Abstract
Opioid abuse is a serious problem in the society. Since the first months of COVID-19 pandemic, several myths, rumors and misconceptions have been spread about the benefits of opium consumption for COVID-19 outcome. In addition, data are limited on the relationship between opium abuse and COVID-19 mortality amongst hospitalized COVID-19 patients. In this historical cohort study, we assessed the risks of several variables for mortality amongst all hospitalized COVID-19 patients from the beginning of COVID-19 pandemic in South of Iran from March 15th, 2021 to October 14th, 2021. Data was acquired from the Medical Care Monitoring Center (MCMC), affiliated to Shiraz University of Medical Sciences. A total of 64,427 hospitalized COVID-19 patients were included into the analysis. The mortality rate was 10.59% (n = 6756). Of all, 2030 (3.15%) patients—1702 males and 328 females—reported the positive history of opium abuse with a mean age of 57 ± 17.21 years. The results of multivariable risk showed that the positive history of opium abuse had a significant association with mortality (adjusted RR: 1.173; p = 0.007). Other significant predictive risk factors were male gender, elder ages, and comorbidities such as pulmonary diseases, cardiovascular disease, cancer, nephrological diseases, neurological diseases, and diabetes. However, being a health care worker and having thyroid gland diseases were protective factors amongst hospitalized COVID-19 patients (adjusted RR: 0.650 and 0.642; p = 0.040 and < .0001, respectively). Opium abuse is a risk factor for mortality amongst hospitalized COVID-19 patients. It is vital to educate societies about the consequences of unauthorized opium consumption.
Keywords: COVID-19, Opium abuse, Mortality, Retrospective cohort, Iran
Introduction
Opium abuse is a serious global problem. According to the latest World Drug Report in 2018, approximately 269 million people suffer from drug use disorders (substances such as opium, alcohol, marijuana, nicotine, cocaine, and heroin),worldwide, which was 30% more than the 2009 estimates (Mahdavi & Aliramezany, 2021). Also, it is estimated that 2.8–9.0% of Iranians are opium abusers (Ignaszewski, 2021). Misconceptions are prevalent in the society regarding the befits and risks of opium consumption in human health and COVID-19 infection (Mahdavi & Aliramezany, 2021). There are plenty of studies about the association between comorbidities and COVID-19 mortality (Sanyaolu et al., 2020; Zaki et al., 2020). Diabetes, hypertension, cardiovascular disease, and higher cholesterol levels are associated with higher COVID-19 severity and mortality (Yang et al., 2020). Based on a systematic review of a total of 54 articles, the links between COVID-19 and some comorbidities such as cancer, kidney disease, and stroke are unclear and need further evaluation (Zaki et al., 2020). Moreover, smoking appears to be associated with a worse prognosis (Patanavanich & Glantz, 2020; Zaki et al., 2020).. Since the effect of opium abuse on COVID-19 prognosis is not well understood, this study was conducted to investigate the association between opium abuse and mortality among hospitalized COVID-19 patients. Due to the lack of a data base for gathering data in the general population, this investigation was performed on hospitalized patients.
The scientific evidence on the impact of opioid abuse on health and disease is conflicting (Ignaszewski, 2021; Mahdavi & Aliramezany, 2021). Besides the insufficient scientific evidence, some myths and rumours have been spread by social media in the community which claimed that opium consumption has protective effects against COVID-19 infection and COVID-19 infection less affect the people with the mild COVID-19 infection (Mahdavi & Aliramezany, 2021). In addition, opium abuse, according to traditional beliefs and studies, has therapeutic effects in cases of headache, toothache, earache, and sexual impotence. It also has analgesic, hypnagogic, antitussive, and antidiarrheal effects (Karam et al., 2004; Farahani et al., 2015; Hasandokht et al., 2018). A recent systematic review found no evidence that opium use protects against cardiovascular disease (Hasandokht et al., 2018; Adib et al., 2020; Riahi et al., 2021). Several studies with small sample sizes have shown that subjects with substance use disorders (SUDs) are at a higher risk of contracting COVID-19 infection (Pirnia et al., 2020; Riahi et al., 2021), as well as poor outcomes (Dubey et al., 2020). Since identification of factors linked to COVID-19 mortality can help in risk reduction and can cause appropriates interventions (Zaki et al., 2020), more studies are needed to better determine the relationship between opium abuse and mortality amongst COVID-19 patients. The main aim of this study was to investigate the association between opium abuse and mortality amongst hospitalized COVID-19 patients in an Iranian population during 2021.
Methods
In this historical cohort study, we assessed the risk of mortality for several variables amongst all hospitalized COVID-19 patients from the early months of COVID-19 pandemic in Fars province, South of Iran, from March 15th, 2021 to October 14th, 2021. This study was approved by Shiraz University of Medical Sciences (SUMS) Local Ethics Committee by the code: IR.SUMS.REC.1399.1165.
