Abstract
The aim of this study was to assess the impact of the COVID-19 pandemic on mental well-being of clinically referred children and adolescents and on their families from the perspective of mental health care professionals in Switzerland during the first year of the pandemic. Psychiatrists and psychologists for children and adolescents participated in an anonymous survey conducted online in April/May 2021. The survey was completed by 454 mental health care professionals, most of them working in outpatient clinics for child and adolescent psychiatry or in independent practices. Most participants indicated an important increase of referrals for depression (86.8% of respondents), anxiety disorders (81.5%), crisis interventions (76.2%), psychosomatic disorders (66.1%), suicidality (63.8%), and behavioral addictions, e.g., excessive gaming (64.6%). In contrast, referrals or treatment demands for disorders such as autism spectrum disorder or psychosis showed no substantial change or a slight decrease, respectively. According to 69% of respondents, patients experienced the highest psychological burden in January/February/March 2021. Family problems very frequently reported by mental health professionals were parents’ worries about loneliness/isolation of the child (49%), child’s education and academic future (33%), increased media use due to missing options of recreational activities (37.6%), as well as multiple stresses of mothers (36.3%). To conclude, the pandemic has substantially changed the pattern of disorders and the number of clinical referrals of children and adolescents with mental health problems, which has serious consequences for the treatment supply in Switzerland.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00702-022-02512-6.
Keywords: COVID-19, Children, Adolescents, Mental disorders, Clinical referral, Psychiatry
Introduction
Children and adolescents from all over the world have suffered from pandemic control measures and their consequences, such as school closures, social distancing, curfews, lack of leisure or group activities, limited possibilities for physical exercise, enhanced family conflicts due to home confinement, or financial insecurities. Population studies worldwide have shown that the pandemic had already dramatic effects on children’s and adolescents’ mental health, with increased depressive and anxious symptoms and increased suicidal ideation (reviews by Deolmi and Pisani 2020; Samji et al. 2021; Singh et al. 2020) and self-harm (Zetterqvist et al. 2021), psychosomatic complaints, worsened quality of life (Ravens-Sieberer et al. 2021), post-traumatic stress disorder (Marques de Miranda et al. 2020; Selçuk et al. 2021), eating disorders and weight gain (Juli et al. 2021; Woolford et al. 2021), as well as attentional problems (Mohler-Kuo et al. 2021), loneliness or isolation (Al Omari et al. 2021; Cost et al. 2021). Parents also experienced heightened stressors and burdens during the COVID-19 situation (Clemens et al. 2021; El-Osta et al. 2021; Huebener et al. 2021), and some of them were at risk to experience distress or to suffer from own mental problems (Tseng et al. 2021). Mothers, and single mothers in particular, were confronted with new challenges, and had to manage work at home, supervision of homeschooling as well as household chores. They were thus at risk for overload, exhaustion and depression (Calvano et al. 2021; McLaren et al. 2020; Taylor et al. 2021). Spending more time in confined spaces also resulted in more frequent family conflicts and sometimes led to physical and sexual abuse or maltreatment (Rodriguez et al. 2021; Sinko et al. 2021).
An increased need for treatment of mental health related problems or disorders in children and adolescents since the pandemic has been reported by several studies. In a survey among university hospitals of child and adolescent psychiatry from 22 European countries, a majority of respondents indicated an increase of cases with suicidal crises (more than 80%), depression (more than over 60%), anxiety (more than 70%), eating disorders (more than 60%) in February/March 2021, while in summer 2020, only a minority had reported an increased demand for treatment (Revet et al. 2021). Mental health related visits to emergency departments have also considerably increased during the pandemic in children and adolescents according to reports from several countries, such as Switzerland (Berger et al. 2022), Canada (Chadi et al. 2021), Italy (Vicari and Pontillo 2021) and United States (Leeb et al. 2020). According to a systematic review on the impact of the pandemic on child and adolescent mental health based on 61 articles (Panchal et al. 2021), anxiety symptoms and depression were among the most frequently reported symptoms, followed by irritability and anger. Adolescent age, female sex, lack of daily routine and excessive exposure to pandemic-related information and media or COVID-19 health-related stress were revealed as risk factors for increased mental problems (e.g.,Bhatia 2020; Kazi and Mushtaq 2021; Mohler-Kuo et al. 2021; Qin et al. 2021; Wang et al. 2022; Wirkner et al. 2022). However, for patients with pre-existent mental health disorders, results were mixed: several studies, especially when conducted at the beginning of the pandemic and during the lockdown, reported a certain relief of stress and decreased symptoms in a minority of patients with social anxiety, school anxiety, learning disorders and ADHD (Bobo et al. 2020; Cost et al. 2021; Melegari et al. 2021). For ADHD, a relief of symptoms, especially during the lockdown, has been reported in 25–30% of cases (Lavenne-Collot et al. 2021; Werling et al. 2021a), but on the other hand, an exacerbation of pre-existing symptoms during COVID-19 school closures has been described for children with ADHD, who also seemed stronger affected by COVID-19 related stress than neurotypically developed peers (Giallonardo et al. 2021). In adolescents with pre-existing mental disorders, the recommendation to adhere to strict hygiene measures and social distancing seem to have triggered or intensified obsessive–compulsive symptoms (Khan et al. 2022). According to a recent German study comparing a clinical and a community sample of children and adolescents, approximately 60–70% of children, adolescents and parents indicate an increase in mental burden, in contrast to 12% indicating a relief (Döpfner et al. 2021). The question has been raised whether the high increase of cases with mental problems are truly caused by the pandemic itself or are only triggered by the coronavirus crisis, induced by a situation of permanent stress and uncertainty, in individuals with a pre-existent vulnerability and poor resilience. Few studies have tried to distinguish between mental symptoms caused by the pandemic, pre-existent symptoms exacerbated by the pandemic, and those unrelated to the pandemic. For a group of adult psychiatric patients, Rohde and colleagues proposed an approach for the classifications of patients according to mental illnesses related or unrelated to the effects of the pandemic based on patient records (Enevoldsen et al. 2022; Jefsen et al. 2021; Rohde et al. 2020). Among the symptoms related to the effects of COVID-19, they identified anxiety symptoms, OCD-symptoms, and, in a smaller number of patients, autism- and ADHD-related symptoms, self-harm and unspecific stress. Several studies have shown an important increase of digital media use in children and adolescents, such as gaming, surfing in the internet or communicating on social media (Kawabe et al. 2020; Masaeli and Farhadi 2021), especially in the lockdown phase of the pandemic (Werling et al. 2021a, b). In adolescents with pre-existing mental health problems, very high media use has been linked to depression or worsening of psychopathology. On the other hand, digital media use had also protective effects during the pandemic, as it was often the only means to socialize with friends.
The aim of the present study was to assess the impact of the COVID-19 pandemic on the mental health of clinically referred children and adolescents and on the situation of their families during the first year of pandemic from the perspective of mental health professionals for children and adolescents. Here, we focus on the mental health-related consequences of the pandemic for patients and their families, while consequences for treatment supply and the situation of mental health professionals have been presented elsewhere (Werling et al. 2022b). In the present study we investigated whether mental health professionals had observed:
– Disorder-specific changes in the frequency of referrals during the pandemic,
– Mental disorders apparently caused or triggered by the pandemic, including observed changes in patients’ digital media-related behavior during the pandemic,
– Mental health problems that seemed specific for the pandemic or had not been encountered before in this form or intensity,
– Subgroups of patients who had been particularly affected by the pandemic,
– Peaks in the severity of psychological burden experienced in the course of the first year of the pandemic.
– Finally, we assessed how frequently mental health professionals had been confronted with pandemic-related complaints and difficulties reported by parents.
Method and procedure
An anonymous online survey was conducted from April 22nd to May 24th, 2021 among psychiatrists and psychologists specialized in the treatment of children and adolescents. They were contacted via email addresses, which were extracted from public directories of professional societies in Switzerland. The invitation email explained the background and goals and contained the link to the survey. Two weeks later, a reminder was sent out. A small group of health professionals with no published email address was contacted by letter, which included a QR code leading to the online survey. This survey for mental health professionals was developed as a complement and follow-up to surveys for patients and their parents on the impact of the pandemic conducted by the authors (Werling et al. 2021a, b; Werling et al. 2022a, b). The online survey was available in German and French, which are the two most frequently spoken languages in Switzerland (main languages for approximately 85% of inhabitants). With few exceptions, where multiple choices were possible, participants had to select a single answer from several options. If they were unwilling or unable to answer the question (e.g., because not applicable to their work context), they could skip the question or specify the answer as a free text comment. The free text comments were analyzed and classified according to content analytical principles.
