Edema is a rare complication of insulin administration most often seen in patients with type 1 diabetes at the initiation of insulin therapy (1–6) or, less commonly, with intensification of insulin treatment (6–9). It has also been reported in patients with type 2 diabetes when insulin is administered in conjunction with thiazolidinediones (10). The presentation is typically mild and self-limited but can vary from isolated lower-extremity edema to, rarely, anasarca with severe cardiopulmonary congestion (3,4,11,12). The mechanism of this edema is not definitively understood, but it has been attributed to increased capillary permeability secondary to the catabolic state caused by insulin deficiency. Insulin administration then inhibits natriuresis, resulting in edema (2). It is a diagnosis of exclusion, and common etiologies of edema should be investigated through diagnostic workup. Here, we report a severe case of prolonged insulin edema that was refractory to standard treatment in a pediatric patient with known type 1 diabetes following insulin infusion for diabetic ketoacidosis (DKA) and subsequent intensification of insulin therapy.
Case Presentation
A 14-year-old girl with a 3-year history of inadequately controlled type 1 diabetes (A1C ≥14% over the previous 2.5 years) presented to the emergency department after 4 days of progressing dyspnea and lower-extremity edema following hospital discharge for treatment of severe DKA (venous blood gas pH 6.86 and serum bicarbonate <5 mmol/L). She received a 1-L normal saline fluid bolus and then was treated with an insulin drip and 3/4 normal saline intravenous (IV) fluids with varying dextrose and potassium content via a two-bag system administered at 1.5 times the maintenance rate. Treatment continued for ∼24 hours to correct the DKA. She also required one dose of IV potassium acetate (16 mEq) and IV potassium phosphate (17 mmol) supplementation for hypokalemia and hypophosphatemia. Because of her history of persistent A1C elevation, the consulting endocrinology attending and fellow physicians counseled the family on adherence to home diabetes management (i.e., a multiple daily injection regimen of insulins glargine and lispro). The morning after discharge, she woke with periorbital edema followed by lower-extremity edema. Over 1 day, her symptoms progressed to include orthopnea with pleuritic chest pain and abdominal pain with distention. She presented to the emergency department and was admitted for severe edema.
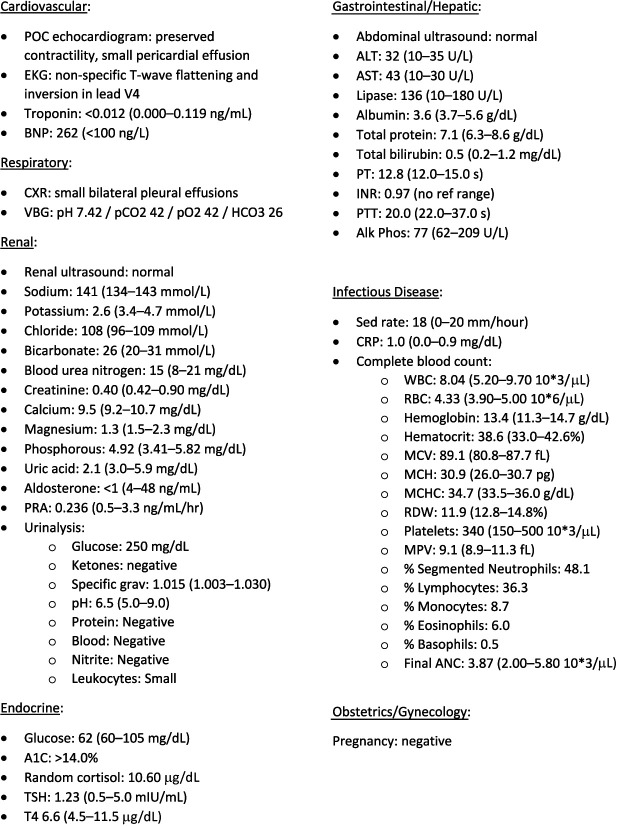
Her vital signs at presentation revealed a 22-lb (10-kg) weight gain since her recent admission for DKA, during which she weighed 125 lb (56.7 kg). She was afebrile, tachycardic (heart rate 113 bpm), tachypneic (respiratory rate 29 bpm), and hypertensive (blood pressure 147/96 mmHg). She had diminished breath sounds at lung bases, abdominal distention with generalized tenderness but no fluid wave, and tender, 1+ pitting edema of the bilateral lower extremities. She underwent evaluation for common etiologies of edema with reassuring results. Specifically, no abnormalities were seen in serum troponin level, cardiac silhouette, cardiac rhythm, or ventricular size or contractility, which suggested against cardiac etiologies, including heart failure. B-type natriuretic peptide was elevated, attributed to fluid overload. Lack of significant hypoalbuminemia with no protein or blood on urinalysis reassured against nephritic and nephrotic syndromes. Additionally, renal function tests were normal, and aminotransferases showed only mild elevation in AST. Other pertinent findings included pleural and pericardial effusions, hypokalemia, and an A1C >14%. Given reassuring workup for other causes of edema, the diagnosis of insulin edema was made. Detailed results are reported in Figure 1.
