who experienced at least one of the three types of IPV (i.e., physical, sexual or emotional violence) were classified as having experienced any IPV during the COVID-19 pandemic.
Independent variables. Sociodemographic characteristics (age, age at marriage, educational level, occupation status, average monthly income, religion, family size, husband education level, husband occupation), women and the husband’s substance use (alcohol, chat, cigarette), female autonomy related (head of household, financial control, decision on family planning and other family related issues), community practice that support IPV against women, and polygamy practice.
Data Collection Tools and Techniques
A questionnaire was adapted from a study done in Ethiopia to assess the reliability of the tools for the assessment of domestic violence against women in a low-income country settings (Semahegn et al., 2019), EDHS-2016 (Central Statistical Agency - CSA/Ethiopia & ICF, 2017), and WHO-2005 multi-country (WHO, 2005) violence against women assessment tools and modified in contexts. The questionnaire was prepared in English and consisted of sociodemographic characteristics, substance use-related (alcohol, chat, cigarette/shisha, or IV drug), female autonomy-related, community-based traditional practice-related, and 18 items for IPV-related questions. The IPV-related questions included six physical IPV, eight psychological IPV, and four sexual IPV related questions.
Physical IPV. Women who experienced any of the following: (a) Has he pushed or shoved you, shaken you, or thrown something at you? (b) Has he punched or hit you with his fist, or twisted your arm or with something that could hurt you? (c) Has he slapped, kicked, dragged, or beaten you? (d) Has he attacked you with a knife, gun, or other type of weapon? (e) Have you been scalded or burnt purposefully by your husband? (f) Has he choked at you that may disgracing you in the last three months?
Emotional IPV. Women who experienced any of the following abusive acts: (a) Have you felt bad until you hated yourself for blasphemy? (b) Have you been threatened by your husband with an object such as a stick, belt, knife, gun, or other type of weapon? (c) Have you been ignored or shown indifference by your husband? (d) Has he belittled or humiliated you in front of other people? (e) Have you been denied by your husband on your basic personal needs? (f) Have you been intentionally not involved by your husband on decision-making in the family? (g) Have your husband intentionally made you sad or angry? (h) Have you intentionally threatened to hurt your family, relatives or anything you love in the last three months?
Sexual IPV. Women who experienced any of the following: (a) Have you been physically forced by your husband to have sex when you did not want to? (b) Have you been intentionally denied or avoided sex by your husband? (c) Did you have sexual intercourse when you did not want because you were afraid of what he might do latter? (d) Has he forced you to do something sexual that you found degrading or humiliating in the last three months?
The questionnaire was translated into the local language (Amharic) and back to English to keep its consistency. The tool was pretested on 5% (21 participants) of samples other than selected kebeles in Dessie and some amendments were made based on the pretest findings. Two days training were provided for data collectors and supervisors regarding the sensitivity and personal nature of the questions, objective, and how to approach study participants with ensuring their privacy. Personal protective equipment such as examination gloves, facemasks and alcohol-based sanitizers were provided for the data collectors and supervisor. Then, data was collected using trained female health extension workers by ensuring the privacy of the study participants.
Data Management and Analysis
The data was checked for completeness, coded, recoded, and entered into Epi data version 3.1 software and exported to Stata version 14.2 for analysis. The descriptive analysis was done and the results were presented using texts, frequency tables, figures and median with interquartile range.
A bivariate logistic regression analysis was done to assess the association between the dependent variable with each independent variable. The sociodemographic factors (women age, age at first marriage, women education, women occupation), women substance use, husband substance use in the last three months, polygamy, female autonomy, and living in the community which is tolerant to violence against women were the independent variables included in the bivariate analysis. Thus, independent variables with p-value less than .25 were considered in the final model. Correlation between independent variables was assessed but we did not find any correlation between independent variables. The model fitness was also checked using Hosmer-Lemeshow model fit-ness test. Finally, multivariable logistic regression analysis was done to control potential confounders and to identify the factors associated with IPV amongst women. A statistical significance level was declared at a p-value of less than 0.05.
