Abstract
Little is known about how people’s beliefs concerning the Coronavirus Disease 2019 (COVID-19) influence their behavior. To shed light on this, we conduct an online experiment () with US and UK residents. Participants are randomly allocated to a control group or to one of two treatment groups. The treatment groups are shown upper- or lower-bound expert estimates of the infectiousness of the virus. We present three main empirical findings. First, individuals dramatically overestimate the dangerousness and infectiousness of COVID-19 relative to expert opinion. Second, providing people with expert information partially corrects their beliefs about the virus. Third, the more infectious people believe that COVID-19 is, the less willing they are to take protective measures, a finding we dub the “fatalism effect”. We develop a formal model that can explain the fatalism effect and discuss its implications for optimal policy during the pandemic.
Keywords: COVID-19, Beliefs, Online experiment, Fatalism
Introduction
The Coronavirus Disease 2019 (COVID-19) has exacted a considerable toll, with impacts measurable in lives lost, freedoms curtailed, and reductions in economic welfare (Baker et al., 2020; Guerrieri et al., 2020; Gormsen & Koijen, 2020; Reis, 2020).1 Even in the presence of effective vaccines, governmental efforts continue to rely on behavioral restrictions and recommendations, such as mask mandates, hygiene requirements and social distancing rules. These measures are likely to remain common in the immediate future.
The mortality benefits of abiding by behavioral restrictions are estimated to be worth around $60000 per US household (Greenstone & Nigam, 2020). Improving compliance with such restrictions could, thus, have large social payoffs. We do not yet know, however, the determinants of individual compliance and how they might change over time (Anderson et al., 2020; Avery et al., 2020; Briscese et al., 2020; Hsiang et al., 2020; Lewnard & Lo, 2020). In particular, we do not understand the role of individual beliefs, and whether these beliefs can be revised in ways that generate greater compliance.
To shed light on these questions, we conducted an online experiment in the US and UK with 3,610 participants. Participants are randomly assigned to a control condition or one of two treatment groups. Those in the first group (referred to as the ‘lower-bound’ condition) are told that those who contract the virus are likely to infect two other people.2 Those in the second group (referred to as the ‘upper-bound’ condition) are told that those who contract the virus are likely to infect five other people. These estimates are from epidemiological studies and reflect uncertainties regarding the characteristics of the virus and people’s behavior (Liu et al., 2020).
Our analysis yields three main empirical findings. First, we find that participants over-estimate the infectiousness and deadliness of COVID-19. For example, participants believe, on average, that one person will infect 28 others; whereas experts estimate that the figure is between one and six (Liu et al., 2020). This result is consistent with previous studies which suggest that individuals are likely to overestimate risks that are unfamiliar, outside of their control, inspire feelings of dread, and receive extensive media coverage (see, e.g., Slovic (2000)).
Second, we show that people update their posterior beliefs about COVID-19 in response to expert information––at least in the short-run. The modal belief is that one person will infect two others in the lower-bound group, while the modal belief is that one person will infect five others in the upper-bound group. However, not all participants fully believe or understand the information conveyed in the treatments, with 46% and 61% of participants believing that one person will infect more than six others in the upper- and lower-bound groups respectively.
Third, we examine how beliefs causally affect behavior. In general, this is a difficult task. Randomly providing certain individuals with information can both influence their beliefs and ‘prime’ them to consider these beliefs when making decisions (Haaland et al., 2020). We are able to overcome this issue by exploiting variability in expert estimates. By providing information about infectiousness to both treatment groups, we make this issue salient for all of our experimental participants (ignoring our control group, which we drop in most analyses). As a result, our findings cannot be attributed to differential priming of our participants; and we are able to estimate the causal impact of beliefs on behavior by using the random assignment of individuals to the upper- or lower-bound groups as an instrument for their beliefs.
This approach yields our third central finding: exaggerated posterior beliefs about the infectiousness of COVID-19 make individuals less willing to comply with best practice behaviors, a phenomenon we call the “fatalism effect”. On average, for every additional person that participants believe someone with COVID-19 will typically infect, they become 0.5 percentage points less likely to say that they would avoid meeting people in high-risk groups. They also become 0.26 percentage points less likely to say that they would wash their hands frequently.
While others have observed the existence of a fatalism effect (see, e.g., Ferrer and Klein (2015) or Shapiro and Wu (2011)), we are among the first to demonstrate the existence of such effects using experimental methods (for another example, see Kerwin (2018)).3 We also develop a basic model that is capable of explaining the fatalism effect. The model applies not just to this pandemic, but also to more general situations where people must choose whether to change their behavior to reduce personal or societal risks.
The intuition of our model is straightforward. Increasing individual estimates of the infectiousness of COVID-19 raises their perception of the probability that they will contract the disease even if they comply with best practice behaviors. This, in turn, reduces the perceived benefit of complying with such behaviors.4 Consistent with this explanation, we also find that increasing individual assessments of the infectiousness of the virus leads people to be less optimistic about their future prospects, suggesting that they interpret information about infectiousness in the way assumed by our model.
The fatalism that we document could cause substantial reductions in individual and societal welfare. For example, by making individuals less likely to regularly wash their hands, it makes them more vulnerable to respiratory illnesses like COVID-19 (Rabie & Curtis, 2006). A conservative back-of-the-envelope calculation suggests that if average beliefs about the infectiousness of COVID-19 increase by eight units (e.g., someone with the virus is likely to infect 18 rather than 10 people), then we expect to see a mortality loss of $3.7 billion in the US alone, solely as a result of reduced handwashing (not counting morbidity losses, spillovers, or further waves of infection).5 Our findings thus suggest that there may be dramatic gains from providing the public with accurate information insofar as this information revises exaggerated beliefs downwards.
This paper contributes to a number of areas in economics and psychology. First, we contribute to the literature on the perception and misperception of risk (see, e.g., Viscusi (1990), Slovic (2000), Cawley and Ruhm (2011) or indeed Fetzer et al. (2020) for a contemporaneous examination of risk perceptions during the COVID-19 pandemic). Second, while we examine individuals’ risk perceptions, we also go on to study the causal effect of these perceptions on their willingness to comply with best practice behaviors.6 Third, we contribute to a small literature on rational fatalism; both by studying this in a novel context (compare Kerwin (2018)’s findings from Malawi) and by providing a model to explain the observed fatalism in the tradition of Kremer (1996). Fourth, we contribute to the growing literature on how policymakers can best respond to the COVID-19 pandemic by showing that it is both possible, and important, to correct people’s beliefs about the virus.7,8
The remainder of the article is structured as follows. Section 2 reviews our experimental design. Section 3 presents the main empirical results. Section 4 develops a formal model of the fatalism effect. Finally, Sect. 5 concludes.
Experimental design
We conducted the experiment between March 26 and March 29, 2020.9 Our sample consists of 3,610 participants (1,859 from the US and 1,751 from the UK). Participants were recruited via the panel provider Prolific Academic.10,11 All participants were paid for their participation.12
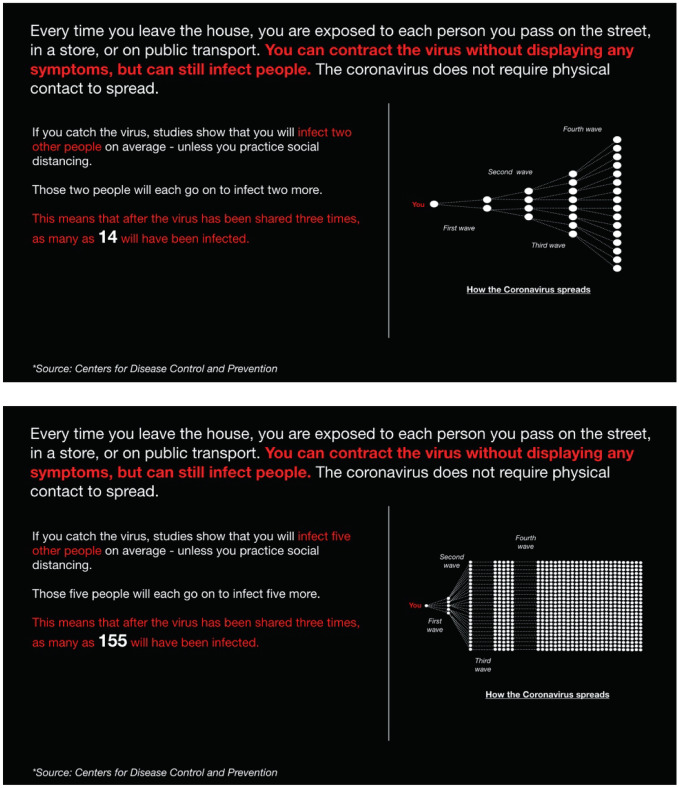
Participants are randomly assigned to a control group that receives no intervention or one of two treatment groups. Those in the first group (the lower-bound treatment) are shown a message explaining that studies show that those who contract COVID-19 will, on average, infect two other people––see Fig. 1. Those in the second group (the upper-bound treatment) are instead told that studies show that those who contract COVID-19 will, on average, infect five other people. Otherwise, the message they receive is the same.13 The treatment messages are coupled with graphics illustrating how COVID-19 might spread if the virus is passed on three times at the respective levels of infectiousness.14 The statistic that we show participants in the treatments is known as in the epidemiological literature and indicates how many people one infected person is likely to infect.
Fig. 1.
Treatment messages. Notes. The first image displays the treatment message showed to the lower-bound group. The second image displays the treatment message showed to the upper-bound group
Both before and after exposing subjects to the treatments, we measure our key object of interest: participants’ beliefs about the infectiousness of COVID-19.15 More specifically, we ask: “On average, how many people do you think will catch the Coronavirus from one contagious person? Please only consider cases transmitted by coughing, sneezing, touch or other direct contact with the contagious person.” Participants are free to enter any integer between 0 and 100.
Next, we ask participants about two other COVID-19-related beliefs: (1) the probability of being hospitalized conditional on contracting the virus; and (2) the probability of dying conditional on being hospitalized for the virus.16,17 We do not reward correct estimates with financial incentives when assessing ‘pre-beliefs’ since we do not want to induce the participants to look up numbers online. We also do not incentivize correct estimates when eliciting post-beliefs since we do not want to encourage individuals to report the number conveyed in their treatment regardless of whether it fits their beliefs. In other words, we suspect that incentivization would simply lead subjects to automatically report the expert estimate with which they were presented in a bid to earn the financial pay-off.18
Further, we ask people about their willingness to comply with three COVID-19-related best practices for 1 week and 2 months. These best practices are: (1) frequent handwashing; (2) working from home; and (3) not meeting people in high-risk groups. We choose these outcomes because they represent behaviors that are common components of governments’ COVID-19 mitigation strategies (see, for example, CDC (2020), Office (2020) and WHO (2020)).19 We only measure stated intentions for future behavior and recognize the limitations of such measures; however, we see no reason to think that these limitations will have more of an effect on one treatment group than another.20
Finally, we ask people whether they are optimistic about their future prospects. Optimism and expectations about the future are key drivers of macroeconomic activity.21 Measuring optimism also allows us to verify that our subjects interpret the information provided about infectiousness in the expected manner.
When analyzing the experimental data, we begin by conducting linear first-stage regressions, estimating the effects of random information assignment on beliefs:
| 1 |
where represents beliefs about ; is a dummy variable indicating whether the participant is randomly assigned to the upper-bound information condition; and represents a vector of socioeconomic and demographic variables (e.g., age and years of education). Thus, represents the average treatment effect on beliefs. We do not use participants in the control group when conducting this analysis (i.e., those in the lower-bound group are the “reference group”).22
We then conduct Two-Stage Least Squares (2SLS) regressions to estimate the Local Average Treatment Effect (LATE) of beliefs about on people’s optimism and their willingness to socially distance:
| 2 |
where represents people’s willingness to socially distance or whether they are optimistic about their future (binary variables); represents the fitted values obtained using Eq. (1); and is a vector representing the same set of demographic and socioeconomic variables. Again, we exclude those in the control group when conducting this analysis to ensure that the exclusion restriction is met. Our estimate of is the LATE of changing beliefs about people’s stated behavior and optimism.23
Results
Participant characteristics
We begin by providing an overview of participant characteristics. Approximately 59% of respondents are female and 75% of respondents are between the ages of 18 and 44. The monthly average pre-tax household income was $4461 in 2019.24 Sixteen percent of participants claim to know someone that has contracted COVID-19; 4% claim to have been in contact with someone that has been diagnosed with COVID-19; 38% of participants claim to display one or more of the known symptoms of COVID-19; and 48% of respondents believe that restrictions will remain in place for more than three months.25
People have exaggerated prior beliefs about the infectiousness and dangerousness of COVID-19
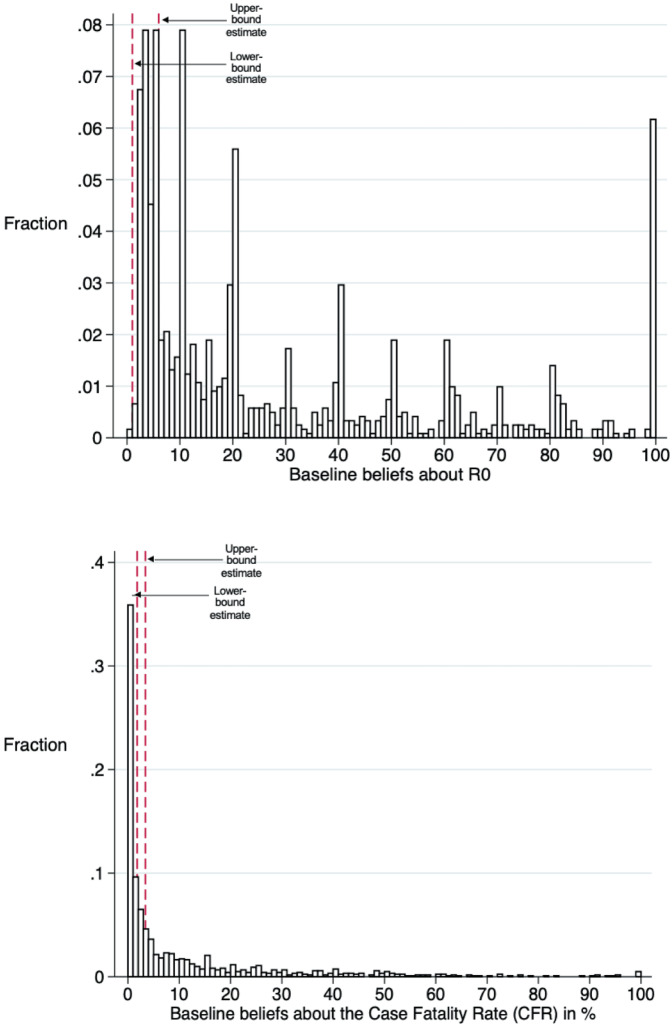
We now study the accuracy of subject beliefs concerning the infectiousness () and Case Fatality Rate (CFR) of COVID-19. As shown in Fig. 2, we find that the overwhelming majority of subject estimates are outside of the bounds of expert consensus.26 On average, participants believe that the typical person with COVID-19 gives it to 28 others; in contrast, expert estimates of at the time of the experiment put it in the 1 to 6 range (Liu et al., 2020). Similarly, participants, on average, believe that the CFR (the share of people who contract COVID-19 that die) is 10.79%; according to the CDC estimates, the case fatality rate in the US is between 1.8 and 3.4% (CDC, 2020).
