Abstract
Introduction/Objectives:
COVID-19 vaccination is important to stop the pandemic. It has been reported that willingness to be vaccinated is associated with system factors as well as individual attitudes and beliefs. Primary care patients include individuals at increased risk of poor outcomes after COVID-19 infection, such as elderly people and those with comorbidities. This study investigated attitudes in this population toward COVID-19 and COVID-19 vaccination, including willingness to be vaccinated and associated factors. This study was conducted in Japan, where the population has low vaccine confidence, during the initial phase of COVID-19 vaccination.
Methods:
Patients from 1 primary care clinic in Kitaibaraki City, Ibaraki, Japan, participated in this study from March to April 2021. They were administered a self-reported questionnaire exploring factors such as willingness to undergo COVID-19 vaccination, perceived susceptibility, and perceived vaccine efficacy. Multivariable logistic regression analysis was conducted to identify factors associated with vaccination.
Results:
Of the 717 patients (response rate, 88.3%), 512 (70.0%) reported they were willing to be vaccinated for COVID-19. Multivariate analysis revealed that vaccination willingness was associated with older age (odds ratio [OR] 1.03, 95% confidence interval [CI] 1.01-1.05), male gender (OR 1.95, 95% CI 1.15-3.30), influenza vaccination in in the 2020/2021 season (OR 2.54, 95% CI 1.49-4.32), recommendation from others (OR 3.11, 95% CI 1.58-6.18), high perceived susceptibility (OR 2.51, 95% CI 1.45-4.33), belief in vaccine efficacy (OR 3.83, 95% CI 1.54-9.56), high perceived susceptibility to vaccine-related adverse events (OR 0.37, 95% CI 0.22-0.64), and high espousal of social norms (OR 8.00, 95% CI 2.78-23.0).
Conclusions:
COVID-19 vaccination was widely acceptable to Japanese primary care patients. In addition to factors such as vaccine efficacy, and past influenza vaccination, social norms may be important in determining COVID-19 vaccination willingness.
Keywords: vaccination, vaccine acceptance, COVID-19, primary care patients
Introduction
COVID-19 vaccines have been rapidly approved with the ultimate purpose of stopping the epidemic. By March 2022, 64.4% of the world population had received at least 1 dose of a COVID-19 vaccine. 1 COVID-19 vaccination began as early as December 2020 in countries such as Israel, the United Kingdom, and the United States. In Japan, vaccination for health care workers began in February 2021, and for the elderly it was initiated on April 12, 2021.
Previous studies in countries other than Japan, as well as those in Japan before COVID-19 vaccination had started, reported that 60% to 70% of individuals were willing to receive COVID-19 vaccines,2-4 although the percentage was lower in countries such as Jordan and Kuwait. 5 Willingness to be vaccinated was associated with individual attitudes and beliefs, like perceived susceptibility 6 and opinions regarding vaccine efficacy. 7 Similar findings were reported in studies that investigated factors associated with influenza vaccination. 8 Since most research on receptiveness to COVID-19 vaccination targeted general populations and consisted of internet surveys, study populations were generally limited to young and healthy individuals whose characteristics differed from those of primary care patients.
It has also been reported that system factors like costs, access, and delivery are associated with vaccination. 9 The characteristics of COVID-19 vaccines and the methods by which they are delivered in Japan differ from those of other adult vaccines. In addition, unlike other vaccines, COVID-19 vaccines are based on mRNA technology. In Japan, people can usually get non-COVID-19 vaccines at any medical facility and do not necessarily have to make an appointment in advance. In contrast, COVID-19 vaccines are administered only at designated medical facilities or other specific locations like public halls, and appointments are required. Other adult vaccines are not free, whereas COVID-19 vaccination is free if individuals present the relevant coupon that was mailed to their home. Although these difference may influence patients’ willingness to get vaccinated, they were not always investigated in previous studies in Japan.2,10
Our study focused on primary care patients, many of whom are elderly or have comorbidities. It is particularly important for this population to be vaccinated against COVID-19, because their risks of poor outcomes and death from COVID-19 are higher than those of the general population. 11
It has been reported that Japanese have low vaccine confidence compared to populations in other countries, which might have led to the human papillomavirus vaccine safety scares in 2013. 12 Many primary care patients may have had negative perceptions and attitudes toward COIVD-19 vaccination when it was being initiated in the general population. The purpose of this study was to investigate perceptions and attitudes regarding COVID-19 and its vaccination, as well as willingness to undergo COVID-19 vaccination and associated factors, immediately before COVID-19 vaccination was started.
Methods
Study Design and Settings
This cross-sectional study was conducted on 20 weekdays between March and April in 2021. Study participants were recruited from outpatients visitors to the Kitaibaraki Center for Family Medicine in Kitaibaraki City, Ibaraki, Japan. This facility is a clinic that provides primary care. Kitaibaraki City is a rural city located 200 km from Tokyo, with a population of about 41 000. Only 1 patient in the city was diagnosed with COVID-19 during the study period.
Participants
We approached new and existing patients aged 20 years and older who attended the clinic during the study period. Patients were excluded if they had already completed the questionnaire, or if their doctors judged them to be unable to do so because of their general health condition or cognitive function. To minimize the risk of COVID-19 transmission, patients were also excluded if they had symptoms of an upper respiratory disease or gastroenteritis. At the end of the examination performed during each patient’s visit, their doctor explained the study to them. If they agreed to participate, they completed the questionnaire in the waiting room and placed it in a box near the reception desk.