Operational Definitions
Partner. A person who has relationship with the women either in the form of marriage or cohabitation in the last three months.
Substance use. The women or her husband use either alcohol, chat, cigarette in the last three months.
Female autonomy. Includes the autonomy of the women to decide on family planning choices and usage, financial control, and equally lead the household with her partner.
Results
Sociodemographic Characteristics of Participants
In this study, a total of 589 married women were involved with a response rate of 95.5%. The median age of the participants was 32 (with Inter Quartile Range of 13) years. In this study, 132 (22.4%) of the women were married before the age of 18 years, 126 (21.4%) of participants were illiterate, 333 (56.5%) of the women were housewife, and 471(80%) of the women had less than five family sizes (Table 1).
Table 1.
Sociodemographic Characteristic of Women, Dessie Town, Northeast Ethiopia, July, 2020.
| Lis of Variable | Variable Category | Frequency (n = 589) | Percentage (%) |
| Age | 16–25 | 109 | 18.5 |
| 26–35 | 281 | 47.7 | |
| > 35 | 199 | 33.8 | |
| Family size | ≤ 5 | 471 | 80.0 |
| > 5 | 118 | 20.0 | |
| Age at the first marriage | < 18 | 132 | 22.4 |
| ≥ 18 | 457 | 77.6 | |
| Religion | Orthodox | 304 | 51.6 |
| Muslim | 269 | 45.7 | |
| Others+ | 16 | 2.7 | |
| Women education | Illiterate | 126 | 21.4 |
| Primary | 121 | 20.5 | |
| Secondary and above | 342 | 58.1 | |
| Partners educational status | Illiterate | 98 | 16.7 |
| Primary | 99 | 16.8 | |
| Secondary | 164 | 27.8 | |
| Tertiary | 228 | 38.7 | |
| Women’s occupation | House wife | 333 | 56.5 |
| Merchant | 97 | 16.5 | |
| Employee | 119 | 20.2 | |
| Others++ | 40 | 6.8 | |
| Partner occupation | Merchant | 202 | 34.3 |
| Government employee | 205 | 34.8 | |
| Self-employee | 116 | 19.7 | |
| Others* | 66 | 11.2 | |
| Income | ≤1000 | 69 | 11.7 |
| 1001–2000 | 110 | 18.7 | |
| 2001–3000 | 76 | 12.9 | |
| 3001–4000 | 59 | 10.0 | |
| > 4000 | 275 | 46.7 |
Note. Others+ (Protestant, Catholic), Others++ (daily laborer, student, NGO-employee, self-employee), Others* (daily laborer, driver, NGO-employee, student, self-employee, Carpenter).
Lifestyle and Behavioral Characteristics of Participants
In this study, 103 (17.5%) of the women reported that polygamy is common practice for men in their community and only 70 (11.9%) of women were autonomous upon their decisions regarding their issues. Regarding substance use, one-fourth (25.3%) of women had used substances (alcohol, cigarette, and chat) in the last three months and one-third of their partner (32.6%) had used any form of substances in the last three months (Table 2).
Table 2.
Lifestyle and Behavioral Characteristics of Women and Husbands in Dessie Town, Northeast Ethiopia.