Fig. 2.
Baseline prior beliefs about and the CFR. Notes. The first diagram displays the distribution of beliefs regarding the infectiousness of COVID-19 () at baseline. The second displays the distribution of beliefs regarding case fatality rate (CFR) at baseline. Participants’ perceived CFR is calculated by multiplying their belief regarding the risk of being hospitalized conditional on contracting COVID-19 by the risk of dying conditional on being hospitalized for COVID-19. See Appendix F for the exact questions that were used to construct these variables
The fact that participants have incorrect prior beliefs about COVID-19 is consistent with many of the findings from the literature on risk perception. According to this literature, the public is likely to overestimate risks when they are new or unfamiliar, seen as outside of their control, inspire feelings of dread, and receive extensive media coverage (see Slovic (2000) for a review). Clearly, all of these apply to COVID-19; so it is perhaps not surprising that subjects overestimate the risk of, and danger posed by, COVID-19. We also note that our finding is consistent with contemporaneous work by Fetzer et al. (2020) who find similar biases in subject beliefs.
We estimate two linear probability models to investigate heterogeneity in subjects’ beliefs (complementing the analysis in de Bruin et al. (2020)). As detailed in Appendix D, we find that men, those who are not in a risk group, and the more educated are significantly less likely to overestimate and the CFR. People in both the UK and the US are likely to overestimate , but those in the US are 12 and 9.5 percentage points more likely than those in the UK to overestimate CFR and respectively (ceteris paribus). Further, those that consume right-wing news are more likely to overestimate . These results are consistent with the general finding that different demographic groups can perceive risks in different ways. It is also consistent with more specific findings from the literature on risk perception: for example, a large number of papers find, as we do in our particular context, that men tend to rate risks as smaller than women do.27
Providing information about the infectiousness of COVID-19 corrects beliefs
Table 1 presents the effects of being assigned to the lower- and upper-bound conditions on beliefs regarding: (1) and (2) the CFR. In other words, Table 1 reports the difference in mean beliefs between the treatment and control groups (controlling for demographic variables).28
Table 1.
Effects of randomly assigned information on beliefs
| (1) | (2) | |
|---|---|---|
| VARIABLES | Beliefs about | Beliefs about the CFR |
| Assigned to lower-bound ( = 2) | -7.889*** | -0.425 |
| (1.139) | (0.720) | |
| Assigned to upper-bound ( = 5) | -2.797** | -0.303 |
| (1.260) | (0.698) | |
| Constant | 52.94*** | 45.15*** |
| (5.663) | (3.932) | |
| Mean in control group | 28.671 | 10.579 |
| p-value lower v. upper means | 0.000 | 0.555 |
| Observations | 3,577 | 3,577 |
| 0.048 | 0.114 |
This table presents results from OLS regressions examining the effects of being assigned to the lower- or upper-bound treatments on beliefs about and the case fatality rate (CFR). All outcomes are measured on a scale from 0 to 100 and demographic control variables (e.g., age, geography, education, and income) are used in all specifications. Comparisons are made relative to the group that receives no treatment. Robust standard errors in parentheses (*** , ** , * )
The table reveals that being shown lower- or upper-bound estimates of decreases average estimates of from 29 to 21 and 26, respectively (see column 1). We also find that, on average, being told that is one percent greater prompts respondents to revise their beliefs upward by 0.16 percent (i.e., the elasticity is 0.16). Further, we obtain an F-statistic of 16.71 when regressing treatment assignment on beliefs about (excluding the control group), suggesting that we have an informative instrument (i.e., a strong ‘first stage’) and can proceed to use treatment assignment as an instrumental variable for beliefs about .29
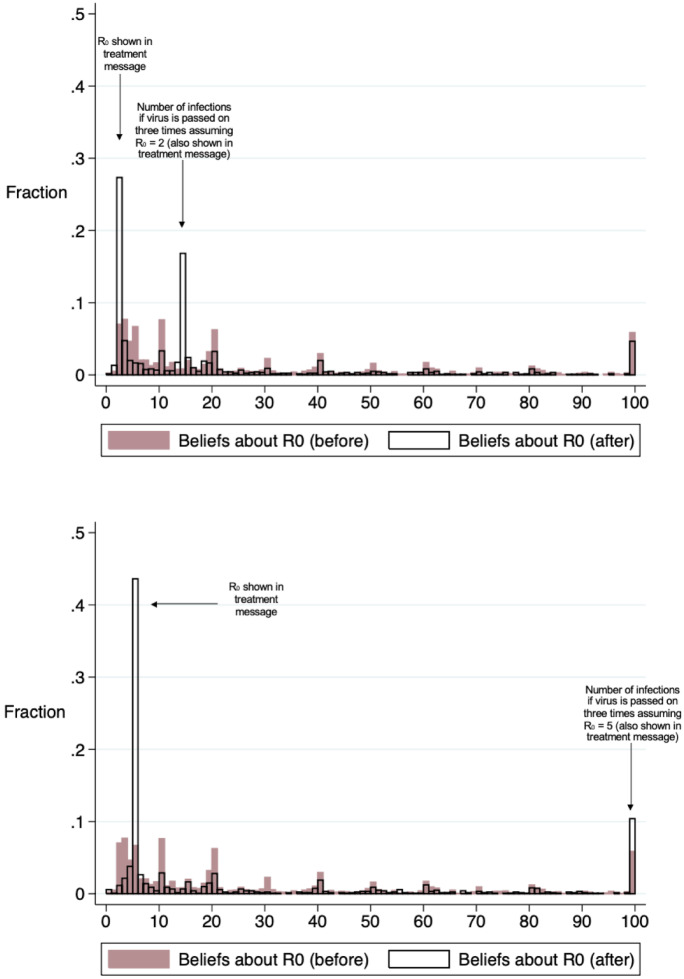
Figure 3 reveals the effect of the treatments on the entire distribution of beliefs about . The treatments shift the modal belief in the expected way: these are 5 and 2 in the upper- and lower-bound groups respectively (i.e., the estimates that the respective groups were presented with). However, not all individuals change their beliefs in line with the information that they are given, with 46% and 61% of participants still believing that is above 6 in the upper- and lower-bound groups respectively.30,31
Fig. 3.
Effect of treatments on posterior beliefs of . Notes. The first diagram displays the distribution of beliefs about in the lower-bound group pre- (prior) and post-treatment (posterior). The second diagram displays the distribution of beliefs about in the upper-bound group pre- and post-treatment. Participants can enter any number between 0 and 100 when stating their beliefs about
Since baseline beliefs are measured prior to information provision (for a randomly selected subset of participants), it is also possible to run a before and after comparison. We find that there are substantial differences in pre- and post-treatment beliefs. Post-treatment beliefs are, for example, more centered around the values that the treatment messages convey, and a greater portion of participants hold beliefs within the expert estimates (i.e., between 1 and 6).
Our analysis suggests that expert information about the infectiousness of can update (and correct) people’s beliefs––at least in the short-term. It also demonstrates that our instrument is informative; we thus proceed with the instrumental variable analysis in the next section.
Increasing people’s posterior beliefs of the infectiousness of COVID-19 makes them less willing to engage in best practices
We now examine whether changing beliefs regarding changes participants’ stated willingness to comply with best practice behaviors. We ask participants how willing they would be to frequently wash their hands, avoid seeing people in high-risk groups, and work from home assuming that “the Coronavirus outbreak is still ongoing 7 days/2 months from today.” Participants provide answers on a five-point scale, with one representing ‘extremely unlikely’ and five representing ‘extremely likely’. We transform this variable into a binary outcome, defined as one if participants state that they would be ‘extremely likely’ or ‘likely’ to adopt a given behavior and otherwise as zero.32
Table 2 reveals that the Local Average Treatment Effect (LATE) point estimates are consistently negative, and statistically significant for the willingness to wash hands frequently (2 months) and visiting risk groups (7 days and 2 months). In other words, we find that increasing the perceived infectiousness rate actually makes individuals less willing to engage in best practice behaviors, a phenomenon we dub the ‘fatalism effect’.33 We view our point estimates as surprisingly large. For example, we estimate that decreasing individual estimates of by one unit makes individuals around 0.5 percentage points more likely to avoid meeting people in high-risk groups (see columns two and four in Table 2). Since the individuals in our sample, on average, overestimate the infectiousness rate by over 20 units, this suggests that there may be substantial gains from correcting public misconceptions on these and related issues.34
Table 2.
The effect of posterior beliefs about on willingness to engage in best practices
| Willingness to avoid meeting people in high-risk groups | ||||
|---|---|---|---|---|
| 7 days ITT | 7 days LATE | 2 months ITT | 2 months LATE | |
| Upper-bound condition | -0.0233** | -0.0255** | ||
| (0.0111) | (0.0109) | |||
| Beliefs about | -0.00451* | -0.00492** | ||
| (0.00232) | (0.00232) | |||
| Constant | 0.909*** | 1.031*** | 0.826*** | 1.048*** |
| Lower-bound mean | 0.932 | 0.937 | ||
| Controls | Yes | Yes | Yes | Yes |
| Observations | 2,404 | 2,404 | 2,405 | 2,405 |
| 0.021 | 0.023 | |||
| Willingness to wash hands frequently | ||||
|---|---|---|---|---|
| 7 days ITT | 7 days LATE | 2 months ITT | 2 months LATE | |
| Upper-bound condition | -0.00591 | -0.0132** | ||
| (0.00589) | (0.00603) | |||
| Beliefs about | -0.00114 | -0.00255** | ||
| (0.00118) | (0.00129) | |||
| Constant | 0.989*** | 1.080*** | 1.008*** | 1.123*** |
| Lower-bound mean | 0.981 | 0.984 | ||
| Controls | Yes | Yes | Yes | Yes |
| Observations | 2,404 | 2,404 | 2,405 | 2,405 |
| 0.014 | 0.017 | |||
| Willingness to work from home | ||||
|---|---|---|---|---|
| 7 days ITT | 7 days LATE | 2 months ITT | 2 months LATE | |
| Upper-bound condition | -0.0276 | -0.0190 | ||
| (0.0186) | (0.0186) | |||
| Beliefs about | -0.00534 | -0.00366 | ||
| (0.00381) | (0.00368) | |||
| Constant | -0.293 | -0.0535 | -0.264 | -0.0992 |
| Lower-bound mean | 0.465 | 0.466 | ||
| Controls | Yes | Yes | Yes | Yes |
| Observations | 2,391 | 2,391 | 2,405 | 2,405 |
| 0.079 | 0.071 | |||
The first and third columns present intention to treat (ITT) estimates of the effect of assignment to the upper-bound condition on our outcomes of interest. The second and fourth columns present local average treatment effect (LATE) estimates of the effect of beliefs about on the same outcomes. The outcomes of interest are whether participants comply with various behaviors if the pandemic were to continue for 7 days/2 months. Demographic control variables are used in all regressions and the control group is excluded from this analysis. Robust standard errors in parentheses (*** , ** , * )
Since these results may seem surprising, we conduct a series of robustness checks. We begin by dropping participants who guessed that at baseline since such participants may not have understood the question. As Table 16 makes clear, removing these outliers does not make any discernible difference to our results.
Table 16.