According to legal and regulatory framework, demographic, medical history, and clinical data for any suspected or confirmed COVID-19 hospital admission or transfer have to be registered by an ER physician. Therefore, for our research purpose, we used an administrative data repository, the “Medical Care Monitoring Center” (MCMC). By announcing COVID-19 pandemic, this system was updated by the Vice-Chancellor of Treatment Affairs of SUMS to record data in a separate database about all suspected COVID-19 hospitalizations (Gray Zones admissions) in all 31 counties under cover of the SUMS, which includes 47 hospitals (https://sums.ac.ir/page-Main/fa/0/form/pId770).
The inclusion criteria were as followed: age ≥ 18 years—since opium abuse is rare at younger ages—and confirmed COVID-19 disease. While, opium abuse defines as any compulsive urge to use opioid (or opioid derivative) drugs, the definition would be different in the regions that opium abuse is a tradition, which is consumed to alleviate acute and chronic pain, mostly by old people. That is, in Iran, the most common type of opium abuse is to inhale on smoke of the burning dark crude material retrieved from Papaver somniferum (Nakhaee et al., 2020). Therefore, in this study, we considered the recent definition.
An individual was excluded if data was not available for any of the studied variables or a patient had more than one admission. Moreover, since the endpoint of study was the hospital outcome of each patient (deceased or discharged), those who were still hospitalized or transferred to another ward or hospital were excluded. For this purpose, MCMC has a feature that shows if a hospitalized COVID-19 patient is (Mahdavi & Aliramezany, 2021) deceased due to COVID-19, (Ignaszewski, 2021) cured of the COVID-19 and discharged from the hospital, (DRUGS UNOO, LABOR, 2021) transferred to another ward (non-Gray Zone) in the same hospital for other medical complaints, or (Sanyaolu et al., 2020) transferred to another hospital to manage for other medical complaints. The reason for excluding the second two conditions was the uncertainty about outlook of COVID-19 and if a patient cured of the COVID-19 or not, since our repository did not contain data after the transfers.
The acquired dataset includes admission date, demographic variables (gender, age), medical history (being health care worker, smoking, opium abusing) and underlying medical condition (HIV or immunodeficiency, pulmonary diseases, cancer, thyroid diseases, hematological diseases, hepatic diseases, nephrological disease, neurological diseases, hyperlipidemia, diabetes, cardiovascular diseases, and hypertension), as well as outcome and its’ date. Data access request was sent to the Vice-Chancellor of Treatment Affairs; upon accepting, the Information Technology (IT) unit of SUMS retrieved our target variables using SQL (Structured Query Language).
For statistical analysis we used ‘GLM’ [denoting Generalized Linear Model], ‘Sandwich’ and ‘lmtest’ packages, implemented in R programing language (version 4.0.4 for MacOS). Hospital outlook of each patients was the outcome (dependent) variable, opium abusing was the exposure variable, and all of the remaining variables considered as the confounding (independent variables). Initially, univariate odds ratio (OR) was calculated for each independent variable. Variables with p value < 0.25 were selected for the multivariable analysis (Bursac et al., 2008). Since OR always overestimates the risk ratio in cohort studies, the single variable relative risk (RR) and adjusted RR were calculated; hence, we used the Poisson single univariable and multivariable regression with robust standard errors, instead of logistic regression (Knol et al., 2012). The null hypothesis was that the coefficient for the association between each independent variable and the outlook of hospitalization due to the COVID-19 was equal to zero. A p value < 0.05 was considered statistically significant. Furthermore, to compare opium-user and non-user hospitalized COVID-19 patients, we used ‡ Pearson’s Chi-square test (or Fisher’s exact test) and independent t-test for qualitative and quantitative variables, respectively. The R codes are yielded in appendix 1.
Results
A total of 64,427 hospitalized COVID-19 patients were included into the analysis (Fig. 1). The mortality rate was 10.59% (n = 6756). Of all, 2030 (3.15%) patients—1702 male and 328 female—reported the positive history of opium abuse with a mean age of 57 ± 17.21 years, ranging 18–96 years old. Opium abuser patients were significantly older and male, and had higher rates of positive history of cigarette smoking, numbers of comorbidities, and mortality (p = 0.032, < 0.0001, < 0.0001, < 0.0001, < 0.0001, 0.001) (Table 1).
Fig. 1.