| Variable | Category | Frequency (n = 589) | Percentage (%) |
| Women use substances (alcohol, chat, cigarette) in life time | No | 432 | 73.3 |
| Yes | 157 | 26.7 | |
| Women use substances (alcohol, chat, cigarette) in the last 3 months (n = 157) | No | 8 | 1.4 |
| Yes | 149 | 25.3 | |
| Frequency of women’s substance use | Daily | 6 | 1.0 |
| One or more a week | 23 | 3.9 | |
| One or more in 2 weeks | 19 | 3.2 | |
| Sometimes | 101 | 17.1 | |
| Partner use substances (alcohol, chat, cigarette) in the last 3 months | No | 397 | 67.4 |
| Yes | 192 | 32.6 | |
| Frequency of partners substances use (n = 192) | Daily | 46 | 7.8 |
| One or more a week | 21 | 3.6 | |
| One or more in 2 weeks | 13 | 2.2 | |
| Sometimes | 112 | 19.0 | |
| Community tolerant attitude to women violence | No | 564 | 95.8 |
| Yes | 25 | 4.2 | |
| Polygamy allowed for men | No | 486 | 82.5 |
| Yes | 103 | 17.5 | |
| Female Autonomy | No | 519 | 88.1 |
| Yes | 70 | 11.9 |
Intimate Partner Violence Against Women
In this study, the overall prevalence of at least one form of IPV (i.e., either physical, sexual or psychological) among married women was 22.4% [95% CI: 19.1%, 25.9%]. Besides, 11%, 20%, and 13.8% of the women had experienced physical, psychological, and sexual IPVs respectively. The study also revealed that 7.3% of the women had experienced all forms of IPVs (physical, psychological, and sexual IPVs) (Figure 1).
Figure 1.
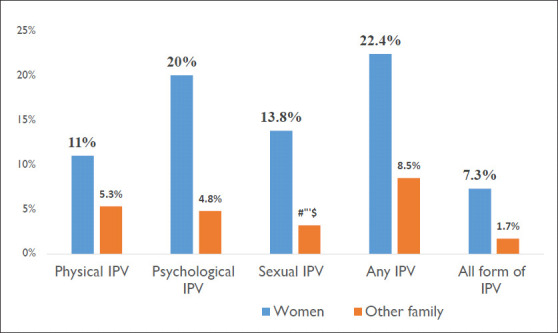
Types of IPV the women and other family members experienced in Dessie town, northeast Ethiopia.
Factors Associated with IPV Against Women During COVID-19 Pandemic Restrictions
The selected covariates include age of women, age at marriage, women education level, women occupation, family size, husband and women substance usage, women autonomy, polygamy practice, and women living in a community that support violence against women.
In this study, the odds of IPV among illiterate women was twice as great compared to women who had attended secondary and above education levels (AOR [Adjusted Odds Ratio] = 2.37: 95% CI 1.29, 4.35). Similarly, women who had illiterate husbands were three times higher odds of IPV compared to their counterparts (AOR = 2.67: 95% CI 1.36, 5.21). This study revealed that women’s husband who were substance users (alcohol, chat, or cigarette) had three times higher risk of IPV compared to those women who had nonuser husbands (AOR = 2.75: 95% CI 1.42, 5.34). The odds of IPV among women in a community tolerant to violence was three-folds higher compared to their counterparts (AOR = 2.97: 95% CI 1.17, 7.61). However, current age of women, age at marriage, women occupation, family size, women substance usage, polygamy practice, and women autonomy were not significantly associated with the IPV (Table 3).
Table 3.
Factors Associated With IPV During COVID-19 Restrictions in Dessie Town, Ethiopia.