Effects of beliefs on willingness to engage in best practices (dropping outliers)
| Willingness to avoid meeting people in high-risk groups | ||||
|---|---|---|---|---|
| 7 days ITT | 7 days LATE | 2 months ITT | 2 months LATE | |
| Upper-bound condition | -0.0240** | -0.0246** | ||
| Beliefs about | -0.00443** | -0.00453** | ||
| Constant | 0.843*** | 1.041*** | 0.822*** | 1.023*** |
| 0.020 | 0.021 | |||
| Willingness to wash hands frequently | ||||
|---|---|---|---|---|
| 7 days ITT | 7 days LATE | 2 months ITT | 2 months LATE | |
| Upper-bound condition | -0.00602 | -0.0134** | ||
| Beliefs about | -0.00111 | -0.00246** | ||
| Constant | 1.028*** | 1.077*** | 1.008*** | 1.117*** |
| 0.014 | 0.017 | |||
| Willingness to work from home | ||||
|---|---|---|---|---|
| 7 days ITT | 7 days LATE | 2 months ITT | 2 months LATE | |
| Upper-bound condition | -0.0288 | -0.0190 | ||
| Beliefs about | -0.00531 | -0.00351 | ||
| Constant | -0.305 | -0.0684 | -0.286 | -0.130 |
| 0.081 | 0.073 | |||
This table presents results from instrumental variable regressions (2SLS) where assignment to the upper-bound exponential condition acts as an instrumental variable for beliefs regarding . The outcomes of interest are whether participants comply with various behaviors if the pandemic continued for 7 days or 2 months. The sample sizes differ slightly between regression due to (as good as randomly allocated) missing values in the dependent variable. Demographic control variables are used in all regressions and the control group is excluded. In all of these analyses, we drop participants that believe that at baseline. We use robust standard errors (*** , ** , * )
Second, we re-estimate the ITT and LATE using a probit model. As can be seen from Table 11, this again makes little difference to our results. As before, we find significant negative effects of beliefs on willingness to avoid high-risk groups; and negative (but still only marginally significant) estimates for willingness to wash hands frequently.
Table 11.
The effect of posterior beliefs about on willingness to engage in best practices (probit)
| Willingness to avoid meeting people in high-risk groups | ||||
|---|---|---|---|---|
| 7 days ITT | 7 days LATE | 2 months ITT | 2 months LATE | |
| Upper-bound condition | -0.170** | -0.184** | ||
| (0.0760) | (0.0780) | |||
| Beliefs about | -0.0246*** | -0.0254*** | ||
| (0.00654) | (0.00604) | |||
| Controls | Yes | Yes | Yes | Yes |
| Observations | 2,404 | 2,404 | 2,405 | 2,405 |
| Willingness to wash hands frequently | ||||
|---|---|---|---|---|
| 7 days ITT | 7 days LATE | 2 months ITT | 2 months LATE | |
| Upper-bound condition | -0.0985 | -0.260** | ||
| (0.115) | (0.118) | |||
| Beliefs about | -0.0169 | -0.0294*** | ||
| (0.0154) | (0.00444) | |||
| Controls | Yes | Yes | Yes | Yes |
| Observations | 2,399 | 2,399 | 2,400 | 2,400 |
| Willingness to work from home | ||||
|---|---|---|---|---|
| 7 days ITT | 7 days LATE | 2 months ITT | 2 months LATE | |
| Upper-bound condition | -0.0773 | -0.0500 | ||
| (0.0549) | (0.0546) | |||
| Beliefs about | -0.0136 | -0.00926 | ||
| (0.00854) | (0.00956) | |||
| Controls | Yes | Yes | Yes | Yes |
| Observations | 2,391 | 2,391 | 2,405 | 2,405 |
The first and third columns present intention to treat (ITT) estimates of the effect of assignment to the upper-bound condition on our outcomes of interest. The second and fourth columns present local average treatment effect (LATE) estimates of the effect of beliefs about on the same outcomes. The outcomes of interest are whether participants comply with various behaviors if the pandemic were to continue for 7 days or 2 months. We use robust standard errors (*** , ** , * )
Third, we re-run the regressions displayed in Table 2 in order to see whether the point estimates differ when including two instruments, rather than one. To do this, we introduce the control group into the analysis. We find that the point estimates remain qualitatively similar (see Table 9 for the full results). However, it is possible that the exclusion restriction is not met here since those in the control group were not primed in the same way as those in the treatment groups (Haaland et al., 2020). As a result, this is not our preferred specification.
Table 9.
Estimation with two instruments
| Willingness to avoid meeting people in high-risk groups | ||||
|---|---|---|---|---|
| 7 days ITT | 7 days LATE | 2 months ITT | 2 months LATE | |
| Upper-bound condition | -0.00740 | 0.0131 | ||
| Lower-bound condition | 0.0169 | 0.0389*** | ||
| Beliefs about | -0.00247* | -0.00495*** | ||
| Constant | 0.909*** | 1.031*** | 0.826*** | 1.048*** |
| Control mean | 0.918 | 0.901 | ||
| 0.023 | 0.029 | |||
| Willingness to wash hands frequently | ||||
|---|---|---|---|---|
| 7 days ITT | 7 days LATE | 2 months ITT | 2 months LATE | |
| Upper-bound condition | -0.00105 | -0.00401 | ||
| Lower-bound condition | 0.00485 | 0.00917 | ||
| Beliefs about | -0.000682 | -0.00134* | ||
| Constant | 0.989*** | 1.080*** | 1.008*** | 1.123*** |
| Control mean | 0.977 | 0.975 | ||
| 0.013 | 0.014 | |||
| Willingness to work from home | ||||
|---|---|---|---|---|
| 7 days ITT | 7 days LATE | 2 months ITT | 2 months LATE | |
| Upper-bound condition | -0.0165 | -0.00315 | ||
| Lower-bound condition | 0.0113 | 0.0165 | ||
| Beliefs about | -0.00193 | -0.00231 | ||
| Constant | -0.293 | -0.0535 | -0.264 | -0.0992 |
| Control mean | 0.683 | 0.674 | ||
| 0.079 | 0.071 | |||
The first and third columns present intention to treat (ITT) estimates of the effect of assignment to the upper-bound condition on our outcomes of interest. The second and fourth columns present local average treatment effect (LATE) estimates of the effect of beliefs about on the same outcomes. The outcomes of interest are whether participants comply with various behaviors if the pandemic were to continue for 7 days or 2 months. In all regressions, the sample size is 3, 577 and demographic control variables are used. We use robust standard errors (*** , ** , * )
Fourth, we conduct a simple OLS analysis (while controlling for a range of demographic and other characteristics) to measure the association between beliefs about and individuals’ willingness to engage in best practices – see Tables 12, 13 and 14. For what it is worth, our OLS estimates again suggest a significant fatalism effect on willingness to avoid seeing people in high-risk groups (but not for the other two outcomes). While this may lend further plausibility to our main findings, these results should be treated with caution in light of possible omitted variable bias.35
Table 12.
The association between posterior beliefs and willingness to avoid seeing people in high-risk groups
| VARIABLES | 7 days | 2 months |
|---|---|---|
| Posterior beliefs about | -0.000455*** | -0.000371** |
| (1.422) | (1.435) | |
| Controls | Yes | Yes |
| Observations | 3,594 | 3,594 |
| 0.024 | 0.028 |
This table presents the association between posterior beliefs about and participants’ willingness to avoid seeing people in high-risk groups if the pandemic continues for 7 days or 2 months. Demographic control variables (e.g., age, geography, education, and income) are used in all specifications. We use robust standard errors (*** , ** , * )
Table 13.
The association between posterior beliefs and willingness to wash hands frequently
| VARIABLES | 7 days | 2 months |
|---|---|---|
| Posterior beliefs about | -4.80e-6 | -8.73e-05 |
| (7.69e-5) | (8.35e-5) | |
| Controls | Yes | Yes |
| Observations | 3,593 | 3,595 |
| 0.013 | 0.013 |
This table presents the association between posterior beliefs about and participants’ willingness to wash their hands frequently if the pandemic continues for 7 days or 2 months. Demographic control variables (e.g., age, geography, education, and income) are used in all specifications. We use robust standard errors (*** , ** , * )
Table 14.
The association between posterior beliefs and willingness to work from home
| VARIABLES | 7 days | 2 months |
|---|---|---|
| Posterior beliefs about | 0.000257 | 0.000217 |
| (0.000253) | (0.000255) | |
| Controls | Yes | Yes |
| Observations | 3,578 | 3,595 |
| 0.013 | 0.013 |
This table presents the association between posterior beliefs about and participants’ willingness to work from home if the pandemic continues for 7 days or 2 months. Demographic control variables (e.g., age, geography, education, and income) are used in all specifications. We use robust standard errors (*** , ** , * )
Fifth, we conduct a heterogeneity analysis that examines whether the effect of beliefs depends on individuals’ prior beliefs about . To do this, we drop individuals for whom we did not elicit baseline beliefs (half the sample) and then split the remaining sample into three subgroups, corresponding to perceived below 33, perceived above 67 and an ‘intermediate’ group. Our estimated coefficients are negative for all outcomes and all groups with the exception of washing hands for those with a baseline belief greater than 67 (see Tables 17 and 18). However, the dramatic reduction in sample size means that our results lose significance.
Table 17.
Effects of beliefs about on willingness to avoid seeing people in high-risk groups by prior beliefs
| Effect of beliefs about if… | 7 days | 2 months |
|---|---|---|
| …prior beliefs of between 0-33 | -0.0018798 | -0.0002758 |
| (.0024674) | (.0023607) | |
| …prior beliefs of between 33-66 | -0.0115226 | -0.0105795 |
| (.0082154) | (.007606) | |
| …prior beliefs of between 66-100 | -0.0171911 | -0.0534486 |
| (.0858171) | (.2502126) |
The coefficients are obtained using six separate 2SLS IV regressions, and represent the effect of beliefs about on people’s willingness to avoid seeing people in high-risk groups. For each regression we restrict the sample to those with prior beliefs between 0 and 33, 33 and 66, and 66 and 100, respectively. Robust standard errors in parentheses (*** , ** , * )
Table 18.
Effects of beliefs about on willingness to wash hands frequently by prior beliefs
| Effect of beliefs about if… | 7 days | 2 months |
|---|---|---|
| …prior beliefs of between 0-33 | -0.0001879 | -0.0012152 |
| (.0014334) | (.0013258) | |
| …prior beliefs of between 33-66 | -0.0046913 | -0.0058641 |
| (.0031882) | (.0039007) | |
| …prior beliefs of between 66-100 | 0.0090644 | 0.0091686 |
| (.0445497) | (.0471777) |
The coefficients are obtained using six separate 2SLS IV regressions, and represent the effect of beliefs about on people’s willingness to wash their hands frequently. For each regression we restrict the sample to those with prior beliefs between 0 and 33, 33 and 66, and 66 and 100, respectively. Robust standard errors in parentheses (*** , ** , * )
Finally, we consider whether our result might somehow be due to subject inattention. In principle, it is not obvious why inattention should be expected to generate a fatalism effect – both because attention should be roughly balanced in both treatment groups (due to the randomization) and because it is unclear how inattention should affect subject responses. Nonetheless, we now investigate this issue more fully by dropping those who proceeded very quickly through the survey (less than ten, eight and six minutes), dropping those who only spent the mandatory amount of time (twenty seconds) on the treatment screen, and dropping those who gave the same response to all the questions about COVID-19 (which were all elicited on the same 0-100 scale). As shown in Tables 19, 20 and 21, none of these exercises appreciably alters the estimated coefficients or standard errors – providing further evidence that our results are not driven by inattention.
Table 19.
Dropping less attentive subjects I
| Outcome | LATE | SE | Exclusion criterion | n |
|---|---|---|---|---|
| Avoid high risk (7 d) | -0.00451 | 0.00232 | None | 2404 |
| -0.00386 | 0.00234 | Total time taken 10min | 2234 | |
| -0.00424 | 0.00231 | Total time taken 8min | 2363 | |
| -0.00454 | 0.00234 | Total time taken 6min | 2386 | |
| -0.00477 | 0.00256 | Time on treatment screen 22s | 2024 | |
| -0.00434 | 0.00231 | Same responses to all belief qs | 2381 | |
| Avoid high risk (2 m) | -0.00492 | 0.00232 | None | 2405 |
| -0.00464 | 0.00239 | Total time taken 10min | 2235 | |
| -0.00482 | 0.00234 | Total time taken 8min | 2364 | |
| -0.00494 | 0.00236 | Total time taken 6min | 2387 | |
| -0.00485 | 0.00254 | Time on treatment screen 22s | 2024 | |
| -0.00489 | 0.00233 | Same responses to all belief qs | 2382 |
This table examines how the LATE estimate of beliefs on willingness to avoid high-risk individuals changes once apparently less attentive subjects are excluded. The first column specifies the relevant outcome (whether an individual is willing to avoid those in high-risk groups over the next 7 days and over the next 2 months). The subsequent columns specify the standard error associated with the LATE, the criterion which determines which subjects were dropped, and the resulting sample size
Table 20.
Dropping less attentive subjects II
| Outcome | LATE | SE | Exclusion criterion | n |
|---|---|---|---|---|
| Washing hands (7 d) | -0.00114 | 0.00118 | None | 2404 |
| -0.00060 | 0.00116 | Total time taken 10min | 2234 | |
| -0.00089 | 0.00115 | Total time taken 8min | 2363 | |
| -0.00102 | 0.00115 | Total time taken 6min | 2386 | |
| -0.00121 | 0.00131 | Time on treatment screen 22s | 2024 | |
| -0.00101 | 0.00115 | Same responses to all belief qs | 2381 | |
| Washing hands (2 m) | -0.00255 | 0.00129 | None | 2405 |
| -0.00158 | 0.00117 | Total time taken 10min | 2235 | |
| -0.00226 | 0.00122 | Total time taken 8min | 2364 | |
| -0.00257 | 0.00126 | Total time taken 6min | 2387 | |
| -0.00255 | 0.00144 | Time on treatment screen 22s | 2024 | |
| -0.00241 | 0.00126 | Same responses to all belief qs | 2382 |
This table examines how the LATE estimate of beliefs on willingness to wash hands changes once apparently less attentive subjects are excluded. The first column specifies the relevant outcome (whether an individual expects to regularly wash their hands over the next 7 days and over the next 2 months). The subsequent columns specify the standard error associated with the LATE, the criterion which determines which subjects were dropped, and the resulting sample size
Table 21.