Questionnaire
The questionnaire was self-administered and anonymous, and was written in Japanese. Survey items potentially associated with willingness to undergo COVID-19 vaccination were determined based on previous reviews of factors associated with vaccination for seasonal influenza 13 and pandemic influenza. 14 We also referred to previous research investigating COVID-19 vaccine intention.4,15 To identify factors not referred to in previous studies, we added items derived from our discussions. Our questionnaire addressed basic characteristics, past vaccinations, experience related to COVID-19, willingness to be vaccinated for COVID-19, attitudes and beliefs about COVID-19 and its vaccination, and influences of vaccine characteristics and the delivery system. An English translation is shown in the Supplemental Material.
Basic characteristics included the following items: living with others, smoking status, employment as a healthcare worker or nursing home staff member, self-rated heath, whether the patient had a family doctor and had regular doctors’ visits, and details of comorbidities. Self-rated health was assessed using a 4-point Likert scale: “very good,” “good,” “bad,” and “very bad.” Regarding past vaccination, participants were asked if they had received an influenza vaccine in the 2020/21 season and pneumococcal vaccine (in those aged 65 years and older), and if they had experienced any vaccine-related adverse events.
Questions regarding experience with COVID-19 included whether they or someone close to them had contracted COVID-19, and whether they had previously been tested for COVID-19 or had been considered to be in close contact. Participants were asked if others had recommended that they undergo COVID-19 vaccination; these questions referred separately to doctors and to family or friends. Possible answers were “yes,” “no,” and “don’t know.”
Willingness to be vaccinated for COVID-19 was assessed as follows: “Are you willing to be vaccinated for COVID-19 in the future?” Answer choices were “yes,” “no,” and “not decided.”
Participants were asked if they agreed with several statements about attitudes and beliefs regarding COVID-19 and its vaccination. Examples of the themes that were addressed included perceived susceptibility to COVID-19, efficacy and safety of COVID-19 vaccination, and social norms. Social norms were asked following 3 questions based on previous studies 16,17: “I think my family doctor/family or friends/government and local community expect me to be vaccinated for COVID-19.” The perceived efficacy of vaccination was assessed using 2 items: “I think COVID-19 vaccination will effectively prevent infection or serious outcomes” and “I think COVID-19 vaccination will effectively stop the COVID-19 epidemic.” Possible responses were “strongly agree,” “agree,” “disagree,” and “totally disagree.” Participants were also asked about the information sources they used and which they trusted most, and whether they thought they had sufficient information about COVID-19. Finally, they were asked whether their willingness to be vaccinated against COVID-19 was influenced by the characteristics of COVID-19 vaccines (3 questions) and by factors related to the vaccine delivery system (7 questions). Examples of these topics included the facts that COVID-19 vaccines were not made in Japan, they use new technology, and they would be free. Possible responses were “highly influenced,” “influenced,” “not influenced,” and “not influenced at all.”
Ethical Consideration
This study was conducted in accordance with the Declaration of Helsinki of 1975. Before answer the questionnaire, all participants gave written informed consent. The ethical committee of Kitaibaraki City Hospital approved this study (approval number 0205).
Statistical Methods
To identify factors associated with willingness to undergo COVID-19 vaccination, we defined willingness as the dependent variable. The answers “not decided” and “no” were combined, as in a previous study. 4 All other variables except for regular doctor’s visits, comorbidity details, and the most trusted information source were independent variables. Categorical variables were divided into 2 categories. The answers “don’t know” and “no” were combined. If a participant responded in the affirmative to any of the questions about recommendations by others, vaccine effectiveness, and social norms, then the participant was considered to have been recommended by others to receive a COVID-19 vaccine, to agree that COVID-19 vaccines are effective, or to agree with social norms, respectively. Differences in means were compared using the t-test or Mann-Whitney U test. Differences in proportions were compared using the chi-square test.
Logistic regression analysis was performed to identify additional factors associated with willingness to get a vaccine. The odds ratio (OR) and 95% confidence interval (CI) were calculated. All variables regarding attitudes and beliefs about COVID-19 and its vaccination, as well as influences of vaccine characteristics and delivery systems, were entered into the model simultaneously. Variables concerning basic characteristics, past vaccinations, and experience related to COVID-19 were entered into the model when P < .1 in univariate analysis. If too few participants were enrolled, we did not enter variables missing more than 10% of values. Multicollinearity was considered present if the variance inflation factor (VIF) was more than 10. Model fitness was assessed by the Hosmer-Lemeshow test. The sample size was calculated and aimed to ensure at least 10 events per variable, based on the assumptions that the confidence level was 95%, that 60% of participants would be willing to undergo COVID-19 vaccination, and that the proportion of associated factors was 50%.2,18,19 Statistical significance was defined as P < .05. Data were analyzed using IBM SPSS Statistics version 27.
Results
One thousand seventy-nine patients visited the clinic for the first time during the study period. Of these, 75 patients had symptoms of an upper respiratory disease or gastroenteritis, and 192 patients were judged by their doctors as unable to complete the questionnaire. Eight hundred twenty-three patients were therefore eligible for participation. Of these, 50 declined to participate, 32 did not return the questionnaire, and 13 returned blank questionnaires. We analyzed 717 patients (response rate 88.3%).
The median age was 67.0 years (interquartile range, 21). Of the 717 participants, 53.7% were considered elderly (age 65 years or older) and 54.8% were women. Six-hundred and twenty-one participants (86.6%) regularly visited doctors. Influenza vaccination coverage in the 2020/21 season was 71.1% (Table 1).