FIGURE 1.
Laboratory and imaging results by system. Alk Phos, alkaline phosphatase; ANC, absolute neutrophil count; BNP, B-type natriuretic peptide; CRP, C-reactive protein; CXR, chest X-ray; EKG, electrocardiogram; grav, gravity; HCO3, bicarbonate; INR, international normalized ratio; MCH, mean corpuscular hemoglobin; MCHC, mean corpuscular hemoglobin concentration; MCV, mean corpuscular volume; MPV, mean platelet volume; POC, point-of-care; PTT, partial thromboplastin time; RBC, red blood count; RDW, red cell distribution width; PRA, plasma renin activity; PT, prothrombin time; Sed, sedimentation; T4, thyroxine; TSH, thyroid-stimulating hormone; VBG, venous blood gases; WBC, white blood count.
Given the severity of presentation, conservative management with only fluid and salt restriction was not appropriate. Nephrology was consulted and assisted with diuresis. Hypokalemia was corrected during hospitalization with oral (40 mEq) and IV (20 mEq) potassium supplementation. Treatment with IV furosemide (25 mg daily) resulted in 5 L of urine output on day 1, with improvement in edema and cardiopulmonary symptoms. The hypertension resolved, and discharge weight after the 2-day hospitalization showed a 12-lb (5.4-kg) weight loss. She was discharged with daily oral furosemide (40 mg/day) and dietary sodium restriction (<2 g/day).
During follow-up with her primary care physician, persistent ankle edema prompted an increase in furosemide to 80 mg daily. Nine days after discharge, she developed facial and neck edema despite the increased furosemide dose and was readmitted to the hospital. She again reported chest pain but denied abdominal pain. Workup remained reassuring, except for a CT scan of the abdomen/pelvis showing malrotation of the jejunum and ileum with abnormal orientation of the superior mesenteric artery and vein, without bowel wall edema. She had no symptoms related to the malrotation, and the surgical team determined it to be an incidental finding. She received IV furosemide 60 mg twice daily on hospitalization day 1 and then transitioned to oral furosemide 120 mg daily with appropriate diuresis. She was discharged after 5 days with furosemide 80 mg daily and continued dietary sodium restriction.
At follow-up with nephrology 10 days after discharge, she was normotensive with normal heart rate but had persistent lower-extremity edema, and her weight remained above baseline at 139 lb (63.1 kg). Because of the persistent edema, 12.5 mg of oral hydrochlorothiazide was added to her daily diuretic regimen. One month later, the edema was completely resolved. She then underwent surgical correction of the malrotation, at which time her weight was similar to that of her initial presentation (145 lb [65.8 kg]), but without edema. Additionally, her A1C had improved to 8.7%. After surgery, the patient discontinued the diuretic medications and the salt-restricted diet. She was evaluated by nephrology 1 month later and found to have no edema on exam.