Dropping less attentive subjects III
| Outcome | LATE | SE | Exclusion criterion | n |
|---|---|---|---|---|
| Working from home (7 d) | -0.00534 | 0.00381 | None | 2391 |
| -0.00568 | 0.00396 | Total time taken 10min | 2221 | |
| -0.00589 | 0.00387 | Total time taken 8min | 2350 | |
| -0.00567 | 0.00383 | Total time taken 6min | 2373 | |
| -0.00646 | 0.00420 | Time on treatment screen 22s | 2011 | |
| -0.00591 | 0.00382 | Same responses to all belief qs | 2368 | |
| Working from home (2 m) | -0.00366 | 0.00368 | None | 2405 |
| -0.00305 | 0.00378 | Total time taken 10min | 2235 | |
| -0.00359 | 0.00370 | Total time taken 8min | 2364 | |
| -0.00383 | 0.00369 | Total time taken 6min | 2387 | |
| -0.00590 | 0.00414 | Time on treatment screen 22s | 2024 | |
| -0.00387 | 0.00367 | Same responses to all belief qs | 2382 |
This table examines how the LATE of beliefs on willingness to work from home changes once apparently less attentive subjects are excluded. The first column specifies the relevant outcome (whether an individual is willing to work from home over the next 7 days and over the next 2 months). The subsequent columns specify the standard error associated with the LATE, the criterion which determines which subjects were dropped, and the resulting sample size
In summary, the ‘fatalism effect’ that we find would appear to be a robust feature of our data. It persists regardless of whether we drop outliers or apparently less attentive subjects, whether we estimate a linear probability model or use probit, and if we introduce a second instrument (through use of the control group). Moreover, we find suggestive evidence of a fatalism effect within almost all of the subgroups we consider. Hence, while such a novel finding inevitably stands in need of replication, the data in our experiment do provide strong evidence that at least some individuals exhibit fatalism in the context of the COVID-19 pandemic.
Believing that COVID-19 is more infectious makes individuals less optimistic
Finally, we study the impact of changing people’s beliefs about COVID-19 on their optimism about the future. We expect people to become less optimistic about the future if they are told that experts estimate that is greater, as this may imply that the virus is likely to have a greater impact on the economy (and society in general). This is exactly what we find. Table 15 shows that when participants are told that is five, as opposed to two, they become significantly less optimistic. Quantitatively, a one-unit increase in beliefs about leads to a one percentage point drop in the share of participants that are optimistic about the future.36 These results are of interest insofar as optimism affects the evolution of key macroeconomic variables. Further, the result suggests that subjects understand that a higher rate of infectiousness translates into a more severe impact from the virus, confirming that they process the information provided in the experiment in the expected way.
Table 15.
The effect of beliefs about on optimism
| (1) | (2) | |
|---|---|---|
| ITT | LATE | |
| VARIABLES | Optimism | Optimism |
| Upper-bound condition ( = 5) | -0.0534*** | |
| (0.0202) | ||
| Beliefs about | -0.0103** | |
| (0.00461) | ||
| Constant | 0.494** | 0.960*** |
| (0.197) | (0.354) | |
| Lower-bound mean | 0.494 | |
| Controls | Yes | Yes |
| Observations | 2,405 | 2,405 |
| 0.032 |
This table presents the results from two regressions. The regression in the first column is an LPM whose independent variables are assignment to the upper-bound condition in addition to the demographic controls. The dependent variable is whether respondents feel optimistic about their future (a binary variable). The regression in the second column uses 2SLS, where assignment to the upper-bound condition acts as an instrumental variable for beliefs regarding . The dependent variable is whether participants are optimistic about their future. Robust standard errors in parentheses (*** , ** , * )
Towards a theory of fatalism
In this section, we propose a model that can explain the fatalism effect that we find in our experiment. The intuition behind the model is straightforward. If individuals come to believe that the virus is more infectious, then they revise upwards their assessment of the probability that they will get the virus even if they socially distance (or follow other best practices such as washing their hands frequently). But if individuals come to believe that they are likely to get the virus no matter what they do, then they may decide to ignore social distancing measures: in other words, we get a rational “fatalism effect”.
More formally, we consider an individual who must choose between two actions: socially distancing (denoted ) or instead socializing as usual (denoted ). If they socially distance, then there is a probability that they will contract the virus nonetheless (e.g. while doing essential shopping). If they socialize as usual, there is a further probability that their friends will give them the virus. Assuming independence of risks for simplicity, their overall probability of contracting the disease is thus in the scenario.37
If the individual socializes, they receive a psychic benefit and their expected utility is given by where measures the rate at which they are willing to trade the benefit of socializing off against the risk.38 If they instead socially distance, then their expected utility is . They therefore choose to socialize if and only if
| 3 |
where we have defined . To capture variation in the cost of socially distancing within the population, we will assume that is drawn from some strictly increasing probability distribution . Thus,
| 4 |
and so the probability that the individual socializes is strictly decreasing in . In other words, the greater the additional risk from socializing, the less likely the individual is to socialize.
Finally, note that the subjective probabilities p and q depend on the individual’s estimate of the infectiousness of the disease, denoted . Accordingly, we will write and ; and we will further assume that p and q are strictly increasing and differentiable functions.
We now examine how the individual’s willingness to socialize depends on their estimate of the infectiousness rate. To this end, it will be convenient to define , i.e. is the ratio of derivatives of the risk functions. It is also helpful to define fatalism more formally. We will say that there is a fatalism effect if and only if
| 5 |
that is, a small increase in the perceived infectiousness rate makes the individual more likely to socialize. We can then observe the following:39
Proposition 1
There is a fatalism effect if and only if .
Proposition 1 sheds some light on when fatalism is likely to arise. First, fatalism is more likely to arise when the background risk p is high. This is not a surprise: if p is large, then the individual is likely to contract the disease anyway so loses little from going outdoors. Second, fatalism is more likely to arise when the relative sensitivity of the background risk to the perceived infection rate is large. This is also not surprising: if increasing e dramatically increases the risk from staying at home, but only slightly increases the risk from socializing, then it may induce individuals to socialize. Finally, a fatalism effect becomes more likely when the socializing risk q becomes larger. While this effect is more subtle, the intuition can be readily grasped by considering the extreme case of : in that case, the individual will socialize with probability 1 (there is no risk in doing so), so increasing e cannot make them more likely to socialize (i.e. there can be no fatalism effect).
While useful, it may be hard to check whether the inequality in Proposition 1 holds in practice. As a result, we now study the relationship between the possibility of a fatalism effect and the overall probability that an individual contracts the disease if they socialize . To this end, let (suppressing the dependence of the probabilities on e for ease of notation) and define the function as follows:
| 6 |
We then have the following result:
Proposition 2
If there is a fatalism effect, then . Conversely, if , then there must exist probabilities and that are consistent with and generate a fatalism effect.
Proposition 2 provides an easily checked inequality that determines the possibility of a fatalism effect. For example, suppose that (i.e. both probabilities are equally sensitive to the estimated infectiousness rate e). Then , so fatalism is possible only if the individual thinks that they have at least a 75% chance of getting the disease if they socialize. Conversely, if the individual thinks that they have at least a 75% chance of getting the disease if they socialize, then we can always find probabilities p and q that generate a fatalism effect (e.g., if , then will work). Note that, in general, the probability need not be as high as 75% to generate fatalism. Indeed, given that , fatalism is consistent with an arbitrarily low probability provided that the ratio of derivatives is sufficiently large.
In summary, our model demonstrates that fatalism is possible under a range of conditions; and that a fatalism effect is more likely to arise if the probabilities p, q and the ratio of derivatives is large. Importantly, our model can also be reinterpreted in various ways. For example, while we described the action as ‘socializing as usual’, it could also be interpreted as ‘not regularly washing one’s hands frequently’ or ‘refusing to work from home’, allowing the model to explain the fatalism effect we also observe for these outcome variables. Similarly, the risks could be re-interpreted as not risks to oneself but rather as risks to others, allowing the model to explain why one might become fatalistic when (for example) deciding whether to visit an elderly relative.
As shown in the appendix, it is possible to extend the basic model in various ways. For example, it is possible to relax the assumption that the risks are independent; and it is also possible to allow for the conjunction of selfish and altruistic motives for social distancing behavior. These extensions slightly complicate the formulae above but do not change the main insights of the model. A more interesting extension is to recognize that the probabilities of contracting the disease p and q actually depend on the fraction who socially distance, which in turn depends on the probabilities p and q. It is thus possible to find ‘equilibrium’ probabilities and levels of social distancing: i.e., probabilities p and q that induce a level of social distancing that is then consistent with p and q.
Finally, we recognize that, while the model provides one explanation for the observed effect, it is not the only plausible explanation. For example, it might be that increasing individual assessments of the infectiousness of disease makes them think that many others will likely get the virus anyway, thereby diminishing the perceived social value of efforts to depress .40 While this explanation is logically distinct from ours, it is similar in spirit insofar as both explanations stress the damaging effect of high assessments on individuals’ motivation to combat the virus.
Conclusion
This paper describes three key results of an online experiment that studies individual beliefs and behaviors during the COVID-19 pandemic. First, individuals overestimate both the infectiousness and dangerousness of COVID-19 relative to expert opinion, a result that is in line with findings from the risk perception literature. Second, messages conveying expert estimates of partially correct people’s beliefs about the infectiousness of COVID-19. Third, individuals who believe that COVID-19 is more infectious are less willing to comply with social distancing measures, a finding we dub the “fatalism effect”.
We are not the first to uncover a fatalism effect in the context of decision-making under uncertainty. Earlier observational studies suggest that higher risk perceptions make anxious individuals less likely to engage in exercise, less likely to meet fruit and vegetable consumption guidelines and less willing to quit smoking (Ferrer and Klein (2015)). We contribute to this literature by demonstrating the existence of a fatalism effect using experimental methods and by providing evidence of such an effect in the context of a pandemic. We also develop a model that is capable of explaining the fatalism effect.
Our study has several limitations. For example, we consider the impact on stated behaviors; we do not measure the long-run impact of beliefs on behavior; and there is a possibility that our results may not generalize to those who do not complete online experiments. These limitations could, perhaps, be overcome by conducting long-term and large-scale natural field experiments.
These limitations notwithstanding, our findings may have important implications for policy in the face of the COVID-19 pandemic. In particular, they suggest substantial gains from providing the public with accurate information, insofar as this information revises public assessments of the virus’ infectiousness downwards. To get a sense of the magnitude of this effect, we perform a conservative benefit calculation, and find that revising individual assessments of downwards by just 8 units could create at least $3.7 billion in mortality benefits in the US simply by getting people to wash their hands more frequently.41 It might also be worthwhile for governments to track how people’s beliefs and sentiments change over the course of the pandemic, as this would inform the need for––and help target––policy interventions.
More generally, our study has implications for how policymakers can best mobilize populations in the face of a crisis. In particular, our findings suggest that policymakers need to tread a fine line, communicating in ways that convey the seriousness of the crisis, but without triggering a fatalism effect. Understanding how exactly to tread that line is an important task for future research.
Acknowledgements
We would like to thank Simge Andi, Luigi Butera, Rena Conti, Zoe Cullen, Keith Ericson, John Friedman, Tal Gross, Nikhil Kalyanpur, Rebecca Koomen, John List, Mario Macis, Paulina Olivia, Ricardo Perez-Truglia, Jim Rebitzer, Cass Sunstein, Dmitry Taubinsky and Jasmine Theilgaard for helpful suggestions. We thank Senan Hogan-Hennessey and Manuel Monti-Nussbaum for their valuable research assistance. Any opinions expressed in this paper are those of the authors and do not necessarily represent those of the institutions with which they are affiliated.
Content
Appendix A: Proofs
Appendix B: Dependent risks and altruistic concerns
Appendix C: Balance table
Appendix D: Descriptive analysis
Appendix E: Robustness checks and alternative specifications
Appendix F: Survey questions
A Proofs
Proof of Proposition 1.
From (4), we see that
| 7 |
Since , it follows that
| 8 |
which is precisely our result.
Proof of Proposition 2.
To prove the first claim, assume that there is a fatalism effect. Then (by Proposition 1) and so . To find a lower bound on the probability , consider the problem
| 9 |
When , the solution is and at which point . We thus conclude that in the case of . Meanwhile, when , we have the (interior) solution of and at which point . We thus conclude that in the case of . Either way, then, a fatalism effect implies that .
To prove the second claim, consider the pair of probabilities (p, q) defined by , if , and otherwise (if ). Clearly, these probabilities are consistent with . Moreover, if , and so . Hence, if , it must be that and so , i.e. the probabilities generate a fatalism effect.
B Dependent risks and altruistic concerns
In this section, we show how the basic set-up can be extended to allow for (1) altruistic concerns and (2) dependent risks. To allow from (1), we will assume (for simplicity) that socializing as usual involves meeting just one friend whom the agent may accidentally infect. Let denote the probability that the friend who contract the virus even if they socially distance and let denote the probability that the agent transmits the virus to their friend if they meet (so and are defined analogously to p and q). To allow for (2), let denote the (conditional) probability that the agent contracts the virus from their friend given that they would have done so anyway; and define analogously.
In this more general setting, the chance that the agent contracts the virus in the scenario is ; and so socializing increases their risk by . Similarly, socializing increases their friend’s risk by . Since the agent cares about both of these, the cost of meeting becomes
| 10 |
If (pure selfishness) and (independence), then we return to the baseline model.