Table 1.
Basic Characteristics and Past Vaccinations.
| N = 717 | |
|---|---|
| Age | 67.0 (21) |
| Elderly | 385 (53.7) |
| Missing | 41 (5.7) |
| Sex | |
| Men | 292 (40.7) |
| Women | 393 (54.8) |
| Living with others | 587 (81.9) |
| Current smoker | 116 (16.2) |
| Employed as a healthcare professional | 22 (3.1) |
| Employed as nursing home staff member | 38 (5.3) |
| Self-rated health | |
| Very good | 197 (27.5) |
| Good | 396 (55.2) |
| Bad | 84 (11.7) |
| Very bad | 5 (0.7) |
| Has a family doctor | 621 (86.6) |
| Regular doctors’ visits | 635 (88.6) |
| Comorbidity | |
| Heart disease | 225 (35.4) |
| Diabetes | 121 (19.1) |
| Respiratory disease | 45 (7.1) |
| Malignancy | 21 (3.3) |
| Influenza vaccination in 2020/21 season | 510 (71.1) |
| Past pneumococcal vaccination (age ≥65 years) | 212 (55.1) |
| Past vaccine-related adverse event | 35 (5.2) |
Age is shown as median (interquartile range), and other variables are shown as n (%). Heart disease includes hypertension.
Five hundred two participants (70.0%) reported they were willing to undergo COVID-19 vaccination, 138 (19.2%) had not yet decided, 20 (2.8%) were unwilling, and 57 (7.9%) did not answer. One hundred eighty three participants (25.5%) were recommended from others; only 65 participants (9.1%) had been advised by doctors to be vaccinated, whereas 158 (22.0%) had been advised by family or friends. No participants had been diagnosed with COVID-19. Two (0.3%) had been designated as close contacts of individuals with COVID-19. Forty-two participants (5.9%) had previously been tested for COVID-19.
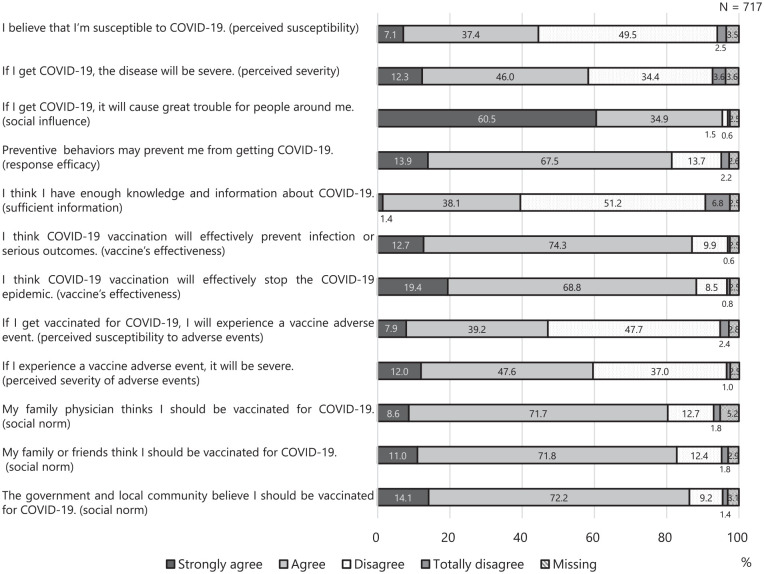
Six hundred eighty-four participants (95.4%) agreed with the statement “If I get COVID-19, it will cause great trouble for people around me.” Most participants believed that vaccination would prevent them from contracting COVID-19 (87.0%) and would stop the epidemic (88.2%). Participants agreed that family doctors (80.3%), family and friends (82.8%), and the government and local community (86.3%) expected them to undergo COVID-19 vaccination (Figure 1). The most popular information source about COVID-19 and its vaccination was television (94.0%), followed by newspapers (51.0%), Internet (32.2%), and family or friends (30.3%). Of these, the most trusted information source was television (60.1%).
Figure 1.
Attitudes toward and beliefs about COVID-19 vaccination.
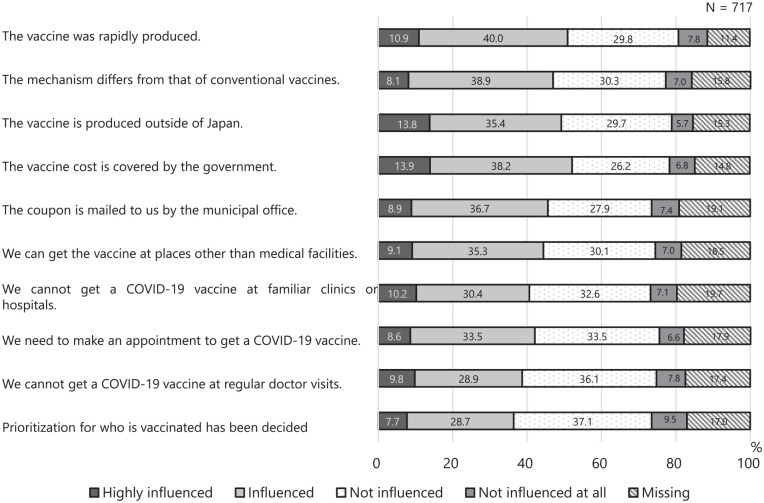
Figure 2 shows the results of questions asking whether COVID-19 vaccine characteristics and delivery system factors influenced decision-making about COVID-19 vaccination. More than half of all participants reported being influenced by all of the questions regarding vaccine characteristics and vaccination policy, for example “COVID-19 vaccines were rapidly developed.”