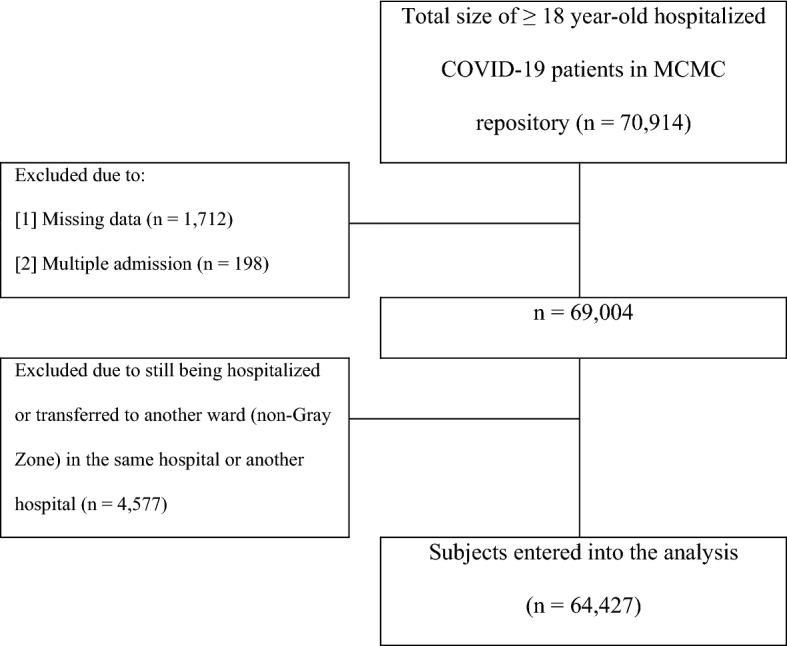
Flowchart of the included subjects into the analysis from MCMC repository
Table 1.
Comparison of hospitalized COVID-19 patients who were opium abuser and opium non-abuser
| Variable | Opium abusers (n = 2030) | Opium non-abusers (n = 62,397) | pa |
|---|---|---|---|
| Age | 57.00 ± 17.21 | 56.11 ± 18.46 | 0.032b |
| Gender | |||
| Male | 1702 (83.8%) | 31,875 (51.1%) | < 0.0001 |
| Female | 328 (16.2%) | 30,522 (48.9%) | |
| History of smoking | |||
| Positive | 750 (36.9%) | 1035 (1.07%) | < 0.0001 |
| Negative | 1280 (63.1%) | 61,362 (98.3%) | |
| Number of comorbidities | |||
| 0 | 0 (0) | 3805 (6.1%) | < 0.0001 |
| 1 | 13 (0.6%) | 14,374 (23.0%) | |
| 2 | 222 (10.9%) | 19,886 (31.9%) | |
| 3 | 526 (25.9%) | 13,469 (21.6%) | |
| 4 | 585 (28.8%) | 7016 (11.2%) | |
| 5 | 389 (19.2%) | 2808 (4.5%) | |
| ≥ 6 | 295 (14.5%) | 1039 (1.7%) | |
| Mean number of comorbidities | 4.05 ± 1.38 | 2.29 ± 1.32 | < 0.0001b |
| Outcome | |||
| Deceased | 260 (12.8%) | 6496 (10.4%) | 0.001 |
| Discharged | 1770 (87.2%) | 55,901 (89.6%) |
aPearson’s Chi-square test or Fisher’s exact test
bIndependent t-test
Table 2 depicts the univariate ORs. positive history of opium abuse was statistically associated with death amongst hospitalized adult COVID-19 patients (OR: 1.264; p = 0.001). Positive history of smoking, immunodeficiency/HIV and hematological diseases were not significant risk factors (OR: 1.030, 1.115 and 1.182; p = 0.706, 0.290 and 0.194, respectively). The first two variables had a P value > 0.25, so these were excluded from multivariate analysis.
Table 2.