Pandemic protection measures in Switzerland
Besides a lockdown period over approximately 8 weeks in spring 2020, COVID-19 protection measures were less restrictive in Switzerland compared to many other European countries. Only during this lockdown period, schools were closed or offered online teaching. The first schools already started on-site teaching in May 2020. Primary schools and many secondary schools remained open during a second serious wave of infections with a peak in autumn 2020. Restriction measures varied in intensity from school to school and changed during the study period. Most recreational activities for children and adolescents, including contact sports or other group activities, were not allowed throughout 2020. Vaccinations for the population started in late December 2020.
Results
Participants
A total of 454 mental health care professionals participated in the anonymous survey. Approximately 1800 invitations were sent out, which corresponds to a response rate of 24%. Among the participants, 38.5% were psychiatrists and 54.4% psychologists specialized in the treatment of children and adolescents, 3.9% indicated other professions (e.g., other therapist, pediatrician) (Table 1). Most of them were from the German speaking part of Switzerland (83.2%), followed by the French speaking part (14.4%) and the Italian speaking part (0.4%) (the latter had responded to the French version of the survey) (Table 1). Based on the language distribution in Switzerland (main language in the population: German 62.1%, French 22.8%, Italian 8%), the French speaking part was slightly underrepresented. Most of the participants (54.4%) worked in independent practice and 29.8% in a clinic for child and adolescent psychiatry and psychotherapy, mainly in outpatient clinics or specialized units (Table 1). Only N = 20 participants indicated to work in inpatient facilities. The majority of professionals (65.0%) indicated to treat the entire age range of children and adolescents. Approximately 13.7% indicated to treat primarily adolescents (13 years and older) and 12.4% school-age children (7–18 years). Only a few therapists indicated to treat primarily children under 7 years of age (1.8%), younger school-age children (7–13 years) (1.3%), or families (3.6%).
Table 1.
Participants
| N | % | |
|---|---|---|
| Professional group | ||
| Child and adolescent psychiatrists | 175 | 38.5 |
| Child and adolescent psychologists | 247 | 54.4 |
| Other | 18 | 3.9 |
| Not stated | 14 | 3.1 |
| Work context | ||
| Independent practice (for child and adolescent psychiatry or psychology) | 247 | 54.4 |
| Clinic for child and adolescent psychiatry | 135 | 29.8 |
| Outpatient services/day clinic | 115 | |
| Inpatient clinic/ward | 20 | |
| Other/not stated | 72 | 15.8 |
| Total participants | 454 | 100 |
The pandemic’s impact on referral, frequency, severity and as trigger of mental disorders
Participants were asked to indicate whether the occurrence of certain disorders or causes for referral had disproportionally increased or decreased during the pandemic. Marked differences between problem areas emerged: depression (46.7%), anxiety disorders (42.2%), as well as emergencies and acute crises (37%) showed strong increases according to the answers of participants, while only a very small number of participants indicated an increased occurrence of disorders, such as psychosis (Table 2). Among the neurodevelopmental disorders, learning disabilities seemed to occur currently more often than before the pandemic (slight increase indicated by 36.3% and strong increase by 19.8%), followed by aggressiveness/behavioral disorders (slight increase 36.3%, strong increase 10.1%). Many participants reported in free text comments that school refusal and social withdrawal had increased (N = 29; Supplement Table S1). Others reported increased apathy/lack of perspective/hopelessness (N = 10) or increased psychological problems of parents (N = 10) (Supplement Table S1).
Table 2.
Changed distribution of reasons for referral during the pandemic (percent of responses)
| Strong decrease | Slight decrease | Unchanged | Slight increase | Strong increase | Not applicable/not stated | |
|---|---|---|---|---|---|---|
| Family conflicts | 0.2 | 0.2 | 20.7 | 46.7 | 23.8 | 8.4 |
| Physical assault, sexual abuse | 0.0 | 0.4 | 42.3 | 20.0 | 2.6 | 34.6 |
| Self-harm | 0.0 | 0.9 | 27.1 | 38.5 | 18.1 | 15.4 |
| Emergencies, crisis intervention | 0.2 | 0.2 | 10.4 | 39.2 | 37.0 | 13.0 |
| Suicidality | 0.0 | 0.9 | 20.7 | 39.4 | 24.4 | 14.5 |
| Depression | 0.2 | 0.0 | 9.0 | 40.1 | 46.7 | 4.0 |
| Anxiety disorders | 0.2 | 0.4 | 12.6 | 39.0 | 42.5 | 5.3 |
| Psychosomatic disorders | 0.2 | 0.4 | 24.2 | 41.0 | 25.1 | 9.0 |
| Adjustment disorders, trauma | 0.2 | 0.7 | 39.4 | 33.0 | 9.9 | 16.7 |
| ADHD | 0.2 | 2.4 | 63.0 | 17.0 | 4.2 | 13.2 |
| Aggressiveness, behavioral/conduct disorder | 0.0 | 2.2 | 36.3 | 36.3 | 10.1 | 15.0 |
| Autism spectrum disorders | 0.2 | 2.2 | 62.4 | 7.6 | 2.6 | 25.0 |
| Learning problems | 0.2 | 2.4 | 27.5 | 36.3 | 19.8 | 13.7 |
| OCD | 0.4 | 0.4 | 33.5 | 35.7 | 9.0 | 20.9 |
| Eating disorders | 0.2 | 0.2 | 32.2 | 29.7 | 11.9 | 25.8 |
| Behavioral addictions (e.g., gaming) | 0.2 | 0.0 | 17.0 | 38.8 | 25.8 | 18.3 |
| Substance-related addictions (e.g., alcohol) | 0.2 | 0.2 | 32.8 | 26.7 | 8.6 | 31.5 |
| Psychosis, schizophrenia | 0.0 | 0.0 | 46.3 | 8.6 | 1.1 | 44.1 |
| Borderline personality disorder | 0.0 | 0.0 | 43.8 | 16.7 | 2.6 | 36.8 |
| Personality disorders in general | 0.0 | 0.0 | 38.1 | 12.6 | 1.3 | 48.0 |
High percentage of “not-applicable”-responses may reflect a low incidence of a disorder or that many clinicians usually do not offer treatment for this group of patients
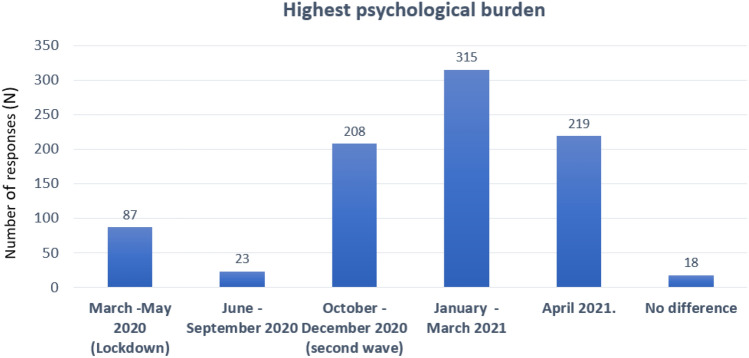
When asked in another question whether according to their experience the severity of disorders had increased during the coronavirus crisis, most participants agreed that disorders and mental problems seemed to be slightly (55.7%) or much more severe (16.5%) than before the pandemic (Supplement Table S2). Some participants argued that problems may have seemed more severe, because waiting times for admission to treatment in psychiatric institutions had considerably increased and patients with severe and acute problems had to recur to independent practices instead or because resources within families were diminished (Supplement Table S2; free text comments). When estimation of severity was analyzed according to the work settings, 86% of professionals working in a clinic for child and adolescent psychiatry and 74% of professionals working in independent practice estimated that the severity of disorders had increased (somewhat more severe/much more severe) since the pandemic (Fig. 1). The difference in the frequency of responses between both groups was borderline significant (Chi2 = 7.764, p = 0.051) with professionals from clinics indicating more often an increase in severity.
Fig. 1.