As before, we have a fatalism effect if and only if
| 11 |
or equivalently
| 12 |
As in Proposition 1, then, fatalism is more likely when the probabilities p, , , are high or when the baseline risks p and are very responsive to e. Moreover, if we assume that both the agent and their friend have the same risk functions (i.e. and for all e), then this inequality reduces to
| 13 |
which is the same condition one would obtain by setting . In this case, then, introducing altruistic concerns makes no difference to the analysis .
C Balance table
Table 3.
Balance table
| Control | Lower-bound | Upper-bound | p-value | |
|---|---|---|---|---|
| Country = UK | 0.482 | 0.485 | 0.488 | 0.957 |
| Gender = male | 0.434 | 0.411 | 0.397 | 0.175 |
| Ages 18-44 | 0.782 | 0.737 | 0.758 | 0.035 |
| Ages 45-54 | 0.117 | 0.121 | 0.132 | 0.511 |
| Ages 55-64 | 0.076 | 0.098 | 0.077 | 0.080 |
| Ages 65-74 | 0.020 | 0.041 | 0.033 | 0.013 |
| Ages 75-84 | 0.005 | 0.003 | 0.001 | 0.172 |
| Years of education | 14.611 | 14.585 | 14.611 | 0.943 |
| Live with a partner | 0.534 | 0.543 | 0.523 | 0.596 |
| Live with children | 0.327 | 0.317 | 0.324 | 0.864 |
| Live with flat or housemates | 0.100 | 0.086 | 0.087 | 0.384 |
| Live with parents | 0.239 | 0.208 | 0.234 | 0.157 |
| Live with relatives | 0.120 | 0.089 | 0.105 | 0.045 |
| Live alone | 0.118 | 0.142 | 0.140 | 0.146 |
| Lives in a rural rea | 0.111 | 0.105 | 0.101 | 0.736 |
| Lives in a city | 0.327 | 0.343 | 0.294 | 0.032 |
| Lives in a suburban area | 0.276 | 0.278 | 0.296 | 0.486 |
| Lives in a village | 0.078 | 0.060 | 0.076 | 0.180 |
| Monthly income 2019 ($) | 4536.483 | 4224.130 | 4487.000 | 0.042 |
| Use social media | 0.931 | 0.919 | 0.912 | 0.226 |
| Took survey on mobile | 0.297 | 0.292 | 0.303 | 0.820 |
| n | 1197 | 1200 | 1213 |
All variables listed in this table are binary, with the exception of ‘years of education’ which is measured in full year increments. We use these variables as controls when conducting our statistical analyses. The final column reports the p-value from a t-test of equality of means between the three treatment groups
D Descriptive analysis
Table 4.
Pre-treatment variables
| VARIABLES | n | Mean | Min | Max |
|---|---|---|---|---|
| Gender = male | 3,579 | 0.414 | 0 | 1 |
| Age = 18 to 44 | 3,610 | 0.759 | 0 | 1 |
| Age = 45 to 54 | 3,610 | 0.123 | 0 | 1 |
| Age = 55 to 64 | 3,610 | 0.084 | 0 | 1 |
| Age = 65 to 74 | 3,610 | 0.031 | 0 | 1 |
| Age = 75 to 84 | 3,610 | 0.003 | 0 | 1 |
| Years of education | 3,610 | 14.60 | 6 | 18 |
| Politics = liberal | 3,610 | 0.544 | 0 | 1 |
| Politics = conservative | 3,610 | 0.219 | 0 | 1 |
| Lives with partner | 3,610 | 0.533 | 0 | 1 |
| Lives with children | 3,610 | 0.322 | 0 | 1 |
| Lives with flat/housemates | 3,610 | 0.091 | 0 | 1 |
| Lives with parents | 3,610 | 0.227 | 0 | 1 |
| Lives with other relatives | 3,610 | 0.105 | 0 | 1 |
| Lives alone | 3,610 | 0.134 | 0 | 1 |
| Lives in rural area | 3,610 | 0.106 | 0 | 1 |
| Lives in city/urban area | 3,610 | 0.321 | 0 | 1 |
| Lives in sub-urban area | 3,610 | 0.283 | 0 | 1 |
| Lives in village | 3,610 | 0.071 | 0 | 1 |
| Monthly pre-tax income in 2019 ($) | 3,608 | 4,416 | 1,000 | 14,634 |
| Know anyone with COVID-19 | 3,610 | 0.158 | 0 | 1 |
| Know anyone lost job due to pandemic | 3,610 | 0.569 | 0 | 1 |
| Been in contact with an infected person | 2,468 | 0.046 | 0 | 1 |
| Currently employed | 3,610 | 0.658 | 0 | 1 |
| Took survey on mobile | 3,610 | 0.298 | 0 | 1 |
| Furloughed | 3,610 | 0.051 | 0 | 1 |
| Consumes right-wing news | 3,610 | 0.307 | 0 | 1 |
| Has symptom: high temperature | 3,610 | 0.016 | 0 | 1 |
| Has symptom: chest pain | 3,610 | 0.033 | 0 | 1 |
| Has symptom: muscle soreness | 3,610 | 0.100 | 0 | 1 |
| Has symptom: diarrhea | 3,610 | 0.043 | 0 | 1 |
| Has symptom: headache | 3,610 | 0.211 | 0 | 1 |
| Has symptom: nausea | 3,610 | 0.024 | 0 | 1 |
| Has symptom: persistent cough | 3,610 | 0.153 | 0 | 1 |
| Has symptom: difficulty breathing | 3,610 | 0.042 | 0 | 1 |
| Number of symptoms | 3,610 | 0.622 | 0 | 8 |
| Has no COVID-19 symptoms | 3,610 | 0.624 | 0 | 1 |
| Likely to become unemployed | 3,610 | 0.112 | 0 | 1 |
| Believes unemployment will rise 10 p.p. by August | 3,610 | 0.889 | 0 | 1 |
| Believes economy will shrink by August | 3,610 | 0.094 | 0 | 1 |
| Likely to experience food insecurity | 3,610 | 0.273 | 0 | 1 |
| Believes restrictions will last more than 3 months | 3,610 | 0.482 | 0 | 1 |
| Country = UK (0 = US) | 3,610 | 0.485 | 0 | 1 |
| Uses social media | 3,610 | 0.920 | 0 | 1 |
| Misinformed about cures for COVID-19 | 3,610 | 0.264 | 0 | 1 |
| Correct beliefs about ETA for vaccine | 3,610 | 0.512 | 0 | 1 |
Table 5.
Post-treatment variables
| VARIABLES | n | Mean | Min | Max |
|---|---|---|---|---|
| Perceived risk of hospitalization after contracting COVID-19 | 2,428 | 31.74 | 0 | 100 |
| Perceived risk of dying if hospitalized for COVID-19 | 2,428 | 20.26 | 0 | 100 |
| Beliefs about | 2,428 | 23.58 | 0 | 100 |
| Optimistic about future prospects | 2,428 | 0.466 | 0 | 1 |
| Willing to work from home for seven days | 2,414 | 0.671 | 0 | 1 |
| Willing to work from home for 2 months | 2,428 | 0.674 | 0 | 1 |
| Willing to avoid meeting people in risk groups for 7 days | 2,427 | 0.920 | 0 | 1 |
| Willing to avoid meeting people in risk groups for 2 months | 2,428 | 0.925 | 0 | 1 |
| Willing to frequently wash hands for 7 days | 2,427 | 0.978 | 0 | 1 |
| Willing to frequently wash hands for 2 months | 2,428 | 0.978 | 0 | 1 |
Table 6.
Predictors of exaggerated CFR and beliefs
| VARIABLES | Overestimate CFR | Overestimate |
|---|---|---|
| In high-risk group | 0.114*** | 0.0469* |
| No COVID-19 symptoms | -0.0180 | -0.0129 |
| Consumes right-wing news | 0.0312 | 0.0452* |
| Currently employed | 0.0132 | 0.0154 |
| Conservative | 0.00594 | 0.0114 |
| Country = UK | -0.125*** | -0.0954*** |
| Gender = male | -0.174*** | -0.133*** |
| Over 55 years of age | 0.243*** | -0.0500 |
| Years of education | -0.0207*** | -0.0269*** |
| Lives with partner | 0.0150 | 0.0345 |
| Lives with children | 0.0748*** | 0.0307 |
| Lives with flat/house mates | -0.0701 | 0.00319 |
| Lives with parents | -0.00481 | 0.0589* |
| Lives with relatives | -0.00953 | -0.0199 |
| Lives alone | 0.0833 | 0.0484 |
| Lives in rural area | -0.0456 | -0.0371 |
| Lives in city | -0.00122 | 0.0381 |
| Lives in suburban area | -0.0821* | -0.0251 |
| Lives in village | -0.0493 | -0.0661 |
| Monthly income in 2019 (US $) | 1.04e-06 | 4.45e-06 |
| Uses social media | 0.0693 | 0.0583 |
| Took survey using mobile | 0.0137 | 0.00899 |
| Constant | 0.754*** | 1.062*** |
| Observations | 1,793 | 1,793 |
| 0.095 | 0.048 |
Table 7.
Treatment effects on beliefs about
| VARIABLES | % overestimate | Change in beliefs |
|---|---|---|
| Assigned to lower-bound condition () | -0.118*** | -10.61*** |
| (0.0191) | (1.035) | |
| Assigned to upper-bound condition () | -0.269*** | -4.564*** |
| (0.0192) | (1.374) | |
| Constant | 1.076*** | -6.356 |
| (0.0877) | (6.723) | |
| Control mean | 0.728 | 0.216 |
| Controls | Yes | Yes |
| Observations | 3,577 | 1,793 |
| 0.073 | 0.046 |
This table presents the results from two regressions. The regression presented in column 1 uses a linear probability model whose outcome is whether individuals overestimate post-treatment. The regression presented in column 2 uses OLS to model the determinants of the difference in pre- and post beliefs. The sample is smaller for the second regression because we randomly elicit beliefs pre-treatment only for half of the sample. Robust standard errors in parentheses (*** , ** , * )
E Robustness checks and alternative specifications
Table 8.
The effects of treatment assignment on beliefs about
| VARIABLES | Beliefs about | Beliefs about squared |
|---|---|---|
| Assigned to lower-bound | -7.889*** | -571.1*** |
| (1.139) | (108.7) | |
| Assigned to upper-bound | -2.797** | 50.80 |
| (1.260) | (123.6) | |
| Constant | 52.94*** | 3,734*** |
| (5.663) | (558.0) | |
| F-statistic | 23.1 | 18.25 |
| Controls | Yes | Yes |
| Observations | 3,577 | 3,577 |
| 0.048 | 0.044 |
This table presents two OLS regressions estimating the effect of being assigned to either of the treatment groups (relative to the control) on beliefs about . The outcome in column 1 is beliefs about , and the outcome in column 2 is squared beliefs about . Demographic control variables are used in both regressions
Table 10.
Testing for linear causal effects
| Willingness to avoid meeting people in high-risk groups | ||||
|---|---|---|---|---|
| VARIABLES | 7 days ITT | 7 days LATE | 2 months ITT | 2 months LATE |
| Assigned to upper-bound | -0.00740 | 0.0131 | ||
| Assigned to lower-bound | 0.0169 | 0.0389*** | ||
| Beliefs about | 0.00168 | -0.00474 | ||
| Beliefs about squared | -5.29e-05 | -2.66e-06 | ||
| Constant | 0.852*** | 0.871*** | 0.838*** | 1.004*** |
| 0.023 | 0.029 | |||
| Willingness to wash hands frequently | ||||
|---|---|---|---|---|
| 7 days ITT | 7 days LATE | 2 months ITT | 2 months LATE | |
| Assigned to upper-bound | -0.00105 | -0.00401 | ||
| Assigned to lower-bound | 0.00485 | 0.00917 | ||
| Beliefs about | 0.000177 | 0.000913 | ||
| Beliefs about squared | -1.09e-05 | -2.87e-05 | ||
| Constant | 0.962*** | 1.015*** | 0.971*** | 1.027*** |
| 0.013 | 0.014 | |||
| Willingness to work from home | ||||
|---|---|---|---|---|
| 7 days ITT | 7 days LATE | 2 months ITT | 2 months LATE | |
| Assigned to upper-bound | -0.0165 | -0.00315 | ||
| Assigned to lower-bound | 0.0113 | 0.0165 | ||
| Beliefs about | 0.00442 | 0.000482 | ||
| Beliefs about squared | -8.09e-05 | -3.56e-05 | ||
| Constant | -0.189** | -0.398** | -0.124 | -0.317 |
| 0.079 | 0.071 | |||
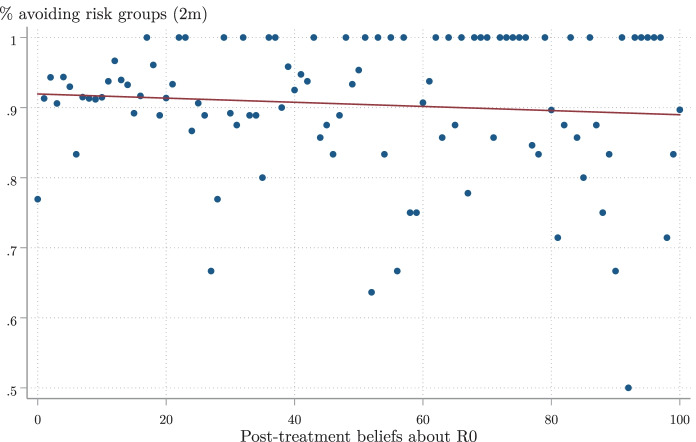
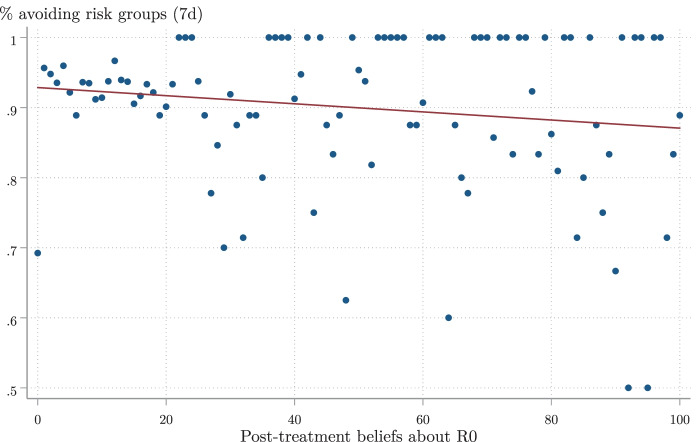
Fig. 4.