Figure 2.
Influence of COVID-19 vaccine characteristics and delivery system factors on vaccination willingness.
Table 2 shows the results of univariate analysis. Older participants, current smokers, having a family doctor, regular doctors’ visits, good self-rated health, and influenza vaccination in the 2020/21 season were associated with willingness to undergo COVID-19 vaccination. Participants who had been advised by others (doctors, or family or friends) to be vaccinated were more likely to be willing than those who had not received such advice (31.5% vs 9.8%, respectively; P < .001). Willing participants were more likely than those who were unwilling to agree to the statements about social norms (98.4% vs 81.4%, respectively; P < .001) and vaccine effectiveness (98.0% vs 77.7%, respectively; P < .001). Willing participants were less likely to agree to the statement about perceived susceptibility of adverse events (41.6% vs 69.7%, respectively; P < .001). Finally, willing participants were less influenced by the following statements than those who were unwilling: “COVID-19 vaccines were rapidly developed” (54.3% vs 69.3%, respectively; P = .002), “COVID-19 vaccines are produced outside of Japan” (54.0% vs 73.7%, respectively; P < .001), and “We cannot get COVID-19 vaccines at familiar clinics or hospitals” (47.1% vs 60.3%, respectively; P = .008) (Table 2).
Table 2.
Factors Associated With Vaccination Willingness (Univariate Analysis).
| n | Willing to get COVID-19 vaccine (n, %) | Unwilling to get vaccine/not decided (n, %) | P-value | |
|---|---|---|---|---|
| Basic characteristics | ||||
| Age (median, interquartile range) | 650 | 68.0 (17) | 56.5 (30) | <.001* |
| Sex | ||||
| Male | 658 | 227 (45.3) | 59 (37.6) | .088 |
| Living with others | 634 | 413 (85.7) | 132 (86.8) | .72 |
| Current smoker | 635 | 68 (14.1) | 41 (27.0) | <.001 |
| Having family physician | 627 | 443 (93.1) | 128 (84.8) | .002 |
| Regular visits | 630 | 455 (94.8) | 131 (87.3) | .002 |
| Self-rated health | ||||
| Good | 629 | 431 (89.8) | 117 (78.5) | <.001 |
| Working as healthcare professional | 627 | 14 (2.9) | 4 (2.6) | .55 |
| Working as nursing home staff member | 626 | 24 (5.0) | 9 (6.1) | .61 |
| Past experience related to vaccine | ||||
| Influenza vaccination in 2020/21 season | 660 | 391 (77.9) | 81 (51.3) | <.001 |
| Past pneumococcal vaccination (for age 65 years and older) | 346 | 183 (61.4) | 24 (50.0) | .14 |
| Experience of vaccine adverse event | 660 | 24 (4.8) | 10 (6.3) | .44 |
| Past experience related to COVID-19 | ||||
| Ever tested for COVID-19 | 660 | 31 (6.2) | 8 (5.1) | .61 |
| Ever designated a close contact of COVID-19 | 660 | 2 (0.4) | 0 (0.0) | 1.0 † |
| People around you have history of COVID-19 diagnosis | 660 | 16 (3.2) | 9 (5.7) | .15 |
| Recommendation from others | 648 | 156 (31.5) | 15 (9.8) | <.001 |
| Information source (multiple choice) | ||||
| Television | 646 | 478 (97.2) | 149 (96.8) | .79 † |
| Newspaper | 284 (57.7) | 52 (33.8) | <.001 | |
| Magazine | 31 (6.3) | 5 (3.2) | .15 | |
| Internet | 158 (32.1) | 60 (39.0) | .12 | |
| Hospital or Clinic | 70 (14.2) | 18 (11.7) | .42 | |
| City or Prefecture | 79 (16.1) | 30 (19.5) | .32 | |
| Family or Friends | 160 (32.5) | 46 (29.9) | .54 | |
| Attitudes and beliefs about COVID-19 and its vaccine | ||||
| Perceived susceptibility | 650 | 243 (49.2) | 57 (36.5) | .006 |
| Perceived severity | 651 | 309 (62.6) | 85 (54.1) | .06 |
| Social influence | 657 | 495 (99.0) | 148 (94.3) | <.001 † |
| Response efficacy | 656 | 425 (85.0) | 123 (78.8) | .07 |
| Sufficient information | 653 | 217 (43.7) | 39 (25.0) | .011 |
| Vaccine’s effectiveness | 658 | 491 (98.0) | 122 (77.7) | <.001 |
| Perceived susceptibility to adverse event | 650 | 206 (41.6) | 108 (69.7) | <.001 |
| Perceived severity of adverse events | 652 | 272 (54.6) | 128 (83.1) | <.001 |
| Social norm | 655 | 491 (98.4) | 127 (81.4) | <.001 |
| Influence of COVID-19 vaccine properties | ||||
| The vaccines were rapidly produced | 588 | 245 (54.3) | 95 (69.3) | .002 |
| The vaccines’ mechanism differs from those of conventional vaccines | 562 | 226 (52.7) | 88 (66.2) | .006 |
| The vaccines are produced outside of Japan | 563 | 232 (54.0) | 98 (73.7) | <.001 |
| Influence of system factors | ||||
| The vaccine cost is covered by government | 568 | 269 (62.1) | 81 (60.0) | .66 |
| The coupon is mailed to us by the municipal office | 544 | 240 (58.1) | 72 (55.0) | .53 |
| We can get a COVID-19 vaccine at places other than medical facilities | 548 | 229 (55.2) | 69 (51.9) | .51 |
| We cannot get a COVID-19 vaccine at familiar clinics or hospitals | 539 | 192 (47.1) | 79 (60.3) | .008 |
| We need to make an appointment to get a COVID-19 vaccine | 549 | 208 (50.1) | 73 (54.5) | .38 |
| We cannot get a COVID-19 vaccine at regular doctor visits | 552 | 183 (44.0) | 73 (53.7) | .049 |
| Prioritization for who is vaccinated has been decided | 554 | 175 (41.8) | 65 (48.1) | .19 |
Mann-Whitney U test.