Descriptive data and univariable derived odds ratio of different variables for mortality amongst hospitalized COVID-19 patients (n = 64,427; deceased = 6756, discharged = 57,671)
| Variable | N | % of death | OR | 95% CI | Pa | |
|---|---|---|---|---|---|---|
| + | − | |||||
| Gender | ||||||
| Male | 33,577 | 11.56% | 88.44% | 1.273 | 1.210–1.340 | < 0.0001 |
| Female (reference) | 30,850 | 9.31% | 90.69% | |||
| Age | – | 68.27 ± 15.72 | 54.71 ± 18.19 | 1.045 | 1.044–1.047 | < 0.0001 |
| Health care worker | ||||||
| Positive | 564 | 3.55% | 96.45% | 0.312 | 0.199–0.487 | < 0.0001 |
| Negative | 63,863 | 10.55% | 89.45% | |||
| History of smoking | ||||||
| Positive | 1787 | 10.76% | 89.24% | 1.030 | 0.885–1.199 | 0.706 |
| Negative | 62,642 | 10.48% | 89.52% | |||
| History of opium abuse | ||||||
| Positive | 2030 | 12.81% | 87.19% | 1.264 | 1.107–1.443 | 0.001 |
| Negative | 62,397 | 10.41% | 89.59% | |||
| HIV or immunodeficiency | ||||||
| Positive | 521 | 11.90% | 88.10% | 1.155 | 0.885–1.507 | 0.290 |
| Negative | 63,906 | 10.47% | 89.53% | |||
| Pulmonary diseases | ||||||
| Positive | 3079 | 13.54% | 86.46% | 1.359 | 1.222–1.512 | < 0.0001 |
| Negative | 61,348 | 10.33% | 89.67% | |||
| Cancer | ||||||
| Positive | 2355 | 17.92% | 82.08% | 1.921 | 1.724–2.141 | < 0.0001 |
| Negative | 62,072 | 10.20% | 89.80% | |||
| Thyroid diseases | ||||||
| Positive | 23,595 | 6.87% | 93.13% | 0.513 | 0.484–0.544 | < 0.0001 |
| Negative | 40,832 | 12.58% | 87.42% | |||
| Hematological diseases | ||||||
| Positive | 568 | 12.15% | 87.85% | 1.182 | 0.918–1.523 | 0.194 |
| Negative | 63,859 | 10.47% | 89.53% | |||
| Hepatic diseases | ||||||
| Positive | 676 | 21.30% | 79.70% | 2.339 | 1.942 -2.817 | < 0.0001 |
| Negative | 63,751 | 10.37% | 89.63% | |||
| Nephrological diseases | ||||||
| Positive | 2478 | 18.20% | 81.80% | 1.964 | 1.767–2.182 | < 0.0001 |
| Negative | 61,949 | 10.18% | 89.82% | |||
| Neurological diseases | ||||||
| Positive | 1866 | 20.10% | 79.90% | 2.214 | 1.972–2.487 | < 0.0001 |
| Negative | 62,561 | 10.20% | 89.80% | |||
| Hyperlipidemia | ||||||
| Positive | 940 | 13.72% | 86.28% | 1.365 | 1.131–1.646 | 0.001 |
| Negative | 63,487 | 10.44% | 89.56% | |||
| Diabetes | ||||||
| Positive | 10,208 | 16.17% | 83.83% | 1.856 | 1.748–1.971 | < 0.0001 |
| Negative | 54,219 | 9.42% | 90.58% | |||
| Cardiovascular disease | ||||||
| Positive | 9142 | 17.52% | 82.48% | 2.065 | 1.942–2.195 | < 0.0001 |
| Negative | 55,285 | 9.32% | 90.68% | |||
| Hypertension | ||||||
| Positive | 14,425 | 16.01% | 83.99% | 1.954 | 1.851–2.062 | < 0.0001 |
| Negative | 50,002 | 8.89% | 91.11% | |||
Bold values indicate statistically significant
aUnivariate logistic regression
The results of univariable and multivariable risk analysis using Poisson regression with robust standard errors are shown in Table 3. According to the multivariable analysis, we found that the positive history of opium abuse was significantly an independent risk factor for mortality amongst hospitalized adult COVID-19 patients (adjusted RR: 1.173; p = 0.007). In addition, controlling the confounding variables, male or elder patients had higher risk of mortality (adjusted RR: 1.036, 1.218; p < 0.0001, < 0.0001). Considering comorbidities, pulmonary diseases, cancer, hepatic diseases, nephrological diseases, neurological diseases, diabetes, and cardiovascular disease were significantly associated with mortality (Table 3). Of note, hepatic diseases had the highest, more than 120%, increase in risk of mortality amongst hospitalized patients (adjusted RR: 2.211; p = 0.007). Interestingly, being a health care worker or have a thyroid gland disease were protective factors for mortality (adjusted RR: 0.650, 0.642; p = 0.040, < 0.0001). Furthermore, while hyperlipidemia and hypertension were associated with mortality in univariable analysis (RR: 1.315, 1.801; p = 0.001, < 0.0001), they were not independent predictive variable for mortality in multivariable analysis (adjusted RR: 0.925, 1.048; p = 0.343, 0.073).
Table 3.