Changed severity of disorders as result of the pandemic as indicated by mental health professionals working in clinics or independent practices (frequency of responses in percent). Percentages refer to each professional group separately
In the next question, participants were asked to indicate, whether and which kind of disorders or mental problems had been caused/triggered by the pandemic in their opinion (Table 3). 67% percent of respondents indicated depression, followed by family conflicts (59.9%), psychosomatic disorders (39.9%), suicidality (37.7%), mutism/school refusal/social isolation (35.5%), addictive behaviors (23.8%), and eating disorders (19.2%) (Table 3). Among psychosomatic disorders, sleep disorders were mentioned most often (N = 154). Problematic gaming was the most frequently reported addictive behavior (N = 99), anorexia and bulimia (N = 70) were most frequently mentioned among eating disorders/problematic eating behaviors, and violence of a parent against the child (N = 49) was the most frequently indicated subcategory of domestic violence. Anxiety disorder (N = 17) and obsessive compulsive disorder (OCD) (N = 7) were additionally mentioned as triggered or caused by the pandemic in free text comments (Table S3). However, according to some other comments, the pandemic was also seen as catalyst rather than as cause of disorders, having a destabilizing effect on a previously effortful maintained balance (N = 11) (Supplement Table S3).
Table 3.
Disorders or mental problems triggered/caused by the pandemic
| N | % | |
|---|---|---|
| Depression | 305 | 67.2 |
| Family conflicts | 272 | 59.9 |
| Psychosomatic disordersa) | 181 | 39.9 |
| Sleep disorders | 154 | |
| Headache | 85 | |
| Other pain | 48 | |
| Suicidality | 162 | 37.7 |
| School refusal, social anxiety | 161 | 35.5 |
| Addiction, drug usea) | 108 | 23.8 |
| Alcohol | 46 | |
| Drugs (e. g. cannabis) | 66 | |
| Gaming (PUI) | 99 | |
| Eating disordersa) | 87 | 19.2 |
| Eating disorder in the strict sense (anorexia, bulimia) | 70 | |
| Uncontrolled food intake | 30 | |
| Severe weight gain | 30 | |
| Unfavorable eating habits (junk food) | 35 | |
| Loss of appetite | 22 | |
| Food refusal | 23 | |
| Domestic violence/abusea) | 63 | 13.9 |
| Violence of the patient against the parent(s) | 33 | |
| Violence of a parent against the child | 49 | |
| Violence between parents | 40 | |
| Sexual abuse | 7 | |
| No, the pandemic was usually not a trigger | 34 | 7.5 |
| Other | 67 | 14.7 |
| Not applicable/not stated | 32 | 7.1 |
a)If the category had been chosen, subcategories could be selected. Multiple answers were possible
Problematic internet and digital media use
Approximately 20% of participants reported to have been confronted before the pandemic quite or very often with problematic use of the internet (PUI)/problematic gaming in their clinical work. During the pandemic, this number increased up to 41.2% (Table 4). When asked about changes in the media use of their patients during the pandemic, 36% of respondent had observed changes in digital media behavior up to a borderline problematic/addictive use quite or very often, and 16% indicated to have observed an important increase of digital media use above a pathological threshold quite or very often (Supplement Table S4).
Table 4.
Frequency of “problematic internet use” (or “video game addiction” or “internet addiction”) as reason for referral or as suspected diagnosis before and since the pandemic
| Never | Seldom | Some-times | Quite often | Very often | Not applicable/not stated | |
|---|---|---|---|---|---|---|
| % | % | % | % | % | % | |
| Before the pandemic | 6.2 | 18.7 | 43.4 | 18.9 | 1.3 | 11.5 |
| Since/during the pandemic | 6.6 | 10.8 | 29.7 | 25.3 | 15.9 | 11.5 |
Impact of the pandemic on pre-existent disorders, on patient subgroups and time course of psychological burden
When asked about the differential effects of the pandemic on pre-existing disorders or mental problems, the majority of participants indicated that effects were negative in general (55.7%), some reported that effects were individual, differing from case to case (23.6%), and only 1.3% reported that effects were positive rather than negative (Supplement Table S5). When asked which psychopathological disorder or group of patients had been particularly affected by the pandemic (Table 5), depression (67.4%) and anxiety disorders (63%) were indicated by far most often, followed by OCD (26%) and ADHD (25.8%).
Table 5.
Patient groups/disorders that have been particularly affected by the pandemic
| N | % | |
|---|---|---|
| Depression | 306 | 67.4 |
| Anxiety disorder | 286 | 63.0 |
| OCD | 127 | 26.0 |
| ADHD | 117 | 25.8 |
| Trauma, adjustment disorder | 99 | 21.1 |
| Eating disorder | 86 | 18.9 |
| Autism spectrum disorder | 45 | 9.9 |
| Psychosis | 22 | 4.8 |
| Other | 14 | 3.1 |
| Not stated | 74 | 16.3 |
Multiple answers were possible
Conversely, when asked to indicate disorders or groups of patients that had been less affected or even had benefited during the pandemic, anxiety disorders (28%) and autism spectrum disorders (29.7%) were selected most often. General benefits were, however, often indicated as only short term (33%) and/or limited to the time period of the lockdown (30%) (Table 6). In free text comments, social anxiety was mentioned particularly often as temporarily improved in consequence to the pandemic (N = 12; Table 6).
Table 6.
Have patient groups been less affected by the pandemic than others, or did they actually benefit?
| N | % | |
|---|---|---|
| No one has benefited | 30 | 6.6 |
| Some patients have benefited | ||
| Some patients with ADHD | 64 | 14.1 |
| Some patients with ASD | 135 | 29.7 |
| Some patients with anxiety disorder | 127 | 28.0 |
| Some patients with depression | 19 | 4.2 |
| Only during the lockdown (March/April 2020) | 140 | 30.8 |
| Only short term | 150 | 33.0 |
| Don’t know/not stated | 64 | 14.1 |
| Other | 37 | 8.1 |
| Free text comments (summary) | ||
| School phobia/school absenteeism | 5 | |
| Social anxiety | 12 | |
| Learning disorders, school problems | 3 | |
| OCD | 1 | |
| Victim of bullying | 2 | |
| Other | 12 | |
Multiple answers were possible
Regarding differential effects of the coronavirus crisis on age groups or gender, a majority (63.9%) found that adolescents had been most severely affected by the pandemic (Table 7). Only 10.1% of participants viewed children between 7 and 12 years as most affected. Most participants estimated that boys and girls had been equally severely affected (65.4%). Nevertheless, 14.1% of the participants found that girls had been more severely affected, while only 3.3% indicated boys as more affected (Supplement Table S6).
Table 7.
Age group most affected by the pandemic
| N | % | |
|---|---|---|
| Younger children (up to 7 years) | 7 | 1.5 |
| Primary school age (7–12 years) | 47 | 10.1 |
| Adolescents (13 years and older) | 290 | 63.9 |
| All about the same | 51 | 11.2 |
| Don’t know/not stated | 56 | 12.2 |
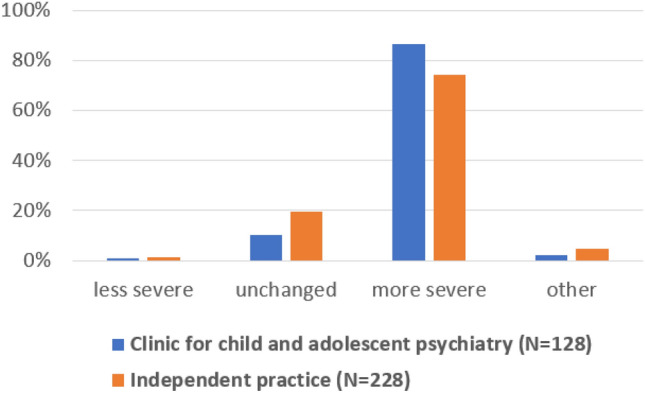
Participants were also asked to indicate the time period in the course of the first year of pandemic, which had been psychologically the most difficult for the patients. Winter 2021 (January, February, March 2021) emerged as the most difficult time period, as indicated by 69% (N = 315) of respondents, followed by autumn 2020 (54.2%; N = 208). The actual lockdown period (March/April 2020) was rarely seen as particularly stressful (19.2%, N = 87) (Fig. 2, Supplement Table S7).
Fig. 2.