| List of predictors | Variable Category | At Least One Form of IPV | COR (95%CI) | AOR (95%CI) | |
| Yes # (%) | No # (%) | ||||
| Women’s age | 16–25 | 25(22.9) | 84(77.1) | 1.00 | 1.00 |
| 26–35 | 60(21.4) | 221(78.6) | 0.91 (0.54, 1.54) | 0.812 (0.45, 1.47) | |
| >35 | 47(23.6) | 152(76.4) | 1.04 (0.59, 1.81) | 0.65 (0.34, 1.24) | |
| Women education | Illiterate | 44 (33.3) | 82 (17.9) | 2.81 (1.75, 4.46) | 2.37 (1.29, 4.35)* |
| Primary | 33 (25.0) | 88 (19.3) | 1.95 (1.19, 3.20) | 1.64 (0.93, 2.91) | |
| Secondary+ | 55 (41.7) | 287 (62.8) | 1.00 | 1.00 | |
| Partner education level | Illiterate | 39 (29.5) | 59 (12.9) | 3.52 (2.05, 6.04) | 2.67 (1.36, 5.21)* |
| Primary | 24 (18.2) | 75 (16.4) | 1.71 (0.95, 3.05) | 1.17 (0.59, 2.33) | |
| Secondary | 33 (25.0) | 131 (28.7) | 1.34 (0.79, 2.26) | 0.92 (0.51, 1.67) | |
| Tertiary | 36 (27.3) | 192 (42.0) | 1.00 | 1.00 | |
| Women occupation | Housewife | 77 (58.3) | 256 (56.0) | 1.00 | 1.00 |
| Merchant | 27(20.5) | 70 (15.3) | 1.28 (0.76, 2.14) | 1.23 (0.69, 2.19) | |
| Employee | 21(15.9) | 98(21.4) | 0.71 (0.42, 1.22) | 1.04 (0.54, 1.99) | |
| Others+ | 7(5.3) | 33(7.3) | 0.70 (0.30, 1.65) | 0.61 (0.24, 1.52) | |
| Women used substance in the last three months | Yes | 61 (46.2) | 96 (21.0) | 3.23 (2.14, 4.86) | 1.60 (0.82, 3.13) |
| No | 71 (54.8) | 361(79.0) | 1.00 | 1.00 | |
| Husband used substances in the last three months | Yes | 71 (53.8) | 121 (26.5%) | 3.23 (2.16, 4.82) | 2.75 (1.42, 5.34)* |
| No | 61 (46.2) | 336 (73.5) | 1.00 | 1.00 | |
| Polygamy practice in the community | Yes | 32 (24.2) | 71 (15.5) | 1.74 (1.08, 2.78) | 1.27 (0.74, 2.18) |
| No | 100 (75.8) | 386 (84.5) | 1.00 | 1.00 | |
| community tolerant attitude to violence against women | Yes | 12 (9.1) | 13 (2.8) | 3.41 (1.52, 7.68) | 2.97 (1.17, 7.61)* |
| No | 120 (90.2) | 444 (97.2) | 1.00 | 1.00 | |
| Women age at first marriage | <18 | 38 (28.8) | 94 (20.6) | 1.00 | 1.00 |
| >=18 | 94 (72.2) | 363 (79.4) | 0.64 (0.41, 0.99) | 0.84 (0.51, 1.41) | |
| Women autonomy on decision making | Yes | 19 (14.4) | 51(11.2) | 1.34 (0.75, 2.36) | 1.19 (0.63, 2.26) |
| No | 113 (85.6) | 406 (78.8) | 1.00 | 1.00 | |
Note. *p < 0.05. Others+ (daily laborer, student, NGO-employee, self-employee), AOR = adjusted odds ratio; COR = crude odds ratio; CI = confidence interval.
Discussions
This study indicated that the prevalence of any IPV amongst married or cohabitated women was comparable to the national prevalence of domestic violence that was conducted prior to the pandemic. The multivariable logistic regression analysis showed that the woman and husband’s education level, husband substance use, and community tolerant attitude toward women violence were the independent predictors of IPV amongst women.
In this study, the overall prevalence of any IPV among women was 22.4% which is higher than a studies conducted in Nigeria (15.2%; Oyediran & Feyisetan, 2017), and South Africa (15%; Sania et al., 2017). The discrepancy might be explained by the differences in the measurement and classification of any IPV. For instance, some of the researchers combined together physical and emotional IPV but the current study combined the three domains of IPV together. Besides, the sociocultural differences (Alsaleh, 2022) and discrepancy in the strength of legal frames implemented to control violence against women at national and district levels may account for the differences.
However, this study has a prevalence lower than the studies conducted in United States (25%) Boserup et al., 2020), EDHS report (34%; Central Statistical Agency - CSA/Ethiopia & ICF, 2017), north western Ethiopia (78%; Semahegn et al., 2013), a review of 36 studies in Ethiopia (37%; Kassa & Abajobir, 2020), Kuwait (71%; Alsaleh, 2022), and Turkey (57.2%); Neslihan Keser Özcan* et al., 2016). This could be justified by the differences in the time frame of the studies, the measurement and classification of any IPV. For example, in our study a woman was asked about their experience of any IPV during the pandemic in Ethiopia, which is a short period compared some of the previous studies those reported experience of IPV at any time or 12 months ago. In addition, the previous studies included the women who sought medical care while this study was community-based only. Subsequently, this may underestimate the prevalence of IPV in our study.