Relative risks (RR) of different variables for mortality amongst hospitalized COVID-19 patients (n = 64,427; deceased = 6756, discharged = 57,671) using Poisson regression with robust standard errors
| Variable | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| RR | 95% CI | Pa | RR | 95% CI | Pa | |
| Age | 1.039 | 1.038–1.041 | < 0.0001 | 1.036 | 1.035–1.038 | < 0.0001 |
| Gender [reference = female] | 1.242 | 1.186–1.300 | < 0.0001 | 1.218 | 1.164–1.274 | < 0.0001 |
| Health care worker | 0.336 | 0.218–0.517 | < 0.0001 | 0.650 | 0.431–0.981 | 0.040 |
| History of opium abuse | 1.230 | 1.096–1.381 | < 0.001 | 1.173 | 1.044–1.312 | 0.007 |
| Pulmonary diseases | 1.311 | 1.195–1.437 | < 0.0001 | 1.162 | 1.062–1.272 | 0.001 |
| Cancer | 1.756 | 1.606–1.921 | < 0.0001 | 1.742 | 1.590–1.908 | < 0.0001 |
| Thyroid diseases | 0.545 | 0.518–0.576 | < 0.0001 | 0.642 | 0.609–0.677 | < 0.0001 |
| Hematological diseases | 1.160 | 0.929–1.449 | 0.191 | 1.093 | 0.873–1.368 | 0.436 |
| Hepatic diseases | 2.054 | 1.774 -2.378 | < 0.0001 | 2.211 | 1.902–2.570 | < 0.0001 |
| Nephrological diseases | 1.788 | 1.640–1.950 | < 0.0001 | 1.431 | 1.312–1.562 | < 0.0001 |
| Neurological diseases | 1.970 | 1.795–2.163 | < 0.0001 | 1.343 | 1.222–1.476 | < 0.0001 |
| Hyperlipidemia | 1.315 | 1.118–1.546 | 0.001 | 0.925 | 0.789–1.086 | 0.343 |
| Diabetes | 1.718 | 1.632–1.808 | < 0.0001 | 1.311 | 1.242–1.384 | < 0.0001 |
| Cardiovascular disease | 1.878 | 1.784–1.977 | < 0.0001 | 1.138 | 1.078–1.202 | < 0.0001 |
| Hypertension | 1.801 | 1.719–1.887 | < 0.0001 | 1.048 | 0.999–1.103 | 0.073 |
| Intercept | – | – | – | 0.010 | 0.009–0.011 | < 0.0001 |
Bold values indicate statistically significant
aPoisson regression with robust standard errors
Discussion
Following the COVID-19 pandemic, research on the impact of drug abuse/smoking or other substance abuse on the outcome of COVID-19 infection outlook has been an area of interest for the research groups. The current study examined the relationship between opium abuse and mortality amongst 64,427 COVID-19 hospitalized patients. According to the findings, opium abuser patients had a 17% higher risk for mortality. In addition, male gender, higher ages and the underlying diseases such as cardiovascular disease, diabetes, cancer, hepatic disease, were significant risk factors for mortality; but hyperlipidemia and hypertension were not found to be significant risk factors.
While the reasons of just-mentioned 17% increase in risk of mortality amongst hospitalized COVID-19 patients who were opium abuser is not clear, it might have something to do with immune system, serum factors and inflammatory biomarkers. Opium contains approximately 20 alkaloids and over 70 other components that can suppress the immune system and increase inflammation (Karam et al., 2004). In this respect, previous studies showed that the levels of most cytokines were changed in opium users—lower levels of IL-4 and higher levels of IL-6 compared to the controls (Nabati et al., 2013; Pirnia et al., 2020). In addition, it has been shown that mortality in COVID-19 patients is linked to the cytokine storm, driven by high levels of interleukin-6 (IL-6) (Nabati et al., 2013; Mahdavi & Aliramezany, 2021). Another possible explanation is about the effect of opium on some serum factors, i.e., HDL, potassium, Fe2+ and TIBC (Total Iron Binding Capacity), which may increase mortality, indirectly (Karam et al., 2004). It is sophisticated to explain this result, but Asadi Karam and colleagues showed that opium decreases HDL, which increases the risk for atherosclerosis. Opium increases serum potassium, which may interfere with water regulation and blood pressure. Furthermore, in males, Fe2 + is shown to be higher in diabetic addicts than non-addicted diabetics (p = 0.0141), but TIBC was lower in diabetic addicts than diabetic non-addicts (p = 0.0098). A previous study found that having a high serum iron level was associated with an increased risk of mortality (Corti et al., 1997; Lan et al., 2018). Furthermore, serum CRP (C-Reactive Protein) levels in opium abusers were shown to be 12-fold greater than controls (Ghazavi et al., 2013). As a result, opium may exacerbate inflammatory responses. However, to draw the full picture of opium abuse and morality in COVID-19 infection, more studies are warranted.