Questions
What workup is needed in the setting of severe edema in youth with type 1 diabetes, and how is insulin edema diagnosed?
What causes insulin edema in youth with type 1 diabetes, including those with longstanding diabetes?
How is treatment of insulin edema different in severe presentations?
Commentary
Edema is an underreported complication of insulin therapy. It was first described in 1928 following initiation of insulin (1) and has since been described in both adult and pediatric patients after initiation of insulin or intensification of insulin therapy such as when starting an insulin pump (11). It is most often reported in type 1 diabetes but is also described in type 2 diabetes when insulin is used in conjunction with thiazolidinediones (10), which act to increase insulin sensitivity. It is more common in females than males (8,9,13), although it has been reported in both.
Insulin edema is a diagnosis of exclusion, so common etiologies of edema should be considered and workup should include standard diagnostics based on the presentation. Symptoms typically include mild, self-limiting lower-extremity edema, but it can rarely present with significant severity such as in this case with anasarca and cardiopulmonary congestion (3,5,11). Resolution often occurs within 2 weeks with no treatment or conservative treatment of fluid and salt restriction (3,8,14). Severe presentations may require treatment with diuretic medications (2,7,8,12), and insulin edema has shown response to many types of diuretics. A 2004 case report by Kalambokis et al. (7) recommended spironolactone because of associated hyperaldosteronism, but hyperaldosteronism is not consistent across all reports of insulin edema.
The mechanism of insulin edema is not definitively understood, but many hypotheses exist. First, insulin’s action at renal proximal tubules encourages sodium retention via the sodium–potassium ATP pump and the sodium–hydrogen exchanger 3 (2,8). Other hypotheses include refeeding edema, as the catabolic state in insulin deficiency mirrors that seen in anorexia nervosa (4,8,12,14). Upon refeeding with carbohydrates, the resultant decrease in glucagon inhibits distal tubule natriuresis (2). Finally, chronic stress during prolonged insulin deficiency may cause dysfunctional release of hypothalamic gonadotropin-releasing hormone (GnRH). Once the catabolic state is corrected via insulin, GnRH secretion normalizes, resulting in increased endothelial growth factors and subsequent capillary vasodilation and edema (2,8).
Our patient’s improvement in A1C from ≥14 to 8.7% was the first A1C decrease in more than 2 years and reflects new adherence to insulin treatment. This result supports the diagnosis of insulin edema and may explain her prolonged, refractory treatment course. Additionally, weight gain is an established side effect of insulin therapy. The improved A1C with resolution of edema suggests that her persistent weight gain was true mass gain as a result of adherence to insulin therapy rather than evidence of a return of edema, which is consistent with other case reports (2,8,13).
According to a 2020 literature review from Sawalha and Geddie (15), there are only 24 published cases of insulin edema in the pediatric population, and reports of severe cases are rare across all age-groups. Ours is the first case of a pediatric patient with known inadequately controlled type 1 diabetes presenting with severe, persistent insulin edema that occurred after treatment with an insulin drip for severe DKA. In this case, the edema persisted for more than 2 months, resulted in multiple hospital admissions, and required treatment with fluid and salt restriction, IV and oral diuretics, and ultimately an outpatient regimen of two diuretic agents to achieve resolution. This case serves to increase awareness and knowledge of this complication for both endocrinologists and primary care providers, including the potential causes, range of severity of presentation, and possible treatment modalities.
Clinical Pearls
Edema is a rare complication of insulin therapy, usually seen after initiation of insulin therapy at diagnosis of type 1 diabetes.
Insulin edema most often presents as mild, self-limiting lower-extremity edema, sometimes requiring salt and fluid restriction.
Severe presentations of insulin edema, including anasarca and cardiopulmonary congestion, are rare but can occur.
Insulin edema may occur after treatment of DKA with insulin infusion in patients with known type 1 diabetes and a history of poor adherence to the insulin regimen.