Furthermore, the odds of IPV among illiterate women was twice greater compared to women who had attended secondary and above educations in this study. Similarly, women who had illiterate husbands were three times higher to be violated by their partners compared to their counterparts. These findings are similar to studies conducted in south west Nigeria (Ajala., 2017b), Ethiopia (Abeya et al., 2011; Alebel et al., 2018), Eastern Sudan (AbdelAziem et al., 2014), and Zambia (Sthephen Lawoko, 2006). This could be justified by the fact that illiterate women may not have the knowledge towards the legal legislatives to protect their right, available health services, and refusal to harmful societal norms. Additionally, the illiterate husbands may not be considered violent against women because of their poor knowledge regarding the legal rights of their wife/partners. Therefore, the illiterate women and husbands are more likely to be violated by their intimate partners compared to the literate women.
This study revealed that women who had a substance user (alcohol, chat, or cigarette) husband were three times greater to be violated compared to those women who had not substance user husbands. This finding is similar with the studies conducted in Awi Zone and western Ethiopia (Abeya et al., 2011; Semahegn et al., 2013), Uganda (Black et al., 2019), Nigeria (Ajala., 2017a), South Africa (Sania et al., 2017), Philippine, Eastern Saudi (N Pearce & Afifi., 2011), and Eastern Sudan (AbdelAziem et al., 2014). This could be justified by use of substances such as alcohol drinking, smoking or khat chewing can affect the thinking and cognitive potential of the users. Therefore, women living with substance user husbands/partners are more likely to be violated compared to those living with non-user husbands.
Finally, in this study, women who live in the community tolerant to violence had three-folds greater odds of IPV compared to their counterparts. This finding is in line with a study done in Kuwait (Alsaleh, 2022). In Ethiopia, there are sociocultural and religious barriers which inhibit women’s autonomy. For instance, only one in five (19.9%) women had reported their violence to the legal authorities (Deribe et al., 2012). The women’s reasons for failing to report to the legal system were related to not knowing where to go, the need to obey community norms and values, and not wanting to expose their personal issue.
Limitation of the study. First, this study was limited to married or cohabitated women. Thus, the findings may not represent unmarried women in the region. Second, the prevalence of IPV might be underestimated because of the personal nature of the problem and under-reported. Finally, the study was not supplemented with qualitative methods since the FGD or other qualitative methods increase risk of COVID infection during data collection.
Conclusions
The study revealed that the prevalence of IPV among married women during COVID-19 restrictions was high. Hence, based on this prevalence, we can infer to the target population (all married/cohabitated women) in the region. The multivariable logistic regression analysis showed that a woman’s education level, husband’s education level, husband substance use, and community tolerant to violence were the independent predictors of IPV amongst women. Therefore, national and regional governments should work toward enhancing gender equality, coupled with addressing risk factors at multiple levels, using community- and institution-based approaches to prevent IPV and to specifically achieve Sustainable Development Goal 5 of eliminating violence against women beyond COVID-19 pandemic by 2030. Furthermore, the accessibility of education for women should be strengthened at local and national levels. Moreover, qualitative studies are recommended to explore the socio-cultural practices that support women violence in the community.
Acknowledgements
We would like to thank Dream science and Technology College for its ethical approval. Furthermore, our deepest gratitude goes to the participants, data collectors and supervisors.
Authors Biographies
Abay Woday Tadesse, MPH, is public health epidemiologist. Currently, he is teaching at Samara University in Afar region, east Ethiopia. His research works are focusing to answer the public health and human rights issues on gender based violence in Eastern African countries including Ethiopia. He designed and conducted different research projects as a leader and co-leader in maternal, adolescent and child health in Ethiopia. Thus, he emphasizes improving community and government systems through collaborative and multidisciplinary efforts.