Such risk factors, independent of opium abuse, may increase the risk of COVID-19 mortality. The current study showed that underlying diseases such as cardiovascular disease, diabetes, cancer, and hepatic disease, were significant risk factors for COVID-19 mortality. In this regard, hepatic and neurological diseases had highest odds ratios (OR: 2.3 and OR: 2.2). This finding could be explained by the fact that some patients with hepatic and neurological diseases had poor prognoses due to malnutrition and lack of appropriate treatment. According to a meta-analysiss, the pooled odds ratios for hypertension, respiratory system disease, and cardiovascular diseases in severe COVID-19 were 2.36, 2.46, and 3.42, respectively, when compared to non-severe patients (Yang et al., 2020b). What is surprising is that hypertension and hyperlipidemia were not significant independent predictive factors for COVID-19 mortality in multivariate analysis. However, in the univariate analysis, hypertension and hyperlipidemia were significant risk factors for COVID-19 mortality. Previous research has linked hypertension by a 2.5-fold increase with the risk of COVID-19 mortality, particularly in elderly (Lippi et al., 2020; Escobedo-de la Peña et al., 2021). This discrepancy result is difficult to explain; it could be attributed to a variety of mechanisms, including angioplasty-converting enzyme 2 (ACE2) receptors, the NADH/NADPH oxidase system, and the inflammatory response and cytokine storm affected by COVID-19 and hypertension. Further biologic and clinical researches are needed to determine the exact mechanisms by which hypertension is linked to the risk of COVID-19 infection and mortality outcomes. Hence, these results should be interpreted with caution. Moreover, male gender was a risk factor for COVID-19 mortality, which is consistent with previous studies (Nguyen et al., 2021). It should be noticed that the age distribution of opium abuser COVID-19 hospitalized patients was bell-shaped, with a mean of 57 ± 17.21 years; that is higher than that of the general population (33.9 years) (Ahmadi et al., 2007). This result might be explained by the fact that the rate of hospitalization due to COVID-19 infection increases with age In addition, the current study found that elderly was a significant risk factor for COVID-19 mortality. One possible explanation for this is that elder patients had other co-morbidities at the time of the infection.
Being a health care worker or having a thyroid gland disease was a protective factor amongst hospitalized COVID-19 patients in current study. It appears that these findings are the result of higher health literacy among health care worker than in the general population. According to a systematic review and meta-analysis, the Iranian population's, health literacy was inadequate and borderline. However, the overall level of health literacy among all health care worker was good to moderate (Dadipoor et al., 2018). Despite the findings of the current study, previous research has shown that thyroid gland diseases increased the risk of COVID-19 poor outcomes and were influenced by the patient's age (Damara et al., 2021). This is a difficult finding to explain, but it could be related to the current study's lack of detailed data collection. Hypothyroidism, hyperthyroidism, and other conditions are not distinguished in this regard.
Although the large sample size might be the most important strength of the present study, this historical cohort study is inherently limited by absence of data on independent variables such as education level, socio economic status, BMI, etc. that potentially could influence the interpretation of the findings.
Conclusion
Despite a part of community belief that opium use is beneficial in preventing COVID-19 infection, we found that opium abuse is a risk factor for mortality amongst hospitalized COVID-19 patients. Opium use is illegal and a major issue in society and government policy, but there was no clear response to the community's belief. In clinical practice, expert opinion and health workers' opinion about the benefits and drawbacks of opium use, as a primary role group in society, can have a significant influence on public belief. We strongly suggest to educate the general population for the risks of unauthorized opium consumption, especially during COVID-19 pandemic. As part of the strategy to control the pandemic in access to healthcare support, it is necessary to highlight the need to screen and treat individuals who abuse opium.
Acknowledgements
We gratefully acknowledge the manager and staff of the Medical Care Monitoring Center (MCMC), which is affiliated with Shiraz University of Medical Sciences, for providing data.
Appendix 1
R codes for univariate logistic regression and univariate and multivariate Poisson regression model with robust standard errors
|
> data <—read.csv("…/data.csv") > attach(data) > library(sandwich) > library(lmtest) > fit_log_1 = glm(outlook ~ var.1, family = binomial(link = 'logit')) ### Iterating univariate logistic regression for each variable |
|
> log2prob = function(log_){return(exp(log_))} ### Returning logs of estimated coefficients > summary(fit_log_1) > log2prob(coef(fit_log_1)) ### Returning ORs > exp(coefci(fit_log_1)) ### Returning 95% Cis > fit_poi_1 = glm(outlook ~ var.1, family = poisson(link = 'log')) ### Iterating univariate Poisson regression model for each variable with P < 0.25 in univariate logistic regression > fit_robust_1 = coeftest(fit_poi_1, vcov = sandwich) ### Iterating univariate Poisson regression model with robust standard errors for each variable with P < 0.25 in univariate logistic regression > fit_robust_1 > log2prob(fit_robust_1) > log2prob(coef(fit_robust_1)) > log2prob(confint(fit_robust_1)) > fit_poi_n = glm(outlook ~ age + gender + health_staff + hx_opium + respiratory_dx + cancer + thyroid_dx + blood_dx + liver_dx + kidney_dx + neuro_dx + hyperlipidemia + diabetes + CVD + HTN, family = poisson(link = 'log')) ### Fitting multivariate Poisson regression model on variables with P < 0.25 in univariate logistic regression fit_robust_n = coeftest(fit_poi_n, vcov = sandwich) > fit_robust_n > log2prob(fit_robust_n) > log2prob(coef(fit_robust_n)) > log2prob(confint(fit_robust_n)) |
Author Contributions
Each named author has substantially contributed to conducting the underlying research and drafting this manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Data Availability
Data is available if needed.