Fisher’s exact test.
To assess variables associated with willingness to undergo COVID-19 vaccination, we used a logistic regression model. The statement “If I get COVID-19, it will cause great trouble for people around me” was agreed upon by more than 90% of patients in both groups, so we did not enter this as a variable. Between 11% and 19% of values were missing for questions about the influence of vaccine characteristics and delivery system factors, while the other questions were missing less than 5% of values. Our sample size was small, so we did not include the former questions as variables in the logistic regression analysis.
Table 3 shows the results of multivariate analysis. Multicollinearity was not observed (VIF < 10). The Hosmer-Lemeshow test showed good model fit (X2 = 9.57, df = 8, P = .30). Willingness to undergo COVID-19 vaccination was associated with older age (OR 1.03, 95% CI 1.01-1.05), male gender (OR 1.95, 95% CI 1.15-3.30), good self-rated health (OR 2.17, 95% CI 1.07-4.12), influenza vaccination in the 2020/21 season (OR 2.54, 95% CI 1.49-4.32), recommendation by others (OR 3.11, 95% CI 1.58-6.18), high perceived susceptibility (OR 2.51, 95% CI 1.45-4.33), belief in vaccine efficacy (OR 3.83, 95% CI 1.54-9.56), and high espousal of social norms (OR 8.00, 95% CI 2.78-23.0). Willingness to undergo COVID-19 vaccination was negatively associated with high perceived susceptibility to vaccine-related adverse events (OR 0.37, 95% CI 0.22-0.64) and high perceived severity of vaccine-related adverse events (OR 0.23, 95% CI 0.13-0.43).
Table 3.
Factors Associated With Willingness to Undergo COVID-19 Vaccination (Multivariate Analysis, n = 585).
| Odds ratio | 95% CI | ||
|---|---|---|---|
| Age | 1.03 | 1.01 | 1.05 |
| Sex (female = 0) | 1.95 | 1.15 | 3.30 |
| Current smoker | 0.65 | 0.35 | 1.22 |
| Has family doctor | 0.84 | 0.36 | 1.96 |
| Self-rated health (bad = 0) | 2.11 | 1.07 | 4.18 |
| Influenza vaccination in the 2020/21 season | 2.54 | 1.49 | 4.32 |
| Recommendation by others | 3.11 | 1.56 | 6.18 |
| Get information from newspaper | 1.15 | 0.68 | 1.94 |
| High perceived susceptibility | 2.51 | 1.45 | 4.33 |
| High perceived severity | 1.08 | 0.62 | 1.89 |
| Response efficacy | 1.30 | 0.68 | 2.48 |
| Sufficient information | 0.97 | 0.57 | 1.66 |
| High vaccine effectiveness | 3.84 | 1.54 | 9.56 |
| High perceived susceptibility of adverse event | 0.37 | 0.22 | 0.64 |
| High perceived severity of adverse event | 0.23 | 0.13 | 0.43 |
| High espousal of social norms | 8.00 | 2.78 | 23.0 |
Abbreviation: 95% CI, 95% confidence interval.
Discussion
In our study, 70% of the participants (502 of 717) were willing to undergo COVID-19 vaccination. This rate is higher than those reported in previous Japanese studies, specifically; 1 study conducted in September 2020 2 and 3 studies conducted between January and March 2021.10,20,21 One hundred thirty-eight participants (19.2%) reported they were not sure if they would be vaccinated, and 32 (4.5%) did not respond. One study from the United States in April 2020 15 and 1 from Japan in September 2020 2 used the same response options as our study, while 31.6% and 22.0% of participants in these studies, respectively, answered “not sure.” Only 20 participants (2.8%) in our study reported that they were unwilling to undergo COVID-19 vaccination, which is a lower rate than in the aforementioned Japanese studies and in studies from other countries.7,22 There are 2 possible reasons for this discrepancy. First, vaccination willingness was reported to be higher in elderly individuals 21 and those with any comorbidities.4,23 Our participants consisted of primary care patients and about half of them were elderly, so the likelihood of vaccination willingness was relatively high. Second, our study was conducted just as COVID-19 vaccination was beginning in Japan, and momentum behind vaccination was increasing; these facts may have contributed to higher vaccination willingness than in previous Japanese studies.
In our study, participants who believed that others expected them to be vaccinated—in other words, participants who espoused social norms—were more likely to be willing to undergo COVID-19 vaccination than those who did not. Social norms are classified as either descriptive or injunctive norms. 24 Descriptive norms refer to beliefs about what is actually done by others in one’s social group, while injunctive norms refer to beliefs about what should be done. 24 An example of a descriptive norm is “I should be vaccinated because everyone around me is vaccinated,” while a related injective norm is “I should be vaccinated because I am expected to do so.” Generally, the combination of both descriptive and injunctive norms results in the highest compliance. 25 As for COVID-19 vaccination, there have been mixed results; 1 study investigated only injunctive norms and found that they were associated with the willingness to be vaccinated, 26 while other studies showed that this willingness was related to descriptive norms but not injunctive norms.27,28 COVID-19-related social norms that affect behavioral outcomes are formed via direct experience, symbolically through media, or through the imagination. 29 Few participants in our study had direct experience with COVID-19, so their norms were most likely based on their interaction with the media and people around them. Our study asked only about an injunctive norm. By clarifying how descriptive and injunctive norms are formed and how they influence the willingness to undergo COVID-19 vaccination, future research will identify methods of increasing vaccination willingness.