Raw associations I. Notes. This figure plots the share who state that they are willing to avoid high-risk groups within the next two months given every possible value of R0. No attempt is made to control for confounding variables
Fig. 5.
Raw associations II. Notes. This figure plots the share who state that they are willing to avoid high-risk groups within the next seven days given every possible value of R0. No attempt is made to control for confounding variables
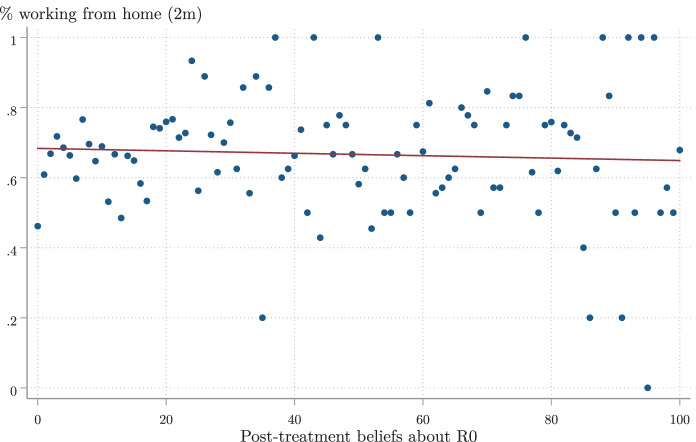
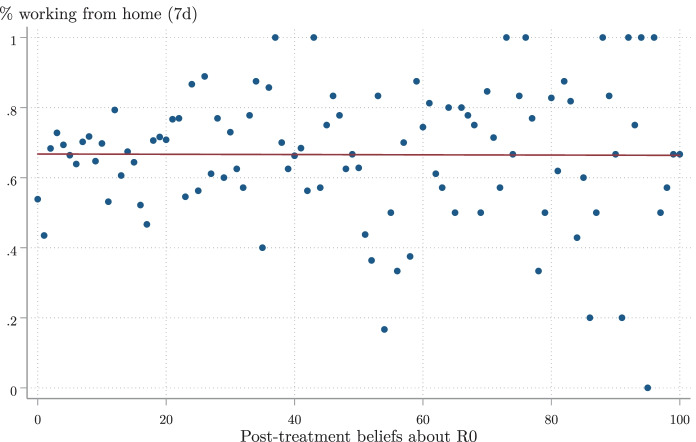
Fig. 6.
Raw associations III. Notes. This figure plots the share who state that they will work from home within the next two months given every possible value of R0. No attempt is made to control for confounding variables
Fig. 7.
Raw associations IV. Notes. This figure plots the share who state that they will work from home within the next seven days given every possible value of R0. No attempt is made to control for confounding variables
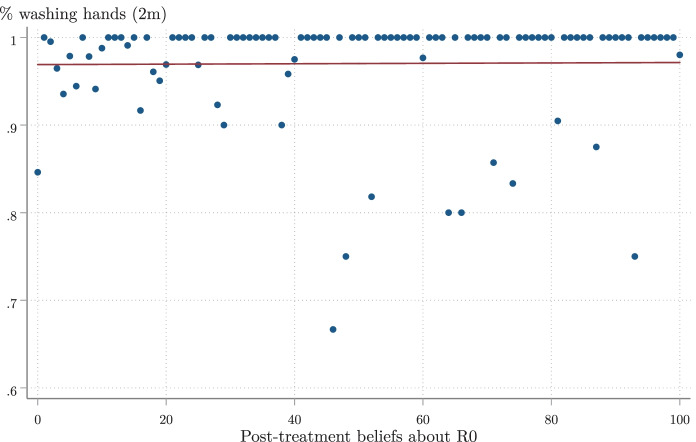
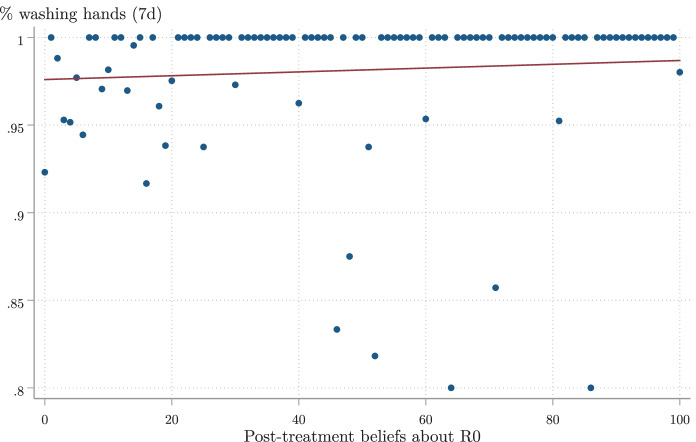
Fig. 8.
Raw associations V. Notes. This figure plots the share who state that they will regularly wash their hands over the next two months given every possible value of R0. No attempt is made to control for confounding variables
Fig. 9.
Raw associations VI. Notes. This figure plots the share who state that they will regularly wash their hands over the next seven days given every possible value of R0. No attempt is made to control for confounding variables
F Survey questions
Overview and sampling
We conducted two surveys, one for UK residents and one for US residents. The questions administered to UK residents are listed below. Some questions were adjusted slightly for the US audience (e.g., spelling, currencies, and the names of education qualifications). The survey took around ten minutes to complete, participants were recruited via Prolific Academic, and the survey was conducted using the Qualtrics platform. No screening or eligibility criteria were applied. We dropped participants who did not complete the full survey from our analysis sample (there were few dropouts, and there was no differential attrition). We paid participants the equivalent of $7.50 an hour in exchange for completing the survey. The order of questions and the response options within questions were randomized when appropriate.
Participants were debriefed at the end of the survey, and we recommended that they visit the CDC or NHS websites (depending on country of residence) for more information about COVID-19.
Survey introduction
Welcome and thanks for participating!
This is a study about the recent Coronavirus pandemic. In this study, you will be asked a set of questions about yourself, your beliefs, and your habits.
The survey should take around 10 minutes to complete.
By clicking the button below, you acknowledge that your participation in the study is voluntary, that you are at least 18 years of age, and that you are aware that you can end your participation in the study at any time and for any reason.
Your data will be kept strictly confidential and will not be shared with any third party. Your data will only be used for research purposes.
Pre-treatment questions
Q1. What do you think the risk is that someone your age is hospitalised if they contract the Coronavirus?
Slider from 0-100%
Q2. What do you think the risk is that someone your age would die, if they are hospitalised as a result of the Coronavirus?
Slider from 0-100%
Q3. On average, how many people do you think will catch the Coronavirus from one contagious person? Please only consider cases transmitted by coughing, sneezing, touch or other direct contact with the first contagious person.
Slider from 0-100
Half of the sample was randomly asked to answer questions 1–3, the other began the survey by answering question 4.
Q4. Please select your gender.
(1) Male (2) Female (3) Other
Q5. Please select your age range.
(1) 18-44 (2) 45-54 (3) 55-64 (4) 65-74 (5) 75-84 (6) 85+
Q6. What is the highest level of education you have completed?
Primary school
Secondary school (GCSE, I-level, AS level, or equivalent)
Secondary school (A-level, BTEC, or equivalent)
University diploma
Undergraduate degree
Postgraduate degree (e.g., MSc or PhD)
Q7. Do you live with any of the following? Please select all that apply.
(1) Partner (2) Children (3) Flat or house mates (4) Parents (5) Other relatives
Q8. What type of area do you live in?
(1) City (2) Town (3) Village (4) Rural
Q9. What was your monthly household income in 2019 (pre-tax)?
(1) €0-1999 (2) €2000-3999 (3) €4000-5999 (4) €6000-7999 (5) €8000-9999 (6) €10,000-11,999 (7) €12,000+
Q10. Do you have any of the following health conditions? Please select all that apply.
(1) Cardiovascular disease (2) Diabetes (3) Chronic respiratory disease (4) Hypertension (5) Asthma (5) Other serious condition (such as cancer) (6) None of the above
Q11. Have you had any of these symptoms within the last 48 hours? Please select all that apply.
(1) High temperature (2) Cough (3) Difficulty breathing or breathlessness (4) Chest pains (5) Headache (6) Muscle soreness (7) Nausea or vomiting (8) Diarrhea (9) None of the above
Q12. Do you personally know someone that has contracted Coronavirus?
(1) Yes (2) No
Q13. Do you personally know someone who has become unemployed because of how the Coronavirus has affected the economy?
Q14. Which political party do your views most align with?
(1) Conservative (2) Labour (3) Liberal Democrats (4) Other (please specify) (5) No political party
Q15. Do you use any of the following news sources (online or in person) on a weekly basis? Please select all that apply.
(1) The Sun (2) The Daily Mail (3) The Telegraph (4) The Guardian (5) The Times (6) The Financial Times (7) The Mirror (8) The Express (9) The Independent (10) The Star (11) BBC (12) ITV (13) Sky News (14) Metro Online (15) Huffington Post (16) Buzzfeed (17) The Canary (18) Westmonster (19) Another Angry Voice (20) Breitbart (21) None of the above
Q16. Do you use any of the following social media platforms? Please select all that apply.
(1) Facebook (2) Twitter (3) Instagram (4) LinkedIn (5) TikTok (6) Snapchat
Q17. Please identify the symptoms of the Coronavirus. Select all that apply.
(1) Fever (2) Dry cough (3) Wet cough (4) Sneezing (5) Rash (6) Chest pains (7) Fatigue (8) Stomach pain (9) Blindness (10) Shortness of breath (11) None of the above
Q18. In the last week, have you or a person who lives with you been in contact with someone who has the Coronavirus?
(1) Yes (2) No (3) Don’t know
Q19. For how long do you believe that Coronavirus-related restrictions on behaviour and free movement are likely to last for in the UK?
(1) One month or less (2) One to three months (3) Three to six months (4) Six months to a year (5) Over a year
Q20. What do you expect the general economic situation in this country to be in August 2020 (compared to January 2020)?
Slider from 1–7 (1 = a lot worse, 4 = the same, 7 = a lot better)
Q21. How likely is it that unemployment will increase by at least 10 percentage points in the next three months?
Slider from 1–7 (1 = extremely unlikely, 4 = neither likely nor unlikely, 7 = extremely likely)
Q22. In how many months do you think a vaccine against the Coronavirus will be made available for the public in the UK? Please select 48 if you believe that it will take more than 48 months.
Slider from 0–48
Q23. Are any of the following effective treatments for the Coronavirus? Please select “Effective treatment”, “Not an effective treatment”, or “Not sure” for each option.
(1) Drinking water every 15 minutes and keeping your mouth moist (2) Avoiding eating ice cream (3) Exposing yourself to sunshine (4) Gargling warm water with salt or vinegar (5) Using a hairdryer to blow hot hair toward your face (6) Ingesting colloidal silver (7) Taking C vitamins
Q24. Are you currently employed?
(1) Yes (2) No (3) No, recently laid off (4) Yes, furloughed
(If response is (1) or (4) to Q24): Q25. How likely is it that you will become unemployed as a result of the Coronavirus pandemic?
Slider from 1-7 (1 = extremely unlikely, 4 = neither likely nor unlikely, 7 = extremely likely)
Treatments
One third of the participants are randomly allocated to the control group. One third of the participants are randomly allocated to the upper-bound group. One third of the participants are randomly allocated to the lower-bound group. Please see Fig. 1 for the treatment images. Prior to administering the treatments, we say “We will now show you a poster about the Coronavirus pandemic. Please have a careful look at the poster and then press next to continue.” Participants are required to stay on the page with the treatment for fifteen seconds before being allowed to proceed.
Post-treatment questions
Q25. What do you think the risk is that someone your age is hospitalised if they contract the Coronavirus?
Slider from 0-100%
Q26. What do you think the risk is that someone your age would die, if they are hospitalised as a result of the Coronavirus?
Slider from 0-100%
Q27. On average, how many people do you think will catch the Coronavirus from one contagious person? Please only consider cases transmitted by coughing, sneezing, touch or other direct contact with the first contagious person.
Slider from 0-100
Q28. How likely are you to do the following during the coming seven days? (Answer 1–5, 1 = extremely unlikely, 3 = neither likely nor unlikely, 5 = extremely likely).
(1) Work from home (2) Avoid people at high risk (i.e., those that are either at least 70 years of age, pregnant, have a long-term condition, or a weakened immune system) (3) Wash your hands with water and soap several times a day
Q29. Assume that the Coronavirus outbreak is still ongoing 2 months from now. How likely would you be to do the following during the average week? (Answer 1–5, 1 = extremely unlikely, 3 = neither likely nor unlikely, 5 = extremely likely).
(1) Work from home (2) Avoid people at high risk (i.e., those that are either at least 70 years of age, pregnant, have a long-term condition, or a weakened immune system) (3) Wash your hands with water and soap several times a day
Q30. How optimistic are you about your future?