Declarations
Conflict of Interest
The Authors declare that there is no competing interest.
Ethical Approval
This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. This study was approved by Shiraz University of Medical Sciences Local Ethics Committee by the code: IR.SUMS.REC.1399.1165.
Consent to Participate
Written informed consent forms were obtained from each participant.
Consent for Publication
All of the authors have approved the contents of this paper and have agreed to the submission policies. Also, each of the authors confirms that this manuscript has not been previously published and is not currently under consideration by any other journal.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Alireza Mirahmadizadeh, Email: mirahmadia@sums.ac.ir.
Alireza Heiran, Email: heiran.alireza@gmail.com.
Amineh Dadvar, Email: dadvara@sums.ac.ir.
Mohammad Javad Moradian, Email: drmoradian@sums.ac.ir.
Mohammad Hossein Sharifi, Email: mhsharifi1350@gmail.com.
Roya Sahebi, Email: rasahebi@yahoo.com.
References
- Adib A, Masoompour SM, Vardanjani HM, Gondomkar A, Poustchi H, Salehi A, et al. Smoking water-pipe, opium use and prevalence of heart disease: A cross-sectional analysis of baseline data from the Pars Cohort Study Southern Iran. Archives of Iranian Medicine. 2020;23(5):289–295. doi: 10.34172/aim.2020.17. [DOI] [PubMed] [Google Scholar]
- Ahmadi J, Pridmore S, Alimi A, Cheraghi A, Arad A, Parsaeyan H, et al. Epidemiology of opium use in the general population. The American Journal of Drug and Alcohol Abuse. 2007;33(3):483–491. doi: 10.1080/00952990701301293. [DOI] [PubMed] [Google Scholar]
- Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code for Biology and Medicine. 2008;3(1):1–8. doi: 10.1186/1751-0473-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corti MC, Guralnik JM, Salive ME, Ferrucci L, Pahor M, Wallace RB, et al. Serum iron level, coronary artery disease, and all-cause mortality in older men and women. American Journal of Cardiology. 1997;79(2):120–127. doi: 10.1016/S0002-9149(96)00697-2. [DOI] [PubMed] [Google Scholar]
- Dadipoor S, Ramezankhani A, Aghamolaei T, Rakhshani F, Safari-Moradabadi A. Evaluation of health literacy in the Iranian population. Health Scope. 2018;7(3):e62212. [Google Scholar]
- Damara FA, Muchamad GR, Ikhsani R, Syafiyah AH, Bashari MH. Thyroid disease and hypothyroidism are associated with poor COVID-19 outcomes: A systematic review, meta-analysis, and meta-regression. Diabetes Metab Syndr. 2021;15(6):102312. doi: 10.1016/j.dsx.2021.102312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DRUGS UNOO, LABOR. WORLD DRUG REPORT 2020 (SET OF 6 BOOKLETS): UN, 2021.