Time period of the pandemic with particularly high psychological burden for patients (frequency of responses). Multiple responses were possible
Pandemic-specific problems
Participants were asked to indicate whether certain problems or disorders encountered during the pandemic were new or different compared to pre-COVID-19 times. 42% of participants responded affirmatively and described pandemic-specific problems in free text comments (Table 8). In the analysis of these comments, three pandemic-specific topics emerged: 1. future-related anxiety/lack of perspective and concrete difficulties in the transition from school to apprenticeship/further education/profession (N = 49), 2. school absenteeism, school anxiety and avoiding returning to school (N = 25), and 3. loneliness and isolation (N = 24). Other relatively common problem areas were the constraints and fears related to hygiene rules and fear of infection (N = 18), and increased consumption of digital media (N = 16) (Table 8).
Table 8.
Pandemic-specific problems/changes (N = 193) (free text summary)
| N | |
|---|---|
| Fear of the future, education more difficult, career entry more difficult, lack of perspective, disorientation, “stolen youth” | 49 |
| School absenteeism, school anxiety, fear of returning to school | 25 |
| Lack of social contact, loneliness | 24 |
| Hypochondria/anxieties/compulsions intensified or newly developed because of pandemic hygiene rules and attention to symptoms | 18 |
| Digital media consumption, digital media addiction | 16 |
| Obsessive–compulsive patients had more time to pursue compulsions, anxiety and compulsions increased or new, panic attacks | 15 |
| Suicidality/depression | 13 |
| Lack of sports opportunities exacerbate hyperactivity and weight problems, no recreational opportunities | 11 |
| Family conflicts, domestic violence | 11 |
| Lack of school and parental guidance, lack of structure | 10 |
| Financial problems, parents’ loss of work promotes conflicts | 7 |
| Loss of stabilizing factors (e.g., meeting friends, future plans, meeting grandparents) leads to decompensation | 6 |
| Difficulty in detaching from parents; adolescents feeling overly controlled by parents | 5 |
| Fear that family members might die or be infected, topic of death, mourning | 5 |
| Activity buildup impossible for patients with depression | 4 |
| Positive aspects: Families benefit from quiet time at home, relief from social pressure for autistic patients, fathers are more present | 4 |
| Drugs | 4 |
| Insufficient regulatory control of families at risk | 1 |
| Long-COVID syndrome | 1 |
The situation of parents during the pandemic
When participants were asked about problems expressed by parents during the pandemic more frequently than before, loneliness/isolation of the child (49%) and worries about the child’s education and academic future (33%) emerged as most frequent concerns expressed by parents. Complaints about general isolation and loneliness of the family, financial problems and problems related to the lack of child care options were also expressed by parents more often than before the pandemic (Table 9).
Table 9.
Frequency of family problems reported by parents before and since the pandemic
| Much less | A little less | No change | A little more | Much more | Not stated | |
|---|---|---|---|---|---|---|
| % | % | % | % | % | % | |
| Conflicts between patient and parent(s) | 0.2 | 0.7 | 13.9 | 56.6 | 19.2 | 9.5 |
| Conflicts between parents | 0.0 | 0.4 | 17.2 | 53.1 | 15.0 | 14.3 |
| Domestic violence | 0.0 | 0.4 | 23.6 | 36.1 | 3.5 | 36.3 |
| Financial problems/job loss | 0.0 | 0.0 | 15.2 | 48.7 | 19.4 | 16.7 |
| General isolation of the family | 0.0 | 0.2 | 11.5 | 48.0 | 24.7 | 15.6 |
| Isolation/loneliness of the child/adolescent | 0.0 | 0.2 | 3.7 | 39.4 | 49.1 | 7.5 |
| Lack of child care options | 0.7 | 0.2 | 18.7 | 36.3 | 25.6 | 18.5 |
| Concern about child's future/education | 0.0 | 0.9 | 15.4 | 38.8 | 33.0 | 11.9 |
| Mental problems of one parent | 0.0 | 0.2 | 34.1 | 34.8 | 7.5 | 23.3 |
| Addiction/alcohol problems of one parent | 0.0 | 0.0 | 37.0 | 25.3 | 3.3 | 34.4 |
When asked about problems reported by parents which are directly related to the pandemic and its consequences, mothers’ multiple workloads regarding office work at home, household activities, and caregiving responsibilities (36.3%), children’s increased media time due to missing alternative leisure activities (37.4%), and parents being overwhelmed in taking care of homeschooling (32.4%) were mentioned very often (Table 10). In free text comments, the loss of family contacts and lacking support by grandparents were also mentioned as frequently encountered problems, among others (N = 11) (Supplement Table S8).
Table 10.
How often did parents report the following effects of the pandemic?
| Never | Rarely | Some-times | Often | Very/extremely often | Not stated | |
|---|---|---|---|---|---|---|
| % | % | % | % | % | % | |
| The child is left alone at home (lack of child care possibilities) | 6.8 | 18.5 | 34.6 | 15.4 | 10.4 | 14.3 |
| Parents cannot adequately take care of the child due to work at home | 4.4 | 11.7 | 33.0 | 23.3 | 13.3 | 14.3 |
| Mothers suffer from the multiple burdens (child care, home office, household) | 0.7 | 2.9 | 16.7 | 31.9 | 36.3 | 11.5 |
| Fathers suffer from the multiple burdens (child care, home office, household) | 2.2 | 12.8 | 31.9 | 25.1 | 13.7 | 14.3 |
| Parents feel overwhelmed by supervision of homeschooling | 0.0 | 3.1 | 21.1 | 32.8 | 32.4 | 10.6 |
| Parent–child conflicts because of homeschooling | 0.7 | 3.7 | 22.9 | 30.4 | 29.3 | 13.0 |
| Parents allow excessive media use to keep child occupied | 0.0 | 3.1 | 17.6 | 29.3 | 37.4 | 12.6 |
| Learning problems due to homeschooling | 0.4 | 5.5 | 20.0 | 31.3 | 30.0 | 13.0 |
Discussion
In the present survey, we investigated the impact of the first year of the COVID-19 pandemic on mental health and family problems of clinically referred children and adolescents from the perspective of mental health care professionals in Switzerland.
Disorder-specific changes in the frequency of referrals during the pandemic
This survey revealed an important change in the disorder-specific pattern of referrals. A strong increase was indicated for depression and anxiety disorders by most respondents (over 40%), followed by crisis intervention, suicidality, psychosomatic complaints and behavioral addictions. This is well in line with other studies reporting an increase in the aforementioned disorders in children and adolescents during the pandemic (Panchal et al. 2021). On the other hand, the majority of respondents reported no relevant change in the number of referrals for autism spectrum disorders or only very small increases for ADHD or psychosis. A decrease of referrals was not reported for any of the disorders. One may assume, in consequence, that the pandemic had a selective impact on certain disorders, especially those associated with internalizing symptoms, but not on psychopathology in general. It has been reported that for some children with ADHD or ASD, containment measures such as staying at home, reduction of social contacts and having no longer to conform to school discipline were experienced as a reduction of pressure and social stress which led to stress reduction and consequently to a relief of symptoms (Bruining et al. 2020; Bobo et al. 2020; Cost et al. 2021). However, this is not reflected by the number of referrals which did not decrease during the pandemic. Among the neurodevelopmental disorders, a relevant increase in referrals was reported for learning disorders and, to a smaller extent, behavioral disorders/aggressiveness. The former may be explained by the fact that children with learning problems might have been unable to keep up with their studies during remote learning or that deficits may have become more visible for parents who had to supervise their child’s schoolwork during homeschooling measures. Increased behavioral dysregulation, anger and irritability during the pandemic have been described in children and adolescents during the pandemic (Mohler-Kuo et al. 2021; see Panchal et al. 2021), often in interaction with enhanced parental stress (Andrés et al. 2022; Montirosso et al. 2021). Referrals for OCD, eating disorders, behavioral addictions and substance had also increased, in agreement with studies on pandemic effects on eating disorders (Otto et al. 2021; Schwartz and Costello 2021), OCD (Alhujaili et al. 2021; Sowmya et al. 2021), substance use disorder (Sen et al. 2021), problematic digital media use (Masaeli and Farhadi 2021). The number of participants who indicate frequent referrals for problematic use of the internet/problematic gaming has more than doubled during the pandemic.