Insulin edema may be refractive and require combination therapy with multiple diuretics, as well as salt and fluid restrictions, to achieve resolution.
Article Information
Acknowledgment
Written informed consent was obtained from the patient’s parent/legal guardian for publication of this case report.
Funding
E.C.C. is funded by National Institutes of Health grants NIH K12DK094712, and M.E.P. is funded by NIH 5T32DK063687-18.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Author Contributions
M.E.P. drafted the manuscript. All authors conceptualized the article, reviewed and revised the manuscript, and approved the final manuscript as submitted. M.E.P. is the guarantor of this work and, as such, had full access to all the data and takes responsibility for the integrity and accuracy of this work.
References
- 1. Leifer A. A case of insulin edema. JAMA 1928;90:610–611 [Google Scholar]
- 2. Kalambokis GN, Tsatsoulis AA, Tsianos EV. The edematogenic properties of insulin. Am J Kidney Dis 2004;44:575–590 [PubMed] [Google Scholar]
- 3. Shaper AG. The insulin-oedema syndrome in African diabetic subjects. Trans R Soc Trop Med Hyg 1966;60:519–525 [DOI] [PubMed] [Google Scholar]
- 4. Ehrlich S, Querfeld U, Pfeiffer E. Refeeding oedema: an important complication in the treatment of anorexia nervosa. Eur Child Adolesc Psychiatry 2006;15:241–243 [DOI] [PubMed] [Google Scholar]
- 5. Derya Bulus A, Andiran N, Osman Köksal A. Insulin edema in type 1 diabetes mellitus: report of a case and brief review of the literature. Iran J Pediatr 2016;26:e5077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Aravamudhan A, Gardner C, Smith C, Senniappan S. Insulin oedema in a child with newly diagnosed diabetes mellitus. Eur J Pediatr 2014;173:685–687 [DOI] [PubMed] [Google Scholar]
- 7. Kalambokis G, Tsatsoulis A, Economou G, Tsianos EV. A case of insulin edema with inappropriate hyperaldosteronism. J Endocrinol Invest 2004;27:957–960 [DOI] [PubMed] [Google Scholar]
- 8. Wong M, Balakrishnan T. Anasarca in newly diagnosed type 1 diabetes: review of the pathophysiology of insulin edema. Cureus 2020;12:e7234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rostami P, Sotoudeh A, Nakhaeimoghadam M, Rabbani A, Rezaei N. Insulin edema in a child with diabetes mellitus type 1. Turk J Pediatr 2012;54:309–311 [PubMed] [Google Scholar]
- 10. Mudaliar S, Chang AR, Henry RR. Thiazolidinediones, peripheral edema, and type 2 diabetes: incidence, pathophysiology, and clinical implications. Endocr Pract 2003;9:406–416 [DOI] [PubMed] [Google Scholar]
- 11. Greco D. Severe weight gain and generalized insulin edema after the starting of an insulin pump. Can J Diabetes 2015;39:21–23 [DOI] [PubMed] [Google Scholar]
- 12. Lee P, Kinsella J, Borkman M, Carter J. Bilateral pleural effusions, ascites, and facial and peripheral oedema in a 19-year-old woman 2 weeks following commencement of insulin lispro and detemir: an unusual presentation of insulin oedema. Diabet Med 2007;24:1282–1285 [DOI] [PubMed] [Google Scholar]
- 13. Chelliah A, Burge MR. Insulin edema in the twenty-first century: review of the existing literature. J Investig Med 2004;52:104–108 [Google Scholar]
- 14. Hirshberg B, Muszkat M, Marom T, Shalit M. Natural course of insulin edema. J Endocrinol Invest 2000;23:187–188 [DOI] [PubMed] [Google Scholar]
- 15. Sawalha N, Geddie H. Insulin edema associated with newly diagnosed type 1 diabetes and high glycated hemoglobin: a case and review of the pediatric literature. Can J Diabetes 2021;45:571–574 [DOI] [PubMed] [Google Scholar]