Setegn Mihret Tarekegn has MSc in Pediatrics. Currently, he is lecturer at Wollo University, School of Nursing and Midwifery in Ethiopia. His research focuses on Infectious Diseases, and Child Health. He is interested in translating research evidences into health care practices at policy-levels.
Gebeyaw Biset Wagaw has MSc in Pediatrics and currently he is lecturer at Wollo University, School of Nursing and Midwifery in Ethiopia. His research focuses on Child Health. He is interested in translating research evidences into health care practices at national-levels.
Muluken Dessalegn Muluneh is an epidemiologist. Currently, leading research, monitoring, evaluation at Amref Health Africa in Ethiopia. He is also a PhD candidate at Western Sydney University in Australia. His research focuses on answering the public health and human rights issues focusing on gender based violence in Sub Saharan African countries. He led and co-lead various projects in maternal, adolescent and child health at Amref Health Africa in Ethiopia. He designed and conducted various research and evaluations projects at various levels in the country.
Ayesheshim Muluneh Kassa has MSc in Project Planning and Management, Currently, he is lecturer at Dessie Health Science College in Ethiopia. His research focuses on Child Health. He is interested in translating research outputs into practice which helps the decisions in the health care systems.
Footnotes
Availability of Data and Materials: All materials and data related to this article are included in the main document of the manuscript. However, if anyone has any interest to have raw data, he/she can contact the corresponding author.
Ethical Issues and Consent to Participate: Ethical approval was obtained from Dream Science and Technology Institutional Health Research Ethics Review Committee with approval letter of DSTC/DHS/002/2020. Then, permission letter was written for Dessie city administration office. We had obtained verbal consent from individual study participants before beginning of data collection. The women who were victims of IPV at the time of data collection were reassured and counseled. However, women who experienced severe IPV and were in need of help were taken to Dessie referral hospital counseling care units. We avoided personal identifier to ensure confidentiality and anonymity of study participants.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
ORCID iDs: Abay Woday Tadesse  https://orcid.org/0000-0003-0499-4690
https://orcid.org/0000-0003-0499-4690
Muluken Dessalegn Muluneh  https://orcid.org/0000-0002-9105-6629
https://orcid.org/0000-0002-9105-6629
References
- AbdelAziem A. A., Yassin K., & Omer R. (2014). Domestic violence against women in Eastern Sudan. BMC Public Health, 14(1136). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4391281/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abeya S. G., Afework M. F., & Yalew A. W. (2011). Intimate partner violence against women in western Ethiopia: Prevalence, patterns, and associated factors. BMC Public Health, 11, 913. 10.1186/1471-2458-11-913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajala A. O. (2017. a). Correlates of sexual violence among married couples in Nigeria. Research on Humanities and Social Sciences, 7(24). https://www.iiste.org/Journals/index.php/RHSS/article/view/40139 [Google Scholar]
- Ajala A. O. (2017. b). Sexual violence against women in marital dyads, prevalence, correlates, and consequences: Among the Ijesa of SouthWestern Nigeria. Archives of Business Research, 5(12), 63–77. 10.14738/abr.512.3902 [DOI] [Google Scholar]
- Alebel A., Kibret G. D., Wagnew F., Tesema C., Ferede A., Petrucka P., Bobo F. T., Birhanu M. Y., Tadesse A. A., & Eshetie S. (2018). Intimate partner violence and associated factors among pregnant women in Ethiopia: A systematic review and meta-analysis. Reproductive Health, 15(1), 196. 10.1186/s12978-018-0637-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alsaleh A. (2022). Violence against Kuwaiti women. Journal of Interpersonal Violence, 3(5–6), NP3628–NP3649. 10.1177/0886260520916280 [DOI] [PubMed] [Google Scholar]