Our study revealed that recommendations from family doctors or family and friends was also associated with willingness to be vaccinated. Consistent with the results of previous studies on the influence of doctors30,31 or family/friends,32,33 the recommendations of others seem to be an important factor impacting COVID-19 vaccine-related decision making in primary care patients.
Participants who rated their health status as good or very good were likely to be willing to undergo COVID-19 vaccination. In contrast, a study of the general population in Portugal reported that those who rated their health status as poor were more likely to accept COVID-19 vaccination. 34 Several reports on influenza vaccination in general populations or outpatients revealed that poor self-rated health status was associated with increased willingness to receive an influenza vaccine.13,35 Participants who rated their health as poor may not have been able to determine whether newly introduced COVID-19 vaccines were safe given their health conditions because the study was conducted at a time when information about these vaccines was limited.
Consistent with previous studies, older age, male gender, past influenza vaccination, and belief in vaccine efficacy and safety were associated with willingness to undergo COVID-19 vaccination.15,36 Past seasonal influenza vaccination was also reported to be associated with the intention to receive newly introduced vaccines such as pneumococcal polysaccharide vaccine 30 and pandemic influenza vaccine. 14 Being skeptical about vaccines in general was reported to be associated with a lower intention to be vaccinated against influenza and COVID-19. 37 Previous studies from other countries suggested that to a certain degree, the COVID-19 pandemic has increased the willingness to undergo influenza vaccination,38-40 although the reason for this was not stated. It is possible that general attitudes toward vaccines and preventive behavior have changed, 38 and further investigation of this issue is needed.
Belief in the efficacy of vaccines and concerns about vaccine-related adverse events and their severity were associated with vaccination willingness in this study. It was previously reported that belief in vaccine efficacy and safety is related not only to the willingness to undergo COVID-19 vaccination, 41 but also to the intention to receive other vaccines.13,30 It is necessary to provide outpatients with information on the efficacy and safety of vaccines, as individuals require this information when deciding whether to receive COVID-19 vaccines.
We also investigated the influence of COVID-19 vaccine characteristics and delivery systems on vaccination decision-making. Reduced vaccination willingness was associated with fear of several facts regarding COVID-19 vaccines: that they were rapidly approved, that they were not produced in Japan, and that they were developed using a new vaccine technology (mRNA). Other studies also showed that people preferred vaccines manufactured domestically over those produced in other countries,42,43 that they worried about rapid vaccine development. 22 In a global survey conducted from January to March 2021, 72.2% of Japanese respondents stated that they did not know much about mRNA vaccines, and this rate was higher than other countries. 44 Insufficient knowledge about mRNA vaccines may predispose individuals to view the new type of vaccine as unsafe. By investigating why these COVID-19 vaccine characteristics cause fear during the vaccination decision-making process, it may be possible to determine what information will reduce this fear.
As for delivery system factors, we found that participants who were willing to undergo COVID-19 vaccination were less influenced by being unable to be vaccinated at familiar clinics or hospitals or during regular visits with clinicians. We assume that being able to be vaccinated in familiar ways may encourage patients to receive the newly introduced vaccines. However, we should interpret these results carefully because the delivery system was not announced when the study was performed.
There are several limitations to our study. First, participants were recruited from 1 clinic where COVID-19 was very uncommon at the time. It may be difficult to generalize our results to primary care patients. The results may differ in larger study samples and other areas. They may also be different in areas with a higher prevalence of COVID-19, but this is not certain; 1 Japanese study reported that risk perception did not vary between epidemic and non-epidemic areas. 45 Second, our survey questionnaire did not investigate reliability or validity. It is possible that our questionnaire could not correctly assess attitudes and beliefs. Larger studies are needed to investigate these issues in other areas and by using validated questionnaires. Third, because participants were asked to participate in this study after they were examined by their doctors, study participation may have been interpreted as a recommendation from their doctors to undergo COVID-19 vaccination. However, we believe this influence was limited because only 6.5% of participants reported that doctors had advised them to be vaccinated.
Conclusion
Our study revealed that 70% of participants at a primary care clinic were willing to undergo COVID-19 vaccination. Willingness to undergo COVID-19 vaccination was associated with older age, male gender, good self-rated health, influenza vaccination in the previous season, recommendations by others, high perceived susceptibility, belief in vaccine efficacy, low perceived susceptibility to vaccine-related adverse events, low perceived severity of vaccine-related adverse event, and high espousal of social norms. Of these, social norms were the most important factor involved in decision-making about vaccination.
This study described people’s perceptions and attitudes in Japan when vaccination was about to be initiated in the general public. It is necessary to clarify if and how people change their minds about vaccination after it is already underway or if the epidemic situation changes, and whether our results are applicable to other regions and countries.