Slider from 1–7 (1 = very pessimistic, 4 = neither optimistic nor pessimistic, 7 = very optimistic)
Debriefing
Thank you for completing our survey.
The Coronavirus pandemic is ongoing and we are still developing our understanding of the risks that it poses to society. As such, the information that you were presented with in this survey may be incorrect.
Please refer to nhs.uk/conditions/coronavirus-covid-19/ for the latest up-to-date information about the Coronavirus pandemic.
Funding
AEA Registry No. AEARCTR-0005775. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations
Conflict of interest
We have no conflicts of interest or competing interests to declare.
Footnotes
Over 4 million deaths have been attributed to COVID-19 worldwide as of 26 August 2021 (Roser et al., 2020), resulting in trillions of dollars of mortality costs (Viscusi, 2020). Even non-fatal COVID-19 cases have had an estimated burden of trillions of dollars (Kniesner & Sullivan, 2020).
In other words, they are told that is two. ––the number of people that one infected person is likely to infect––is a central parameter that determines the evolution of the virus over time. As a result, it is frequently covered in the media and brought up in public statements by government officials (see, for example, Gallagher (2020)).
Kerwin (2018)––who studies HIV in Malawi––also finds evidence of fatalism among certain subgroups of the population he studies. Unlike Kerwin (2018), we actually find an average fatalism effect.
Kremer (1996) and Kerwin (2018) develop similar models in the context of risky sexual decisions. However, their models view the risky action as a continuous variable so are less suited to the (binary) set-up of our experiment.
The lower-bound treatment reduced average beliefs about the infectiousness of COVID-19 by around eight units relative to the control group.
See also Jensen (2010); Dupas (2011); Cruces et al. (2013); Wiswall and Zafar (2015); Liebman and Luttmer (2015); Armantier et al. (2016); Bergman (2020); Cavallo et al. (2017); Bleemer and Zafar (2018); Bursztyn et al. (2018); Conlon et al. (2018); Fuster et al. (2018); Dizon-Ross (2019) for other studies of the effects of beliefs. Two recent papers that use a similar methodology to the one adopted here are Cullen and Perez-Truglia (2018) and Bursztyn et al. (2021). Both use instrumental variables to estimate the causal effects of beliefs on behaviors.
See, for example, Acemoglu et al. (2020); Alvarez et al. (2020); Baker et al. (2020); Berger et al. (2020); Brynjolfsson et al. (2020); Cappelen et al. (2020); Farboodi et al. (2020); Van Bavel et al. (2020).
We also contribute to the literature on perceived self-efficacy (see, for instance, Bernard et al. (2011); Krishnan and Krutikova (2013); Tanguy et al. (2014) or Jorgensen et al. (2020)) by providing a theoretical model that explains when rational agents may believe that their actions make little difference to their outcomes.
Over this period, the total number of confirmed (tested) cases worldwide rose from 468,049 to 656,866 (Roser et al., 2020). In the UK, they almost doubled from 9,529 to 17,089, and in the USA from 69,194 to 124,665. The death toll in the USA rose from 1,050 to 2,191, and in the UK from 463 to 1019 (ibid). The UK introduced a full national lockdown two days prior (Holden, 2020), while various US states introduced restrictions on movement during the experimental period (Gershman, 2020).
More information about Prolific Academic can be found at https://www.prolific.co/. Peer et al. (2017) show that participants recruited via Prolific Academic are less dishonest, are less likely to fail attention checks, and produce higher quality data than participants recruited via other comparable online research platforms.
See Appendix D for descriptive statistics.
The survey also asked a range of socio-economic and demographic questions. We also collect data regarding, for example, media consumption, how informed participants are about COVID-19, which COVID-19 ‘best practices’ they engage in, and whether they know someone that has been infected. A full list of variables can be found in Appendix D.
We did not deceive participants when displaying the two treatments. There was, at the time of the experiment, substantial uncertainty regarding the infectiousness of COVID-19. For example, Liu et al. (2020) show that expert estimates of range from 1 to 6 in a review of epidemiological studies. Thus, the claim that ‘studies show that ’ and the (apparently contradictory) claim that ‘studies show that ’ were in fact both true at the time of the experiment.
The randomization is balanced. See Table 3 for a balance table.
We only elicit pre-beliefs for half the sample.
By multiplying participants’ beliefs regarding the risk of being hospitalized and the risk of dying conditional on being hospitalized, we obtain their implied beliefs about the Case Fatality Rate (CFR), which is the risk of dying conditional on contracting COVID-19.
We conducted power calculations prior to launching the experiment, using beliefs about as our primary outcome of interest. We assumed that participants would, on average, believe that was 2 in the lower-bound group, with a standard deviation of 15. We set the minimum detectable effect size to 2. This meant that we needed around 883 participants per group (i.e., 1,766 in total) in order to achieve 80% statistical power with a 5% significance level when comparing the lower- and the upper-bound groups.
We also note that, since participants have no financial incentives to misreport their beliefs, and since most people have a default preference for honesty (Abeler et al., 2019), it seems reasonable to take subject responses at face value. Moreover, the empirical evidence that does exist on incentivization in these types of belief experiments suggests little benefit from financial incentivization—and even a possibility that incentives can be harmful (Haaland et al., 2020). At worst, the lack of incentivization could have led to some subject inattention; but as we show in Sect. 3.4, this is not responsible for our main results.
When recording whether participants are willing to work from home, wash their hands, or avoid seeing people in high-risk groups, we ask participants: (1) “How likely are you to do the following during the coming seven days?” and (2) “Assume that the coronavirus outbreak is still ongoing 2 months from today. How likely would you be to do the following during the average week?” Respondents could answer on a scale from 1 to 5, with 5 being extremely likely and 1 being extremely unlikely.
Stated behaviors in online experiments have also been shown to be predictive of actual behaviors in a variety of domains (see, e.g., Mosleh et al. (2020)).
See, for example, Cass and Shell (1983); Akerlof and Shiller (2010); Benhabib et al. (2016); Di Bella and Grigoli (2019).
We use a similar specification as the one presented in Eq. (1) when estimating the Intention to Treat (ITT). The main difference is that we use people’s stated willingness to socially distance (i.e., work from home, avoid seeing people in high-risk groups, and frequently wash their hands for seven days and two months, respectively) as the outcomes. We also include participants in the control group when conducting this analysis.
These 2SLS regressions help us understand how beliefs are likely to influence people’s decisions to socially distance. We also learn how beliefs about influence people’s optimism. While we obtain consistent estimates of the effects of beliefs on the aforementioned outcomes, we are unable to measure the extent to which beliefs influence action through optimism as an intermediary variable. This is an interesting question for future research.
The pandemic appears to be having a profound effect on the economic outlook of the survey participants. For example, 89% believe that unemployment will grow by over 10 percentage points in the next three months, 57% claim to know someone that has become unemployed as a result of the pandemic, and 10% believe that they are likely to become unemployed as a result of the pandemic. See Appendix D for full descriptive statistics tables.
The symptoms that we asked about are: (1) high temperature, (2) chest pains, (3) muscle soreness, (4) diarrhea, (5) headache, (6) nausea, (7) a persistent cough, and (8) difficulty breathing. See https://www.who.int/news-room/q-a-detail/q-a-coronaviruses for more information about the symptoms of COVID-19.
As can be seen in Fig. 2, many individuals estimate that is 100 (since they are not allowed to provide higher estimates). Our estimated effects remain similar after dropping such individuals from the analysis.
See for instance Brody (1984); Steger and Witt (1989); Gwartney-Gibbs and Lach (1991); Savage (1993); DeJoy (1992); Spigner et al. (1993); Finucane et al. (2000).
Although the treatment assignment is random, we control for country of residence, gender, age, years of education, living situation (with partner, children, parents, relatives, or flat/housemates), living in an urban, rural or suburban area, monthly income in 2019, social media use, and whether the survey was completed on a mobile phone. These control variables are used throughout the results section.
Our finding that information updates people’s beliefs about the virus is broadly consistent with Bursztyn et al. (2020). The authors argue that two Fox News personas––Tucker Carlson and Sean Hannity––presented differing assessments regarding the seriousness of the virus, with Carlson warning viewers and Hannity downplaying the threat posed by the pandemic. Their analysis suggests that Hannity viewers held incorrect beliefs and changed behavior later than Carlson viewers, and were subsequently more likely to contract COVID-19.
It is not immediately clear how risk perceptions and beliefs will update in response to new information. There are, for example, studies suggesting that individuals fail to update their beliefs when presented with expert information (see, for example, Nyhan and Reifler (2010)). There is, however, evidence that people are better at updating their beliefs when subjects are given good news (Eil & Rao, 2011), as is the case here (COVID-19 is not as infectious as people think), or when they are making decisions in a ‘threatening’ environment (Garrett et al., 2018).
A portion of the respondents bunch at round numbers both before and after receiving the treatment (and in both treatment groups), suggesting that they are unsure regarding what to answer (Manski & Molinari, 2010)
The vast majority of participants state that they are willing to adhere to best practices. For example, 98% of participants in the lower-bound group state that they would wash their hands frequently if the pandemic continues for two months. Further, 94% of participants in the same group state that they would avoid seeing people in high-risk groups if the pandemic continues for two months. Fewer state that they would be willing to work from home (47%) if the pandemic continues for two months, largely because they are unable to work from home. These statistics are important because people’s willingness to engage in ‘best practice’ behaviors are central parameters in epidemiological models, and we do not yet have a good grasp of how behavior changes over time (Avery et al., 2020).
Observe that, since our results are based on randomly giving different individuals different information about , it is not possible that our results are due to reverse causality or omitted variables.
We also examine the linearity of the relationship between people’s beliefs about and their willingness to engage in best practices. To do this, we instrument for beliefs using two binary variables: a dummy variable representing assignment to the lower bound group, and a dummy representing assignment to the upper-bound group. Thus, we introduce the control group into the analysis (see Table 8 for first-stage regressions on beliefs). We then conduct a 2SLS IV estimation where we instrument beliefs about and squared beliefs about with the two aforementioned treatment dummies (see Table 10 for the results). We find that the estimated effects of beliefs about on people’s willingness to engage in the three behaviors are similar to those presented in Table 2, and that the point estimates of the squared terms are smaller than 0.001 (with 95% confidence intervals tightly bound around zero). While only suggestive, this provides some preliminary evidence that the relationship is roughly linear, at least over the relevant interval.
See also Figs. 4, 5, 6, 7, 8 and 9 for simple plots of posterior beliefs against stated willingness to socially distance. While some of these figures again suggest a negative relationship, they should be treated with even more caution since they do not even attempt to control for confounding variables (and, like the OLS estimates, are not based on any kind of randomized inference).
Table 15 excludes participants in the control group because we cannot be sure that the exclusion restriction holds for this group.
Recall that for any two independent events A, B.
The assumptions of additive utility with fixed can be dropped entirely if we are willing to directly assume that the agent is less likely to socialize if the risk from doing so increases. In this sense, these assumptions are superfluous.
All proofs appear in Appendix A.
To calculate this number, we assumed that handwashing reduces the risk of contracting the virus by 16% (see Rabie and Curtis (2006)) and that there will be an additional 208,000 COVID-19 deaths in the US (IMHE, 2020). Because this estimate ignores deaths after April 1 2021, it likely understates the true number. We also assumed a value of a statistical life of $10 million (see Viscusi and Aldy (2003) for a review of such estimates) and ignored any positive spillovers from handwashing (ignoring spillovers again suggests that we underestimate the benefits).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Abeler J, Nosenzo D, Raymond C. Preferences for truth-telling. Econometrica. 2019;87:1115–1153. doi: 10.3982/ECTA14673. [DOI] [Google Scholar]
- Acemoglu, D., Chernozhukov, V., Werning, I., & Whinston, M. D. (2020). A multi-risk SIR model with optimally targeted lockdown. NBER Working Papers.
- Akerlof, G. A., & Shiller, R. J. (2010). Animal spirits: How human psychology drives the economy, and why it matters for global capitalism. Princeton University Press.
- Alvarez, F. E., Argente, D., & Lippi, F. (2020). A simple planning problem for COVID-19 lockdown. NBER Working Papers.
- Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD. How will country-based mitigation measures influence the course of the Covid-19 epidemic? The Lancet. 2020;395:931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armantier O, Nelson S, Topa G, van der Klaauw W, Zafar B. The price is right: updating inflation expectations in a randomized price information experiment. Review of Economics and Statistics. 2016;98:503–523. doi: 10.1162/REST_a_00499. [DOI] [Google Scholar]
- Avery, C., Bossert, W., Clark, A., Ellison, G., & Ellison, S. F. (2020). Policy implications of models of the spread of coronavirus: perspectives and opportunities for economists. NBER Working Papers.
- Baker, S. R., Bloom, N., Davis, S. J., Kost, K. J., Sammon, M. C., & Viratyosin, T. (2020). The unprecedented stock market impact of COVID-19. NBER Working Papers.
- Benhabib J, Liu X, Wang P. Sentiments, financial markets, and macroeconomic fluctuations. Journal of Financial Economics. 2016;120:420–443. doi: 10.1016/j.jfineco.2016.01.008. [DOI] [Google Scholar]
- Berger, D. W., Herkenhoff, K. F., & Mongey, S. (2020). An SEIR infectious disease model with testing and conditional quarantine. NBER Working Papers.
- Bergman P. Parent-child information frictions and human capital investment: evidence from a field experiment investment. Journal of Political Economy. 2020;129:286–322. doi: 10.1086/711410. [DOI] [Google Scholar]
- Bernard, T., Dercon, S., & Taffesse, A. S. (2011). Beyond fatalism: an empirical exploration of self-efficacy and aspirations failure in Ethiopia. CSAE Working Paper Series.