- Black E., Worth H., Clarke S., Obol J. H., Akera P., Awor A., Shabiti M. S., Fry H., & Richmond R. (2019). Prevalence and correlates of intimate partner violence against women in conflict affected northern Uganda: A cross-sectional study. Conflict and Health, 13, 35. 10.1186/s13031-019-0219-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boserup B., McKenney M., & Elkbuli A. (2020). Alarming trends in US domestic violence during the COVID-19 pandemic. The American Journal of Emergency Medicine, 38(12), 2753–2755. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7195322/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell A. M. (2020). An increasing risk of family violence during the Covid-19 pandemic: Strengthening community collaborations to save lives. Forensic Science International: Reports, 100089. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7152912/ [DOI] [PMC free article] [PubMed]
- Central Statistical Agency (CSA) Ethiopia & ICF. (2017). Ethiopia demographic and health survey 2016. Author. https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf
- Davis M., Gilbar O., & Padilla-Medina D. (2020). Intimate partner violence victimization and perpetration among US adults during COVID-19: A brief report. https://www.medrxiv.org/content/10.1101/2020.06.08.20125914v1 [DOI] [PubMed]
- Deribe K., Beyene B. K., Tolla A., Memiah P., Biadgilign S., & Amberbir A. (2012). Magnitude and correlates of intimate partner violence against women and its outcome in Southwest Ethiopia. PLoS ONE, 7(4), Article 36189. 10.1371/journal.pone.0036189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong Y., Mo X., Hu Y., Qi X., Jiang F., Jiang Z., & Tong S. (2020). Epidemiology of COVID-19 among children in China. Pediatrics, 145(6), Article e20200702. 10.1542/peds.2020-0702 [DOI] [PubMed] [Google Scholar]
- Duncan T. K., Weaver J. L., Zakrison T. L., Joseph B., Campbell B. T., Christmas A. B., Stewart R. M., Kuhls D. A., & Bulger E. M. (2020). Domestic violence and safe storage of firearms in the CoVID-19 era. Annals of Surgery, 272(2), e55–e57. 10.1097/SLA.0000000000004088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal Minstry of Health (FMOH). (2020. a). COVID-19 Handbook for health professionals Federal Ministry of Health, Ethiopia. https://www.moh.gov.et
- FMOH. (2020a). COVID-19 Handbook for health professionals Federal Ministry of Health, Ethiopia, Availabile: https://www.moh.gov.et
- FMOH. (2020b). Infection prevention and control interim protocol for covid-19 in health care settings in Ethiopia. Author. http://www.moh.gov.et/ejcc/am/Infection%20Prevention%20and%20Control%20Interim%20Protocol%20for%20COVID-19%20In%20Health%20Care%20Settings%20in%20Ethiopia
- Hatchimonji J. S., Swendiman R. A., Seamon M. J., & Nance M. L. (2020). Trauma does not quarantine: Violence during the COVID-19 pandemic. Annals of Surgery, 272(2), e53–e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarnecke A. M., & Flanagan J. C. (2020). Staying safe during COVID-19: How a pandemic can escalate risk for intimate partner violence and what can be done to provide individuals with resources and support. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jemal B., Ferede Z. A., Mola S., Hailu S., Abiy S., Wolde G. D., Tilahun A., Tesfaye B., Lemma D. T., Alimaw A. A., Neme D., Regasa T., Mulugeta H., Moges K., & Bedru M. (2020). Knowledge, attitude and practice of healthcare workers towards COVID-19 and its prevention in Ethiopia: A multicenter study. https://assets.researchsquare.com/files/rs-29437/v1/2802c94a-b237-458f-ac48-aee72c4ae793.pdf [DOI] [PMC free article] [PubMed]
- John N., Casey S. E., Carino G., & McGovern T. (2020). Lessons never learned: Crisis and gender-based violence. Developing World Bioethics, 20(2), 65–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassa G. M., & Abajobir A. A. (2020). Prevalence of violence against women in Ethiopia: A meta-analysis. Trauma, Violence, & Abuse, 21(3), 624–637. 10.1177/1524838018782205 [DOI] [PubMed] [Google Scholar]