Supplemental Material
Supplemental material, sj-docx-1-jpc-10.1177_21501319221097282 for COVID-19 Vaccination Willingness and Associated Factors in Japanese Primary Care Patients: A Cross-Sectional Study by Natsuki Kajikawa, Shoji Yokoya and Tetsuhiro Maeno in Journal of Primary Care & Community Health
Acknowledgments
We acknowledge all staff at Kitaibaraki Center for Family Medicine for their valuable help in administering the survey.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Natsuki Kajikawa  https://orcid.org/0000-0001-7220-7738
https://orcid.org/0000-0001-7220-7738
Supplemental Material: Supplemental material for this article is available online.
Reference
- 1. Our World in Data [internet]. Coronavirus (COVID-19) vaccinations. Updated March 31, 2022. Accessed March 31, 2022. https://ourworldindata.org/covid-vaccinations
- 2. Yoda T, Katsuyama H. Willingness to receive covid-19 vaccination in japan. Vaccines. 2021;9:1-8. doi: 10.3390/vaccines9010048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Largent EA, Persad G, Sangenito S, Glickman A, Boyle C, Emanuel EJ. US public attitudes toward COVID-19 vaccine mandates. JAMA Netw Open. 2020;3:e2033324. doi: 10.1001/jamanetworkopen.2020.33324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Reiter PL, Pennell ML, Katz ML. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine. 2020;38:6500-6507. doi: 10.1016/j.vaccine.2020.08.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sallam M, Dababseh D, Eid H, et al. High rates of covid-19 vaccine hesitancy and its association with conspiracy beliefs: a study in Jordan and Kuwait among other Arab countries. Vaccines. 2021;9:1-16. doi: 10.3390/vaccines9010042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wang J, Jing R, Lai X, et al. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines. 2020;8:1-14. doi: 10.3390/vaccines8030482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Taylor S, Landry CA, Paluszek MM, Groenewoud R, Rachor GS, Asmundson GJG. A proactive approach for managing COVID-19: the importance of understanding the motivational roots of vaccination hesitancy for SARS-CoV2. Front Psychol. 2020;11:575950-575955. doi: 10.3389/fpsyg.2020.575950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Schmid P, Rauber D, Betsch C, Lidolt G, Denker ML. Barriers of influenza vaccination intention and behavior - a systematic review of Influenza vaccine hesitancy, 2005 - 2016. PLoS One. 2017;12:e0170550. doi: 10.1371/journal.pone.0170550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nagata JM, Hernández-Ramos I, Kurup AS, Albrecht D, Vivas-Torrealba C, Franco-Paredes C. Social determinants of health and seasonal influenza vaccination in adults ≥65 years: a systematic review of qualitative and quantitative data. BMC Public Health. 2013;13:388. doi: 10.1186/1471-2458-13-388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Machida M, Nakamura I, Kojima T, et al. Acceptance of a covid-19 vaccine in Japan during the covid-19 pandemic. Vaccines. 2021;9:1-11. doi: 10.3390/vaccines9030210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shahid Z, Kalayanamitra R, McClafferty B, et al. COVID-19 and older adults: what we know. J Am Geriatr Soc. 2020;68:926-929. doi: 10.1111/jgs.16472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. de Figueiredo A, Simas C, Karafillakis E, Paterson P, Larson HJ. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. Lancet. 2020;396:898-908. doi: 10.1016/S0140-6736(20)31558-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kan T, Zhang J. Factors influencing seasonal influenza vaccination behaviour among elderly people: a systematic review. Public Health. 2018;156:67-78. doi: 10.1016/j.puhe.2017.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bish A, Yardley L, Nicoll A, Michie S. Factors associated with uptake of vaccination against pandemic influenza: a systematic review. Vaccine. 2011;29:6472-6484. doi: 10.1016/j.vaccine.2011.06.107 [DOI] [PubMed] [Google Scholar]
- 15. Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of U.S. adults. Ann Intern Med. 2020;173:964-973. doi: 10.7326/m20-3569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Frew PM, Painter JE, Hixson B, et al. Factors mediating seasonal and influenza A (H1N1) vaccine acceptance among ethnically diverse populations in the urban south. Vaccine. 2012;30:4200-4208. doi: 10.1016/j.vaccine.2012.04.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gargano LM, Painter JE, Sales JM, et al. Seasonal and 2009 H1N1 influenza vaccine uptake, predictors of vaccination and self-reported barriers to vaccination among secondary school teachers and staff. Hum Vaccin. 2011;7:89-95. doi: 10.4161/hv.7.1.13460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49:1373-1379. doi: 10.1016/s0895-4356(96)00236-3 [DOI] [PubMed] [Google Scholar]
- 19. Hulley SB. Designing Clinical Research (Masako K, Trans.). 4th ed. Medical Sciences International; 2007. [Google Scholar]
- 20. Nomura S, Eguchi A, Yoneoka D, et al. Reasons for being unsure or unwilling regarding intention to take COVID-19 vaccine among Japanese people: a large cross-sectional national survey. Lancet Reg Health West Pacific. 2021;14:100223. doi: 10.1016/j.lanwpc.2021.100223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yoneoka D, Eguchi A, Nomura S, et al. Identification of optimum combinations of media channels for approaching COVID-19 vaccine unsure and unwilling groups in Japan. Lancet Reg Health West Pacific. 2022;18:100330. doi: 10.1016/j.lanwpc.2021.100330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ward JK, Alleaume C, Peretti-Watel P. The French public’s attitudes to a future COVID-19 vaccine: the politicization of a public health issue. Soc Sci Med. 2020;265:113414. doi: 10.1016/j.socscimed.2020.113414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Williams L, Flowers P, McLeod J, Young D, Rollins L; The Catalyst Project TEAM. Social patterning and stability of intention to accept a COVID-19 vaccine in Scotland: will those most at risk accept a vaccine? Vaccines. 2021;9:17. doi: 10.3390/vaccines9010017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cialdini RB, Reno RR, Kallgren CA. A focus theory of normative conduct: recycling the concept of norms to reduce littering in public places. J Pers Soc Psychol. 1990;58:1015-1026. doi: 10.1037/0022-3514.58.6.1015 [DOI] [Google Scholar]