Interestingly, for disorders such as psychosis or schizophrenia, most health professionals indicated no change in the number of referrals. This is consistent with literature according to which patients with internalizing/affective disorders are more affected by the pandemic than patients with psychotic disorders (Gul and Demirci 2021; van Loon et al. 2021). The latter have shown, however, a higher risk of being infected with COVID-19 (Karaoulanis and Christodoulou 2021). The high number of missing responses in this category may be explained by its lower prevalence and by the fact that many child and adolescent psychotherapists do not treat patients with psychosis. When only valid responses are considered, about 20% of remaining respondents reported a slight increase of psychoses during the pandemic. This may be indicative of a heightened psychological distress under COVID-19 conditions in this vulnerable group. An increase in prevalence of psychosis or (reactive) brief psychotic episodes during the pandemic has been described for adults (Segev et al. 2021). However, a relative increase was reported for all disorders and may also reflect a generally increased demand for treatment due to the distress during the corona crisis. All in all, a pattern emerged, with an important increase of referrals for internalizing disorders including depression, anxiety disorders and psychosomatic problems, and also for domestic conflicts, crisis intervention, suicidality, and behavioral addictions, whereas referrals of disorders, such as psychosis and ASD remained relatively stable.
Mental problems caused or triggered by the pandemic
When we asked for problems caused or triggered by the pandemic, depression and family conflicts were explicitly attributed to the pandemic by the majority of participants. Psychosomatic disorders, especially sleep problems, suicidality, (social) anxiety, were still linked to the pandemic by more than a third of participants. Addictive behaviors and eating disorders were considered to be caused or triggered by the pandemic by approximately 20%. These percentages may partly be confounded with differences in the prevalence of the disorders or by the fact that certain disorders are usually treated by a small number of specialists. General anxiety disorder was not included among the response options but was mentioned by several respondents in free text comments as caused by the pandemic. In contrast, the number of mental health professionals who explicitly denied a relation between the pandemic and the increase of mental problems was very small (7.5%). Nevertheless, some participants assumed in free text comments a pre-existent vulnerability in patients that may have prevented a successful coping with the corona crisis and which led to the need for treatment.
Severity of disorders
There was a general agreement among participants that the severity of disorders had increased during the pandemic, which may be related to the reported high occurrence of acute crises and suicidality and which is in accordance with studies showing an exacerbation of symptoms during the pandemic (Tanir et al. 2020). Participants working in clinics for child and adolescent psychiatry reported a slightly higher increase in severity than those working in independent practice. This probably reflects the fact that usually the more severe, complex, or acute cases are seen and subsequently treated in clinics for child and adolescent psychiatry rather than in independent practice settings. As emergencies dramatically increased during the corona crisis in Switzerland among children and adolescents with mental health problems (Berger et al. 2022; Werling et al. 2022b), along with a shortage of treatment places and longer waiting time before admission to treatment, many mental health professionals working in independent practice must have been confronted with severe cases, which in normal times would rather have been treated in clinics for child and adolescent psychiatry. This was also reported in the free text sections.
The question arises whether the increased rate of affective disorders, acute crises and suicidality reported by professionals in this survey is reflected by an increase of emergency consultations and suicide rates as more objective measures. According to a recently published Swiss retrospective cohort study of a child and adolescent psychiatric out-patient emergency facility based on electronic patient records, the demand of emergency service considerably increased during the pandemic (Berger et al. 2022). Compared to before the pandemic, emergency bridging interventions increased by 230% and inpatient admissions of minors to adult psychiatric inpatient units, necessary because of lacking treatment capacity in child and adolescent psychiatry, more than doubled, due to significant increase of suicidality and self-harm behavior. Other studies also reported an increase of minors presenting with suicidality in emergency departments (Carison et al. 2022) or reported higher rates of suicide attempts among adolescents psychiatrically hospitalized during the pandemic in comparison to the year before (Thompson et al. 2021). Stressors during the pandemic-like loneliness, social isolation or financial burden amongst others were made responsible for the increased suicide risk (e.g., Sher 2020).
Pandemic-specific effects
Specific topics that emerged as new and direct effects of the pandemic, were related to consequences of confinement: the fear of the future/lack of perspective reported by adolescents, school anxiety and absenteeism, and lack of social contact, loneliness. Other, less frequently reported topics were newly developed or intensified compulsions because of pandemic hygiene rules and increased self-observation for possible signs of infection.
Differential effects on subgroups of patients and of time periods
The majority of professionals assumed that the pandemic had hit adolescents particularly hard, which has been confirmed by other (epidemiological) studies (Hawes et al. 2021). In adolescence, social relationships with peers outside the core family become a high priority. Consequently, since pandemic’s restriction measures focusing on social distancing, it is not surprising that adolescents seem to have suffered most during this time. In terms of gender effects, the majority (64%) of professionals claimed that girls and boys had been affected to the same extent by effects of the pandemic, and only 14% of the participants indicated that girls had been more severely affected than boys (while the opposite was indicated by 3%). This is a relatively small difference compared to other results showing that negative effects of the pandemic on mental health are more severe in females (Halldorsdottir et al. 2021; Liu et al. 2022; Ma et al. 2021). However, in the present sample, participants refer to patients who all suffered from mental health problems, irrespective of their gender. Thus, in a clinical sample, an advantage for boys in adapting to the pandemic may still exist, but to a lesser degree than in epidemiological samples. January/February/March 2021 emerged as the time period with the highest psychological burden for patients, which was slightly delayed to the peak of the “second wave” of COVID-19 infections in October/November 2020 in Switzerland. The lockdown period in March/April 2020 and the summer months of 2020 were not associated with a particular high burden. This time course is in agreement with reports from Germany (Döpfner et al. 2021). When asked to indicate the subgroups of patients/disorders that had been most affected by the pandemic, depression and anxiety disorders were indicated by most participants. In a German study, patients with depressive disorders, especially girls, were also identified as the group with the highest psychological burden (Gilsbach et al. 2021). ADHD and OCD were still indicated by approximately 25% as among the most severely affected. On the other hand, ADHD was also among the disorders that were supposed to have benefited but this was only indicated by a small number of participants (14%), compared to ASD (29%) or anxiety disorders (28%). This confirms the inconsistent effects of the pandemic on ADHD and anxiety disorder reported previously, with improved symptoms due to a relief of pressure during school closures and limited social contacts in some patients, but increased symptoms under pandemic conditions in others.
Pandemic-related complaints and difficulties reported by parents
Isolation/loneliness of the child and concern about the child’s education/academic and professional future emerged as the worries reported most often by parents since the pandemic, followed by domestic conflicts, the isolation as a family and lack of child care options due to confinement measures. Other frequently reported effects on families were that parents felt constrained to allow excessive media use in the absence of other leisure activities, multiple burdens imposed by pandemic restrictions especially on mothers, and parents feeling overwhelmed by the supervision of homeschooling tasks. The burden experienced by mothers under COVID-19 has been reported in the literature (Calvano et al. 2021; McLaren et al. 2020; Taylor et al. 2021), and mothers of children with depression or developmental disorders are known to be under extra strain (Babore et al. 2021; Burnett et al. 2021; Chafouleas and Iovino 2021; Wang et al. 2021).
Support and measures taken to date during the pandemic
Since the pandemic with its restrictions has also led to a strain on mental health and psyche in the general population, several support services had been already expanded during the pandemic in Switzerland. Various low-threshold psychosocial counselling services, information platforms and websites were implemented for the prevention of psychiatric disorders and maintenance of mental health for the general population of all ages (ECDC 2020). For the protection of the mental health of the Swiss population, providers such as “Dargebotene Hand”, “Pro Juventute” and “Pro Mente Sana” had expanded their counselling services since spring 2020 (Stocker et al. 2021). The Federal Office of Public Health (FOPH) additionally supported two information platforms for the general population (www.dureschnufe.ch and www.reden-kann-retten.ch).
For patients, especially for children and adolescents with pre-existing psychiatric disorders, the pandemic was particularly challenging. However, medical support in general and therapeutic care were limited to (acute) crises or carried out partly via telemedicine. To continue to provide necessary care, minor patients were triaged to adult psychiatry for inpatient treatment even more frequently than before the pandemic. In addition, special temporary regulations had been introduced for the billing of telemedicine consultation.
Taken together, the effects of the pandemic reported by parents and the new and pandemic-specific topics that emerged in therapy, such as loneliness, fear of the future, worry about educational goals, isolation of the family, suggested a direct effect of the confinement measures on the deterioration of mental health. It may be difficult to distinguish whether the apparent rise of mental illness during the corona crisis is entirely caused by the pandemic, triggered by the pandemic in individuals with heightened pre-existent vulnerability, or simply an exacerbation of pre-existent symptoms. In this study, most mental health professionals perceived anxiety disorder, depression, and suicidal crises in patients treated during the first year of pandemic as triggered or caused by the corona crisis. Also, adolescence is in general a period of heightened vulnerability and emotional imbalance (Larsen and Luna 2018), which may more easily lead to reactive mental problems than at other periods of life, and which challenges a clear differentiation between typical and psychopathological reactions.