- Lee J. (2020). Mental health effects of school closures during COVID-19. The Lancet Child & Adolescent Health, 4(6), 421. 10.1016/S2352-4642(20)30109-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazza M., Marano G., Lai C., Janiri L., & Sani G. (2020). Danger in danger: Interpersonal violence during COVID-19 quarantine. Psychiatry Research, 289, 113046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreira D. N., Costa Da, & M. P. (2020). The impact of the Covid-19 pandemic in the precipitation of intimate partner violence. International Journal of Law and Psychiatry, 71, 101606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Özcan* Neslihan Keser, Günaydin SevilÇitil E. T. (2016). Domestic violence against women in Turkey: A systematic review and meta analysis. Archives of Psychiatric Nursing, 30(5), 620–629. [DOI] [PubMed] [Google Scholar]
- Oyediran K. A., & Feyisetan B. (2017). Prevalence and contexual determinants of intimate partner violence in Nigeria. African Population Studies, 31(1). https://aps.journals.ac.za/pub/article/view/1003 [Google Scholar]
- Pearce N., & Afifi. Z. (2011). Determinants of domestic violence against women in an Eastern Saudi Community. Journal of Epidemiology & Community Health, 65(1). 10.1136/jech.2011.142976b.18 [DOI] [Google Scholar]
- Roesch E., Amin A., Gupta J., & García-Moreno C. (2020). Violence against women during covid-19 pandemic restrictions. https://www.bmj.com/content/369/bmj.m1712 [DOI] [PMC free article] [PubMed]
- Sania A., Brittain K., Phillips T. K., Zerbe A., Ronan A., Myer L., & Abrams E. J. (2017). Effect of alcohol consumption and psychosocial stressors on preterm and small-for-gestational-age births in HIV-infected women in South Africa: A cohort study. BMJ, 7(3), 8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5372146/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semahegn A., Torpey K., Manu A., Assefa N., & Ankomah A. (2019). Adapted tool for the assessment of domestic violence against women in a low-income country setting: A reliability analysis. International Journal of Women’s Health, 11, 65–73. 10.2147/IJWH.S181385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semahegn A., Belachew T., & & Abdulahi M. (2013). Domestic violence and its predictors among married women in reproductive age in Fagitalekoma Woreda, Awi zone, Amhara regional state, North Western Ethiopia. Reproductive Health, 10(63). https://reproductive-health-journal.biomedcentral.com/articles/10.1186/1742-4755-10-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sthephen L. P. (2006). Factors associated with attitudes towards intimate partner violence: A study of women in Zambia. Violence and Victims, 21(5), 645–656. [PubMed] [Google Scholar]
- Taub A. (2020). A new Covid-19 crisis: Domestic abuse rises worldwide. The New York Times, 6. [Google Scholar]
- Van Gelder N., Peterman A., Potts A., O'Donnell M., Thompson K., Shah N., & Oertelt-Prigione S. (2020). COVID-19: Reducing the risk of infection might increase the risk of intimate partner violence. EClinicalMedicine, 21. https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(20)30092-4/fulltext [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (WHO). (2005). WHO multi-country study on women’s health and domestic violence against women. Author. https://www.who.int/reproductivehealth/publications/violence/24159358X/en/
- WHO. (2012). Global and regional estimates of violence against women: Prevalence and health effects of intimate partner violence and non-partner sexual violence. Author.
- WHO. (2020. a). Coronavirus disease (COVID-19) situation report – 131. Author. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200530-covid-19-sitrep-131.pdf?sfvrsn=d31ba4b3_2
- WHO. (2020. b). COVID-19 and violence against women what the health sector/system can do. Author. https://www.who.int/reproductivehealth/publications/emergencies/COVID-19-VAW-full-text.pdf
- Wu D., Wu T., Liu Q., & Yang Z. (2020). The SARS-CoV-2 outbreak: what we know. International Journal of Infectious Diseases, 94, 44–48. 10.1016/j.ijid.2020.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]