- Dubey MJ, Ghosh R, Chatterjee S, Biswas P, Chatterjee S, Dubey S. COVID-19 and addiction. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2020;14(5):817–823. doi: 10.1016/j.dsx.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escobedo-de-la Peña J, Rascón-Pacheco RA, de Ascencio-Montiel IJ, González-Figueroa E, Fernández-Gárate JE, Medina-Gómez OS, Borja-Bustamante P, Santillán-Oropeza JA, Borja-Aburto VH. Hypertension, diabetes and obesity, major risk factors for death in patients with COVID-19 in Mexico. Archives of Medical Research. 2021;52(4):443–9. doi: 10.1016/j.arcmed.2020.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farahani MA, Ghaffari F, Fatemi NS. Opium addiction in patients with coronary artery disease: A grounded theory study. Medical Journal of the Islamic Republic of Iran. 2015;29:267. [PMC free article] [PubMed] [Google Scholar]
- Ghazavi A, Mosayebi G, Solhi H, Rafiei M, Moazzeni SM. Serum markers of inflammation and oxidative stress in chronic opium (Taryak) smokers. Immunology Letters. 2013;153(1–2):22–26. doi: 10.1016/j.imlet.2013.07.001. [DOI] [PubMed] [Google Scholar]
- Hasandokht T, Salari A, Pour SS, Tirani HD, Shad B, Rajabi E. Does opium have benefit for coronary artery disease? A systematic review. Research in Cardiovascular Medicine. 2018;7(2):51. doi: 10.4103/rcm.rcm_12_17. [DOI] [Google Scholar]
- Ignaszewski MJ. The epidemiology of drug abuse. Journal of Clinical Pharmacology. 2021;61(Suppl 2):S10–S17. doi: 10.1002/jcph.1937. [DOI] [PubMed] [Google Scholar]
- Karam GA, Reisi M, Kaseb AA, Khaksari M, Mohammadi A, Mahmoodi M. Effects of opium addiction on some serum factors in addicts with non-insulin-dependent diabetes mellitus. Addiction Biology. 2004;9(1):53–58. doi: 10.1080/13556210410001674095. [DOI] [PubMed] [Google Scholar]
- Knol MJ, Le Cessie S, Algra A, Vandenbroucke JP, Groenwold RH. Overestimation of risk ratios by odds ratios in trials and cohort studies: Alternatives to logistic regression. CMAJ. 2012;184(8):895–899. doi: 10.1503/cmaj.101715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lan P, Pan KH, Wang SJ, Shi QC, Yu YX, Fu Y, et al. High serum iron level is associated with increased mortality in patients with sepsis. Science and Reports. 2018;8(1):11072. doi: 10.1038/s41598-018-29353-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lippi G, Wong J, Henry BM. Hypertension and its severity or mortality in Coronavirus Disease 2019 (COVID-19): A pooled analysis. Pol Arch Intern Med. 2020;130(4):304–309. doi: 10.20452/pamw.15272. [DOI] [PubMed] [Google Scholar]
- Mahdavi A, Aliramezany M. Addiction and Covid-19 disease: Risks and misconceptions. Addiction and Health. 2021;13(1):66–67. doi: 10.22122/ahj.v13i1.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nabati S, Asadikaram G, Arababadi MK, Shahabinejad G, Rezaeian M, Mahmoodi M, et al. The plasma levels of the cytokines in opium-addicts and the effects of opium on the cytokines secretion by their lymphocytes. Immunology Letters. 2013;152(1):42–46. doi: 10.1016/j.imlet.2013.04.003. [DOI] [PubMed] [Google Scholar]
- Nakhaee S, Ghasemi S, Karimzadeh K, Zamani N, Alinejad-Mofrad S, Mehrpour O. The effects of opium on the cardiovascular system: A review of side effects, uses, and potential mechanisms. Substance Abuse Treatment, Prevention, and Policy. 2020;15(1):30. doi: 10.1186/s13011-020-00272-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen NT, Chinn J, De Ferrante M, Kirby KA, Hohmann SF, Amin A. Male gender is a predictor of higher mortality in hospitalized adults with COVID-19. PLoS ONE. 2021;16(7):e0254066. doi: 10.1371/journal.pone.0254066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patanavanich R, Glantz SA. Smoking is associated with COVID-19 progression: A meta-analysis. Nicotine and Tobacco Research. 2020;22(9):1653–1656. doi: 10.1093/ntr/ntaa082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirnia B, Dezhakam H, Pirnia K, Malekanmehr P, Soleimani AA, Zahiroddin A, et al. COVID-19 pandemic and addiction: Current problems in Iran. Asian Journal of Psychiatry. 2020;54:102313. doi: 10.1016/j.ajp.2020.102313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riahi T, Sadeghzadeh-Bazargan A, Shokri S, Ahmadvand D, Hassanlouei B, Baghestani A, et al. The effect of opium on severity of COVID-19 infection: An original study from Iran. Medical Journal of the Islamic Republic of Iran (MJIRI). 2021;35(1):870–874. doi: 10.47176/mjiri.35.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanyaolu A, Okorie C, Marinkovic A, Patidar R, Younis K, Desai P, et al. Comorbidity and its impact on patients with COVID-19. SN Comprehensive Clinical Medicine. 2020;2(8):1069–1076. doi: 10.1007/s42399-020-00363-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: A systematic review and meta-analysis. International Journal of Infectious Diseases. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. International Journal of Infectious Diseases. 2020;10(10):1016. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaki N, Alashwal H, Ibrahim S. Association of hypertension, diabetes, stroke, cancer, kidney disease, and high-cholesterol with COVID-19 disease severity and fatality: A systematic review. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2020;14(5):1133–1142. doi: 10.1016/j.dsx.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is available if needed.