Limitations
The first limitation is that all information is based on subjective reports and not on objective patient statistics provided by the individual therapists. In addition, data relating to pre-COVID condition were collected retrospectively and may thus be subject to bias. Another limitation is that we did not include anxiety disorders among the preselected categories in the question on mental disorders triggered by the pandemic. Furthermore, the response rate of 24% was rather low, although still remarkable for a group of people with extreme work overload during pandemic times. In consequence, the representativity of the study is uncertain. Finally, a possible impact of the mediatization of the pandemic and de-stigmatization of psychiatric and psychological care on the increase of referrals cannot be ruled out. Also, opinions of professionals may have been influenced in the same way.
Conclusions
In this study, based on reports by mental health professionals, it was shown that during the first year of pandemic, the number of clinically referred children and adolescents to psychiatric or psychological treatment had substantially increased and the pattern of disorders had changed. In particular internalizing disorders such as depression, anxiety disorders, acute crises including suicidality and psychosomatic problems along with problematic internet use were treated more frequently than before the pandemic, while the frequency of other disorders, such as psychosis or autism spectrum disorder, remained relatively stable. For most mental health professionals, the reported changes seemed directly related to the effects of the corona crisis and its restrictions. As the development of the COVID-19 pandemic or other crises is not predictable, measures should be taken to prevent similar catastrophic effects on youth in the future. This includes measures against the shortage of treatment supply in mental health care for children and adolescents, as well as measures to avoid social isolation of children and adolescents, to provide better support for families during crises, and to identify adolescents at risk early.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors acknowledge the support of all mental health professionals within Switzerland who participated in this survey. In addition, the authors thank the Swiss Society for Child and Adolescent Psychiatry and Psychotherapy and the Zurich Society for Child and Adolescent Psychiatry and Psychotherapy for their collaboration. No financial support was received for this study.
Funding
Open access funding provided by University of Zurich.
Declarations
Conflict of interest
S. Walitza has received in the last 5 years royalties from Thieme Hogrefe, Kohlhammer, Springer, Beltz, Elsevier. Her work was supported in the last 5 years by the Swiss National Science Foundation (SNF), diff. EU FP7s, Bfarm Germany, ZInEP, Gertrud Thalmann, Vontobel, Unicentia, Erika Schwarz Fonds. Outside professional activities and interests are declared under the link of the University of Zurich www.uzh.ch/prof/ssl-dir/interessenbindungen/client/web/. RD has received royalties from Hogrefe and her work has been supported by the SNF in the last 5 years. The other authors declare no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Anna Maria Werling, Email: anna.werling@pukzh.ch.
Susanne Walitza, Email: susanne.walitza@pukzh.ch.
Stephan Eliez, Email: Stephan.Eliez@unige.ch.
Renate Drechsler, Email: renate.drechsler@kjpd.uzh.ch.
References
- Al Omari O, Al Sabei S, Al Rawajfah O, Abu Sharour L, Al-Hashmi I, Al Qadire M, Khalaf A. Prevalence and predictors of loneliness among youth during the time of COVID-19: a multinational study. J Am Psychiatr Nurses Assoc. 2021 doi: 10.1177/10783903211017640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alhujaili N, Alghamdi A, Abo Talib T, Alhaqbani M, Alfelali M, Alghamdi W. The impact of COVID-19 pandemic on obsession and compulsion symptoms in Saudi Arabia. Cureus. 2021 doi: 10.7759/cureus.20021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrés ML, Galli JI, del Valle M, Vernucci S, López-Morales H, Gelpi-Trudo R, Canet-Juric L. Parental perceptions of child and adolescent mental health during the COVID-19 pandemic in Argentina. Child Youth Care Forum. 2022 doi: 10.1007/s10566-021-09663-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babore A, Trumello C, Lombardi L, Candelori C, Chirumbolo A, Cattelino E, Baiocco R, Bramanti SM, Viceconti ML, Pignataro S, Morelli M. Mothers’ and children’s mental health during the COVID-19 pandemic lockdown: the mediating role of parenting stress. Child Psychiatry Hum Dev. 2021 doi: 10.1007/s10578-021-01230-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger G, Häberling I, Lustenberger A, Probst F, Franscini M, Pauli D, Walitza S. The mental distress of our youth in the context of the corona pandemic. Swiss Med Wkly. 2022;2022(152):30142. doi: 10.4414/smw.2022.w30142. [DOI] [PubMed] [Google Scholar]
- Bhatia R. Effects of the COVID-19 pandemic on child and adolescent mental health. Curr Opin Psychiatry. 2020;33(6):568–570. doi: 10.1097/YCO.0000000000000651. [DOI] [PubMed] [Google Scholar]
- Bobo E, Lin L, Acquaviva E, Caci H, Franc N, Gamon L, Picot MC, Pupier F, Speranza M, Falissard B, Purper-Ouakil D. How do children and adolescents with attention deficit hyperactivity disorder (ADHD) experience lockdown during the COVID-19 outbreak? Encephale. 2020;46(3):S85–S92. doi: 10.1016/j.encep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruining H, Bartels M, Polderman TJC, Popma A. COVID-19 and child and adolescent psychiatry: an unexpected blessing for part of our population? Eur Child Adolesc Psychiatr. 2020 doi: 10.1007/s00787-020-01578-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnett D, Masi A, Diaz AM, Rizzo R, Lin PI, Eapen V. Distress levels of parents of children with neurodevelopmental disorders during the COVID-19 pandemic: a comparison between Italy and Australia. Int J Environ Res Public Health. 2021 doi: 10.3390/ijerph182111066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calvano C, Engelke L, Di Bella J, Kindermann J, Renneberg B, Winter SM (2021) Families in the COVID-19 pandemic: parental stress, parent mental health and the occurrence of adverse childhood experiences—results of a representative survey in Germany. Eur Child Adolesc Psychiatr 1–13. 10.1007/s00787-021-01739-0 [DOI] [PMC free article] [PubMed]
- Carison A, Babl FE, O'Donnell SM. Increased paediatric emergency mental health and suicidality presentations during COVID-19 stay at home restrictions. Emerg Med Australas. 2022;34(1):85–91. doi: 10.1111/1742-6723.13901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chadi N, Spinoso-Di Piano C, Osmanlliu E, Gravel J, Drouin O. Mental health-related emergency department visits in adolescents before and during the COVID-19 pandemic: a multicentric retrospective study. J Adolesc Health. 2021 doi: 10.1016/j.jadohealth.2021.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chafouleas SM, Iovino EA. Comparing the initial impact of covid-19 on burden and psychological distress among family caregivers of children with and without developmental disabilities. School Psychol. 2021;36(5):358–366. doi: 10.1037/spq0000426. [DOI] [PubMed] [Google Scholar]
- Clemens V, Beschoner P, Jarczok MN, Weimer K, Kempf M, Morawa E, Geiser F, Albus C, Steudte-Schmiedgen S, Gündel H. The mediating role of COVID-19-related burden in the association between adverse childhood experiences and emotional exhaustion: results of the egePan–voice study. Eur J Psychotraumatol. 2021;12(1):1976441. doi: 10.1080/20008198.2021.1976441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cost KT, Crosbie J, Anagnostou E, Birken CS, Charach A, Monga S, Kelley E, Nicolson R, Maguire JL, Burton CL, Schachar RJ, Arnold PD, Korczak DJ. Mostly worse, occasionally better: impact of COVID-19 pandemic on the mental health of Canadian children and adolescents. Eur Child Adolesc Psychiatry. 2021 doi: 10.1007/s00787-021-01744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deolmi M, Pisani F. Psychological and psychiatric impact of COVID-19 pandemic among children and adolescents. Acta Biomed. 2020;91(4):1–5. doi: 10.2375/abm.v91i4.10870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Döpfner M, Adam J, Habbel C, Schulte B, Schulze-Husmann K, Simons M, Heuer F, Wegner C, Bender S (2021) Die psychische Belastung von Kindern, Jugendlichen und ihren Familien während der COVID-19-Pandemie und der Zusammenhang mit emotionalen und Verhaltensauffälligkeiten. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz, 64(12):1522–1532. [DOI] [PMC free article] [PubMed]