- Bleemer Z, Zafar B. Intended college attendance: evidence from an experiment on college returns and costs. Journal of Public Economics. 2018;157:184–211. doi: 10.1016/j.jpubeco.2017.11.002. [DOI] [Google Scholar]
- Briscese, G., Lacetera, N., Macis, M., & Tonin, M. (2020). Compliance with COVID-19 social-distancing measures in italy: the role of expectations and duration. NBER Working Papers. [DOI] [PMC free article] [PubMed]
- Brody CJ. Differences by sex in support for nuclear power. Social forces. 1984;63:209–228. doi: 10.2307/2578866. [DOI] [Google Scholar]
- de Bruin WB, Saw H-W, Goldman DP. Political polarization in us residents’ COVID-19 risk perceptions, policy preferences, and protective behaviors. Journal of risk and uncertainty. 2020;61:177–194. doi: 10.1007/s11166-020-09336-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brynjolfsson, E., Horton, J., Ozimek, A., Rock, D., Sharma, G., & Ye, H. Y. T. (2020). COVID-19 and remote work: an early look at us data. NBER Working Papers.
- Bursztyn L, Cantoni D, Yang D, Yuchtman N, Zhang J. Persistent political engagement: social interactions and the dynamics of protest movements. American Economic Review: Insights. 2021;3:233–250. [Google Scholar]
- Bursztyn, L., González, A. L., & Yanagizawa-Drott, D. (2018). Misperceived social norms: female labor force participation in Saudi Arabia. NBER Working Papers.
- Bursztyn, L., Rao, A., Roth, C., & Yanagizawa-Drott, D. (2020). Misinformation during a pandemic. University of Chicago, Becker Friedman Institute for Economics Working Paper.
- Cappelen, A. W., Falch, R., Sørensen, E. Ø., & Tungodden, B. (2020). Solidarity and fairness in times of crisis. NHH Dept. of Economics Discussion Paper. [DOI] [PMC free article] [PubMed]
- Cass D, Shell K. Do sunspots matter? Journal of Political Economy. 1983;91:193–227. doi: 10.1086/261139. [DOI] [Google Scholar]
- Cavallo A, Cruces G, Perez-Truglia R. Inflation expectations, learning, and supermarket prices: evidence from survey experiments. American Economic Journal: Macroeconomics. 2017;9:1–35. [Google Scholar]
- Cawley J, Ruhm CJ. The economics of risky health behaviors. Handbook of health economics. 2011;2:95–199. doi: 10.1016/B978-0-444-53592-4.00003-7. [DOI] [Google Scholar]
- CDC (2020). Severe outcomes among patients with Coronavirus Disease 2019 (COVID-19) – United States, February 12–March 16, 2020. Accessed 2021-13-10. https://www.cdc.gov/mmwr/volumes/69/wr/mm6912e2.htm [DOI] [PMC free article] [PubMed]
- Conlon, J. J., Pilossoph, L., Wiswall, M., & Zafar, B. (2018). Labor market search with imperfect information and learning. NBER Working Papers.
- Cruces G, Perez-Truglia R, Tetaz M. Biased perceptions of income distribution and preferences for redistribution: evidence from a survey experiment. Journal of Public Economics. 2013;98:100–112. doi: 10.1016/j.jpubeco.2012.10.009. [DOI] [Google Scholar]
- Cullen, Z., & Perez-Truglia, R. (2018). How much does your boss make? the effects of salary comparisons. NBER Working Papers.
- DeJoy DM. An examination of gender differences in traffic accident risk perception. Accident Analysis & Prevention. 1992;24:237–246. doi: 10.1016/0001-4575(92)90003-2. [DOI] [PubMed] [Google Scholar]
- Di Bella G, Grigoli F. Optimism, pessimism, and short-term fluctuations. Journal of Macroeconomics. 2019;60:79–96. doi: 10.1016/j.jmacro.2019.01.010. [DOI] [Google Scholar]
- Dizon-Ross R. Parents’ beliefs about their children’s academic ability: implications for educational investments. American Economic Review. 2019;109:2728–65. doi: 10.1257/aer.20171172. [DOI] [Google Scholar]
- Dupas P. Do teenagers respond to hiv risk information? Evidence from a field experiment in kenya. American Economic Journal: Applied Economics. 2011;3:1–34. [Google Scholar]
- Eil D, Rao JM. The good news-bad news effect: asymmetric processing of objective information about yourself. American Economic Journal: Microeconomics. 2011;3:114–38. [Google Scholar]
- Farboodi, M., Jarosch, G., & Shimer, R. (2020). Internal and external effects of social distancing in a pandemic. NBER Working Papers.
- Ferrer RA, Klein WM. Risk perceptions and health behavior. Current opinion in psychology. 2015;5:85–89. doi: 10.1016/j.copsyc.2015.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fetzer, T., Hensel, L., Hermle, J., & Roth, C. (2020). Coronavirus perceptions and economic anxiety. arXiv preprint.
- Finucane ML, Slovic P, Mertz CK, Flynn J, Satterfield TA. Gender, race, and perceived risk: the “white male” effect. Health, risk & society. 2000;2:159–172. doi: 10.1080/713670162. [DOI] [Google Scholar]
- Fuster, A., Perez-Truglia, R., Wiederholt, M., & Zafar, B. (2018). Expectations with endogenous information acquisition: an experimental investigation. NBER Working Papers.
- Gallagher, J. (2020). Coronavirus r: is this the crucial number? Accessed: 2021-13-10. https://www.bbc.co.uk/news/health-52473523
- Garrett N, González-Garzón AM, Foulkes L, Levita L, Sharot T. Updating beliefs under perceived threat. Journal of Neuroscience. 2018;38:7901–7911. doi: 10.1523/JNEUROSCI.0716-18.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gershman, J. (2020). A guide to state coronavirus lockdowns. Accessed 2021-13-10. https://www.wsj.com/articles/a-state-by-state-guide-to-coronavirus-lockdowns-11584749351
- Gormsen, N. J., & Koijen, R. S. (2020). Coronavirus: impact on stock prices and growth expectations. University of Chicago, Becker Friedman Institute for Economics Working Paper.
- Greenstone, M., & Nigam, V. (2020). Does social distancing matter? University of Chicago, Becker Friedman Institute for Economics Working Paper.
- Guerrieri, V., Lorenzoni, G., Straub, L., & Werning, I. (2020). Macroeconomic implications of COVID-19: can negative supply shocks cause demand shortages? NBER Working Papers.
- Gwartney-Gibbs PA, Lach DH. Sex differences in attitudes toward nuclear war. Journal of Peace Research. 1991;28:161–174. doi: 10.1177/0022343391028002003. [DOI] [Google Scholar]
- Haaland, I., Roth, C., & Wohlfart, J. (2020). Designing information provision experiments. CEBI Working Paper Series.
- Holden, M. (2020). Uk lockdown put in place to protect the nhs during COVID-19. Accessed 2020-18-05. https://www.weforum.org/agenda/2020/03/britain-wakes-up-to-coronavirus-lockdown-confusion-continues/
- Hsiang, S., Allen, D., Annan-Phan, S., Bell, K., Bolliger, I., Chong, T., Druckenmiller, H., Hultgren, A., Huang, L. Y., Krasovich, E. et al. (2020). The effect of large-scale anti-contagion policies on the coronavirus (COVID-19) pandemic. MedRxiv Working Paper. [DOI] [PubMed]
- IMHE (2020). Covid-19 projections. Accessed: 2021-13-10. https://covid19.healthdata.org/united-states-of-america?view=total-deathstab=trend
- Jensen R. The (perceived) returns to education and the demand for schooling. Quarterly Journal of Economics. 2010;125:515–548. doi: 10.1162/qjec.2010.125.2.515. [DOI] [Google Scholar]
- Jorgensen, F., Bor, A., & Bang Petersen, M. (2020). Compliance without fear: predictors of protective behavior during the first wave of the COVID-19 pandemic. Working Paper. [DOI] [PMC free article] [PubMed]
- Kerwin, J. T. (2018). Scared straight or scared to death? the effect of risk beliefs on risky behaviors. Working Paper.
- Kniesner TJ, Sullivan R. The forgotten numbers: a closer look at COVID-19 non-fatal valuations. Journal of Risk and Uncertainty. 2020;61:155–176. doi: 10.1007/s11166-020-09339-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kremer M. Integrating behavioral choice into epidemiological models of aids. Quarterly Journal of Economics. 1996;111:549–573. doi: 10.2307/2946687. [DOI] [Google Scholar]
- Krishnan P, Krutikova S. Non-cognitive skill formation in poor neighbourhoods of urban India. Labour Economics. 2013;24:68–85. doi: 10.1016/j.labeco.2013.06.004. [DOI] [Google Scholar]
- Lewnard, J. A., & Lo, N. C. (2020). Scientific and ethical basis for social-distancing interventions against COVID-19. The Lancet Infectious Diseases, 20. [DOI] [PMC free article] [PubMed]
- Liebman JB, Luttmer EF. Would people behave differently if they better understood social security? Evidence from a field experiment. American Economic Journal: Economic Policy. 2015;7:275–99. [Google Scholar]
- Liu, Y., Gayle, A. A., Wilder-Smith, A., & Rocklöv, J. (2020). The reproductive number of COVID-19 is higher compared to sars coronavirus. Journal of Travel Medicine, 27. [DOI] [PMC free article] [PubMed]
- Manski CF, Molinari F. Rounding probabilistic expectations in surveys. Journal of Business & Economic Statistics. 2010;28:219–231. doi: 10.1198/jbes.2009.08098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosleh, M., Pennycook, G., & Rand, D. G. (2020). Self-reported willingness to share political news articles in online surveys correlates with actual sharing on twitter. Plos one, 15, e0228882. [DOI] [PMC free article] [PubMed]
- Nyhan B, Reifler J. When corrections fail: the persistence of political misperceptions. Political Behavior. 2010;32:303–330. doi: 10.1007/s11109-010-9112-2. [DOI] [Google Scholar]
- Office, C. (2020). Coronavirus action plan: a guide to what you can expect across the UK. Accessed 2021-13-10. https://www.gov.uk/government/publications/coronavirus-action-plan/coronavirus-action-plan-a-guide-to-what-you-can-expect-across-the-uk.
- Peer E, Brandimarte L, Samat S, Acquisti A. Beyond the turk: alternative platforms for crowdsourcing behavioral research. Journal of Experimental Social Psychology. 2017;70:153–163. doi: 10.1016/j.jesp.2017.01.006. [DOI] [Google Scholar]
- Rabie T, Curtis V. Handwashing and risk of respiratory infections: a quantitative systematic review. Tropical Medicine & International Health. 2006;11:258–267. doi: 10.1111/j.1365-3156.2006.01568.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reis, R. (2020). How do countries differ in their response to the coronavirus economic crisis? Accessed: 2020-18-05. https://www.theguardian.com/commentisfree/2020/apr/03/coronavirus-economic-crisis-financial-impact
- Roser, M., Ritchie, H., Ortiz-Ospina, E., & Hasell, J. (2020). Coronavirus disease (COVID-19). Accessed 2020-18-05. https://ourworldindata.org/coronavirus
- Savage I. Demographic influences on risk perceptions. Risk Analysis. 1993;13:413–420. doi: 10.1111/j.1539-6924.1993.tb00741.x. [DOI] [PubMed] [Google Scholar]
- Shapiro J, Wu S. Fatalism and savings. Journal of Socio-Economics. 2011;40:645–651. doi: 10.1016/j.socec.2011.05.003. [DOI] [Google Scholar]
- Slovic, P. E. (2000). The perception of risk.. Earthscan Publications.
- Spigner C, Hawkins WE, Loren W. Gender differences in perception of risk associated with alcohol and drug use among college students. Women & Health. 1993;20:87–97. doi: 10.1300/J013v20n01_06. [DOI] [PubMed] [Google Scholar]
- Steger MAE, Witt SL. Gender differences in environmental orientations: a comparison of publics and activists in Canada and the US. Western Political Quarterly. 1989;42:627–649. [Google Scholar]
- Tanguy, B., Dercon, S., Orkin, K., & Taffesse, A. S. (2014). The future in mind: aspirations and forward-looking behaviour in rural Ethiopia.
- Van Bavel JJ, Baicker K, Boggio PS, Capraro V, Cichocka A, Cikara M, Crockett MJ, Crum AJ, Douglas KM, Druckman JN, et al. Using social and behavioural science to support COVID-19 pandemic response. Nature Human Behaviour. 2020;4:1–12. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- Viscusi WK. Do smokers underestimate risks? Journal of Political Economy. 1990;98:1253–1269. doi: 10.1086/261733. [DOI] [Google Scholar]
- Viscusi WK. Pricing the global health risks of the COVID-19 pandemic. Journal of Risk and Uncertainty. 2020;61:101–128. doi: 10.1007/s11166-020-09337-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viscusi WK, Aldy JE. The value of a statistical life: a critical review of market estimates throughout the world. Journal of Risk and Uncertainty. 2003;27:5–76. doi: 10.1023/A:1025598106257. [DOI] [Google Scholar]
- Weiss, H. H. (2013). The sir model and the foundations of public health. Working Paper.
- WHO (2020). COVID-19 strategy update - 14 April 2020. Accessed 2021-13-10. https://www.who.int/publications-detail/covid-19-strategy-update---14-april-2020
- Wiswall M, Zafar B. Determinants of college major choice: identification using an information experiment. Review of Economic Studies. 2015;82:791–824. doi: 10.1093/restud/rdu044. [DOI] [Google Scholar]