- 25. Lapinski MK, Rimal RN. An explication of social norms. Commun Theory. 2005;15:127-147. doi: 10.1111/j.1468-2885.2005.tb00329.x [DOI] [Google Scholar]
- 26. Shmueli L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health. 2021;21:804. doi: 10.1186/s12889-021-10816-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chu H, Liu S. Integrating health behavior theories to predict American’s intention to receive a COVID-19 vaccine. Patient Educ Couns. 2021;104:1878-1886. doi: 10.1016/j.pec.2021.02.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Graupensperger S, Abdallah DA, Lee CM. Social norms and vaccine uptake: college students’ COVID vaccination intentions, attitudes, and estimated peer norms and comparisons with influenza vaccine. Vaccine. 2021;39:2060-2067. doi: 10.1016/j.vaccine.2021.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rimal RN, Storey JD. Construction of meaning during a pandemic: the forgotten role of social norms. Health Commun. 2020;35:1732-1734. doi: 10.1080/10410236.2020.1838091 [DOI] [PubMed] [Google Scholar]
- 30. Mieczkowski TA, Wilson SA. Adult pneumococcal vaccination: a review of physician and patient barriers. Vaccine. 2002;20:1383-1392. doi: 10.1016/S0264-410X(01)00463-7 [DOI] [PubMed] [Google Scholar]
- 31. Sekimoto M, Asai A, Ohnishi M, et al. Patients’ preferences for involvement in treatment decision making in Japan. BMC Fam Pract. 2004;5:1-10. doi: 10.1186/1471-2296-5-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Takahashi O, Noguchi Y, Rahman M, et al. Influence of family on acceptance of influenza vaccination among Japanese patients. Fam Pract. 2003;20(2):162-166. doi: 10.1093/fampra/20.2.162 [DOI] [PubMed] [Google Scholar]
- 33. Lau L, Lau Y, Lau YH. Prevalence and correlates of influenza vaccination among non-institutionalized elderly people: an exploratory cross-sectional survey. Int J Nurs Stud. 2009;46:768-777. doi: 10.1016/j.ijnurstu.2008.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Soares P, Rocha JV, Moniz M, et al. Factors associated with COVID-19 vaccine hesitancy. Vaccines. 2021;9(3):00. doi: 10.3390/vaccines9030300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. van Essen GA, Kuyvenhoven MM, de Melker RA. Why do healthy elderly people fail to comply with influenza vaccination? Age Ageing. 1997;26:275-279. doi: 10.1093/ageing/26.4.275 [DOI] [PubMed] [Google Scholar]
- 36. Dror AA, Eisenbach N, Taiber S, et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35:775-779. doi: 10.1007/s10654-020-00671-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Caserotti M, Girardi P, Rubaltelli E, Tasso A, Lotto L, Gavaruzzi T. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc Sci Med. 2021;272:113688. doi: 10.1016/j.socscimed.2021.113688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Williams L, Gallant AJ, Rasmussen S, et al. Towards intervention development to increase the uptake of COVID-19 vaccination among those at high risk: outlining evidence-based and theoretically informed future intervention content. Br J Health Psychol. 2020;25:1039-1054. doi: 10.1111/bjhp.12468 [DOI] [PubMed] [Google Scholar]
- 39. Mercadante AR, Law AV. Will they, or won’t they? Examining patients’ vaccine intention for flu and COVID-19 using the health belief model. Res Soc Adm Pharm. 2021;17:1596-1605. doi: 10.1016/j.sapharm.2020.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Domnich A, Cambiaggi M, Vasco A, et al. Attitudes and beliefs on influenza vaccination during the covid-19 pandemic: results from a representative Italian survey. Vaccines. 2020;8:1-20. doi: 10.3390/vaccines8040711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lazarus JV, Ratzan SC, Palayew A, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225-228. doi: 10.1038/s41591-020-01226-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Pogue K, Jensen JL, Stancil CK, et al. Influences on attitudes regarding potential COVID-19 vaccination in the United States. Vaccines. 2020;8:1-14. doi: 10.3390/vaccines8040582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP. Understanding COVID-19 vaccine demand and hesitancy: a nationwide online survey in China. PLoS Negl Trop Dis. 2020;14:e0008961. doi: 10.1371/journal.pntd.0008961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wong LP, Alias H, Danaee M, et al. COVID-19 vaccination intention and vaccine characteristics influencing vaccination acceptance: a global survey of 17 countries. Infect Dis Poverty. 2021;10(1):122. doi: 10.1186/s40249-021-00900-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Yamagata M, Teraguchi T, Miura A. Japanese society and psychology during the COVID-19 pandemic. Jpn J Psychol. 2021;92:452-462. doi: 10.4992/jjpsy.92.20222 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jpc-10.1177_21501319221097282 for COVID-19 Vaccination Willingness and Associated Factors in Japanese Primary Care Patients: A Cross-Sectional Study by Natsuki Kajikawa, Shoji Yokoya and Tetsuhiro Maeno in Journal of Primary Care & Community Health