- El-Osta A, Alaa A, Webber I, Sasco ER, Bagkeris E, Millar H, Vidal-Hall C, Majeed A. How is the COVID-19 lockdown impacting the mental health of parents of school-age children in the UK? A cross-sectional online survey. BMJ Open. 2021;11(5):e043397. doi: 10.1136/bmjopen-2020-043397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enevoldsen KC, Danielsen AA, Rohde C, Jefsen OH, Nielbo KL, Østergaard SD. Monitoring of COVID-19 pandemic-related psychopathology using machine learning. Acta Neuropsychiatrica. 2022 doi: 10.1017/neu.2022.2. [DOI] [PubMed] [Google Scholar]
- European Centre for Disease Prevention and Control (2020) Increased transmission of COVID-19 in the EU/EEA and the UK – thirteenth update. 23 October 2020. ECDC, Stockholm
- Giallonardo M, Uccella S, Nobili L, Bruni O, Melegari MG (2021) Stress symptoms and Coronavirus disease 2019 (COVID-19): a comparative study between Attention Deficit Hyperactivity Disorder and typically developing children and adolescents. Min Pediatr. 10.23736/s2724-5276.21.06477-6 [DOI] [PubMed]
- Gilsbach S, Herpertz-Dahlmann B, Konrad K. Psychological impact of the COVID-19 pandemic on children and adolescents with and without mental disorders. Front Public Health. 2021 doi: 10.3389/fpubh.2021.679041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gul MK, Demirci E. Psychiatric disorders and symptoms in children and adolescents during the COVID-19 pandemic: a review. Eur J Med Oncol. 2021;5(1):20. [Google Scholar]
- Halldorsdottir T, Thorisdottir IE, Meyers CCA, Asgeirsdottir BB, Kristjansson AL, Valdimarsdottir HB, Allegrante JP, Sigfusdottir ID. Adolescent well-being amid the COVID-19 pandemic: are girls struggling more than boys? JCPP Adv. 2021;1(2):e12027. doi: 10.1002/jcv2.12027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawes MT, Szenczy AK, Klein DN, Hajcak G, Nelson BD. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol Med. 2021 doi: 10.1017/S0033291720005358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huebener M, Waights S, Spiess CK, Siegel NA, Wagner GG. Parental well-being in times of Covid-19 in Germany. Rev Econ Household. 2021;19(1):91–122. doi: 10.1007/s11150-020-09529-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefsen OH, Rohde C, Nørremark B, Østergaard SD. Editorial perspective: COVID-19 pandemic-related psychopathology in children and adolescents with mental illness. J Child Psychol Psychiatr All Discipl. 2021;62(6):798–800. doi: 10.1111/jcpp.13292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juli MR, Juli G, Juli R. An epidepic in the pandemic: the most difficult challenge for young adolescents. Psychiatr Danub. 2021;33(Suppl 9):142–147. [PubMed] [Google Scholar]
- Karaoulanis SE, Christodoulou NG. Do patients with schizophrenia have higher infection and mortality rates due to COVID-19? A systematic review. Psychiatriki. 2021;32(3):219–223. doi: 10.22365/jpsych.2021.027. [DOI] [PubMed] [Google Scholar]
- Kawabe K, Hosokawa R, Nakachi K, Yoshino A, Horiuchi F, Ueno SI. Excessive and problematic internet use during the coronavirus disease 2019 school closure: comparison between Japanese youth with and without autism spectrum disorder. Front Public Health. 2020 doi: 10.3389/fpubh.2020.609347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazi F, Mushtaq A. Adolescents navigating the COVID-19 pandemic. Lancet Child Adolesc Health. 2021;5(10):692. doi: 10.1016/S2352-4642(21)00279-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan YS, Jouda M, Albobali Y, et al (2022) COVID-19 pandemic fears and obsessive-compulsive symptoms in adolescents with pre-existing mental disorders: An exploratory cross-sectional study. Clin Child Psychol Psychiatr 27(1):89–103. 10.1177/13591045211017606 [DOI] [PMC free article] [PubMed]
- Larsen B, Luna B. Adolescence as a neurobiological critical period for the development of higher-order cognition. Neurosci Biobehav Rev. 2018;94:179–195. doi: 10.1016/j.neubiorev.2018.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavenne-Collot N, Ailliot P, Badic S, Favé A, François G, Saint-André S, Thierry A, Bronsard G. Did child-psychiatry patients really experience the dreaded clinical degradation during the COVID-19 pandemic lockdown? Neuropsychiatrie De L’enfance Et De L’adolescence. 2021;69(3):121–131. doi: 10.1016/j.neurenf.2021.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeb RT, Bitsko RH, Radhakrishnan L, Martinez P, Njai R, Holland KM. Mental health–related emergency department visits among children aged< 18 years during the COVID-19 pandemic—United States, January 1–October 17, 2020. Morb Mortal Wkly Rep. 2020;69(45):1675. doi: 10.15585/mmwr.mm6945a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu SR, Davis EP, Palma AM, Sandman CA, Glynn LM. The acute and persisting impact of COVID-19 on trajectories of adolescent depression: sex differences and social connectedness. J Affect Disord. 2022;299:246–255. doi: 10.1016/j.jad.2021.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma L, Mazidi M, Li K, Li Y, Chen S, Kirwan R, Zhou H, Yan N, Rahman A, Wang W, Wang Y. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disorders. 2021;293:78–89. doi: 10.1016/j.jad.2021.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques de Miranda D, da Silva Athanasio B, Sena Oliveira AC, Simoes-e-Silva AC. How is COVID-19 pandemic impacting mental health of children and adolescents? Int J Disas Risk Reduct. 2020 doi: 10.1016/j.ijdrr.2020.101845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masaeli N, Farhadi H. Prevalence of Internet-based addictive behaviors during COVID-19 pandemic: a systematic review. J Addict Dis. 2021 doi: 10.1080/10550887.2021.1895962. [DOI] [PubMed] [Google Scholar]
- McLaren HJ, Wong KR, Nguyen KN, Mahamadachchi KND. Covid-19 and women’s triple burden: Vignettes from Sri Lanka, Malaysia. Vietnam Australia Social Sci. 2020;9(5):87. [Google Scholar]
- Melegari MG, Giallonardo M, Sacco R, Marcucci L, Orecchio S, Bruni O. Identifying the impact of the confinement of Covid-19 on emotional-mood and behavioural dimensions in children and adolescents with attention deficit hyperactivity disorder (ADHD) Psychiatry Res. 2021 doi: 10.1016/j.psychres.2020.113692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohler-Kuo M, Dzemaili S, Foster S, Werlen L, Walitza S. Stress and mental health among children/adolescents, their parents, and young adults during the first COVID-19 lockdown in Switzerland. Int J Environ Res Public Health. 2021;18(9):4668. doi: 10.3390/ijerph18094668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montirosso R, Mascheroni E, Guida E, Piazza C, Sali ME, Molteni M, Reni G. Stress symptoms and resilience factors in children with neurodevelopmental disabilities and their parents during the COVID-19 pandemic. Health Psychol. 2021;40(7):428–438. doi: 10.1037/hea0000966. [DOI] [PubMed] [Google Scholar]
- Otto AK, Jary JM, Sturza J, Miller CA, Prohaska N, Bravender T, Van Huysse J (2021) Medical admissions among adolescents with eating disorders during the COVID-19 Pandemic. Pediatrics 148(4). 10.1542/peds.2021-052201 [DOI] [PubMed]
- Panchal U, Salazar de Pablo G, Franco M, Moreno C, Parellada M, Arango C, Fusar-Poli P. The impact of COVID-19 lockdown on child and adolescent mental health: systematic review. Eur Child Adolesc Psychiatr. 2021 doi: 10.1007/s00787-021-01856-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin Z, Shi L, Xue Y, Lin H, Zhang J, Liang P, Lu Z, Wu M, Chen Y, Zheng X. Prevalence and risk factors associated with self-reported psychological distress among children and adolescents during the COVID-19 pandemic in China. JAMA Netw Open. 2021;4(1):e2035487–e2035487. doi: 10.1001/jamanetworkopen.2020.35487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravens-Sieberer U, Kaman A, Erhart M, Otto C, Devine J, Löffler C, Hurrelmann K, Bullinger M, Barkmann C, Siegel NA, Simon AM, Wieler LH, Schlack R, Hölling H (2021) Quality of life and mental health in children and adolescents during the first year of the COVID-19 pandemic: results of a two-wave nationwide population-based study. Eur child Adolesc Psychiatr. 10.1007/s00787-021-01889-1 [DOI] [PMC free article] [PubMed]
- Revet A, Hebebrand J, Anagnostopoulos D, Kehoe LA, Klauser P (2021) ESCAP CovCAP survey of heads of academic departments to assess the perceived initial (April/May 2020) impact of the COVID-19 pandemic on child and adolescent psychiatry services. Eur Child Adolesc Psychiatr 1–10. 10.1007/s00787-020-01699-x [DOI] [PMC free article] [PubMed]
- Rodriguez CM, Lee SJ, Ward KP, Pu DF. The perfect storm: hidden risk of child maltreatment during the COVID-19 pandemic. Child Maltreat. 2021;26(2):139–151. doi: 10.1177/1077559520982066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde C, Jefsen OH, Nørremark B, Danielsen AA, Østergaard SD. Psychiatric symptoms related to the COVID-19 pandemic. Acta Neuropsychiatrica. 2020;32(5):274–276. doi: 10.1017/neu.2020.24. [DOI] [PubMed] [Google Scholar]
- Samji H, Wu J, Ladak A, Vossen C, Stewart E, Dove N, Long D, Snell G (2021) Mental health impacts of the COVID‐19 pandemic on children and youth–a systematic review. Child Adolesc Mental Health 27(2):173–189. 10.1111/camh.12501 [DOI] [PMC free article] [PubMed]
- Schwartz MD, Costello KL. Eating disorder in teens during the COVID-19 pandemic. J Adolesc Health. 2021;68(5):1022. doi: 10.1016/j.jadohealth.2021.02.014. [DOI] [PubMed] [Google Scholar]
- Segev A, Hirsch-Klein E, Kotz G, Kamhi-Nesher S, Halimi S, Qashu K, Schreiber E, Krivoy A. Trends of new-onset psychosis or mania in psychiatric emergency departments during the COVID19 pandemic: a longitudinal comparative study. Sci Rep. 2021 doi: 10.1038/s41598-021-00310-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selçuk EB, Demir AÇ, Erbay LG, Özcan ÖÖ, Gürer H, Dönmez YE. Anxiety, depression and post-traumatic stress disorder symptoms in adolescents during the COVID-19 outbreak and associated factors. Int J Clin Pract. 2021;75(11):e14880. doi: 10.1111/ijcp.14880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen LT, Siste K, Hanafi E, Murtani BJ, Christian H, Limawan AP, Siswidiani LP. Insights into adolescents’ substance use in a low–middle-income country during the COVID-19 pandemic. Front Psychiatr. 2021 doi: 10.3389/fpsyt.2021.739698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM. 2020;113(10):707–712. doi: 10.1093/qjmed/hcaa202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh S, Roy D, Sinha K, Parveen S, Sharma G, Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatr Res. 2020 doi: 10.1016/j.psychres.2020.113429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinko L, He Y, Kishton R, Ortiz R, Jacobs L, Fingerman M. “The stay at home order is causing things to get heated up”: family conflict dynamics during COVID-19 from the perspectives of youth calling a national child abuse hotline. J Family Violence. 2021 doi: 10.1007/s10896-021-00290-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sowmya AV, Singh P, Samudra M, Javadekar A, Saldanha D. Impact of COVID-19 on obsessive-compulsive disorder: a case series. Ind Psychiatry J. 2021;30(Suppl 1):S237–S239. doi: 10.4103/0972-6748.328818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stocker D, Jäggi J, Liechti L, Schläpfer D, Németh P, Künzi K (2021) Der Einfluss der COVID-19-Pandemie auf die psychische Gesundheit der Schweizer Bevölkerung und die psychiatrisch-psychotherapeutische Versorgung in der Schweiz. Schlussbericht. Bern: Bundesamt für Gesundheit.
- Tanir Y, Karayagmurlu A, Kaya İ, Kaynar TB, Türkmen G, Dambasan BN, Meral Y, Coşkun M. Exacerbation of obsessive compulsive disorder symptoms in children and adolescents during COVID-19 pandemic. Psychiatry Res. 2020;293:113363. doi: 10.1016/j.psychres.2020.113363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor ZE, Bailey K, Herrera F, Nair N, Adams A. Strengths of the heart: stressors, gratitude, and mental health in single mothers during the COVID-19 pandemic. J Fam Psychol. 2022;36(3):346–357. doi: 10.1037/fam0000928. [DOI] [PubMed] [Google Scholar]
- Thompson EC, Thomas SA, Burke TA, Nesi J, MacPherson HA, Bettis AH, Wolff JC. Suicidal thoughts and behaviors in psychiatrically hospitalized adolescents pre-and post-COVID-19: a historical chart review and examination of contextual correlates. J Affective Disord Rep. 2021;4:100100. doi: 10.1016/j.jadr.2021.100100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tseng H-W, Tsai C-S, Chen Y-M, Hsiao RC, Chou F-H, Yen C-F. Poor mental health in caregivers of children with attention-deficit/hyperactivity disorder and its relationships with caregivers’ difficulties in managing the children’s behaviors and worsened psychological symptoms during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(18):9745. doi: 10.3390/ijerph18189745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Loon AWG, Creemers HE, Vogelaar S, Miers AC, Saab N, Westenberg PM, Asscher JJ. Prepandemic risk factors of COVID-19-related concerns in adolescents during the COVID-19 pandemic. J Res Adolesc. 2021;31(3):531–545. doi: 10.1111/jora.12651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vicari S, Pontillo M. Developmental psychopathology in the COVID-19 period. COVID-19 pandemic impact on children and adolescents’ mental health. Psychiatr Danub. 2021;33(11):33–35. [PubMed] [Google Scholar]
- Wang L, Li D, Pan S, Zhai J, Xia W, Sun C, Zou M. The relationship between 2019-nCoV and psychological distress among parents of children with autism spectrum disorder. Glob Health. 2021;17(1):1–14. doi: 10.1186/s12992-020-00651-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang MT, Henry DA, Scanlon CL, Del Toro J, Voltin SE (2022) Adolescent psychosocial adjustment during COVID-19: an intensive longitudinal study. J Clin Child Adolesc Psychol 1–16. 10.1080/15374416.2021.2007487 [DOI] [PubMed]
- Werling AM, Walitza S, Drechsler R. Impact of the COVID-19 lockdown on screen media use in patients referred for ADHD to child and adolescent psychiatry: an introduction to problematic use of the internet in ADHD and results of a survey. J Neural Transm. 2021 doi: 10.1007/s00702-021-02332-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werling AM, Walitza S, Drechsler R (2021b) Einfluss des Lockdowns auf Psyche und Mediengebrauch in der Kinder- und Jugendpsychiatrie. Paediatrica 32(2):27–32. 10.35190/d2021.2.5
- Werling AM, Walitza S, Gerstenberg M, Grünblatt E, Drechsler R. Media use and emotional distress under COVID-19 lockdown in a clinical sample referred for internalizing disorders: a Swiss adolescents’ perspective. J Psychiatr Res. 2022;147:313–323. doi: 10.1016/j.jpsychires.2022.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werling AM, Walitza S, Eliez S, Drechsler R. The impact of the COVID-19 pandemic on mental health care of children and adolescents in switzerland: results of a survey among mental health care professionals after one year of COVID-19. Int J Environ Res Public Health. 2022;19(6):3252. doi: 10.3390/ijerph19063252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wirkner J, Christiansen H, Knaevelsrud C, Lüken U, Wurm S, Schneider S, Brakemeier E-L. mental health in times of the covid-19 pandemic. Eur Psychol. 2022;26:310–322. doi: 10.1027/1016-9040/a000465. [DOI] [Google Scholar]
- Woolford SJ, Sidell M, Li X, Else V, Young DR, Resnicow K, Koebnick C. Changes in body mass index among children and adolescents during the COVID-19 pandemic. JAMA J Am Med Assoc. 2021 doi: 10.1001/jama.2021.15036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zetterqvist M, Jonsson LS, Landberg Å, Svedin CG. A potential increase in adolescent nonsuicidal self-injury during covid-19: A comparison of data from three different time points during 2011–2021. Psychiatry Res. 2021 doi: 10.1016/j.psychres.2021.114208. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.